Abstract
Study Design
Retrospective cohort study
Objectives
This study aimed to investigate whether early surgery shortens the duration of opioid use in patients who underwent surgery with lumbar disc herniation.
Methods
We extracted patients who underwent surgery at least 2 weeks after they were diagnosed with lumbar disc herniation between April 2014 and May 2021. Opioid use after surgery was compared between patients who underwent surgery within 90 days (early surgery group) and 90 days or later (late surgery group). Propensity-score-matching analysis and multivariable Cox hazard regression analysis with a restricted cubic spline model were conducted to evaluate the association between the timing of surgery and termination of opioid use after surgery.
Results
A total of 1597 eligible patients were identified, with 807 (51%) in the early surgery group. In the propensity-score-matched cohort, the early surgery group had a significantly lower proportion of opioid use than the control group (28% vs 48%, percent difference −20%, P < .001). Multivariable Cox hazard regression analysis showed that early surgery was significantly associated with the earlier termination of opioid use (HR, 3.13; 95% CI, 1.97-4.97; P < .001). Restricted cubic spline model showed a monotonically decreased hazard ratio and decreased hazard ratio of .50 in patients who underwent surgery 111 days or later after the diagnosis.
Conclusions
Early surgery, especially within 90 days, was associated with earlier opioid use termination after surgery. Regarding the duration of opioid use following surgery, surgical treatment may be preferable to perform within around 4 months after the diagnosis.
Keywords: lumbar disc herniation, analgesic, opioid use termination, postoperative pain, early surgery, timing of surgery
Introduction
Lumbar disc herniation (LDH) is a well-known cause of low back pain and leg pain with high prevalence among individuals aged 30 to 50 years old. Patients with LDH are initially treated conservatively. Surgery is generally performed for those who do not respond to the conservative treatment,1-4 with a wide variation in its timing. The reported time from the onset of symptoms to surgery is inconsistent, ranging from several weeks to several months.5,6 Despite the common use of surgical treatment for LDH, its optimal timing is not well understood.
Although surgery for LDH is generally associated with favorable outcomes, some patients continue to suffer from residual symptoms after surgery. For such patients, analgesics like opioids are often used to alleviate persistent pain. Recent reports showed that a significant number of patients remained on opioids for a long period after surgery for LDH,7,8 in spite of a growing concern over their adverse effects. It remains unknown whether if the risk of prolonged opioid use after surgery is associated with the timing of surgical treatment.
In this study using a large administrative claims database covering young, middle-aged, and elderly people in Japan, we examined the relationship between the timing of surgery and postoperative opioid use in patients with LDH. This study aimed to clarify the optimal timing of surgery for LDH using the postoperative termination of opioid use as a clinical indicator.
Materials & Methods
DeSC Database
The DeSC database, which consists of the administrative claims data of 3 million insurance subscribers provided by DeSC Healthcare Inc. Tokyo, Japan, was used. This database is constructed based on anonymized medical data gathered by three of the Japanese public health insurers 9 : (1) association/union-administered health insurance for salaried employees in large companies; (2) National Health Insurance for self-employed individuals, retried individuals, and their dependents; (3) and Advanced Elderly Medical Service System for all people aged 75 years or older. Thus, this newly developed database covers young, middle-aged, and elderly people in Japan.
A previous study showed that the population included in the DeSC database represented the whole population of Japan. 10 The database contains encrypted unique identifiers, birth date, sex, height and weight, diagnoses coded according to the 10th revision of the International Classification of Diseases and Japanese tests, information on medications, surgical and nonsurgical procedures, admission and discharge date, and costs of examinations, procedures, surgery, and anesthesia. The pre-existing comorbidities were: diabetes mellitus (E10–E14), hypertension (I10–I15), chronic lung disease (J40–J47), history of cerebrovascular disease (I60–I69), cardiac disease (I20–I25, I30–I52), and hepatic cirrhosis (K74).
The study protocol was approved by the institutional review board of the Graduate School of Medicine, (2021010NI). The study was conducted in accordance with the principles of the Helsinki Declaration. The requirement for informed consent was waived because of the anonymous nature of the data.
Study Design, Covariates, and Outcome
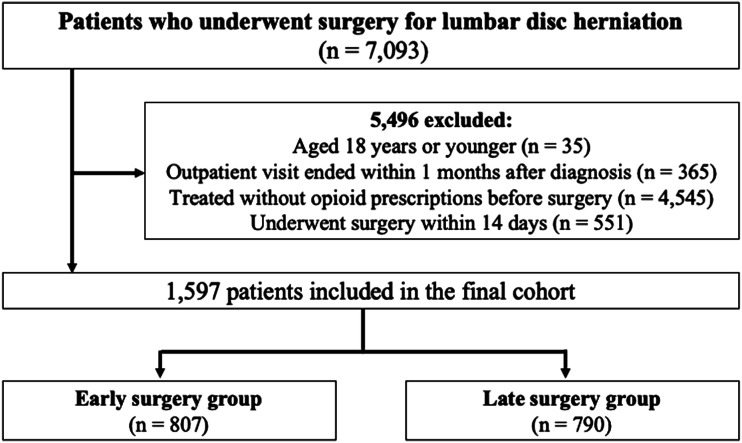
This retrospective observational study used the DeSC database to extract all patients who were diagnosed with LDH from April 2014 to May 2021 and treated with any of the following analgesics (Figure 1): acetaminophen, non-steroidal anti-inflammatory drugs, pregabalin, mirogabalin, and opioids (oxycodone, hydrocodone, morphine, tramadol, hydromorphone, codeine, buprenorphine, and fentanyl). The following patients were excluded: (a) aged 18 years or younger; (b) terminated outpatient visits for at least one months after the diagnosis; (c) treated without opioid prescriptions before surgery; and (d) underwent surgery within 2 weeks because they may have had worse conditions with cauda equina syndrome, altered bladder function, and progressive muscle weakness or neurological deficits.
Figure 1.
Flowchart of patient selection.
The primary outcome was the termination of opioid use, which is defined as patients terminating opioid use 3 months after surgery, according to previous studies.11,12 This definition is considered as chronic use of pain medications for those requiring prescriptions over a period of 90 days or longer.
Statistical Analysis
The distribution of the baseline characteristics between the early surgery and control groups was described. Early surgery was defined as surgery within 90 days after the diagnosis of LDH, based on the median days from the diagnosis to the surgery. Subsequently, propensity score matching analysis was performed to balance the measured potential confounders between the groups. 13 The propensity scores for receiving early surgery were estimated using a multivariable logistic regression model. All measured baseline covariates were included as predictive variables. The one-to-one nearest neighbor method was used with a caliper width of .2 of the standard deviation of the estimated propensity scores. Each patient in the early surgery group was matched to one patient in the control group without replacement. The absolute standardized differences were calculated for each covariate before and after matching, and the balanced distribution of covariates between the groups was confirmed.
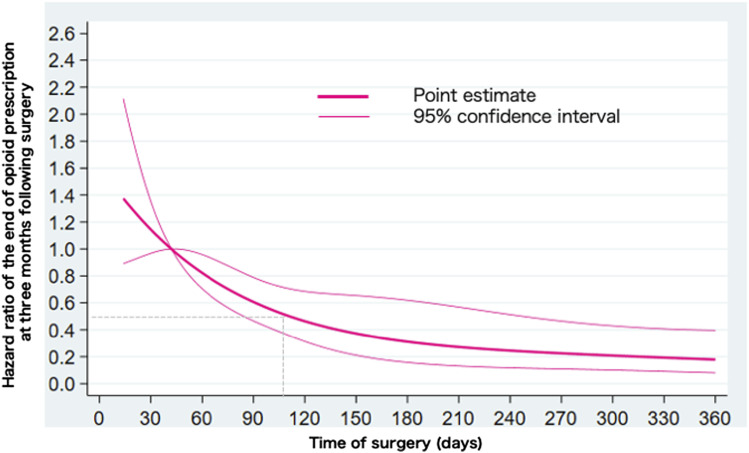
After propensity score matching, the proportion of analgesic prescriptions at 3-month, 6-month, and one year after surgery between the early and late surgery groups were compared. Subsequently, a multivariable cox proportional hazard model was constructed to compare the time of opioid use termination after surgery between the groups. A non-linear relationship between the timing of surgery and opioid use termination was modeled using a restricted cubic spline with standard points of 4 knots placed at the fifth, 25th, 75th, and 95th percentiles. 14 Each model was adjusted for age, sex, and pre-existing comorbidities. Since clinicians are interested in the time when the effectiveness of surgery is not different between the groups regarding opioid use termination after surgery, we set the reference at 42 days (6 weeks) after diagnosis in the restricted cubic spline model because many guidelines suggest an observational period of 6 weeks. The restricted cubic spline model resulted in point estimates using hazard ratios (HRs) and 95% confidence intervals (CIs).
Continuous variables are presented as mean (standard deviation) or median (interquartile range) as appropriate, and categorical variables are described as numbers (%). The outcomes after propensity score matching were compared between the early surgery and control groups using the χ 2 test. A two-sided P-value <.05 was considered statistically significant for all tests. All analyses were performed using Stata/MP version 16 (StataCorp, College Station, TX).
Results
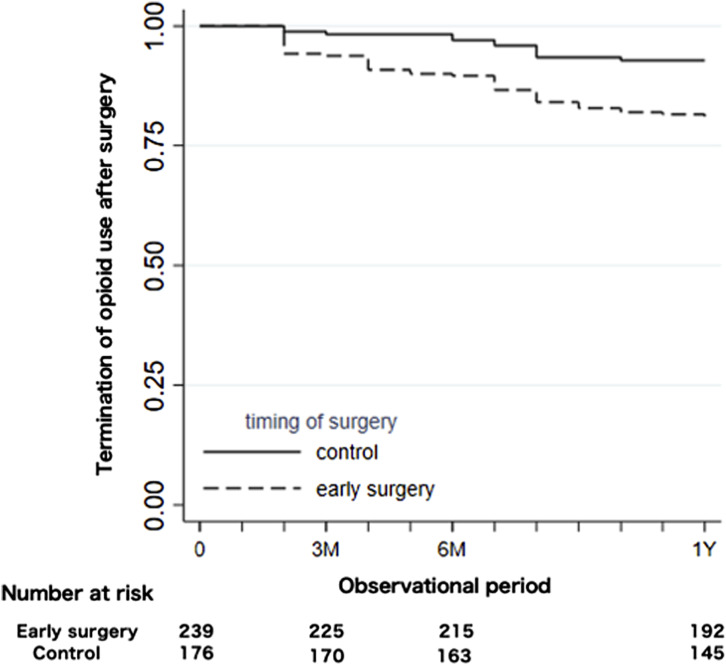
A total of 1597 eligible patients who underwent lumbar discectomy (mean age, 64 years; male, 62%) were identified (Table 1). Overall, the median observational period was 349 days, and 807 patients were included in the early surgery group (51%). Compared with patients in the late surgery group, patients in the early surgery group had (a) a shorter observational period; (b) higher proportions of male patients and at least one comorbidity, especially in diabetes mellitus and cardiac disease; and (c) lower proportions of preoperative analgesic use. After propensity score matching, 465 pairs were yielded and showed negligible imbalances between the groups. Table 2 shows the outcomes between the groups. In the matching cohort, patients who underwent early surgery showed a lower proportion of opioid use at three- and 6-months after surgery (28% vs 48%, percent difference −20%, P < .001; 23% vs 32%, percent difference −9%, P = .001), whereas a significant difference was not observed at 1-year after surgery (15% vs 17%, percent difference −2%, P = .53). The other analgesic prescription, except for acetaminophen, was similar to those of the opioid prescription. Table 3 and Figure 2 show the results of the multivariable cox proportional hazard regression analysis. Compared with the late surgery group, the early surgery group was significantly associated with earlier opioid use termination (hazard ratio, 3.13; 95% CI, 1.97-4.97; P < .001). The restricted cubic spline analysis showed an L-shaped association between the time of surgery and opioid use termination after surgery (Figure 3). The HR declined monotonically as the time of surgery increased from 42 days (reference) and fell below .5 when the time of surgery was 111 days (approximately 4 months) or later.
Table 1.
Baseline characteristics of patients who underwent lumbar discectomy by early and late surgery before and after propensity score matching.
| Characteristics | Unmatched Cohort | Matched Cohort | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Early Surgery | Late Surgery | ASD, % | Early Surgery | Late Surgery | ASD, % | |||||
| N | (N = 807) | (N = 790) | (N = 465) | (N = 465) | ||||||
| Observational period, median days (IQR) | 178 | (64,444) | 624 | (275,1422) | 69 | 354 | (193,674) | 260 | (79,678) | 0.8 |
| Age, mean (±SD) | 64 | 17 | 65 | 17 | 3.3 | 63 | 17 | 63 | 17 | 3.6 |
| Age category | ||||||||||
| 19-49 | 187 | 23 | 169 | 21 | 4.3 | 118 | 25 | 115 | 25 | 1.5 |
| 50-64 | 137 | 17 | 143 | 18 | 3.0 | 89 | 19 | 83 | 18 | 3.3 |
| 65– | 483 | 60 | 478 | 61 | 1.3 | 258 | 55 | 267 | 57 | 3.9 |
| Male | 518 | 64 | 465 | 59 | 11 | 275 | 59 | 281 | 60 | 2.6 |
| Comorbid conditions | ||||||||||
| Diabetes mellitus | 44 | 5.5 | 23 | 2.9 | 13 | 17 | 3.7 | 18 | 3.9 | 1.1 |
| Hypertension | 52 | 6.4 | 36 | 4.6 | 8.3 | 28 | 6.0 | 25 | 5.4 | 2.8 |
| Chronic lung disase | 36 | 4.5 | 26 | 3.3 | 6.1 | 22 | 4.7 | 18 | 3.9 | 4.2 |
| Cerebrovascular disease | 44 | 5.5 | 34 | 4.3 | 5.3 | 24 | 5.2 | 21 | 4.5 | 3.0 |
| Cardiac disease | 83 | 10 | 54 | 6.8 | 12 | 41 | 8.8 | 38 | 8.2 | 2.3 |
| Hepatic disease | 3 | 0.4 | 4 | 0.5 | 2.0 | 3 | 0.6 | 1 | 0.2 | 6.6 |
| At least one comorbidity | 175 | 22 | 128 | 16 | 14.0 | 87 | 19 | 79 | 17 | 4.5 |
| Preoperative prescription | ||||||||||
| Acetaminophen | 111 | 14 | 266 | 34 | 48 | 93 | 20 | 80 | 17 | 7.2 |
| NSAIDs | 396 | 49 | 593 | 75 | 56 | 315 | 68 | 289 | 62 | 11 |
| Pregabalin/Mirogabalin | 486 | 60 | 580 | 73 | 28 | 334 | 72 | 318 | 68 | 7.5 |
ASD; absolute standardized difference, IQR; interquartile range, SD; standardized deviation, NSAIDs; non-steroidal anti-inflammatory drugs
Table 2.
Comparison of analgesic prescription after surgery between early and late surgery after propensity score matching.
| Total (N = 930) | Early surgery (N = 465) | Late surgery (N = 465) | Difference (%) | P Value | ||||
|---|---|---|---|---|---|---|---|---|
| At Three months after Surgery | ||||||||
| Type of analgesic | ||||||||
| Overall | 779 | 84 | 329 | 71 | 450 | 97 | −26 | <.001 |
| Opioid | 356 | 38 | 132 | 28 | 224 | 48 | −20 | <.001 |
| Acetaminophen | 654 | 70 | 318 | 68 | 336 | 72 | −4 | .20 |
| NSAIDs | 627 | 67 | 261 | 56 | 366 | 79 | −23 | <.001 |
| Pregabalin/Mirogabalin | 547 | 59 | 225 | 48 | 322 | 69 | −21 | <.001 |
| At 6 months after surgery | ||||||||
| Type of analgesic | ||||||||
| Overall | 599 | 64 | 260 | 56 | 339 | 73 | −17 | <.001 |
| Opioid | 254 | 27 | 105 | 23 | 149 | 32 | −9 | .001 |
| Acetaminophen | 604 | 65 | 297 | 64 | 307 | 66 | −2 | .49 |
| NSAIDs | 473 | 51 | 211 | 45 | 262 | 56 | −11 | <.001 |
| Pregabalin/Mirogabalin | 422 | 45 | 188 | 40 | 234 | 50 | −10 | .002 |
| At one year after surgery | ||||||||
| Type of analgesic | ||||||||
| Overall | 360 | 39 | 170 | 37 | 190 | 41 | −4 | .18 |
| Opioid | 147 | 16 | 70 | 15 | 77 | 17 | −2 | .53 |
| Acetaminophen | 554 | 60 | 273 | 59 | 281 | 60 | −2 | .59 |
| NSAIDs | 291 | 31 | 143 | 31 | 148 | 32 | −1 | .72 |
| Pregabalin/Mirogabalin | 300 | 32 | 146 | 31 | 154 | 33 | −2 | .57 |
NSAIDs; non-steroidal anti-inflammatory drugs
Table 3.
Multivariable cox regression analysis predicting opioid use termination after surgery.
| Variable | Hazard Ratio | 95% Confidence Interval | P Value |
|---|---|---|---|
| Early surgery | 3.13 | 1.97-4.97 | <.001 |
| Age, years | .98 | .96-.99 | <.001 |
| Male | 1.08 | .74-1.57 | .703 |
| Comorbidities | |||
| Diabetes mellitus | .58 | .40-1.89 | .724 |
| Hypertension | 1.58 | .49-2.23 | .900 |
| Chronic lung disease | .78 | .38-1.79 | .623 |
| Cerebrovascular disease | 1.14 | .84-2.94 | .156 |
| Cardiac disease | 1.53 | .72-2.23 | .413 |
| Hepatic disease | 2.23 | .06-12.7 | .898 |
| At least one comorbidity | .86 | .33-2.22 | .751 |
Figure 2.
Kaplan–Meier curves of opioid use termination following surgery between the early and late surgery groups during the observational period.
Figure 3.
Restricted cubic spline curb showing the association between the time of surgery and opioid use termination following surgery.
Discussion
This study examined whether early surgery shortened the duration of opioid use in patients who underwent lumbar discectomy and found that early surgery, especially within 90 days after the diagnosis of LDH, had higher HR of postoperative opioid use termination than late surgery. The HR decreased monotonically as the time of surgery increased and fell below .50 when the time of surgery was 4 months or later.
Opioids are widely used for neural pain including postoperative pain control. However, they may have several side effects, including increased risk of ileus and infection, prolonged hospital stay, and higher readmission rate.12,15-17 Opioid use is affected by several factors that can substantially differ across countries. 18 In the United States, although the number of chronic opioid use following primary lumbar discectomy has declined, one in 5 patients still use opioids after even surgical treatment. 7 Furthermore, a recent study showed that 33% of patients had opioid prescription before surgery, and 7.6% of patients who underwent lumbar discectomy still used opioids at one year after surgery. 11 In more strictly regulated settings, only 3.3% of Taiwanese patients sustained postoperative opioid use at 90 to 180 days after surgery. 19 In this study, 36% of patients who underwent surgery were treated with opioid preoperatively, which was comparable to those in previous studies. However, 16% of patients, who underwent lumbar discectomy, still used opioids at one year after surgery. Moreover, opioids are not strictly regulated in Japan compared to Western countries. Although the preoperative opioid use in Japan was comparable to those in other countries, clinicians must be vigilant in monitoring patients to avoid chronic opioid use.
Prolonged opioid use is associated with future opioid dependence, which has an enormous societal impact.20,21 Regarding the opioid prescription period, a previous study showed that the proportion of patients who used one or more opioids decreased to under 10% at 9 to 12 months after lumbar discectomy and concluded that a minority of patients who underwent lumbar discectomy continued to use opioids up to 15 months after surgery. 11 However, 90% of acute attacks of sciatica in patients with LDH settle with conservative treatment during the first 6 week. Nevertheless, some patients still use opioids for over one year after surgery. This study showed that early surgery, especially within 90 days, was significantly associated with opioid use termination at 3 months after surgery. Guidelines recommend surgery if patients have prolonged pain despite conservative treatments. 22 According to the restricted cubic spline analysis, the likelihood of opioid use termination may decline to an HR of .5 when patients undergo surgery 4 months after the diagnosis of LDH. This may be one of the possible cut points for the preference for surgery to reduce chronic opioid prescription.
Nevertheless, this study has several limitations. First, we could not obtain information on image findings, and type and severity of LDH. Second, we could not identify indications for surgery. For patients who presented with severe cauda equina symptoms, neurological deficit, and muscle weakness, emergency surgery may be performed even for patients with LDH. Therefore, we excluded patients who underwent surgery within 2 weeks after the diagnosis. Third, unmeasured confounding may not be completely removed even with propensity score analyses. However, we believe that measured confounding was minimized on this cohort through use of propensity matching analysis. Fourth, we could not determine the reasons for prolonged post-operative opioid use, whether it was patient’s dependence on opioids or their doctor’s prescription of opioids. Despite these limitations, the findings from this study may provide additional useful information for surgeons regarding opioid prescription after surgery and prevention of chronic opioid use. Further studies are warranted to clarify whether early surgery is preferable regarding cost effectiveness and long-term prognosis.
In conclusion, early surgery, especially within 90 days, may shorten the duration of postoperative opioid use in patients with LDH. Moreover, postoperative opioid use may decrease when patients undergo surgery in 4 months or later after the diagnosis of LDH.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by grants from the Ministry of Health, Labour and Welfare, Japan (21AA2007 and 20AA2005) and the Ministry of Education, Culture, Sports, Science and Technology, Japan (20H03907).
Level of Evidence: Prognostic Level Ⅲ
ORCID iDs
Akira Honda https://orcid.org/0000-0001-8462-6024
Eiji Takasawa https://orcid.org/0000-0002-7995-6093
Sho Ishiwata https://orcid.org/0000-0002-6730-977X
References
- 1.Williams RW. Microlumbar discectomy. A 12-year statistical review. Spine (Phila Pa 1976). 1986;11:851-852. [PubMed] [Google Scholar]
- 2.Moore AJ, Chilton JD, Uttley D. Long-term results of microlumbar discectomy. Br J Neurosurg. 1994;8:319-326. DOI: 10.3109/02688699409029620. [DOI] [PubMed] [Google Scholar]
- 3.Harrington JF, French P. Open versus minimally invasive lumbar microdiscectomy: comparison of operative times, length of hospital stay, narcotic use and complications. Minim Invasive Neurosurg. 2008;51:30-35. DOI: 10.1055/s-2007-1004543. [DOI] [PubMed] [Google Scholar]
- 4.Deyo RA, Mirza SK, Martin BI, Kreuter W, Goodman DC, Jarvik JG. Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA. 2010;303:1259-1265. DOI: 10.1001/jama.2010.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wu X, Zhuang S, Mao Z, Chen H. Microendoscopic discectomy for lumbar disc herniation: surgical technique and outcome in 873 consecutive cases. Spine. 2006;31:2689-2694. DOI: 10.1097/01.brs.0000244615.43199.07. [DOI] [PubMed] [Google Scholar]
- 6.Gugliotta M, da Costa BR, Dabis E, et al. Surgical versus conservative treatment for lumbar disc herniation: a prospective cohort study. BMJ Open. 2016;6:e012938. DOI: 10.1136/bmjopen-2016-012938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Harris AB, Zhang B, Marrache M, et al. Chronic opioid use following lumbar discectomy: Prevalence, risk factors, and current trends in the United States. Neurospine. 2020;17:879-887. DOI: 10.14245/ns.2040122.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.O’Donnell JA, Anderson JT, Haas AR, et al. Preoperative Opioid Use is a Predictor of Poor Return to Work in Workers’ Compensation Patients After Lumbar Diskectomy. Spine. 2018;43:594-602. DOI: 10.1097/BRS.0000000000002385. [DOI] [PubMed] [Google Scholar]
- 9.Yasunaga H. Real World Data in Japan: Chapter I NDB. Ann Clin Epidemiol. 2019;1:28-30. DOI: 10.37737/ace.1.2_28. [DOI] [Google Scholar]
- 10.Okada A, Yasunaga H. Prevalence of noncommunicable diseases in Japan using a newly developed administrative claims database covering young, middle-aged, and elderly people. JMA J. 2022;5:190-198. DOI: 10.31662/jmaj.2021-0189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ziino C, Karhade AV, Schoenfeld AJ, Harris MB, Schwab JH. Characteristics of postoperative opioid prescription use following lumbar discectomy. J Neurosurg Spine. 2021;35:710-714. DOI: 10.3171/2021.2.SPINE202041. [DOI] [PubMed] [Google Scholar]
- 12.Goyal A, Payne S, Sangaralingham LR, et al. Incidence and risk factors for prolonged postoperative opioid use following lumbar spine surgery: a cohort study. J Neurosurg Spine. 2021:1-9. Online ahead of print. DOI: 10.3171/2021.2.SPINE202205. [DOI] [PubMed] [Google Scholar]
- 13.Rosenbaum PR, Rubin DB. Constructing a control group using multivariate matched sampling methods that incorporate the propensity score. Am Stat. 1985;39:33-38. DOI: 10.1080/00031305.1985.10479383. [DOI] [Google Scholar]
- 14.Badhiwala JH, Wilson JR, Witiw CD, et al. The influence of timing of surgical decompression for acute spinal cord injury: a pooled analysis of individual patient data. Lancet Neurol. 2021;20:117-126. DOI: 10.1016/S1474-4422(20)30406-3. [DOI] [PubMed] [Google Scholar]
- 15.Turcotte J, Sanford Z, Broda A, Patton C. Centers for Medicare & Medicaid Services Hierarchical Condition Category score as a predictor of readmission and reoperation following elective inpatient spine surgery. J Neurosurg Spine. 2019;31:1-7. DOI: 10.3171/2019.3.SPINE1999. [DOI] [PubMed] [Google Scholar]
- 16.Dunn LK, Durieux ME, Fernández LG, et al. Influence of catastrophizing, anxiety, and depression on in-hospital opioid consumption, pain, and quality of recovery after adult spine surgery. J Neurosurg Spine. 2018;28:119-126. DOI: 10.3171/2017.5.SPINE1734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sodhi N, Anis HK, Acuña AJ, et al. Opioid use disorder is associated with an increased risk of infection after total joint arthroplasty: a large database study. Clin Orthop Relat Res. 2020;478:1752-1759. DOI: 10.1097/CORR.0000000000001390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rahavard BB, Candido KD, Knezevic NN. Different pain responses to chronic and acute pain in various ethnic/racial groups. Pain Manag. 2017;7:427-453. DOI: 10.2217/pmt-2017-0056. [DOI] [PubMed] [Google Scholar]
- 19.Yen HK, Ogink PT, Huang CC, et al. A machine learning algorithm for predicting prolonged postoperative opioid prescription after lumbar disc herniation surgery. An external validation study using 1,316 patients from a Taiwanese cohort. Spine J. 2022;22:1119-1130. DOI: 10.1016/j.spinee.2022.02.009. [DOI] [PubMed] [Google Scholar]
- 20.Gomes T, Tadrous M, Mamdani MM, Paterson JM, Juurlink DN. The burden of opioid-related mortality in the United States. JAMA Netw Open. 2018;1:e180217. DOI: 10.1001/jamanetworkopen.2018.0217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lin TC, Ger L-P, Pergolizzi JV, Jr, Raffa RB, Wang JO, Ho S-T. Long-term use of opioids in 210 officially registered patients with chronic noncancer pain in Taiwan: A cross-sectional study. J Formos Med Assoc. 2017;116:257-265. DOI: 10.1016/j.jfma.2016.10.015. [DOI] [PubMed] [Google Scholar]
- 22.Kreiner DS, Hwang SW, Easa JE, et al. An evidence-based clinical guideline for the diagnosis and treatment of lumbar disc herniation with radiculopathy. Spine J. 2014;14:180-191. DOI: 10.1016/j.spinee.2013.08.003. [DOI] [PubMed] [Google Scholar]