Abstract
Background
Diarrhoea is a major contributor to the global disease burden, particularly amongst children under five years in low‐ and middle‐income countries (LMICs). As many of the infectious agents associated with diarrhoea are transmitted through faeces, sanitation interventions to safely contain and manage human faeces have the potential to reduce exposure and diarrhoeal disease.
Objectives
To assess the effectiveness of sanitation interventions for preventing diarrhoeal disease, alone or in combination with other WASH interventions.
Search methods
We searched the Cochrane Infectious Diseases Group Specialized Register, CENTRAL, MEDLINE, Embase, LILACS, and Chinese language databases available under the China National Knowledge Infrastructure (CNKI‐CAJ). We also searched the metaRegister of Controlled Trials (mRCT) and conference proceedings, contacted researchers, and searched references of included studies. The last search date was 16 February 2022.
Selection criteria
We included randomized controlled trials (RCTs), quasi‐RCTs, non‐randomized controlled trials (NRCTs), controlled before‐and‐after studies (CBAs), and matched cohort studies of interventions aimed at introducing or expanding the coverage and/or use of sanitation facilities in children and adults in any country or population. Our primary outcome of interest was diarrhoea and secondary outcomes included dysentery (bloody diarrhoea), persistent diarrhoea, hospital or clinical visits for diarrhoea, mortality, and adverse events. We included sanitation interventions whether they were conducted independently or in combination with other interventions.
Data collection and analysis
Two review authors independently assessed eligible studies, extracted relevant data, assessed risk of bias, and assessed the certainty of evidence using the GRADE approach. We used meta‐analyses to estimate pooled measures of effect, described results narratively, and investigated potential sources of heterogeneity using subgroup analyses.
Main results
Fifty‐one studies met our inclusion criteria, with a total of 238,535 participants. Of these, 50 studies had sufficient information to be included in quantitative meta‐analysis, including 17 cluster‐RCTs and 33 studies with non‐randomized study designs (20 NRCTs, one CBA, and 12 matched cohort studies). Most were conducted in LMICs and 86% were conducted in whole or part in rural areas. Studies covered three broad types of interventions: (1) providing access to any sanitation facility to participants without existing access practising open defecation, (2) improving participants' existing sanitation facility, or (3) behaviour change messaging to improve sanitation access or practices without providing hardware or subsidy, although many studies overlapped multiple categories. There was substantial heterogeneity amongst individual study results for all types of interventions.
Providing access to any sanitation facility
Providing access to sanitation facilities was evaluated in seven cluster‐RCTs, and may reduce diarrhoea prevalence in all age groups (risk ratio (RR) 0.89, 95% confidence interval (CI) 0.73 to 1.08; 7 trials, 40,129 participants, low‐certainty evidence). In children under five years, access may have little or no effect on diarrhoea prevalence (RR 0.98, 95% CI 0.83 to 1.16, 4 trials, 16,215 participants, low‐certainty evidence). Additional analysis in non‐randomized studies was generally consistent with these findings. Pooled estimates across randomized and non‐randomized studies provided similar protective estimates (all ages: RR 0.79, 95% CI 0.66 to 0.94; 15 studies, 73,511 participants; children < 5 years: RR 0.83, 95% CI 0.68 to 1.02; 11 studies, 25,614 participants).
Sanitation facility improvement
Interventions designed to improve existing sanitation facilities were evaluated in three cluster‐RCTs in children under five and may reduce diarrhoea prevalence (RR 0.85, 95% CI 0.69 to 1.06; 3 trials, 14,900 participants, low‐certainty evidence). However, some of these interventions, such as sewerage connection, are not easily randomized. Non‐randomized studies across participants of all ages provided estimates that improving sanitation facilities may reduce diarrhoea, but may be subject to confounding (RR 0.61, 95% CI 0.50 to 0.74; 23 studies, 117,639 participants, low‐certainty evidence). Pooled estimates across randomized and non‐randomized studies provided similar protective estimates (all ages: RR 0.65, 95% CI 0.55 to 0.78; 26 studies, 132,539 participants; children < 5 years: RR 0.70, 95% CI 0.54 to 0.91, 12 studies, 23,353 participants).
Behaviour change messaging only (no hardware or subsidy provided)
Strategies to promote behaviour change to construct, upgrade, or use sanitation facilities were evaluated in seven cluster‐RCTs in children under five, and probably reduce diarrhoea prevalence (RR 0.82, 95% CI 0.69 to 0.98; 7 studies, 28,909 participants, moderate‐certainty evidence). Additional analysis from two non‐randomized studies found no effect, though with very high uncertainty. Pooled estimates across randomized and non‐randomized studies provided similar protective estimates (RR 0.85, 95% CI 0.73 to 1.01; 9 studies, 31,080 participants). No studies measured the effects of this type of intervention in older populations.
Any sanitation intervention
A pooled analysis of cluster‐RCTs across all sanitation interventions demonstrated that the interventions may reduce diarrhoea prevalence in all ages (RR 0.85, 95% CI 0.76 to 0.95, 17 trials, 83,938 participants, low‐certainty evidence) and children under five (RR 0.87, 95% CI 0.77 to 0.97; 14 trials, 60,024 participants, low‐certainty evidence). Non‐randomized comparisons also demonstrated a protective effect, but may be subject to confounding. Pooled estimates across randomized and non‐randomized studies provided similar protective estimates (all ages: RR 0.74, 95% CI 0.67 to 0.82; 50 studies, 237,130 participants; children < 5 years: RR 0.80, 95% CI 0.71 to 0.89; 32 studies, 80,047 participants). In subgroup analysis, there was some evidence of larger effects in studies with increased coverage amongst all participants (75% or higher coverage levels) and also some evidence that the effect decreased over longer follow‐up times for children under five years.
There was limited evidence on other outcomes. However, there was some evidence that any sanitation intervention was protective against dysentery (RR 0.74, 95% CI 0.54 to 1.00; 5 studies, 34,025 participants) and persistent diarrhoea (RR 0.57, 95% CI 0.43 to 0.75; 2 studies, 2665 participants), but not against clinic visits for diarrhoea (RR 0.86, 95% CI 0.44 to 1.67; 2 studies, 3720 participants) or all‐cause mortality (RR 0.99, 95% CI 0.89 to1.09; 7 studies, 46,123 participants).
Authors' conclusions
There is evidence that sanitation interventions are effective at preventing diarrhoea, both for young children and all age populations. The actual level of effectiveness, however, varies by type of intervention and setting. There is a need for research to better understand the factors that influence effectiveness.
Keywords: Adult; Child, Preschool; Humans; China; Controlled Before-After Studies; Diarrhea; Diarrhea/epidemiology; Diarrhea/prevention & control; Dysentery; Non-Randomized Controlled Trials as Topic; Randomized Controlled Trials as Topic; Sanitation
Plain language summary
Interventions to improve sanitation for preventing diarrhoea
What is the aim of this review?
The aim of this Cochrane Review was to assess if diarrhoea is reduced by sanitation interventions to provide, upgrade, or encourage people to use toilets or latrines. We collected and analysed all relevant studies of certain prespecified rigorous study design types and found 51 studies involving 238,535 people.
Key messages
We found evidence that sanitation interventions may be protective against diarrhoea. However, the effects varied by the type of intervention and setting, and the certainty of the evidence ranged from very low to moderate.
What was studied in this review?
Diarrhoea is a major cause of death and disease, especially amongst young children in low‐income countries. Many of the pathogens that cause diarrhoea are transmitted through exposure to human faeces. Sanitation facilities, such as toilets and latrines, serve as a primary barrier to separate pathogens excreted in human faeces from the environment. This review examined intervention studies to improve sanitation access, facilities, or use. We identified 51 studies of such interventions, most of which were from low‐ or middle‐income countries.
What were the main results of this review?
The results suggest that sanitation interventions reduce diarrhoea by about 15% to 26%, both in vulnerable young children and all age populations. However, not all interventions were protective, and effects varied substantially by the type of intervention and setting. We estimated that an intervention to provide sanitation access to people practising open defecation would probably reduce diarrhoea by about 11% to 21%, an intervention to improve existing sanitation facilities may reduce diarrhoea by about 15% to 35%, and a behaviour change intervention to improve sanitation access or use without providing infrastructure or subsidies would probably reduce diarrhoea by about 15% to 18%. However, the certainty of the evidence ranged from moderate to very low, and additional research is likely to change these estimates, particularly for interventions that provide sanitation access or improve existing sanitation facilities. Further research is also necessary to understand which type of interventions would yield the most protective health effects in various types of settings.
How up‐to‐date is this review?
We searched for studies that had been published up to 16 February 2022.
Summary of findings
Summary of findings 1. Summary of findings table 1.
| Providing access to any sanitation facility intervention compared with no intervention for preventing diarrhoea | ||||||
|
Patient or population: adults and children Settings: any country or population Intervention: providing access to any sanitation facility intervention Comparison: no intervention | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| No intervention | Intervention | |||||
| Cluster‐RCTs | ||||||
|
Diarrhoea prevalence (All ages) |
3 episodes per person per year | 2.67 episodes per person per year (2.19 to 3.24) | RR 0.89 (0.73 to 1.08)a | 40,129 (7 studies) | ⊕⊕⊝⊝ lowb,c | The intervention may reduce diarrhoea prevalence. However, the range where the actual effect may be (the confidence interval or "margin of error") indicates that the intervention may have little or no effect on diarrhoea prevalence in all participants. |
|
Diarrhoea prevalence (Children < 5) |
3 episodes per person per year | 2.94 episodes per person per year (2.49 to 3.48) | RR 0.98 (0.83 to 1.16)a | 16,215 (4 studies) | ⊕⊕⊝⊝ lowb,d | The intervention may have little or no effect on diarrhoea prevalence in children under 5 years. |
| Non‐randomized studies** | ||||||
|
Diarrhoea prevalence (All ages) |
3 episodes per person per year | 2.16 episodes per person per year (1.59 to 2.91) | RR 0.72 (0.53 to 0.97)a | 33,382 (8 studies) | ⊕⊝⊝⊝ very lowe,f | We are uncertain whether or not the intervention reduces diarrhoea prevalence in all participants. |
|
Diarrhoea prevalence (Children < 5) |
3 episodes per person per year | 2.28 episodes per person per year (1.65 to 3.15) | RR 0.76 (0.55 to 1.05)a | 9399 (7 studies) | ⊕⊝⊝⊝ very lowe,f | We are uncertain whether or not the intervention reduces diarrhoea prevalence in children under 5 years. |
| *The assumed risk for diarrhoea is taken from WHO 2017 and Fischer Walker 2012 and represents an estimated mean for the incidence of diarrhoea in low‐ and middle‐income countries. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). **Non‐randomized studies included here are non‐randomized controlled trials (NRCTs) and matched cohort studies. CI: confidence interval; RCT: randomized controlled trial; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High certainty: further research is very unlikely to change our confidence in the estimate of effect. Moderate certainty: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low certainty: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low certainty: we are very uncertain about the estimate. | ||||||
aAlthough we are unable to rate the certainty of the evidence, the pooled effect estimates for cluster‐RCTs and non‐randomized studies combined were RR 0.79 (95% CI 0.66 to 0.94; 15 studies, 73,511 participants) for all participants, and RR 0.83 (95% CI 0.68 to 1.02; 11 studies, 25,614 participants) for children under five years. bDowngraded one level for risk of bias: all studies measured the diarrhoea outcome by self‐ or caregiver‐reported diarrhoea, which is susceptible to bias because the studies were unblinded. cDowngraded one level for indirectness: only includes one study in households in rural sub‐Saharan Africa, which is an important target intervention population. dDowngraded one level for indirectness: four studies in rural areas, three of which were in India and one in Zimbabwe. eDowngraded two levels for risk of bias: over half of the studies measured the diarrhoea outcome as self‐ or caregiver‐reported diarrhoea, which is susceptible to bias because the studies were unblinded. Additionally, most studies did not control for potential confounding factors in study design or analysis. fDowngraded one level for inconsistency: considerable statistical heterogeneity (I2 = 86% for all ages; I2 = 88% for children under five).
Summary of findings 2. Summary of findings table 2.
| Sanitation facility improvement intervention compared with no intervention for preventing diarrhoea | ||||||
|
Patient or population: adults and children Settings: any country or population Intervention: sanitation facility improvement intervention Comparison: no intervention | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| No intervention | Intervention | |||||
| Cluster‐RCTs | ||||||
|
Diarrhoea prevalence (Children < 5a) |
3 episodes per person per year | 2.55 episodes per person per year (2.07 to 3.18) | RR 0.85 (0.69 to 1.06)b | 14,900 (3 studies) | ⊕⊕⊝⊝ lowc,d,e | The intervention may reduce diarrhoea prevalence. However, the range where the actual effect may be (the confidence interval or "margin of error") indicates that the intervention may have little or no effect on diarrhoea prevalence in children under 5 years. |
| Non‐randomized studies** | ||||||
|
Diarrhoea prevalence (All ages) |
3 episodes per person per year | 1.83 episodes per person per year (1.50 to 2.22) |
RR 0.61 (0.50 to 0.74)b |
117,639 (23 studies) | ⊕⊕⊝⊝ lowf | The intervention may reduce diarrhoea prevalence in all participants. |
|
Diarrhoea prevalence (Children < 5) |
3 episodes per person per year | 1.92 episodes per person per year (1.29 to 2.88) | RR 0.64 (0.43 to 0.96)b | 8453 (9 studies) | ⊕⊝⊝⊝ very lowf,g | We are uncertain whether or not the intervention reduces diarrhoea prevalence in children under 5 years. |
| *The assumed risk for diarrhoea is taken from WHO 2017 and Fischer Walker 2012 and represents an estimated mean for the incidence of diarrhoea in low‐ and middle‐income countries. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). **Non‐randomized studies included here are non‐randomized controlled trials (NRCTs), controlled before‐and‐after studies (CBAs), and matched cohort studies. CI: confidence interval; RCT: randomized controlled trial; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High certainty: further research is very unlikely to change our confidence in the estimate of effect. Moderate certainty: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low certainty: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low certainty: we are very uncertain about the estimate. | ||||||
aRepresents the same study population as an 'all ages' model as all studies for this intervention type only measured effects in children under five years old. bAlthough we are unable to rate the certainty of the evidence, the pooled effect estimates for cluster‐RCTs and non‐randomized studies combined were RR 0.65 (95% CI 0.55 to 0.78; 26 studies, 132,539 participants) for all participants, and RR 0.70 (95% CI 0.54 to 0.91; 12 studies, 23,353 participants) for children under five years. cDowngraded one level for risk of bias: all studies measured the diarrhoea outcome as self‐ or caregiver‐reported diarrhoea, which is susceptible to bias because the studies were unblinded. dDowngraded one level for indirectness: only three studies, all from rural areas (one in Bangladesh, one in Kenya, one in the Democratic Republic of Congo). eNo serious inconsistency: while there was considerable statistical heterogeneity (I2 = 79%), there was consistency in the direction of the effect (all studies showed protective intervention effects). fDowngraded two levels for risk of bias: over half the studies measured the diarrhoea outcome as self‐ or caregiver‐reported diarrhoea, which is susceptible to bias because the studies were unblinded. Additionally, less than half of the studies controlled for potential confounding factors in study design or analysis. gDowngraded one level for inconsistency: considerable statistical heterogeneity (I2 = 75% for children under five).
Summary of findings 3. Summary of findings table 3.
| Behaviour change messaging only intervention compared with no intervention for preventing diarrhoea | ||||||
|
Patient or population: adults and children Settings: any country or population Intervention: behaviour change messaging only intervention Comparison: no intervention | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| No intervention | Intervention | |||||
| Cluster‐RCTs | ||||||
|
Diarrhoea prevalence (Children < 5a) |
3 episodes per person per year | 2.46 episodes per person per year (2.07 to 2.94) | RR 0.82 (0.69 to 0.98)b | 28,909 (7 studies) | ⊕⊕⊕⊝ moderatec | The intervention probably reduces diarrhoea prevalence in children under 5 years. |
| NRCTs | ||||||
|
Diarrhoea prevalence (Children < 5a) |
3 episodes per person per year | 3.06 episodes per person per year (2.73 to 3.42) | RR 1.02 (0.91 to 1.14)b | 2171 (2 studies) | ⊕⊝⊝⊝ very lowd,e | We are uncertain whether the intervention reduces diarrhoea prevalence in children under 5 years. |
| *The assumed risk for diarrhoea is taken from WHO 2017 and Fischer Walker 2012 and represents an estimated mean for the incidence of diarrhoea in low‐ and middle‐income countries. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; NRCT: non‐randomized controlled trial; RCT: randomized controlled trial; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High certainty: further research is very unlikely to change our confidence in the estimate of effect. Moderate certainty: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low certainty: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low certainty: we are very uncertain about the estimate. | ||||||
aRepresents the same study population as an 'all ages' model as all studies for this intervention type only measured effects in children under five years old. bAlthough we are unable to rate the certainty of the evidence, the pooled effect estimate for cluster‐RCTs and non‐randomized studies combined was RR 0.85 (95% CI 0.73 to 1.01; 9 studies, 31,080 participants) for children under five years. cDowngraded one level for risk of bias: all studies measured the diarrhoea outcome as self‐ or caregiver‐reported diarrhoea, which is susceptible to bias because the studies were unblinded. dDowngraded two levels for risk of bias: all studies measured the diarrhoea outcome as self‐ or caregiver‐reported diarrhoea, which is susceptible to bias because the studies were unblinded. Additionally, none of the studies controlled for potential confounding factors in study design or analysis. eDowngraded one level for indirectness: only two studies, both from rural areas (one in Bangladesh and one in India).
Summary of findings 4. Summary of findings table 4.
| Any sanitation intervention compared with no intervention for preventing diarrhoea | ||||||
|
Patient or population: adults and children Settings: any country or population Intervention: any sanitation intervention Comparison: no intervention | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| No intervention | Intervention | |||||
| Cluster‐RCTs | ||||||
|
Diarrhoea prevalence (All ages) |
3 episodes per person per year | 2.55 episodes per person per year (2.28 to 2.85) | RR 0.85 (0.76 to 0.95)a | 83,938 (17 studies) | ⊕⊕⊝⊝ lowb,c | The intervention may reduce diarrhoea prevalence in all participants. |
|
Diarrhoea prevalence (Children < 5) |
3 episodes per person per year | 2.61 episodes per person per year (2.31 to 2.91) | RR 0.87 (0.77 to 0.97)a | 60,024 (14 studies) | ⊕⊕⊝⊝ lowb,c | The intervention may reduce diarrhoea prevalence in children under five years. |
| Non‐randomized studies** | ||||||
|
Diarrhoea prevalence (All ages) |
3 episodes per person per year | 2.01 episodes per person per year (1.71 to 2.34) | RR 0.67 (0.57 to 0.78)a | 153,192 (33 studies) | ⊕⊝⊝⊝ very lowd,e | We are uncertain whether or not the intervention reduces diarrhoea prevalence in all participants. |
|
Diarrhoea prevalence (Children < 5) |
3 episodes per person per year | 2.16 episodes per person per year (1.74 to 2.73) | RR 0.72 (0.58 to 0.91)a | 20,023 (18 studies) | ⊕⊝⊝⊝ very lowd,e | We are uncertain whether or not the intervention reduces diarrhoea prevalence in children under five years. |
| *The assumed risk for diarrhoea is taken from WHO 2017 and Fischer Walker 2012 and represents an estimated mean for the incidence of diarrhoea in low‐ and middle‐income countries. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). **Non‐randomized studies included here are non‐randomized controlled trials (NRCTs), controlled before‐and‐after studies (CBAs), and matched cohort studies. CI: confidence interval; RCT: randomized controlled trial; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High certainty: further research is very unlikely to change our confidence in the estimate of effect. Moderate certainty: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low certainty: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low certainty: we are very uncertain about the estimate. | ||||||
aAlthough we are unable to rate the certainty of the evidence, the pooled effect estimates for cluster‐RCTs and non‐randomized studies combined were RR 0.74 (95% CI 0.67 to 0.82; 50 studies, 237,130 participants) for all participants, and RR 0.80 (95% CI 0.71 to 0.89, 32 studies, 80,047 participants) for children under five years. bDowngraded one level for risk of bias: all studies measured the diarrhoea outcome as self‐ or caregiver‐reported diarrhoea, which is susceptible to bias because the studies were unblinded. cDowngraded one level for inconsistency, because there was substantial variation between sanitation intervention types. dDowngraded two levels for risk of bias: over half of studies measured the diarrhoea outcome as self‐ or caregiver‐reported diarrhoea, which is susceptible to bias because the studies were unblinded. Additionally, most studies did not control for potential confounding factors in study design or analysis. eDowngraded one level for inconsistency: considerable statistical heterogeneity (I2 = 79% for all ages; I2 = 85% for children under five).
Background
Description of the condition
Diarrhoeal disease is the fifth leading cause of death in low‐income countries (WHO 2020), and was responsible for approximately 1.5 million deaths globally in 2019 (GBD 2020; IHME 2019). Young children are particularly vulnerable and diarrhoeal disease is still the second leading cause of death in children under five years old globally (IHME 2019; WHO 2017). Additionally, as diarrhoeal diseases inhibit normal ingestion of foods and absorption of nutrients, repeated diarrhoea episodes can lead to malnutrition and stunted growth (Checkley 2008; Guerrant 2012), which could result in reduced resistance to infection, as well as impaired cognitive function later in life and lower adult economic productivity (Guerrant 2012). However, although young children are a particularly vulnerable population, diarrhoea can lead to morbidity and mortality amongst all ages. It is estimated that almost three‐quarters of the deaths due to diarrhoea worldwide occur in individuals over five years old, including a high burden in adults over 70 years of age (Troeger 2018).
The infectious enteric pathogens associated with diarrhoeal disease are transmitted primarily through the faecal‐oral route, and a wide variety of bacterial, viral, and protozoan pathogens excreted in the faeces of humans and animals cause diarrhoea (Feachem 1983). Some pathogens that may contribute to the greatest burden of diarrhoea include rotavirus, Cryptosporidium spp, certain pathogenic strains of Escherichia coli, Shigella, Campylobacter spp, Vibrio cholerae, Norovirus GII, and astrovirus (Kotloff 2013; Platts‐Mills 2015). However, the importance of individual pathogens likely varies between settings, seasons, and conditions.
Sanitation facilities are critical in reducing the transmission of enteric pathogens, as these facilities serve as a primary barrier to separate pathogens excreted in human faeces from the environment. However, despite major international efforts such as the past Millennium Development Goals (MDGs) and current Sustainable Development Goals (SDGs) to expand sanitation coverage, many still lack access to adequate sanitation facilities. In 2020, an estimated 1.7 billion people (21% of the world’s population) lacked access to basic sanitation service, an indicator used to measure progress under the SDG sanitation target, which is defined as a flush or pour‐flush facility that flushes to a piped sewer system, septic tank, or pit latrine; a pit latrine with a slab; a ventilated improved pit (VIP) latrine; or a composting toilet not shared with other households (WHO/UNICEF 2021). This includes an estimated 494 million people who still practise open defecation. Sanitation coverage is particularly low in the least developed countries, where only one in three people (31%) in rural areas and half in urban areas (48%) have access to basic sanitation services (43% of the total population). Regionally, the coverage is lowest in sub‐Saharan Africa, where only 33% of the population has access to basic sanitation (WHO/UNICEF 2021).
While access to and use of sanitation facilities is essential for containing human excreta, preventing exposure to faecal pathogens also requires attention to the safe management of faecal sludge as part of a comprehensive sanitation solution. Faecal sludge management applies both to on‐site facilities, such as pit latrines, as well as off‐site systems where sludge is flushed into sewers. Currently, only 54% of the world’s population uses a 'safely managed' sanitation service, the highest rung on the WHO/UNICEF sanitation ladder, which requires basic sanitation facilities where the excreta is safely disposed of in situ or is treated off‐site (WHO/UNICEF 2021).
Description of the intervention
Sanitation interventions are aimed at introducing, improving, or expanding coverage or use of facilities or systems for human excreta disposal and management. More specifically, sanitation interventions may include steps to reduce open defecation by constructing latrines or toilets, encouraging behaviour change to increase latrine or toilet use, as well as the upgrading of facilities to achieve a higher level of service. They may also include improvements to safely remove, convey, and treat faecal sludge, such as pit emptying and sewerage.
Several definitions for the level of sanitation service are relevant for this review, as interventions are often described in terms of these definitions. The Joint Monitoring Programme for Water Supply, Sanitation and Hygiene (JMP), which monitors progress towards international water, sanitation, and hygiene targets, has several definitions of sanitation that are commonly used in studies. Prior to the SDGs, the JMP defined improved sanitation and unimproved sanitation in terms of the facilities for the disposal of human excreta (WHO/UNICEF 2015), as follows.
Improved sanitation: a private flush or pour‐flush facility (that flushes to a piped sewer system, septic tank, or pit latrine), a pit latrine with a slab, a VIP latrine, or a composting toilet.
Unimproved sanitation: any other flush or pour‐flush facility (that flushes elsewhere), a pit latrine without a slab, a bucket latrine, a hanging latrine, any public or shared facility, or open defecation.
For monitoring the SDGs that began in 2016, new sanitation service levels were defined along a sanitation ladder, which users can move up as upgrades to sanitation are made. This ladder includes the five levels of service defined as safely managed, basic, limited, unimproved, and open defecation (WHO/UNICEF 2017), as follows.
Safely managed: use of improved facilities that are not shared and with excreta safely disposed of in situ or treated off‐site.
Basic service: use of improved facilities that are not shared.
Limited service: use of improved facilities that are shared with other households.
Unimproved service: use of pit latrines without a slab or platform, hanging toilets, or bucket toilets.
Open defecation: disposal of human faeces in fields, surface water, forests, bushes, or with solid waste.
Our systematic review will evaluate the following three separate types of sanitation interventions.
Interventions that move participants’ access to sanitation from open defecation (no sanitation facility) to any sanitation facility.
Interventions that improve participants’ existing sanitation facilities (whether these improvements lead to a defined higher level of service or not).
Interventions that encourage participants to increase or improve the use of existing sanitation facilities.
How the intervention might work
The infectious pathogens excreted in the faeces of humans and animals that cause diarrhoeal disease are transmitted primarily through the faecal‐oral route (Feachem 1983), with sanitation facilities acting as a primary barrier to contain faeces and prevent pathogens excreted in human faeces from entering the environment. If not properly contained, these pathogens may be transmitted through the ingestion of contaminated food, water, soil, by person‐to‐person contact, and by direct or indirect contact with infected faeces. Due to the complexity of multiple pathways, environmental interventions for the prevention of diarrhoeal disease often include steps to improve the proper disposal of human faeces through sanitation interventions, as well as improving water quality (Clasen 2015), water quantity and access (Stelmach 2015), and promoting handwashing (Ejemot‐Nwadiaro 2021) and other hygiene practices (collectively referred to as WASH). Although this review will focus only on evaluating sanitation interventions and will not include the evaluation of other individual WASH interventions, the effectiveness of individual sanitation interventions may vary between settings due to exposure to pathogens from other transmission pathways not addressed by a sanitation intervention. However, understanding the effect of sanitation interventions alone compared to other individual or combined WASH interventions assessed in other reviews can help policymakers prioritise interventions.
In addition to diarrhoea, there are other important health risks associated with poor sanitation. These include the infectious diseases of schistosomiasis, soil‐transmitted helminth infection (including ascariasis, trichuriasis, and hookworm infection), and trachoma, as well as nutritional status (Freeman 2017). Nutritional status could be affected from repeated diarrhoea episodes or soil‐transmitted helminth infection (Bethony 2006; Checkley 2008), as well as environmental enteric dysfunction (also called environmental enteropathy). Environmental enteric dysfunction is a subclinical disorder of the small intestine that leads to chronic gut inflammation and impaired nutrient absorption. Environmental enteric dysfunction is hypothesized to be caused by repeated ingestion of faecal bacteria and associated infection and is thought to lead to impaired growth (Humphrey 2009; Korpe 2012). There is also evidence that poor sanitation can adversely impact cognitive and motor development (Sania 2019; Sclar 2017). However, these health risks are outside the scope of this review.
Why it is important to do this review
This review supersedes a Cochrane Review (Clasen 2010). Clasen 2010, which used narrower study design criteria and identified only 13 eligible studies, concluded that while there was a wide range of effects and the certainty of the evidence was poor, there was some evidence that sanitation interventions to improve excreta disposal were protective against diarrhoea. However, many of the studies combined sanitation with other WASH interventions, thus preventing an estimate of the effect of sanitation alone. The review also found substantial heterogeneity in the interventions and methods of assessment that prevented a comparison of studies or the pooling of results and meta‐analysis. It concluded with a recommendation for rigorous studies across multiple settings to provide evidence to better assess the potential effectiveness of sanitation interventions on diarrhoea.
Several new studies have been published since the publication of Clasen 2010, including rigorous studies of sanitation interventions. In this Cochrane Review, we expanded the inclusion criteria to include controlled before‐and‐after and matched cohort studies; updated the search terms; extracted data from newly identified studies; and repeated data extraction from previously identified studies. We adopted the Cochrane tool to assess risk of bias and apply the GRADE approach to assess the certainty of the evidence. We also included meta‐analyses and subgroup analyses after the inclusion of new studies.
Objectives
To assess the effectiveness of sanitation interventions for preventing diarrhoeal disease, alone or in combination with other WASH interventions.
Methods
Criteria for considering studies for this review
Types of studies
We included randomized controlled trials (RCTs), quasi‐RCTs, non‐randomized controlled trials (NRCTs), controlled before‐and‐after studies (CBAs), and matched cohort studies. For randomized trials, we included studies with a unit of randomization of individuals, families, households, villages, communities, or other clusters. For cluster‐RCTs, we only included studies that had at least two clusters per arm. For CBAs, we only included studies that had at least two sites per arm and contemporaneous data collection in the intervention and control arms. For matched cohort studies, we only included studies that had at least two sites per arm. A matched cohort study is a rigorous observational study method that allows for causal inference to be assessed from a non‐randomized pre‐existing development intervention implemented at a group or community level (Arnold 2010). A quasi‐RCT refers to a controlled trial that uses a method of participant allocation that is not truly random, but that is intended to produce similar groups as randomization (for example, allocation by date of birth, medical record number, or every other person) (Cochrane Community 2018). We used Cochrane EPOC's definitions of NRCTs and CBAs to differentiate between the two study design types, with both types of studies including an intervention study with a control and intervention group that is non‐randomized and measures outcomes in both groups after (and sometimes before) the intervention (Cochrane EPOC 2019). However, if allocation of the intervention to control and intervention groups was made by the investigators, then we classified it as a NRCT and if allocation to control and intervention groups was not under the control of the investigator, then we classified it as a CBA. If the study did not report who allocated the intervention to control and intervention groups, we classified the study as a NRCT.
In this review, we expanded the inclusion criteria of Clasen 2010 to include controlled before‐and‐after and matched cohort studies, two types of relatively rigorous non‐randomized study designs. The inclusion of rigorous non‐randomized studies of sanitation interventions enables the review to address important interventions that are not readily randomized, such as municipal sewerage and other downstream measures to manage faecal sludge beyond the user interface. The differences they present from RCTs in terms of causal inference can be adequately managed by subgroup analysis and risk of bias assessment.
Types of participants
Children and adults in any country or population.
Types of interventions
Interventions
The interventions relevant to this review are aimed at introducing or expanding the coverage and/or use of sanitation facilities designed to reduce direct or indirect contact with human faeces. Our systematic review evaluated the following three separate types of sanitation interventions.
Providing access to any sanitation facility: interventions that provide participants who do not have access to a sanitation facility with access to some kind of sanitation facility. This includes constructing or subsidizing the construction of facilities for participants who practise open defecation.
Sanitation facility improvement: interventions that improve participants’ existing sanitation facility. This may include upgrading access to a higher level of service (as defined by JMP for SDGs monitoring), although this upgrade is not necessary for the intervention to be classified as a sanitation facility improvement. Additionally, this may include interventions that encourage the building of new facilities including pit latrines, VIP latrines, composting toilets, and water‐sealed flush or pour‐flush toilets, as long as the facility is an improvement over the existing facility. It may also include interventions to promote the safe management of faecal sludge, such as pit emptying, sewerage connection, and composting or other treatment that could upgrade the sanitation level of service. This also includes providing individual household latrines to participants relying on shared sanitation.
Behaviour change messaging only: behaviour change interventions that encourage participants to increase sanitation access or improve the use of existing sanitation facilities without providing or improving facilities or providing subsidies for the same. However, these interventions may still include messaging to encourage participants to build a latrine for themselves or upgrade their existing latrine with their own funds or labour.
As many sanitation interventions fell into multiple categories (for example, providing new latrine access in some intervention households that had previously been open defecating while also improving latrines in other intervention households that already had access to a sanitation facility), we also included a final comparison in our meta‐analysis that includes any of the foregoing interventions. We also assigned these studies to one of the above three categories for our meta‐analysis by sanitation intervention type based on what we assessed to be the primary sanitation intervention. If the intervention included components of providing new latrine access to some households and improving existing latrines of other households, we assigned it to the infrastructure category which most households fell into. If the intervention included infrastructure and behaviour change components, we assigned the study to the relevant infrastructure category.
We included sanitation interventions whether they were conducted independently or in combination with other interventions, such as interventions to improve water quality, water quantity or access, hygiene practices, and/or child nutrition. We encountered some studies with multiple intervention groups, such as studies with one arm receiving a sanitation intervention and another arm receiving a sanitation intervention coupled with water and hygiene interventions, with each compared to the same control arm. In such cases, we extracted the data comparing the sanitation‐only arm to the control arm to include in our analysis of sanitation‐only interventions, and extracted the data comparing the combined water, sanitation, and hygiene arm to the control arm to include in our analysis of combined sanitation intervention with water and/or hygiene interventions.
We excluded interventions aimed solely at the safe disposal of child faeces, such as the promotion of potties, unless safe disposal of child faeces was part of a larger sanitation intervention covering adults and children. We also excluded interventions aimed solely at the containment of animal faeces. Although faeces from young children and animals may be important sources of exposure to faecal pathogens capable of infecting humans, other reviews focus specifically on the disposal of faeces from children (Majorin 2019) and animals (Penakalapati 2017). Finally, this review did not extend to interventions that are not aimed principally at the sanitary disposal and management of human faeces, thus it does not include efforts to promote the use of human waste in agricultural applications, or efforts to improve drainage, recycling or reuse of wastewater or stormwater, or management of solid waste.
Control
Study participants who practise open defecation or who continue to follow their current practices with respect to excreta disposal or faecal sludge management rather than the prescribed intervention. We excluded any controls that received a separate intervention to reduce diarrhoea that was not also introduced to the intervention arm. However, we included controls that received a separate intervention to reduce diarrhoea if that intervention was also introduced into the intervention group alongside the sanitation intervention.
Types of outcome measures
Primary outcomes
Diarrhoea amongst individuals, whether or not confirmed by microbiological or clinical examination.
The World Health Organization (WHO) definition of diarrhoea is three or more loose or fluid stools (that take the shape of the container) in a 24‐hour period (WHO 1993). However, we defined diarrhoea and an episode in accordance with the case definitions used in each study. We excluded studies that had no clinical outcomes, for example studies that reported only on microbiological pathogens in the stool. Where data are provided, we extracted and analysed data from the studies describing the method of diarrhoea surveillance and reporting, as well as persistent diarrhoea, the appearance of dysentery or blood in stool, and hospital admission or clinical visits in response to diarrhoea.
Secondary outcomes
Mortality (all‐cause or diarrhoea‐related).
Persistent diarrhoea (episodes continuing for 14 days or longer).
Dysentery (bloody diarrhoea).
Hospital or clinical visits for diarrhoea (inpatient or outpatient).
Adverse events (harmful effects of an intervention).
Studies that did not report on one of the above primary or secondary outcomes were excluded. If a study mentioned that they collected data for one of the above outcomes but did not report data for the outcome directly (for example, if the study used diarrhoea information to calculate a larger child health index), then we contacted the study authors to attempt to obtain the relevant outcome results from them and only excluded the study if we were unable to obtain outcome results for at least one of the primary or secondary outcomes.
Search methods for identification of studies
We attempted to identify all relevant studies regardless of language or publication status (whether published, unpublished, in press, or ongoing).
Electronic searches
We searched the following databases using the search terms detailed in Appendix 1: Cochrane Infectious Diseases Group Specialized Register; Cochrane Central Register of Controlled Trials (CENTRAL) published in the Cochrane Library; MEDLINE; Embase; and LILACS (Latin American and Caribbean Health Science Information database). We also searched Chinese language databases available under the China National Knowledge Infrastructure (CNKI‐CAJ) using comparable Chinese language search terms. We also searched the metaRegister of Controlled Trials (mRCT) using ‘diarrhoea’ and ‘sanitation or latrine or toilet or privy or disposal or sewerage’ as search terms. Databases were searched from their inception until the search date. All databases were searched on 16 February 2022.
Searching other resources
Conference proceedings
We searched the conference proceedings of the following organizations for relevant abstracts: International Water Association and the Water, Engineering and Development Centre, Loughborough University, UK.
Researchers and organizations
We contacted individual researchers working in the field, as well as the following organizations for ongoing or unpublished studies: the Water, Sanitation and Health Programme of the WHO; World Bank Water and Sanitation Program; UNICEF Water, Sanitation and Hygiene; Environmental Health Project; IRC International Water and Sanitation Centre; Foodborne and Diarrheal Diseases Branch, Division of Bacterial and Mycotic Diseases, Centers for Disease Control and Prevention (CDC); US Agency for International Development (USAID); and the UK Department for International Development (DFID).
Reference lists
We checked the reference lists of all studies identified by the above methods.
Data collection and analysis
Selection of studies
Two review authors independently screened the titles and abstracts identified by the searches and selected all potentially relevant studies. After obtaining the full‐text articles of these studies, two review authors independently assessed each study to determine if it met the inclusion criteria by completing an eligibility form. For Chinese language search results, two review authors fluent in Chinese (WY and JL) undertook the same process individually to independently determine the eligibility of the study. This process was supervised by VB, who made the final decision about study eligibility.
Review author TC had been involved in studies that met the inclusion criteria of this review. To help ensure independence on assessment of eligibility and risk of bias, we assigned review authors who were not involved in any of these included studies to tasks for studies that involved a review author. Furthermore, no author of an included study performed any data extraction on their own study.
We resolved any disagreements regarding study eligibility between independent review authors by consulting review author VB. We listed any studies excluded after full‐text assessment and discussion with third review author VB and the reasons for their exclusion in the Characteristics of excluded studies tables.
Data extraction and management
Two data extractors used a pre‐piloted form to independently extract and record the data described in Appendix 2, under the supervision of VB. When discrepancies arose from data extraction, one review author (VB) assessed the item in question, discussed it with the two data extractors, and made the final decision. As an additional quality control measure, review author VB checked that outcome data for meta‐analysis was correctly extracted from all English and French studies regardless of whether there was a discrepancy and discussed the extracted data with the extractors for the Chinese language studies. One review author (VB) entered the extracted data into RevMan 2020.
Assessment of risk of bias in included studies
We used the Cochrane risk of bias assessment tool to assess the risk of bias for RCTs (Higgins 2011). Specifically, we assessed risk of bias for the following six criteria for RCTs:
random sequence generation;
allocation concealment;
blinding of participants and personnel;
blinding of outcome assessment;
incomplete outcome data; and
selective reporting.
We assessed each criterion as either at low, high, or unclear risk of bias based on Cochrane risk of bias tool guidelines. For cluster‐RCTs, we also assessed the following five risk of bias criteria recommended for cluster‐RCTs in the Cochrane Handbook for Systematic Reviews of Interventions:
recruitment bias;
baseline imbalance;
loss of clusters;
incorrect analysis; and
comparability with individually randomized trials.
For other study designs (quasi‐RCTs, non‐randomized controlled trials, CBA studies, and matched cohort studies), we used the Cochrane Effective Practice and Organisation of Care (EPOC) tool to assess the risk of bias (Cochrane EPOC 2017), which included an assessment of random sequence generation, allocation concealment, incomplete outcome data, selective reporting, and other biases, criteria that are similar to those assessed for RCTs, as well as the following criteria.
Baseline outcome measurements similar: we assigned low risk if there were no important differences between groups at baseline for diarrhoea measurement or if adjusted analysis was performed to account for this difference; unclear risk if no baseline measures were taken for these variables; or high risk if important differences were present and not corrected for in analysis.
Baseline characteristics similar: we assigned low risk if there were no important differences between groups at baseline for age category, socioeconomic status, access to water, hygiene practices, or sanitation facilities or if adjusted analysis was performed to account for this difference; unclear risk if no baseline measures were taken for these variables; or high risk if important differences were present and not corrected for in analysis.
Protection against contamination: we assigned low risk if allocation was assigned by community or group in a manner such that it is unlikely that the control group received the intervention; unclear risk if it is possible that the control group received the intervention; and high risk if it is likely that the control group received the intervention.
For other sources of bias of quasi‐RCT, NRCT, CBA, and matched cohort study designs, we evaluated whether confounders were controlled for or if there were any other major sources of bias identified that were unique to the study. For potential confounders, we considered age category, socioeconomic status, and access to water, hygiene practices, or sanitation facilities. We assigned low risk if the study controls for all the relevant listed confounders in the design (for example, matching) or the analysis (for example, multivariable statistical modelling), high risk if no adjustment for confounding variables was conducted, and unclear risk if it was not mentioned in the paper or if only some, but not all, of the relevant confounders listed above were adjusted for.
Two review authors (VB and FM) independently reviewed the risk of bias criteria and resolved any disagreements by discussion amongst each other or by consulting a third review author (TC) if necessary.
Measures of treatment effect
We recorded diarrhoea morbidity based on the measure used in the study. We expected that we would encounter studies that measure and report diarrhoea prevalence as a dichotomous outcome, as well as studies that measure and report diarrhoea incidence as a count outcome. We did not pool results based on these different measures of disease frequency. Rather, we assessed which outcome is more commonly used by studies and attempted to convert the effect measures for other studies to a similar form for meta‐analysis. In other words, we attempted to convert the effect measures for each study into a relative risk with 95% confidence interval (CI) for diarrhoea. If the relative risk was not reported in the study, we attempted to calculate it from the reported data. If the relative risk or the raw data necessary to calculate it were not reported, we attempted to obtain these data by contacting the study author. If we were unable to obtain these data, then we used the effect measure reported in the study.
Unit of analysis issues
For cluster‐RCTs and other studies that included clusters (such as NRCTs), we assessed whether the statistical methods used properly accounted for the cluster design, and then extracted the effect measure and confidence interval reported from analysis that accounts for the cluster design in an attempt to avoid unit of analysis errors. In cases where measures of effect were not adjusted for clustering in a cluster‐RCT or other clustered study, we attempted to adjust the data using an intracluster correlation coefficient (ICC). If an ICC was not reported in the study, we used an external estimate of an ICC from a similar study to adjust the data and reported our assumed ICC in a footnote on the relevant analysis forest plot. We did not include any unadjusted measures of effect from cluster‐RCTs or other clustered studies in our meta‐analyses.
When outcomes were measured and reported at multiple post‐intervention time points, we used the data with the longest follow‐up period for determining the effect measure, when possible. However, if a study only reported combined data from multiple time points and there was not enough information to calculate an effect measure for the longest follow‐up period, then we used the effect measured for the combined data.
Dealing with missing data
In the case that data needed to assess eligibility criteria or the outcomes were missing, we attempted to contact study authors to obtain the missing data. We report the number of participants in each study as well as the number lost to follow‐up. We also evaluated whether the missing data from participants lost to follow‐up were likely to be missing at random or not.
Assessment of heterogeneity
We assessed heterogeneity amongst studies by visually examining the confidence intervals for overlap on forest plots, using the Chi2 test, and calculating the I2 statistic. We applied the Chi2 test with an assumption that a P < 0.10 is significant and indicates potential heterogeneity. We used the I2 statistic to quantify the level of heterogeneity present, estimating that an I2 value of 75% or greater indicates considerable heterogeneity based on cutoffs given in the Cochrane Handbook for Systematic Reviews of Interventions (Section 10.10.2) while also considering that complex environmental health interventions like sanitation are inherently heterogeneous (Murad 2017). We also prespecified in our protocol that we would explore methodological heterogeneity as a possible explanation for any observed heterogeneity in outcome results, including methodological reasons such as differences in study participants, interventions, and levels of diarrhoea prevalence in controls.
Assessment of reporting biases
When sufficient data were available (10 or more included studies), we assessed potential publication bias by creating funnel plots and visually inspecting the plots for asymmetry. When sufficient data were not available to construct funnel plots, we assessed potential publication bias by plotting the relative risk against the number of clusters in each study, as done in the previous version of this review (Clasen 2010). To assess for potential selective reporting of outcomes, we also compared the outcomes listed in the published protocol or methods sections to the study results outcomes presented.
Data synthesis
We compiled and analysed data using RevMan 2020. We stratified our primary analysis by study design and the type of sanitation intervention being evaluated. We performed a meta‐analysis to estimate a pooled effect measure for outcomes. We used random‐effects models for all meta‐analyses to incorporate heterogeneity into the analysis.
Subgroup analysis and investigation of heterogeneity
We identified sufficient studies to perform subgroup analysis by the following:
outcome assessment by age of the participant (grouping by children under five years versus all ages);
study design (cluster‐RCTs versus non‐randomized designs);
sanitation coverage levels (including the change in coverage level due to the intervention and the coverage level at the end of the study); and
length of follow‐up (the amount of time that passed from when the intervention was delivered until the health outcomes were measured).
Sensitivity analysis
We conducted a sensitivity analysis to see if using a fixed‐effect model instead of a random‐effects model would have influenced the results. We also checked if grouping interventions in schools and households together impacted the results.
Summary of findings and assessment of the certainty of the evidence
We used the GRADE approach to assess the overall certainty of the evidence for each outcome as either high, moderate, low, or very low certainty (Guyatt 2011). As prespecified in our protocol, we started with a ‘high’ certainty rating for outcomes with results from RCTs, quasi‐RCTs, non‐randomized controlled trials, CBA studies, and matched cohort studies. Following the GRADE approach, we downgraded the certainty of the evidence by one level for each serious risk and two levels for each very serious risk of any of the following criteria: (1) risk of bias, (2) inconsistency, (3) indirectness, (4) imprecision, or (5) publication bias (Guyatt 2011) as detailed below. We reported the results of this assessment for each outcome in the summary of findings tables.
We created summary of findings tables using RevMan 2020. We only summarized the evidence for our primary outcome of diarrhoea in these tables, because few studies measured our secondary outcomes and, when reported, they were typically secondary outcomes that the study was not adequately powered for.
We used the following criteria to complete GRADE assessment of our outcomes in the summary of findings tables:
Risk of bias: We downgraded the outcome by up to two levels for very serious risk of bias. We downgraded the outcome one level for serious risk of bias if most studies used a self‐reported/not objective diarrhoea outcome that was susceptible to bias due to the studies being unblinded. Additionally, we downgraded the outcome by an additional level for very serious risk of bias if most studies for the outcome did not account for potential confounders either through study design (RCTs) or statistical analysis (non‐randomized designs).
Inconsistency: We downgraded the outcome one level if there was considerable (I² of 75% or greater) heterogeneity that cannot be explained through subgroup analyses.
Indirectness: We downgraded the outcome if there were limited populations or settings in the included the studies for an outcome, which did not allow us to make generalizations about the findings to other settings relevant to this review.
Imprecision: We downgraded the outcome if the studies had a small sample size and large confidence intervals that included important effects in both direction (at least a 25% increase and decrease in risk (that is, ≤ 0.75 and ≥ 1.25)).
Publication bias: We downgraded the outcome if there was evidence of publication bias based on visual inspection of funnel plots and the published evidence includes a number of small studies, which are industry‐funded.
Results
Description of studies
Results of the search
The searches identified 13,639 separate records, including 5257 from English databases, 8152 from Chinese databases, and 230 from other sources (160 from trial registers, 38 from manually checking the references of included studies, 14 from manually checking the references of other systematic reviews, five from researchers contacted, 10 from conference abstract searches, and three from the authors' knowledge of sanitation studies). We screened all titles and abstracts, and further assessed the full text for 325 articles. Of these, 51 met the inclusion criteria (see Figure 1).
1.
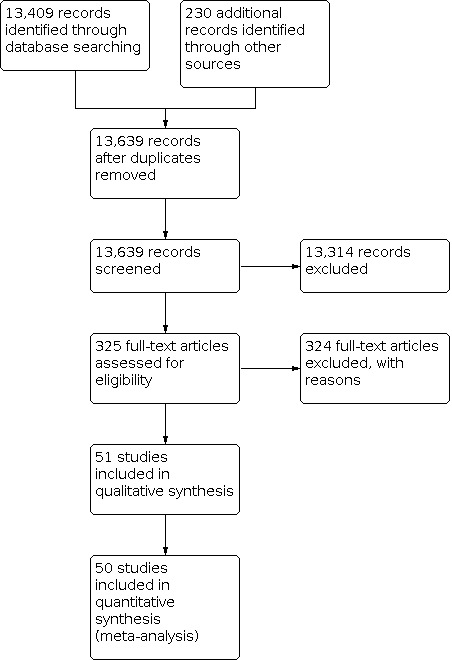
PRISMA flow diagram
Included studies
The 51 included studies included a total of 238,535 participants (see Characteristics of included studies table). Of these, 50 studies had sufficient information to be included in quantitative meta‐analysis, including 17 cluster‐RCTs and 33 studies with non‐randomized study designs (20 were non‐randomized controlled trials (NRCTs), one was a controlled before‐and‐after study (CBA), and 12 were matched cohort studies). Huttly 1990 was only included in qualitative synthesis, as it reported insufficient information to calculate the standard errors or 95% confidence intervals associated with the reported effect measures needed for quantitative synthesis. Studies were primarily in LMICs and spanned several regions, with 17 (33%) in sub‐Saharan Africa, 16 (31%) in East Asia and Pacific, 10 (20%) in South Asia, three (6%) in Latin America & the Caribbean, three (6%) in the Middle East and North Africa, and two (4%) in North America.
Types of interventions by study design
Comparison 1: Providing access to any sanitation facility
Sixteen studies assessed interventions to provide access to sanitation facilities in settings where the population relied primarily on open defecation. This included 15 studies covering 73,511 participants that were included in quantitative meta‐analysis synthesis as well as one study of an estimated 1405 participants that could only be included in qualitative synthesis. The sanitation facilities varied significantly among studies, from government‐supported construction of improved household latrines to community toilets as an alternative to open defecation. Coverage and adoption of the intervention varied. While interventions were primarily at the household level, three were at schools.
Cluster‐RCTs
There were seven cluster‐RCT studies that primarily evaluated interventions intended to provide a sanitation facility to participants with little or no access to a sanitation facility (that is, practised open defecation). These were sometimes done in combination with other types of sanitation interventions (like Community‐Led Total Sanitation or CLTS) or WASH interventions (like water supply improvements).
Clasen 2014, Hammer 2016, and Patil 2014 were all cluster‐RCTs in rural India evaluating India's Total Sanitation Campaign (TSC). For Clasen 2014, this included latrine promotion and construction as well as subsidies for below‐poverty‐line households. The intervention was similar for Hammer 2016, where TSC included latrine promotion through CLTS style activities as well as the construction of fully subsidized standard TSC brick household pit latrines. For Patil 2014, the TSC intervention included subsidies for construction and promotion of improved household latrines as well as school sanitation and hygiene education, Anganwadi (preschool) latrines, and community sanitation complexes. Subsidies were provided to households below the poverty line to construct a two‐pit latrine with water seal and a brick walled superstructure. The TSC also included several features such as ongoing social mobilization and behaviour change activities.
Humphrey 2019 was a cluster‐RCT in rural Zimbabwe. The sanitation intervention included construction of ventilated improved pit latrines. The intervention also included other WASH components related to drinking water treatment as well as handwashing and other hygiene. One intervention arm included the WASH intervention and one intervention arm included the WASH intervention in combination with a nutrition intervention.
Freeman 2014 was a cluster‐RCT in rural Kenyan schools. The sanitation intervention included the installation of ventilated improved pit latrines in schools. The intervention also included other WASH components, including the promotion of handwashing and water treatment. The study included two separate evaluations of interventions: one in water‐available schools (Freeman 2014a) and one in water‐scarce schools (Freeman 2014b). In water‐scarce schools, an additional water supply intervention was also included in the intervention package.
Chard 2019 was a cluster‐RCT in Laos primary schools. The sanitation intervention included the installation of school sanitation facilities, which consisted of three separate toilet compartments designated for boys, girls, and disabled students. The sanitation intervention also included a software component to encourage toilet cleanliness by organizing student teams to clean and maintain toilets. Additionally, the intervention included other WASH components related to provision of a school water supply, installation of handwashing stations, and hygiene education.
Non‐randomized study designs
There were nine non‐randomized studies that primarily evaluated interventions that moved participants' access from no sanitation facility to any sanitation facility, including five NCRTs, three matched cohort studies, and one CBA study. Similar to cluster‐RCTs, these were sometimes done in combination with other types of WASH interventions.
Arnold 2010 and Reese 2019 were both matched cohort studies in rural India. Arnold 2010 evaluated a sanitation intervention that included community mobilization campaigns to build toilets, formation of village water and sanitation committees, construction or renovation of primary school toilets, formation of self‐help groups to promote toilet use and construction, technical support and local training for toilet construction, capital cost assistance with subsidized loans for some families, and certification of villages as open defecation‐free. The sanitation intervention was conducted in combination with water and hygiene interventions. Reese 2019 instead evaluated a sanitation intervention that was combined with a water supply intervention and had the following intervention components: (1) a household pour‐flush latrine with dual soak‐away pits, (2) an attached bathing room, and (3) household piped water connections in the latrine, bathing room, and kitchen. Households needed to construct their own toilet and bathing rooms while the programme provided the installation of a piped water system. All households in a village needed to complete construction of their household latrine before the village water supply was turned on.
Two further studies evaluated sanitation interventions in Asia. Aziz 1990 was a cluster NRCT in rural Bangladesh. The sanitation intervention included the installation of a locally manufactured double pit water‐sealed latrine and messaging about the need for all the members of the household, including young children, to use sanitary latrines. The latrines were installed at no or nominal cost, but the users had to install the superstructures or contribute towards their installation. The sanitation intervention was conducted in combination with water and hygiene interventions. Azurin 1974 was a cluster NCRT in urban and peri‐urban Philippines, which evaluated a sanitation intervention that included the installation of community toilets (one toilet for every 25 to 30 residents) in communities that had no previous sanitation. One cluster of the trial received the sanitation intervention alone and one cluster received the sanitation intervention in combination with a piped water intervention.
Four studies evaluated sanitation interventions in rural sub‐Saharan Africa, three at the household level and one at the school level. Garrett 2008 was a cluster NRCT in rural Kenya, which evaluated a sanitation intervention that included the promotion of latrines with cement sanitary platforms and VIP latrines, as well as education about the link between sanitation and health. The programme paid for 40% of latrine costs and community members paid for 60% of costs and provided the labour. The sanitation intervention was conducted in combination with a water supply and quality intervention. Messou 1997 was a cluster NRCT in rural Côte d'Ivoire, which evaluated a sanitation intervention that included the construction of latrines. The intervention also included other WASH components, including water supply improvement and health education. Huttly 1990 was a CBA study in rural Nigeria, which evaluated a sanitation intervention that included the promotion and construction of VIP latrines. The intervention also included other WASH components, including the water supply improvement and health and hygiene education. Boubacar Maïnassara 2014 was a cluster NRCT in Niger, which evaluated a sanitation intervention that included the construction of latrines in schools and messaging regarding the use of latrines. The sanitation intervention was conducted in combination with water and hygiene interventions.
Pradhan 2002b was a matched cohort study in rural and urban Nicaragua. The sanitation intervention included investments from a social fund for public access latrine facilities at the request of local communities.
Comparison 2: Sanitation facility improvement
Twenty‐six studies covering 132,539 participants assessed interventions designed to improve participants’ existing sanitation facilities. This consisted primarily of upgrading latrines in some way, though not necessarily to the level of improved sanitation. In some cases, the intervention included upgrades to faecal sludge management such as biogas digesters or sewerage connections. Once again, coverage and actual adoption of the intervention varied, if reported at all. While interventions were primarily at the household level, some were at schools.
Cluster‐RCTs
There were three cluster‐RCT studies that primarily evaluated interventions that improved participants' sanitation facilities. Two of these studies were part of the WASH Benefits trial. Luby 2018 evaluated a sanitation intervention in rural Bangladesh that included providing households with new or upgraded household latrines, sani‐scoops (a hand tool to remove faeces from the compound), potties for children under three years, and behaviour change promotion to encourage use, cleaning, and proper maintenance of latrines as well as safe disposal of faeces into latrines. If the household had an existing latrine, latrines that did not have a slab, a functional water seal, or did not prevent surface runoff of a faecal stream into the community were replaced. If the household did not have a latrine, then a double pit latrine with a water seal was constructed. Similarly, Null 2018 evaluated a sanitation intervention in rural Kenya that included providing households with new or upgraded household latrines, sani‐scoops, potties for children under three years, and behaviour change promotion to encourage latrine use and safe disposal of faeces into latrines. If the household had an existing unimproved latrine, the latrine was upgraded to an improved latrine by installing a plastic slab. If the household did not have a latrine or the existing latrine was unlikely to last for two years, then an improved latrine was constructed. For both studies, one study arm included only the sanitation intervention, another WASH study arm included the sanitation intervention in combination with water storage and treatment and handwashing interventions, and a third study arm included all WASH components in combination with a nutrition intervention.
Quattrochi 2021 reported the third study, a cluster‐RCT in rural Democratic Republic of Congo that evaluated a combined WASH intervention as part of a national programme known as ‘Healthy Villages & Schools’. The sanitation intervention included $2000 USD in financing for new or improved sanitation infrastructure and training for volunteers on maintenance of latrines and sanitation. It was conducted in combination with water and hygiene interventions.
Non‐randomized study designs
There were 23 non‐randomized studies that primarily evaluated interventions that improved participants' sanitation facilities, including 13 NCRTs, nine matched cohort studies, and one CBA study. These were sometimes done in combination with other types of WASH interventions.
Fourteen of the studies were conducted in China, including 13 in rural and one in urban areas. Five of these studies in rural China were matched cohort studies. Cao 2007 evaluated a sanitation intervention that included the installation of biogas toilets, which was an upgrade from non‐leaking pit latrines that households had before the intervention. One cluster of the trial received the sanitation intervention alone and one cluster received the sanitation intervention in combination with a water supply intervention. Similarly, Jin 2009 evaluated a sanitation intervention that included the installation of a sanitary latrine at households, which was typically a biogas toilet. One study arm included only the sanitation intervention and another study arm included the sanitation intervention in combination with a water supply improvement intervention. Li 2009 evaluated the installation of improved household toilets. Lin 2013 also evaluated the installation of improved toilets (flushing toilets with either septic tanks or double vault funnels). One study arm included only the sanitation intervention and another study arm instead included the sanitation intervention in combination with a water supply improvement intervention. Wen 2005 evaluated a sanitation intervention that included the installation of upgraded toilet and faecal sludge management facilities. Sanitation facilities varied across villages but were either double vault funnel toilets, three grate compost toilet, or toilets with a biogas digester.
Another six of the studies in rural China were cluster NRCTs evaluating sanitation improvements in households. Lou 1989 evaluated a sanitation intervention that included the installation of improved double vault funnel toilets with slab in 90% of intervention households. The intervention also included water supply improvements. Xing 2002 evaluated the installation of upgraded toilets with faecal sludge treatment. The intervention also included other WASH components, including water supply improvements and promotion of personal hygiene and sanitation. Xu 1994 evaluated the installation of upgraded toilet facilities in households to safely dispose of faeces. The type of sanitation facility installed varied across villages, but was either a composting double vault funnel toilet, a three layer septic tank toilet, or toilets with a biogas digester. Yan 1986 evaluated the installation of upgraded household toilet facilities that were double vault funnel toilets. Zhang 2000 evaluated the installation of improved double vault funnel toilets with a cement slab in households. The intervention also included water supply improvements. Zhou 1995 evaluated a sanitation intervention that included the installation of upgraded toilet facilities with septic tanks, supervision of households to ensure that toilets were cleaned regularly, and regular emptying of septic tanks.
Two of the cluster NRCT studies in rural China evaluated sanitation improvements in schools. Wei 1998 evaluated a combined school‐based WASH intervention. The sanitation intervention included making improvements to toilet facilities to improve the cleanness of the toilet and the faeces treatment, such as upgrading facilities to new flush toilets with septic tanks. The intervention also included water quality and hygiene improvements in the schools. Zhu 1997 evaluated the installation of improved toilets in schools, including treatment of the faecal sludge. The specific type of toilet and treatment varied across schools, but was either a flush toilet with composting or an enclosed pit latrine with faecal sludge treatment by heat or chemical. The intervention also included other WASH related components including the installation of handwashing stations, either the installation of water boiling facilities or instructions for children to bring clean drinking water to school for themselves, and health education.
Seven of the studies evaluated sanitation interventions in urban areas, including five evaluating installation of household sewerage connections. Klasen 2012 was a matched cohort study in urban Yemen with in two separate populations: a coastal region (Klasen 2012a) and a mountain region (Klasen 2012b). The sanitation intervention included household connections to a sewerage system connected to a wastewater treatment plant. The sanitation intervention was conducted in combination with a water supply intervention. Kolahi 2009 was a cluster NRCT in urban Iran that evaluated the provision of household connections to the urban sewerage system. Moraes 2003 was a cluster NRCT in urban Brazil that evaluated a sanitation intervention, which included the installation of a simplified sewerage system with household connections and drainage channels that sewerage flowed through before discharging into the local river. Pradhan 2002a was a matched cohort study in urban Nicaragua that evaluated investments from a social fund for sewerage projects for households to connect to with a flush toilet at the request of local communities.
The remaining two studies in urban areas included the installation of public or shared sanitation facilities. Xu 1990 was a cluster NRCT that evaluated a sanitation intervention in urban China that included the installation of upgraded public toilets that were three compartment composting toilets. Knee 2021 was a CBA study in urban Mozambique, which evaluated a sanitation intervention that included the installation of shared sanitation facilities including communal sanitation blocks in relatively larger compounds and shared latrines in relatively smaller compounds. Both communal sanitation blocks and shared latrines include flushing toilets with septic tanks, however intervention compounds receiving communal sanitation blocks also received water supply and hygiene infrastructure improvements as part of the intervention.
Two cluster NRCTs were conducted over 50 years ago in the rural USA. Mcabe 1954 evaluated a sanitation intervention that included providing households with new or upgraded household privies by constructing a new privy or rehabilitating the old privy with an 8‐foot‐deep bored hole. Privies were also remodelled at schools, churches, and commercial buildings. Rubenstein 1969 evaluated a sanitation intervention that was combined with a water supply intervention and included the construction of indoor plumbing lines (piped water and sanitation) to households.
Finally, Trinies 2016 was a matched cohort study in urban and rural Mali. The intervention was a combined school‐based WASH intervention that included components of sanitation improvement, hygiene improvement and education, water supply improvement and WASH governance/management at the school level. Sanitation improvements include the installation or rehabilitation of latrines.
Comparison 3: Behaviour change messaging only (no hardware or subsidy provided)
Nine studies covering 31,080 participants assessed interventions intended to promote sanitation through behaviour change without the provision or subsidizing of any facility or other hardware. This consisted of behaviour change, educational, social marketing, or other communication strategies designed primarily to encourage the target population to construct or upgrade facilities at the household or school and/or to use existing sanitation consistently.
Cluster‐RCTs
There were seven cluster‐RCT studies that primarily evaluated interventions of behaviour change messaging to increase use of existing or new sanitation facilities. These were sometimes done in combination with other WASH interventions.
Five of the trials were conducted in rural sub‐Saharan Africa. Briceno 2017 evaluated a total sanitation and sanitation marketing (TSSM) intervention in rural Tanzania which used a combination of CLTS and social marketing techniques to motivate households to move up the sanitation ladder. No subsidies were provided, although local masons were trained in latrine construction. One cluster of the trial received the sanitation intervention alone and one cluster received the sanitation intervention in combination with a handwashing intervention. Hashi 2017 evaluated a sanitation intervention in rural Ethiopia that included behaviour change messaging to promote having a latrine and using it properly. The intervention also included behaviour change messaging for other WASH related components including the promotion of safer water storage and handwashing at key times. Cha 2021 was also conducted in rural Ethiopia, and evaluated a CLTS programme focused on collective behaviour change to encourage community members to build improved toilets. No material or financial subsidies were provided for construction of household latrines. Pickering 2015 evaluated a sanitation intervention in rural Mali that was a CLTS intervention to end open defecation in villages. The programme did not provide any subsidies for latrine building and instead encouraged latrine designs built with local and available materials. Sinharoy 2017 evaluated a sanitation intervention in rural Rwanda that included community health clubs programmes that promoted WASH related health behaviours, including sanitation, drinking water quality, hygiene, and other health education. Sanitation messages included recommendations to not defecate in the open, to have children defecate in chamber pots, and to bury faeces if the household does not have access to a latrine.
Two trials were conducted in rural Asia. Cameron 2013 evaluated a TSSM sanitation intervention in rural Indonesia, which consisted of three main components: CLTS, social marketing of sanitation, and strengthening the enabling environment. The intervention is aimed at increasing the demand for sanitation and increasing the supply of sanitation products and services, and does not provide infrastructure or include subsidies for households. Dickinson 2015 evaluated a sanitation intervention in rural India that was a behaviour change intervention with CLTS style participatory activities to promote community‐wide latrine adoption, subsidies for households that were below the poverty line, promotion of health and non‐health benefits of latrine use.
Non‐randomized study designs
There were two cluster NRCT studies in rural Asia that primarily evaluated interventions of behaviour change messaging to increase use of existing or new sanitation facilities. Huda 2012 evaluated a sanitation intervention in rural Bangladesh that included behaviour change messaging to promote use of a hygienic latrine by all family members, properly cleaning and maintenance of the latrine, and construction of a new latrine when the pit fills up. The intervention also included behaviour change messaging for other WASH related components including drinking water and hygiene. Saha 2015 evaluated a sanitation intervention in rural India that included the promotion of low cost sanitary latrines.
Comparison 4: Any sanitation intervention compared to no intervention
The final comparison includes all 50 studies (237,130 participants) that met the review’s eligibility criteria for inclusion in the quantitative meta‐analysis for the primary outcome. In this way, it compares results from any sanitation intervention compared to no intervention. It is represented by 17 cluster‐RCTs and 33 non‐randomized studies described above. One CBA described above is excluded from this analysis due to insufficient information to include in the meta‐analysis, and therefore only qualitative results are presented from this study (Huttly 1990).
Primary outcome measure of diarrhoea
Of the 50 studies that measured diarrhoea, 21 used a definition of three or more loose or watery stools in a 24‐hour period, which is aligned with the WHO definition (Aziz 1990; Cao 2007; Cha 2021; Clasen 2014; Freeman 2014a; Freeman 2014b; Garrett 2008; Huda 2012; Humphrey 2019; Huttly 1990; Jin 2009; Kolahi 2009; Li 2009; Lin 2013; Pickering 2015; Reese 2019; Sinharoy 2017; Trinies 2016; Wei 1998; Wen 2005; Zhu 1997). An additional five studies used a similar definition of three or more loose or watery stools in a 24‐hour period or a single stool with blood or mucus (Arnold 2010; Briceno 2017; Cameron 2013; Knee 2021; Patil 2014). Five more studies had diarrhoea outcomes that were clinically confirmed and double‐checked through monthly household visits to ensure no cases were missed (Lou 1989; Xu 1994; Yan 1986; Zhang 2000; Zhou 1995), and one study had a diarrhoea outcome that was clinically confirmed (Xu 1990). Other definitions of diarrhoea included three or more loose stools within a 24‐hour period or at least one stool with blood (Luby 2018; Null 2018), looser than usual stool consistency and increased frequency, as noted by mothers/guardians (Moraes 2003), having diarrhoea (based on local terminology) and defecating three or more times in a 24‐hour period (Chard 2019), and cholera diarrhoea, defined as someone with gastrointestinal symptoms and a rectal swab positive for cholera vibrios (Azurin 1974).
Thirteen studies did not report the case definition used for diarrhoea in the study (Boubacar Maïnassara 2014; Dickinson 2015; Hammer 2016; Hashi 2017; Klasen 2012a; Klasen 2012b; Mcabe 1954; Messou 1997; Pradhan 2002a; Pradhan 2002b; Quattrochi 2021; Saha 2015; Xing 2002).
Excluded studies
We have described the 23 studies excluded after full‐text assessment in the Characteristics of excluded studies table. Common reasons for exclusion were the study not having an eligible study design (not a RCT, quasi‐RCT, NRCT, CBA, or matched cohort study), not having an eligible outcome (any of the primary or secondary outcomes defined above), or not including an eligible sanitation intervention. The reasons for excluding the remaining studies is summarized in Figure 1.
Risk of bias in included studies
Risk of bias for included studies is summarized in Figure 2 (cluster‐RCTs) and Figure 3 (non‐randomized studies), as well as in the Characteristics of included studies table.
2.
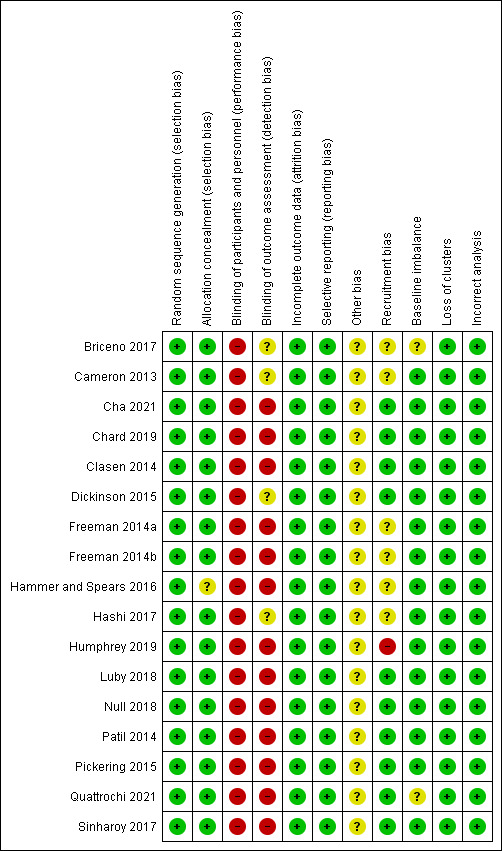
Risk of bias summary for cluster‐RCT studies: review authors' judgements about each risk of bias item for each included cluster‐RCT study.
3.

Risk of bias summary for non‐randomized study designs: review authors' judgements about each risk of bias item for each included non‐randomized study.
Allocation
Among cluster‐RCTs, we considered the method used to generate the random allocation sequence low risk for all studies. We considered all non‐randomized study designs (NRCTs, CBAs, matched‐cohorts) high risk. We considered concealment of allocation low risk for 18 studies, unclear risk for 16 studies, and high risk for 17 studies (including NCTs and CBAs of Huda 2012; Huttly 1990; Knee 2021; Moraes 2003; Rubenstein 1969). We also considered all matched cohorts studies high risk for concealment of allocation since the researchers selected control village by matching to villages that had previously received the intervention.
Blinding
It is not possible to blind sanitation interventions at the participant level. Most can also not be blinded at the field assessor level due to the presence of visible hardware or messaging within the village. For the criteria blinding of participants and personnel, we considered all cluster‐RCT studies high risk. Similarly, for the blinding of outcome assessment, we considered most high risk (13 studies), none low risk, and four unclear risk (Briceno 2017; Cameron 2013; Dickinson 2015; Hashi 2017).
Incomplete outcome data
Amongst cluster‐RCTs, we assessed the incomplete outcome data criteria as low risk for all studies. Among non‐randomized study designs (NRCTs, CBAs, matched‐cohorts) we considered incomplete outcome data low risk for 10 studies (Arnold 2010; Azurin 1974; Boubacar Maïnassara 2014; Knee 2021; Lou 1989; Reese 2019; Rubenstein 1969; Saha 2015; Trinies 2016; Zhang 2000), unclear risk for 22 studies (Aziz 1990; Cao 2007; Huda 2012; Huttly 1990; Jin 2009; Klasen 2012a; Klasen 2012b; Kolahi 2009; Li 2009; Lin 2013; Mcabe 1954; Moraes 2003; Pradhan 2002a; Pradhan 2002b; Wei 1998; Wen 2005; Xing 2002; Xu 1990; Xu 1994; Yan 1986; Zhou 1995; Zhu 1997), and high risk for two studies (Garrett 2008; Messou 1997).
Selective reporting
Almost all studies had low risk of selective reporting, including all cluster‐RCTs and all but four non‐randomized studies. Only one study had high risk (Kolahi 2009) and three studies had unclear risk (Knee 2021; Wei 1998; Zhang 2000).
Other potential sources of bias
No other sources of bias were identified for any cluster‐RCT studies. For non‐randomized studies, we considered adjustment of confounders in the assessment of other potential sources of bias. Considering these criteria, five studies included adjustment for potential confounders in the models and were at low risk (Arnold 2010; Garrett 2008; Knee 2021; Reese 2019; Trinies 2016), and 26 studies did not include any adjustment and we considered them high risk. We considered Pradhan 2002a and Pradhan 2002b unclear risk because while they adjusted for socioeconomic status/poverty at the village level in matching used in the matched cohort study, they did not adjust for potential confounders in analysis models.
Risk of bias specific to cluster‐randomized controlled trials
Amongst cluster‐RCTs, 10 were at low risk (Cha 2021; Chard 2019; Clasen 2014; Dickinson 2015; Luby 2018; Null 2018; Patil 2014; Pickering 2015; Quattrochi 2021; Sinharoy 2017), six were at unclear risk (Briceno 2017; Cameron 2013; Freeman 2014a; Freeman 2014b; Hammer 2016; Hashi 2017), and one was at high risk for recruitment bias (Humphrey 2019). For risk of bias associated with baseline imbalance, all were at low risk except for Briceno 2017 and Quattrochi 2021, which had an unclear risk. For loss of clusters, all were at low risk. When considering risk of bias from incorrect analysis, all were at low risk.
Risk of bias specific to non‐randomized studies
For the 'baseline outcome measurements similar' criteria, 10 were at low risk, 17 were at unclear risk, and seven were at high risk. For 'baseline characteristics similar', seven were at low risk (Arnold 2010; Knee 2021; Lou 1989; Reese 2019; Trinies 2016; Yan 1986; Zhu 1997), 25 were at unclear risk, and two were at high risk (Boubacar Maïnassara 2014; Saha 2015). For 'protection against contamination', 27 were at low risk and seven were at unclear risk.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4
Comparison 1: Providing access to any sanitation facility
Diarrhoea
In a pooled analysis across different study designs, interventions aimed at providing access to sanitation facilities in settings where the population relied primarily on open defecation were protective against diarrhoea (risk ratio (RR) 0.79, 95% confidence interval (CI) 0.66 to 0.94, 15 studies, 73,511 participants, Analysis 1.1). However, the effect was statistically significant only among non‐randomized studies (RR 0.72, 95% CI 0.53 to 0.97, 8 studies, 33,382 participants, Analysis 1.1.2) and not cluster‐RCTs (RR 0.89, 95% CI 0.73 to 1.08, 7 studies, 40,129 participants, Analysis 1.1.1). Amongst children under five years, the effect was not quite statistically significant for all pooled studies designs (RR 0.83, 95% CI 0.68 to 1.02, 11 studies, 25,614 participants, Analysis 1.2), or in either cluster‐RCTs or non‐randomized studies on their own (Analyses 1.2.1, 1.2.2). In the pooled analyses the I2 values suggest substantial heterogeneity among study results.
1.1. Analysis.

Comparison 1: Providing access to any sanitation facility intervention versus control, Outcome 1: Diarrhoea: all ages
1.2. Analysis.

Comparison 1: Providing access to any sanitation facility intervention versus control, Outcome 2: Diarrhoea: children < 5 years
Dysentery (bloody diarrhoea)
Only two studies reported the effects of interventions aimed at providing access to sanitation facilities on dysentery, including one cluster‐RCT and one NRCT. Both only reported the effects on children under five years. In a pooled analysis of these two studies, there was no evidence on an effect on dysentery in children under five years (RR 0.74, 95% CI 0.47 to 1.17; 5076 participants, Analysis 1.3), but the evidence was limited.
1.3. Analysis.

Comparison 1: Providing access to any sanitation facility intervention versus control, Outcome 3: Dysentery (bloody diarrhoea): children < 5 years (same for all ages)
Persistent diarrhoea
Only one NRCT study reported effects of an intervention to provide access to sanitation facilities on persistent diarrhoea, and it only reported this effect for children under five years (Aziz 1990). The intervention was protective against persistent diarrhoea in children under five in this study (RR 0.58, 95% CI 0.44 to 0.77; 1390 participants, Analysis 1.4), although the evidence was limited.
1.4. Analysis.

Comparison 1: Providing access to any sanitation facility intervention versus control, Outcome 4: Persistent diarrhoea: children < 5 years (same for all ages)
Hospital or clinical visits for diarrhoea
No studies measured the effect of interventions to provide access to sanitation facilities on hospital or clinic visits for diarrhoea.
Mortality
Three studies reported the effects of interventions to provide access to sanitation facilities on all‐cause mortality, and one study on diarrhoea‐related mortality. In a pooled analysis across different study designs, there was no evidence that the interventions had an effect on all‐cause mortality (RR 0.93, 95% CI 0.69 to 1.24; 25,229 participants, Analysis 1.5), although the evidence was limited. Results were similar for all‐cause mortality among children under five (RR 0.82, 95% CI 0.59 to 1.15; 8826 participants, Analysis 1.6), with limited evidence and no measured effect. The one study measuring the effect of this intervention on diarrhoea‐related mortality did find a large protective effect (RR 0.09, 95% CI 0.01 to 0.88; 1260 participants, Analysis 1.7), although this was a NRCT and the confidence interval was quite large (Messou 1997).
1.5. Analysis.

Comparison 1: Providing access to any sanitation facility intervention versus control, Outcome 5: All‐cause mortality: all ages
1.6. Analysis.

Comparison 1: Providing access to any sanitation facility intervention versus control, Outcome 6: All‐cause mortality: children < 5 years
1.7. Analysis.

Comparison 1: Providing access to any sanitation facility intervention versus control, Outcome 7: Diarrhoea‐related mortality: children < 5 years (same for all ages)
Adverse events
No studies reported adverse events from the intervention.
Narrative description
Cluster‐RCTs
Only one of the three trials in rural India found an effect on diarrhoea. Hammer 2016 found that the intervention reduced reported diarrhoea prevalence by 2.8 percentage points (standard error 0.013, P = 0.029). The intervention marginally increased latrine coverage from 14.6% of control households that owned a latrine to 22.8% of intervention households. However, Clasen 2014 found no evidence that the sanitation intervention reduced diarrhoea (prevalence ratio (PR) 0.97, 95% CI 0.83 to 1.12 for children under five years and 1.02, 95% CI 0.88 to 1.18 for all ages). Although latrine coverage and use improved in intervention arms, it still remained low overall with 36% of households having a functional latrine with signs of present use in the intervention arm compared to 9% in the control. Additionally, Patil 2014 found no evidence that the sanitation intervention reduced diarrhoea (diarrhoea incidence of 7.4% in the intervention group versus 7.7% in the control group; adjusted risk difference ‐0.002, 95% CI ‐0.019 to 0.015). However, although latrine coverage improved in intervention arms, it still remained low overall with 44.1% of households in the intervention group having a household latrine at endline compared to 24.2% in the control group. Open defecation also remained high with 74.6% of men, 73.2% of women, and 83.9% of children reporting practising open defecation at endline in the intervention group compared to 84.1%, 83.5%, and 89.2% in the control group.
Humphrey 2019 found that the WASH intervention had no effect on diarrhoea prevalence at either the 12‐month or 18‐month visits (PR 1.18, 95% CI 0.87 to 1.61) for the WASH arm at 12 months and PR 1.15, 95% CI 0.93 to 1.41) for the WASH and nutrition arm at 18 months). The intervention made substantial improvements in latrine coverage with 99% of households having access to an improved latrine in the intervention arms compared to 28% having access to an improved latrine and 32% having access to any latrine in the control arm.
For school‐based interventions, Freeman 2014a found evidence that the intervention reduced diarrhoea prevalence in water‐scarce schools where the intervention also included water supply improvements (adjusted RR 0.34, 95% CI 0.17 to 0.64), but not in water‐available schools (adjusted RR 0.88, 95% CI 0.60 to 1.28; Freeman 2014b). Dreibelbis 2014 also measured the effect of this school‐based intervention on diarrhoea prevalence in younger siblings (under five years old) of pupils enrolled in the intervention and also found reduced prevalence of diarrhoea for water‐scarce schools (odds ratio (OR) 0.45, 95% CI 0.27 to 0.73) but not water‐available schools (OR 0.77, 95% CI 0.51 to 1.14). However, as this Dreibelbis 2014 study measured "spillover effects" it was not eligible for inclusion per our review’s definition of sanitation intervention. In Laos primary schools, Chard 2019 found no evidence that the intervention reduced diarrhoea in schoolchildren (adjusted RR 0.80, 95% CI 0.51 to 1.26).
Non‐randomized study designs
Neither of the two studies in rural India reported an effect of the intervention on diarrhoea. Arnold 2010 found no difference in the prevalence of diarrhoea reported in the past two weeks for children under five years between intervention and control arms in unadjusted or adjusted models (adjusted longitudinal prevalence difference 0.003, 95% CI ‐0.001 to 0.008). However, it is important to note that the prevalence of diarrhoea was very low in both arms (1.96% in intervention, 1.67% in control children). The intervention increased latrine coverage from 26% among control households to 57% among intervention households. Reese 2019 found no evidence that the combined sanitation and water supply intervention reduced diarrhoea in children under five years (adjusted OR 0.98, 95% CI 0.77 to 1.25) or household members of all ages (adjusted OR 0.86, 95% CI 0.74 to 1.03). However, the intervention did improve sanitation coverage (85.0% of intervention households had an improved toilet compared to 17.7% of control households) and latrine use (59.3% of all ages reported to use latrine in intervention households compared to 12.9% in control households).
However, both of the other two studies in Asia did measure an effect of the intervention on diarrhoea. Aziz 1990 found that the intervention decreased the incidence of diarrhoea (incidence density ratio (IDR) 0.75, 95% CI 0.70 to 0.80), frequent diarrhoea (IDR 0.58, 95% CI 0.52 to 0.65), and dysentery (IDR 0.73, 95% CI 0.61 to 0.88) in children under five years. Although the sanitation coverage in the control group was not reported, it was stated that the intervention installed latrines in 92% of intervention households. Azurin 1974 found that both the sanitation‐only intervention and the sanitation intervention combined with water source improvements reduced the incidence of cholera (diarrhoea incidence of 7.4% in sanitation arm and 5.4% in combined arm versus 23.0% in control arm).
Results for the four studies in rural sub‐Saharan Africa were mixed, with two finding an effect on diarrhoea and two finding no effect. Garrett 2008 found evidence that the intervention reduced diarrhoea incidence in children under five years (adjusted RR 0.31, 95% CI 0.23 to 0.41). The intervention also increased latrine coverage with 49% of person‐weeks with working latrine observed in intervention villages compared to 27% in controls. Messou 1997 also found that the sanitation intervention reduced diarrhoea and diarrhoea‐related mortality (diarrhoea rate of 20% and 16% in intervention villages after the intervention compared to 25% in control villages; diarrhoea‐related mortality rate of 18% and 4% in intervention villages after intervention compared to 28% and 34% in control villages). However, sanitation coverage levels in intervention and control villages were not reported.
In contrast, Huttly 1990 did not find evidence that the intervention reduced the incidence of diarrhoea in children under six years (incidence of 3.19% and 2.08% in two intervention villages versus 2.51% and 2.91% in two control villages). While it was not reported how the intervention improved access to VIP latrines, the authors did note that the construction of VIP latrines had a delayed start and only 46% of households in the intervention area were using them at the end of the study. It was not reported how many households in the control area had access to VIP latrines at the end of the study, although at baseline 74% of children two to five years old and adults in control villages reported usually defecating in the bushes or fields. Boubacar Maïnassara 2014 also found no difference in the prevalence of diarrhoea between intervention and control arms (3.1% in intervention group versus 2.4% in control group). However, there was a reduction in the prevalence of diarrhoea noted for all pupils in both intervention and control arms after the project (3.9% before versus 2.7% after, P = 0.04).
The single study in Latin America found no evidence that the latrines intervention reduced diarrhoea in children under six years (diarrhoea incidence of 29.2% in intervention versus 24.5% in control group for the latrines intervention, P = 0.37) (Pradhan 2002b).
Comparison 2: Sanitation facility improvement
Diarrhoea
In the pooled analysis across study designs, interventions to improve sanitation facilities were protective against diarrhoea (RR 0.65, 95% CI 0.55 to 0.78, 26 studies, 132,539 participants, Analysis 2.1). Once again, however, the protective effect was stronger in non‐randomized studies (RR 0.61, 95% CI 0.50 to 0.74, 23 studies, 117,639 participants, Analysis 2.1.2), while results from the three cluster‐RCTs (all in children under five years) yielded a pooled effect that was not statistically significant (RR 0.85, 95% CI 0.69 to 1.06; 3 studies, 14,900 participants, Analysis 2.1.1). For children under five years, the pooled estimate denoted that the intervention is protective (RR 0.70, 95% CI 0.54 to 0.91; 12 studies, 23,353 participants, Analysis 2.2), though when separated this was only true for the non‐randomized studies (RR 0.85, 95% CI 0.69 to 1.06; 9 studies, 8453 participants, Analysis 2.2.2). Again, in the pooled analyses the I2 statistic suggests substantial heterogeneity across study results.
2.1. Analysis.

Comparison 2: Sanitation facility improvement intervention versus control, Outcome 1: Diarrhoea: all ages
2.2. Analysis.

Comparison 2: Sanitation facility improvement intervention versus control, Outcome 2: Diarrhoea: children < 5 years
Dysentery (bloody diarrhoea)
Only one NRCT study reported an effect of an intervention to improve sanitation facilities on dysentery (Zhou 1995). It found no evidence of an effect (RR 1.00, 95% CI 0.09 to 11.28, 19,991 participants, Analysis 2.3).
2.3. Analysis.

Comparison 2: Sanitation facility improvement intervention versus control, Outcome 3: Dysentery (bloody stool): all ages
Persistent diarrhoea
Again, only one NRCT study reported the effects of an intervention to improve sanitation facilities on persistent diarrhoea, and only reported this effect for children under five years (Moraes 2003). There was no evidence of an effect of the intervention on persistent diarrhoea in children under five in this study after correcting for clustering (RR 0.47, 95% CI 0.17 to 1.31, 1275 participants, Analysis 2.4), but the evidence was limited.
2.4. Analysis.

Comparison 2: Sanitation facility improvement intervention versus control, Outcome 4: Persistent Diarrhoea ‐ Children <5 years
Hospital or clinical visits for diarrhoea
Only two NRCT studies reported effects of interventions to improve sanitation facilities on clinic visits for diarrhoea, though several other studies included in the analysis for the main diarrhoea outcome above measured diarrhoea through a combination of clinic visit records and monthly household visits to capture all diarrhoea cases. There was no evidence of an effect on clinic visits for diarrhoea (RR 0.86, 95% CI 0.44 to 1.67, 3720 participants, Analysis 2.5). Additionally, only one NRCT study measured this effect in children (Rubenstein 1969). The Rubenstein 1969 study only measured clinic visits for diarrhoea in children under one year, finding no evidence of an intervention effect (RR 1.03, 95% CI 0.48 to 2.19, 121 participants, Analysis 2.6).
2.5. Analysis.

Comparison 2: Sanitation facility improvement intervention versus control, Outcome 5: Clinic visits for diarrhoea: all ages
2.6. Analysis.

Comparison 2: Sanitation facility improvement intervention versus control, Outcome 6: Clinic visits for diarrhoea: children < 5 years
Mortality
Three studies (two cluster‐RCTs and one NRCT) reported the effects of an intervention to improve sanitation facilities on all‐cause mortality, only measuring it in children under five years. In the pooled analysis, there was no evidence of an intervention effect (RR 1.00, 95% CI 0.75 to 1.34, 14,575 participants, Analysis 2.7).
2.7. Analysis.

Comparison 2: Sanitation facility improvement intervention versus control, Outcome 7: All‐cause mortality: children < 5 years (same for all ages)
Adverse events
No studies reported adverse events from the intervention.
Narrative description
Cluster‐RCTs
The evidence from the WASH Benefits studies was mixed, with one trial finding an effect on diarrhoea and one trial finding no effect. Luby 2018 found the sanitation intervention reduced diarrhoea prevalence in children compared to the control group at one‐year and two‐year follow‐up in all arms receiving the sanitation intervention (sanitation only arm PR 0.61, 95% CI 0.46 to 0.81, WASH arm PR 0.69, 95% CI 0.53 to 0.90, WASH + nutrition arm PR 0.62, 95% CI 0.47 to 0.81). This reduction occurred despite a relatively low diarrhoea prevalence of 5.7% in the control group. However, the reduction in diarrhoea prevalence in the combined WASH group was no larger than in the individual sanitation group. The sanitation intervention and combined WASH intervention had no effect on mortality, although mortality was reduced in the nutrition and WASH plus nutrition arms of the trial. Among all three arms that included the sanitation intervention, at least 94% of households within the arm had a latrine with a functional water seal at the time of outcome assessment compared to 31% or less in the control. Although not eligible for inclusion in our review, Benjamin‐Chung 2018 also measured the spillover effects of the WASH intervention on diarrhoea prevalence in children under five years in neighbouring compounds of those that received the intervention and found no effect on child diarrhoea (PR 1.06, 95% CI 0.76 to 1.47).
On the other hand, Null 2018 found the sanitation intervention had no effect on diarrhoea prevalence in children compared to the control group at one‐year and two‐year follow‐up in all arms receiving the sanitation intervention (sanitation only arm PR 0.99, 95% CI 0.88 to 1.10, WASH arm PR 0.96, 95% CI 0.86 to 1.07, WASH + nutrition arm PR 1.05, 95% CI 0.94 to 1.16). There was no reduction in diarrhoea here with a relatively high diarrhoea prevalence (27.1% in active control group) in comparison to the Bangladesh counterpart of this trial (Luby 2018), which found a diarrhoea reduction. The sanitation intervention and combined WASH intervention also had no effect on mortality in any arms. Among all three arms that included the sanitation intervention, at least 78% of households within the arms had access to an improved latrine at the time of outcome assessment compared to 20% or less in the control. One potential explanation for this difference in effects measured in each WASH Benefits settings is the increase in promoter contact in Bangladesh, where promoters visited households six times per month compared to monthly in Kenya (Pickering 2019).
Similar to the results of Null 2018, Quattrochi 2021 found no evidence that the sanitation intervention reduced diarrhoea (diarrhoea prevalence of 27% in intervention versus 32% in control group, risk difference ‐0.02, 95% CI ‐0.11 to 0.05). However, diarrhoea was a secondary outcome that the study was not powered for. Additionally, although access to improved latrines increased in the intervention arm, it still remained low overall with 46% of households in the intervention group having an improved sanitation facility at endline compared to 18% in the control group.
Non‐randomized study designs
All 13 studies in rural China reported evidence of an effect of the intervention on diarrhoea, however most of these were not statistically significant once effect measures were calculated that corrected for clustering (Analysis 2.1). Among matched‐cohort studies, Cao 2007 found that the combined sanitation and water supply intervention reduced diarrhoea incidence compared to villages that only received one of the interventions (sanitation or water supply) and control villages (Chi2 test, P < 0.05; incidence rate in villages with both interventions 0.17%, one intervention 0.93%, control 0.7%). However, there was no difference in diarrhoea incidence between villages receiving only one intervention and control villages. Wen 2005 found that the intervention reduced diarrhoea incidence by 42.62% in all residents (P < 0.0001, though it was unclear if this was a comparison at endline or a comparison of the baseline and endline values combined). Jin 2009 found that the sanitation intervention significantly reduced diarrhoea prevalence compared to villages receiving no intervention (diarrhoea prevalence in intervention villages was 0.91% compared to 1.30% in control villages, P < 0.01). However, there was no difference in diarrhoea prevalence between villages receiving both water and sanitation interventions compared to villages receiving only one intervention (diarrhoea prevalence in villages receiving both was 0.70%, P > 0.05). Li 2009 found that the improved latrines intervention decreased diarrhoea incidence (3.35% in intervention compared to 7.22% in control villages, P < 0.05). Lin 2013 found that the improved toilet intervention reduced diarrhoea incidence compared to the control in villages receiving only the sanitation intervention as well as villages receiving both the sanitation and water supply interventions (P < 0.05, diarrhoea incidence = 1.81% in sanitation only villages, 1.59% in combined sanitation and water villages, and 2.55% in control villages). For the above three studies, the exact coverage differences between control and intervention villages were not reported, but for Jin 2009 and Lin 2013 it was generalized that intervention villages had coverage of centralized water supply in more than 90% of households and sanitary latrines in more than 70% of households compared to control villages, which were below those percentages. For Li 2009, intervention villages had coverage of more than 80% of households having improved toilets while the control groups had less than 20% of households with improved toilets.
Among NRCTs in rural China, Lou 1989 found that the improved toilet intervention decreased diarrhoea incidence compared to the control group (11.1% in intervention group, 36.4% in control group). The intervention had high coverage with 100% of intervention households receiving the piped water supply intervention and 90% of households receiving the improved toilet intervention. Control group households only had access to well water and traditional outdoor open toilet throughout the entire follow‐up period. Xing 2002 found that the intervention reduced diarrhoea incidence by 69.52% in residents. Xu 1994 found that the intervention reduced incidence of diarrhoea in residents by 14% (P < 0.01, incidence rate 7.96% in intervention group compared to 9.25% in control). Yan 1986 found that the intervention decreased diarrhoea incidence rates by 35.0%, 72.4%, and 83.2% in the intervention village compared to that in the control village in 1983, 1984, and 1985, respectively. Zhang 2000 found that the intervention decreased diarrhoea incidence rates at one‐year, three‐year, and 10‐year follow‐up. Additionally, Zhou 1995 found that the intervention decreased diarrhoea incidence by 38.3% (P < 0.001).
Reductions in diarrhoea were also seen for school‐based studies in rural China. Wei 1998 found that the school‐based WASH intervention reduced the diarrhoea incidence rate in intervention school students compared to control schools (diarrhoea prevalence of 3.33% in intervention schools compared to 16.3% in control schools, P < 0.01). Zhu 1997 found that the intervention decreased diarrhoea incidence by 42.5%.
Among studies of household sewerage connections in urban areas the evidence was mixed, with two of the five studies finding an effect on diarrhoea. Kolahi 2009 found that the diarrhoea incidence decreased by 46% in the intervention group after the invention (10.1% after, 18.6% before), compared to a decrease of 37% in the control group (10.5% after, 16.6% before). The intervention resulted in 76% of households connected to the sewerage system compared to none in the control group. Moraes 2003 found that the sanitation intervention reduced diarrhoeal incidence (diarrhoea incidence 1.73% in the intervention group compared to 5.55% in the control group; incidence density ratio 0.31, 95% CI 0.28 to 0.34). The incidence of frequent diarrhoea was also higher in the control group compared to the intervention group (frequent diarrhoea incidence 3.8% in the intervention group compared to 28.0% in the control group; adjusted OR 8.10, 95% CI 4.99 to 13.16). After the intervention, only 1.8% of intervention households reported excreta disposal on the ground or open drain compared to 45% in the control group.
Alternatively, Klasen 2012 found no difference in the incidence of diarrhoea reported in the past four weeks for children under five years and all household members between the intervention and control arms in the coastal region of Yemen with no water rationing (incidence difference ‐0.0223 for children under five, t = 0.51; ‐0.0207 for all household members, t = 1.3; Klasen 2012a) or within the mountain region of Yemen with frequent water rationing (incidence difference 0.0150 for children under five, t = 0.42; 0.0087 for all household members, t = 0.62; Klasen 2012b), although diarrhoea was suggestively lower in areas with a reliable water supply and higher in areas with water rationing. The intervention resulted in 85% of households in intervention towns in the coastal region and 32% of households in the intervention towns in the mountain region connected to the sewerage system compared to none in control towns. Pradhan 2002a also found no evidence that the sewerage intervention reduced diarrhoea in children under six years (diarrhoea incidence of 9.4% in the intervention group versus 21.9% in the control group, P = 0.24), however the sample size also may have been too small to measure an effect.
The two studies in urban areas of the installation of public or shared sanitation facilities also had mixed effects. Knee 2021 found no difference in the prevalence of diarrhoea reported for children in the past seven days at 12‐ or 24‐month follow‐up (PR 1.69, 95% CI 0.89 to 3.21 at 12 months; PR 0.84, 95% CI 0.47 to 1.51 at 24 months). All intervention compounds had pour‐flush toilets to septic tanks with soakaway pits installed whereas controls continued to use their "poor‐condition sanitation" for the duration of the study. However, Xu 1990 found that the intervention reduced the incidence of diarrhoea leading to clinic visits in residents, though the effect did not remain significant once an effect measure was calculated that corrected for clustering (Analysis 2.1).
Both studies conducted over 50 years ago in the rural USA found an impact of the intervention on diarrhoea, though again these did not remain statistically significant once effect measures were calculated that corrected for clustering (Analysis 2.1; Analysis 2.5). Mcabe 1954 found that the sanitation intervention reduced diarrhoea compared to control towns (diarrhoea rate of 1.02% in intervention town compared to 2.04% in control towns in warm weather and 0.57% versus 1.06% during cool weather). It was reported that all excreta disposal facilities in the intervention town were satisfactory after the intervention completed compared to 52% that were unsatisfactory before the intervention. However, privy coverage and quality in the control towns were not reported. Rubenstein 1969 found that the intervention decreased outpatient visits for diarrhoea.
Trinies 2016 found that the school‐based WASH intervention reduced reported diarrhoea among pupils (OR 0.71, 95% CI 0.60 to 0.85). The intervention also improved latrine quality with 47% of intervention schools meeting standards for sanitation related to latrine location, quality, and cleanliness and only 4% of control schools meeting these standards.
Comparison 3: Behaviour change messaging only (no hardware or subsidy provided)
Diarrhoea
In the pooled analysis across study designs, there was some evidence that behaviour change messaging interventions were protective against diarrhoea (RR 0.85, 95% CI 0.73 to 1.01, 9 studies, 31,080 participants, Analysis 3.1). However, in this case it was the cluster‐RCTs that were protective (RR 0.82, 95% CI 0.69 to 0.98, 7 studies, 28,909 participants, Analysis 3.1.1), while the pooled estimate of non‐randomized studies were not protective (RR 1.02, 95% CI 0.91 to 1.14, 2 studies, 2171 participants, Analysis 3.1.2). For children under five years, the pooled estimates were identical as they included the same populations as the all ages estimate since all included studies only measured diarrhoea in children under five years. In the pooled analyses the I2 values also suggest substantial heterogeneity across these study results.
3.1. Analysis.

Comparison 3: Behaviour change messaging only intervention versus control, Outcome 1: Diarrhoea: children < 5 years (same for all ages)
Dysentery (bloody diarrhoea)
There was no evidence of an effect of behaviour change messaging interventions on dysentery in the pooled analysis (RR 0.67, 95% CI 0.35 to 1.28, 2 studies, 8958 participants, Analysis 3.2), although the evidence was limited. The I2 value for this outcome only suggests mild to moderate heterogeneity across study results.
3.2. Analysis.

Comparison 3: Behaviour change messaging only intervention versus control, Outcome 2: Dysentery (bloody stool): children < 5 years (same for all ages)
Persistent diarrhoea
No studies measured the effect of behaviour change messaging interventions on persistent diarrhoea.
Hospital or clinic visits for diarrhoea
No studies measured the effect of behaviour change messaging interventions on hospital or clinic visits for diarrhoea.
Mortality
Only one study reported the effects of a behaviour change messaging intervention on all‐cause mortality and diarrhoea‐related mortality (Pickering 2015). Results were from 3984 households and similar for all ages and children under five years. There was no evidence of an effect of the intervention on all‐cause mortality for either population (all ages: RR 0.98, 95% CI 0.85 to 1.13, Analysis 3.3; children under five: RR 0.95, 95% CI 0.71 to 1.27, Analysis 3.4). However, the intervention was protective against diarrhoea‐related mortality (all ages: RR 0.46, 95% CI 0.26 to 0.83, Analysis 3.5; children under five: RR 0.47, 95% CI 0.23 to 0.98, Analysis 3.6).
3.3. Analysis.

Comparison 3: Behaviour change messaging only intervention versus control, Outcome 3: All‐cause mortality: all ages
3.4. Analysis.

Comparison 3: Behaviour change messaging only intervention versus control, Outcome 4: All‐cause mortality: children < 5
3.5. Analysis.

Comparison 3: Behaviour change messaging only intervention versus control, Outcome 5: Diarrhoea‐related mortality: all ages
3.6. Analysis.

Comparison 3: Behaviour change messaging only intervention versus control, Outcome 6: Diarrhoea‐related mortality: children < 5
Adverse events
No studies reported adverse events from the intervention.
Narrative description
Cluster‐RCTs
Of the five trials conducted in rural sub‐Saharan Africa, only Hashi 2017 found that the intervention reduced diarrhoea incidence in children under five years at endline. Diarrhoea incidence was reduced by 35% in the intervention arm compared to the control arm (RR 0.65, 95% CI 0.57 to 0.73). However, it was not reported if the intervention improved latrine coverage or use. Cha 2021 found some evidence that the intervention reduced diarrhoea, but only at three months follow‐up, with the effect reducing over time and no evidence of an effect at 10 months follow‐up for endline (RR 0.66, 95% CI 0.45 to 0.98 at three months, RR 0.75, 95% CI 0.35 to 1.60 at 10 months). However, there were similarities in latrine access and use among both groups at endline. Most households at endline in both intervention and control groups had access to a household latrine (99.5% in intervention, 90.8% in control), but 35% of intervention households had access to an improved latrine compared to 2.8% in control households. Latrine use based on direct observation was also similar across arms with 36.9% in intervention households compared to 44.8% in control households.
The remaining three cluster‐RCTs found no effect of the intervention on diarrhoea. Briceno 2017 found no difference in the prevalence of diarrhoea between intervention and control arms, including both the sanitation only and sanitation with handwashing intervention arms and seven‐day and 14‐day recall periods. However, the effect of the intervention was borderline significant for the combined intervention arm when considering 14‐day recall of diarrhoea (2.1 percentage points decline in diarrhoea (95% CI ‐0.4 to 4.6) compared to a control group mean of 16.8%). The sanitation and combined interventions increased latrine coverage and latrine quality. The probability of households building a new latrine was 8.2 percentage points higher in sanitation‐only arms (95% CI 1.5 to 14.9, control mean 57.1%) and 7.7 percentage points (95% CI 1.6 to 13.8) higher in combined arms. The probability of using improved sanitation also increased by 15.1 (95% CI 8.2 to 22, control mean 49.7%) and 10.6 percentage points (95% CI 4.5 to 16.7) in sanitation‐only and combined arms, respectively. Pickering 2015 found no evidence that the CTLS sanitation intervention reduced diarrhoea in children under five years (PR 0.98, 95% CI 0.82 to 1.17) or all‐cause mortality in children under five years (PR 0.95, 95% CI 0.71 to 1.27). However, the intervention did reduce blood in stool in children under five years (PR 0.68. 95% CI 0.48 to 0.97), diarrhoea‐related mortality in children under five years (PR 0.47, 95% CI 0.23 to 0.98), and diarrhoea‐related mortality in all ages (PR 0.46, 95% CI 0.26 to 0.83). The intervention also improved latrine coverage, with 64.8% of households having access to a private latrine in the intervention group compared to 34.6% in the control group. Sinharoy 2017 found that the behaviour change intervention had no effect on diarrhoea in children under five years (Lite intervention PR 0.97, 95% CI 0.81 to 1.16; Classic intervention PR 0.99, 95% CI 0.85 to 1.15). There was also no improvement in coverage of improved sanitation in households receiving the Lite intervention (30% in control and Lite intervention groups), although there was a slight improvement in improved latrine coverage among households receiving the Classic intervention (37%).
The results were also mixed for trials in Asia, with one finding an effect on diarrhoea and one finding no effect. Cameron 2013 found that the intervention reduced diarrhoea prevalence in children under five years. The intervention was associated with a 1.3 percentage point reduction in diarrhoea prevalence (2.4% in intervention versus 3.8% in control) with a seven‐day recall and a 1.4 percentage point reduction (1.6% in intervention versus 3.1% in control) with a two‐day recall period. However, no improvements in improved sanitation use and open defecation reduction were observed as a result of the intervention (42.6% intervention households reported members normally defecate in improved sanitation facility versus 43.5% control households, 34.8% intervention households practising open defecation versus 36.3% control households). Dickinson 2015 found no evidence that the sanitation intervention reduced diarrhoea prevalence (beta coefficient ‐0.21, P = 0.36). Latrine coverage increased to 35% of households in the intervention arm compared to 15% in the control arm.
Non‐randomized study designs
Neither study found an effect on diarrhoea. Huda 2012 did not find evidence that the intervention reduced the prevalence of diarrhoea in children under five years (diarrhoea prevalence of 10.1% in intervention and 9.9% in control arms, P = 0.56). There was also no difference in access to an improved latrine between the two groups at endline (38% of households in the intervention and control arms reported access), though there were slightly more households in the control group without access to any latrine (8.5% in control versus 6.8% in intervention arm). Saha 2015 also found no evidence that the sanitation intervention reduced diarrhoea in children under two years (adjusted OR 0.86, 95% CI 0.42 to 1.76). However, the intervention marginally increased the presence of a toilet at home from 51.8% of control households that owned a latrine to 62.6% of intervention households.
Comparison 4: Any sanitation intervention
Diarrhoea
In the pooled analysis across study designs and all interventions to improve sanitation, interventions yielded a protective effect on diarrhoea (RR 0.74, 95% CI 0.67 to 0.82, 50 studies, 237,130 participants, Analysis 4.1). The size of the effect was only about half as large in cluster‐RCTs (RR 0.85, 95% CI 0.76 to 0.95, 17 studies, 83,938 participants, Analysis 4.4.1) than in non‐randomized studies (RR 0.67, 95% CI 0.57 to 0.78, 33 studies, 153,192 participants, Analysis 4.1.2). For children under five years, the pooled estimate across study designs and interventions was also protective (RR 0.80, 95% CI 0.71 to 0.89, 32 studies, 80,047 participants, Analysis 4.2), just as it was for both cluster‐RCTs (RR 0.87, 95% CI 0.77 to 0.97, 14 studies, 60,024 participants, Analysis 4.2.1) and non‐randomized studies (RR 0.72, 95% CI 0.58 to 0.91, 18 studies, 20,023 participants, Analyses 4.2.2). Once again, heterogeneity across all studies was substantial.
4.1. Analysis.

Comparison 4: Any sanitation intervention, Outcome 1: Diarrhoea: all ages
4.2. Analysis.

Comparison 4: Any sanitation intervention, Outcome 2: Diarrhoea: children < 5 years
Dysentery (bloody diarrhoea)
In the pooled analysis, there was some evidence that any intervention to improve sanitation was protective against dysentery (RR 0.74, 95% CI 0.54 to 1.00, five studies, 34,025 participants, Analysis 4.3). Results were also similar with some evidence that the intervention was protective for children under five (RR 0.73, 95% CI 0.54 to 1.00, four studies, 14,034 participants, Analysis 4.4). Results were similar across cluster‐RCTs and NRCTs and there was minimal heterogeneity across all studies for this outcome.
4.3. Analysis.

Comparison 4: Any sanitation intervention, Outcome 3: Dysentery (bloody stool): all ages
4.4. Analysis.

Comparison 4: Any sanitation intervention, Outcome 4: Dysentery (bloody diarrhoea): children < 5 years
Persistent diarrhoea
Across all study designs and interventions, only two NCRTS measured the effect on persistent diarrhoea, and only in children under five years. In this pooled analysis, sanitation interventions were protective against persistent diarrhoea (RR 0.57, 95% CI 0.43 to 0.75, 2665 participants, Analysis 4.5).
4.5. Analysis.

Comparison 4: Any sanitation intervention, Outcome 5: Persistent diarrhoea: children < 5 years (same for all ages)
Hospital or clinical visits for diarrhoea
Clinic visits for diarrhoea were only reported as an outcome for two intervention studies in Comparison 2 above, both of which were NRCTs. There was no evidence of an effect of the intervention on clinic visits for diarrhoea (RR 0.86, 95% CI 0.44 to 1.67; 3720 participants, Analysis 2.5) in all ages or in children under one year (RR 1.03, 95% CI 0.48 to 2.19; one study, 121 participants, Analysis 2.6).
Mortality
When pooled across study designs and sanitation interventions, there was no evidence of an effect of interventions on all‐cause mortality (RR 0.99, 95% CI 0.89 to 1.09, 7 studies, 46,123 participants, Analysis 4.8), which was true for both cluster‐RCTs and NRCTs (Analyses 4.8.1, 4.8.2). Results for children under five years were similar, with no evidence on an effect of the intervention against all‐cause mortality (RR 0.93, 95% CI 0.79 to 1.09, 7 studies, 29,720 participants, Analysis 4.9). When looking separately at the pooled results for diarrhoea‐related mortality, there was suggestive evidence of a protective effect of sanitation interventions (RR 0.30, 95% CI 0.07 to 1.24; 2 studies, 46,123 participants, Analysis 4.10), but the evidence was limited from the random‐effects meta‐analysis model despite each individual study showing protective effects of the intervention. Results were also similar for children under five years old (Analysis 4.11). There was moderate heterogeneity across studies for each mortality outcome.
4.8. Analysis.

Comparison 4: Any sanitation intervention, Outcome 8: All‐cause mortality: all ages
4.9. Analysis.

Comparison 4: Any sanitation intervention, Outcome 9: All‐cause mortality ‐ Children < 5 years
4.10. Analysis.

Comparison 4: Any sanitation intervention, Outcome 10: Diarrhoea‐related mortality: all ages
4.11. Analysis.

Comparison 4: Any sanitation intervention, Outcome 11: Diarrhoea‐related mortality: children < 5
Adverse events
No studies reported adverse events from the intervention.
Comparisons 5 to 8: Sub‐analyses
Sub‐analyses did reduce heterogeneity, though possibly due to a reduction in the number of included studies. Nevertheless, they did provide some insights into the impact (or lack thereof) of certain conditions on the effectiveness of the interventions.
Comparison 5: Sanitation only or sanitation combined with other WASH interventions
Across study designs, we identified large numbers of studies that investigated the effects on diarrhoea of both sanitation alone (23 studies, 142,602 participants, Analysis 5.1) and sanitation combined with other WASH interventions (33 studies, 140,119 participants, Analysis 5.3). Pooled estimates of effects from these groups, however, provided no clear evidence of an additional benefit by combining sanitation with other WASH interventions (sanitation only: RR 0.78, 95% CI 0.69 to 0.89; sanitation with other WASH interventions: RR 0.74, 95% CI 0.65 to 0.83). This was true both for all age populations or children under five years (Analysis 5.2; Analysis 5.4). However, for children under five years, there was suggestive evidence that there may have been an additional benefit by combining sanitation with other WASH interventions, although the confidence intervals for the two subgroups overlapped (Analysis 5.2; Analysis 5.4).
5.1. Analysis.

Comparison 5: Sub‐analysis: Sanitation only versus with other WASH interventions, Outcome 1: Sanitation only: diarrhoea ‐ all ages
5.3. Analysis.

Comparison 5: Sub‐analysis: Sanitation only versus with other WASH interventions, Outcome 3: With other WASH interventions: diarrhoea ‐ all ages
5.2. Analysis.

Comparison 5: Sub‐analysis: Sanitation only versus with other WASH interventions, Outcome 2: Sanitation only: diarrhoea: children < 5 years
5.4. Analysis.

Comparison 5: Sub‐analysis: Sanitation only versus with other WASH interventions, Outcome 4: With other WASH interventions: diarrhoea ‐ children < 5 years
Comparison 6: Sanitation coverage
Thirty‐two studies reported on the level of coverage achieved in the intervention study population. There is some evidence that the protective effect of the intervention increases with higher levels of coverage. Among all age populations, sanitation interventions that achieved < 75% coverage were somewhat protective (RR 0.87, 95% CI 0.77 to 0.99, 18 studies, 98,839 participants, Analysis 6.1), while those with 75% or greater coverage were substantially more protective (RR 0.66, 95% CI 0.52 to 0.83, 14 studies, 69,776 participants, Analysis 6.3). However, the confidence intervals overlapped and separate inspection of the percent coverage in the intervention group graphed against the RR found no clear trends in the data as coverage increased or evidence of threshold coverage values for increased protective effects. Much of the result for the protective effect in the 75% or greater coverage subgroup was also driven by non‐randomized studies, many of which evaluated sewerage interventions. Results were also similar among children under five years (Analysis 6.2; Analysis 6.4).
6.1. Analysis.

Comparison 6: Sub‐analysis: Sanitation coverage, Outcome 1: Coverage < 75%: diarrhoea ‐ all ages
6.3. Analysis.

Comparison 6: Sub‐analysis: Sanitation coverage, Outcome 3: Coverage 75% or higher: diarrhoea ‐ all ages
6.2. Analysis.

Comparison 6: Sub‐analysis: Sanitation coverage, Outcome 2: Coverage < 75%: diarrhoea ‐ children < 5 years
6.4. Analysis.

Comparison 6: Sub‐analysis: Sanitation coverage, Outcome 4: Coverage 75% or higher: diarrhoea ‐ children < 5 years
Comparison 7: Increase in coverage
Only 24 of the included studies reported on the increase in sanitation coverage in the intervention group compared to the control. Among studies that reported the level of increase in coverage, there was no clear evidence of larger protective effects for greater increases in coverage. Among all age populations, sanitation interventions that achieved a 50% or higher increase in coverage were protective (RR 0.77, 95% CI 0.62 to 0.96, 8 studies, 45,934 participants, Analysis 7.3), but the level of protection was similar for interventions that achieved < 50% increase in coverage (RR 0.79, 95% CI 0.67 to 0.94, 16 studies, 73,163 participants, Analysis 7.1). Separate inspection of the percent increase in coverage graphed against the RR also found no clear trends in the data. Results were also similar among children under five years (Analysis 7.2; Analysis 7.4))
7.3. Analysis.

Comparison 7: Sub‐analysis: Increase in coverage, Outcome 3: Coverage increase 50% or more: diarrhoea ‐ all ages
7.1. Analysis.

Comparison 7: Sub‐analysis: Increase in coverage, Outcome 1: Coverage increase < 50%: diarrhoea ‐ all ages
7.2. Analysis.

Comparison 7: Sub‐analysis: Increase in coverage, Outcome 2: Coverage increase < 50%: diarrhoea ‐ children < 5 years
7.4. Analysis.

Comparison 7: Sub‐analysis: Increase in coverage, Outcome 4: Coverage increase 50% or more: diarrhoea ‐ children < 5 years
Comparison 8: Length of follow‐up
Subgrouping of study results across all study designs provided no clear evidence that effectiveness against diarrhoea is impacted by length of follow‐up (that is, the amount of time that passed from when the intervention was delivered until the last health outcomes were measured). Pooled estimates of effect for all ages overlapped among studies that followed participants for one year or less (RR 0.70, 95% CI 0.58 to 0.84, 19 studies, 93,094 participants, Analysis 8.1), studies with follow‐up between one and two years (RR 0.80, 95% CI 0.70 to 0.92, 17 studies, 74,889 participants, Analysis 8.3), and studies with follow‐up of three or more years (RR 0.71, 95% CI 0.58 to 0.87, 11 studies, 63,256 participants, Analysis 8.5). In children, the evidence was suggestive that the reported protective effect may diminish over time, but confidence levels overlapped for the different lengths of time after the intervention before the outcome was measured (one year or less: RR 0.75, 95% CI 0.59 to 0.94, Analysis 8.2; one to two years: RR 0.83, 95% CI 0.70 to 0.97, Analysis 8.4; three years or more: RR 0.80, 95% CI 0.70 to 0.93, Analysis 8.6).
8.1. Analysis.

Comparison 8: Sub‐analysis: Length of follow‐up, Outcome 1: 1 year or less: diarrhoea ‐ all ages
8.3. Analysis.

Comparison 8: Sub‐analysis: Length of follow‐up, Outcome 3: > 1 year to 2 years: diarrhoea ‐ all ages
8.5. Analysis.

Comparison 8: Sub‐analysis: Length of follow‐up, Outcome 5: 3 years or more: diarrhoea ‐ all ages
8.2. Analysis.

Comparison 8: Sub‐analysis: Length of follow‐up, Outcome 2: 1 year or less: diarrhoea ‐ children < 5 years
8.4. Analysis.

Comparison 8: Sub‐analysis: Length of follow‐up, Outcome 4: > 1 year to 2 years: diarrhoea ‐ children < 5 years
8.6. Analysis.

Comparison 8: Sub‐analysis: Length of follow‐up, Outcome 6: 3 years or more: diarrhoea ‐ children < 5 years
Sensitivity analysis
The choice of using random‐effects versus fixed‐effect models in our meta‐analysis did influence some results, with random‐effects often yielding wider confidence intervals and less statistically significant results. Of note is our Comparison 3, where using a fixed‐effect model instead of a random‐effects model would have led to a statistically significant reduction in diarrhoea (RR 0.86, 95% CI 0.80 to 0.92), which was not seen in the random‐effects model of pooled results (RR 0.85, 95% CI 0.73 to 1.01). The other main difference between a fixed‐effect and random‐effects model for our primary outcome was for the pooled results for children under five years for Comparison 1, where a fixed‐effect model yielded a statically significant result with less of a protective effect for diarrhoea (RR 0.91, 95% CI 0.84 to 0.98) compared to the result given by the random‐effects model (RR 0.83, 95% CI 0.68 to 1.02). Among the secondary outcomes in our Comparison 4, using a fixed‐effect model instead of a random‐effects model would have led to a statistically significant reduction in diarrhoea‐related mortality for all ages (RR 0.42, 95% CI 0.24 to 0.74) and children under five years (RR 0.41, 95% CI 0.20 to 0.81) not seen in our random‐effects models (all ages: RR 0.30, 95% CI 0.07 to 1.24; children under five: RR 0.30, 95% CI 0.07 to 1.29). The decision to use a random‐effects versus a fixed‐effect model did not affect the direction or statistical significance of any other main pooled comparisons of our primary or secondary outcomes.
Removing studies with populations in schools from main meta‐analysis comparisons had no major influence on the results or conclusions. Additionally, when analysing the seven studies conducted in schools separately from the rest of the studies, school‐based interventions still had a protective effect on diarrhoea (RR 0.70, 95% CI 0.57 to 0.86).
Furthermore, the choice to correct for clustering in non‐randomized studies substantially increased the confidence intervals of these studies in meta‐analyses and likely rendered the pooled estimate of effect to not be statistically significant in some cases when it would have been significant without these corrections to NRCTs.
Discussion
Summary of main results
Providing access to sanitation facilities to households or schools without any existing sanitation facilities (that is, previously practising open defecation) may reduce diarrhoea prevalence in all ages. However, the pooled effect varied by study design. The effect was weaker in cluster‐RCTs (risk ratio (RR) 0.89, 95% confidence interval (CI) 0.73 to 1.08; low‐certainty evidence) compared to non‐randomized studies, which provided uncertain evidence (RR 0.72, 95% CI 0.53 to 0.97; very low‐certainty evidence), and a pooled estimate of randomized and non‐randomized studies (RR 0.79, 95% CI 0.66 to 0.94). There was also less evidence of an effect in children under five years, with evidence from four cluster‐RCTs suggesting that access may have little or no effect on diarrhoea prevalence (RR 0.98, 95% CI 0.83 to 1.16; low‐certainty evidence), generally consistent with evidence from non‐randomized studies (RR 0.76, 95% CI 0.55 to 1.05; very low‐certainty evidence) and all study designs pooled together (RR 0.83, 95% CI 0.68 to 1.02).
Improving existing sanitation facilities may reduce diarrhoea in all ages and children under five years. The pooled effect was protective but weaker in the three cluster‐RCTs (RR 0.85, 95% CI 0.69 to 1.06; low‐certainty evidence), all for children under five. However, some of these interventions, such as sewerage connections, are not easily randomized and there was evidence of a stronger effect in non‐randomized studies of all ages (RR 0.61, 95% CI 0.50 to 0.74; low‐certainty evidence) and children under five (RR 0.64, 95% CI 0.43 to 0.96; very low‐certainty evidence). Pooled estimates across randomized and non‐randomized studies provided similar protective estimates (all ages: RR 0.65, 95% CI 0.55 to 0.78; children under five years: RR 0.70, 95% CI 0.54 to 0.91).
Strategies to promote behaviour change to improve access to or use of sanitation facilities without the provision of any hardware or subsidy probably reduce diarrhoea prevalence in children under five based on evidence from seven cluster‐RCTs (RR 0.82, 95% CI 0.69 to 0.98; moderate‐certainty evidence). Evidence from two non‐randomized studies found no effect, though with high uncertainty (RR 1.02, 95% CI 0.91 to 1.14; very low‐certainty evidence). Pooled estimates across randomized and non‐randomized studies in children under five years provided similar protective estimates (RR 0.85, 95% CI 0.73 to 1.01). No studies measured the effects of this type of intervention in older populations.
Pooled analysis of studies across all types of sanitation interventions demonstrated that sanitation interventions may reduce diarrhoea prevalence in all ages and children under five. This result was similar across cluster‐RCTs and non‐randomized studies, although the effect size and certainty of the evidence varied between cluster‐RCTs and non‐randomized studies. In cluster‐RCTs, the effect size was lower with higher certainty of evidence (all ages: RR 0.85, 95% CI 0.76 to 0.95, low‐certainty evidence; children under five years: RR 0.87, 95% CI 0.77 to 0.97, low‐certainty evidence) compared to non‐randomized studies, which may be subject to confounding (all ages: RR 0.67, 95% CI 0.57 to 0.78, very low‐certainty evidence; children under five years: RR 0.72, 95% CI 0.58 to 0.91, very low‐certainty evidence). Pooled estimates across randomized and non‐randomized studies provided similar protective estimates (all ages: RR 0.74, 95% CI 0.67 to 0.82; children under five years: RR 0.80, 95% CI 0.71 to 0.89). However, there was substantial heterogeneity across individual studies, so all types of sanitation interventions may not have a similar effect in all settings.
In subgroup analysis, there was some evidence of larger effects in studies with increased coverage amongst all participants (75% or higher coverage levels), and also some evidence that the effect decreased over longer follow‐up times for children under five years.
Overall completeness and applicability of evidence
Fifty‐one studies met our inclusion criteria, with 50 of these studies providing sufficient information to be used in quantitative meta‐analysis. Most were conducted in low‐ or middle‐income countries. Most studies were also conducted in whole or part in rural areas (86%). About half of the included studies were conducted isolating the sanitation intervention from other WASH interventions, with the other half including other WASH components as part of a more comprehensive intervention, such as an improvement in water supply. A few studies (12%) included multiple intervention arms, with one arm evaluating a sanitation‐only intervention and another arm evaluating a sanitation intervention in combination with another WASH intervention component, which allowed us to include data from different study arms in our Comparison 5 sub‐analysis. Additionally, most studies (86%) evaluated interventions delivered at the household level, although 14% evaluated interventions at schools. All sanitation interventions at schools included the provision of hardware, so they were either part of Comparison 1 or 2, with none included in Comparison 3.
For interventions that provided a sanitation facility to households with no existing facility, studies were completed in a variety of low‐ and middle‐income countries (LMICs) in rural, peri‐urban, and urban areas. All studies provided access to pit latrines, which were typically improved. Most studies were conducted among households, with a few in schools. Most were also conducted in rural areas.
For interventions that improved an existing sanitation facility, studies were completed in a variety of low‐, middle‐, and high‐income countries in rural and urban areas although about half of these studies (14 out of 26) were completed in China. The type of improvements varied considerably, from upgrades to existing latrines, to better faecal sludge management of latrine sludge, to sewerage connection. The provision of sewerage is likely only applicable to urban or peri‐urban areas, and as such this type of intervention included more urban populations than other interventions. Most studies were also conducted among households, with a few in schools.
However, for interventions that used behaviour change messaging to improve sanitation access or practices without the provision of any hardware, studies were completed in a variety of low‐ middle‐income countries, but only in rural areas. Therefore, the results may not be reproducible in urban areas, though these types of studies are also less applicable to urban areas where residents often have less control over household infrastructure. Most interventions used Community‐Led Total Sanitation (CLTS) or social marketing techniques for behaviour change.
Certainty of the evidence
The certainty of the evidence for the effects of different types of sanitation interventions and study designs ranges from moderate to very low (Table 1; Table 2; Table 3; Table 4), with the certainty of the evidence generally higher for cluster‐RCTs and lower for non‐randomized study designs.
One of the primary reasons for downgrading the certainty of evidence across all comparisons for the primary outcome was the risk of bias from unblinded studies evaluating the effect of an intervention on a self‐reported outcome. While this is a potential source of bias, it is not possible to blind any sanitation interventions at the study participant level or any sanitation interventions involving infrastructure or visual messaging in villages at the field assessor level. Other reasons for downgrading certain comparisons included downgrading an additional level for risk of bias if most studies did not control for potential confounding factors in study design or analysis, inconsistency, and indirectness.
Potential biases in the review process
Most included studies were published in English (71%), however the review also includes several studies (28%) that were published in Chinese (and one study published in French). Although all students conducting article screening and data extraction were trained by the same author (VB), there were separate students reviewing Chinese studies and English studies, which may have led to minor variations in the review and eligibility assessment process. We tried to limit this potential by having author VB have detailed discussions about study design with students screening and extracting data from the English and Chinese studies. Additionally, all Chinese studies were included in Comparison 2, with none eligible for Comparison 1 or Comparison 3.
Agreements and disagreements with other studies or reviews
Our results are generally consistent with the conclusions of the prior version of this Cochrane Review (Clasen 2010), but are much more expansive as the previous review only included 13 eligible studies and did not do a quantitative meta‐analysis. The results are also generally consistent with other more recent sanitation reviews (Freeman 2017; Norman 2010; Waddington 2009; Wolf 2018), which found sanitation to be protective against diarrhoea although the magnitudes of effect varied. One of these reviews also found that increased sanitation coverage yielded higher protective effects on diarrhoea, which is also consistent with our results (Wolf 2018).
Authors' conclusions
Implications for practice.
Sanitation interventions are effective at preventing diarrhoea. However, evidence suggests that the effectiveness of individual sanitation interventions will vary by type of intervention and setting. It will also likely vary based on other factors, including levels of adoption and consistent use, exposure to pathogens from other transmission pathways such as animal faeces, and downstream exposures from unsafe treatment or disposal of faeces from sanitation facilities. Heterogeneous results also underscore the need for implementers to undertake site‐specific assessments that identify important sources of exposure while engaging the community in developing sanitation solutions that they would use consistently and that address both containment and eventual treatment or safe disposal. Local piloting of a specific intervention before scaling up could also help address exclusive and sustained use by all members of the household, including use for child faeces management.
Implications for research.
While there is evidence that sanitation interventions are effective at preventing diarrhoea, the heterogeneity of effects, even among the same types of interventions, implies the presence of effect modifiers that research has yet to fully identify. There is a need for rigorous research to better understand the determinants of intervention effectiveness and how to optimize adoption and use by the entire community. These studies would benefit from improved methods and consistent reporting of the effects of interventions on salient exposure pathways, as well as downstream faecal sludge management. This will help understand which sanitation interventions would be effective at improving health and wellbeing in various settings so that interventions can be better targeted in the future.
Additional rigorous randomized controlled trials of various approaches to sanitation interventions that use objective outcomes to avoid reporting bias could also help clarify the potential effect of sanitation interventions on diarrhoea.
History
Protocol first published: Issue 5, 2019
Acknowledgements
We thank Olivia Zarella, Christen Landon, Amylee Anyoha, Alan Guo, and Kasthuri Sivalogan for their help with study screening and data extraction, and Gloria Sclar for her review of the protocol. We also gratefully acknowledge Kristof Bostoen, Wolf‐Peter Schmidt, Sophie Boisson, Isaac C‐H Fung, Marion W Jenkins, Beth Scott, Steven Sugden, and Sandy Cairncross, co‐authors of the Cochrane Review superseded by this review (Clasen 2010).
Editorial and peer reviewer contributions
The following people conducted the editorial process for this article:
Sign‐off Editors (final editorial decision): Professor Mical Paul; Professor Paul Garner
Managing Editor (selected peer reviewers, collated peer reviewer comments, provided editorial guidance to authors, edited the article): Dr Deirdre Walshe, CIDG;
Copy Editor (copy editing and production): Jenny Bellorini, Cochrane Central Production Service
-
Peer reviewers (provided comments and recommended an editorial decision):
Dr Dani Barrington, The University of Western Australia; Nguyen Tien Huy, School of Tropical Medicine and Global Health, Nagasaki University, Japan (clinical/content review);
Andrew Bäck, Statistical Editor, Cochrane (statistical/methods review).
The editorial base of the Cochrane Infectious Diseases Group is funded by UK aid from the UK government for the benefit of LMICs (project number 300342‐104). The views expressed do not necessarily reflect the UK government’s official policies.
Appendices
Appendix 1. Detailed search strategy
| Search set | CIDG SRa | CENTRAL | MEDLINEb | Embaseb | LILACS |
| 1 | excreta disposal | “excreta disposal” [ti, ab, kw] | “excreta disposal” [ti, ab] | “excreta disposal” [ti, ab] | excreta disposal |
| 2 | sanitation | Sanitation [Mesh terms] | Sanitation [Mesh] | environmental sanitation [Emtree] | sanitation |
| 3 | latrine OR toilet OR water closet OR privy OR sewer* |
latrine OR toilet OR water closet OR privy OR sewer* [ti, ab, kw] |
latrine OR toilet OR water closet OR privy OR sewer* [ti, ab] |
Sanitation [Emtree] | latrine OR toilet OR water closet OR privy OR sewer* |
| 4 | faeces OR defecation OR excrement OR waste OR sludge |
faeces OR defecation OR excrement OR waste OR sludge [ti, ab, kw] |
faeces OR defecation OR excrement OR waste OR sludge [ti, ab] |
solid waste management [Emtree] | faeces OR defecation OR excrement OR waste OR sludge |
| 5 | 1 OR 2 OR 3 OR 4 | 1 OR 2 OR 3 OR 4 | 1 OR 2 OR 3 OR 4 | latrine OR toilet OR water closet OR privy OR sewer* [ti, ab] |
1 OR 2 OR 3 OR 4 |
| 6 | diarrhea | “diarrhea/epidemiology”[Mesh Terms] OR “diarrhea/microbiology”[Mesh Terms] OR “diarrhea/prevention and control”[Mesh Terms] | “diarrhea/epidemiology”[Mesh ] OR “diarrhea/microbiology”[Mesh ] OR “diarrhea/prevention and control”[Mesh ] | faeces OR defecation OR excrement OR Waste OR sludge [ti, ab] |
diarrhea OR cholera OR shigell* OR dysenter* OR cryptosporid* or giardia* OR Escherichia OR clostridium |
| 7 | waterborne OR foodborne | (waterborne OR foodborne) AND (infection* OR illness*) |
(waterborne OR foodborne) AND (infection* OR illness*) |
1‐6/OR | waterborne OR foodborne |
| 8 | 6 OR 7 | cholera OR shigell* OR dysenter* OR cryptosporid* or giardia* OR Escherichia OR clostridium [ti, ab, kw] |
cholera OR shigell* OR dysenter* OR cryptosporid* or giardia* OR Escherichia OR clostridium |
diarrhea/dm, ep, pc [Disease Management, Epidemiology, Prevention] | 6 OR 7 |
| 9 | 5 AND 8 | "Enterobacteriaceae Infections"[Mesh] | "Enterobacteriaceae Infections"[Mesh] | (waterborne OR foodborne) AND (infection* OR illness*) |
5 AND 8 |
| 10 | ‐ | 6 OR 7 OR 8 OR 9 | 6 OR 7 OR 8 OR 9 | cholera OR shigell* OR dysenter* OR cryptosporid* or giardia* OR Escherichia OR clostridium [ti, ab] |
‐ |
| 11 | ‐ | 5 AND 10 | 5 AND 10 | Enterobacteriaceae infection [Emtree] | ‐ |
| 12 | ‐ | ‐ | Limit 11 to Human | 8 OR 9 OR 10 OR 11 | ‐ |
| 13 | ‐ | ‐ | ‐ | 7 AND 12 | ‐ |
| 14 | ‐ | ‐ | ‐ | Limit 13 to Human | ‐ |
aCochrane Infectious Diseases Group Specialized Register. bSearch terms used in combination with the search strategy for retrieving trials developed by Cochrane (Lefebvre 2011).
Chinese Language Search Terms used:
((TI = '排泄物处理' OR TI = '粪便处理' OR TI = '卫生' OR TI = '环境卫生' OR TI = '厕所' OR TI = '卫生间' OR TI = '洗手间' OR TI = '茅坑' OR TI = '粪便' OR TI = '排泄物') AND (TI = '腹泻' OR TI = '泄泻' OR TI = '霍乱' OR TI = '痢疾' OR TI = ('水传染'+'介水' + '水性') OR TI = ('食物传播'+'食物传染') )) OR ((AB = '排泄物处理' OR AB = '粪便处理' OR AB = '卫生' OR AB = '环境卫生' OR AB = '厕所' OR AB = '卫生间' OR AB = '洗手间' OR AB = '茅坑' OR AB = '粪便' OR AB = '排泄物') AND (AB = '腹泻' OR AB = '泄泻' OR AB = '霍乱' OR AB = '痢疾' OR AB = ('水传染'+'介水' + '水性') OR AB = ('食物传播'+'食物传染') )) OR ((KY = '排泄物处理' OR KY = '粪便处理' OR KY = '卫生' OR KY = '环境卫生' OR KY = '厕所' OR KY = '卫生间' OR KY = '洗手间' OR KY = '茅坑' OR KY = '粪便' OR KY = '排泄物') AND (KY = '腹泻' OR KY = '泄泻' OR KY = '霍乱' OR KY = '痢疾' OR KY = ('水传染'+'介水' + '水性') OR KY = ('食物传播'+'食物传染') ))
Appendix 2. Data to extract from included studies
| Type of data | Fields |
| General information | Study ID |
| Name of data extractor | |
| Date of data extraction | |
| Study citation | |
| Publication type | |
| Publication status | |
| Funding source | |
| Study eligibility | Type of study – RCT, quasi‐RCT, non‐randomized controlled trial, CBA, matched cohort |
| Participants – children or adults in any country or population | |
| Type of intervention – sanitation intervention to introduce or upgrade sanitation facilities, or expand the coverage or use of sanitation facilities | |
Outcome
| |
| If excluded, provide reason for exclusion and stop data extraction | |
| Study data | Country and setting (urban, rural) |
| Year of study | |
| Number of participants/groups/clusters and average number of participants per group/cluster | |
| Age of participants | |
| Method of participant recruitment | |
| Inclusion/exclusion criteria for study participation. Matching criteria used for matched cohort studies. | |
| Unit of randomization and whether measurement of effect adjusts for clustering where randomization is done by groups other than individual | |
| If participants are blinded and method of blinding participants | |
| Types and details of the sanitation intervention, including factors that may augment or diminish effectiveness (for example, location, emptying practices, overflow protection) | |
| Description of sanitation facilities and practices at baseline in control and intervention groups | |
| Other components of intervention (for example, hygiene message, improved water supply, improved water quality, improved storage) | |
| Duration of intervention and duration of follow‐up | |
| Definition of control group and description of sanitation facilities and practices | |
| Whether water is protected to point of use (that is, by pipe, residual disinfection, or safe storage) | |
| Hygiene practices | |
| Child defecation practices | |
| Child faeces disposal practices | |
| Sanitation use levels and open defecation prevalence at baseline, endline, and other time points measured | |
| Sanitation coverage levels at baseline and postintervention at time of outcome assessment | |
| Any measurements of environmental contamination measured (for example, water, hands, soil, flies) | |
| Description of any missing data with reason for loss | |
| Prescribed criteria of risk of bias assessments – varies based on study design | |
| Outcomes | Time points measured and reported, including season (wet/dry) of each outcome measurement |
| Case definition of outcome | |
| Method for outcome assessment (self reported, caregiver reported, observed, clinically confirmed, or other surveillance method) | |
| If self or caregiver reported, what is the recall period used? | |
| Effect measure and 95% confidence interval for each age group reported. For non‐randomized studies, unadjusted and adjusted effect measures and 95% confidence intervals, including a list of factors that were adjusted for. For cluster‐RCT, record whether effect measure is adjusted for clustering and the ICC. | |
| Mortality attributed to diarrhoea | |
| Diarrhoea prevalence (or incidence) in control and intervention groups at baseline, endline, and other time points measured | |
| Rate of utilisation of intervention and manner of assessing it | |
| Number or per cent of participants/groups lost to withdrawal or follow‐up with reason | |
| Key conclusions of the study authors |
Data and analyses
Comparison 1. Providing access to any sanitation facility intervention versus control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Diarrhoea: all ages | 15 | Risk Ratio (IV, Random, 95% CI) | 0.79 [0.66, 0.94] | |
| 1.1.1 Cluster‐RCTs | 7 | Risk Ratio (IV, Random, 95% CI) | 0.89 [0.73, 1.08] | |
| 1.1.2 NRCTs | 8 | Risk Ratio (IV, Random, 95% CI) | 0.72 [0.53, 0.97] | |
| 1.2 Diarrhoea: children < 5 years | 11 | Risk Ratio (IV, Random, 95% CI) | 0.83 [0.68, 1.02] | |
| 1.2.1 Cluster‐RCTs | 4 | Risk Ratio (IV, Random, 95% CI) | 0.98 [0.83, 1.16] | |
| 1.2.2 NRCTs | 7 | Risk Ratio (IV, Random, 95% CI) | 0.76 [0.55, 1.05] | |
| 1.3 Dysentery (bloody diarrhoea): children < 5 years (same for all ages) | 2 | Risk Ratio (IV, Random, 95% CI) | 0.74 [0.47, 1.17] | |
| 1.3.1 Cluster‐RCTs | 1 | Risk Ratio (IV, Random, 95% CI) | 0.96 [0.11, 8.14] | |
| 1.3.2 NRCTs | 1 | Risk Ratio (IV, Random, 95% CI) | 0.73 [0.46, 1.17] | |
| 1.4 Persistent diarrhoea: children < 5 years (same for all ages) | 1 | Risk Ratio (IV, Random, 95% CI) | Totals not selected | |
| 1.4.1 NRCTs | 1 | Risk Ratio (IV, Random, 95% CI) | Totals not selected | |
| 1.5 All‐cause mortality: all ages | 3 | Risk Ratio (IV, Random, 95% CI) | 0.93 [0.69, 1.24] | |
| 1.5.1 Cluster‐RCTs | 2 | Risk Ratio (IV, Random, 95% CI) | 1.05 [0.88, 1.25] | |
| 1.5.2 NRCTs | 1 | Risk Ratio (IV, Random, 95% CI) | 0.56 [0.32, 0.99] | |
| 1.6 All‐cause mortality: children < 5 years | 3 | Risk Ratio (IV, Random, 95% CI) | 0.82 [0.59, 1.15] | |
| 1.6.1 Cluster‐RCTs | 2 | Risk Ratio (IV, Random, 95% CI) | 0.95 [0.72, 1.26] | |
| 1.6.2 NRCTs | 1 | Risk Ratio (IV, Random, 95% CI) | 0.56 [0.32, 0.99] | |
| 1.7 Diarrhoea‐related mortality: children < 5 years (same for all ages) | 1 | Risk Ratio (IV, Random, 95% CI) | Totals not selected | |
| 1.7.1 NRCTs | 1 | Risk Ratio (IV, Random, 95% CI) | Totals not selected |
Comparison 2. Sanitation facility improvement intervention versus control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Diarrhoea: all ages | 26 | Risk Ratio (IV, Random, 95% CI) | 0.65 [0.55, 0.78] | |
| 2.1.1 Cluster‐RCTs | 3 | Risk Ratio (IV, Random, 95% CI) | 0.85 [0.69, 1.06] | |
| 2.1.2 NRCTs | 23 | Risk Ratio (IV, Random, 95% CI) | 0.61 [0.50, 0.74] | |
| 2.2 Diarrhoea: children < 5 years | 12 | Risk Ratio (IV, Random, 95% CI) | 0.70 [0.54, 0.91] | |
| 2.2.1 Cluster‐RCTs | 3 | Risk Ratio (IV, Random, 95% CI) | 0.85 [0.69, 1.06] | |
| 2.2.2 NRCTs | 9 | Risk Ratio (IV, Random, 95% CI) | 0.64 [0.43, 0.96] | |
| 2.3 Dysentery (bloody stool): all ages | 1 | Risk Ratio (IV, Random, 95% CI) | Totals not selected | |
| 2.3.1 NRCTs | 1 | Risk Ratio (IV, Random, 95% CI) | Totals not selected | |
| 2.4 Persistent Diarrhoea ‐ Children <5 years | 1 | Risk Ratio (IV, Random, 95% CI) | Totals not selected | |
| 2.4.1 NRCTs | 1 | Risk Ratio (IV, Random, 95% CI) | Totals not selected | |
| 2.5 Clinic visits for diarrhoea: all ages | 2 | Risk Ratio (IV, Random, 95% CI) | 0.86 [0.44, 1.67] | |
| 2.5.1 NRCTs | 2 | Risk Ratio (IV, Random, 95% CI) | 0.86 [0.44, 1.67] | |
| 2.6 Clinic visits for diarrhoea: children < 5 years | 1 | Risk Ratio (IV, Random, 95% CI) | Totals not selected | |
| 2.6.1 NRCTs | 1 | Risk Ratio (IV, Random, 95% CI) | Totals not selected | |
| 2.7 All‐cause mortality: children < 5 years (same for all ages) | 3 | Risk Ratio (IV, Random, 95% CI) | 1.00 [0.75, 1.34] | |
| 2.7.1 Cluster‐RCTs | 2 | Risk Ratio (IV, Random, 95% CI) | 0.99 [0.74, 1.33] | |
| 2.7.2 NRCTs | 1 | Risk Ratio (IV, Random, 95% CI) | 1.49 [0.25, 8.88] |
Comparison 3. Behaviour change messaging only intervention versus control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Diarrhoea: children < 5 years (same for all ages) | 9 | Risk Ratio (IV, Random, 95% CI) | 0.85 [0.73, 1.01] | |
| 3.1.1 Cluster‐RCTs | 7 | Risk Ratio (IV, Random, 95% CI) | 0.82 [0.69, 0.98] | |
| 3.1.2 NRCTs | 2 | Risk Ratio (IV, Random, 95% CI) | 1.02 [0.91, 1.14] | |
| 3.2 Dysentery (bloody stool): children < 5 years (same for all ages) | 2 | Risk Ratio (IV, Random, 95% CI) | 0.67 [0.35, 1.28] | |
| 3.2.1 Cluster‐RCTs | 2 | Risk Ratio (IV, Random, 95% CI) | 0.67 [0.35, 1.28] | |
| 3.3 All‐cause mortality: all ages | 1 | Risk Ratio (IV, Random, 95% CI) | Totals not selected | |
| 3.3.1 Cluster‐RCTs | 1 | Risk Ratio (IV, Random, 95% CI) | Totals not selected | |
| 3.4 All‐cause mortality: children < 5 | 1 | Risk Ratio (IV, Random, 95% CI) | Totals not selected | |
| 3.4.1 Cluster‐RCTs | 1 | Risk Ratio (IV, Random, 95% CI) | Totals not selected | |
| 3.5 Diarrhoea‐related mortality: all ages | 1 | Risk Ratio (IV, Random, 95% CI) | Totals not selected | |
| 3.5.1 Cluster‐RCTs | 1 | Risk Ratio (IV, Random, 95% CI) | Totals not selected | |
| 3.6 Diarrhoea‐related mortality: children < 5 | 1 | Risk Ratio (IV, Random, 95% CI) | Totals not selected | |
| 3.6.1 Cluster‐RCTs | 1 | Risk Ratio (IV, Random, 95% CI) | Totals not selected |
Comparison 4. Any sanitation intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 Diarrhoea: all ages | 50 | Risk Ratio (IV, Random, 95% CI) | 0.74 [0.67, 0.82] | |
| 4.1.1 Cluster‐RCTs | 17 | Risk Ratio (IV, Random, 95% CI) | 0.85 [0.76, 0.95] | |
| 4.1.2 NRCTs | 33 | Risk Ratio (IV, Random, 95% CI) | 0.67 [0.57, 0.78] | |
| 4.2 Diarrhoea: children < 5 years | 32 | Risk Ratio (IV, Random, 95% CI) | 0.80 [0.71, 0.89] | |
| 4.2.1 Cluster‐RCTs | 14 | Risk Ratio (IV, Random, 95% CI) | 0.87 [0.77, 0.97] | |
| 4.2.2 NRCTs | 18 | Risk Ratio (IV, Random, 95% CI) | 0.72 [0.58, 0.91] | |
| 4.3 Dysentery (bloody stool): all ages | 5 | Risk Ratio (IV, Random, 95% CI) | 0.74 [0.54, 1.00] | |
| 4.3.1 Cluster‐RCTs | 3 | Risk Ratio (IV, Random, 95% CI) | 0.74 [0.49, 1.11] | |
| 4.3.2 NRCTs | 2 | Risk Ratio (IV, Random, 95% CI) | 0.74 [0.47, 1.17] | |
| 4.4 Dysentery (bloody diarrhoea): children < 5 years | 4 | Risk Ratio (IV, Random, 95% CI) | 0.73 [0.54, 1.00] | |
| 4.4.1 Cluster‐RCTs | 3 | Risk Ratio (IV, Random, 95% CI) | 0.74 [0.49, 1.11] | |
| 4.4.2 NRCTs | 1 | Risk Ratio (IV, Random, 95% CI) | 0.73 [0.46, 1.17] | |
| 4.5 Persistent diarrhoea: children < 5 years (same for all ages) | 2 | Risk Ratio (IV, Random, 95% CI) | 0.57 [0.43, 0.75] | |
| 4.5.1 NRCTs | 2 | Risk Ratio (IV, Random, 95% CI) | 0.57 [0.43, 0.75] | |
| 4.6 Clinic visits for diarrhoea: all ages | 2 | Risk Ratio (IV, Random, 95% CI) | 0.86 [0.44, 1.67] | |
| 4.6.1 NRCTs | 2 | Risk Ratio (IV, Random, 95% CI) | 0.86 [0.44, 1.67] | |
| 4.7 Clinic visits for diarrhoea: children < 5 years | 1 | Risk Ratio (IV, Random, 95% CI) | Totals not selected | |
| 4.7.1 NRCTs | 1 | Risk Ratio (IV, Random, 95% CI) | Totals not selected | |
| 4.8 All‐cause mortality: all ages | 7 | Risk Ratio (IV, Random, 95% CI) | 0.99 [0.89, 1.09] | |
| 4.8.1 Cluster‐RCTs | 5 | Risk Ratio (IV, Random, 95% CI) | 1.00 [0.90, 1.11] | |
| 4.8.2 NRCTs | 2 | Risk Ratio (IV, Random, 95% CI) | 0.62 [0.35, 1.13] | |
| 4.9 All‐cause mortality ‐ Children < 5 years | 7 | Risk Ratio (IV, Random, 95% CI) | 0.93 [0.79, 1.09] | |
| 4.9.1 Cluster‐RCTs | 5 | Risk Ratio (IV, Random, 95% CI) | 0.96 [0.82, 1.14] | |
| 4.9.2 NRCTs | 2 | Risk Ratio (IV, Random, 95% CI) | 0.62 [0.35, 1.13] | |
| 4.10 Diarrhoea‐related mortality: all ages | 2 | Risk Ratio (IV, Random, 95% CI) | 0.30 [0.07, 1.24] | |
| 4.10.1 Cluster‐RCTs | 1 | Risk Ratio (IV, Random, 95% CI) | 0.46 [0.26, 0.83] | |
| 4.10.2 NRCTs | 1 | Risk Ratio (IV, Random, 95% CI) | 0.09 [0.01, 0.88] | |
| 4.11 Diarrhoea‐related mortality: children < 5 | 2 | Risk Ratio (IV, Random, 95% CI) | 0.30 [0.07, 1.29] | |
| 4.11.1 Cluster‐RCTs | 1 | Risk Ratio (IV, Random, 95% CI) | 0.47 [0.23, 0.98] | |
| 4.11.2 NRCTs | 1 | Risk Ratio (IV, Random, 95% CI) | 0.09 [0.01, 0.88] |
4.6. Analysis.

Comparison 4: Any sanitation intervention, Outcome 6: Clinic visits for diarrhoea: all ages
4.7. Analysis.

Comparison 4: Any sanitation intervention, Outcome 7: Clinic visits for diarrhoea: children < 5 years
Comparison 5. Sub‐analysis: Sanitation only versus with other WASH interventions.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 5.1 Sanitation only: diarrhoea ‐ all ages | 23 | Risk Ratio (IV, Random, 95% CI) | 0.78 [0.69, 0.89] | |
| 5.1.1 Cluster‐RCTs | 10 | Risk Ratio (IV, Random, 95% CI) | 0.89 [0.79, 0.99] | |
| 5.1.2 NRCTs | 13 | Risk Ratio (IV, Random, 95% CI) | 0.65 [0.49, 0.85] | |
| 5.2 Sanitation only: diarrhoea: children < 5 years | 15 | Risk Ratio (IV, Random, 95% CI) | 0.88 [0.79, 0.98] | |
| 5.2.1 Cluster‐RCTs | 10 | Risk Ratio (IV, Random, 95% CI) | 0.88 [0.79, 0.98] | |
| 5.2.2 NRCTs | 5 | Risk Ratio (IV, Random, 95% CI) | 0.80 [0.57, 1.14] | |
| 5.3 With other WASH interventions: diarrhoea ‐ all ages | 33 | Risk Ratio (IV, Random, 95% CI) | 0.74 [0.65, 0.83] | |
| 5.3.1 Cluster‐RCTs | 10 | Risk Ratio (IV, Random, 95% CI) | 0.84 [0.72, 0.97] | |
| 5.3.2 NRCTs | 23 | Risk Ratio (IV, Random, 95% CI) | 0.66 [0.54, 0.81] | |
| 5.4 With other WASH interventions: diarrhoea ‐ children < 5 years | 21 | Risk Ratio (IV, Random, 95% CI) | 0.77 [0.66, 0.89] | |
| 5.4.1 Cluster‐RCTs | 7 | Risk Ratio (IV, Random, 95% CI) | 0.87 [0.74, 1.02] | |
| 5.4.2 NRCTs | 14 | Risk Ratio (IV, Random, 95% CI) | 0.68 [0.52, 0.89] |
Comparison 6. Sub‐analysis: Sanitation coverage.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 6.1 Coverage < 75%: diarrhoea ‐ all ages | 18 | Risk Ratio (IV, Random, 95% CI) | 0.87 [0.77, 0.99] | |
| 6.1.1 Cluster‐RCTs | 10 | Risk Ratio (IV, Random, 95% CI) | 0.94 [0.88, 1.01] | |
| 6.1.2 NRCTs | 8 | Risk Ratio (IV, Random, 95% CI) | 0.77 [0.51, 1.16] | |
| 6.2 Coverage < 75%: diarrhoea ‐ children < 5 years | 15 | Risk Ratio (IV, Random, 95% CI) | 0.88 [0.77, 0.99] | |
| 6.2.1 Cluster‐RCTs | 10 | Risk Ratio (IV, Random, 95% CI) | 0.93 [0.87, 1.00] | |
| 6.2.2 NRCTs | 5 | Risk Ratio (IV, Random, 95% CI) | 0.82 [0.52, 1.30] | |
| 6.3 Coverage 75% or higher: diarrhoea ‐ all ages | 14 | Risk Ratio (IV, Random, 95% CI) | 0.66 [0.52, 0.83] | |
| 6.3.1 Cluster‐RCTs | 3 | Risk Ratio (IV, Random, 95% CI) | 0.90 [0.65, 1.24] | |
| 6.3.2 NRCTs | 11 | Risk Ratio (IV, Random, 95% CI) | 0.58 [0.43, 0.78] | |
| 6.4 Coverage 75% or higher: diarrhoea ‐ children < 5 years | 10 | Risk Ratio (IV, Random, 95% CI) | 0.71 [0.55, 0.92] | |
| 6.4.1 Cluster‐RCTs | 3 | Risk Ratio (IV, Random, 95% CI) | 0.90 [0.65, 1.24] | |
| 6.4.2 NRCTs | 7 | Risk Ratio (IV, Random, 95% CI) | 0.62 [0.43, 0.90] |
Comparison 7. Sub‐analysis: Increase in coverage.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 7.1 Coverage increase < 50%: diarrhoea ‐ all ages | 16 | Risk Ratio (IV, Random, 95% CI) | 0.79 [0.67, 0.94] | |
| 7.1.1 Cluster‐RCTs | 10 | Risk Ratio (IV, Random, 95% CI) | 0.94 [0.88, 1.01] | |
| 7.1.2 NRCTs | 6 | Risk Ratio (IV, Random, 95% CI) | 0.69 [0.40, 1.18] | |
| 7.2 Coverage increase < 50%: diarrhoea ‐ children < 5 years | 16 | Risk Ratio (IV, Random, 95% CI) | 0.79 [0.66, 0.94] | |
| 7.2.1 Cluster‐RCTs | 10 | Risk Ratio (IV, Random, 95% CI) | 0.93 [0.87, 1.00] | |
| 7.2.2 NRCTs | 6 | Risk Ratio (IV, Random, 95% CI) | 0.69 [0.40, 1.18] | |
| 7.3 Coverage increase 50% or more: diarrhoea ‐ all ages | 8 | Risk Ratio (IV, Random, 95% CI) | 0.77 [0.62, 0.96] | |
| 7.3.1 Cluster‐RCTs | 3 | Risk Ratio (IV, Random, 95% CI) | 0.90 [0.65, 1.24] | |
| 7.3.2 NRCTs | 5 | Risk Ratio (IV, Random, 95% CI) | 0.64 [0.42, 0.96] | |
| 7.4 Coverage increase 50% or more: diarrhoea ‐ children < 5 years | 7 | Risk Ratio (IV, Random, 95% CI) | 0.87 [0.71, 1.05] | |
| 7.4.1 Cluster‐RCTs | 3 | Risk Ratio (IV, Random, 95% CI) | 0.90 [0.65, 1.24] | |
| 7.4.2 NRCTs | 4 | Risk Ratio (IV, Random, 95% CI) | 0.82 [0.61, 1.10] |
Comparison 8. Sub‐analysis: Length of follow‐up.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 8.1 1 year or less: diarrhoea ‐ all ages | 19 | Risk Ratio (IV, Random, 95% CI) | 0.70 [0.58, 0.84] | |
| 8.1.1 Cluster‐RCTs | 7 | Risk Ratio (IV, Random, 95% CI) | 0.88 [0.73, 1.05] | |
| 8.1.2 NRCTs | 12 | Risk Ratio (IV, Random, 95% CI) | 0.55 [0.41, 0.74] | |
| 8.2 1 year or less: diarrhoea ‐ children < 5 years | 12 | Risk Ratio (IV, Random, 95% CI) | 0.75 [0.59, 0.94] | |
| 8.2.1 Cluster‐RCTs | 7 | Risk Ratio (IV, Random, 95% CI) | 0.88 [0.73, 1.05] | |
| 8.2.2 NRCTs | 5 | Risk Ratio (IV, Random, 95% CI) | 0.52 [0.29, 0.94] | |
| 8.3 > 1 year to 2 years: diarrhoea ‐ all ages | 17 | Risk Ratio (IV, Random, 95% CI) | 0.80 [0.70, 0.92] | |
| 8.3.1 Cluster‐RCTs | 10 | Risk Ratio (IV, Random, 95% CI) | 0.84 [0.73, 0.97] | |
| 8.3.2 NRCTs | 7 | Risk Ratio (IV, Random, 95% CI) | 0.76 [0.55, 1.06] | |
| 8.4 > 1 year to 2 years: diarrhoea ‐ children < 5 years | 11 | Risk Ratio (IV, Random, 95% CI) | 0.83 [0.70, 0.97] | |
| 8.4.1 Cluster‐RCTs | 7 | Risk Ratio (IV, Random, 95% CI) | 0.88 [0.77, 1.00] | |
| 8.4.2 NRCTs | 4 | Risk Ratio (IV, Random, 95% CI) | 0.76 [0.46, 1.25] | |
| 8.5 3 years or more: diarrhoea ‐ all ages | 11 | Risk Ratio (IV, Random, 95% CI) | 0.71 [0.58, 0.87] | |
| 8.5.1 NRCTs | 11 | Risk Ratio (IV, Random, 95% CI) | 0.71 [0.58, 0.87] | |
| 8.6 3 years or more: diarrhoea ‐ children < 5 years | 8 | Risk Ratio (IV, Random, 95% CI) | 0.80 [0.70, 0.93] | |
| 8.6.1 NRCTs | 8 | Risk Ratio (IV, Random, 95% CI) | 0.80 [0.70, 0.93] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Arnold 2010.
| Study characteristics | ||
| Methods | Matched cohort study among 25 clusters (12 intervention, 13 control villages) | |
| Participants | 900 households with 1284 children < 5 years | |
| Interventions | Combined WASH intervention that included components of sanitation and hygiene promotion, water supply improvements, and microcredit loans. The sanitation intervention included a community mobilization campaigns to build toilets, formation of village water and sanitation committees, construction or renovation of primary school toilets, formation of self‐help groups to promote toilet use and construction, technical support and local training for toilet construction, capital cost assistance with subsidized loans for some families, and certification of villages as open defecation‐free. Intervention details varied slightly by village. | |
| Outcomes | Prevalence of diarrhoea in children < 5 years; anthropometric outcomes. Diarrhoea was defined as 3 or more loose or watery stools in 24 hours or a single stool with blood or mucus, with a 14‐day recall period. | |
| Notes | Location: India, rural Length of study: 1.5 years ("Between January 2008 and April 2009 we visited each participating household once per month for a total of 12 visits.") Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomized trial (not randomly assigned) |
| Allocation concealment (selection bias) | High risk | Matched cohort study, so the researchers selected control villages by matching to villages that had previously received the intervention |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing data from children lost to follow‐up are similar across intervention and control villages |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Low risk | Analysis adjusted for potential relevant confounders |
| Baseline outcome measurements similar | Unclear risk | Baseline measurements for outcomes not reported |
| Baseline characteristics similar | Low risk | Baseline characteristics similar |
| Protection against contamination | Low risk | Intervention allocated by village and it is unlikely that the control group received the intervention |
Aziz 1990.
| Study characteristics | ||
| Methods | Cluster non‐randomized controlled trial amongst 5 clusters (2 intervention villages and 3 control villages) | |
| Participants | 1570 households with approximately 9600 people and 1390 children < 5 years | |
| Interventions | Combined WASH intervention that included components of sanitation, water supply improvement, and hygiene education. The sanitation intervention included the installation of a locally manufactured double pit water‐sealed latrine and messaging about the need for all the members of the household, including young children, to use sanitary latrines. The latrines were installed at no or nominal cost, but the users had to install the superstructures or contribute towards their installation. | |
| Outcomes | Incidence of diarrhoea, persistent diarrhoea, and dysentery in children < 5 years. Diarrhoea was defined as 3 or more loose motions in a 24‐hour period, with a 7‐day recall period. Persistent diarrhoea was defined as an episode lasting more than 14 days. Dysentery was defined as blood being present in stools. | |
| Notes | Location: Bangladesh, rural Length of study: 4 years (a baseline census was completed in January 1984. Hand pumps were installed in 1984 and latrine improvements were complete by the end of 1985. Information on diarrhoeal morbidity in children under 5 years old was collected from March 1984 to December 1987 through weekly visits). Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomized trial (not randomly assigned) |
| Allocation concealment (selection bias) | Unclear risk | Not specified who allocated the intervention to units |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Missing outcome data not specified in paper |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | High risk | Logistic regression controlled for confounding variables within intervention area comparison, but not for the intervention‐control comparison reported in this review |
| Baseline outcome measurements similar | Low risk | No baseline differences in outcome measurements |
| Baseline characteristics similar | Unclear risk | No report of baseline characteristics (other than outcomes) |
| Protection against contamination | Low risk | Intervention allocated by village and it is unlikely that the control group received the intervention |
Azurin 1974.
| Study characteristics | ||
| Methods | Cluster non‐randomized controlled trial amongst 4 clusters (3 intervention, 1 control village) | |
| Participants | 462 households with 3089 individuals of all ages and 527 children < 5 | |
| Interventions | Improved toilets and improved water (1 cluster): a piped water system was installed. Communal toilet buildings were installed with each building housing 8 flush‐type toilets and divided sections for males and females. Each building had its own septic tank built of hollow blocks and reinforced concrete. Waste was discharged untreated into nearby canals or creaks that drained into the sea. One toilet was provided for every 28 to 30 inhabitants. All construction materials were provided by the research project and the city government as well as the specialized labour for plumbing and carpentry. Improved toilets, poor water (1 cluster): communal toilets were built, which included 1 toilet for about every 4 households (1 toilet for every 25 to 30 residents). All construction materials were provided by the research project, while the community supplied the labour. No changes were made to the community's water, which was supplied by 4 wells with hand pumps. Improved water, poor toilets (1 cluster): water supply was improved to provide piped water treated with chlorination. No changes were made to the community's sanitation and no households in the community had toilets. |
|
| Outcomes | Incidence of cholera. A cholera case was defined as someone with gastrointestinal diarrhoea symptoms and a rectal swab positive for cholera vibrios. | |
| Notes | Location: Philippines, urban and peri‐urban Length of study: 4.5 years (1 June 1968 to 31 December 1972) Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomized trial (not randomly assigned) |
| Allocation concealment (selection bias) | Unclear risk | Not specified who allocated the intervention to units |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome data for main outcome are complete |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | High risk | No adjustment for confounding variables |
| Baseline outcome measurements similar | High risk | Baseline differences in diarrhoea not adjusted for |
| Baseline characteristics similar | Unclear risk | No baseline characteristics for socioeconomic status or access to water or sanitation facilities were reported |
| Protection against contamination | Low risk | Intervention allocated by village and it is unlikely that the control group received the intervention |
Boubacar Maïnassara 2014.
| Study characteristics | ||
| Methods | Cluster non‐randomized controlled trial among 6 clusters (3 intervention, 3 control schools) | |
| Participants | 696 school children aged 7 to 12 years | |
| Interventions | Combined WASH intervention in schools that included components of sanitation, water supply improvement, installation of handwashing stations, and hygiene education. The sanitation intervention included the construction of latrines and educational messaging regarding the use of latrines. | |
| Outcomes | Prevalence of self‐reported diarrhoea, abdominal pains, and vomiting. Prevalence of parasites in stool samples. Student absence from school. The case definition of diarrhoea used in the study was not reported. | |
| Notes | Location: Niger, rural Length of study: ~1.5 years (the first field survey was carried out in November 2007 prior to the start of the programme, and the second in May 2008) Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomized trial (not randomly assigned) |
| Allocation concealment (selection bias) | Unclear risk | Not specified who allocated the intervention to units |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Few outcome data missing |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | High risk | No adjustment for confounding variables |
| Baseline outcome measurements similar | Low risk | No baseline differences in outcome measurements |
| Baseline characteristics similar | High risk | There was a higher proportion of girls and students who use the latrine at home in the intervention group at baseline. This difference was not adjusted for in the analysis. |
| Protection against contamination | Unclear risk | Intervention and control schools were close to each other and it is possible that communication about the project could have occurred between students at the different schools. |
Briceno 2017.
| Study characteristics | ||
| Methods | Cluster‐randomized controlled trial among 181 clusters (44 sanitation intervention, 46 sanitation + handwashing intervention, 45 handwashing intervention, 46 control wards) | |
| Participants | 3619 households with 5797 children < 5 years | |
| Interventions | The sanitation intervention was labelled Total Sanitation and Sanitation Marketing (TSSM), which used CLTS and sanitation marketing techniques. CLTS included a triggering event and formation of a local committee to motivate households to move up the sanitation ladder. The sanitation marketing campaign focused on marketing hygienic latrines as something to aspire to and primarily targeted the head of household. These activities were also complemented with training of local masons in latrine construction and marketing. No subsidies were provided. The handwashing intervention targeted mothers with children < 5 years using social marketing messages to increase awareness of the importance of handwashing and provide technical assistance for building tippy tap handwashing stations. |
|
| Outcomes | Prevalence of diarrhoea in children < 5 years, anaemia, anthropometric outcomes. Diarrhoea was defined as 3 or more loose or watery stools in a 24‐hour period or a single stool with blood or mucus, with 7‐day and 14‐day recall periods. | |
| Notes | Location: Tanzania, rural Length of follow‐up: ~12 months after intervention (sanitation campaign: June 2009 to June 2011; endline: May to December 2012) Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used a computer random number generator: "The ward‐level randomization was stratified by district and population size using Stata." |
| Allocation concealment (selection bias) | Low risk | Allocation was performed centrally by study investigators |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding. Diarrhoea outcome is caregiver‐reported in this study, so there is potential for courtesy bias. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Steps were taken to reduce enumerator bias for outcome assessors: "To mitigate enumerator bias, survey firms were never provided information on treatment status of participating wards." However, it is unclear if enumerators could have inferred intervention status due to visual components of the intervention. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Limited migration and attrition in the study area |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | NA |
| Recruitment bias | Unclear risk | Randomization was completed before participant recruitment, but it is unclear if participants were aware of the village's intervention status at the time of recruitment |
| Baseline imbalance | Unclear risk | The study did not have a baseline so it is not possible to assess baseline balance |
| Loss of clusters | Low risk | No clusters lost |
| Incorrect analysis | Low risk | Standard error in model accounts for clustering: "Standard errors are clustered at the ward level" |
Cameron 2013.
| Study characteristics | ||
| Methods | Cluster‐randomized controlled trial among 160 clusters (80 intervention, 80 control sub‐villages in 10 intervention and 10 control villages) | |
| Participants | 2500 households with 2639 children < 5 years | |
| Interventions | The sanitation intervention was labelled TSSM, which consisted of 3 main components: CLTS, social marketing of sanitation, and strengthening the enabling environment. The intervention is aimed at increasing the demand for sanitation and increasing the supply of sanitation products and services, and does not provide infrastructure or include subsidies for households. | |
| Outcomes | Prevalence of diarrhoea, mucus or blood in stool (dysentery), helminth infections, acute lower respiratory infection, and acute respiratory infection. Diarrhoea was defined as 3 or more loose or watery stools per day or blood and/or mucus is visible in the stool, with 2‐day and 7‐day recall periods. | |
| Notes | Location: Indonesia, rural Length of follow‐up: 2 years (baseline survey was conducted in August to September 2008; endline survey was conducted in between November 2010 and February 2011) Publication status: working paper |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used a computer random number generator: "Using a random number generator in STATA, the IE team randomly selected 10 treatment and 10 control villages from each district list." |
| Allocation concealment (selection bias) | Low risk | Allocation was performed centrally by the impact evaluation team |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding. Diarrhoea outcome is caregiver‐reported in this study, so there is potential for courtesy bias. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | It is unclear if the outcome assessors were blinded to intervention status or not |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rates were similar in control and intervention groups |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | NA |
| Recruitment bias | Unclear risk | Randomization was completed before participant recruitment, but it is unclear if participants were aware of the village's intervention status at the time of recruitment |
| Baseline imbalance | Low risk | Characteristics were similar for control and intervention groups at baseline |
| Loss of clusters | Low risk | No clusters lost |
| Incorrect analysis | Low risk | Standard error in model adjusts for clustering: "All specifications also allow for village‐level clustering of the standard errors. " |
Cao 2007.
| Study characteristics | ||
| Methods | Matched cohort study among 12 clusters (4 sanitation + water supply intervention, 5 sanitation or water supply intervention, 3 control villages) | |
| Participants | 5146 residents | |
| Interventions | Improved sanitation intervention: installation of biogas toilets at households Improved water supply intervention: improved water supply with a separate water source for piped water |
|
| Outcomes | Diarrhoea incidence in all residents. Diarrhoea was defined as 3 or more loose or watery stools per day, but the recall period was not specified. | |
| Notes | Location: China, rural Length of study: not reported Publication status: Journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomized trial (not randomly assigned) |
| Allocation concealment (selection bias) | High risk | Matched cohort study, so the researchers selected control villages by matching to villages that had previously received the intervention |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Missing outcome data not specified in paper |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | High risk | No adjustment for confounding variables |
| Baseline outcome measurements similar | Unclear risk | Baseline measures of outcome not reported |
| Baseline characteristics similar | Unclear risk | Baseline characteristics not reported |
| Protection against contamination | Low risk | Intervention allocated by village and it is unlikely that the control group received the intervention |
Cha 2021.
| Study characteristics | ||
| Methods | Cluster‐randomized controlled trial among 48 clusters (24 intervention, 24 control villages) | |
| Participants | 906 households with children < 5 years | |
| Interventions | Community‐led total sanitation (CLTS) strategies to encourage community members to build improved toilets. The CLTS programme focused on collective behaviour change to create open defecation‐free villages, enabling communities to become aware of the sanitation situation and initiating desire to improve community‐wide sanitation. While CLTS interventions do not typically prescribe toilet types, during this trial community members were encouraged to build improved toilets because the coverage of simple pit toilets was already high and open defecation was relatively uncommon. No material or financial subsidies were provided for construction of household latrines. | |
| Outcomes | Incidence, longitudinal prevalence, and 7‐day period prevalence of diarrhoea in children < 5. Diarrhoea was defined as 3 or more loose or watery stools within 24 hours, with a 7‐day recall. | |
| Notes | Location: Ethiopia, rural Length of follow‐up: 10 months (outcomes measured at 3, 5, 9, and 10 months after CLTS initiation) Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomized with community lottery ceremony: "Randomization was performed during a community lottery ceremony by community leaders in each district. The allocation ratio was 1:1, with 24 villages in the intervention group and 24 villages in the control groups. If the two villages in a kebele happened to be allocated to the same arm during the lottery, then we asked community leaders to perform the lottery again until the two villages were finally assigned to different arms." |
| Allocation concealment (selection bias) | Low risk | Allocation took place at a public lottery ceremony |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding. Diarrhoea outcome is caregiver‐reported in this study, so there is potential for courtesy bias. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not blinded: "Enumerators were not informed of the allocation to an intervention or control village; however, because some components of the intervention were visible, particularly toilet construction, they could not be masked to their intervention status" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rates and reasons were similar in control and intervention groups |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | NA |
| Recruitment bias | Low risk | Participants were recruited before allocation |
| Baseline imbalance | Low risk | Diarrhoea prevalence was higher in the intervention than control group at baseline (22.2% versus 17.1%), and the coverage of improved water and sanitation was lower in the intervention group than in the control group at baseline. However, these factors were adjusted for in the statistical model. |
| Loss of clusters | Low risk | No clusters lost |
| Incorrect analysis | Low risk | Models adjust for clustering: "We accounted for intra‐village and intra‐individual correlations and adjusted for stratification by kebele." |
Chard 2019.
| Study characteristics | ||
| Methods | Cluster‐randomized controlled trial among 100 clusters (50 WASH intervention, 50 control schools) | |
| Participants | 3545 primary school students from grades 3 to 5 | |
| Interventions | Combined WASH intervention in schools that included components of sanitation, provision of a school water supply, installation of handwashing stations, and hygiene education. The hardware component of the sanitation intervention included the school sanitation facilities, which consisted of 3 separate toilet compartments designated for boys, girls, and disabled students. The software component of the sanitation intervention encourage toilet cleanliness, with pre‐organized teams of male and female students performing light routine cleaning and maintenance of toilets. | |
| Outcomes | Prevalence of diarrhoea, respiratory infection, and conjunctivitis/non‐vision related eye illness in students, as well as absence from school and other educational impacts. Diarrhoea was defined as having diarrhoea (based on local terminology) and defecating 3 or more times in a 24‐hour period, with a 1‐week recall period. | |
| Notes | Location: Laos Length of follow‐up: 2 to 3 years Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used a computer random number generator: "Schools were randomly selected from a list of 222 eligible schools provided by UNICEF Lao PDR...Using a random number generator in Excel (Microsoft Corporation, Redmond, WA, USA), 100 schools were selected from this list for inclusion in the evaluation." |
| Allocation concealment (selection bias) | Low risk | Allocation was performed centrally by the research manager |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding. Diarrhoea outcome is self‐reported in this study, so there is potential for courtesy bias. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not possible to blind enumerators to intervention status due to the nature of the intervention |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rates and reasons were similar in control and intervention groups |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | NA |
| Recruitment bias | Low risk | Randomization was completed before participant recruitment, but it is unlikely participants were aware of the school's intervention status at the time of recruitment: "Given the need to plan for the intervention, we randomized the schools prior to baseline. Enumerators were blinded to this allocation at baseline." |
| Baseline imbalance | Low risk | Characteristics were similar for control and intervention groups at baseline |
| Loss of clusters | Low risk | No clusters lost |
| Incorrect analysis | Low risk | Models adjust for clustering: "Random intercepts at the school and pupil levels were included to account for clustering of pupils within schools and for repeated measures of pupils over time, respectively." |
Clasen 2014.
| Study characteristics | ||
| Methods | Cluster‐randomized controlled trial among 100 clusters (50 intervention, 50 control villages) | |
| Participants | 20,283 individuals, including 3880 children < 5 years | |
| Interventions | India's Total Sanitation Campaign (TSC), which combines social mobilization with a post hoc subsidy and included latrine promotion and construction. The latrine design consisted of a pour‐flush latrine with a single pit and Y‐joint for a future second pit. Subsidies were provided to households that met below‐poverty‐line criteria. Each participating below‐poverty‐line household was to be provided with a latrine and households contributed sand, bricks, and labour. The subsidy did not cover the cost of full walls, door, and roof. | |
| Outcomes | Prevalence of diarrhoea in children < 5 years and all household members, soil‐transmitted helminths in participants aged 5 to 40 years, anthropometric outcomes in children < 5 years, and faecal contamination in households. Diarrhoea was defined as 3 or more loose stools in 24 hours, with a 7‐day recall. | |
| Notes | Location: India, rural Length of follow‐up: 18 months Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used a computer‐generated sequence: "A member of staff who was involved in neither data collection nor intervention delivery randomly assigned villages (1:1), with a computer‐generated sequence, to undergo either latrine promotion and construction in accordance with the Total Sanitation Campaign or to receive no intervention (control)." |
| Allocation concealment (selection bias) | Low risk | Allocation was performed centrally by a member of staff who was involved in neither data collection nor intervention delivery |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding. Diarrhoea outcome is caregiver‐reported in this study, so there is potential for courtesy bias. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Although the surveillance team was different from the intervention team, they could not be blinded of intervention status because the intervention included visible components |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rates and reasons were similar in control and intervention groups |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | NA |
| Recruitment bias | Low risk | Participants were recruited before allocation ‐ the baseline survey occurred before randomization |
| Baseline imbalance | Low risk | Characteristics were similar for control and intervention groups at baseline |
| Loss of clusters | Low risk | No clusters lost |
| Incorrect analysis | Low risk | Standard error in model accounts for clustering: "Village‐level clustering was accounted for by generalised estimating equations with robust SEs. " |
Dickinson 2015.
| Study characteristics | ||
| Methods | Cluster‐randomized controlled trial among 40 clusters (20 intervention, 20 control villages) | |
| Participants | 1050 households with 1256 children < 5 years | |
| Interventions | Behaviour change sanitation intervention with CLTS style participatory activities to promote community‐wide latrine adoption, including a walk of shame, faecal calculation, and special mapping activities. The campaign subsidized materials and labour for latrine construction for households that were below the poverty line. The campaign also promoted health and non‐health benefits of latrine use. | |
| Outcomes | Prevalence of diarrhoea and anthropometric outcomes in children < 5 years. The case definition of diarrhoea used in the study was not reported, but the recall period for diarrhoea was 14 days. | |
| Notes | Location: India, rural Length of follow‐up: 3 to 4 months (the intervention took place in March and May 2006 and postintervention data were collected in August and September 2006) Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Publicly drew lots from a bucket for randomization: "in a town hall–style gathering of village leaders, we randomly selected 20 of the 40 sample villages from a bucket containing slips of paper with village names. These 20 villages were assigned to the “treatment” group, while the other 20 villages served as “controls." " |
| Allocation concealment (selection bias) | Low risk | Allocation took place at a public lottery by drawing random village names out of a bucket |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding. Diarrhoea outcome is caregiver‐reported in this study, so there is potential for courtesy bias. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | It is unclear if the outcome assessors were blinded to intervention status or not |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rates and reasons were similar in control and intervention groups |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | NA |
| Recruitment bias | Low risk | Participants were recruited before allocation ‐ the baseline survey occurred before randomization |
| Baseline imbalance | Low risk | Characteristics were generally similar for control and intervention groups at baseline |
| Loss of clusters | Low risk | No clusters lost |
| Incorrect analysis | Low risk | Standard error in model accounts for clustering: "Standard errors clustered at the village level, and robust p‐values calculated for all covariates" |
Freeman 2014a.
| Study characteristics | ||
| Methods | Cluster‐randomized controlled trial among 135 water‐available clusters (45 WASH intervention, 45 hygiene + water intervention, 45 control water‐available schools) and 50 water‐scarce clusters (25 WASH intervention, 25 control water‐scarce schools) Freeman 2014a refers to the intervention and results from water‐available schools |
|
| Participants | 2913 pupils in water‐available schools and 1053 pupils in water‐scarce schools | |
| Interventions | Water‐available schools: WASH intervention – installation of ventilated improved pit latrines (number based on existing pupil:latrine ratios), teacher training on hygiene behaviour change, providing containers for safe drinking water storage, buckets with taps to be used for handwashing, and a 1‐year supply of WaterGuard (a liquid chlorine‐based sodium hypochlorite solution used for point‐of‐use water treatment) Water‐scarce schools: WASH intervention – installation of an improved water supply at school + the intervention described above for water‐available schools |
|
| Outcomes | Diarrhoea prevalence, pupil absence from school. Diarrhoea was defined as 3 or more loose or watery stools over a 24‐hour period, with a 7‐day recall period. | |
| Notes | Location: Kenya, rural Length of study: 1.5 years (baseline survey: February to March 2007; endline survey after implementation: September to October 2008) Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used a computer random number generator: "All random selection and allocation was conducted by the research manager using a random number generator in Microsoft Excel" |
| Allocation concealment (selection bias) | Low risk | Allocation was performed centrally by the research manager |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding. Diarrhoea outcome is self‐reported in this study, so there is potential for courtesy bias. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding of outcome assessment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No schools lost to follow‐up; < 1% of pupils did not provide diarrhoeal data |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | NA |
| Recruitment bias | Unclear risk | Randomization was completed before participant recruitment, but it is unclear if participants were aware of the school's intervention status at the time of recruitment |
| Baseline imbalance | Low risk | Models were adjusted for baseline characteristics |
| Loss of clusters | Low risk | No clusters lost |
| Incorrect analysis | Low risk | Standard error in model adjusts for clustering: "adjusted our variance to account for clustering at the school level using robust standard error" |
Freeman 2014b.
| Study characteristics | ||
| Methods | Cluster‐randomized controlled trial among 135 water‐available clusters (45 WASH intervention, 45 hygiene + water intervention, 45 control water‐available schools) and 50 water‐scarce clusters (25 WASH intervention, 25 control water‐scarce schools) Freeman 2014b refers to the intervention and results from water‐scarce schools |
|
| Participants | 2913 pupils in water‐available schools and 1053 pupils in water‐scarce schools | |
| Interventions | Water‐available schools: WASH intervention – installation of ventilated improved pit latrines (number based on existing pupil:latrine ratios), teacher training on hygiene behaviour change, providing containers for safe drinking water storage, buckets with taps to be used for handwashing, and a 1‐year supply of WaterGuard (a liquid chlorine‐based sodium hypochlorite solution used for point‐of‐use water treatment) Water‐scarce schools: WASH intervention – installation of an improved water supply at school + the intervention described above for water‐available schools |
|
| Outcomes | Diarrhoea prevalence; pupil absence from school. Diarrhoea was defined as 3 or more loose or watery stools over a 24‐hour period, with a 7‐day recall period. | |
| Notes | Location: Kenya, rural Length of study: 1.5 years (baseline survey: February to March 2007; endline survey after implementation: September to October 2008) Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used a computer random number generator: "All random selection and allocation was conducted by the research manager using a random number generator in Microsoft Excel" |
| Allocation concealment (selection bias) | Low risk | Allocation was performed centrally by the research manager |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding. Diarrhoea outcome is self‐reported in this study, so there is potential for courtesy bias. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding of outcome assessment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No schools lost to follow‐up; < 1% of pupils did not provide diarrhoeal data |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | NA |
| Recruitment bias | Unclear risk | Randomization was completed before participant recruitment, but it is unclear if participants were aware of the school's intervention status at the time of recruitment |
| Baseline imbalance | Low risk | Models were adjusted for baseline characteristics |
| Loss of clusters | Low risk | No clusters lost |
| Incorrect analysis | Low risk | Standard error in model adjusts for clustering: "adjusted our variance to account for clustering at the school level using robust standard error" |
Garrett 2008.
| Study characteristics | ||
| Methods | Cluster non‐randomized controlled trial among 18 clusters (12 intervention, 6 control villages) | |
| Participants | 960 children < 5 years | |
| Interventions | Combined WASH intervention that included components of sanitation and water supply and quality improvement. The sanitation intervention included the promotion of latrines with cement sanitary platforms and VIP latrines, each of which was lined with cement trapezoidal blocks and had a superstructure made of bricks or tree branches. Communities were also taught about the link between sanitation and health. Interested persons were provided training in manufacture of cement platforms and blocks as well as construction of both types of latrine. The programme paid for 40% of latrine costs and community members paid for 60% of costs and provided the labour. The water supply and quality intervention included digging shallow wells, promoting rainwater harvesting, and the promotion and selling of chlorine‐based water disinfection solution and safe storage containers in villages, including a social marketing campaign. | |
| Outcomes | Diarrhoea incidence in children < 5 years. Diarrhoea was defined as 3 or more loose stools in a 24‐hour period, with a 7‐day recall period. | |
| Notes | Location: Kenya, rural Length of study: 2 years (outcome assessment occurred 2 years post‐intervention through weekly household visits over 8 weeks from March to May 2001) Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomized trial (not randomly assigned) |
| Allocation concealment (selection bias) | Unclear risk | Not specified who allocated the intervention to units |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 2 intervention villages were removed from the results due to concerns that data were being fabricated by 2 enumerators |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Low risk | Analysis adjusted for potential WASH confounders and reported that other potential confounders like age, education, and socio‐economic status did not modify the association of interventions with diarrhoea risk |
| Baseline outcome measurements similar | Unclear risk | Baseline measurements of outcomes not collected |
| Baseline characteristics similar | Unclear risk | The intervention was already in progress when the "baseline" was completed |
| Protection against contamination | Low risk | Intervention allocated by village and it is unlikely that the control group received the intervention |
Hammer 2016.
| Study characteristics | ||
| Methods | Cluster‐randomized controlled trial among 60 clusters (30 intervention, 30 control villages) | |
| Participants | 3440 children < 5 years | |
| Interventions | India's Total Sanitation Campaign for latrine promotion and construction. This sanitation intervention included 2 components: (1) fully subsidized construction of standard TSC brick household pit latrines by local governments, and (2) village‐level sanitation motivation by a representative of the district government inspired by the procedures of CLTS the programme. For this behaviour change promotion, a sanitation promoter visited the village and held a series of meetings where information, persuasion, demonstration, and social forces were employed in an attempt to “trigger” a community‐wide switch to latrine use. | |
| Outcomes | Prevalence of diarrhoea and anthropometric outcomes in children < 5 years. The case definition of diarrhoea used in the study was not reported. | |
| Notes | Location: India, rural Length of follow‐up: 18 months after intervention Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used a computer random number generator: "Sixty villages in each district were identified as eligible for randomization, and of these 30 each were randomly assigned to treatment and control groups using pseudo‐random number generator functions in Microsoft Excel, in a different “worksheet” spreadsheet page for each district." |
| Allocation concealment (selection bias) | Unclear risk | It is unclear who performed the method of allocation |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding. Diarrhoea outcome is caregiver‐reported in this study, so there is potential for courtesy bias. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | The outcome assessors could not be blinded to intervention status because the intervention included visible components |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rates were similar in control and intervention groups |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | NA |
| Recruitment bias | Unclear risk | The order of recruitment and randomization is not reported |
| Baseline imbalance | Low risk | Characteristics were similar for control and intervention groups at baseline |
| Loss of clusters | Low risk | No clusters lost |
| Incorrect analysis | Low risk | Standard error in model accounts for clustering: "Because the experimental treatment was assigned at the village level, in all regression estimates standard errors clustered by village." |
Hashi 2017.
| Study characteristics | ||
| Methods | Cluster‐randomized controlled trial among 24 clusters (12 intervention, 12 control kebele clusters) | |
| Participants | 1199 children < 5 years | |
| Interventions | Combined WASH intervention that included health education behaviour change messaging related to sanitation, water storage, and handwashing. The sanitation intervention included messaging to have a latrine and use it properly and if you don't have a latrine to share with the nearest neighbourhood and build a latrine. Messaging related to water storage and handwashing included instructions to keep their water storage container clean and covered, and to wash their hands and children's hands ideally with soap after defecation and other key times. Twelve sessions of health education on these key WASH messages and demonstration of handwashing with soap were given to all of the intervention clusters by clinical nurse professionals (field workers) every 2 weeks. | |
| Outcomes | Incidence of diarrhoea in children < 5 years; bacteriological quality of household drinking water. Diarrhoea was defined as 3 or more liquid or semi‐liquid stools in a 24‐hour period or the passage of at least 1 liquid or semi‐liquid stool with blood or mucus, with a 14‐day recall period. | |
| Notes | Location: Ethiopia, rural Length of follow‐up: 6 months (the follow‐up study started on 1 February 2015 and ended 30 July 2015) Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used a combination of a public lottery and a computer random number generator: "Eligible Kebelles in the north and south were assigned randomly to intervention and control groups respectively by using lottery method in the presence of community leaders...Twenty‐four Sub‐Kebelles were then randomly selected from the 56 total sub‐Kebelles by using simple randomization (computer generated numbers)." |
| Allocation concealment (selection bias) | Low risk | Allocation of administrative units to intervention/control took place at a public lottery and the selected sub‐Kebelles were selected centrally by study investigators |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding. Diarrhoea outcome is caregiver‐reported in this study, so there is potential for courtesy bias. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | It is unclear is outcome assessors were blinded to intervention status and whether they would have been able to ascertain whether households were part of the intervention or not |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rates and reasons were similar in control and intervention groups |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | NA |
| Recruitment bias | Unclear risk | Randomization was completed before participant recruitment, but it is unclear if participants were aware of the village's intervention status at the time of recruitment |
| Baseline imbalance | Low risk | Characteristics were similar for control and intervention groups at baseline |
| Loss of clusters | Low risk | No clusters lost |
| Incorrect analysis | Low risk | Model accounts for clustering: "We used GEE model to adjust which accounts for clustering based on the average estimated covariates among observations within each cluster." |
Huda 2012.
| Study characteristics | ||
| Methods | Cluster non‐randomized controlled trial among up to 100 clusters (50 intervention, 50 control villages) | |
| Participants | 1699 children < 5 years | |
| Interventions | Combined WASH intervention that included behaviour change promotional messaging for sanitation, drinking water, and hygiene. The intervention was known as SHEWA‐B, and involved promotional activities where community hygiene promoters visited households, facilitated courtyard meetings, and organized social mobilization activities. The key sanitation messages given by promoters included to "use hygienic latrine by all family members including children", "clean and maintain latrine", and "construct a new latrine if the existing one is full and fill the pit with soil/ash". Other health messaging was given related to handwashing at key times, safe collection and storage of drinking water, disposing of children's faeces into the latrine, safe food cleaning and storage, and safe menstrual hygiene. | |
| Outcomes | Prevalence of diarrhoea and respiratory illness in children < 5 years. Diarrhoea was defined as the passage of 3 or more loose or watery stools within 24‐hour period, with a 2‐day recall period. | |
| Notes | Location: Bangladesh, rural Length of follow‐up: 18 months, with interim assessment at 6 months Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomized trial (not randomly assigned) |
| Allocation concealment (selection bias) | High risk | Intervention allocation was determined by the government and UNICEF independent of the researchers |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Missing outcome data not specified in paper |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | High risk | No adjustment for confounding variables |
| Baseline outcome measurements similar | Unclear risk | Diarrhoea at baseline was higher in control group, but unclear if there was a statistical difference between the groups |
| Baseline characteristics similar | Unclear risk | Water and sanitation baseline characteristics are slightly different at baseline, but unclear if there was a statistical difference between the groups |
| Protection against contamination | Low risk | Intervention allocated by village and it is unlikely that the control group received the intervention |
Humphrey 2019.
| Study characteristics | ||
| Methods | Cluster‐randomized controlled trial among 211 clusters (53 WASH intervention, 53 nutrition intervention, 53 WASH + nutrition intervention, 52 control villages) | |
| Participants | 3686 infants born into the intervention | |
| Interventions | Combined WASH intervention that included components of sanitation, drinking water treatment, and hygiene. The intervention consisted of 3 separate intervention arms: WASH, IYCF (infant and young child feeding), WASH + IYCF. ‐ WASH intervention: the sanitation intervention included the construction of ventilated improved pit latrines. Other components of the intervention included standard‐of‐care messages, plus information about safe disposal of faeces, handwashing with soap at key times, protection of infants from geophagia and ingestion of animal faeces, chlorination of drinking water (especially for infants), and hygienic preparation of complementary food. Two handwashing stations were installed, a plastic mat and play yard were delivered, and soap and chlorine were provided. ‐ IYCF intervention: standard‐of‐care messages plus information about the importance of nutrition for infant health, growth, and development. Participants also received monthly deliveries of 30 sachets of the small‐quantity lipid‐based nutrient supplement to feed infants aged 6 months to 18 months postnatal. |
|
| Outcomes | Diarrhoea prevalence, dysentery prevalence, mortality, anthropometric outcomes, haemoglobin concentration and anaemia, acute respiratory infection prevalence. Diarrhoea was defined as 3 or more loose or watery stools in 24 hours and dysentery was defined as stool with blood or mucus, both with a 7‐day recall. | |
| Notes | Location: Zimbabwe, rural Length of follow‐up: 12 and 18 months (diarrhoea outcomes reported from 12‐ and 18‐month follow‐up visits) Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used a combination of computer generated random allocations that met balance criteria and a public event: "the study's senior statistician, used a constrained randomisation technique 11 to identify 5000 allocation schemes that achieved balance across the groups for 14 variables related to geography, demography, water access, and sanitation coverage, and also met bias and validity specifications (appendix). From these, ten allocations were randomly selected. The final allocation was selected at a public randomisation event attended by elected representatives of the study districts." |
| Allocation concealment (selection bias) | Low risk | Allocation was performed centrally by a study investigator |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding. Diarrhoea outcome is caregiver‐reported in this study, so there is potential for courtesy bias. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Although investigators were blinded to the intervention status until after the final analysis was complete, the data collectors for outcome assessment were not blinded as the intervention was visible. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rates and reasons were similar in control and intervention groups |
| Selective reporting (reporting bias) | Low risk | All primary outcomes reported (some papers with secondary outcomes may be forthcoming) |
| Other bias | Unclear risk | NA |
| Recruitment bias | High risk | Women were enrolled after randomization occurred. They were enrolled during their pregnancy over a period of 2.5 years and could have seen or been aware of intervention activities at the time of their enrollment from other previously enrolled women. |
| Baseline imbalance | Low risk | Characteristics were similar for control and intervention groups at baseline and adjusted analyses controlled for baseline covariates |
| Loss of clusters | Low risk | No clusters lost in clusters that included the sanitation intervention or control |
| Incorrect analysis | Low risk | Standard error in model accounts for clustering: "For primary analyses, we used generalised estimating equations that accounted for within‐cluster correlation" |
Huttly 1990.
| Study characteristics | ||
| Methods | Controlled before‐and‐after study among 4 clusters (2 intervention villages and 2 control villages) | |
| Participants | 1405 households with approximately 7400 individuals and an estimated 1405 children < 6 years of age (noted as wife/child household units) | |
| Interventions | Combined WASH intervention that included components of sanitation, water supply improvement, and health and hygiene education. The sanitation intervention included the promotion and construction of ventilated improved pit (VIP) latrines. Water supply improvement included borehole drilling and hand pump installation. Village‐based workers provided health and hygiene education related to breastfeeding, nutrition, water use, personal hygiene, environmental sanitation, diarrhoea prevention, and oral rehydration therapy, though it was noted to have limitations. | |
| Outcomes | Incidence of diarrhoea in children < 6 years, Dracunculiasis (guinea‐worm) in all ages, and anthropometric outcomes in children < 3 years. Diarrhoea was defined as 3 or more stools of a consistency less than normal in a 24‐hour period. Diarrhoeal episodes were defined to be new if they were preceded by at least 3 diarrhoea‐free days. | |
| Notes | Location: Nigeria, rural Length of follow‐up: 2 years Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomized trial (not randomly assigned) |
| Allocation concealment (selection bias) | High risk | Allocation performed by state government officials |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Missing outcome data not specified in paper |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | High risk | Subgroup analysis is reported as their method of controlling for confounding for some factors such as age, however it appears that this is only done for the within‐intervention area comparison and not the intervention‐control comparison reported in this review |
| Baseline outcome measurements similar | High risk | Baseline differences in diarrhoea not adjusted for |
| Baseline characteristics similar | Unclear risk | No baseline characteristics for access to water or sanitation facilities reported |
| Protection against contamination | Low risk | Intervention allocated by village and it is unlikely that the control group received the intervention |
Jin 2009.
| Study characteristics | ||
| Methods | Matched cohort study among 12 clusters (2 sanitation intervention, 3 water intervention, 4 combined water + sanitation intervention, 3 control villages) | |
| Participants | 5118 households with 20,551 residents | |
| Interventions | The study included an individual sanitation intervention arm as well as a combined WASH intervention arm that included a sanitation and water supply improvement intervention Sanitation intervention: installation of a sanitary latrine at households. Type of latrine varied slightly across households: 96.8% received a biogas toilet, 0.9% received a septic tank, and 1.1% received flushing toilet with sewer system. Improved water supply intervention: centralized water supply with electric water pump |
|
| Outcomes | Diarrhoea incidence in all residents. The case definition of diarrhoea used in the study was defined as 3 or more loose or watery stools per day with a recall period of 3 months. New cases of diarrhoea were considered after 7 days of recovery. | |
| Notes | Location: China, rural Length of follow: 9 months Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomized trial (not randomly assigned) |
| Allocation concealment (selection bias) | High risk | Matched cohort study, so the researchers selected control villages by matching to villages that had previously received the intervention |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Missing outcome data not specified in paper |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | High risk | No adjustment for confounding variables |
| Baseline outcome measurements similar | Unclear risk | No baseline comparison |
| Baseline characteristics similar | Unclear risk | No baseline comparison |
| Protection against contamination | Unclear risk | Unclear if some control households could have received the intervention |
Klasen 2012a.
| Study characteristics | ||
| Methods | Matched cohort study among 4 clusters (2 intervention, 2 control towns) in the coastal region with no water rationing and the mountain region with substantial water rationing (no water available about 60% of the time). Klasen 2014a refers to the intervention and results from towns in the coastal region. | |
| Participants | 2418 households with 18,225 individuals (8706 of which were from the coastal region) | |
| Interventions | Combined WASH intervention that included components of sanitation and water supply improvement. The sanitation intervention included household connections to a sewerage system connected to a wastewater treatment plant. Connection to the sewerage system required household to have connections to piped water supply. | |
| Outcomes | Incidence of diarrhoea in children < 5, incidence of diarrhoea in all household members, severity of diarrhoea in children < 5, severity of diarrhoea in all household members, incidence of waterborne disease in children < 5, incidence of waterborne disease in all household members, missed schooldays of all household members enrolled in school, and missed workdays in all household members of working age. The case definition of diarrhoea used in the study is not reported, but the recall period for diarrhoea was 4 weeks. | |
| Notes | Location: Yemen, urban Length of follow‐up: 4 years (in the coastal region piped water supply was installed in 1998 and sewerage connections were installed in 2005; endline data were collection in 2009) Publication status: working paper |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomized trial (not randomly assigned) |
| Allocation concealment (selection bias) | High risk | Matched cohort study, so the researchers selected control households by matching to households that had previously received the intervention |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Missing outcome data not specified in paper |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | High risk | No adjustment for the specific confounding variables listed in protocol. "The propensity score model used here includes the education level of the household head, household size, dependency ratio, house ownership, and an indicator for knowledge of water‐related diseases." |
| Baseline outcome measurements similar | Unclear risk | Baseline outcome measurements not collected |
| Baseline characteristics similar | Unclear risk | Baseline characteristics not reported |
| Protection against contamination | Low risk | Control towns are located at a distance of 10 to 20 km from treatment towns, so it is unlikely that the control group received the intervention |
Klasen 2012b.
| Study characteristics | ||
| Methods | Matched cohort study among 4 clusters (2 intervention, 2 control towns) in the coastal region with no water rationing and the mountain region with substantial water rationing (no water available about 60% of the time). Klasen 2014a refers to the intervention and results from towns in the mountain region. | |
| Participants | 2418 households with 18,225 individuals (9519 of which were from the mountain region) | |
| Interventions | Combined WASH intervention that included components of sanitation and water supply improvement. The sanitation intervention included household connections to sewerage system connected to wastewater treatment plants. Connection to the sewerage system required household to have connections to piped water supply. | |
| Outcomes | Incidence of diarrhoea in children < 5, incidence of diarrhoea in all household members, severity of diarrhoea in children < 5, severity of diarrhoea in all household members, incidence of waterborne disease in children < 5, incidence of waterborne disease in all household members, missed schooldays of all household members enrolled in school, and missed workdays in all household members of working age. The case definition of diarrhoea used in the study is not reported, but the recall period for diarrhoea was 4 weeks. | |
| Notes | Location: Yemen, urban Length of follow‐up: 5 years (in the mountain region piped water supply was installed in 2002 and sewerage connections were installed in 2004; endline data were collection in 2009) Publication status: working paper |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomized trial (not randomly assigned) |
| Allocation concealment (selection bias) | High risk | Matched cohort study, so the researchers selected control households by matching to households that had previously received the intervention |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Missing outcome data not specified in paper |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | High risk | No adjustment for the specific confounding variables listed in protocol |
| Baseline outcome measurements similar | Unclear risk | Baseline outcome measurements not collected |
| Baseline characteristics similar | Unclear risk | Baseline characteristics not reported |
| Protection against contamination | Low risk | Control towns are located at a distance of 10 to 20 km from treatment towns, so it is unlikely that the control group received the intervention |
Knee 2021.
| Study characteristics | ||
| Methods | Controlled before‐and‐after study among 495 clusters (208 intervention and 287 control compounds) | |
| Participants | 987 children aged 1 to 48 months at baseline | |
| Interventions | The sanitation intervention includes the installation of shared sanitation facilities including communal sanitation blocks (multiple cabins/drop holes serving compounds with a minimum of 21 people with 1 stall allocated per 20 residents) and shared latrines (1 cabin/drop hole serving compounds with a minimum of 12 people). Both communal sanitation blocks and shared latrines include flushing toilets with septic tanks. Communal sanitation blocks also included rainwater harvesting systems, a municipal shared water connection, elevated water tanks for storage of municipal water, a handwashing basin, a laundry facility, and a well‐drained area for bathing. Intervention compounds were expected to pay approximately 10% to 15% of the construction costs (~$64 for shared latrines and ~$97 for communal sanitation blocks) within 1 year of construction, with 25% of the total due upfront. | |
| Outcomes | Prevalence of diarrhoea, combined prevalence of selected enteric infections, combined prevalence of soil‐transmitted helminth reinfection, EED biomarkers in stool, all‐cause mortality, and anthropomorphic outcomes in children aged 1 to 48 months at baseline or follow‐up. The case definition of diarrhoea used in the study was defined as 3 or more loose or liquid stools in a 24‐hour period or any stool with blood with a recall period of 7 days. | |
| Notes | Location: Mozambique, urban Length of follow‐up: 12 and 24 months (outcomes measured at 12 months and 24 months post‐intervention implementation) Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomized trial (not randomly assigned) |
| Allocation concealment (selection bias) | High risk | An NGO selected intervention compounds and the researchers selected control compounds |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing data were similar across study arms. Attrition was high (26% to 33% at 24‐month follow‐up), but a relatively similar number of children were unavailable in intervention and control compounds. However, this number was slightly higher in control compounds due to the need to remove children in compounds that were intended to be controls but received the intervention after the baseline survey. |
| Selective reporting (reporting bias) | Unclear risk | Not all outcomes listed in the study protocol have been reported in the results, but it is likely that they will be reported in future publications |
| Other bias | Low risk | Models were adjusted for potential relevant confounders |
| Baseline outcome measurements similar | Low risk | No baseline differences in outcome measurements |
| Baseline characteristics similar | Low risk | There were some differences in WASH‐related characteristics at baseline, but these were adjusted for in models |
| Protection against contamination | Low risk | Some of the intended control children did receive the intervention, however they were removed from the 24‐month follow‐up analysis |
Kolahi 2009.
| Study characteristics | ||
| Methods | Cluster non‐randomized controlled trial among 80 clusters (40 intervention, 40 control villages) | |
| Participants | 2096 children 6 to 60 months | |
| Interventions | The sanitation intervention was known as the Tehran Sewerage Project, and it provided districts in Tehran with household connections to the urban sewerage system | |
| Outcomes | Incidence of diarrhoea in children 6 to 60 months. The case definition of diarrhoea used in the study was the passage of loose or watery stools at least 3 times in a 24‐hour period with a 14‐day recall period. | |
| Notes | Location: Iran, urban Length of follow‐up: 5 years (baseline survey: May 2001, intervention implemented 4 to 6 months after baseline survey; endline survey: May 2006) Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomized trial (not randomly assigned) |
| Allocation concealment (selection bias) | Unclear risk | Not specified who allocated the intervention to units |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Missing outcome data not specified in paper |
| Selective reporting (reporting bias) | High risk | Some outcomes mentioned in the methods were not reported in the results |
| Other bias | High risk | No adjustment for confounding variables |
| Baseline outcome measurements similar | Unclear risk | Diarrhoea at baseline was slightly higher in the intervention group, but unclear if there was a statistical difference between the groups |
| Baseline characteristics similar | Unclear risk | No baseline characteristics for access to water or sanitation facilities reported |
| Protection against contamination | Low risk | Intervention allocated by village and it is unlikely that the control group received the intervention |
Li 2009.
| Study characteristics | ||
| Methods | Matched cohort study among 4 clusters (2 intervention, 2 control villages) | |
| Participants | 801 participants | |
| Interventions | The sanitation intervention included the installation of improved household toilets | |
| Outcomes | Diarrhoea incidence, fly density, and parasitic disease incidence in all residents. The case definition of diarrhoea used in the study was defined as 3 or more loose or watery stools per day but the recall period was not specified. | |
| Notes | Location: China, rural Length of follow‐up: less than 1 year (the intervention occurred 2005 to 2007 and this study collected data in 2007 for the whole year) Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomized trial (not randomly assigned) |
| Allocation concealment (selection bias) | High risk | Matched cohort study, so the researchers selected control villages by matching to villages that had previously received the intervention |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Missing outcome data not specified in paper |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | High risk | No adjustment for confounding variables |
| Baseline outcome measurements similar | Unclear risk | No baseline comparison |
| Baseline characteristics similar | Unclear risk | No baseline comparison |
| Protection against contamination | Unclear risk | Unclear if some control households could have received the intervention |
Lin 2013.
| Study characteristics | ||
| Methods | Matched cohort study among 6 clusters (3 sanitation intervention, 2 combined water + sanitation intervention, 1 control village) | |
| Participants | 742 households with 2566 people | |
| Interventions | The study included an individual sanitation intervention arm as well as a combined WASH intervention arm that included a sanitation and water supply improvement intervention Sanitation intervention: installation of improved toilets (flushing toilets with either septic tanks or double vault funnels) Improved water supply intervention: centralized water supply |
|
| Outcomes | Diarrhoea incidence in all household members. The case definition of diarrhoea used in the study was defined as 3 or more loose or watery stools per day with a recall period of 3 months. New cases of diarrhoea were considered after 7 days of recovery. | |
| Notes | Location: China, rural Length of study: 1 year (surveys were conducted in March, June, September, and December) Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomized trial (not randomly assigned) |
| Allocation concealment (selection bias) | High risk | Matched cohort study, so the researchers selected control villages by matching to villages that had previously received the intervention |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Missing outcome data not specified in paper |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | High risk | No adjustment for confounding variables |
| Baseline outcome measurements similar | Unclear risk | No baseline comparison |
| Baseline characteristics similar | Unclear risk | No baseline comparison |
| Protection against contamination | Unclear risk | Unclear if some control households could have received the intervention. |
Lou 1989.
| Study characteristics | ||
| Methods | Cluster non‐randomized controlled trial among 3 clusters (2 intervention, 1 control village) | |
| Participants | 3305 individuals, including 315 children < 5 years | |
| Interventions | Combined WASH intervention that included a sanitation and water supply improvement. The sanitation intervention included the installation of improved double vault funnel toilets with slab. The water supply intervention included installation of a centralized water supply system. | |
| Outcomes | Diarrhoea incidence in all residents; pathogens in stool samples; observation of flies; total coliforms in drinking water. Diarrhoea was clinically confirmed. | |
| Notes | Location: China, rural Length of study: 5 years (pre‐intervention survey completed in 1983, water supply improvements completed in 1985, and sanitation improvements completed in 1986 and early 1987; surveys completed to measure outcomes in 1986 and 1987) Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomized trial (not randomly assigned) |
| Allocation concealment (selection bias) | Unclear risk | Not specified who allocated the intervention to units |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing data |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | High risk | No adjustment for confounding variables |
| Baseline outcome measurements similar | Low risk | Intervention and control villages are similar in terms diarrhoea incidence rate |
| Baseline characteristics similar | Low risk | Intervention and control villages are similar in terms of age distribution, culture, SES, sanitation related factors |
| Protection against contamination | Low risk | Intervention allocated by village and it is unlikely that the control group received the intervention |
Luby 2018.
| Study characteristics | ||
| Methods | Cluster‐randomized controlled trial among 720 clusters (90 water intervention, 90 sanitation intervention, 90 handwashing intervention, 90 WASH intervention, 90 nutrition intervention, 90 WASH + nutrition intervention, 180 control villages) | |
| Participants | 5551 pregnant women allocated to an study arm with 14,425 children who were < 3 years at enrollment that had diarrhoea outcomes measured (7331 children in year 1, 7094 children in year 2) | |
| Interventions | The trial included an individual sanitation intervention arm as well as a combined WASH intervention arm with hardware improvements for sanitation, water, hygiene, and nutrition as well as education. The trial consisted of 6 separate intervention arms: sanitation, water, handwashing, WASH, nutrition, and WASH + nutrition: Sanitation: the sanitation intervention included providing households with new or upgraded household latrines, sani‐scoops (a hand tool to remove faeces from the compound), potties for children < 3 years, and behaviour change promotion. If the household had an existing latrine, latrines that did not have a slab, a functional water seal, or did not prevent surface runoff of a faecal stream into the community were replaced. If the household did not have a latrine, then a double pit latrine with a water seal was constructed. Community promoters delivered behaviour change messaging to encourage use of latrines, potty training of children, safe disposal of faeces into latrines, and encourage latrine cleanliness, maintenance and pit switching. Water: the water intervention included providing households with a 10 L water storage vessel with lid and tap, as well as a regular supply of sodium dichloroisocyanurate tablets (Aquatabs) for water treatment. All household members, and especially children < 5 years, were encouraged to drink water that had been treated and safely stored. Handwashing: the handwashing intervention included providing households with 2 handwashing stations including a basin for rinse water, a soapy water bottle, and a regular supply of detergent for making soapy water. Community promoters encouraged residents to wash their hands with soapy water before preparing food, before eating or feeding a child, after defecating, and after cleaning a child who has defected. WASH: the combined water, sanitation and handwashing intervention included all interventions from the three separate arms. Nutrition: the nutrition included providing mothers with index children aged 6 to 24 months with a regular supply of sachets of lipid‐based nutrient supplements. Promoters also encouraged caregivers to exclusively breastfeed their children during the first 6 months and then to provide a diverse, nutrient‐dense diet for children older than 6 months (in addition to the nutrient supplements provided). WASH + nutrition: the combined water, sanitation, handwashing, and nutrition intervention included all interventions from the 4 separate arms |
|
| Outcomes | Prevalence of diarrhoea for children who were in utero or < 3 years at enrollment (and therefore < 5 years at the time of outcome measurement), all‐cause mortality, and anthropomorphic outcomes for index children (who were in utero children of enrolled pregnant women). The case definition of diarrhoea used in this study was 3 or more loose stools within a 24‐hour period or at least 1 stool with blood, with a 7‐day recall period. | |
| Notes | Location: Bangladesh, rural Length of follow‐up: 12 and 24 months (primary outcomes measured at 12 months and 24 months post‐intervention implementation) Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used a computer random number generator: "Clusters were randomly allocated to treatment using a random number generator by a co‐investigator at University of California, Berkeley (BFA)." |
| Allocation concealment (selection bias) | Low risk | Allocation was performed centrally by a study investigator |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding. Diarrhoea outcome is caregiver‐reported in this study, so there is potential for courtesy bias. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Although data analysis was completed in duplicate by analyzers who were blinded to the intervention status, the data collectors for outcome assessment were not blinded as the intervention was visible |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rates and reasons were similar in control and intervention groups |
| Selective reporting (reporting bias) | Low risk | All primary outcomes reported (some papers with secondary outcomes may be forthcoming) |
| Other bias | Unclear risk | NA |
| Recruitment bias | Low risk | Participants were recruited before allocation ‐ the baseline survey occurred before randomization |
| Baseline imbalance | Low risk | Characteristics were similar for control and intervention groups at baseline and secondary analysis adjusted for baseline covariates |
| Loss of clusters | Low risk | No clusters lost |
| Incorrect analysis | Low risk | Analysis accounts for clustering |
Mcabe 1954.
| Study characteristics | ||
| Methods | Cluster non‐randomized controlled trial among 4 clusters (1 intervention, 3 control towns) | |
| Participants | 1332 individuals of all ages | |
| Interventions | Excreta disposal facilities at households were improved by constructing a new privy or rehabilitating the old privy with an 8‐foot‐deep bored hole. Privies were also remodelled at schools, churches, and commercial buildings. Informational leaflets were distributed through schools to explain the programme and a notice was stenciled on the seat lid that flies carry on sickness and should be kept out of privies. | |
| Outcomes | Diarrhoea incidence in all family members, prevalence of Shigella spp. cultures isolated from stools of children < 10 years of age, prevalence of Musca domestica flies breeding in privies (via adult fly and larvae count). The case definition of diarrhoea used in the study was not reported. | |
| Notes | Location: USA, rural Length of follow‐up: 18 months (assessments occurred monthly over the 18‐month study period) Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomized trial (not randomly assigned) |
| Allocation concealment (selection bias) | Unclear risk | Not specified who allocated the intervention to units |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Missing outcome data not specified in paper |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | High risk | No adjustment for confounding variables was conducted |
| Baseline outcome measurements similar | High risk | Baseline differences in diarrhoea not adjusted for |
| Baseline characteristics similar | Unclear risk | Characteristics are mentioned in the text as similar, but no data presented |
| Protection against contamination | Low risk | Intervention allocated by town and it is unlikely that the control group received the intervention |
Messou 1997.
| Study characteristics | ||
| Methods | Cluster non‐randomized controlled trial among 4 clusters (2 intervention, 2 control village) | |
| Participants | 1260 children < 5 years | |
| Interventions | Combined WASH intervention that included components of sanitation, water supply improvement, and health education. The sanitation intervention included the construction of latrines. Health education was provided related to prevention of diarrhoea, hygiene promotion, and oral rehydration solution use. | |
| Outcomes | Incidence of diarrhoea, deaths related to diarrhoea in children < 5 years. The case definition of diarrhoea used in the study was not reported but a recall period of 15 days was noted. | |
| Notes | Location: Côte d'Ivoire, rural Length of study: 5 years (surveys taken in 1988, 1990, and 1992, with the survey in 1988 occurring before the intervention and the surveys in 1990 and 1992 after the intervention) Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomized trial (not randomly assigned) |
| Allocation concealment (selection bias) | Unclear risk | Not specified who allocated the intervention to units |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Higher percentage of missing children in the intervention villages compared to the control in the follow‐up years |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | High risk | No adjustment for confounding variables was conducted |
| Baseline outcome measurements similar | High risk | The incidence of diarrhoea was higher in intervention villages than control villages at baseline |
| Baseline characteristics similar | Unclear risk | No baseline characteristics for access to water or sanitation facilities reported |
| Protection against contamination | Low risk | Intervention allocated by village and it is unlikely that the control group received the intervention |
Moraes 2003.
| Study characteristics | ||
| Methods | Non‐randomized controlled trial among 9 clusters (3 sewage and drainage intervention, 3 drainage only intervention, 3 control neighbourhoods) | |
| Participants | 1275 children < 5 years | |
| Interventions | Combined WASH intervention that included components of sanitation and drainage improvement. The intervention consisted of 2 intervention arms: combined sewage and drainage, and drainage only. Combined sewage and drainage: simplified sewerage system with households connections. Sewage pipes connected to covered reinforced concrete rainwater drainage channels which would connect to larger channels until discharging into the local river. Drainage only: drainage system installed in this area, which was characterized by a system of covered rainwater drainage channels made from prefabricated components of reinforced concrete that acted as footpath. Lateral openings within the drainage channels allow for the entry of surface water and sewage connections from nearby houses. The channels eventually drain into a local river. |
|
| Outcomes | Diarrhoea incidence; frequent diarrhoea incidence in children < 5 years. The case definition of diarrhoea used in the study was looser than usual stool consistency and increased frequency, as noted by mothers/guardians. A 2‐week calendar was used by mothers/guardians to reduce recall bias. Diarrhoea episodes were described as 1 or more days of diarrhoea separated from any other episode by at least 2 diarrhoea symptom‐free days. Frequent diarrhoea was described as more than twice the expected number of episodes. | |
| Notes | Location: Brazil, urban Length of follow‐up: 1 year (diarrhoea outcome information was collected over a period of 1 year; field workers interviewed the mothers every 2 weeks about each episode of diarrhoea in their children) Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomized trial (not randomly assigned) |
| Allocation concealment (selection bias) | High risk | Allocation was selected based on politico‐administrative criteria |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Missing outcome data not specified in paper |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | High risk | Only the outcome of 'frequent diarrhoea' was adjusted for in analysis. The main outcome for this review of diarrhoea incidence was not adjusted. |
| Baseline outcome measurements similar | Unclear risk | No baseline data collected |
| Baseline characteristics similar | Unclear risk | No baseline data collected |
| Protection against contamination | Low risk | Intervention allocated by village and it is unlikely that the control group received the intervention |
Null 2018.
| Study characteristics | ||
| Methods | Cluster‐randomized controlled trial among 702 clusters (77 water intervention, 77 sanitation intervention, 77 handwashing intervention, 76 WASH intervention, 78 nutrition intervention, 79 WASH + nutrition intervention, 158 active control, 80 passive control villages) | |
| Participants | 8246 households with index children (6134 children in year 1, 6494 children in year 2) | |
| Interventions | The trial included an individual sanitation intervention arm as well as a combined WASH intervention arm with hardware improvements for sanitation, water, hygiene, and nutrition as well as education. The trial consisted of 6 separate intervention arms: sanitation, water, handwashing, WASH, nutrition, and WASH + nutrition: Sanitation: the sanitation intervention included providing households with new or upgraded household latrines, sani‐scoops (a hand tool to remove faeces from the compound), potties for children < 3 years, and behaviour change promotion. If the household had an existing unimproved latrine, the latrine was upgraded to an improved latrine by installing a plastic slab. If the household did not have a latrine or the existing latrine was unlikely to last for 2 years, then an improved latrine was constructed. Community promoters delivered behaviour change messaging to encourage use of latrines and safe disposal of child and animal faeces into latrines. Water: the water intervention included the installation of chlorine dispensers at community water sources for point of collection water treatment, distribution of liquid chlorine for point of use treatment of drinking water from other sources, and behaviour change messaging to promote water treatment. Handwashing: the handwashing intervention included providing households with 2 handwashing stations with foot‐pedal‐operated jerry‐cans that dispensed a light flow of rinse water and soapy water and a regular supply of bar soap for making soapy water. Community promoters encouraged residents to wash their hands with soap before handling food, after defecating, and after cleaning a child who has defected. WASH: the combined water, sanitation, and handwashing intervention included all interventions from the three separate arms Nutrition: the nutrition included providing mothers with index children aged 6 to 24 months with a regular supply of sachets of lipid‐based nutrient supplements. Promoters also encouraged caregivers to exclusively breastfeed their children during the first 6 months and then to provide a diverse, nutrient‐dense diet for children older than 6 months (in addition to the nutrient supplements provided). WASH + nutrition: the combined water, sanitation, handwashing, and nutrition intervention included all interventions from the 4 separate arms |
|
| Outcomes | Diarrhoea prevalence at year 1 and 2 of follow‐up, all‐cause child mortality, and anthropomorphic outcomes for index children (who were in utero children of enrolled pregnant women). The case definition of diarrhoea used in this study was either 3 or more watery or soft stools in 24 hours or by a single episode of blood in the stool, with a 7‐day recall period. | |
| Notes | Location: Kenya, rural Length of follow‐up: 12 and 24 months (primary outcomes measured at 12 months and 24 months post‐intervention implementation) Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used a computer random number generator: "Clusters were randomly allocated to treatment using a random number generator with reproducible seed at the University of California, Berkeley." |
| Allocation concealment (selection bias) | Low risk | Allocation was performed centrally by a study investigator |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding. Diarrhoea outcome is caregiver‐reported in this study, so there is potential for courtesy bias. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Outcome data collectors were not blinded from the intervention allocation as the interventions were visible |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rates and reasons were similar in control and intervention groups |
| Selective reporting (reporting bias) | Low risk | All primary outcomes reported (some papers with secondary outcomes may be forthcoming) |
| Other bias | Unclear risk | NA |
| Recruitment bias | Low risk | Participants were recruited before allocation ‐ the baseline survey occurred before randomization |
| Baseline imbalance | Low risk | Characteristics were similar for control and intervention groups at baseline and secondary analysis adjusted for baseline covariates |
| Loss of clusters | Low risk | No clusters lost |
| Incorrect analysis | Low risk | Analysis accounts for clustering |
Patil 2014.
| Study characteristics | ||
| Methods | Cluster‐randomized controlled trial among 80 clusters (40 intervention, 40 control villages) | |
| Participants | 5209 children < 5 years | |
| Interventions | India's Total Sanitation Campaign (TSC). The TSC included subsidies for and promotion of improved household latrines (IHLs) that can safely confine faeces (similar to JMP defined improved sanitation facilities), school sanitation and hygiene education, Anganwadi (preschool) latrines, and community sanitation complexes. The TSC also supported rural sanitary marts and production centres to provide good‐quality but affordable material for toilet construction. Additionally, the TSC included several features such as ongoing social mobilization and behaviour change activities at state, district, and village levels, flexible technology options for toilets, and a community award given to communities that were determined to be "open defecation free" (defined as a community where all households have and use IHLs that can safely confine faeces) and meet all of the other "total sanitation" requirements defined by the Indian government. In Madhya Pradesh, Nimal Vatika (Clean House) provides additional financial/material subsidies for households. A total of 4200 rubies (2200 via TSC and 2000 via Clean House) can be provided to households below the poverty line to construct a 2‐pit latrine with water seal and a brick walled superstructure. | |
| Outcomes | Prevalence of diarrhoea in children < 5, prevalence of gastrointestinal disease in children < 5, prevalence of anaemia in children between 6 and 60 months, child stool parasitology in oldest household child between 21 and 60 months, anthropomorphic outcomes in children < 24 months, and household water quality. The case definition of diarrhoea used in the study was 3 or more loose or watery stools in 24 hours or a single stool with blood/mucus, with a 7‐day recall period. | |
| Notes | Location: India, rural Length of follow‐up: 2 years (baseline: May to July 2009; intervention installed between baseline and follow‐up surveys; follow‐up: February to April 2011) Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used a public lottery: "The randomization took place in a public lottery led by study investigators. The Block TSC coordinators or their representatives picked the lottery ticket that assigned villages to treatment groups." |
| Allocation concealment (selection bias) | Low risk | Allocation took place at a public lottery led by study investigators: "The randomization took place in a public lottery led by study investigators.The Block TSC coordinators or their representatives picked the lottery ticket that assigned villages to treatment groups." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding. Diarrhoea outcome is caregiver‐reported in this study, so there is potential for courtesy bias. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Outcome assessors not blinded: "Field interviewers were not informed of group assignment, but it was possible for them to identify intervention villages during interviews of Block officers or the village secretary." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rates and reasons were similar in control and intervention groups |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | NA |
| Recruitment bias | Low risk | Participants were recruited before allocation ‐ the baseline survey occurred before randomization |
| Baseline imbalance | Low risk | Models were adjusted for baseline characteristics |
| Loss of clusters | Low risk | No clusters lost |
| Incorrect analysis | Low risk | Standard error in model accounts for clustering: "Since we would expect behaviors and child health outcomes to be correlated within villages, all estimates used Huber‐White robust standard errors for the parameter b clustered at the village level" |
Pickering 2015.
| Study characteristics | ||
| Methods | Cluster‐randomized controlled trial among 121 clusters (60 intervention, 61 control villages) | |
| Participants | 4031 households with 6319 children < 5 | |
| Interventions | Community‐led total sanitation (CLTS) intervention to end open defecation in villages. The CLTS programme focused on mobilizing communities towards behavioural changes via emotional drivers to reduce open defecation and promote latrine construction. The programme did not provide any financial or hardware subsidies for latrine building and instead encouraged latrine designs built with local and available materials. | |
| Outcomes | Prevalence of diarrhoea, prevalence of blood in stool, prevalence of respiratory illness, and anthropomorphic outcomes in children < 5 years. Incidence of mortality in all children < 5, incidence of diarrhoea‐related mortality in all ages and children < 5 (although mortality was not a prespecified analysis). The case definition of diarrhoea used in the study was 3 or more loose or watery stools in 24 hours with 2‐day and 14‐day recall periods. | |
| Notes | Location: Mali, rural Length of follow‐up: 18 months after intervention (24 months post‐baseline) Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used a computer‐generated algorithm: "One of the study investigators (MLA) used a computer‐generated algorithm that randomly assigned villages (1:1) to treatment and control groups. " |
| Allocation concealment (selection bias) | Low risk | Allocation was performed centrally by one of the study investigators |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding. Diarrhoea outcome is caregiver‐reported in this study, so there is potential for courtesy bias |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Outcome assessors (field staff) could have inferred treatment status based on village signage |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rates and reasons were similar in control and intervention groups |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | NA |
| Recruitment bias | Low risk | Participants were recruited before allocation ‐ the baseline survey occurred before randomization |
| Baseline imbalance | Low risk | Characteristics related to age, socioeconomic status, access to water, hygiene practices, or sanitation facilities were similar for control and intervention groups at baseline. |
| Loss of clusters | Low risk | No clusters lost |
| Incorrect analysis | Low risk | Standard error in model accounts for clustering: "We estimated standard errors and confidence intervals using robust standard errors (the Huber‐White Sandwich estimator) to account for correlated outcomes at the village level." |
Pradhan 2002a.
| Study characteristics | ||
| Methods | Matched cohort study among 68 households (23 sewerage intervention, 45 control households) Pradhan 2002a refers to the intervention and results from the sewerage intervention included in this study |
|
| Participants | 68 households included in sewerage study | |
| Interventions | The sanitation intervention was conducted as part of the distribution of funds from the social fund known as Nicaraguan Emergency Social Investment Fund (fise). The social fund financed infrastructure improvements in schools, health centres, water systems, and sanitation facilities at the request of local communities. Two separate types of sanitation investments were made as part of this fund in different communities: sewerage projects for households to connect to with a flush toilet, and public access latrine facilities. | |
| Outcomes | Incidence of diarrhoea in children < 6 years, prevalence of anthropometric outcomes in children < 6 years. The case definition of diarrhoea used in the study was not reported, but a 1‐month recall period was noted. | |
| Notes | Location: Nicaragua, rural and urban Length of follow‐up: 7 years (investments occurred in infrastructure from 1991 to 1998, follow‐up survey occurred in 1998) Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomized trial (not randomly assigned) |
| Allocation concealment (selection bias) | High risk | Matched cohort study, so the researchers selected control villages by matching to villages that had previously received the intervention |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Missing outcome data not specified in paper |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | Confounding variables were not adjusted in analysis, but villages were matched to intervention or control based on propensity score matching of variables (which were collected post‐intervention), which included socioeconomic status and poverty category of the municipality as one of the matching criteria |
| Baseline outcome measurements similar | Unclear risk | No baseline data collected |
| Baseline characteristics similar | Unclear risk | No baseline data collected |
| Protection against contamination | Unclear risk | There was some potential for people living outside the intervention areas to benefit from the intervention |
Pradhan 2002b.
| Study characteristics | ||
| Methods | Matched cohort study among 677 households (226 latrines intervention, 451 control households) Pradhan 2002b refers to the intervention and results from the latrines intervention in this study |
|
| Participants | 677 households included in latrines study | |
| Interventions | The sanitation intervention was conducted as part of the distribution of funds from the social fund known as Nicaraguan Emergency Social Investment Fund (fise). The social fund financed infrastructure improvements in schools, health centres, water systems, and sanitation facilities at the request of local communities. Two separate types of sanitation investments were made as part of this fund in different communities: sewerage projects for households to connect to with a flush toilet, and public access latrine facilities. | |
| Outcomes | Incidence of diarrhoea in children < 6 years, prevalence of anthropometric outcomes in children < 6 years. The case definition of diarrhoea used in the study was not reported, but a 1‐month recall period was noted. | |
| Notes | Location: Nicaragua, rural and urban Length of follow‐up: 7 years (investments occurred in infrastructure from 1991 to 1998, follow‐up survey occurred in 1998) Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomized trial (not randomly assigned) |
| Allocation concealment (selection bias) | High risk | Matched cohort study, so the researchers selected control villages by matching to villages that had previously received the intervention |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Missing outcome data not specified in paper |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | Confounding variables were not adjusted in analysis, but villages were matched to intervention or control based on propensity score matching of variables (which were collected post‐intervention) which included socioeconomic status and poverty category of the municipality as one of the matching criteria |
| Baseline outcome measurements similar | Unclear risk | No baseline data collected |
| Baseline characteristics similar | Unclear risk | No baseline data collected |
| Protection against contamination | Unclear risk | There was some potential for people living outside the intervention areas to benefit from the intervention |
Quattrochi 2021.
| Study characteristics | ||
| Methods | Cluster‐randomized controlled trial among 121 clusters (50 intervention, 71 control clusters). Clusters included one or more villages, with 145 villages in the intervention group and 183 villages in the control group. | |
| Participants | 1312 households | |
| Interventions | Combined WASH intervention as part of a national programme known as ‘Healthy Villages & Schools’ (in French ‘Villages et Ecoles Assainis’, abbreviated VEA). The intervention was a comprehensive 9‐step programme that mobilises communities to become Healthy Villages with 3 to 6 months of support from government health officials and local NGOs, including $2000 USD of financing for new or improved water infrastructure, $2000 USD for new or improved sanitation infrastructure and $3000 for personnel costs per village. Sanitation‐related intervention activities include training for volunteers on maintenance of latrines and sanitation, community electing a village WASH committee, and the community building new infrastructure over 90 to 180 days. Key messages about sanitation and hygiene are also discussed during sensitization meetings or during visits to families by the WASH committee, community health workers or other volunteers. Staff are expected to visit the community monthly or weekly during this time, depending on the type of staff. | |
| Outcomes | Diarrhoea, fever, and cough prevalence among children 10 to 59 months old, a child health index accounting for the prevalence of all 3, school attendance, and other non‐health outcomes related to WASH. The case definition of diarrhoea used in the study was not reported but a recall period of 2 weeks was noted. | |
| Notes | Location: Democratic Republic of Congo, rural Length of follow‐up: median of 5 months after new water and sanitation infrastructure was built Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used a computer random number generator: "We used statistical software (Stata V.16) to randomise the sample into 50 treatment clusters (containing 145 treatment villages) and 71 control clusters (183 control villages)." |
| Allocation concealment (selection bias) | Low risk | Allocation was performed centrally by the research team |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding was not possible due to the nature of the intervention |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Enumerators were not informed of intervention status, but it could be inferred: "Data collectors were blinded to treatment assignment, but one module in the questionnaire covered programme participation." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rates and reasons were similar in control and intervention groups |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | NA |
| Recruitment bias | Low risk | Villages were enrolled before randomization |
| Baseline imbalance | Unclear risk | Baseline demographics were similar across all groups, but baseline levels for WASH statistics or health outcomes were not reported. |
| Loss of clusters | Low risk | 1 intervention village (2%) and 3 control villages (4%) could not be reached for the endline survey. As these are a small percentage of overall clusters and clusters were lost for similar reasons in intervention and control groups, it is unlikely that this loss would heavily influence the results. |
| Incorrect analysis | Low risk | Standard errors in model accounts for clustering: "SEs are clustered by the randomisation unit (clusters of villages)." |
Reese 2019.
| Study characteristics | ||
| Methods | Matched cohort study among 90 clusters (45 intervention, 45 control villages) | |
| Participants | 2398 households with 13,752 individuals, including 3301 children < 5 | |
| Interventions | The Movement and Action Network for the Transformation of Rural Areas (MANTRA) program, which is a combined sanitation and water supply improvement intervention. The intervention components include: 1) a household pour‐flush latrine with dual soak‐away pits; 2) an attached bathing room; and 3) household piped water connections in the latrine, bathing room, and kitchen. Households needed to construct their own toilet and bathing rooms while the programme provided the development of a piped water system. All households in a village needed to complete construction of their household latrine before the village water supply was turned on. The villages are responsible for their maintenance and operation costs. |
|
| Outcomes | Diarrhoea prevalence in children < 5 and all ages, soil‐transmitted helminth infections in children < 5 and all ages, respiratory infection prevalence in children < 5 and all ages, and anthropomorphic outcomes in children < 5 and children < 2. The case definition used for diarrhoea in this study is at least 1 occasion of 3 or more loose stools within the previous 24 hours with a 7‐day recall period. | |
| Notes | Location: India, rural Length of follow‐up: at least 5 years post‐intervention, follow‐up occurred over 4 visits with each visit every 4 months Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomized trial (not randomly assigned) |
| Allocation concealment (selection bias) | High risk | Matched cohort study, so the researchers selected control villages by matching to villages that had previously received the intervention |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing data were similar across study arms |
| Selective reporting (reporting bias) | Low risk | All primary outcomes reported (some papers with secondary outcomes may be forthcoming) |
| Other bias | Low risk | Models were adjusted for potential relevant confounders |
| Baseline outcome measurements similar | Unclear risk | Baseline outcome measurements not collected |
| Baseline characteristics similar | Low risk | Baseline characteristics are similar |
| Protection against contamination | Low risk | Intervention allocated by village and it is unlikely that the control group received the intervention |
Rubenstein 1969.
| Study characteristics | ||
| Methods | Cluster non‐randomized controlled trial among 2 clusters (1 intervention, 1 control village) | |
| Participants | 121 children < 1 year of age | |
| Interventions | Combined WASH intervention that included components of sanitation and water supply improvement. Indoor plumbing lines (piped water and sanitation) were constructed. | |
| Outcomes | Incidence of diarrhoea based on outpatient visits to the hospital for diarrhoea, outpatient visits for all causes, admissions to the hospital for diarrhoea, admissions for all causes for children < 1 year. | |
| Notes | Location: USA, rural Length of follow‐up: 1 year (first year of child’s life); included children who completed first year of life within 3 years of intervention completion Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomized trial (not randomly assigned) |
| Allocation concealment (selection bias) | High risk | Allocation of units based on villager co‐operation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing data are minimal (3 children who died in control group) and unlikely to alter the effect seen |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | High risk | No adjustment for confounding variables |
| Baseline outcome measurements similar | High risk | Baseline differences in clinic visits for diarrhoea not adjusted for |
| Baseline characteristics similar | Unclear risk | No baseline characteristics for access to water or sanitation facilities reported |
| Protection against contamination | Low risk | Intervention allocated by village and it is unlikely that the control group received the sanitation intervention |
Saha 2015.
| Study characteristics | ||
| Methods | Cluster non‐randomized controlled trial among 34 clusters (17 intervention, 17 control villages) | |
| Participants | 472 participants | |
| Interventions | The sanitation intervention was delivered as part of a health and hygiene promotion intervention targeting microfinance‐based self‐help groups (SHGs). The sanitation component of the intervention included the promotion of low‐cost sanitary latrines. Other intervention components included health education and training, home visits by a village health worker, and access to primary health care and insurance. | |
| Outcomes | Prevalence of diarrhoea in children < 2, institutional delivery of newborn babies, breastfeeding of newborn babies, prevalence of household toilets, and money spent on healthcare treatments. The case definition of diarrhoea used in the study was not reported but a 14‐day recall period was noted. | |
| Notes | Location: India, rural Length of follow‐up: 12 months Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomized trial (not randomly assigned) |
| Allocation concealment (selection bias) | Unclear risk | Not specified who allocated the intervention to units |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome data missing from only a few individuals |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | High risk | No adjustment for confounding variables |
| Baseline outcome measurements similar | Low risk | No baseline differences in outcome measurements |
| Baseline characteristics similar | High risk | There was a higher proportion of girls and students who use the latrine at home in the intervention group at baseline. This difference was not adjusted for in the analysis. |
| Protection against contamination | Unclear risk | Intervention and control schools were close to each other and it is possible that communication about the project could have occurred between students at the different schools |
Sinharoy 2017.
| Study characteristics | ||
| Methods | Cluster‐randomized controlled trial among 150 clusters (50 classic intervention, 50 lite intervention, 50 control villages). | |
| Participants | 7934 households with 10,793 children < 5 years | |
| Interventions | Combined WASH intervention that included components of sanitation, drinking water quality, hygiene, and health education. The intervention included 2 different versions of the programme: a "Classic" version and a "Lite" version. Community health clubs in villages allocated to the Lite intervention held 8 sessions on village mapping, personal hygiene, handwashing, diarrhoea, water sources, safe storage of drinking water, treatment of drinking water, and sanitation. The Classic intervention included 20 sessions, consisting of all the Lite sessions plus common diseases, skin diseases, infant care (weaning and immunization), worms and intestinal parasites, food hygiene, nutrition, food safety and food security, the model home, good parenting, respiratory disease, malaria, bilharzia (schistosomiasis), and HIV/AIDS. Sanitation messages included recommendations to not defecate in the open, to have children defecate in chamber pots, and to bury faeces if the household does not have access to a latrine. | |
| Outcomes | Prevalence of diarrhoea in children < 5, anthropomorphic outcomes in children < 5, presence of improved drinking water sources, presence of improved sanitation facilities, food security, and sanitary disposal of child’s faeces. The case definition of diarrhoea used in this study was 3 or more loose stools within a 24‐hour period, with a 7‐day recall period. | |
| Notes | Location: Rwanda, rural Length of follow‐up: 6 months after intervention implementation completed Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used a computer random number generator: "To minimise contamination, we randomly selected five complete study samples of 150 villages each, then requested that NISR map the five samples. Based on the resulting maps, we chose the one sample that minimised the number of villages with shared borders. For each of the five samples, the study team had used a simple random sampling routine in Stata to select at most two villages from large cells (≥3 villages) and one village from small cells (<3 villages). We then randomly sorted the cells and selected the villages numbered from 1 to 150 to comprise the study sample." |
| Allocation concealment (selection bias) | Low risk | Allocation was performed centrally by one of the study investigators |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding. Diarrhoea outcome is caregiver‐reported in this study, so there is potential for courtesy bias. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding of outcome assessment: "It was also not possible to mask treatment status during data collection because of the nature of the survey questions, which pertained to participation in the health clubs." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rates and reasons were similar in control and intervention groups |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | NA |
| Recruitment bias | Low risk | Participants were recruited before allocation ‐ the baseline survey occurred before randomization |
| Baseline imbalance | Low risk | Characteristics were similar for control and intervention groups at baseline |
| Loss of clusters | Low risk | No clusters lost |
| Incorrect analysis | Low risk | Model accounts for clustering: "For dichotomous outcomes at the individual level, we used log‐binomial regression with a log‐link function and generalised estimating equations (GEE) to account for village‐level clustering, then calculated the exponential of the coefficients to obtain prevalence ratios (PRs)." |
Trinies 2016.
| Study characteristics | ||
| Methods | Matched cohort study among 200 clusters (100 intervention, 100 control schools) | |
| Participants | 200 schools and 9730 pupils enrolled, 8942 pupils at follow‐up. Pupils were from grades 3 to 6. | |
| Interventions | Combined school‐based WASH intervention that included components of sanitation improvement, hygiene improvement and education, water supply improvement and WASH governance/management at the school level. Sanitation improvements include the installation or rehabilitation of latrines and other intervention activities included installing or rehabilitating water points, distributing WASH supplies, and hygiene promotion activities. | |
| Outcomes | Prevalence of diarrhoea, pupil absence, incidence of respiratory infection in pupils from grades 3 to 6. The case definition of diarrhoea used in the study was students reporting the local terminology that referred to loose stool and had also defecated 3 or more times in a day. A recall periods of 2 days and 7 days were both used in the study. | |
| Notes | Location: Mali, urban and rural Length of follow‐up: 14 months (enumerators visited each school every 6 to 8 weeks between January 2013 and May 2014, excluding the summer break from June to September 2013, for a total of 5 to 6 visits per school) Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomized trial (not randomly assigned) |
| Allocation concealment (selection bias) | High risk | Matched cohort study, so the researchers selected control schools by matching to schools that had previously received the intervention |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Exclusions and attrition of children similar across intervention and control schools |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Low risk | Models were assessed and adjusted for potential relevant confounders |
| Baseline outcome measurements similar | Unclear risk | Baseline outcome measurements not collected |
| Baseline characteristics similar | Low risk | Baseline characteristics are similar |
| Protection against contamination | Low risk | Intervention allocated by school and it is unlikely that the control group received the intervention |
Wei 1998.
| Study characteristics | ||
| Methods | Cluster non‐randomized controlled trial among 4 clusters (2 intervention, 2 control schools) | |
| Participants | Number of participants not specified | |
| Interventions | Combined WASH intervention including sanitation, water quality, and hygiene improvements in schools. The sanitation intervention included making improvements toilet facilities to improve the cleanness of the toilet and the faeces treatment, such as upgrading facilities to new flush toilets with septic tanks. Other WASH intervention components included rebuilding water heating facilities to boil water for student drinking water, building handwashing facilities, encouraging students to wash hands before eating lunch and after using toilet, and health education to promote disease prevention. | |
| Outcomes | Diarrhoea incidence in school‐age children. The case definition of diarrhoea used in the study was defined as 3 or more loose or watery tools per day but the recall period was not specified. | |
| Notes | Location: China, rural Length of study: 1 year Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomized trial (not randomly assigned) |
| Allocation concealment (selection bias) | Low risk | Allocation was performed by researchers |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Missing outcome data not specified in paper |
| Selective reporting (reporting bias) | Unclear risk | Study objective was not reported |
| Other bias | High risk | No adjustment for confounding variables |
| Baseline outcome measurements similar | High risk | Baseline differences in diarrhoea not adjusted for |
| Baseline characteristics similar | Unclear risk | No report of baseline characteristics (other than outcomes) |
| Protection against contamination | Low risk | Intervention allocated by school and it is unlikely that the control group received the intervention |
Wen 2005.
| Study characteristics | ||
| Methods | Matched cohort study among 24 clusters (12 intervention, 12 control villages) | |
| Participants | 11,586 participants | |
| Interventions | The sanitation intervention included the installation of upgraded toilet and faecal sludge management facilities. The 12 intervention villages were split between 3 different types of improved toilets: double vault funnel toilet (4 villages), 3‐grate compost toilet (4 villages), and biogas digesters (4 villages). | |
| Outcomes | Diarrhoeal incidence in all residents. The case definition of diarrhoea used in the study was defined as 3 or more loose or watery stools per day but the recall period was not specified. | |
| Notes | Location: China, rural Length of study: 1 year Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomized trial (not randomly assigned) |
| Allocation concealment (selection bias) | High risk | Matched cohort study, so the researchers selected control villages by matching to villages that had previously received the intervention |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Missing outcome data not specified in paper |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | High risk | No adjustment for confounding variables |
| Baseline outcome measurements similar | Unclear risk | Baseline measures of outcome not reported |
| Baseline characteristics similar | Unclear risk | Baseline characteristics not reported |
| Protection against contamination | Low risk | Intervention allocated by village and it is unlikely that the control group received the intervention |
Xing 2002.
| Study characteristics | ||
| Methods | Cluster non‐randomized controlled trial among 2 water intervention, 2 combined water and sanitation intervention, and unspecified number of control villages | |
| Participants | 6302 participants | |
| Interventions | Combined WASH intervention that included components of sanitation and water supply hardware improvements and education. The intervention consisted of 2 separate intervention arms: water and water + sanitation: Water + sanitation arm: the sanitation hardware intervention included installation of upgraded toilets with faecal sludge treatment. Education and promotion was also provided about personal hygiene and sanitation. The water supply was also improved as described below. Water arm: the water intervention included the installation of a sealed pressured tank that was part of a centralized water supply system. The water supply system supplied deep underground water to the households. |
|
| Outcomes | Diarrhoea incidence in all residents. The case definition and recall period used in this study was not specified. | |
| Notes | Location: China, rural Length of study: 1 year Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomized trial (not randomly assigned) |
| Allocation concealment (selection bias) | Unclear risk | Not specified who allocated the intervention to units |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Missing outcome data not specified in paper |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | High risk | No adjustment for confounding variables |
| Baseline outcome measurements similar | High risk | Baseline differences in diarrhoea not adjusted for |
| Baseline characteristics similar | Unclear risk | No report of baseline characteristics (other than outcomes) |
| Protection against contamination | Low risk | Intervention allocated by village and it is unlikely that the control group received the intervention |
Xu 1990.
| Study characteristics | ||
| Methods | Cluster non‐randomized controlled trial among 2 clusters (1 intervention, 1 control cluster) | |
| Participants | 3599 participants | |
| Interventions | The sanitation intervention included the installation of upgraded public toilets that were 3‐compartment composting toilets | |
| Outcomes | Diarrhoea incidence in all residents. Diarrhoea was clinically confirmed. | |
| Notes | Location: China, urban Length of follow‐up: 3 years Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomized trial (not randomly assigned) |
| Allocation concealment (selection bias) | Unclear risk | Not specified who allocated the intervention to units |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Missing outcome data not specified in paper |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | High risk | No adjustment for confounding variables |
| Baseline outcome measurements similar | Unclear risk | Baseline measures of outcome not reported |
| Baseline characteristics similar | Unclear risk | Baseline characteristics not reported |
| Protection against contamination | Low risk | Intervention allocated by community and it is unlikely that the control group received the intervention |
Xu 1994.
| Study characteristics | ||
| Methods | Cluster non‐randomized controlled trial among 10 clusters (5 intervention, 5 control villages) | |
| Participants | 14,787 participants | |
| Interventions | The sanitation intervention included the installation of upgraded toilet facilities in households to safely dispose of faeces. The type of sanitation facility installed varied across villages, but was either a composting double vault funnel toilet, a 3‐layer septic tank toilet, or toilets with a biogas digester. | |
| Outcomes | Diarrhoea incidence in all residents. Diarrhoea was diarrhoea was defined as either a report of 3 or more diarrhoeal stools per day or a clinic visit for diarrhoea. | |
| Notes | Location: China, rural Length of study: 4 years (intervention construction was complete at the end of 1985. The study looked at retrospective analysis of 1986 to 1988 and then collected data for prospective analysis from May to September 1989). Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomized trial (not randomly assigned) |
| Allocation concealment (selection bias) | Unclear risk | Not specified who allocated the intervention to units |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Missing outcome data not specified in paper |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | High risk | No adjustment for confounding variables |
| Baseline outcome measurements similar | Low risk | Baseline outcomes are similar |
| Baseline characteristics similar | Unclear risk | No difference in baseline SES, but no baseline characteristics for access to water or sanitation facilities reported |
| Protection against contamination | Low risk | Intervention allocated by village and it is unlikely that the control group received the intervention |
Yan 1986.
| Study characteristics | ||
| Methods | Cluster non‐randomized controlled trial among 3 clusters (2 intervention, 1 control village) | |
| Participants | 421 households with 2022 participants | |
| Interventions | The sanitation intervention included the installation of upgraded household toilet facilities that were double vault funnel toilets | |
| Outcomes | Diarrhoea incidence in all residents; fly density. Diarrhoea was defined by either a report of diarrhoea symptoms (symptoms of intestinal infectious diseases described in Infectious Diseases by Jiwu Wang) or a clinic visit for diarrhoea. | |
| Notes | Location: China, rural Length of study: 4 years (1982 baseline, 1983 follow‐up 1, 1984 follow‐up 2, 1985 endline) Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomized trial (not randomly assigned) |
| Allocation concealment (selection bias) | Low risk | Allocation was performed by researchers |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Missing outcome data not specified in paper |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | High risk | No adjustment for confounding variables |
| Baseline outcome measurements similar | Low risk | Diarrhoea prevalence at baseline similar |
| Baseline characteristics similar | Low risk | Intervention and control villages are similar in terms of age distribution, culture, SES, and sanitation‐related factors |
| Protection against contamination | Low risk | Intervention allocated by village and it is unlikely that the control group received the intervention |
Zhang 2000.
| Study characteristics | ||
| Methods | Cluster non‐randomized controlled trial among 2 clusters (1 intervention, 1 control village) | |
| Participants | 723 households with 3036 participants | |
| Interventions | Combined WASH intervention including sanitation and water supply improvements. The sanitation intervention included the installation of improved double vault funnel toilets with a cement slab in households. The water intervention included the installation of a simplified centralized water supply system which supplied deep underground water to households. | |
| Outcomes | Diarrhoea incidence in all residents, density of flies, and ascarid infection rate in pupils. Diarrhoea was defined as either a report of 3 or more diarrhoeal stools per day or a clinic visit for diarrhoea. | |
| Notes | Location: China, rural Length of follow‐up: 10 years (outcome measurements were collected 1 year, 3 years, and 10 years after the sanitation intervention) Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomized trial (not randomly assigned) |
| Allocation concealment (selection bias) | Unclear risk | Not specified who allocated the intervention to units |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing data |
| Selective reporting (reporting bias) | Unclear risk | Intended study outcomes were not reported (only stated objective as measuring long‐term effects of the intervention) |
| Other bias | High risk | No adjustment for confounding variables |
| Baseline outcome measurements similar | Low risk | Outcomes similar at baseline |
| Baseline characteristics similar | Unclear risk | Intervention and control villages were reported to have similar natural conditions, demographics, and SES factors, but no baseline characteristics for access to water or sanitation facilities reported |
| Protection against contamination | Low risk | Intervention allocated by village and it is unlikely that the control group received the intervention |
Zhou 1995.
| Study characteristics | ||
| Methods | Cluster non‐randomized controlled trial among 14 clusters (7 intervention, 7 control villages) | |
| Participants | 19,991 participants | |
| Interventions | The sanitation intervention included the installation of upgraded toilet facilities with septic tanks, supervision of households to ensure that toilets were cleaned regularly, and regular emptying of septic tanks | |
| Outcomes | Diarrhoea incidence and diarrhoeal disease (dysentery, cholera, typhoid, hepatitis A) incidence in all residents. Diarrhoea as either a report of 3 or more diarrhoeal stools per day or a clinic visit for diarrhoea. | |
| Notes | Location: China, rural Length of follow‐up: 1 year Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomized trial (not randomly assigned) |
| Allocation concealment (selection bias) | Unclear risk | Not specified who allocated the intervention to units |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Missing outcome data not specified in paper |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | High risk | No adjustment for confounding variables |
| Baseline outcome measurements similar | Low risk | Baseline outcomes similar |
| Baseline characteristics similar | Unclear risk | No difference in gender, age, education, income, but no baseline characteristics for access to water or sanitation facilities reported |
| Protection against contamination | Low risk | Intervention allocated by village and it is unlikely that the control group received the intervention |
Zhu 1997.
| Study characteristics | ||
| Methods | Cluster non‐randomized controlled trial among 20 clusters (10 intervention, 10 control schools) | |
| Participants | 3472 schoolchildren | |
| Interventions | Combined school‐based WASH intervention including sanitation, water, and hygiene improvements. The sanitation intervention included the installation of improved toilets in schools, including treatment of the faecal sludge. The specific type of toilet and treatment varied across schools, but was either a flush toilet with composting or an enclosed pit latrine. Faecal sludge from the flush toilet was composted and faecal sludge from the pit latrine was either treated with high temperatures to convert the faeces to fertilizer or treated with a chemical. The water component of the intervention included installation of water boiling facilities for water treatment in some schools. In schools that did not receive this upgrade, children to bring clean drinking water for themselves to school. The hygiene component of the intervention included the installation of handwashing facilities and providing health education. | |
| Outcomes | Diarrhoea incidence among schoolchildren. The case definition of diarrhoea used in the study was defined as self‐reported cases of 3 or more loose or watery stools per day with a daily recall period with students instructed to report when they have diarrhoea to a school registry. | |
| Notes | Location: China, rural Length of follow‐up: less than 1 year (data collected 1 May to 30 September 1995 before intervention and 1 May to 30 September 1996 after intervention, but the exact time the intervention was completed was not reported) Publication status: journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomized trial (not randomly assigned) |
| Allocation concealment (selection bias) | Unclear risk | Not specified who allocated the intervention to units |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Missing outcome data not specified in paper |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | High risk | No adjustment for confounding variables |
| Baseline outcome measurements similar | Low risk | Baseline outcomes similar |
| Baseline characteristics similar | Low risk | Baseline characteristics similar |
| Protection against contamination | Low risk | Intervention allocated by school and it is unlikely that the control group received the intervention |
CLTS: community‐led total sanitation EED: environmental enteric dysfunction JMP: Joint Monitoring Programme for Water Supply, Sanitation and Hygiene NA: not applicable NGO: non‐governmental organization SES: socioeconomic status TSC: Total Sanitation Campaign TSSM: total sanitation and sanitation marketing WASH: water, sanitation, and hygiene
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Aiga 1999 | Study design not eligible (not a RCT, quasi‐RCT, NRCT, CBA, or matched cohort study) |
| Altmann 2018 | No eligible sanitation intervention |
| Aw 2019 | No eligible study outcomes |
| Benjamin‐Chung 2018 | The study measures “spillover effects” in neighbouring communities of the sanitation intervention reported in Luby 2018 and is not eligible per the review’s definition of sanitation intervention |
| Burström 2005 | Study design not eligible (not a RCT, quasi‐RCT, NRCT, CBA, or matched cohort study) |
| Butala 2010 | Study design not eligible (not a RCT, quasi‐RCT, NRCT, CBA, or matched cohort study) |
| Dreibelbis 2014 | The study measures “spillover effects” in younger siblings of pupils of the sanitation intervention reported in Freeman 2014a and Freeman 2014b and is not eligible per the review’s definition of sanitation intervention |
| el Gaddal 1985 | Study design not eligible (not a RCT, quasi‐RCT, NRCT, CBA, or matched cohort study) |
| Ercumen 2018 | No eligible study outcomes. This paper reported environmental contamination results of the sanitation intervention reported in Luby 2018. |
| Fang 1992 | An intervention‐control comparison for the sanitation intervention is not reported |
| Garn 2016 | The study measures the effect of adherence on outcomes reported in the Freeman 2014 studies included in our review and is not a separate sanitation intervention study eligible for inclusion |
| George 2016 | No eligible sanitation intervention |
| Godfrey 2014 | No eligible study outcomes |
| Johansen 2015 | No eligible sanitation intervention |
| Kmietowicz 2014 | News article summarizing results of Clasen 2014 |
| Linquist 2014 | This study presents the results of a water filter intervention, with an arm that received WASH behaviour change communication. It was unclear from the paper if this intervention included any sanitation‐related messaging to encourage participants to increase sanitation access or improve the use of existing sanitation facilities consistent with our sanitation intervention eligibility definition. We reached out to the study authors for more information about their WASH behaviour change communication intervention, but did not receive a response, so we classified this study an ineligible because the paper included no information about an eligible sanitation intervention and reported no endline measurements related to sanitation. |
| Morse 2020 | No eligible sanitation intervention |
| Nery 2015 | No eligible study outcomes |
| Overgaard 2016 | No eligible sanitation intervention |
| Rasella 2013 | Study design not eligible (not a RCT, quasi‐RCT, NRCT, CBA, or matched cohort study) |
| Vally 2019 | Study design not eligible (not a RCT, quasi‐RCT, NRCT, CBA, or matched cohort study) |
| Walker 1999 | Study design not eligible (not a RCT, quasi‐RCT, NRCT, CBA, or matched cohort study) |
| Xiao 1997 | No eligible sanitation intervention |
CBA: controlled before‐and‐after study NRCT: non‐randomized controlled trial RCT: randomized controlled trial
Characteristics of ongoing studies [ordered by study ID]
Cha 2017.
| Study name | 'The impact of improved sanitation on the diarrhoeal reduction of under‐five children in Democratic Republic of Congo' |
| Methods | Cluster‐randomized controlled trial among 18 clusters (9 intervention, 9 control quartiers) |
| Participants | Approximately 720 children < 4 |
| Interventions | The sanitation intervention employs the approach applied in UNICEF’s “Village Assani” (Healthy Villages) programme. WASH committees in each cluster were established to promote community mobilization on latrine improvement, education regarding hygienic practices and monitoring of sanitation progress. Households were partially subsidized by the programme ($7.50 USD) to promote the construction of a latrine that had (1) a 1.5 m or more pit, (2) a superstructure with roof, (3) a cement slab, (4) a pit‐hole cover, and (5) handwashing facility. |
| Outcomes | Primary outcomes:
Secondary outcomes:
|
| Starting date | March 2015 |
| Contact information | JaeEun Lee, Korea International Cooperation Agency, Seongnam |
| Notes | Location: Idiofa Territory of the Kwilu District, DRC, urban Trial Registration Number: ISRCTN10419317 |
Dockx 2019.
| Study name | 'Software interventions for improving hand washing and sanitation in rural Tanzania: an impact evaluation' |
| Methods | Cluster‐randomized controlled trial among 3 cohorts (1 contextualized intervention, 1 non‐contextualized intervention, and 1 control cohort) |
| Participants | Approximately 1500 households |
| Interventions | Combined WASH intervention that included components of sanitation, water, and hygiene hardware and education. The intervention consisted of 2 arms: contextualized intervention and non‐contextualized intervention. Basic intervention: all arms of the intervention, as well as the control cohort, will include a basic intervention aimed at improving infrastructure. Sanitation improvements in the basic intervention include distribution of 350 pans for pour‐flush latrines, construction of sanitation blocks for schools, as well as education on how to improve latrines. Additionally, Community‐led Total Sanitation (CLTS), Sanitation and Hygiene (SWASH) clubs, and Participatory Hygiene and Sanitation Transformation (PHAST) will be used to mobilize communities to investigate their hygiene behaviours. Water and hygiene interventions include the rehabilitation/extension of gravity flow water systems, distribution of tippy taps, and education on the construction of tippy taps and creation of liquid soap. Contextualized intervention: the contextualized intervention will include 9 household visits that focus on the “Risk, Attitudes, Norms, Abilities, Self‐regulation” (RANAS) model, which focuses on the behavioural factors that are considered to drive WASH behaviour. The RANAS model will be applied to the context of the cohort’s situation. The contextualized intervention will also include all aspects of the basic intervention. Non‐contextualized intervention: the non‐contextualized intervention will also include 9 household visits that focus on the (RANAS) model. However, the intervention will apply the model as a universal WASH intervention instead of to the context of the cohort’s situation. The contextualized intervention will also include all aspects of the basic intervention. |
| Outcomes | Primary outcome:
Secondary outcomes:
|
| Starting date | May 2018 |
| Contact information | Kim Dockx, Belgian Red Cross, Mechelen |
| Notes | Location: Buhigwe District, Tanzania, rural Trial Registration Number: NCT03709368 |
NCT03594279.
| Study name | 'Community Mobilization and Incentivization for Childhood diarrhea and pneumonia (CoMIC)' |
| Methods | Cluster randomized controlled trial among approximately 42 clusters (14 arm 1 intervention, 14 arm 2 intervention, and 14 control villages) |
| Participants | Not specified |
| Interventions | Combined WASH intervention that included components of sanitation, water, and hygiene hardware and education. The intervention consisted of 2 arms. Arm 1: Arm 1 intervention will include the creation of separate male and female village committees (VC), which will be trained on prevention and management of child diarrhoea and pneumonia. Village committees will facilitate village meetings on WASH, childhood nutrition, vaccines, and management of diarrhoea and pneumonia in children. Arm 2: Arm 2 intervention will include the intervention methods in Arm 1 but will also include a community‐based incentives (cash transfers, voucher schemes, or social insurance schemes) based on the village's ability to improve child immunization, oral rehydration therapy usage, and sanitation index. |
| Outcomes | Primary outcomes:
Secondary outcome:
|
| Starting date | July 2017 |
| Contact information | Dr Jai Kumar Das, Aga Khan University, Karachi |
| Notes | Location: Tando Muhammad Khan, Pakistan, rural Trial Registration Number: NCT03594279 |
Raso 2018.
| Study name | 'An integrated approach to fight parasitic worms and diarrhoea' |
| Methods | Cluster‐randomized controlled trial among 56 clusters (14 preventative chemotherapy intervention, 14 preventative chemotherapy + community‐led total sanitation (CLTS) intervention, 14 preventative chemotherapy + community health education programme (CHEP) intervention, and 14 preventative chemotherapy + CLTS + CHEP intervention) |
| Participants | Approximately 1680 communities with approximately 8512 children |
| Interventions | Combined WASH intervention that included components of sanitation, hygiene, and preventative chemotherapy. The intervention consisted of 4 arms: preventative chemotherapy, preventative chemotherapy + community‐led total sanitation (CLTS), preventative chemotherapy + community health education programme (CHEP), preventative chemotherapy + CLTS + CHEP. Preventative chemotherapy intervention: the preventative chemotherapy intervention included giving all participants testing positive for helminths with 40 mg/kg of praziquantel (for individuals over > 4), 400 mg of albendazole for children > 2 or 200 mg of albendazole for children < 2 Preventative chemotherapy + CLTS intervention: the CLTS intervention uses facilitators with participatory tools to help community members realize health effects of open defecation. CLTS mobilizes communities towards behavioural changes, via emotional drivers, to reduce open defecation and promote latrine construction. The CLTS intervention did not provide subsidies or standard design for latrine construction. The preventative chemotherapy intervention includes the intervention above. Preventative chemotherapy + CHEP intervention: the CHEP intervention includes the formation of a community‐based health theatre group, which prepared sketches to deliver hygiene and health messages to the rest of the community. Additionally, a cartoon, Koko et les lunettes magiques, was presented to the communities to promote key health hygiene behaviours. The preventative chemotherapy intervention includes the intervention above. Preventative chemotherapy + CLTS + CHEP intervention: the combined preventative chemotherapy, CLTS, and CHEP intervention includes all interventions noted above |
| Outcomes | Primary outcome:
Secondary outcomes:
|
| Starting date | September 2014 |
| Contact information | Giovanna Raso, Swiss Tropical and Public Health Institute, Basel |
| Notes | Location: Taabo, Dejekanou and Toumodi, Cote d’Ivoire, rural Trial registration number: ISRCTN53102033 |
CHEP: community health education programme CLTS: community‐led total sanitation WASH: water, sanitation and hygiene
Differences between protocol and review
In the published protocol (Bauza 2019), we specified that we would define the second type of sanitation intervention to improve existing facilities as interventions that move participants’ access to sanitation from any sanitation facility to a higher level of service (as defined by the Joint Monitoring Programme for Water Supply, Sanitation and Hygiene (JMP) for Sustainable Development Goals (SDGs) monitoring). However, our intention when writing the protocol was to include as many sanitation intervention studies as possible in the review and it was not always possible to know details of the existing sanitation infrastructure in study areas. Therefore, we modified the definition of this type of sanitation intervention to include interventions that improve participants’ existing sanitation facilities (whether these improvements lead to a defined higher level of service or not).
We also specified that we would stratify results by sanitation‐only versus sanitation plus another WASH component in the intervention. However, for better clarity and pooling of results within the review, we decided to instead include this breakdown as a sub‐analysis within our results (Comparison 5).
Contributions of authors
TC planned the review.
VB drafted the protocol.
WY and JL developed the search strategy for Chinese studies with feedback from VB, conducted the Chinese database search, screened abstracts and full‐texts, and completed data extraction from Chinese studies.
VB supervised and checked study screening and data extraction from English and French studies completed by students listed in the Acknowledgements.
VB computed estimates of effect and entered data into RevMan 2020.
VB and FM assessed risk of bias and GRADE.
VB drafted the review.
All review authors reviewed, revised, and approved the final version of the review.
Sources of support
Internal sources
Liverpool School of Tropical Medicine, UK
External sources
-
Foreign, Commonwealth, and Development Office (FCDO), UK
Project number 300342‐104
-
National Institute of Environmental Health Sciences, USA
This research is supported in part by a grant from the National Institute of Environmental Health Sciences, USA (T32ES012870 to VB).
Declarations of interest
VB has no known conflicts of interest.
WY has no known conflicts of interest.
JL has no known conflicts of interest.
FM has no known conflicts of interest.
TC has no known conflicts of interest.
New
References
References to studies included in this review
Arnold 2010 {published data only}
- Arnold BF, Khush RS, Ramaswamy P, London AG, Rajkumar P, Ramaprabha P, et al. Causal inference methods to study nonrandomized, preexisting development interventions. Proceedings of the National Academy of Sciences of the United States of America 2010;107(52):22605-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Aziz 1990 {published data only}
- Aziz KM, Hoque BA, Hasan KZ, Patwary MY, Huttly SR, Rahaman MM, et al. Reduction in diarrhoeal diseases in children in rural Bangladesh by environmental and behavioural modifications. Transactions of the Royal Society of Tropical Medicine and Hygiene 1990;84(3):433-8. [DOI] [PubMed] [Google Scholar]
Azurin 1974 {published data only}
- Azurin JC, Alvero M. Field evaluation of environmental sanitation measures against cholera. Bulletin of the World Health Organization 1974;51(1):19-26. [PMC free article] [PubMed] [Google Scholar]
Boubacar Maïnassara 2014 {published data only}
- Boubacar Maïnassara H, Tohon Z. Assessing the health impact of the following measures in schools in Maradi (Niger): construction of latrines, clean water supply, establishment of hand washing stations, and health education. Journal of Parasitology Research 2014;2014:190451. [DOI] [PMC free article] [PubMed] [Google Scholar]
Briceno 2017 {published data only}
- Briceño B, Coville A, Gertler P, Martinez S. Are there synergies from combining hygiene and sanitation promotion campaigns: evidence from a large-scale cluster-randomized trial in rural Tanzania. PLOS One 2017;12(11):e0186228. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cameron 2013 {published data only}
- Cameron L, Shah M, Olivia S. Impact evaluation of a large-scale rural sanitation project in Indonesia. 2013. Policy Research Working Paper; No. 6360. World Bank, Washington, DC. openknowledge.worldbank.org/handle/10986/13166 (accessed 18 June 2019).
Cao 2007 {published data only}
- Cao DQ, Zhang R. Investigation of water and latrine improvement intervention of diarrhea disease control in rural areas. Zhong Guo Nong Cun Wei Sheng Shi Ye Guan Li [Chinese Rural Health Service Administration] 2007;27(6):466-7. [Google Scholar]
Cha 2021 {published data only}
- Cha S, Jung S, Bizuneh DB, Abera T, Doh YA, Seong J, et al. Effect of a community-led total sanitation intervention on the incidence and prevalence of diarrhea in children in rural Ethiopia: a cluster-randomized controlled trial. American Journal of Tropical Medicine and Hygiene 2021;105(2):532-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jung S, Doh YA, Bizuneh DB, Beyene H, Seong J, Kwon H, et al. The effects of improved sanitation on diarrheal prevalence, incidence, and duration in children under five in the SNNPR State, Ethiopia: study protocol for a randomized controlled trial. Trials 2016;17:204. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chard 2019 {published data only}
- Chard AN, Garn JV, Chang HH, Clasen T, Freeman MC. Impact of a school-based water, sanitation, and hygiene intervention on school absence, diarrhea, respiratory infection, and soil-transmitted helminths: results from the WASH HELPS cluster-randomized trial. Journal of Global Health 2019;9(2):020402. [DOI] [PMC free article] [PubMed] [Google Scholar]
Clasen 2014 {published data only}
- Clasen T, Boisson S, Routray P, Torondel B, Bell M, Cumming O, et al. Effectiveness of a rural sanitation programme on diarrhoea, soil-transmitted helminth infection, and child malnutrition in Odisha, India: a cluster-randomised trial. Lancet Global Health 2014;2(11):e645-53. [DOI] [PubMed] [Google Scholar]
Dickinson 2015 {published data only}
- Dickinson KL, Patil SR, Pattanayak SK, Poulos C, Yang JH. Nature’s call: impacts of sanitation choices in Orissa, India. Economic Development and Cultural Change 2015;64:1-29. [Google Scholar]
Freeman 2014a {published data only}
- Freeman MC, Clasen T, Dreibelbis R, Saboori S, Greene LE, Brumback B, et al. The impact of a school-based water supply and treatment, hygiene, and sanitation programme on pupil diarrhoea: a cluster-randomized trial. Epidemiology & Infection 2014;142(2):340-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Freeman 2014b {published data only}
- Freeman MC, Clasen T, Dreibelbis R, Saboori S, Greene LE, Brumback B, et al. The impact of a school-based water supply and treatment, hygiene, and sanitation programme on pupil diarrhoea: a cluster-randomized trial. Epidemiology & Infection 2014;142(2):340-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Garrett 2008 {published data only}
- Garrett V, Ogutu P, Mabonga P, Ombeki S, Mwaki A, Aluoch G, et al. Diarrhoea prevention in a high-risk rural Kenyan population through point-of-use chlorination, safe water storage, sanitation, and rainwater harvesting. Epidemiology & Infection 2008;136(11):1463-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hammer 2016 {published data only}
- Hammer J, Spears D. Village sanitation and child health: effects and external validity in a randomized field experiment in rural India. Journal of Health Economics 2016;48:135-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hashi 2017 {published data only}
- Hashi A, Kumie A, Gasana J. Hand washing with soap and WASH educational intervention reduces under-five childhood diarrhoea incidence in Jigjiga District, Eastern Ethiopia: a community-based cluster randomized controlled trial. Preventive Medicine Reports 2017;6:361-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Huda 2012 {published data only}
- Huda TM, Unicomb L, Johnston RB, Halder AK, Yushuf Sharker MA, Luby SP. Interim evaluation of a large scale sanitation, hygiene and water improvement programme on childhood diarrhea and respiratory disease in rural Bangladesh. Social Science & Medicine 2012;75(4):604-11. [DOI] [PubMed] [Google Scholar]
Humphrey 2019 {published data only}
- Humphrey JH, Mbuya MNN, Ntozini R, Moulton LH, Stoltzfus RJ, Tavengwa NV, et al. Independent and combined effects of improved water, sanitation, and hygiene, and improved complementary feeding, on child stunting and anaemia in rural Zimbabwe: a cluster-randomised trial. Lancet Global Health 2019;7(1):e132-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
Huttly 1990 {published data only}
- Huttly SR, Blum D, Kirkwood BR, Emeh RN, Okeke N, Ajala M, et al. The Imo State (Nigeria) Drinking Water Supply and Sanitation Project, 2. Impact on dracunculiasis, diarrhoea and nutritional status. Transactions of the Royal Society of Tropical Medicine and Hygiene 1990;84(2):316-21. [DOI] [PubMed] [Google Scholar]
Jin 2009 {published data only}
- Jin LJ, Zhang CY, Yang L, Zhang ZF, Sun L, Zhu HB, et al. Water supply and latrine improvement and prevention of diarrheal diseases in rural areas in Sichuan Province. Huan Jing Yu Jian Kang Za Zhi [Journal of Environmental Health] 2009;26(1):56-8. [Google Scholar]
Klasen 2012a {published data only}
- Klasen S, Lechtenfeld T, Meier K, Rieckmann J. Benefits trickling away: the health impact of extending access to piped water and sanitation in urban Yemen. Journal of Development Effectiveness 2012;4(4):537-65. [Google Scholar]
Klasen 2012b {published data only}
- Klasen S, Lechtenfeld T, Meier K, Rieckmann J. Benefits trickling away: the health impact of extending access to piped water and sanitation in urban Yemen. Journal of Development Effectiveness 2012;4(4):537-65. [Google Scholar]
Knee 2021 {published data only}
- Brown J, Cumming O, Bartram J, Cairncross S, Ensink J, Holcomb D, et al. A controlled, before-and-after trial of an urban sanitation intervention to reduce enteric infections in children: research protocol for the Maputo Sanitation (MapSan) study, Mozambique. BMJ Open 2015;5(6):e008215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knee J, Sumner T, Adriano Z, Anderson C, Bush F, Capone D, et al. Effects of an urban sanitation intervention on childhood enteric infection and diarrhea in Maputo, Mozambique: a controlled before-and-after trial. Elife 2021;10:e62278. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kolahi 2009 {published data only}
- Kolahi AA, Rastegarpour A, Sohrabi MR. The impact of an urban sewerage system on childhood diarrhoea in Tehran, Iran: a concurrent control field trial. Transactions of the Royal Society of Tropical Medicine and Hygiene 2009;103(5):500-5. [DOI] [PubMed] [Google Scholar]
Li 2009 {published data only}
- Li ZC, Liu HC, Chen J, Huang XJ. Evaluation of effect of improved latrines in rural areas of Chengdu. Ji Bing Jian Ce Yu Kong Zhi Za Zhi [Journal of Diseases Monitor and Control] 2009;3(3):135-6. [Google Scholar]
Lin 2013 {published data only}
- Lin Y, Shen ZM, Jiang WP, Zhou WL. Study on the effect of hygiene intervention measures on diarrheal diseases in the rural areas of Jiaxing City. Shi Yong Yu Fang Yi Xue [Practical Preventive Medicine] 2013;20(11):1343-5. [Google Scholar]
Lou 1989 {published data only}
- Lou H, Liu XM, Song SM, Li QM, Zhang WP, Xu GX, et al. Evaluating the effects of diarrhea disease control and associated economic benefits by intervention measure to improve environmental hygiene in rural villages. He Nan Wei Sheng Fang Yi [Henan Health and Disease Control] 1989;1:25-9. [Google Scholar]
Luby 2018 {published data only}
- Luby SP, Rahman M, Arnold BF, Unicomb L, Ashraf S, Winch PJ, et al. Effects of water quality, sanitation, handwashing, and nutritional interventions on diarrhoea and child growth in rural Bangladesh: a cluster randomised controlled trial. Lancet Global Health 2018;6(3):e302-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mcabe 1954 {published data only}
- McCabe LJ, Haines TW. Diarrheal disease control by improved human excreta disposal. Public Health Reports 1957;72(10):921-8. [PMC free article] [PubMed] [Google Scholar]
Messou 1997 {published data only}
- Messou E, Sangaré SV, Josseran R, Le Corre C, Guélain J. Effect of hygiene measures, water sanitation and oral rehydration therapy on diarrhea in children less than five years old in the south of Ivory Coast. Bulletin de la Société de Pathologie Exotique 1997;90(1):44-7. [PubMed] [Google Scholar]
Moraes 2003 {published data only}
- Moraes LR, Cancio JA, Cairncross S, Huttly S. Impact of drainage and sewerage on diarrhoea in poor urban areas in Salvador, Brazil. Transactions of the Royal Society of Tropical Medicine and Hygiene 2003;97(2):153-8. [DOI] [PubMed] [Google Scholar]
Null 2018 {published data only}
- Null C, Stewart CP, Pickering AJ, Dentz HN, Arnold BF, Arnold CD, et al. Effects of water quality, sanitation, handwashing, and nutritional interventions on diarrhoea and child growth in rural Kenya: a cluster-randomised controlled trial. Lancet Global Health 2018;6(3):e316-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
Patil 2014 {published data only}
- Patil SR, Arnold BF, Salvatore AL, Briceno B, Ganguly S, Colford JM Jr, et al. The effect of India's total sanitation campaign on defecation behaviors and child health in rural Madhya Pradesh: a cluster randomized controlled trial. PLOS Medicine 2014;11(8):e1001709. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pickering 2015 {published data only}
- Pickering AJ, Djebbari H, Lopez C, Coulibaly M, Alzua ML. Effect of a community-led sanitation intervention on child diarrhoea and child growth in rural Mali: a cluster-randomised controlled trial. Lancet Global Health 2015;3(11):e701-11. [DOI] [PubMed] [Google Scholar]
Pradhan 2002a {published data only}
- Pradhan M, Rawlings LB. The impact and targeting of social infrastructure investments: lessons from the Nicaraguan Social Fund. World Bank Economic Review 2002;16(2):275-95. [Google Scholar]
Pradhan 2002b {published data only}
- Pradhan M, Rawlings LB. The impact and targeting of social infrastructure investments: lessons from the Nicaraguan Social Fund. World Bank Economic Review 2002;16(2):275-95. [Google Scholar]
Quattrochi 2021 {published data only}
- Quattrochi JP, Coville A, Mvukiyehe E, Dohou CJ, Esu F, Cohen B, et al. Effects of a community-driven water, sanitation and hygiene intervention on water and sanitation infrastructure, access, behaviour, and governance: a cluster-randomised controlled trial in rural Democratic Republic of Congo. BMJ Global Health 2021;6(5):e005030. [DOI] [PMC free article] [PubMed] [Google Scholar]
Reese 2019 {published data only}
- Reese H, Routray P, Torondel B, Sinharoy SS, Mishra S, Freeman MC, et al. Assessing longer-term effectiveness of a combined household-level piped water and sanitation intervention on child diarrhoea, acute respiratory infection, soil-transmitted helminth infection and nutritional status: a matched cohort study in rural Odisha, India. International Journal of Epidemiology 2019;48(6):1757-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rubenstein 1969 {published data only}
- Rubenstein A, Boyle J, Odoroff CL, Kunitz SJ. Effect of improved sanitary facilities on infant diarrhea in a Hopi village. Public Health Reports 1969;84(12):1093-7. [PMC free article] [PubMed] [Google Scholar]
Saha 2015 {published data only}
- Saha S, Kermode M, Annear PL. Effect of combining a health program with a microfinance-based self-help group on health behaviors and outcomes. Public Health 2015;129(11):1510-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sinharoy 2017 {published data only}
- Sinharoy SS, Schmidt WP, Wendt R, Mfura L, Crossett E, Grépin KA, et al. Effect of community health clubs on child diarrhoea in western Rwanda: cluster-randomised controlled trial. Lancet Global Health 2017;5(7):e699-709. [DOI] [PMC free article] [PubMed] [Google Scholar]
Trinies 2016 {published data only}
- Trinies V, Garn JV, Chang HH, Freeman MC. The impact of a school-based water, sanitation, and hygiene program on absenteeism, diarrhea, and respiratory infection: a matched-control trial in Mali. American Journal of Tropical Medicine and Hygiene 2016;94(6):1418-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wei 1998 {published data only}
- Wei XN, Shao BC, Fang CH, Gao M, Zhu XL. Assessment of effects of diarrhea and roundworm disease prevention by intervention measures of school environmental hygiene in rural areas. Zhong Guo Gong Gong Wei Sheng [China Public Health] 1998;14(4):228. [Google Scholar]
Wen 2005 {published data only}
- Wen ZK, Yang Y, Wu CY. Economic and social benefit analysis of improvement of latrines in countryside of Hunan Province, China. Huang Jing Yu Jiang Kang Za Zhi [Journal of Environment and Health] 2005;22(6):445-7. [Google Scholar]
Xing 2002 {published data only}
- Xing L, Si HX, Wang JR. Investigation of diarrhea disease prevention and control. Zhi Ye Yu Jian Kang [Occupation and Health] 2002;18(8):87-8. [Google Scholar]
Xu 1990 {published data only}
- Xu JZ. Observation on the efficacy of three squares septic tank lavatory for disease prevention. Huan Jing Yu Jian Kang Za Zhi [Journal of Environment and Health] 1990;1990:250-2. [Google Scholar]
Xu 1994 {published data only}
- Xu GX, Zhu XL. The assessment of the effects for prevention of diseases by non-hazardous treatment of night soil at experimental spots in rural areas. Wei Sheng Yan Jiu [Journal of Hygiene Research] 1994;23(1):23-7. [Google Scholar]
Yan 1986 {published data only}
- Yan ZS, Wang GF, Cui C, Yin LS, Su CH, Liu F, et al. Observation of effects on diarrhea prevention and fly density reduction via double vault funnel latrines. He Nan Wei Sheng Fang Yi [Henan Health and Disease Control] 1986;3:73-6. [Google Scholar]
Zhang 2000 {published data only}
- Zhang WP, Liu MX, Yin WH, Zhang HJ, Li GF, Liu LP, et al. Evaluation of a long-term effect on improving drinking water and lavatories in rural areas for prevention of diseases. Ji Bing Kong Zhi Za Zhi [Chinese Journal of Disease Control and Prevention] 2000;4(1):76-8. [Google Scholar]
Zhou 1995 {published data only}
- Zhou YT, Wang ZS, Gu BK, Tan JD, Su ZL, Fan P-H. Evaluation and cost effectiveness analysis of strategies to manage feces and control diarrhea disease. Shang Hai Yu Fang Yi Xue [Shanghai Journal of Preventive Medicine] 1995;7(9):388-91. [Google Scholar]
Zhu 1997 {published data only}
- Zhu XL, Xia QY, Meng ZY, Wang XC, Shao BC, Yang SY, Shang Q. Assessment of effects of disease prevention by intervention measures of school environmental hygiene in rural areas. Wei Sheng Yan Jiu [Journal of Hygiene Research] 1997;26(6):378-80. [Google Scholar]
References to studies excluded from this review
Aiga 1999 {published data only}
- Aiga H, Arai Y, Marui E, Umenai T. Impact of improvement of water supply on reduction of diarrheal incidence in a squatter area of Manila. Environmental Health and Preventive Medicine 1999;4(3):111-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Altmann 2018 {published data only}
- Altmann M, Altare C, Spek N, Barbiche JC, Dodos J, Bechir M, et al. Effectiveness of a household water, sanitation and hygiene package on an outpatient program for severe acute malnutrition: a pragmatic cluster-randomized controlled trial in Chad. American Journal of Tropical Medicine and Hygiene 2018;98(4):1005-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Aw 2019 {published data only}
- Aw JY, Clarke NE, McCarthy JS, Traub RJ, Amaral S, Huque MH, et al. Giardia duodenalis infection in the context of a community-based deworming and water, sanitation and hygiene trial in Timor-Leste. Parasites & Vectors 2019;12(1):491. [DOI] [PMC free article] [PubMed] [Google Scholar]
Benjamin‐Chung 2018 {published data only}
- Benjamin-Chung J, Amin N, Ercumen A, Arnold BF, Hubbard AE, Unicomb L, et al. A randomized controlled trial to measure spillover effects of a combined water, sanitation, and handwashing intervention in rural Bangladesh. American Journal of Epidemiology 2018;187(8):1733-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
Burström 2005 {published data only}
- Burström B, Macassa G, Oberg L, Bernhardt E, Smedman L. Equitable child health interventions: the impact of improved water and sanitation on inequalities in child mortality in Stockholm, 1878 to 1925. American Journal of Public Health 2005;95(2):208-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Butala 2010 {published data only}
- Butala NM, VanRooyen MJ, Patel RB. Improved health outcomes in urban slums through infrastructure upgrading. Social Science & Medicine 2010;71(5):935-40. [DOI] [PubMed] [Google Scholar]
Dreibelbis 2014 {published data only}
- Dreibelbis R, Freeman MC, Greene LE, Saboori S, Rheingans R. The impact of school water, sanitation, and hygiene interventions on the health of younger siblings of pupils: a cluster-randomized trial in Kenya. American Journal of Public Health 2014;104(1):e91-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
el Gaddal 1985 {published data only}
- el Gaddal AA. The Blue Nile Health Project: a comprehensive approach to the prevention and control of water-associated diseases in irrigated schemes of the Sudan. Journal of Tropical Medicine and Hygiene 1985;88(2):47-56. [PubMed] [Google Scholar]
Ercumen 2018 {published data only}
- Ercumen A, Mertens A, Arnold BF, Benjamin-Chung J, Hubbard AE, Ahmed MA, et al. Effects of single and combined water, sanitation and handwashing interventions on fecal contamination in the domestic environment: a cluster-randomized controlled trial in rural Bangladesh. Environmental Science & Technology 2018;52(21):12078-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fang 1992 {published data only}
- Fang HS, Guo PH, Wang JX, Jia M. Investigation on health education and prevention of child diarrhea diseases. Zhong Guo Fu You Bao Jian [Maternal and Child Health Care of China] 1992;7(1):37-46. [Google Scholar]
Garn 2016 {published data only}
- Garn JV, Brumback BA, Drews-Botsch CD, Lash TL, Kramer MR, Freeman MC. Estimating the effect of school water, sanitation, and hygiene improvements on pupil health outcomes. Epidemiology 2016;27(5):752-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
George 2016 {published data only}
- George CM, Monira S, Sack DA, Rashid MU, Saif-Ur-Rahman KM, Mahmud T, et al. Randomized controlled trial of hospital-based hygiene and water treatment intervention (CHoBI7) to reduce cholera. Emerging Infectious Diseases 2016;22(2):233-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
Godfrey 2014 {published data only}
- Godfrey S, Van der Velden M, Muianga A, Vigh M, Gunning JW, Elbers C. Impact study of the One Million Initiative rural water and sanitation programme in Mozambique. Waterlines 2014;33(1):35-44. [Google Scholar]
Johansen 2015 {published data only}
- Johansen A, Denbæk AM, Bonnesen CT, Due P. The Hi Five study: design of a school-based randomized trial to reduce infections and improve hygiene and well-being among 6-15 year olds in Denmark. BMC Public Health 2015;15:207. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kmietowicz 2014 {published data only}
- Kmietowicz Z. More toilets in India did not improve health, finds study. BMJ 2014;349:g6169. [DOI] [PubMed] [Google Scholar]
Linquist 2014 {published data only}
- Lindquist ED, George CM, Perin J, Neiswender de Calani KJ, Norman WR, Davis TP, et al. A cluster randomized controlled trial to reduce childhood diarrhea using hollow fiber water filter and/or hygiene–sanitation educational interventions. American Journal of Tropical Medicine and Hygiene 2014;91(1):190-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Morse 2020 {published data only}
- Morse T, Tilley E, Chidziwisano K, Malolo R, Musaya J. Health outcomes of an integrated behaviour-centred water, sanitation, hygiene and food safety intervention–a randomised before and after trial. International Journal of Environmental Research and Public Health 2020;17(8):2648. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nery 2015 {published data only}
- Nery SV, McCarthy JS, Traub R, Andrews RM, Black J, Gray D, et al. A cluster-randomised controlled trial integrating a community-based water, sanitation and hygiene programme, with mass distribution of albendazole to reduce intestinal parasites in Timor-Leste: the WASH for WORMS research protocol. BMJ Open 2015;5(12):e009293. [DOI] [PMC free article] [PubMed] [Google Scholar]
Overgaard 2016 {published data only}
- Overgaard HJ, Alexander N, Matiz MI, Jaramillo JF, Olano VA, Vargas S, et al. A cluster-randomized controlled trial to reduce diarrheal disease and dengue entomological risk factors in rural primary schools in Colombia. PLOS Neglected Tropical Diseases 2016;10(11):e0005106. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rasella 2013 {published data only}
- Rasella D. Impact of the Water for All Program (PAT) on childhood morbidity and mortality from diarrhea in the Bahia State, Brazil [Impacto do Programa Água para Todos (PAT) sobre a morbi-mortalidade por diarreia em crianças do Estado da Bahia, Brasil]. Cadernos de Saude Publica 2013;29(1):40-50. [DOI] [PubMed] [Google Scholar]
Vally 2019 {published data only}
- Vally H, McMichael C, Doherty C, Li X, Guevarra G, Tobias P. The impact of a school-based water, sanitation and hygiene intervention on knowledge, practices, and diarrhoea rates in the Philippines. International Journal of Environmental Research and Public Health 2019;16(21):4056. [DOI] [PMC free article] [PubMed] [Google Scholar]
Walker 1999 {published data only}
- Walker I, Cid R, Ordoñez F, Rodríguez F. Ex-post evaluation of the Honduran social investment fund (FHIS 2). 1999. ghdx.healthdata.org/record/ex-post-evaluation-honduran-social-investment-fund-fhis-2 (accessed 21 June 2019).
Xiao 1997 {published data only}
- Xiao S, Lin C, Chen K. Evaluation of effectiveness of comprehensive control for diarrhea diseases in rural areas of east Fujian and analysis of its cost-benefit. Zhonghua Yu Fang Yi Xue Za Zhi [Chinese Journal of Preventive Medicine] 1997;31(1):40-1. [PubMed] [Google Scholar]
References to ongoing studies
Cha 2017 {published data only}
- Cha S, Lee J, Seo D, Park BM, Mansiangi P, Bernard K, et al. Effects of improved sanitation on diarrheal reduction for children under five in Idiofa, DR Congo: a cluster randomized trial. Infectious Diseases of Poverty 2017;6(1):137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ISRCTN82492848. The impact of improved sanitation on the diarrhoeal reduction of under-five children in Ethiopia. isrctn.com/ISRCTN82492848 (first received 22 January 2015).
Dockx 2019 {published data only}
- Dockx K, Van Remoortel H, De Buck E, Schelstraete C, Vanderheyden A, Lievens T, et al. Effect of contextualized versus non-contextualized interventions for improving hand washing, sanitation, and health in rural Tanzania: study design of a cluster randomized controlled trial. International Journal of Environmental Research and Public Health 2019;16(14):2529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT03709368. Software interventions for improving hand washing and sanitation in rural Tanzania: an impact evaluation [Effect of two add-on software interventions for improving hand washing and sanitation in rural Tanzania: an impact evaluation]. clinicaltrials.gov/ct2/show/NCT03709368 (first received 17 October 2018).
NCT03594279 {published data only}
- NCT03594279. Community mobilization and incentivization for childhood diarrhea and pneumonia (CoMIC) [Evaluation of a community engagement and demand creation strategy for childhood diarrhea and pneumonia in Pakistan]. clinicaltrials.gov/ct2/show/NCT03594279 (first received 20 July 2018).
Raso 2018 {published data only}
- ISRCTN53102033. An integrated approach to fight parasitic worms and diarrhoea [An integrated approach to fight neglected tropical diseases and diarrhoea]. isrctn.com/ISRCTN53102033 (first received 24 February 2014).
- Raso G, Essé C, Dongo K, Ouattara M, Zouzou F, Hürlimann E, et al. An integrated approach to control soil-transmitted helminthiasis, schistosomiasis, intestinal protozoa infection, and diarrhea: protocol for a cluster randomized trial. JMIR Research Protocols 2018;7(6):e145. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Bethony 2006
- Bethony J, Brooker S, Albonico M, Geiger SM, Loukas A, Diemert D, et al. Soil-transmitted helminth infections: ascariasis, trichuriasis, and hookworm. Lancet 2006;367(9521):1521-32. [DOI] [PubMed] [Google Scholar]
Checkley 2008
- Checkley W, Buckley G, Gilman RH, Assis AM, Guerrant RL, Morris SS, et al. Multi-country analysis of the effects of diarrhoea on childhood stunting. International Journal of Epidemiology 2008;37(4):816-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Clasen 2015
- Clasen TF, Alexander KT, Sinclair D, Boisson S, Peletz R, Chang HH, et al. Interventions to improve water quality for preventing diarrhoea. Cochrane Database of Systematic Reviews 2015, Issue 10. Art. No: CD004794. [DOI: 10.1002/14651858.CD004794.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cochrane Community 2018
- Cochrane Community. Glossary. community.cochrane.org/glossary (accessed 10 December 2018).
Cochrane EPOC 2017
- Cochrane Effective Practice and Organisation of Care. Suggested risk of bias criteria for EPOC reviews. 2017. epoc.cochrane.org/sites/epoc.cochrane.org/files/public/uploads/Resources-for-authors2017/suggested_risk_of_bias_criteria_for_epoc_reviews.pdf (accessed 10 December 2018).
Cochrane EPOC 2019
- Cochrane Effective Practice and Organisation of Care. What study designs should be included in an EPOC review and what should they be called? https://epoc.cochrane.org/sites/epoc.cochrane.org/files/public/uploads/EPOC%20Study%20Designs%20About.pdf (accessed 29 May 2019).
Ejemot‐Nwadiaro 2021
- Ejemot-Nwadiaro RI, Ehiri JE, Arikpo D, Meremikwu MM, Critchley JA. Hand washing promotion for preventing diarrhoea. Cochrane Database of Systematic Reviews 2021, Issue 1. Art. No: CD004265. [DOI: 10.1002/14651858.CD004265.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Feachem 1983
- Feachem RG, Bradley DJ, Garelick H, Mara DD. Sanitation and Disease. Health Aspects of Wastewater and Excreta Management. World Bank Studies in Water Supply and Sanitation. Vol. 3. Chichester (UK): John Wiley & Sons, 1983. [Google Scholar]
Fischer Walker 2012
- Fischer Walker CL, Perin J, Aryee MJ, Boschi-Pinto C, Black RE. Diarrhea incidence in low- and middle-income countries in 1990 and 2010: a systematic review. BMC Public Health 2012;12:220. [DOI] [PMC free article] [PubMed] [Google Scholar]
Freeman 2017
- Freeman MC, Garn JV, Sclar GD, Boisson S, Medlicott K, Alexander KT, et al. The impact of sanitation on infectious disease and nutritional status: a systematic review and meta-analysis. International Journal of Hygiene and Environmental Health 2017;220(6):928-49. [DOI] [PubMed] [Google Scholar]
GBD 2020
- GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020;396(10258):1204-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Guerrant 2012
- Guerrant RL, DeBoer MD, Moore SR, Scharf RJ, Lima AA. The impoverished gut - a triple burden of diarrhoea, stunting and chronic disease. Nature Reviews Gastroenterology & Hepatology 2012;10(4):220-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Guyatt 2011
- Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE Guidelines: 1. Introduction - GRADE evidence profiles and summary of findings tables. Journal of Clinical Epidemiology 2011;64(4):383-94. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
Humphrey 2009
- Humphrey JH. Child undernutrition, tropical enteropathy, toilets, and handwashing. Lancet 2009;374(9694):1032-5. [DOI] [PubMed] [Google Scholar]
IHME 2019
- Institute for Health Metrics and Evaluation. GBD results tool. https://vizhub.healthdata.org/gbd-results/ (accessed 24 September 2021).
Korpe 2012
- Korpe PS, Petri WA Jr. Environmental enteropathy: critical implications of a poorly understood condition. Trends in Molecular Medicine 2012;18(6):328-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kotloff 2013
- Kotloff KL, Nataro JP, Blackwelder WC, Nasrin D, Farag TH, Panchalingam S, et al. Burden and aetiology of diarrhoeal disease in infants and young children in developing countries (the Global Enteric Multicenter Study, GEMS): a prospective, case-control study. Lancet 2013;382(9888):209-22. [DOI] [PubMed] [Google Scholar]
Lefebvre 2011
- Lefebvre C, Manheimer E, Glanville J. Chapter 6: Searching for studies. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Majorin 2019
- Majorin F, Torondel B, Ka Seen Chan G, Clasen T. Interventions to improve disposal of child faeces for preventing diarrhoea and soil‐transmitted helminth infection. Cochrane Database of Systematic Reviews 2019, Issue 9. Art. No: CD011055. [DOI: 10.1002/14651858.CD011055.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Murad 2017
- Murad MH, Almasri J, Alsawas M, Farah W. Grading the quality of evidence in complex interventions: a guide for evidence-based practitioners. BMJ Evidence-Based Medicine 2017;22(1):20-2. [DOI] [PubMed] [Google Scholar]
Norman 2010
- Norman G, Pedley S, Takkouche B. Effects of sewerage on diarrhoea and enteric infections: a systematic review and meta-analysis. Lancet Infectious Diseases 2010;10(8):536-44. [DOI] [PubMed] [Google Scholar]
Penakalapati 2017
- Penakalapati G, Swarthout J, Delahoy MJ, McAliley L, Wodnik B, Levy K, et al. Exposure to animal feces and human health: a systematic review and proposed research priorities. Environmental Science and Technology 2017;51(20):11537-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pickering 2019
- Pickering AJ, Null C, Winch PJ, Mangwadu G, Arnold BF, Prendergast AJ, et al. The WASH Benefits and SHINE trials: interpretation of WASH intervention effects on linear growth and diarrhoea. Lancet Global Health 2019;7(8):e1139-46. [DOI] [PubMed] [Google Scholar]
Platts‐Mills 2015
- Platts-Mills JA, Babji S, Bodhidatta L, Gratz J, Haque R, Havt A, et al. Pathogen-specific burdens of community diarrhoea in developing countries: a multisite birth cohort study (MAL-ED). Lancet Global Health 2015;3(9):e564-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
RevMan 2020 [Computer program]
- Review Manager 5 (RevMan 5). Version 5.4. Copenhagen: The Cochrane Collaboration, 2020.
Sania 2019
- Sania A, Sudfeld CR, Danaei G, Fink G, McCoy DC, Zhu Z, et al. Early life risk factors of motor, cognitive and language development: a pooled analysis of studies from low/middle-income countries. BMJ Open 2019;9(10):e026449. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sclar 2017
- Sclar GD, Garn JV, Penakalapati G, Alexander KT, Krauss J, Freeman MC, et al. Effects of sanitation on cognitive development and school absence: a systematic review. International Journal of Hygiene and Environmental Health 2017;220(6):917-27. [DOI] [PubMed] [Google Scholar]
Stelmach 2015
- Stelmach RD, Clasen T. Household water quantity and health: a systematic review. International Journal of Environmental Research and Public Health 2015;12(6):5954-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
Troeger 2018
- Troeger C, Blacker BF, Khalil IA, Rao PC, Cao S, Zimsen SRM, et al. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of diarrhoea in 195 countries: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Infectious Diseases 2018;18(11):1211-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
Waddington 2009
- Waddington H, Snilstveit B, White H, Fewtrell L. Water, sanitation and hygiene interventions to combat childhood diarrhoea in developing countries. August 2009. Delhi: International Initiative for Impact Evaluation. 3ieimpact.org/sites/default/files/2019-01/sr1-WASH.pdf.
WHO/UNICEF 2015
- WHO/UNICEF. Progress on sanitation and drinking water – 2015 update and MDG assessment. Available at unicef.org/reports/progress-sanitation-and-drinking-water (accessed 16 August 2018).
WHO/UNICEF 2017
- WHO/UNICEF. Progress on drinking water, sanitation and hygiene: 2017 update and SDG baselines. Available at washdata.org/sites/default/files/documents/reports/2019-05/JMP-2017-report-final.pdf (accessed 16 August 2018).
WHO/UNICEF 2021
- WHO/UNICEF Joint Monitoring Programme for Water Supply, Sanitation and Hygiene. Progress on household drinking water, sanitation and hygiene 2000-2020: five years into the SDGs. 13 September 2021. Available at who.int/publications/i/item/9789240030848.
WHO 1993
- World Health Organization. The management and prevention of diarrhoea. Practical guidelines. 3rd edition. apps.who.int/iris/bitstream/handle/10665/37036/9241544546_eng.pdf?sequence=1&isAllowed=y (accessed 29 March 2018).
WHO 2017
- World Health Organization. Diarrhoeal disease fact sheet. 2 May 2017. www.who.int/mediacentre/factsheets/fs330/en/ (accessed 29 March 2018).
WHO 2020
- World Health Organization. The top 10 causes of death. who.int/mediacentre/factsheets/fs310/en/ (accessed 15 September 2021).
Wolf 2018
- Wolf J, Hunter PR, Freeman MC, Cumming O, Clasen T, Bartram J, et al. Impact of drinking water, sanitation and handwashing with soap on childhood diarrhoeal disease: updated meta‐analysis and meta‐regression. Tropical Medicine & International Health 2018;23(5):508-25. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Bauza 2019
- Bauza V, Sclar G, Majorin F, Clasen T. Interventions to improve sanitation for preventing diarrhoea. Cochrane Database of Systematic Reviews 2019, Issue 5. Art. No: CD013328. [DOI: 10.1002/14651858.CD013328] [DOI] [PMC free article] [PubMed] [Google Scholar]
Clasen 2010
- Clasen TF, Bostoen K, Schmidt WP, Boisson S, Fung IC, Jenkins MW, et al. Interventions to improve disposal of human excreta for preventing diarrhoea. Cochrane Database of Systematic Reviews 2010, Issue 6. Art. No: CD007180. [DOI: 10.1002/14651858.CD007180.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]


