IMPORTANCE:
High safety-net burden hospitals (HBHs) treating large numbers of uninsured or Medicaid-insured patients have generally been linked to worse clinical outcomes. However, limited data exist on the impact of the hospitals’ safety-net burden on in-hospital cardiac arrest (IHCA) outcomes in the United States.
OBJECTIVES:
To compare the differences in survival to discharge, routine discharge home, and healthcare resource utilization between patients at HBH with those treated at low safety-net burden hospital (LBH).
DESIGN, SETTING, AND PARTICIPANTS:
Retrospective cohort study across hospitals in the United States: Hospitalized patients greater than or equal to 18 years that underwent cardiopulmonary resuscitation (CPR) between 2008 and 2018 identified from the Nationwide Inpatient Database. Data analysis was conducted in January 2022.
EXPOSURE:
IHCA.
MAIN OUTCOMES AND MEASURES:
The primary outcome is survival to hospital discharge. Other outcomes are routine discharge home among survivors, length of hospital stay, and total hospitalization cost
RESULTS:
From 2008 to 2018, an estimated 555,016 patients were hospitalized with IHCA, of which 19.2% occurred at LBH and 55.2% at HBH. Compared with LBH, patients at HBH were younger (62 ± 20 yr vs 67 ± 17 yr) and predominantly in the lowest median household income (< 25th percentile). In multivariate analysis, HBH was associated with lower chances of survival to hospital discharge (adjusted odds ratio [aOR], 0.88; 95% CI, 0.85–0.96) and lower odds of routine discharge (aOR, 0.6; 95% CI, 0.47–0.75), compared with LBH. In addition, IHCA patients at publicly owned hospitals and those with medium and large hospital bed size were less likely to survive to hospital discharge, while patients with median household income greater than 25th percentile had better odds of hospital survival.
CONCLUSIONS AND RELEVANCE:
Our study suggests that patients who experience IHCA at HBH may have lower rates and odds of in-hospital survival and are less likely to be routinely discharged home after CPR. Median household income and hospital-level characteristics appear to contribute to survival.
Keywords: cardiopulmonary resuscitation, in-hospital cardiac arrest, outcomes, safety net, survival
KEY POINTS
Question: Do hospitals’ safety-net burden impact outcomes and resource utilization among patients having an in-hospital cardiac arrest (IHCA)?
Findings: In this cohort study evaluating hospitalizations with IHCA in the United States, patients treated at high safety-net burden hospitals (HBHs) were less likely to survive to hospital discharge compared with low safety-net burden hospitals (LBHs). Survivors at HBH were also less likely to be routinely discharged home compared with LBH.
Meaning: There is an urgent need for more research to identify evidence-based policies and regulations that may mitigate the observed disparities.
More than 200,000 patients undergo cardiopulmonary resuscitation (CPR) in the United States annually for in-hospital cardiac arrest (IHCA), with a survival rate of approximately 18–30% (1–3). Although there has been a considerable improvement in survival over the last 2 decades secondary to updates of scientific CPR guidelines and efforts of hospitals to improve the quality of care (4, 5), there remains a significant disparity in survival across hospitals (6, 7). Several factors have been identified to explain this disparity, including hospital CPR volumes and insurance status. For example, a study by Akintoye et al (8) demonstrated worse survival among patients treated at hospitals with high CPR volumes and uninsured patients.
Hospitals with a significant burden of safety net (Medicaid and uninsured) patients have worse outcomes across several medical and surgical conditions due to resource constraints and more advanced disease presentation (9–11). Currently, there is limited data on the effect of safety-net burden on outcomes of IHCA in the United States. A better understanding of the relationship between hospital safety-net burden and outcomes of patients with IHCA may inform better resource allocation and evidence-based policies to improve the quality of care.
Using a nationally representative database of inpatient stays in the United States, we evaluated the impact of hospital safety-net burden on survival to hospital discharge, resource utilization, and discharge status (discharged home without home healthcare) among Medicaid and uninsured patients hospitalized with IHCA. We hypothesized that IHCA at high safety-net burden hospitals (HBHs) would be associated with lower survival, routine home discharge rates, and increased resource utilization.
METHODS
Data Sources
Patient hospitalization data and discharge information were obtained from 2008 to 2018 Nationwide Inpatient Sample (NIS) database. The NIS is part of the Healthcare Cost and Utilization Project (HCUP), administered by the Agency for Healthcare Research and Quality. NIS captures a 20% stratified random sample of all inpatient discharges across hospitals in the United States to provide nationally representative estimates (12). Notably, in 2012, the NIS methodology changed from sampling all discharges at 20% of hospitals to 20% of records at all participating hospitals. The NIS uses trends for 2007–2011 and discharge weights for 2012–2017 data to provide accurate nationally representative estimates and account for clustering. We used the appropriate discharge weights provided by the NIS for our analysis (13).
The Morehouse School of Medicine waived the institutional review board approval and informed consent requirement because the NIS is a publicly available database with de-identified data. Procedures were followed in accordance with the ethical standards of the responsible committee on human experimentation (institutional or regional) and with the Helsinki Declaration of 1975. Study and article preparation followed the Strengthening the Reporting of Observational Studies in Epidemiology (14).
Study Population
We identified patients greater than or equal to 18 years old who experienced IHCA and underwent CPR using the International Classification of Diseases, 9th Edition, Clinical Modification (ICD-9-CM), and International Classification of Diseases, 10th Edition, Clinical Modification (ICD-10-CM) diagnosis and procedure codes. These codes have been extensively used in previously published studies on cardiac arrest using the NIS (3, 15, 16). Accompanying primary diagnoses and inpatient procedures were extracted using their respective ICD codes. A comprehensive list of all ICD codes used for this study is available in Supplementary Table 1 (http://links.lww.com/CCX/B123).
Patient sociodemographic data, including age, sex, race, insurance, household income, and hospital characteristics such as hospital bed size, teaching status, region, and geographical location, were defined according to the NIS data dictionary (17). Income quartile was defined according to HCUP as the estimated median annual household income based on a patient’s zip code. Hospital bed size was categorized based on the number of beds, location, and teaching status into small (1–49 in rural, 1–124 in urban nonteaching, and 1–249 in urban teaching hospitals), medium (50–99 in rural, 125–199 in urban nonteaching, and 250–424 in teaching hospitals) and large (100+ in rural, 200+ in urban nonteaching, and 425+ in urban teaching hospitals) (Supplementary Table 2, http://links.lww.com/CCX/B123). Comorbidities were presented using their ICD-9 and ICD-10 diagnosis codes.
Safety-Net Burden
Hospital safety-net burden was defined as the proportion of IHCA patients with Medicaid or uninsured payer status that underwent CPR per hospital. Hospitals were classified into low safety-net burden hospitals (LBHs), medium safety-net burden hospitals, or HBHs using tertiles with thresholds at the 33rd and 66th percentiles of this proportion. For the final analysis, only HBH and LBH were included. This safety-net burden determination method has been previously used in similar studies evaluating hospital safety-net burden (18–20).
Study Outcomes
The primary outcome of interest was survival to hospital discharge. Secondary outcomes were routine discharge (discharged home without home healthcare) and healthcare resource utilization determined by hospitalization costs and total length of hospital stay (LOS). Hospitalization costs were derived from total charges using hospital-specific cost-to-charge ratios and were inflation-adjusted further to the 2017 Personal Healthcare Index (21).
Study Analysis
Categorical and continuous variables were reported as frequency (percentage) and mean with sds. Pearson chi-square and adjusted Wald tests were used to compare categorical and continuous variables, respectively. The Cochran-Armitage test was used to evaluate the trends in the occurrence and survival rates of cardiac arrest over the study period. A nonparametric rank-based test (nptrend) was used to assess the significance of trends over the study period.
Multivariate linear and logistic regression models adjusting for primary hospitalization diagnosis and clinically relevant patient and hospital characteristics (age, sex, household income, hospital region, hospital type, hospital ownership, Charlson Comorbidity Index [CCI], tobacco abuse, obesity, history of diabetes mellitus, chronic kidney disease, end-stage renal disease on hemodialysis, chronic liver disease, hypertension, congestive heart failure, myocardial infarction, and stroke) were developed to estimate the rates of selected inpatient procedures and the odds of primary and secondary outcomes comparing HBH to LBH (reference). We accounted for hospital site and level clustering using the mixed-methods approach.
Using multivariate logistic regression., we determined the socioeconomic and hospital-level factors associated with in-hospital survival in HBH and LBH adjusted for age, gender, race, sex, CCI, tobacco abuse, obesity, history of diabetes mellitus, chronic kidney disease, end-stage renal disease on hemodialysis, chronic liver disease, hypertension, congestive heart failure, myocardial infarction, stroke, and selected inpatient procedures.
Regression results are reported as adjusted odds ratios (aORs) for categorical variables and β coefficients for continuous variables, with 95% CIs reported for both. A two-tailed p value of less than 0.05 was considered statistically significant. All analyses were performed using IBM SPSS Statistics for Windows, Version 26.0 (IBM Corp, Armonk, NY).
RESULTS
Of an estimated 555,016 adult hospitalizations of patients that experienced IHCA and underwent CPR, 108,783 (19.6%) occurred at LBHs, and 3,036,369 (55.2%) occurred at HBHs (Supplementary Table 3, http://links.lww.com/CCX/B123). Compared with LBHs, patients at HBHs, on average, were younger (62 ± 20 yr vs 67 ± 12 yr; p < 0.001) and less likely to be of White race (60.4% vs 74%; p < 0.001). HBH patients were more likely to be in the lowest median household income (36.3% vs 24.2%; p < 0.001) and have severe comorbidity burden (11.4% 7.7%; p < 0.001). HBH were more likely to be urban teaching hospitals (63.8% vs 47.9%; p < 0.001), located in the Western region (26.4% vs 15%), and publicly owned (14.9% vs 5.8%; p < 0001).
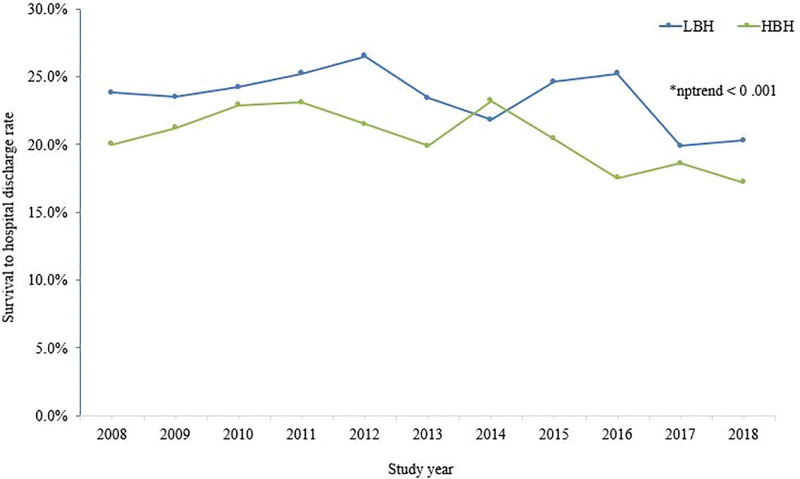
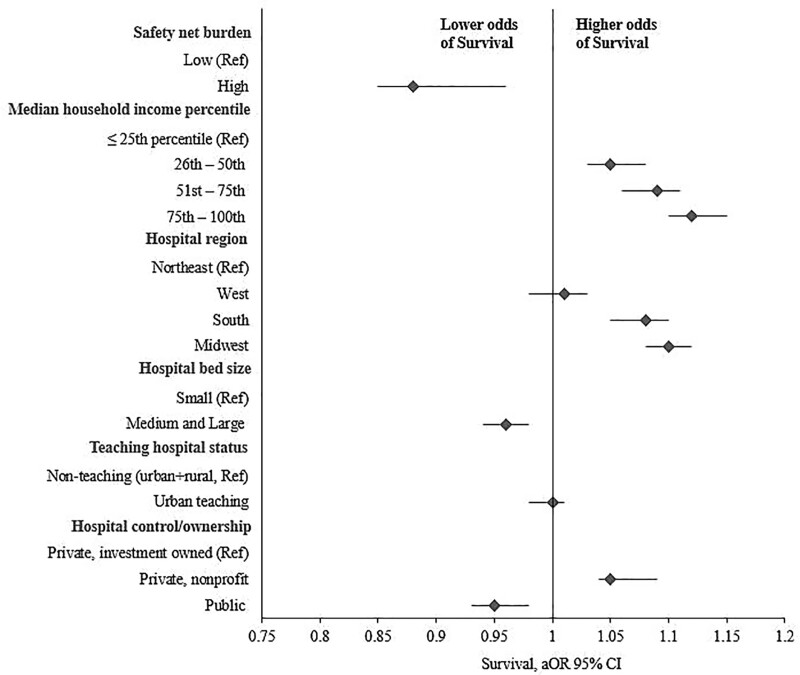
From 2008 to 2018, there was a decline in survival rates at both HBH (20.0–17.2.%; nptrend < 0.001) and LBH (23.8–20.3.%; nptrend < 0.001) (Fig. 1). The overall survival to hospital discharge rate was lower among patients at HBH compared with LBH (20.5% vs 23.5%; p < 0.001) (Table 1). In multivariate regression analysis, HBH (aOR, 0.88; 95% CI, 0.85–0.96) was associated with lower adjusted odds of survival to hospital discharge, compared with LBH and lower odds of routine discharge home (aOR, 0.58; 95% CI, 0.47–0.75; p < 0.001), compared with LBH. (Table 1 and Fig. 2). Other factors associated with a lower likelihood of survival to hospital discharge were treatment at medium or large hospital bed-sized hospitals (aOR, 0.96; 95% CI, 0.94–0.98) and public hospital ownership (OR, 0.95; 95% CI, 0.93–0.98). Conversely, median household income in the 26th–50th (aOR, 1.05; 95% CI, 1.03–1.08), 51st–75th (OR, 1.09; 95% CI, 1.06–1.11), and 75th–100th percentiles (aOR, 1.12; 95% CI, 1.10–1.15); private, nonprofit hospital ownership (aOR, 1.06; 95% CI, 1.04–1.09), and hospitals located in the Midwest (OR, 1.09; 95% CI, 1.08–1.12) and the South (OR, 1.08; 95% CI, 1.05–1.11) were associated with improved odds of survival (Fig. 2). There were no significant and clinically relevant differences in total healthcare cost and LOS between HBH and LBH (Table 2).
Figure 1.
Temporal trends in the survival rates of in-hospital cardiac arrest patients at low safety-net burden hospital (LBH) and high safety-net burden hospital (HBH). nptrend = nonparametric rank-based test.
TABLE 1.
Survival to Hospital Discharge and Routine Discharge Outcomes by Safety-Net Burden
| Outcomes | LBH, n (%) | HBH, n (%) | p | HBH vs LBH (OR [95% CI]) | p |
|---|---|---|---|---|---|
| Survival to hospital discharge | 25,564 (23.5) | 62,806 (20.5) | < 0.001 | 0.88 (0.85–0.96) | < 0.001 |
| Routine discharge | 18,167 (16.7) | 46,568 (15.2) | < 0.001 | 0.58 (0.47–0.75) | < 0.001 |
HBH = high safety-net burden hospital, LBH = low safety-net burden hospital, OR = odds ratio.
OR of survival to hospital discharge and routine discharge among in-hospital cardiac arrest patients at HBH vs LBH (reference). ORs adjusted for age, sex, household income, hospital region, hospital type, hospital ownership, Charlson Comorbidity Index, tobacco abuse, obesity, history of diabetes mellitus, chronic kidney disease, end-stage renal disease on hemodialysis, chronic liver disease, hypertension, congestive heart failure, myocardial infarction, stroke, and selected inpatient procedures.
Routine discharge—home discharge without home health.
Figure 2.
Socioeconomic and hospital-level factors associated with survival to hospital discharge among in-hospital cardiac arrest patients at U.S. hospitals. More detailed information on the specific dollar amounts in each category of median household income and the number of hospital beds in each category can be found in Supplementary Table 2 (http://links.lww.com/CCX/B123) and nationwide inpatient sample description of data elements Healthcare Cost and Utilization Project US Home Page (ahrq.gov). Adjusted odds ratios (aORs) adjusted for age, sex, Charlson Comorbidity Index, tobacco abuse, obesity, history of diabetes mellitus, chronic kidney disease, end-stage renal disease on hemodialysis, chronic liver disease, hypertension, congestive heart failure, myocardial infarction, and stroke. Ref = reference.
TABLE 2.
Adjusted Mean Cost and Length of Stay
| Hospital Burden | Total Hospital Cost, $ | β Coefficient (95% CI) ($) | Length of Stay (d) | β Coefficient (95% CI) (d) |
|---|---|---|---|---|
| High safety-net burden | 16,667 (16,645–17,689) | 13 (13–14) | 21.9 (20.5–23.5) | 0 |
| Low safety-net burden | 16,680 (16,658–17,703) | 21.9 (20.4–23.5) |
Outcomes adjusted for age, sex, household income, hospital region, hospital type, hospital ownership, Charlson Comorbidity Index, tobacco abuse, obesity, history of diabetes mellitus, chronic kidney disease, end-stage renal disease on hemodialysis, chronic liver disease, hypertension, congestive heart failure, myocardial infarction, stroke, and selected inpatient procedures.
Patients at HBH were less likely to undergo advanced modalities such as coronary angiography (aOR, 0.93; 95% CI, 0.91–0.95; p < 0.001), percutaneous coronary intervention (PCI) (aOR, 0.93; 95% CI, 0.89–0.96; p < 0.001), therapeutic hypothermia (aOR, 0.93; 95% CI, 0.88–0.99), and intra-aortic balloon pump insertion (aOR, 0.81; 95% CI, 0.78–0.85; p < 0.001) (Table 3), compared with LBH. On the other hand, HBH patients had higher odds of invasive mechanical ventilation (aOR, 1.11; 95% CI, 1.01–1.13; p < 0.001) and extracorporeal membrane oxygenation (ECMO) use (aOR, 1.20; 95% CI, 1.07–1.35; p < 0.001). The annual proportion of procedures performed at both HBH and LBH are shown in Supplementary Table 4 (http://links.lww.com/CCX/B123).
TABLE 3.
Selected Procedures Performed at Low Safety-Net Burden Hospital and High Safety-Net Burden Hospital in Patients That Underwent ICPR for In-Hospital Cardiac Arrest
| Selected Procedures | LBH (%) | HBH (%) | HBH vs LBH | p |
|---|---|---|---|---|
| Adjusted OR (95% CI) | ||||
| Coronary angiography | 19,799 (18.2) | 48,406 (15.8) | 0.93 (0.91–0.95) | < 0.001 |
| Percutaneous coronary intervention | 9,464 (8.7) | 22,365 (7.3) | 0.93 (0.89–0.96) | < 0.001 |
| Invasive mechanical ventilation | 69,621 (64) | 217,828 (71.1) | 1.11 (1.01–1.13) | < 0.001 |
| Therapeutic hypothermia | 2,284 (2.1) | 5,821 (1.9) | 0.93 (0.88–0.99) | 0.01 |
| Tracheostomy | 8,594 (7.9) | 24,816 (8.1) | 1.01 (0.97–1.03) | 0.9 |
| Ventricular assist device | 435 (0.4) | 1,838 (0.6) | 1.07 (0.96–1.20) | 0.2 |
| Intra-aortic balloon pump | 5,222 (4.8) | 11,029 (3.6) | 0.81 (0.78–0.85) | < 0.001 |
| Extracorporeal membrane oxygenation | 435 (0.4) | 2,451 (0.8) | 1.20 (1.07–1.35) | < 0.001 |
HBH = high safety-net burden hospital, LBH = low safety-net burden hospital, OR = odds ratio.
Adjusted OR of performing selected procedures at HBH vs LBH (reference). OR adjusted for age, sex, household income, hospital region, hospital type, hospital ownership, Charlson Comorbidity Index, tobacco abuse, obesity, history of diabetes mellitus, chronic kidney disease, end-stage renal disease on hemodialysis, chronic liver disease, hypertension, congestive heart failure, myocardial infarction, and stroke.
DISCUSSION
IHCA survival largely depends on the quality of acute and post-resuscitation care, and hospitals with more resources tend to perform better (5, 22–24). High hospital safety-net burden have been associated with inferior outcomes across multiple clinical conditions due to limited resources (20, 25).
In this evaluation of IHCA outcomes across hospitals in the United States, the overall survival to hospital discharge rate was lower at HBH compared with LBH. Importantly, HBH was independently associated with a lesser chance of survival to hospital discharge and lower odds of routine discharge home among IHCA survivors. Medium to large hospital bed size and public ownership of hospitals were significantly associated with lower odds of survival. In contrast, relatively wealthier patients with household income levels in the 25th percentile–100th percentile and those treated at safety-net hospitals located in the Midwest and Southern regions were more likely to survive to discharge. There was no significant difference in Hospital LOS and costs between LBH and HBH.
The overall IHCA survival rates in both LBH (23.5%) and HBH (20.5%) were lower than recently reported across hospitals in the United States (26–29). We also found a slight decline in the survival trend in both LBH and HBH during the study period in contrast with demonstrated improvement in IHCA survival outcomes over the last 2 decades (23, 24, 27). Lack of health insurance and underinsurance has been linked to higher in-hospital mortality in cardiac arrest patients (8, 30, 31). We only evaluated IHCA patients with Medicaid or no health insurance categorized by safety-net burden across U.S. hospitals, which likely explains the lower survival rates in both LBH and HBH compared with the general population. Additionally, a high safety-net burden likely limits the implementation of strategies that have been shown to improve IHCA outcomes, including participation in quality improvement registries, the presence of high-functioning resuscitation teams, and appropriate post-arrest care (23, 24, 27, 32, 33).
Compared with LBH, patients at HBH experienced lower survival to hospital discharge, and those who survived were less likely to be routinely discharged home, consistent with our hypothesis. Similar studies have theorized that limited hospital resources, financial constraints, and unfavorable national policies contribute to poorer medical and surgical outcomes in safety-net hospitals (6, 20, 25, 34). In the context of our study population, we noted significant variations between patients treated at HBH and LBH, which may shed some light on our findings. HBH patients were more likely to be of lower socioeconomic status (SES) and have a higher comorbidity burden, which are associated with poor outcomes after IHCA (12, 35, 36). Additionally, HBH were less likely to perform advanced procedures such as coronary angiography with PCI and intra-aortic balloon pump that may improve survival, particularly in patients with post-resuscitation cardiogenic shock (37–39). Although targeted temperature management was more common in LBH, its use is limited in IHCA due to the low quality of evidence supporting that it improves outcomes (40). ECMO has been shown to improve survival in cardiac arrest patients (41, 42) and was performed more frequently at HBH. However, it is difficult to ascertain how these procedures combined contributed to the disparate outcomes between HBH and LBH observed in our study. One possibility might be that the availability of ECMO is higher at HBH, therefore, making the consideration and use more likely. We believe that these findings warrant further investigation.
Low household income, relatively larger hospital bed size and public ownership of hospitals were associated with a lower likelihood of survival to hospital discharge in HBH and LBH independent of demographics, comorbidity burden, and inpatient procedures in our study. Median household income is a proxy for SES, while a large bed size and public ownership of a hospital indicate the provision of care to a proportionately larger share of vulnerable populations (43, 44). Low SES is generally associated with worse survival outcomes across a spectrum of clinical conditions, and a higher burden of patients seeking care is likely to place enormous strain on already resource-constrained HBH, which may explain the lower odds of survival (45–47).
Multiple studies have examined the impact of geographical location on healthcare outcomes with variable findings (15, 29, 48). HBH and LBH located in the countries’ Midwestern and Southern regions had better survival odds than the Northeast in our study. Kolte et al (29) reported similar findings in IHCA survival across U.S. hospitals between 2003 and 2011. Reasons for these variations remain unclear and may be explained by regional differences in IHCA preparedness, such as availability or organization of rapid response or code teams, quality of CPR and post-resuscitation care, institutional leadership, and participation in CPR quality improvement programs, regulatory requirements and safety-net hospital administration and funding, all of which may impact outcomes (49, 50). These findings present preliminary data to prompt further investigation.
The Patient Protection and Affordable Care Act, signed into law in 2010, proposed to increase the pool of insured patients and expand Medicaid coverage for all patients, invariably lessening the burden on safety-net hospitals (51). However, the law was accompanied by a significant reduction in the disproportionate-share funding that hospitals have used to offset uncompensated and unreimbursed care costs (52). Reports show that the Medicaid disproportionate-share hospital funding does not correlate with the proportion of uninsured and Medicaid patients at safety-net hospitals, coupled with the resistance to Medicaid expansion in some States, which may see some HBHs not receiving the appropriate financial support they need (53–55). Furthermore, the ongoing COVID-19 pandemic has further widened socioeconomic inequalities, likely increasing the number of uninsured and Medicaid-reliant patients, negatively impacting HBH already operating on thin financial margins (56, 57). Due to the critical role of safety-net hospitals in the healthcare system, their financial health and sustainability are more important than ever and should be at the forefront of policy discussions.
Clinical care is often complex, and it can be challenging to make comparisons across hospitals and understand the specific component of care contributing to outcomes. However, our findings suggest that patients’ SES and hospital-level size and ownership are independently associated with survival in hospitals with a large safety-net burden of IHCA patients. Our study provides additional data that could help policymakers reimagine the allocation of finances and resources to hospitals with high safety-net burden, which may improve the quality of resuscitation care.
The present study has several significant limitations inherent to the retrospective nature of the database. The NIS captures diagnosis using ICD codes subject to coding errors and hospital variations. Also, granular hospital-level data on factors known to affect cardiac arrest outcomes, such as the presence of resuscitation teams, protocols, duration of cardiac arrest, time until resuscitative efforts started, and specific location of cardiac arrests such as the ICU, emergency department, or medical and surgical wards are not available and could not be studied. We are not able to accurately ascertain if patients had shockable rhythm or not at the time of cardiac arrest, which may have impacted survival outcomes. Lastly, NIS only contains in-hospital data limiting our ability to evaluate these patients’ post-discharge and long-term outcomes. Our data only reflect in-hospital outcomes and cannot provide insights into the long-term outcomes of these admissions. Despite these limitations, the NIS is the largest all-payer inpatient database and, with its survey-weighted design, capable of providing generalizable, nationally representative results.
CONCLUSIONS
Patients who had an IHCA and subsequently underwent CPR at HBH were less likely to survive to hospital discharge and be routinely discharged home compared to LBH. These findings demonstrate an urgent need for more research to identify evidence-based policies and regulations targeted at mitigating the observed disparities.
Supplementary Material
Footnotes
Drs. Olanipekun and Abe contributed equally to the research and are both lead authors.
Drs. Olanipekun and Abe conceptualized the study, conducted the statistical analysis, and wrote the article. Drs. Chris-Olaiya and Effoe contributed to statistical analysis and critical revision of the article. Drs. Bhardwaj, Harrison, Moreno Franco, Guru, and Sanghavi contributed to the critical revision of the article for accuracy and important intellectual content. Drs. Olanipekun and Abe had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
The authors have disclosed that they do not have any potential conflicts of interest.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/ccejournal).
REFERENCES
- 1.Ehlenbach WJ, Barnato AE, Curtis JR, et al. : Epidemiologic study of in-hospital cardiopulmonary resuscitation in the elderly. N Engl J Med 2009; 361:22–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Merchant RM, Yang L, Becker LB, et al. ; American Heart Association Get With The Guidelines-Resuscitation Investigators: Incidence of treated cardiac arrest in hospitalized patients in the United States. Crit Care Med 2011; 39:2401–2406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mallikethi-Reddy S, Briasoulis A, Akintoye E, et al. : Incidence and survival after in-hospital cardiopulmonary resuscitation in nonelderly adults. Circ Cardiovasc Qual Outcomes 2017; 10:e003194. [DOI] [PubMed] [Google Scholar]
- 4.Honarmand K, Mepham C, Ainsworth C, et al. : Adherence to advanced cardiovascular life support (ACLS) guidelines during in-hospital cardiac arrest is associated with improved outcomes. Resuscitation 2018; 129:76–81 [DOI] [PubMed] [Google Scholar]
- 5.Edelson DP, Litzinger B, Arora V, et al. : Improving in-hospital cardiac arrest process and outcomes with performance debriefing. Arch Intern Med 2008; 168:1063–1069 [DOI] [PubMed] [Google Scholar]
- 6.Rasmussen TP, Riley DJ, Sarazin MV, et al. : Variation across hospitals in in-hospital cardiac arrest incidence among Medicare beneficiaries. JAMA Netw Open 2022; 5:e2148485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Girotra S, Nallamothu BK, Spertus JA, et al. ; American Heart Association Get with the Guidelines–Resuscitation Investigators: Trends in survival after in-hospital cardiac arrest. N Engl J Med 2012; 367:1912–1920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Akintoye E, Adegbala O, Egbe A, et al. : Association between hospital volume of cardiopulmonary resuscitation for in-hospital cardiac arrest and survival to hospital discharge. Resuscitation 2020; 148:25–31 [DOI] [PubMed] [Google Scholar]
- 9.McKinley LP, Wen T, Gyamfi-Bannerman C, et al. : Hospital safety-net burden and risk for readmissions and severe maternal morbidity. Am J Perinatol 2021; 38:E359–E366 [DOI] [PubMed] [Google Scholar]
- 10.Wong RJ, Hirode G: The effect of hospital safety-net burden and patient ethnicity on in-hospital mortality among hospitalized patients with cirrhosis. J Clin Gastroenterol 2021; 55:624–630 [DOI] [PubMed] [Google Scholar]
- 11.Rosero EB, Modrall JG, Joshi GP: Failure to rescue after major abdominal surgery: The role of hospital safety net burden. Am J Surg 2020; 220:1023–1030 [DOI] [PubMed] [Google Scholar]
- 12.Steiner C, Elixhauser A, Schnaier J: The healthcare cost and utilization project: An overview. Eff Clin Pract 2002; 5:143–151 [PubMed] [Google Scholar]
- 13.Healthcare Cost and Utilization Project: Overview of the National (Nationwide) Inpatient Sample (NIS). Available online: http://www.hcup-us.ahrq.gov/nisoverview.jsp. Accessed January 22, 2022.
- 14.von Elm E, Altman DG, Egger M, et al. ; STROBE Initiative: The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J Clin Epidemiol 2008; 61:344–349 [DOI] [PubMed] [Google Scholar]
- 15.Atreya AR, Patlolla SH, Devireddy CM, et al. : Geographic variation and temporal trends in management and outcomes of cardiac arrest complicating acute myocardial infarction in the United States. Resuscitation 2022; 170:339–348 [DOI] [PubMed] [Google Scholar]
- 16.Hadaya J, Dobaria V, Aguayo E, et al. : National trends in utilization and outcomes of extracorporeal support for in- and out-of-hospital cardiac arrest. Resuscitation 2020; 151:181–188 [DOI] [PubMed] [Google Scholar]
- 17.Agency for Healthcare Research and Quality: National (Nationwide) Inpatient Database Documentation Archive. Rockville, MD. 2016. Available at: www.hcup-us.ahrq.gov/db/nation/nis/nisarchive.jsp. Accessed January 22, 2022 [Google Scholar]
- 18.Werner RM, Goldman LE, Dudley RA: Comparison of change in quality of care between safety-net and non-safety-net hospitals. JAMA 2008; 299:2180–2187 [DOI] [PubMed] [Google Scholar]
- 19.Genther DJ, Gourin CG: The effect of hospital safety-net burden status on short-term outcomes and cost of care after head and neck cancer surgery. Arch Otolaryngol Head Neck Surg 2012; 138:1015–1022 [DOI] [PubMed] [Google Scholar]
- 20.Williamson CG, Hadaya J, Mandelbaum A, et al. : Outcomes and resource use associated with acute respiratory failure in safety net hospitals across the United States. Chest 2021; 160:165–174 [DOI] [PubMed] [Google Scholar]
- 21.Dunn A, Grosse SD, Zuvekas SH: Adjusting health expenditures for inflation: A review of measures for health services research in the United States. Health Serv Res 2018; 53:175–196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ofoma UR, Basnet S, Berger A, et al. ; American Heart Association Get With the Guidelines – Resuscitation Investigators: Trends in survival after in-hospital cardiac arrest during nights and weekends. J Am Coll Cardiol 2018; 71:402–411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nallamothu BK, Guetterman TC, Harrod M, et al. : How do resuscitation teams at top-performing hospitals for in-hospital cardiac arrest succeed? A qualitative study. Circulation 2018; 138:154–163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rasmussen TP, Bullis TC, Girotra S: Targeted temperature management for treatment of cardiac arrest. Curr Treat Options Cardiovasc Med 2020; 22:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gandjian M, Williamson C, Xia Y, et al. : Association of hospital safety net status with outcomes and resource use for extracorporeal membrane oxygenation in the United States. J Intensive Care Med 2022; 37:535–542 [DOI] [PubMed] [Google Scholar]
- 26.Sawyer KN, Camp-Rogers TR, Kotini-Shah P, et al. : Sudden cardiac arrest survivorship: A scientific statement from the American Heart Association. Circulation 2020; 141:E654–E685 [DOI] [PubMed] [Google Scholar]
- 27.Girotra S, Nallamothu BK, Spertus JA, et al. : Trends in survival after in-hospital cardiac arrest for the American Heart Association Get With the Guidelines – Resuscitation (GWTG- Resuscitation) investigators. N Engl J Med 2013; 367:1912–1920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Holmberg MJ, Granfeldt A, Girotra S, et al. ; American Heart Association’s Get With The Guidelines®-Resuscitation Investigators: Trends in survival and introduction of the 2010 and 2015 guidelines for adult in-hospital cardiac arrest. Resuscitation 2020; 157:112–120 [DOI] [PubMed] [Google Scholar]
- 29.Kolte D, Khera S, Aronow WS, et al. : Regional variation in the incidence and outcomes of in-hospital cardiac arrest in the United States. Circulation 2015; 131:1415–1425 [DOI] [PubMed] [Google Scholar]
- 30.Pancholy SB, Patel GA, Patel DD, et al. : Association between insurance status and in-hospital outcomes in patients with out-of-hospital ventricular fibrillation arrest. Clin Cardiol 2021; 44:511–517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stecker EC, Reinier K, Rusinaru C, et al. : Health insurance expansion and incidence of out-of-hospital cardiac arrest: A pilot study in a US metropolitan community. J Am Heart Assoc 2017; 6:e005667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Peberdy MA, Callaway CW, Neumar RW, et al. : Part 9: Post-cardiac arrest care: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2010; 122:S768–S786 [DOI] [PubMed] [Google Scholar]
- 33.Wakeam E, Hevelone ND, Maine R, et al. : Failure to rescue in safety-net hospitals availability of hospital resources and differences in performance. JAMA Surg 2014; 149:229–235 [DOI] [PubMed] [Google Scholar]
- 34.Fujisaki T, Kassim F, Kassim G, et al. : Biventricular Takotsubo syndrome with COVID-19 in an Asian male. J Cardiol Cases 2021; 24:6–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kuo WT, Gould MK, Louie JD, et al. : Catheter-directed therapy for the treatment of massive pulmonary embolism: Systematic review and meta-analysis of modern techniques. J Vasc Interv Radiol 2009; 20:1431–1440 [DOI] [PubMed] [Google Scholar]
- 36.Thomas EH, Lloyd AR, Leopold N: Frailty, multimorbidity and in-hospital cardiopulmonary resuscitation: Predictable markers of outcome? Clin Med (Lond) 2021; 21:E342–E362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.O’Gara PT, Kushner FG, Ascheim DD, et al. : 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: A report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines. J Am Coll Cardiol 2013; 61:e78–e140 [DOI] [PubMed] [Google Scholar]
- 38.Dhruva SS, Ross JS, Mortazavi BJ, et al. : Use of mechanical circulatory support devices among patients with acute myocardial infarction complicated by cardiogenic shock. JAMA Netw Open 2021; 4:e2037748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Patel NJ, Patel N, Bhardwaj B, et al. : Trends in utilization of mechanical circulatory support in patients hospitalized after out-of-hospital cardiac arrest. Resuscitation 2018; 127:105–113 [DOI] [PubMed] [Google Scholar]
- 40.Granfeldt A, Holmberg MJ, Nolan JP, et al. ; International Liaison Committee on Resuscitation (ILCOR) Advanced Life Support Task Force: Targeted temperature management in adult cardiac arrest: Systematic review and meta-analysis. Resuscitation 2021; 167:160–172 [DOI] [PubMed] [Google Scholar]
- 41.Cummings MJ, Baldwin MR, Abrams D, et al. : Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: A prospective cohort study. Lancet 2020; 395:1763–1770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Richardson ASC, Schmidt M, Bailey M, et al. : ECMO cardio-pulmonary resuscitation (ECPR), trends in survival from an international multicentre cohort study over 12-years. Resuscitation 2017; 112:34–40 [DOI] [PubMed] [Google Scholar]
- 43.Estabragh ZR, Mamas MA: The cardiovascular manifestations of influenza: A systematic review. Int J Cardiol 2013; 167:2397–2403 [DOI] [PubMed] [Google Scholar]
- 44.Popescu I, Fingar KR, Cutler E, et al. : Comparison of 3 safety-net hospital definitions and association with hospital characteristics. JAMA Netw Open 2019; 2:e198577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Schultz WM, Kelli HM, Lisko JC, et al. : Socioeconomic status and cardiovascular outcomes: Challenges and interventions. Circulation 2018; 137:2166–2178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Quan D, Luna Wong L, Shallal A, et al. : Impact of race and socioeconomic status on outcomes in patients hospitalized with COVID-19. J Gen Intern Med 2021; 36:1302–1309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jakobsen L, Niemann T, Thorsgaard N, et al. : Dimensions of socioeconomic status and clinical outcome after primary percutaneous coronary intervention. Circ Cardiovasc Interv 2012; 5:641–648 [DOI] [PubMed] [Google Scholar]
- 48.Godøy A, Huitfeldt I: Regional variation in health care utilization and mortality. J Health Econ 2020; 71:102254. [DOI] [PubMed] [Google Scholar]
- 49.Ornato JP, Peberdy MA, Reid RD, et al. ; NRCPR Investigators: Impact of resuscitation system errors on survival from in-hospital cardiac arrest. Resuscitation 2012; 83:63–69 [DOI] [PubMed] [Google Scholar]
- 50.Morrison LJ, Neumar RW, Zimmerman JL, et al. ; American Heart Association Emergency Cardiovascular Care Committee, Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation, Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology, and Council on P: Strategies for improving survival after in-hospital cardiac arrest in the United States: 2013 consensus recommendations: A consensus statement from the American Heart Association. Circulation 2013; 127:1538–1563 [DOI] [PubMed] [Google Scholar]
- 51.Chokshi DA, Chang JE, Wilson RM: Health reform and the changing safety net in the United States. N Engl J Med 2016; 375:1790–1796 [DOI] [PubMed] [Google Scholar]
- 52.Cole ES, Walker D, Mora A, et al. : Identifying hospitals that may be at most financial risk from Medicaid disproportionate-share hospital payment cuts. Health Aff 2014; 33:2025–2033 [DOI] [PubMed] [Google Scholar]
- 53.Kuo WT, Sista AK, Faintuch S, et al. : Society of interventional radiology position statement on catheter-directed therapy for acute pulmonary embolism. J Vasc Interv Radiol 2018; 29:293–297 [DOI] [PubMed] [Google Scholar]
- 54.Dobson A, Davanzo J, Haught R: The financial impact of the American Health Care Act’s Medicaid provisions on safety-net hospitals. Commonw Fund 2017. 2017. Available at: https://www.commonwealthfund.org/publications/fund-reports/2017/jun/financial-impact-american-health-care-acts-medicaid-provisions. Accessed January 22, 2022. [PubMed]
- 55.Mobley EM, Ullrich F, Mueller KJ: Distribution of disproportionate share hospital payments to rural and critical access hospitals. Rural Policy Brief 2017; 2017:1–6 [PubMed] [Google Scholar]
- 56.Ku L, Brantley E: Widening social and health inequalities during the COVID-19 pandemic. JAMA Heal Forum 2020; 1:e200721. [DOI] [PubMed] [Google Scholar]
- 57.Mullangi S, Knudsen J, Chokshi DA: Shoring up the US safety net in the era of coronavirus disease 2019. JAMA Heal Forum 2020; 1:e200730. [DOI] [PubMed] [Google Scholar]