Abstract
Objective
To estimate health care and health-related productivity costs associated with excessive sedentary behaviour (> 8 h/day and > 9 h/day) in Canadian adults.
Methods
Three pieces of information were used to estimate costs: (1) the pooled relative risk estimates of adverse health outcomes consistently shown to be associated with excessive sedentary behaviour, gathered from meta-analyses of prospective cohort studies; (2) the prevalence of excessive sedentary behaviour in Canadian men and women, obtained using waist-worn accelerometry in a nationally representative sample of adults (Canadian Health Measures Survey 2018–2019); and (3) the direct (health care) and indirect (lost productivity due to premature mortality) costs of the adverse health outcomes, selected using the Economic Burden of Illness in Canada 2010 data. The 2010 costs were then adjusted to 2021 costs to account for inflation, population growth, and higher average earnings. A Monte Carlo simulation was conducted to account for uncertainty in the model.
Results
The total costs of excessive sedentary behaviour in Canada were $2.2 billion (8 h/day cut-point) and $1.8 billion (9 h/day cut-point) in 2021, representing 1.6% and 1.3% of the overall burden of illness costs, respectively. The two most expensive chronic diseases attributable to excessive sedentary behaviour were cardiovascular disease and type 2 diabetes. A 10% decrease in excessive sedentary behaviour (from 87.7% to 77.7%) would save an estimated $219 million per year in costs.
Conclusion
Excessive sedentary behaviour significantly contributes to the economic burden of illness in Canada. There is a need for evidence-based and cost-effective strategies that reduce excessive sedentary behaviour in the population.
Keywords: Sedentary time, Sedentariness, Sitting time, Economic cost, Health care cost, Public health
Résumé
Objectif
Estimer le coût des soins de santé et le coût de productivité lié à la santé associés au comportement sédentaire excessif (> 8 heures/jour et > 9 heures/jour) chez les Canadiennes et les Canadiens adultes.
Méthode
Trois informations ont servi à estimer ces coûts : 1) les estimations combinées du risque relatif des résultats sanitaires indésirables uniformément associés au comportement sédentaire excessif, collectées à partir de méta-analyses d’études prospectives de cohortes; 2) la prévalence du comportement sédentaire excessif chez les Canadiennes et les Canadiens, obtenue à l’aide d’un accéléromètre porté à la taille par un échantillon représentatif national d’adultes (Enquête canadienne sur les mesures de la santé 2018-2019); et 3) les coûts directs (soins de santé) et indirects (perte de productivité due à la mortalité prématurée) des résultats sanitaires indésirables sélectionnés, d’après les données du Fardeau économique de la maladie au Canada de 2010. Les coûts de 2010 ont ensuite été ajustés aux coûts de 2021 pour tenir compte de l’inflation, de la croissance démographique et de la hausse moyenne des revenus. Nous avons effectué une simulation de Monte-Carlo pour tenir compte de l’incertitude du modèle.
Résultats
Les coûts totaux du comportement sédentaire excessif au Canada étaient de 2,2 milliards de dollars (point de coupure de 8 heures/jour) et de 1,8 milliard de dollars (point de coupure de 9 heures/jour) en 2021, ce qui représente 1,6 % et 1,3 % du fardeau global des coûts des maladies, respectivement. Les deux maladies chroniques les plus chères imputables au comportement sédentaire excessif étaient les maladies cardiovasculaires et le diabète de type 2. Une baisse de 10 % du comportement sédentaire excessif (de 87,7 % à 77,7 %) économiserait environ 219 millions de dollars de coûts par année.
Conclusion
Le comportement sédentaire excessif contribue de façon significative au fardeau économique de la maladie au Canada. Il nous faut des stratégies fondées sur les preuves et efficaces par rapport au coût pour réduire le comportement sédentaire excessif dans la population.
Mots-clés: Temps de sédentarité, sédentarité, temps passé assis, coût économique, coût des soins de santé, santé publique
Introduction
Sedentary behaviour is defined as “any waking behaviour characterized by an energy expenditure ≤1.5 metabolic equivalents (METs), while in a sitting, reclining or lying posture” (Tremblay et al. 2017). In contrast, physical inactivity is a term used to identify individuals who do not get the recommended level of regular physical activity (e.g., at least 150 min per week of moderate-to-vigorous physical activity). Excessive time spent sedentary is highly prevalent, with the average Canadian adult spending 9–10 h per day engaging in sedentary behaviours (Prince et al. 2020). The health impact of excessive sedentary behaviour has been extensively studied in recent years (Katzmarzyk et al. 2019; Saunders et al. 2020; Dempsey et al. 2020a), prompting the development and release of the first global sedentary behaviour guidelines by the World Health Organization in 2020 (Bull et al. 2020).
Although excessive sedentary behaviour is a highly prevalent and modifiable risk factor, data on its economic burden are largely nonexistent. Nguyen et al. (2022) recently published a systematic review on the economics of sedentary behaviour and only found three studies that examined health care costs associated with excessive sedentary behaviour. Available studies were from Australia, China, and the United Kingdom and reported important health care costs. Quantifying the economic burden associated with excessive sedentary behaviour in Canada is needed and could help policy makers make informed decisions about the funding of health care priorities. In particular, estimating costs that could be avoided by reducing sedentary behaviour in the population could inform investments in evidence-based intervention strategies.
This study aimed to provide national estimates of health care and health-related productivity costs associated with excessive sedentary behaviour in Canadian adults. Another aim was to estimate costs that could be avoided if the prevalence of excessive sedentary behaviour in the population was reduced by 10%.
Methods
The economic costs associated with excessive sedentary behaviour in Canadian adults in 2021 were calculated using a prevalence-based approach. Three key pieces of information were used to generate the cost estimates: (i) the pooled relative risk (RR) estimates of health outcomes consistently associated with excessive sedentary behaviour in adults; (ii) the prevalence of sedentary behaviour in Canadian adults; and (iii) the direct and indirect costs of these health outcomes. This prevalence-based approach has been instrumental in estimating the economic costs of many public health issues in Canada such as obesity (Katzmarzyk and Janssen 2004), physical inactivity (Janssen 2012), and short sleep duration (Chaput et al. 2022). Using the same methodology as in previous studies allows comparisons across risk factors in Canada. The methodology used to calculate cost estimates of sedentary behaviour in Canada is described.
Step 1
The first step aimed to retrieve, from the available literature, the pooled RR estimates of adverse health outcomes consistently shown to be associated with excessive sedentary behaviour in adults. The pooled RR is defined as the probability of having a selected illness for those with excessive sedentary behaviour divided by the probability of having the selected illness for those who do not have excessive sedentary behaviour. To do so, we first examined the meta-analyses of prospective cohort studies used for the 2018 US Physical Activity Guidelines Advisory Committee Scientific Report (Katzmarzyk et al. 2019; Physical Activity Guidelines Advisory Committee 2018), the 2020 Canadian 24-Hour Movement Guidelines for Adults (Saunders et al. 2020; Ross et al. 2020), and the 2020 World Health Organization guidelines on physical activity and sedentary behaviour (Dempsey et al. 2020a; Bull et al. 2020). We also conducted an updated search in PubMed for systematic reviews published in the past 2 years. We extracted the RR estimates of the following eight health outcomes: cardiovascular disease (Jingjie et al. 2022), type 2 diabetes (Bailey et al. 2019), colorectal cancer (Shen et al. 2014), endometrial cancer (Shen et al. 2014), lung cancer (Shen et al. 2014), breast cancer (Shen et al. 2014), dementia (Yan et al. 2020), and depression (Zhai et al. 2015). Other health outcomes were considered but were ultimately not included in this cost analysis due to their lack of consistent association with sedentary behaviour including obesity (Thorp et al. 2011), osteoporosis (McMichan et al. 2021), musculoskeletal pain (Castro et al. 2018), and outcomes that do not have burden of illness costs available (e.g., cognitive function or quality of life). Of note, the pooled RR estimates used in this cost analysis were derived from fully adjusted models calculated with random-effects models. Covariates in the models included sociodemographic characteristics (age, sex, socioeconomic status, ethnoracial background, marital status), lifestyle behaviours (cigarette smoking, alcohol consumption, physical activity level, sleep, eating habits), body mass index, chronic diseases, medication use, mental health, and history of health problems. Detailed information can be found elsewhere (Jingjie et al. 2022; Bailey et al. 2019; Shen et al. 2014; Yan et al. 2020; Zhai et al. 2015). Sedentary behaviour was assessed using self-reports and device-based measures in the primary studies, and pooled RR estimates were computed by comparing the highest versus lowest sedentary behaviour categories.
Step 2
The second step calculated the population attributable risk (PAR%) for each health outcome to estimate the proportion of the eight health outcomes explained by excessive sedentary behaviour in Canadian adults. The PAR% combines the pooled RR estimate with the population prevalence (P) of excessive sedentary behaviour using the following formula:
The prevalence of excessive sedentary behaviour in Canadians aged 18 years and older was obtained from the Canadian Health Measures Survey (CHMS), which provides nationally representative estimates. CHMS cycle 6 (2018–2019) was used as this is the most recent available cycle. Briefly, participants wore an Actical accelerometer (Philips Respironics, OR, USA) over their right hip for 7 consecutive days while awake. A minimum of four valid days of accelerometer data, defined as 10 or more hours of wear time while awake, were needed for inclusion (Colley et al. 2011; Wong et al. 2011). Data were collected in 1-min epochs, and non-wear time was defined as 60 consecutive minutes or more of zero counts, with an allowance of up to 2 min of counts between 0 and 100. The number of wear time minutes when counts per minute were between 0 and 100 were summed to calculate time spent in sedentary behaviour (Puyau et al. 2004). Detailed information can be found elsewhere (Rollo et al. 2022).
Adults who engaged in more than 8 h per day of sedentary behaviour were considered to have excessive sedentary time, in agreement with the Canadian 24-Hour Movement Guidelines for Adults (Ross et al. 2020). A sensitivity analysis using a 9-h sedentary behaviour cutoff was also conducted because some dose-response meta-analyses suggest that a 9-h threshold may be more appropriate when dealing with accelerometer data (Saunders et al., 2020; Ekelund et al. 2019). It was found that 87.7% of Canadian adults accumulate > 8 h per day of sedentary behaviour (85.3% in men and 90.0% in women) and that 69.8% accumulate > 9 h per day (70.4% in men and 69.2% in women) (ParticipACTION 2021).
Step 3
The third and final step aimed to calculate how much of the direct (health care costs), indirect (lost productivity due to premature mortality), and total costs (direct + indirect costs) were attributable to excessive sedentary behaviour for each of the eight health outcomes. In this step, the PAR% for each health outcome was multiplied by the health care and productivity costs of that health outcome separately for men and women. We used the Economic Burden of Illness in Canada (EBIC) 2010 online tool to determine the overall direct and indirect costs (in Canadian dollars) of the eight health outcomes (https://www.canada.ca/en/public-health/services/chronic-diseases/chronic-disease-knowledge-development-exchange/economic-burden-illness-canada.html). Direct costs in EBIC include expenses related to physician care expenditures, hospital care expenditures, and prescription drug expenditures. Indirect costs in EBIC were limited to lost production due to premature mortality.
Adjustments
Differences between the ways diseases were defined in the EBIC online tool and our study necessitated adjustments. We summed the EBIC costs of “acute myocardial infarction” and “other ischemic heart diseases” to generate a broader cost for cardiovascular disease. We multiplied the broader “diabetes mellitus” costs in EBIC by 90% to generate a more specific cost for type 2 diabetes; this adjustment reflects that 90% of diabetes cases in Canada are type 2 (Diabetes in Canada 2017). We multiplied the broader “mood (affective) disorders” costs in EBIC by 91.4% to avoid overestimating the costs of depression as depression accounts for 91.4% of mood disorders in Canada (Pearson et al. 2013). The other health outcomes were comparable to the categories used in EBIC and did not require adjustment.
The 2010 costs reported in EBIC were adjusted to 2021 costs to account for inflation, population growth, and higher average earnings. For direct costs, the 2010 costs were increased by 17.3% to reflect the inflation in health care costs that occurred between 2010 and 2021 as reported in the Consumer Price Index (Statistics Canada 2022a). This was in turn increased by 13.5% to reflect the increase in the Canadian adult population that occurred between 2010 and 2021 (Statistics Canada 2022b). For indirect costs associated with premature mortality, the 2010 costs were increased by 13.6% to reflect the higher average earnings in Canadian adults in 2021 (Statistics Canada 2022c) and then by 13.5% to reflect population growth (Statistics Canada 2022b).
Monte Carlo simulation analysis
In order to account for uncertainty in our model, we conducted a Monte Carlo simulation. The simulations were based on a uniform distribution in the range of the 95% confidence intervals for each health outcome. We ran 1000 simulations and the simulation analysis only included the uncertainty surrounding the RR of the diseases. The prevalence estimates for sedentary behaviour were from a custom analysis completed for the adult ParticipACTION Report Card and the 95% confidence intervals were not presented. Similarly, the EBIC report does not include 95% confidence intervals and therefore uncertainty could not be accounted for in our model.
Impact of a theoretical decrease in sedentary behaviour on economic costs
We conducted an additional analysis to estimate the health care savings that would occur if there was a theoretical 10% decrease in the prevalence of excessive sedentary behaviour in Canadian adults. To do so, we reran the same calculations but replaced the prevalence estimates of sedentary behaviour (> 8 h/day) by the following estimates: 75.3% for men and 80.0% for women (decrease by 10%).
Results
Table 1 shows the pooled RR estimates for the eight health outcomes associated with excessive sedentary behaviour, as reported in recent meta-analyses of prospective cohort studies. The RR estimates ranged from an increase in risk of 13% (type 2 diabetes) to 30% (colorectal cancer and dementia) among adults with excessive sedentary behaviour compared to those with the lowest sedentary behaviour levels. Furthermore, the PAR% values in Table 2 indicate that between 10.0% (type 2 diabetes) and 20.4% (colorectal cancer and dementia) of the health outcomes were attributable to excessive sedentary behaviour among Canadian men, and that between 10.5% (type 2 diabetes) and 21.3% (colorectal cancer and dementia) of the health outcomes were attributable to excessive sedentary behaviour among Canadian women when an 8-h per day cutoff point was applied. When a 9-h per day cutoff point was applied to define excessive sedentary behaviour, between 8.4% (type 2 diabetes) and 17.4% (colorectal cancer and dementia) of the health outcomes were attributable to sedentary behaviour among men, and between 8.3% (type 2 diabetes) and 17.2% (colorectal cancer and dementia) of the health outcomes were attributable to sedentary behaviour among women.
Table 1.
Pooled relative risk (RR) estimates for the health outcomes associated with sedentary behaviour in recent meta-analyses of prospective cohort studies in adults
| Health outcome | RR (95% CI) |
|---|---|
| Cardiovascular disease1 | 1.29 (1.13–1.47) |
| Type 2 diabetes | 1.13 (1.04–1.22) |
| Colorectal cancer | 1.30 (1.12–1.49) |
| Endometrial cancer | 1.28 (1.08–1.53) |
| Lung cancer | 1.27 (1.06–1.52) |
| Breast cancer | 1.17 (1.03–1.33) |
| Dementia | 1.30 (1.12–1.51) |
| Depression | 1.14 (1.06–1.21) |
1Acute myocardial infarction, coronary heart disease, and stroke
RR, relative risk; CI, confidence interval
Table 2.
Population attributable risk (PAR%) estimates for the health outcomes associated with excessive sedentary behaviour in the Canadian adult population in 2018–2019
| > 8 h/day of sedentary time | > 9 h/day of sedentary time | |||
|---|---|---|---|---|
| PAR% | PAR% | PAR% | PAR% | |
| (men) | (women) | (men) | (women) | |
| Cardiovascular disease1 | 19.8 | 20.7 | 17.0 | 16.7 |
| Type 2 diabetes | 10.0 | 10.5 | 8.4 | 8.3 |
| Colorectal cancer | 20.4 | 21.3 | 17.4 | 17.2 |
| Endometrial cancer | N/A | 20.1 | N/A | 16.2 |
| Lung cancer | 18.7 | 19.5 | 16.0 | 15.9 |
| Breast cancer | 12.7 | 13.3 | 10.7 | 10.5 |
| Dementia | 20.4 | 21.3 | 17.4 | 17.2 |
| Depression | 10.7 | 11.2 | 9.0 | 8.8 |
1Acute myocardial infarction, coronary heart disease, and stroke
N/A, not applicable
Table 3 reports the direct (health care), indirect (lost productivity due to premature mortality), and total costs of excessive sedentary behaviour (> 8 h/day) among Canadian adults. The direct, indirect, and total costs of excessive sedentary behaviour in 2021 were $2.1 billion, $50.4 million, and $2.2 billion, respectively. The total cost of excessive sedentary behaviour represented 1.6% of the overall burden of illness costs for 2021. When a 9-h per day cutoff point was applied to define excessive sedentary behaviour (Table 4), the total costs was $1.8 billion, representing 1.3% of the overall burden of illness costs for 2021.
Table 3.
Direct, indirect, and total costs of excessive sedentary behaviour (> 8 h/day) in Canadian adults in 2021
| Cost attributable to excessive sedentary behaviour1 | % of overall cost attributable to excessive sedentary behaviour2 | |||||
|---|---|---|---|---|---|---|
| Sex | Direct | Indirect3 | Total | Direct | Indirect3 | Total |
| Men | 1157 (615–1618) | 35.2 (17.9–51.7) | 1192.2 (634.0–1669.8) | 1.9 | 5.7 | 1.9 |
| Women | 987 (581–1334) | 15.2 (7.9–22.6) | 1002.2 (591.8–1354.0) | 1.4 | 6.8 | 1.4 |
| Both | 2144 (1261–2974) | 50.4 (26.2–72.6) | 2194.4 (1292.4–3042.0) | 1.6 | 6.0 | 1.6 |
Data are presented as mean values, along with 95% confidence intervals from the Monte Carlo simulation
1Costs are in millions of Canadian dollars
2Calculated as cost attributable to sedentary behaviour in adults divided by overall cost in the population × 100
3Indirect costs include lost production due to premature mortality
Table 4.
Direct, indirect, and total costs of excessive sedentary behaviour (> 9 h/day) in Canadian adults in 2021
| Cost attributable to excessive sedentary behaviour1 | % of overall cost attributable to excessive sedentary behaviour2 | |||||
|---|---|---|---|---|---|---|
| Sex | Direct | Indirect3 | Total | Direct | Indirect3 | Total |
| Men | 985 (517–1392) | 30.1 (15.1–44.9) | 1015.1 (532.9–1436.9) | 1.6 | 4.9 | 1.6 |
| Women | 790 (459–1078) | 12.3 (6.2–18.5) | 802.3 (467.7–1094.2) | 1.1 | 5.5 | 1.1 |
| Both | 1175 (1034–2488) | 42.4 (21.7–61.8) | 1817.4 (1059.8–2545.6) | 1.3 | 5.0 | 1.3 |
Data are presented as mean values, along with 95% confidence intervals from the Monte Carlo simulation
1Costs are in millions of Canadian dollars
2Calculated as cost attributable to sedentary behaviour in adults divided by overall cost in the population × 100
3Indirect costs include lost production due to premature mortality
As reported in Table 5, the two most expensive chronic diseases attributable to excessive sedentary behaviour were cardiovascular disease ($748 million) and type 2 diabetes ($609 million). Similar findings were observed when a 9-h per day cutoff point was applied to define excessive sedentary behaviour (Table 6). The main contributors of health care (direct) costs were related to prescription drugs for type 2 diabetes and depression, and hospital care for cardiovascular disease, cancer (all types), and dementia (Table 7).
Table 5.
Direct, indirect, and total costs of excessive sedentary behaviour (> 8 h/day) for specific health outcomes in Canadian adults in 2021
| Health outcome | Cost attributable to excessive sedentary behaviour (> 8 h/day)1 | |||
|---|---|---|---|---|
| Direct | Indirect2 | Total | % of total cost | |
| Cardiovascular disease3 | 725.4 | 22.5 | 747.9 | 34.1 |
| Type 2 diabetes | 607.4 | 2.0 | 609.4 | 27.8 |
| Colorectal cancer | 141.2 | 6.3 | 147.5 | 6.7 |
| Endometrial cancer | 22.6 | 1.3 | 23.9 | 1.1 |
| Lung cancer | 115.5 | 14.9 | 130.4 | 5.9 |
| Breast cancer | 48.1 | 3.3 | 51.4 | 2.3 |
| Dementia | 161.6 | 0.2 | 161.8 | 7.4 |
| Depression | 322.3 | 0.02 | 322.3 | 14.7 |
1Costs are in millions of Canadian dollars
2Indirect costs include lost production due to premature mortality
3Acute myocardial infarction, coronary heart disease, and stroke
Table 6.
Direct, indirect, and total costs of excessive sedentary behaviour (> 9 h/day) for specific health outcomes in Canadian adults in 2021
| Health outcome | Cost attributable to excessive sedentary behaviour (> 9 h/day)1 | |||
|---|---|---|---|---|
| Direct | Indirect2 | Total | % of total cost | |
| Cardiovascular disease3 | 611.3 | 19.1 | 630.4 | 34.7 |
| Type 2 diabetes | 499.0 | 1.6 | 500.6 | 27.5 |
| Colorectal cancer | 118.2 | 5.2 | 123.4 | 6.8 |
| Endometrial cancer | 18.2 | 1.0 | 19.2 | 1.1 |
| Lung cancer | 96.9 | 12.5 | 109.4 | 6.0 |
| Breast cancer | 38.0 | 2.6 | 40.6 | 2.2 |
| Dementia | 133.8 | 0.2 | 134.0 | 7.4 |
| Depression | 259.6 | 0.01 | 259.6 | 14.3 |
1Costs are in millions of Canadian dollars
2Indirect costs include lost production due to premature mortality
3Acute myocardial infarction, coronary heart disease, and stroke
Table 7.
Contributors of direct (health care) costs and their relative contribution for each health outcome in Canadian adults
| Health outcome | Relative contribution (%) to the direct costs | ||
|---|---|---|---|
| Physician care | Hospital care | Prescription drugs | |
| Cardiovascular disease1 | 10.1 | 84.1 | 5.8 |
| Type 2 diabetes | 17.7 | 11.4 | 70.9 |
| Colorectal cancer | 15.9 | 82.1 | 2.0 |
| Endometrial cancer | 24.2 | 75.8 | 0 |
| Lung cancer | 17.3 | 73.0 | 9.7 |
| Breast cancer | 33.6 | 66.4 | 0 |
| Dementia | 29.8 | 59.4 | 10.8 |
| Depression | 22.5 | 34.3 | 43.2 |
1Acute myocardial infarction, coronary heart disease, and stroke
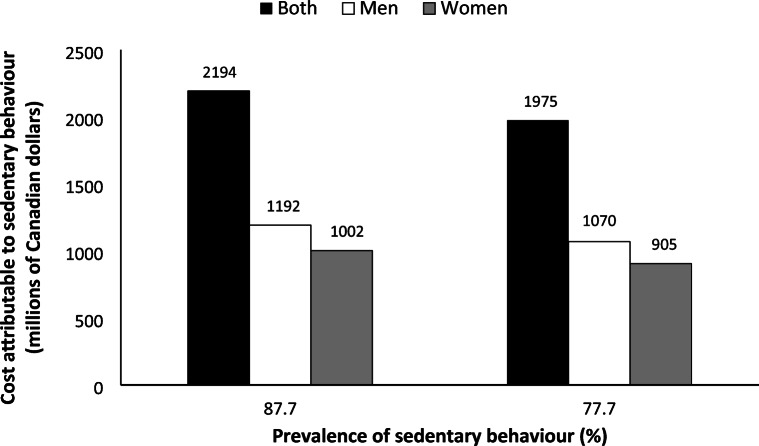
Figure 1 shows the potential costs that would be avoided if the prevalence of sedentary behaviour was reduced by 10% in the Canadian adult population. A 10% decrease in sedentary behaviour (from 87.7% to 77.7%) would result in an estimated $219 million per year in costs avoided, equivalent to a 10% cost reduction.
Fig. 1.
Projected economic costs attributable to excessive sedentary behaviour if the prevalence in Canadian adults decreased by 10% (from 87.7% to 77.7%)
Discussion
Findings from this cost analysis show that excessive sedentary behaviour significantly contributes to health care spending in Canada. Using an 8-h per day threshold, the total annual economic burden of excessive sedentary behaviour in Canadian adults is estimated at $2.2 billion, representing 1.6% of the overall burden of illness costs for 2021 in Canada. Using a 9-h per day threshold, the total annual economic burden of excessive sedentary behaviour is estimated at $1.8 billion, representing 1.3% of the overall burden of illness costs. Results from the Monte Carlo simulation analysis, that accounts for the uncertainty in the RR for the various health outcomes, show that the total costs of excessive sedentary behaviour in Canada ranged from $1.3 to $3.0 billion (8 h/day cut-point) and from $1.1 billion to $2.5 billion (9 h/day cut-point) in 2021. Finally, we estimated that $219 million per year would be saved if the prevalence of excessive sedentary behaviour in the population was reduced by 10%.
Studies providing economic costs associated with sedentary behaviour are scarce. In fact, only three studies were identified in a 2022 systematic review of this topic (Nguyen et al. 2022). Heron et al. (2019) estimated the total National Health Service costs attributable to prolonged sedentary behaviour (≥ 6 h/day) in the UK in 2016–2017 at £0.7 billion ($1.1 billion CAD). Yu and Schwingel (2019) reported that sedentary behaviour was associated with an increase in annual out-of-pocket health care expenditures of $37 USD ($48 CAD) for each additional sedentary hour in Chinese older adults. Finally, Peeters et al. (2014) estimated that the annual health care cost associated with high sedentary behaviour (> 8 h/day) was $1648 AU ($1474 CAD) per person. More recently, and after the publication of the above systematic review, Kolu et al. (2022) estimated that the total costs attributable to high sedentary behaviour (≥ 8 h/day) in Finland in 2017 was €1.5 billion ($2.0 billion CAD). The present study is the first to estimate economic costs associated with sedentary behaviour in Canada and will greatly contribute to the limited evidence base in the field.
Studies that have assessed the economic burden of sedentary behaviour (Heron et al. 2019; Yu and Schwingel 2019; Peeters et al. 2014; Kolu et al. 2022) vary in their methodology and it is difficult to compare cost estimates across countries. Fortunately, studies that have estimated the economic costs of other chronic disease risk factors in Canada (obesity [Katzmarzyk and Janssen 2004], physical inactivity [Janssen 2012], and insufficient sleep duration [Chaput et al. 2022]) have relied on the same methodological approach with EBIC data, thereby facilitating comparisons. As a matter of comparison, the total economic costs of physical inactivity ($6.8 billion CAD in 2009), obesity ($4.3 billion CAD in 2001), and insufficient sleep duration ($502 million CAD in 2020) have been estimated to represent 3.7%, 2.2%, and 0.5% of the overall burden of illness costs, respectively. Thus, the estimated $2.2 billion (8 h/day cut-point) or $1.8 billion (9 h/day cut-point) for excessive sedentary behaviour, representing 1.6% or 1.3% of the overall burden of illness costs, respectively, would place sedentary behaviour after obesity in terms of its percentage of overall burden of illness costs.
Cost-effective and evidence-based interventions aimed at reducing sedentary behaviour in the population are needed. Economic evaluations of interventions targeting sedentary behaviour reduction are limited, but most are likely to be cost-effective (Nguyen et al. 2022). The most promising interventions identified, from a cost-effectiveness standpoint, are those that include physical environmental changes in the workplace, such as sit-stand desks and active workstations (Nguyen et al. 2022). Given the high prevalence of sedentary behaviour, public health policy makers and employers are encouraged to make evidence-based decisions regarding the economic feasibility and scalability of reducing sitting time in specific settings and populations.
The mechanisms linking sedentary behaviour to chronic disease are still largely unknown (Dempsey et al. 2020b). More research is needed to examine the specific pathophysiological pathways through which sedentary behaviour may independently influence chronic disease risk, and to what extent the pathways differ with those associated with insufficient physical activity. Triangulation of evidence from observational, biological, behavioural, and experimental research will be needed to deepen our understanding of whether, how, and why sedentary behaviour is causally related to chronic disease (Dempsey et al. 2020b).
Behaviour change strategies used in sedentary behaviour reduction interventions among adults have been systematically reviewed (Gardner et al. 2016). Promising interventions tend to specifically target sedentary behaviour instead of physical activity and involve environmental restructuring, persuasion, or education. Self-monitoring, problem solving, and restructuring the social or physical environment appear to be promising behaviour change strategies (Gardner et al. 2016).
The prevalence of sedentary behaviour used in this study comes from cycle 6 of the CHMS (2018–2019). This is the most recent Canadian survey that provides nationally representative prevalence estimates of excessive sedentary behaviour using accelerometry. This means that the prevalence of excessive sedentary behaviour used in this cost analysis was based on data collected before the COVID-19 pandemic. Studies have reported substantial increases in sedentary behaviour during the COVID-19 pandemic. For example, a meta-analysis showed that adults increased their sedentary time by 127 min/day and older adults by 47 min/day during the pandemic, with no differences between men and women (Runacres et al. 2021). A higher prevalence of excessive sedentary behaviour would result in higher cost estimates, suggesting that the economic burden of sedentary behaviour during the COVID-19 pandemic is larger in magnitude than what is reported in this study. This observation highlights the importance of public health prevention strategies to effectively reduce sedentary time in the population.
An interesting aspect of this study was the projected costs that could be avoided by a 10% reduction in the prevalence of excessive sedentary behaviour. The observation that $219 million per year could be avoided is important and highlights the need to find ways to break up sitting time in the workplace and throughout the day to reduce time spent sedentary and its negative health consequences (Nguyen et al. 2022). Assessing the impact of populational changes in sedentary behaviour is important to inform policy makers about the funding of future health care priorities in a context of strong competition for preventive health funds.
Some limitations need to be considered when interpreting the findings of this study. First, cost estimates calculated with a prevalence-based approach rely on assumptions and may not reflect true costs; however, this is a common methodology in the field and has been used in Canada to estimate the economic burden of many other risk factors (Katzmarzyk and Janssen 2004; Janssen 2012; Chaput et al. 2022). Second, indirect costs in EBIC do not include costs related to lost productivity due to morbidity (e.g., presenteeism and absenteeism) or informal caregiving, suggesting that they are underestimated. Third, this cost analysis is for total sedentary behaviour and not for specific sedentary behaviours such as recreational screen time. Finally, this cost analysis relied on pooled RR estimates coming from different meta-analyses. Primary studies used different measurement tools to assess sedentary behaviour and different cutoff points for the comparisons. Cost estimates generated in the present study reflect this heterogeneity.
Conclusion
This study shows that excessive sedentary behaviour is an important contributor to health care spending in Canada, contributing to 1.3–1.6% of the overall burden of illness costs for 2021. Evidence-based and cost-effective strategies that aim to reduce sedentary behaviour in the population are warranted.
Contributions to knowledge
What does this study add to existing knowledge?
Excessive sedentary behaviour is a highly prevalent and modifiable risk factor; however, data on its economic burden are largely nonexistent. This study provides the first national estimates of health care and health-related productivity costs associated with excessive sedentary behaviour in Canadian adults.
The total costs of excessive sedentary behaviour in Canada were $2.2 billion (8 hours/day cut-point) and $1.8 billion (9 hours/day cut-point) in 2021, representing 1.6% and 1.3% of the overall burden of illness costs, respectively.
We also estimated that $219 million per year could be saved if the prevalence of excessive sedentary behaviour was reduced by 10% in the population.
What are the key implications for public health interventions, practice, or policy?
The economic burden of excessive sedentary behaviour is similar to the economic burden of obesity in Canada. This quantification of costs associated with excessive sedentary behaviour will help policy makers make informed decisions about the funding of health care priorities.
The costs that could be avoided by reducing sedentary behaviour in the population is helpful to inform investments in evidence-based intervention strategies.
Acknowledgements
Jean-Philippe Chaput is supported by the Canadian Institutes of Health Research and the CHEO Research Institute.
Author contributions
JPC, IJ, JJL, and HSK conceptualized the study; JPC analyzed the data; JPC drafted the manuscript; JPC, IJ, JJL, and HSK interpreted the data; and IJ, JJL, and HSK revised the manuscript critically for important intellectual content. All of the authors approved the final version submitted for publication.
Data availability
Data are publicly available at: https://www.canada.ca/en/public-health/services/chronic-diseases/chronic-disease-knowledge-development-exchange/economic-burden-illness-canada.html.
Declarations
Ethics approval
N/A
Code availability
N/A
Consent to participate
N/A
Consent for publication
N/A
Conflict of interest
The authors declare no competing interests.
Disclaimer
The content and views expressed in this article are those of the authors and do not necessarily reflect those of the Government of Canada.
Footnotes
Contributions to knowledge
What does this study add to existing knowledge?
• Excessive sedentary behaviour is a highly prevalent and modifiable risk factor; however, data on its economic burden are largely nonexistent. This study provides the first national estimates of health care and health-related productivity costs associated with excessive sedentary behaviour in Canadian adults.
• The total costs of excessive sedentary behaviour in Canada were $2.2 billion (8 h/day cut-point) and $1.8 billion (9 h/day cut-point) in 2021, representing 1.6% and 1.3% of the overall burden of illness costs, respectively.
• We also estimated that $219 million per year could be saved if the prevalence of excessive sedentary behaviour was reduced by 10% in the population.
What are the key implications for public health interventions, practice, or policy?
• The economic burden of excessive sedentary behaviour is similar to the economic burden of obesity in Canada. This quantification of costs associated with excessive sedentary behaviour will help policy makers make informed decisions about the funding of health care priorities.
• The costs that could be avoided by reducing sedentary behaviour in the population is helpful to inform investments in evidence-based intervention strategies.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Bailey DP, Hewson DJ, Champion RB, Sayegh SM. Sitting time and risk of cardiovascular disease and diabetes: A systematic review and meta-analysis. Am J Prev Med. 2019;57(3):408–416. doi: 10.1016/j.amepre.2019.04.015. [DOI] [PubMed] [Google Scholar]
- Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54(24):1451–1462. doi: 10.1136/bjsports-2020-102955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castro O, Bennie J, Vergeer I, Bosselut G, Biddle SJH. Correlates of sedentary behaviour in university students: A systematic review. Prev Med. 2018;116:194–202. doi: 10.1016/j.ypmed.2018.09.016. [DOI] [PubMed] [Google Scholar]
- Chaput JP, Carrier J, Bastien C, Gariépy G, Janssen I. Economic burden of insufficient sleep duration in Canadian adults. Sleep Health. 2022;8:298–302. doi: 10.1016/j.sleh.2022.02.001. [DOI] [PubMed] [Google Scholar]
- Colley RC, Garriguet D, Janssen I, Craig CL, Clarke J, Tremblay MS. Physical activity of Canadian children and youth: Accelerometer results from the 2007 to 2009 Canadian health measures survey. Health Reports. 2011;22(1):15–23. [PubMed] [Google Scholar]
- Dempsey PC, Biddle SJH, Buman MP, Chastin S, Ekelund U, Friedenreich CM, et al. New global guidelines on sedentary behaviour and health for adults: Broadening the behavioural targets. Int J Behav Nutr Phys Act. 2020;17(1):151. doi: 10.1186/s12966-020-01044-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dempsey PC, Matthews CE, Dashti SG, Doherty AR, Bergouignan A, van Roekel EH, et al. Sedentary behavior and chronic disease: Mechanisms and future directions. J Phys Act Health. 2020;17(1):52–61. doi: 10.1123/jpah.2019-0377. [DOI] [PubMed] [Google Scholar]
- Diabetes in Canada. (2017). Highlights from the Canadian Chronic Disease Surveillance System. Public Health Agency of Canada. https://www.canada.ca/en/public-health/services/publications/diseases-conditions/diabetes-canada-highlights-chronic-disease-surveillance-system.html
- Ekelund U, Tarp J, Steene-Johannessen J, Hansen BH, Jefferis B, Fagerland MW, et al. Dose-response associations between accelerometry measured physical activity and sedentary time and all cause mortality: Systematic review and harmonised meta-analysis. BMJ. 2019;366:l4570. doi: 10.1136/bmj.l4570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardner B, Smith L, Lorencatto F, Hamer M, Biddle SJ. How to reduce sitting time? A review of behaviour change strategies used in sedentary behaviour reduction interventions among adults. Health Psychol Rev. 2016;10(1):89–112. doi: 10.1080/17437199.2015.1082146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heron L, O’Neill C, McAneney H, Kee F, Tully MA. Direct healthcare costs of sedentary behaviour in the UK. J Epidemiol Community Health. 2019;73(7):625–629. doi: 10.1136/jech-2018-211758. [DOI] [PubMed] [Google Scholar]
- Janssen I. Health care costs of physical inactivity in Canadian adults. Appl Physiol Nutr Metab. 2012;37(4):803–806. doi: 10.1139/h2012-061. [DOI] [PubMed] [Google Scholar]
- Jingjie W, Yang L, Jing Y, Ran L, Yiqing X, Zhou N. Sedentary time and its association with risk of cardiovascular diseases in adults: An updated systematic review and meta-analysis of observational studies. BMC Public Health. 2022;22(1):286. doi: 10.1186/s12889-022-12728-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katzmarzyk PT, Janssen I. The economic costs associated with physical inactivity and obesity in Canada: An update. Can J Appl Physiol. 2004;29:90–115. doi: 10.1139/h04-008. [DOI] [PubMed] [Google Scholar]
- Katzmarzyk, P. T., Powell, K. E., Jakicic, J. M., Troiano, R. P., Piercy, K., Tennant, B., the 2018 Physical Activity Guidelines Advisory Committee. (2019). Sedentary behavior and health: Update from the 2018 physical activity guidelines advisory committee. Medicine and Science in Sports and Exercise,51(6), 1227–1241. [DOI] [PMC free article] [PubMed]
- Kolu P, Kari JT, Raitanen J, Sievänen H, Tokola K, Havas E, et al. Economic burden of low physical activity and high sedentary behaviour in Finland. J Epidemiol Community Health. 2022;76(7):677–684. doi: 10.1136/jech-2021-217998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMichan L, Dick M, Skelton DA, Chastin SFM, Owen N, Dunstan DW, et al. Sedentary behaviour and bone health in older adults: A systematic review. Osteoporos Int. 2021;32(8):1487–1497. doi: 10.1007/s00198-021-05918-2. [DOI] [PubMed] [Google Scholar]
- Nguyen P, Le LK, Ananthapavan J, Gao L, Dunstan DW, Moodie M. Economics of sedentary behaviour: A systematic review of cost of illness, cost-effectiveness, and return on investment studies. Prev Med. 2022;156:106964. doi: 10.1016/j.ypmed.2022.106964. [DOI] [PubMed] [Google Scholar]
- ParticipACTION. (2021). Moving toward a better normal. The 2021 ParticipACTION Report Card on Physical Activity for Adults. Toronto, ON, Canada.
- Pearson, C., Janz, T., & Ali, J. (2013). Mental and substance use disorders in Canada. Statistics Canada, Catalogue no.82-624-X, Health at a Glance.
- Peeters GM, Mishra GD, Dobson AJ, Brown WJ. Health care costs associated with prolonged sitting and inactivity. Am J Prev Med. 2014;46(3):265–272. doi: 10.1016/j.amepre.2013.11.014. [DOI] [PubMed] [Google Scholar]
- Physical Activity Guidelines Advisory Committee. (2018). 2018 Physical Activity Guidelines Advisory Committee Scientific Report. US Department of Health and Human Services, Washington, DC, USA.
- Prince SA, Melvin A, Roberts KC, Butler GP, Thompson W. Sedentary behaviour surveillance in Canada: Trends, challenges and lessons learned. Int J Behav Nutr Phys Act. 2020;17(1):34. doi: 10.1186/s12966-020-00925-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puyau MR, Adolph AL, Vohra FA, Zakeri I, Butte NF. Prediction of activity energy expenditure using accelerometers in children. Med Sci Sports Exerc. 2004;36(9):1625–1631. [PubMed] [Google Scholar]
- Rollo, S., Lang, J. J., Roberts, K. C., Bang, F., Carson, V., Chaput, J. P., et al. (2022). Health associations with meeting the Canadian 24-hour Movement Guidelines for Adults: Results from the Canadian Health Measures Survey. Health Reports, 33(1), 16–26. [DOI] [PubMed]
- Ross, R., Chaput, J. P., Giangregorio, L. M., Janssen, I., Saunders, T. J., Kho, M. E., et al. (2020). Canadian 24-hour Movement Guidelines for Adults aged 18-64 years and Adults aged 65 years or older: An integration of physical activity, sedentary behaviour, and sleep. Applied Physiology, Nutrition, and Metabolism, 45(10 (Suppl. 2)), S57–S102. [DOI] [PubMed]
- Runacres A, Mackintosh KA, Knight RL, Sheeran L, Thatcher R, Shelley J, et al. Impact of the COVID-19 pandemic on sedentary time and behaviour in children and adults: A systematic review and meta-analysis. Int J Environ Res Public Health. 2021;18(21):11286. doi: 10.3390/ijerph182111286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders TJ, McIsaac T, Douillette K, Gaulton N, Hunter S, Rhodes RE, et al. Sedentary behaviour and health in adults: An overview of systematic reviews. Appl Physiol Nutr Metab. 2020;45(10 (Suppl. 2)):S197–S217. doi: 10.1139/apnm-2020-0272. [DOI] [PubMed] [Google Scholar]
- Shen D, Mao W, Liu T, Lin Q, Lu X, Wang Q, et al. Sedentary behavior and incident cancer: A meta-analysis of prospective studies. PLoS One. 2014;9(8):e105709. doi: 10.1371/journal.pone.0105709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Statistics Canada (2022a). Table 18-10-0006-01. Consumer Price Index, monthly, seasonally adjusted. 10.25318/1810000601-eng
- Statistics Canada (2022b). Table 17-10-0005-01. Population estimates on July 1st, by age and sex. 10.25318/1710000501-eng
- Statistics Canada (2022c). Table 14-10-0064-01. Employee wages by industry, annual (x 1,000). 10.25318/1410006401-eng
- Thorp AA, Owen N, Neuhaus M, Dunstan DW. Sedentary behaviors and subsequent health outcomes in adults: A systematic review of longitudinal studies, 1996-2011. Am J Prev Med. 2011;41(2):207–215. doi: 10.1016/j.amepre.2011.05.004. [DOI] [PubMed] [Google Scholar]
- Tremblay, M. S., Aubert, S., Barnes, J. D., Saunders, T. J., Carson, V., Latimer-Cheung, A. E., et al. (2017). Sedentary Behavior Research Network (SBRN) - Terminology Consensus Project process and outcome. International Journal of Behavioral Nutrition and Physical Activity, 14(1), 75. [DOI] [PMC free article] [PubMed]
- Wong SL, Colley RC, Connor Gorber S, Tremblay MS. Actical accelerometer sedentary activity thresholds for adults. J Phys Act Health. 2011;8(4):587–591. doi: 10.1123/jpah.8.4.587. [DOI] [PubMed] [Google Scholar]
- Yan S, Fu W, Wang C, Mao J, Liu B, Zou L, et al. Association between sedentary behavior and the risk of dementia: A systematic review and meta-analysis. Transl Psychiatry. 2020;10(1):112. doi: 10.1038/s41398-020-0799-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu H, Schwingel A. Associations between sedentary behavior, physical activity, and out-of-pocket health care expenditure: Evidence from Chinese older adults. J Aging Phys Act. 2019;27:108–115. doi: 10.1123/japa.2017-0206. [DOI] [PubMed] [Google Scholar]
- Zhai L, Zhang Y, Zhang D. Sedentary behaviour and the risk of depression: A meta-analysis. Br J Sports Med. 2015;49(11):705–709. doi: 10.1136/bjsports-2014-093613. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are publicly available at: https://www.canada.ca/en/public-health/services/chronic-diseases/chronic-disease-knowledge-development-exchange/economic-burden-illness-canada.html.