Highlights
-
•
Negative urgency was significantly positively associated with negative alcohol-related consequences and coping motives for alcohol, but not past 30-day binge frequency or past 30-day alcohol quantity.
-
•
Negative urgency does not moderate the association between PTSD symptoms and alcohol outcomes.
-
•
Consistent with prior work, greater PTSD symptoms were associated with greater coping-oriented alcohol use and associated negative consequences.
Keywords: Posttraumatic stress disorder, Negative urgency, Alcohol use
Introduction
Theoretical models of trauma and alcohol use suggest that trauma-exposed individuals with higher levels of PTSD symptoms are at increased risk of problematic and coping-oriented alcohol use to alleviate unwanted internal states. The goal of the current study was to evaluate whether these associations are enhanced among young adults who report engaging in impulsive behavior in the context of negative affect (i.e., high negative urgency). It was hypothesized that (a) higher negative urgency would be associated with problematic alcohol use; and that (b) negative urgency would moderate the association between PTSD symptoms and problematic alcohol use. Methods: This study used a cross-sectional, secondary data analysis design run on 213 participants: college students, ages 18–25, who endorsed both having an interpersonal traumatic event and current weekly alcohol use. Participants completed a series of assessments and self-report questionnaires. Results: Results of hierarchical linear regression models indicated that greater negative urgency was significantly associated with greater negative alcohol-related consequences and greater coping motives for alcohol, but not past 30-day binge frequency or past 30-day alcohol quantity. Negative urgency did not moderate associations between PTSD symptoms and alcohol outcomes. Conclusions: PTSD symptoms and negative urgency are uniquely associated with indices of alcohol risk in college students with a history of trauma exposure. However, individuals high in negative urgency are not necessarily consuming more alcohol, nor does negative urgency increase the association between PTSD symptoms and drinking outcomes in this population.
1. Introduction
Heavy drinking and related consequences in college continue to be a major public health problem, and exposure to trauma can further exacerbate the likelihood of problem drinking in this population (Read et al., 2015). Trauma exposure (i.e., experienced or witnessed a dangerous, scary, threatened death, actual or threatened serious injury, or actual or threatened sexual violence; (Mccauley et al., 2012, National Institute of Mental Health, 2022), is common among college students with an estimated 59 % to 75 % of college students reporting lifetime exposure to at least one traumatic event (Read et al., 2011). Trauma-exposed college students are disproportionately at risk for heavy alcohol consumption and negative consequences from alcohol use compared to those with no trauma exposure (Anthenelli et al., 2018, Read et al., 2015). Although the rates of posttraumatic stress disorder (PTSD) among college students are equivalent to the general population (8 % to 9 %) (Mccauley et al., 2012, Read et al., 2011), college students who self-report symptoms of PTSD or have been diagnosed with higher levels of PTSD symptoms also manifest higher levels of alcohol consumption compared to college students who do not have PTSD (Read et al., 2015, Simpson et al., 2014). This finding has been attributed primarily to negative coping in response to trauma and symptoms of PTSD (Berenz et al., 2021).
Much evidence supports the role of coping-oriented drinking (i.e., alcohol use to avoid displeasing emotional states; Cooper, 1994) in the association between PTSD symptoms and alcohol use. In studies that examined relationships among coping drinking motives, alcohol use, and alcohol-related problems, coping motives were positively associated with alcohol consumption and alcohol-related problems, such that individuals with high scores for coping motives demonstrated higher levels of alcohol consumption and alcohol-related problems (Martens et al., 2008, Park and Levenson, 2002). Another study supported elevated coping motives in predicting higher PTSD symptom severity and greater alcohol consumption among individuals with a history of interpersonal trauma (Kaysen et al., 2007). In addition, a daily monitoring study supported an association between higher PTSD symptom severity and same- and next-day increases in alcohol consumption among individuals with higher levels of coping motives (Simpson et al., 2014). Similarly, college students with PTSD reported motivation to drink alcohol to decrease PTSD symptoms (Hruska and Delahanty, 2012, Simpson et al., 2012), with coping-oriented alcohol use leading to increased alcohol consumption over time (Giaconia et al., 2000, Read et al., 2014). However, it is important to note that associations between PTSD and alcohol use and problems are influenced by a number of factors (Berenz et al., 2019), and individuals with PTSD symptoms drink alcohol for many reasons (Smith & Cottler, 2018). For example, college students with PTSD are more likely to drink for motives other than coping, such as to have a good time with friends, or to enhance positive mood than those without PTSD symptoms (Radomski and Read, 2016, Simpson et al., 2014). Given that coping-oriented alcohol use is characteristic of chronic problems with alcohol (Kaysen et al., 2007), understanding which trauma-exposed individuals are most susceptible to coping-oriented drinking is important.
Individuals high in negative urgency may be particularly likely to use alcohol to alleviate negative affect. Negative urgency, a facet of impulsivity, is defined as the tendency to engage in impulsive behavior and make rash decisions in the context of intense negative emotions (Hahn et al., 2015). It may be that individuals high in negative urgency experience acute negative affect (e.g., during an intrusive trauma memory) and act on impulse to consume alcohol to reduce that negative affect. This position has some support in that negative affect has been shown to prompt emotional changes that motivate trauma-exposed students to drink more frequently and in greater quantities than their non-trauma-exposed peers (Weiss et al., 2018). In addition, studies have documented significant associations between negative urgency and coping motives for alcohol (Adams et al., 2012, Littlefield et al., 2010), providing support for the role of negative urgency and drinking in the context of negative emotions. Furthermore, recent studies have shown that coping motives mediate associations between negative urgency and drinking-related outcomes (Black et al., 2018, Brown et al., 2021, Junglen et al., 2019, Morris et al., 2020, Wardell et al., 2016). Impulsivity, defined more broadly, has evidenced associations with PTSD symptoms, alcohol consumption, and binge drinking (Bountress et al., 2017, Walker et al., 2018).
Although, several studies have examined relationships between PTSD, negative urgency, and alcohol or substance use, including two studies that have specifically tested negative urgency as a mechanism of PTSD and drinking risk, most of the studies were conducted in veterans (Black et al., 2018, Brown et al., 2021). One study examined the associations between PTSD, negative urgency, and the five factor models of personality traits with multiple alcohol consumption patterns on drinking patterns among post-deployment veterans. This study found that the associations between personality traits, PTSD, and drinking may depend on which drinking outcome is selected. For example, maximum drinks in a day were significantly associated with low agreeableness and an interaction between negative urgency and PTSD, whereas number of binge drinking days was significantly associated with extraversion, low agreeableness, and negative urgency (Brown et al., 2021). In addition, a pilot study also found a positive within-time association between PTSD symptom change and number of drinks, and these association was significantly moderated by trait impulsivity (Black et al., 2018). Although several studies have shown that individuals with PTSD develop alcohol problems to a greater degree than those with no PTSD (Kaysen et al., 2007, Smith and Cottler, 2018), not all individuals with PTSD develop an alcohol problem (Wilson et al., 2017). Our focus on characterizing individuals with PTSD who develop alcohol problem versus those who don’t is that the relationship between PTSD and alcohol risk is hypothesized to be stronger for young adults with higher negative urgency, which is characterized by impulsive behavior to alleviate acute negative affect, including alcohol use.
Given that individuals high in negative urgency are characterized by impulsive behavior to alleviate PTSD symptoms, including alcohol use, it would follow that individuals experiencing more frequent and more intense episodes of PTSD symptoms might have worse alcohol-related outcomes compared to those with less frequent or severe episodes.
The aim of the current study was to evaluate the associations among negative urgency, PTSD, and problematic alcohol use. We hypothesized that (a) higher negative urgency would be associated with greater coping motives for alcohol, greater alcohol consumption (such as past 30-day alcohol quantity and frequency of binge drinking), and more negative consequences from alcohol; and that (b) Negative urgency would moderate associations between PTSD symptoms and alcohol outcomes, such that alcohol outcomes would be more severe among those high compared to low in negative urgency (Fig. 1).
Fig. 1.
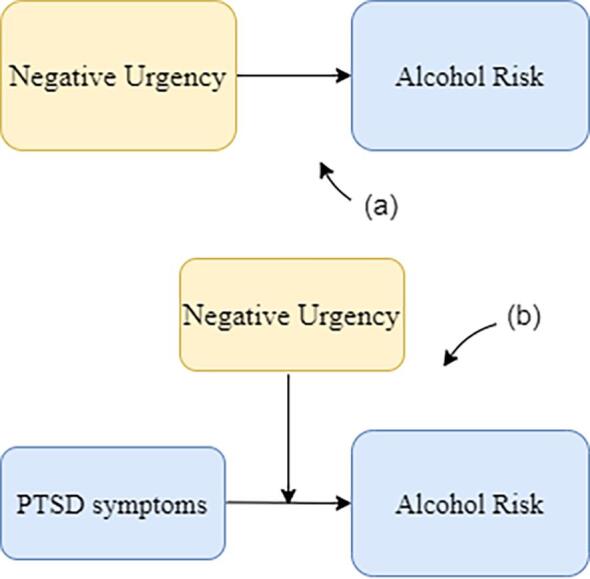
Theoretical framework of this study: Alcohol risk was defined as coping motives for alcohol, past 30-day alcohol quantity, binge drinking and negative consequences from alcohol use).
2. Method
2.1. Participants
This study utilized secondary data from a laboratory investigation of trauma and alcohol cue reactivity (Berenz et al., 2021). Participants were college students, ages 18–25, who responded to advertisements for a study on stressful life experiences and alcohol use. Participants were recruited from a mid-sized East coast university, and a mid-sized university in a large Midwest city, using flyers posted on campus and online advertisements. This study was comprised of 213 participants (50.7 % female), with an ability to consent and complete the study in English, who endorsed both a history of one or more interpersonal traumatic events (e.g., sexual or physical assault) meeting DSM-5 Criterion A for PTSD and current weekly alcohol use (i.e., alcohol use frequency ≥ 1 day/week). An initial 223 individuals were enrolled in the study following completion of the phone screen. Of these, n = 10 were excluded due to missing values on negative urgency measure. Participants completed a series of assessments and self-report questionnaires, that are described in greater detail in previous paper (Berenz et al., 2021). Only data collected as part of the assessment session were used for the present study.
2.1.1. Measures
Traumatic Life Events Questionnaire (TLEQ;Kubany et al., 2000): a 23-item self-administered measure assessing a range of potentially traumatic events (PTEs) (interpersonal and non-interpersonal, e.g., physical assault, natural disasters) reflecting current or past exposure. Each item has an initial question of whether a particular type of traumatic event was experienced by the individual, followed by a 6-point ordinal level response scale if they had, which provides 7 results (never, once, twice, 3 times, 4 times, 5 times, more than 5 times) (Kubany et al., 2000). TLEQ was used to verify interpersonal trauma exposure and index cumulative trauma history. TLEQ is a recommended measure for potentially traumatic event exposure and has demonstrated strong psychometric properties (Gray et al., 2004). The current study utilized a count of the number of lifetime trauma categories endorsed as an index of cumulative trauma.
Modified Clinician Administered PTSD scale for DSM-5 (CAPS-5;Weathers et al., 2018): a semi-structured interview assessing past 30-day PTSD symptom severity and diagnosis, using DSM-5 diagnostic criteria. Each CAPS administration was conducted by a trained Masters-level or doctoral student. CAPS interviewers underwent extensive training that was provided by the PI. Participants’ symptoms were rated on a four-point scale (0:Absent, 1:Mild/Subthreshold, 2:Moderate/Threshold, 3:Severe/Markedly Elevated, 4:Extreme/Incapacitating), based on past 30-day frequency and intensity. Participants were asked to consider symptoms related to all interpersonal potentially traumatic events they endorsed on the TLEQ when responding to questions on the CAPS-5. The current study utilized the total score on the CAPS-5 (i.e., sum of all items) as a continuous measure of PTSD symptom severity. The CAPS-5 was administered with respect to all Criterion A, interpersonal traumatic events, as opposed to one single event. A current (past-month) DSM-5 diagnosis of PTSD also was determined (0 = absent, 1 = present). The CAPS was used to assess PTSD diagnostic status using DSM-5 criteria, as well as a total PTSD symptom severity score, computed by summing the severity scores for all individual items (possible range: 0–80). The CAPS has been found to be a highly reliable and valid measure of PTSD symptom severity (Blake et al., 1995, Weathers et al., 2001), and has successfully been used in studies of college students (Borsari et al., 2018). CAPS has also demonstrated excellent psychometrics properties; excellent inter-rater reliability (alpha for symptom severity score = 0.99; range of alphas for subscales scores = 0.96 – 0.98; kappa for diagnostic status = 0.89) among college students in a primary sample from this study with 189 participants (Berenz et al., 2021).
Mini-International Neuropsychiatric Interview for DSM-5 (MINI;Sheehan et al., 1998): a semi-structured clinical interview for DSM-5 disorders assessing DSM-5 anxiety disorders, substance use disorders, psychosis and eating disorders. Participants’ responses on the MINI were used to determine their AUD diagnostic status and severity (i.e., mild, moderate, severe). MINI was administered by trained masters-level and doctoral students. Inter-rater reliability for MINI diagnoses was strong (range of kappas = 0.84–0.89) for a primary sample from this study with 189 participants. In addition, validity of MINI has been established (Sheehan et al., 1998).
Short version of UPPS-P Impulsive Behavior Scale (SUPPS-P;Cyders et al., 2014): this short version included a 20-item self-report measure assessing five facets of impulsivity; sensation seeking (i.e., “I would enjoy the sensation of skiing very fast down a high mountain slope”); lack of premeditation (i.e., “I tend to value and follow a rational, “sensible” approach to things”); lack of perseverance (i.e., “Unfinished tasks really bother me”); negative urgency (i.e., “Sometimes when I feel bad, I can’t seem to stop what I am doing even though it is making me feel worse”); and positive urgency (i.e., “When I am in great mood, I tend to get into situations that could cause me problems”). All items are rated on a four-point Likert-type scale (1-agree strongly to 4-disagree strongly). Negative urgency subscale (SUPPS-NU) was used (using a reverse scored possible range of 4–16). Given that SUPPS-NU items are reverse-coded, high levels on the NU subscale are consistent with low levels of NU. SUPPS-P has been validated and demonstrated strong reliability and validity (Cyders et al., 2014).
Timeline Follow Back (TLFB;Sobell & Sobell, 1992): a calendar drinking assessment method assessing past 30-day presence, and estimated quantity, of daily alcohol use. Variables were calculated from TLFB: alcohol use frequency (i.e., number of days of alcohol use in past 30 days), past 30-day alcohol quantity (total number of drinks in past 30 days), and past 30-day binge frequency (i.e., the number of days participants consumed 5 + standard alcohol drinks (4 + for women) in past 30 days). TLFB scores for all individual items (possible range: 0–30). TLFB has demonstrated good psychometric properties (Sobell et al., 1996).
Rutgers Alcohol Problem Inventory (RAPI;White & Labouvie, 1989): an 18-item self-administered measure assessing past 6-month problem drinking in adolescence and negative consequences associated with alcohol use (e.g., “Was told by a friend or neighbor to stop or cut down drinking”). RAPI items are rated on a 5-point Likert scale (0: None, 1: 1–2 times, 2: 3–5 times, 3: More than 5 times) and were used to assess problem drinking and negative consequences associated with alcohol use among participants. The RAPI total score (possible range 0 – 54) was utilized as an index of negative alcohol-related consequences. RAPI was successfully used to assess alcohol-use related consequences in college samples in many previous studies (Orona et al., 2016) and has demonstrated good psychometric properties (Raskin White & Labouvie, 1989).
Drinking Motives Questionnaire-Revised (DMQ-R;Cooper, 1994): a 20-item self-administered measure assessing reasons why people might be motivated to drink alcohol. A 5-point Likert-style scale indicates how frequently each listed reason motivated participants to drink alcohol and yields four subscales: Social (i.e., “Because it improves parties and celebrations”), Coping (i.e., “To forget your worries”), Enhancement (i.e., “Because you like the feeling”), and Conformity (i.e., “Because your friends pressure you to drink”). Participants rate each item with respect to how frequently they use alcohol for the stated reasons on a scale of 1–5 (1: Almost Never/Never, 2: Some of the time, 3: Half the time, 4: Most of the time, 5: Almost Always/Always). DMQ-R Coping motives subscale was used as a primary outcome measure. Strong validity and reliability have been established for DMQ-R (Cooper, 1994).
2.1.2. Procedure
A university institutional review board approved all study procedures. Individuals who responded to study advertisements completed a preliminary telephone screen that assessed inclusion and exclusion criteria. Initial eligibility was determined by using an abbreviated version of the Traumatic Life Events Questionnaire (TLEQ; Kubany et al., 2000) to assess for interpersonal traumatic exposure and typical quantity and frequency of alcohol use. Participants who met eligibility were scheduled for the baseline assessment session in the laboratory. During the baseline assessment session, participants completed informed consent procedures and provided written documentation of consent, after which they completed diagnostic interviews and questionnaires. Participants were compensated $25 for completing the baseline assessment.
2.2. Data analytic plan
The analysis was conducted using IBM-SPSS version 27. Listwise deletion was completed since there were small amounts of missing data. The distributions of study variables were examined to check for non-normal distributions. RAPI and TLFB past 30-day binge drinking and past 30-day alcohol quantity variables were transformed using square root transformation to correct non-normality. Descriptive statistics and zero-order (bivariate) correlations were examined for key study variables. A series of hierarchical linear regression models were conducted to evaluate the main and interactive effects of PTSD symptoms and negative urgency on alcohol risk. Step one: covariates of sex (1 = male, 2 = female), cumulative trauma (i.e., number of lifetime traumatic event types endorsed on TLEQ), and data collection site (0 = East coast university, 1 = university in large Midwest city) were entered. Step two: standardized main effects of CAPS total score and SUPPS-NU were entered. Step three: interaction terms (CAPS*SUPPS-NU) were entered. The criterion variables included RAPI total score, past 30-day alcohol quantity, past 30-day binge frequency, and DMQ-Coping motives. The covariates were selected a priori based on theoretical relevance. Gender was included as a covariate due to established gender differences in PTSD symptoms, alcohol use, and potentially PTSD-alcohol associations (Brown et al., 2021). Cumulative trauma was included as a covariate given prior studies demonstrating correlations between trauma exposure and negative urgency (Brown et al., 2021), to ensure that associations among PTSD symptoms, negative urgency, and alcohol use were not better explained by trauma exposure. Significant interactions were to planned to be evaluated graphically (Cohen & Cohen, 1983) and statistically. Significant interactions were planned to be evaluated by inserting specific values for each predictor variable (1 SD above and below the mean) into the regression equation associated with the described analysis (Cohen, & Cohen, 1983, pp. 323, 419). Afterwards, it was planned that a post hoc probing analysis will be conducted to examine simple slope significance at each level of the moderator (Holmbeck, 2002).
2.3. Results
2.3.1. Descriptive statistics and Zero-Order (Bivariate) correlations
Descriptive statistics for key study variables are presented in Table 1. The sample was diverse, with 50.7 % being female, 46.3 % identifying as non-white, and 15.7 % identifying as Hispanic. Additionally, 49.8 % met criteria for current (past-month) PTSD diagnosis. The most commonly endorsed PTEs included sexual assault as an adult, threatened death or serious injury and witnessing family violence growing up. Additionally, 80.3 % screened positive for AUD on MINI AUD diagnosis: 26.5 %, 22 %, and 31.8 % reported severe, moderate, and mild AUD, respectively. Zero individuals met criteria for psychosis. Comprehensive data on trauma characteristics of this sample are published elsewhere (Berenz et al., 2021).
Table 1.
Descriptive Statistics (N = 213).
| Variable | Total M (SD) or n % |
|---|---|
| Number of Lifetime Trauma Types | 6.60 (3.28) |
| Total PTSD Symptom Severity | 15.60 (11.41) |
| Past-Month PTSD Diagnosis | 111 (49.8 %) |
| Current MINI AUD Diagnosis | 179 (80.3 %) |
| Mild | 71 (31.8 %) |
| Moderate | 49 (22.0 %) |
| Severe | 59 (26.5 %) |
| Alcohol Quantity (past 30 days) | 44.91 (36.91) |
| Alcohol Use Frequency (past 30 days) | 9.97 (5.06) |
| Alcohol Binge Frequency (past 30 days) | 4.51 (4.08) |
| RAPI total score | 9.51 (8.68) |
| SUPPS-Negative Urgency | 10.85 (3.14) |
| DMQ-R coping motives | 12.54 (5.30) |
Note: Negative Urgency assessed via SUPPS-P (Short version of the UPPS-P Impulsive Behavior Scale). Past 30-day binge frequency assessed via TLFB (Timeline Follow Back). Number of lifetime trauma types assessed via TLEQ (Traumatic Life Events Questionnaire). Coping motives for alcohol assessed via DMQ-R (Drinking Motives Questionnaire-Revised). Negative consequences from alcohol use assessed via RAPI (Rutgers Alcohol Problem Inventory). Alcohol use frequency = total number of drinking days; Alcohol binge frequency = total number of binge (i.e., 5 or more drinks for men/4 or more drinks for women) drinking days. Alcohol Use Disorder (AUD) Symptoms assessed via MINI (Mini-International Neuropsychiatric Interview). Total PTSD symptom severity assessed via CAPS-5 (Modified Clinician Administered PTSD Scale for DSM-5) Total Score.
Correlations among key variables are presented in Table 2. Negative urgency was positively correlated with cumulative trauma, CAPS total score, and RAPI total score, but was not significantly correlated with past 30-day binge frequency and past 30-day alcohol quantity. Greater PTSD symptoms were associated with greater cumulative trauma and higher RAPI total score, but were not significantly correlated with past 30-day binge frequency and past 30-day alcohol quantity.
Table 2.
Zero-Order (Bivariate) Correlations.
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|
|
__ | ||||||||
|
0.19** | __ | |||||||
|
0.29** | -0.02 | __ | ||||||
|
0.08 | 0.27** | 0.51** | __ | |||||
|
0.03 | 0.07 | 0.15* | 0.31** | __ | ||||
|
0.25** | 0.02 | 0.33** | 0.41** | -0.44** | __ | |||
|
0.19** | 0.01 | 0.38** | 0.40** | -0.47** | 0.55** | __ | ||
|
0.00 | -0.10 | 0.18** | 0.06 | -0.08 | 0.19** | 0.48** | __ | |
|
0.05 | -0.20** | 0.18** | 0.08 | -0.07 | 0.18** | 0.50** | 0.92** | __ |
Note.**p <.01, *p <.05. Study site = Data collection site coded as binary (0 = a mid-sized university on the East coast, 1 = university in a large city in the Midwest). Note: Negative Urgency assessed via SUPPS-P (Short version of the UPPS-P Impulsive Behavior Scale). Past 30-day binge frequency and past 30-day Alcohol quantity assessed via TLFB (Timeline Follow Back). Number of lifetime trauma types assessed via TLEQ (Traumatic Life Events Questionnaire). Coping motives for alcohol assessed via DMQ-R (Drinking Motives Questionnaire-Revised). Negative consequences from alcohol use assessed via RAPI (Rutgers Alcohol Problem Inventory). Alcohol Use Disorder (AUD) Symptoms assessed via MINI (Mini-International Neuropsychiatric Interview). Total PTSD symptom severity assessed via CAPS-5 (Modified Clinician Administered PTSD Scale for DSM-5) Total Score.
2.3.2. PTSD symptoms, negative urgency, and alcohol risk
The first model examined relationships between PTSD, negative urgency, and past 30-day alcohol quantity. See Table 3 for regression output. The model accounted for 6.7 % of variance in past 30-day alcohol quantity total score (F(6,212) = 2.457, p =.026). Step one accounted for a significant 6.3 % of variance, with TLEQ positively associated with past 30-day alcohol quantity. Step two accounted for a non-significant 0.3% of variance, with the main effect of PTSD symptoms and negative urgency not significantly associated with past 30-day alcohol quantity. The interaction term at step three accounted for a non-significant 0.1% of variance.
Table 3.
Associations Among Posttraumatic Stress Disorder (PTSD) Symptoms, negative urgency and alcohol risks.
| ΔR2 | t | β | sr2 | p | |
|---|---|---|---|---|---|
| Criterion variable: Past 30-day Alcohol quantity | |||||
| Level 1 | 0.063 | 0.004 | |||
| Sex | −2.638 | −0.180 | 0.031 | 0.009 | |
| Number of Lifetime PTEs | 2.512 | 0.175 | 0.028 | 0.013 | |
| Data Collection Site | −0.081 | −0.006 | 0.000 | 0.936 | |
| Level 2 | 0.003 | 0.711 | |||
| CAPS-5 | 0.199 | 0.017 | 0.000 | 0.842 | |
| Negative Urgency | 0.602 | 0.044 | 0.002 | 0.548 | |
| Level 3 | 0.001 | 0.637 | |||
| Interaction term | −0.472 | −0.033 | 0.001 | 0.637 | |
| Criterion variable: Past 30-day binge frequency | |||||
| Level 1 | 0.027 | 0.123 | |||
| Sex | −0.626 | −0.044 | 0.001 | 0.532 | |
| Number of Lifetime PTEs | 2.305 | 0.164 | 0.024 | 0.022 | |
| Data Collection Site | −1.276 | −0.094 | 0.007 | 0.204 | |
| Level 2 | 0.004 | 0.652 | |||
| CAPS-5 | −0.899 | −0.079 | 0.003 | 0.370 | |
| Negative Urgency | 0.448 | 0.032 | 0.000 | 0.655 | |
| Level 3 | 0.000 | 0.773 | |||
| Interaction term | 0.289 | 0.021 | 0.000 | 0.773 | |
| Criterion variable: Negative consequences from alcohol use | |||||
| Level 1 | 0.144 | < 0.001 | |||
| Sex | 0.613 | 0.042 | 0.001 | 0.541 | |
| Number of Lifetime PTEs | 4.915 | 0.338 | 0.105 | < 0.001 | |
| Data Collection Site | 1.466 | 0.104 | 0.009 | 0.144 | |
| Level 2 | 0.217 | < 0.001 | |||
| CAPS-5 | 2.488 | 0.184 | 0.020 | 0.014 | |
| Negative Urgency | 6.807 | 0.412 | 0.152 | < 0.001 | |
| Level 3 | 0.001 | 0.652 | |||
| Interaction term | 0.451 | 0.027 | 0.000 | 0.652 | |
| Criterion variable: Coping motives for alcohol | |||||
| Level 1 | 0.148 | < 0.001 | |||
| Sex | 0.848 | 0.055 | 0.002 | 0.398 | |
| Number of Lifetime PTEs | 4.457 | 0.296 | 0.081 | < 0.001 | |
| Data Collection Site | 2.693 | 0.182 | 0.029 | 0.008 | |
| Level 2 | 0.181 | < 0.001 | |||
| CAPS-5 | 3.348 | 0.244 | 0.036 | < 0.001 | |
| Negative Urgency | 5.489 | 0.331 | 0.098 | < 0.001 | |
| Level 3 | 0.000 | 0.995 | |||
| Interaction term | −0.007 | 0.000 | 0.000 | 0.995 | |
Note: Negative Urgency = SUPPS-P (Short version of the UPPS-P Impulsive Behavior Scale). Number of lifetime PTE’s = (Traumatic Life Events Questionnaire). CAPS-5 = (Modified Clinician Administered PTSD Scale for DSM-5) for PTSD symptom severity.
The second model examined relationships between PTSD, negative urgency, and 30-day binge frequency. The model accounted for 3.2 % of variance in past 30-day binge frequency (F(6,210) = 1.119, p =.352). Step one accounted for a significant 2.7 % of variance, with TLEQ positively associated with past 30-day binge frequency. Step two accounted for a non-significant 0.4% of variance, with the main effect of PTSD symptoms and negative urgency not significantly associated with past 30-day binge frequency. The interaction term at step three accounted for a non-significant 0.0% of variance.
The third model examined relationships between PTSD, negative urgency, and RAPI total score. The model accounted for 36.1 % of variance in RAPI total score (F(6,199) = 18.200, p <.001). Step one accounted for a significant 14.4 % of variance, with TLEQ positively associated with RAPI total score. Step two accounted for a significant 21.7 % of variance, with the main effect of PTSD symptoms and negative urgency being significantly associated with negative consequences from alcohol use. The interaction term at step three accounted for a non-significant 0.1% of variance.
The fourth model examined relationships between PTSD, negative urgency, and DMQ-R coping motives subscale. The model accounted for 32.9 % of variance DMQ-R coping motives subscale (F(6,210) = 16.690, p <.001). Step one accounted for a significant 14.8 % of variance, with TLEQ positively associated with DMQ-R coping motives subscale. Step two accounted for a significant 18.1 % of variance, with the main effects of PTSD symptoms and negative urgency being significantly associated with coping motives for alcohol. The interaction term at step three accounted for a non-significant 0.0% of variance.
2.4. Discussion
This study’s aim was to evaluate the associations among negative urgency, PTSD, and problematic alcohol use among college-aged drinkers. Higher levels of negative urgency were significantly associated with greater coping motives for alcohol and greater negative alcohol-related consequences, even after accounting for the effects of both theoretically relevant covariates and PTSD symptoms. These findings are consistent with prior literature (Cyders et al., 2009, Shishido et al., 2013). Contrary to expectations, negative urgency was not associated with past 30-day binge frequency or past 30-day alcohol quantity. These findings differed from prior studies - finding negative urgency as a significant predictor of college-aged alcohol consumption and binge drinking (Bø et al., 2016, Shishido et al., 2013). Taken together, negative urgency may be more relevant to reasons for drinking and drinking-related consequences, compared to levels of alcohol use in college students with a history of interpersonal trauma. Negative urgency may not influence the amount of alcohol consumed, or recent drinking patterns that characterize the binge drinking per se. Interventions geared towards decreasing impulsivity in the context of negative affect among college-aged drinkers may buffer against coping-oriented use and related consequences.
The differences in findings concerning the role of negative urgency may be due to one, or more factors, including: (1) this study’s focus on individuals with PTSD; (2) the Shishido study’s focus on individuals with alexithymia; (3) the Bø study’s focus on college students in Norway; (4) differences in measures of binge drinking and measure of drinks between studies; and (5) different look back periods, specifically past 30-day consumption, past 3-month consumption, and past year-consumption (Bo et al., 2016, Shishido et al., 2013). College students in Norway allegedly differ, as US college students allegedly tend to be younger and have been subject to a legal minimum age for alcohol consumption. Therefore, it is surmised, US college students are likely newer to experiencing adulthood, significant freedom from parental control, and unrestrained alcohol consumption. With respect to the different periods each study considered, US colleges tend to have quizzes, tests, and/or papers throughout the semester and, it is surmised that, this study’s significantly shorter past 30-day consumption period is more likely to be significantly skewed if participants experienced significant grading events during this shorter period, or perhaps otherwise, by the participant being more likely to recall specific time periods where a participant avoided drinking significantly.
Contrary to our hypotheses, negative urgency did not moderate the association between PTSD symptoms and alcohol variables. The main effects of PTSD symptoms and negative urgency may be more useful to current models of problematic alcohol use in trauma-exposed college-aged drinkers. Specifically, PTSD and negative urgency may have an additive rather than an interactive effect on coping motives for alcohol and negative consequences but not on past 30-day binge frequency and past 30-day alcohol quantity. Early detection of elevated impulsivity, specifically negative urgency, may help identify at-risk college-aged drinkers and help evaluate interventions to decrease impulsive behavior to reduce or prevent alcohol misuse (Ralph-Nearman et al., 2020). Empirically supported treatments for PTSD (e.g., exposure-based interventions, cognitive processing therapy) might be helpful to reduce PTSD symptoms and help reduce or prevent alcohol misuse in this population (Foa, et al., 2007). We believe that interventions geared towards simultaneously treating PTSD symptoms (exposure therapy) (Rothbaum & Schwartz, 2002), and decreasing impulsive decision making (e.g., emotion modulation intervention) (Weiss et al., 2015), may have a greater impact on college-aged drinkers because it should decrease instances where an untreated issue may contribute to a bout of problem drinking, thereby decreasing instances of what might be viewed as a “failure,” while simultaneously encouraging the problem drinker by having a greater amount of what might be viewed as “success.”.
In addition, there was positive association between number of traumatic events and alcohol variables. These findings are consistent with prior studies- demonstrating the relationship between PSTD and AUD (Anthenelli et al., 2018, Chilcoat and Menard, 2004). Individuals with past traumatic events may drink alcohol to deal with anxiety or depression associated with the past traumatic event. Further, the self-medication model suggests that an individual with PTSD is more susceptible to AUD and may use alcohol to cope with a trauma-related experience (Bountress et al., 2019). In addition, AUD may play a causal role in the development of PTSD. Drinking increases the risk for trauma exposure, such as sexual assault or date rape, and alcohol-related unintentional injuries, including motor-vehicle crashes (Hingson et al., 2005, Hingson et al., 2009).
These findings should be interpreted in the context of several study limitations. This study used a college-aged sample where the inclusion criteria recruited the highest severity assault trauma types and frequent alcohol use; therefore, the study findings may not generalize to treatment-seeking populations, other age cohorts, or populations with non-assaultive trauma exposures (e.g., combat veterans or accidental trauma survivors). Future studies could replicate this study’s aims in diverse samples to support generalizability. Additionally, this study used cross-sectional data; thus, a causal direction for these associations cannot be determined. Future research would benefit from longitudinal designs to examine the timing of negative urgency, PTSD onset, subsequent alcohol use patterns, and problematic alcohol use risk. Furthermore, this study participants included young adults, and studies have demonstrated that this age-group have elevated risk for the onset of PTSD and AUD (Kessler et al., 2005, O’Malley and Johnston, 2002, Overstreet et al., 2017); and the inclusion criteria recruited the highest severity trauma types and frequent alcohol use, so the findings of this study may not generalize to individuals who have been suffering from long-standing symptoms of PTSD-AUD or other age-groups. Further, although, inter-rater reliability was not computed for the current sample used in this secondary analysis, the primary paper of this study showed acceptable inter-rater reliability.
Interestingly, even though negative urgency was negatively correlated with RAPI and coping motives in the bivariate correlations, after adjusting for covariates of sex, cumulative trauma, and data collection site in step 1, CAPS total score in step two of regression models led to a suppression effect, hence, negative urgency was positively correlated with RAPI and coping motives (positive betas) in the regression. In addition, negative urgency was significantly positively correlated with cumulative trauma, CAPS total score in the bivariate correlation, which may have changed the directions in the regression models leading to negative urgency being positively correlated with RAPI and coping motives in the regression. Finally, although self-report measures used in this study are well validated, future studies would benefit from including objective drinking behavior measures (e.g., wearable sensors).
Our results extend prior findings in important ways and yield important clinical implications. Although previous studies examined impulsivity-related traits and behaviors among young adults and college students (Moore et al., 2017), this study, to our knowledge, is the first investigation of whether negative urgency moderates an association between PTSD symptoms and alcohol variables among this population. Furthermore, our study sample has a unique characteristic: 80.3 % of the sample was found to meet criteria for an alcohol use disorder and all participants had to have experienced at least 1 interpersonal trauma. Individuals who have not recovered from trauma experiences (i.e., those with PTSD) are at a greater risk for experiencing elevated negative affect in response to trauma reminders. Recent studies (Dugal et al., 2020, Dugal et al., 2021) have found that negative urgency may predispose individuals to experience interpersonal trauma, suggesting negative urgency may be higher among individuals with this type of trauma. It is likely that negative urgency which is characterized by impulsive behavior to alleviate acute negative affect, including alcohol use, might be more severe among college students who have not recovered from trauma experiences. Finally, the rates of PTSD and AUD are high in our current study because of the inclusion criteria (i.e., recruiting the highest severity trauma types and frequent alcohol use). Most college student studies published do not recruit on these characteristics.
2.4.1. Conclusion
This study supports the hypothesis that the main effect of negative urgency was significantly related to coping motives for alcohol and negative consequences from alcohol use, above and beyond the effects of PTSD symptoms. Early detection and treatment of PTSD and impulsive traits, such as negative urgency, may reduce risk for alcohol misuse in college-aged young adults.
Author Agreement: This is to certify that all authors have read and approved the manuscript for submission to Addictive Behaviors Reports. None of the original material contained in the manuscript has been submitted for consideration nor will any of it be published elsewhere except in abstract form in connection with scientific meetings.
Funding: This research was supported by a National Institute on Alcohol Abuse and Alcoholism (NIAAA) grant awarded to Erin Berenz (R00AA022385), and by a NIAAA T32 training grant supporting Hagar Hallihan and Hanaan Bing-Canar (T32AA026577).
CRediT authorship contribution statement
Hagar Hallihan: Writing – original draft, Writing – review & editing. Hanaan Bing-Canar: Data curation, reviewing and editing. Katherine Paltell: Software, Data curation, Formal analysis. Erin C. Berenz: Conceptualization, Methodology, Funding acquisition, Writing – review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Data availability
Data will be made available on request.
References
- Adams Z.W., Kaiser A.J., Lynam D.R., Charnigo R.J., Milich R. Drinking motives as mediators of the impulsivity-substance use relation: Pathways for negative urgency, lack of premeditation, and sensation seeking. Addictive Behaviors. 2012;37(7):848–855. doi: 10.1016/J.ADDBEH.2012.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anthenelli, R. M., Brady, K. T., Grandison, L., & Roach, D. (2018). Co-Occurring Alcohol Use Disorder and Post-Traumatic Stress Disorder. Alcohol Research : Current Reviews, 39(2), 111. /pmc/articles/PMC6561396/. [PMC free article] [PubMed]
- Berenz E.C., Edalatian Zakeri S., Demos A.P., Paltell K.C., Bing-Canar H., Kevorkian S., Ranney R. Negative affect and alcohol craving in trauma-exposed young adult drinkers. Alcoholism: Clinical and Experimental Research. 2021;45(7):1479–1493. doi: 10.1111/ACER.14641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berenz E.C., McNett S., Paltell K. Development of Comorbid PTSD and Substance Use Disorders. Posttraumatic Stress and Substance Use Disorders. 2019;11–27 doi: 10.4324/9781315442648-2. [DOI] [Google Scholar]
- Black A.C., Cooney N.L., Sartor C.E., Arias A.J., Rosen M.I. Impulsivity interacts with momentary PTSD symptom worsening to predict alcohol use in male veterans. American Journal of Drug and Alcohol Abuse. 2018;44(5):524–531. doi: 10.1080/00952990.2018.1454935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blake D.D., Weathers F.W., Nagy L.M., Kaloupek D.G., Gusman F.D., Charney D.S., Keane T.M. The development of a Clinician-Administered PTSD Scale. Journal of Traumatic Stress. 1995;8(1):75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- Bo L., Lehr D., Reis D., Vis C., Riper H., Berking M., Ebert D.D. Reliability and validity of assessing user satisfaction with web-based health interventions. Journal of Medical Internet Research. 2016;18(8) doi: 10.2196/jmir.5952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bø R., Billieux J., Landrø N.I. Which facets of impulsivity predict binge drinking? Addictive Behaviors Reports. 2016;3:43–47. doi: 10.1016/J.ABREP.2016.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsari B., Yalch M.M., Pedrelli P., Radomski S., Bachrach R.L., Read J.P. Associations among trauma, depression, and alcohol use profiles and treatment motivation and engagement in college students. Journal of American College Health : J of ACH. 2018;66(7):644–654. doi: 10.1080/07448481.2018.1446438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bountress K., Adams Z.W., Gilmore A.K., Amstadter A.B., Thomas S., Danielson C.K. Associations among Impulsivity, Trauma History, and Alcohol Misuse within a Young Adult Sample. Addictive Behaviors. 2017;64:179. doi: 10.1016/J.ADDBEH.2016.08.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bountress K.E., Cusack S.E., Sheerin C.M., Hawn S., Dick D.M., Kendler K.S., Amstadter A.B. Alcohol consumption, interpersonal trauma, and drinking to cope with trauma-related distress: An auto-regressive, cross-lagged model. Psychology of Addictive Behaviors. 2019;33(3):221–231. doi: 10.1037/ADB0000457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown R.C., Mortensen J., Hawn S.E., Bountress K., Chowdhury N., Kevorkian S.…Amstadter A.B. Drinking Patterns of Post-Deployment Veterans: The Role of Personality, Negative Urgency, and Posttraumatic Stress. Military Psychology : The Official Journal of the Division of Military Psychology, American Psychological Association. 2021;33(4):240. doi: 10.1080/08995605.2021.1902183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chilcoat H.D., Menard C. Epidemiological investigations: Comorbidity of posttraumatic stress disorder and substance use disorder. Trauma and Substance Abuse: Causes, Consequences, and Treatment of Comorbid Disorders. 2004;9–28 doi: 10.1037/10460-001. [DOI] [Google Scholar]
- Cohen, J., & Cohen, P. (1983). Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences. Hillsdale, NJ Erlbaum. - References - Scientific Research Publishing. (n.d.). Retrieved May 4, 2022, from https://www.scirp.org/(S(lz5mqp453edsnp55rrgjct55))/reference/ReferencesPapers.aspx?ReferenceID=1550601.
- Cooper M.L. Motivations for alcohol use among adolescents: Development and validation of a four-factor model. Psychological Assessment. 1994;6(2):117–128. doi: 10.1037/1040-3590.6.2.117. [DOI] [Google Scholar]
- Cyders M.A., Flory K., Rainer S., Smith G.T. The role of personality dispositions to risky behavior in predicting first-year college drinking. Addiction (Abingdon, England) 2009;104(2):193–202. doi: 10.1111/J.1360-0443.2008.02434.X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cyders M.A., Littlefield A.K., Coffey S., Karyadi K.A. Examination of a short English version of the UPPS-P Impulsive Behavior Scale. Addictive Behaviors. 2014;39(9):1372–1376. doi: 10.1016/J.ADDBEH.2014.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dugal C., Bélanger C., Brassard A., Godbout N. A Dyadic Analysis of the Associations Between Cumulative Childhood Trauma and Psychological Intimate Partner Violence: The Mediating Roles of Negative Urgency and Communication Patterns. Journal of Marital and Family Therapy. 2020;46(2):337–351. doi: 10.1111/JMFT.12414. [DOI] [PubMed] [Google Scholar]
- Dugal, C., Girard , M., Bélanger, C., Sabourin, S., Bates, E.A., & Godbout, N. (2021). Psychological Intimate Partner Violence and Childhood Cumulative Trauma: The Mediating Role of Affect Dysregulation, Maladaptive Personality Traits an d Negative Urgency. 10.1177/0886260518801022, 36 (11 –12), 5101 –5121. 10.1177/ 0886260518801022. [DOI] [PubMed]
- Foa E.B., Hembree E.A., Rothbaum B.O. Oxford University Press; New York, NY: 2007. Prolonged exposure therapy for PTSD: Emotional processing of traumatic experiences – Therapist guide. – GeroCentral. (n.d.). Retrieved May 4, 2022, from. [Google Scholar]
- Giaconia R.M., Reinherz H.Z., Hauf A.C., Paradis A.D., Wasserman M.S., Langhammer D.M. Comorbidity of substance use and post-traumatic stress disorders in a community sample of adolescents. American Journal of Orthopsychiatry. 2000;70(2):253–262. doi: 10.1037/H0087634. [DOI] [PubMed] [Google Scholar]
- Gray M.J., Litz B.T., Hsu J.L., Lombardo T.W. Psychometric properties of the life events checklist. Assessment. 2004;11(4):330–341. doi: 10.1177/1073191104269954. [DOI] [PubMed] [Google Scholar]
- Hahn A.M., Tirabassi C.K., Simons R.M., Simons J.S. Military sexual trauma, combat exposure, and negative urgency as independent predictors of PTSD and subsequent alcohol problems among OEF/OIF veterans. Psychological Services. 2015;12(4):378–383. doi: 10.1037/SER0000060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hingson, R., Heeren, T., Winter, M., & Wechsler, H. (2005). Magnitude of alcohol-related mortality and morbidity among U.S. college students ages 18-24: Changes from 1998 to 2001. In Annual Review of Public Health (Vol. 26, pp. 259–279). Annu Rev Public Health. 10.1146/annurev.publhealth.26.021304.144652. [DOI] [PubMed]
- Hingson, R. W., Zha, W., & Weitzman, E. R. (2009). Magnitude of and Trends in Alcohol-Related Mortality and Morbidity Among U.S. College Students Ages 18-24, 1998-2005. Journal of Studies on Alcohol and Drugs. Supplement, 16(16), 12. 10.15288/JSADS.2009.S16.12. [DOI] [PMC free article] [PubMed]
- Holmbeck G.N. Post-hoc probing of significant moderational and mediational effects in studies of pediatric populations. Journal of Pediatric Psychology. 2002;27(1):87–96. doi: 10.1093/jpepsy/27.1.87. [DOI] [PubMed] [Google Scholar]
- Hruska B., Delahanty D.L. Application of the stressor vulnerability model to understanding posttraumatic stress disorder (PTSD) and alcohol-related problems in an undergraduate population. Psychology of Addictive Behaviors. 2012;26(4):734–746. doi: 10.1037/a0027584. [DOI] [PubMed] [Google Scholar]
- Junglen A., Hruska B., Jensen T., Boros A., Delahanty D.L. Improving our understanding of the relationship between emotional abuse and substance use disorders: the mediating roles of negative urgency and posttraumatic stress disorder. 2019 doi: 10.1080/10826084.2019.1594905. [DOI] [PubMed] [Google Scholar]
- Kaysen D., Dillworth T.M., Simpson T., Waldrop A., Larimer M.E., Resick P.A. Domestic violence and alcohol use: Trauma-related symptoms and motives for drinking. Addictive Behaviors. 2007;32(6):1272–1283. doi: 10.1016/J.ADDBEH.2006.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R.C., Berglund P., Demler O., Jin R., Merikangas K.R., Walters E.E. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62(6):593–602. doi: 10.1001/ARCHPSYC.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kubany E.S., Leisen M.B., Kaplan A.S., Watson S.B., Haynes S.N., Owens J.A., Burns K. Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: The Traumatic Life Events Questionnaire. Psychological Assessment. 2000;12(2):210–224. doi: 10.1037//1040-3590.12.2.210. [DOI] [PubMed] [Google Scholar]
- Littlefield A.K., Sher K.J., Wood P.K. Do Changes in Drinking Motives Mediate the Relation between Personality Change and “Maturing Out” of Problem Drinking? Journal of Abnormal Psychology. 2010;119(1):93. doi: 10.1037/A0017512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martens, M. P., Neighbors, C., Lewis, M. A., Lee, C. M., Oster-Aaland, L., & Larimer, M. E. (2008). The roles of negative affect and coping motives in the relationship between alcohol use and alcohol-related problems among college students. Journal of Studies on Alcohol and Drugs, 69(3), 412–419. 10.15288/JSAD.2008.69.412. [DOI] [PMC free article] [PubMed]
- Mccauley J.L., Killeen T., Gros D.F., Brady K.T., Back S.E. Posttraumatic Stress Disorder and Co-Occurring Substance Use Disorders: Advances in Assessment and Treatment. Clinical Psychology : A Publication of the Division of Clinical Psychology of the American Psychological Association. 2012;19(3):283–304. doi: 10.1111/CPSP.12006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore A.A., Overstreet C., Kendler K.S., Dick D.M., Adkins A., Amstadter A.B. Potentially traumatic events, personality, and risky sexual behavior in undergraduate college students. Psychological Trauma : Theory, Research, Practice and Policy. 2017;9(1):105–112. doi: 10.1037/TRA0000168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris V.L., Huffman L.G., Naish K.R., Holshausen K., Oshri A., McKinnon M. Impulsivity as a mediating factor in the association between posttraumatic stress disorder symptoms and substance use. Psychological Trauma: Theory, Research, Practice, and Policy. 2020;12(6):659–668. doi: 10.1037/TRA0000588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute of Mental Health. (2022). Post-Traumatic Stress Disorder. Www.Nimh.Nih.Gov/Health. Retrieved April 7, 2022, from https://www.nimh.nih.gov/health/topics/post-traumatic-stress-disorder-ptsd.
- O’Malley, P. M., & Johnston, L. D. (2002). Epidemiology of alcohol and other drug use among American college students. Journal of Studies on Alcohol. Supplement, 63(14), 23–39. 10.15288/JSAS.2002.S14.23. [DOI] [PubMed]
- Orona, J. A., Blume, A. W., Morera, O. F., & Perez, S. (2016). Examining Drinking Consequences and Reasons for Drinking in a Bilingual College Sample: Http://Dx.Doi.Org/10.1177/0739986306294873, 29(1), 101–115. 10.1177/0739986306294873.
- Overstreet C., Berenz E.C., Kendler K.S., Dick D.M., Amstadter A.B. Predictors and mental health outcomes of potentially traumatic event exposure. Psychiatry Research. 2017;247:296–304. doi: 10.1016/J.PSYCHRES.2016.10.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park, C. L., & Levenson, M. R. (2002). Drinking to cope among college students: prevalence, problems and coping processes. Journal of Studies on Alcohol, 63(4), 486–497. 10.15288/JSA.2002.63.486. [DOI] [PubMed]
- Radomski S.A., Read J.P. Mechanistic role of emotion regulation in the PTSD and alcohol association. Traumatology. 2016;22(2):113–121. doi: 10.1037/TRM0000068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ralph-Nearman C., Stewart J.L., Jones K.A. The role of negative urgency in risky alcohol drinking and binge-eating in United Kingdom male and female students. Addictive Behaviors Reports. 2020;11 doi: 10.1016/J.ABREP.2020.100274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raskin White, H., & Labouvie, E. W. (1989). Towards the assessment of adolescent problem drinking. Journal of Studies on Alcohol, 50(1), 30–37. 10.15288/jsa.1989.50.30. [DOI] [PubMed]
- Read J.P., Griffin M.J., Wardell J.D., Ouimette P. Coping, PTSD Symptoms and Alcohol Involvement in Trauma-Exposed College Students in the First Three Years of College. Psychology of Addictive Behaviors : Journal of the Society of Psychologists in Addictive Behaviors. 2014;28(4):1052. doi: 10.1037/A0038348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read J.P., Ouimette P., White J., Colder C., Farrow S. Rates of DSM–IV–TR Trauma Exposure and Posttraumatic Stress Disorder Among Newly Matriculated College Students. Psychological Trauma : Theory, Research, Practice and Policy. 2011;3(2):148. doi: 10.1037/A0021260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read, J. P., Radomski, S., & Borsari, B. (2015). Associations among Trauma, Posttraumatic Stress, and Hazardous Drinking in College Students: Considerations for Intervention. In Current Addiction Reports (Vol. 2, Issue 1, pp. 58–67). 10.1007/s40429-015-0044-0. [DOI] [PMC free article] [PubMed]
- Rothbaum B.O., Schwartz A.C. Exposure therapy for posttraumatic stress disorder. American Journal of Psychotherapy. 2002;56(1):59–75. doi: 10.1176/APPI.PSYCHOTHERAPY.2002.56.1.59. [DOI] [PubMed] [Google Scholar]
- Sheehan D.V., Lecrubier Y., Sheehan K.H., Amorim P., Janavs J., Weiller E.…Dunbar G.C. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry. 1998;59(SUPPL. 20):22–33. https://psycnet.apa.org/record/1998-03251-004 [PubMed] [Google Scholar]
- Shishido H., Gaher R.M., Simons J.S. I don’t know how I feel, therefore I act: Alexithymia, urgency, and alcohol problems. Addictive Behaviors. 2013;38(4):2014–2017. doi: 10.1016/J.ADDBEH.2012.12.014. [DOI] [PubMed] [Google Scholar]
- Simpson T.L., Stappenbeck C.A., Luterek J.A., Lehavot K., Kaysen D.L. Drinking motives moderate daily relationships between PTSD symptoms and alcohol use. Journal of Abnormal Psychology. 2014;123(1):237–247. doi: 10.1037/A0035193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson T.L., Stappenbeck C.A., Varra A.A., Moore S.A., Kaysen D. Symptoms of posttraumatic stress predict craving among alcohol treatment seekers: Results of a daily monitoring study. Psychology of Addictive Behaviors. 2012;26(4):724–733. doi: 10.1037/A0027169. [DOI] [PubMed] [Google Scholar]
- Smith, N. D. L., & Cottler, L. B. (2018). The Epidemiology of Post-Traumatic Stress Disorder and Alcohol Use Disorder. Alcohol Research : Current Reviews, 39(2), 113. /pmc/articles/PMC6561398/. [PMC free article] [PubMed]
- Sobell L.C., Brown J., Leo G.I., Sobell M.B. The reliability of the Alcohol Timeline Followback when administered by telephone and by computer. Drug and Alcohol Dependence. 1996;42(1):49–54. doi: 10.1016/0376-8716(96)01263-X. [DOI] [PubMed] [Google Scholar]
- Sobell L.C., Sobell M.B. Timeline follow-back, Measuring alcohol consumption. Humana Press; Totowa, NJ: 1992. pp. 41–72. [Google Scholar]
- Walker J., Bountress K.E., Calhoun C.D., Metzger I.W., Adams Z., Amstadter A.…Danielson C.K. Impulsivity and Comorbid PTSD and Binge Drinking. Journal of Dual Diagnosis. 2018;14(2):89–95. doi: 10.1080/15504263.2018.1439212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wardell J.D., Strang N.M., Hendershot C.S. Negative urgency mediates the relationship between childhood maltreatment and problems with alcohol and cannabis in late adolescence. Addictive Behaviors. 2016;56:1–7. doi: 10.1016/J.ADDBEH.2016.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers F.W., Bovin M.J., Lee D.J., Sloan D.M., Schnurr P.P., Kaloupek D.G.…Marx B.P. The clinician-administered PTSD Scale for DSM-5 (CAPS-5): Development and initial psychometric evaluation in military veterans. Psychological Assessment. 2018;30(3):383–395. doi: 10.1037/pas0000486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers F.W., Keane T.M., Davidson J.R.T. Clinician-administered PTSD scale: A review of the first ten years of research. Depression and Anxiety. 2001;13(3):132–156. doi: 10.1002/DA.1029. [DOI] [PubMed] [Google Scholar]
- Weiss N.H., Bold K.W., Contractor A.A., Sullivan T.P., Armeli S., Tennen H. Trauma exposure and heavy drinking and drug use among college students: Identifying the roles of negative and positive affect lability in a daily diary study. Addictive Behaviors. 2018;79:131–137. doi: 10.1016/J.ADDBEH.2017.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss N.H., Tull M.T., Davis L.T., Searcy J., Williams I., Gratz K.L. A Preliminary Experimental Investigation of Emotion Dysregulation and Impulsivity in Risky Behaviours. Behaviour Change : Journal of the Australian Behaviour Modification Association. 2015;32(2):127. doi: 10.1017/BEC.2015.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White H.R., Labouvie E.W. Towards assessment of adolescent problem drinking. Journal of Studies on Alcohol. 1989;50:30–37. doi: 10.15288/jsa.1989.50.30. [DOI] [PubMed] [Google Scholar]
- Wilson S.M., Krenek M., Dennis P.A., Yard S.S., Browne K.C., Simpson T.L. Daily associations between PTSD, drinking, and self-appraised alcohol-related problems. Psychology of Addictive Behaviors : Journal of the Society of Psychologists in Addictive Behaviors. 2017;31(1):27. doi: 10.1037/ADB0000238. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.


