Abstract
Objectives
Inferior alveolar nerve neurosensory deficit is a worrisome complication of surgical extraction of impacted mandibular third molars. A novel approach using two-stage partial coronectomy has been proposed as an alternative surgical procedure to reduce this complication. This study compared neurosensory deficits of inferior alveolar nerve following impacted mandibular third molar extraction using one-stage complete extraction with the two-stage partial coronectomy technique.
Material and Methods
Subjects with mesioangular or horizontal impacted mandibular third molar with an intimate relationship with inferior dental canal who met the inclusion criteria were recruited for the study. Subjects were divided into one-stage and two-stage partial coronectomy techniques. The subjects were evaluated for the presence of inferior alveolar neurosensory deficit, and the relationships of neurosensory nerve deficit with sex, age and type of impaction.
Results
Neurosensory deficit was observed in 5 subjects (7.8%), with all cases seen in the one-stage group. This difference was statistically significant (p = 0.03). The relationship between the incidence of neurosensory deficit and age, sex, type of impaction, surgical difficulty, operating time and root morphology was not statistically significant (p > 0.05).
Conclusion
Findings from this study suggest partial coronectomy compared to one-stage complete extraction reduces the incidence of Inferior alveolar nerve neurosensory deficit.
Keywords: Inferior alveolar nerve, Partial coronectomy, Impacted mandibular third molar, Neurosensory deficit
Introduction
Management of impacted mandibular third molars (IMTMs) may include surgical exposure, transplantation, surgical extraction or long-term observation in cases where a decision is made to retain the impacted tooth [1]. Surgical extraction of IMTMs is a common procedure in oral surgery. The procedure may be associated with many complications, including infection, alveolar osteitis, tooth displacement, aspiration, mandibular fracture, damage to adjacent teeth and paraesthesia/anaesthesia of the inferior alveolar nerve and the lingual nerve [1–4]. Of more concern is the risk of nerve damage, particularly the inferior alveolar nerve (IAN) and the lingual nerve [4, 5].
Injury to IAN can occur from compression of the nerve, either indirectly by forces transmitted through the root during elevation or directly by the elevators. The nerve may also become transected by rotary instruments during removal of a tooth whose root is grooved or perforated by the IAN [6]. IAN injury usually presents as paraesthesia or anaesthesia of the lower lip, teeth, chin and buccal gingivae on the affected side. The incidence of IAN injury reported in the literature ranges between 0.26 and 8.4% [7]. In Nigeria, an incidence of 2.6% has been reported [8]. Injury to the IAN can be troublesome, causing problems with speech and mastication and may adversely affect the patient’s quality of life [9, 10]. They also constitute one of the most frequent causes of complaints and litigation [10].
Several methods have been devised to minimise the risk of IAN injury, and these include orthodontic-assisted extraction [11], coronectomy [12, 13] and staged surgical removal of the IMTMs [14]. Of these methods, the two-stage approach proposed by Landi et al. [14] appears to be a safer and effective method reported to reduce the risk considerably. This novel approach described in a case series is an alternative approach to one-stage extraction of horizontally and mesioangularly inclined IMTMs with the root apexes in close contact with the IAN [14]. This study aimed to compare the incidence of neurosensory deficits of the inferior alveolar nerve following impacted mandibular third molar extraction using the two-stage technique described by Landi et al. [14] with a one-stage complete surgical extraction technique in a randomised controlled clinical study.
Material and Method
Study Settings and Design
The study was carried out at a tertiary health facility in Lagos, Nigeria. It was a prospective randomised controlled clinical study to compare the incidence of IAN neurosensory deficit following removal of IMTMs using a two-stage (partial coronectomy) followed by surgical extraction) with one-stage (complete) surgical technique. The two-stage technique described by Landi et al. [14] will be referred to as the "partial coronectomy" technique in subsequent sections of this paper.
Study Population
Included in this study were consecutive subjects 18 years and above with mesioangularly or horizontally IMTMs, who required surgical extraction and provided written consent to the study. Eligible subjects were those without any significant systemic diseases (American Society of Anesthesiologists (ASA) physical status class I) with a full complement of teeth in the quadrant of interest and presence of at least a radiological marker (periapical radiograph or orthopantomograph) suggesting an intimate relationship between IMTM teeth and the IAN as described by Rood and Sheehab criteria [15].
Ethics
This study was approved by the institutional Health Research and Ethics Committee ADM/DCST/HREC/APP/1307, and written informed consent was obtained from the participants.
Study Procedures
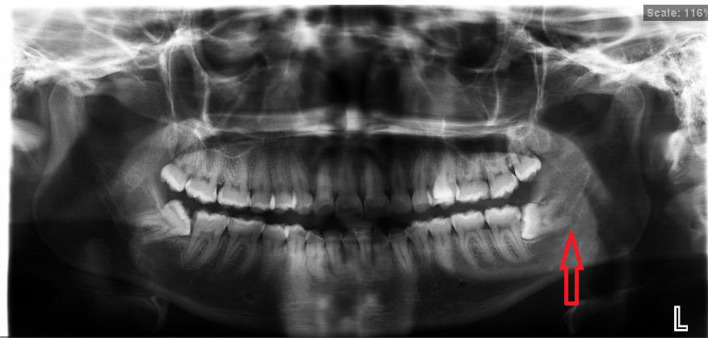
Clinical examination of the oral cavity was conducted for all subjects to evaluate teeth present, supernumerary teeth, eruptive state and type of the mandibular third molars. All subjects had an orthopantomograph (OPG) of the jaws (Fig. 1). Furthermore, periapical radiograph(s) and OPG of the area were also taken pre-operatively and post-surgery (Fig. 2) and kept for follow-up comparison. The type of impaction (winters classification), the morphology of the root (conical, club or divergent) and the relationship of the IMTM root with inferior dental canal according to Rood and Shehab [15] criteria were assessed and documented.
Fig. 1.
OPG of the left impacted mandibular third molar tooth with the mesial root within the Inferior Dental Canal
Fig. 2.
OPG of same tooth after partial coronectomy showing the clearance of the apex of the mesial root of the left impacted mandibular third molar tooth from the inferior dental canal
Randomisation
Subjects were randomised into 2 groups: Group A—control (one-stage technique) and Group B—study group (partial coronectomy technique), using computer-generated randomisation software. The unit of randomisation was each tooth. The allocated sequence was kept by a third party (assigned nurse) and concealed from both the operator and subject until surgery time.
Surgical Techniques
All surgeries were performed by a single surgeon (AOO). Anaesthesia of the area was achieved for the two groups through inferior alveolar, lingual nerve and buccal nerves block using 2% lignocaine hydrochloride in 1:80,000 adrenaline.
For participants in Group A, one-stage complete surgical extraction using the technique described by Leung et al. [16] was performed, and for those in Group B, the two-stage partial coronectomy using the procedure described by Landi et al. [14] was also performed. During extraction of the mesial aspect of the crown, care was taken to avoid pulpal exposure. Exposure of the pulp was considered a failed partial coronectomy. Subsequent extraction of residual crown and root complex was performed after adequate migration away from the mandibular canal was achieved.
The surgical wounds were thoroughly debrided and irrigated with saline and closed primarily with 3.0 black silk suture. Postoperative instructions were given, and subjects commenced warm saline mouth-rinse 6 times daily 24 h after the surgery. In addition, subjects were placed on Ibuprofen Tablets (Ketovail, May and Baker, Nig Plc.) 400 mg, 8 hourly for 3 days, Amoxicillin capsules (Glaxo SmithKline, Nig Plc.) 500 mg 8-hourly for 5 days and 0.2% chlorhexidine mouth-rinse 10mls twice a day for 10 days.
Follow-Up Protocol
All participants were recalled one week postoperatively at the clinic for sutures removal and follow-up review, including subjective and objective assessments for subjects who presented with IAN injury.
For participants in Group B, a monthly examination was scheduled for the first 3 months. At 3 months, a new periapical x-ray and OPG were taken to assess the degree of migration of the IMTMs. Follow-up reviews of the subject continued with radiographic assessment monthly until 12 months or till the tooth was adjudged to be risk-free. Once the tooth migration was assessed to be adequate for a risk-free extraction, the surgical removal of the impacted tooth was carried out in the second stage.
Measurement of Outcomes
The outcome of the study was the presence of IAN neurosensory deficit. This could be in the form of anaesthesia (total loss of sensation); hypoaesthesia (decreased sensitivity to stimulation); paraesthesia (abnormal sensation, spontaneous or evoked); dysaesthesia (unpleasant abnormal sensation, spontaneous or evoked) or hyperaesthesia (increased sensitivity to stimulation) at one week, 3, 6 and 12 months. Postoperative pain on days 1, 3 and 7 was assessed as a secondary outcome in both groups. Pain was recorded on a visual analogue scale (VAS) ranging from 0 to 10, with 0 indicating the absence of any pain sensation and 10 the most severe pain sensation ever experienced by the participant.
Assessment of Neurosensory Deficits
Neurosensory deficit was assessed as the presence or absence of altered sensation (self-reported and objectively assessed) or reduced areas of numbness in the affected site compared to those recorded as a baseline. Subjective assessments were self-reported sensory changes by the subjects. Those who reported numbness or altered sensation of the lip and or gums were further examined objectively to assess the extent of the damage by standard assessment of light touch, pinprick and 2-point discrimination. Light touch test was assessed with a small cotton wisp, and pinprick sensation test was elicited with a dental probe and two-point discrimination, measured with a calliper [16]. Inferior alveolar nerve deficit was considered present, if the subjective and objective measurements are different from those on the unaffected side of the pre-operative baseline. Evaluation of nerve function was repeated after 7 days postoperatively at 3, 6, 12 months for recovery.
Data Analysis
Data were analysed using the statistical package for social sciences (SPSS) for Windows (version 20.0, Chicago, IL, USA). Descriptive statistics were used as appropriate. The chi-square test was used to examine whether there were differences between the 2 groups in terms of the incidence of neurosensory deficit. Univariable and multivariable logistic regression models were used to assess the relationships between the incidence of IAN neurosensory deficit with age, sex, weight, type of impaction (mesioangular vs horizontal impaction), surgical difficulty (measured using Pedersen’s index), duration of operation (in minutes) and root morphology. Pain scores on days 1, 3 and 7 were analysed using mean scores, standard deviations, medians and interquartile ranges and illustrated on boxplots. Univariable logistic regression models were also used to analyse the pain scores (independent variables) by study groups (dependent outcome variable). P-value of < 0.05 was considered statistically significant.
Results
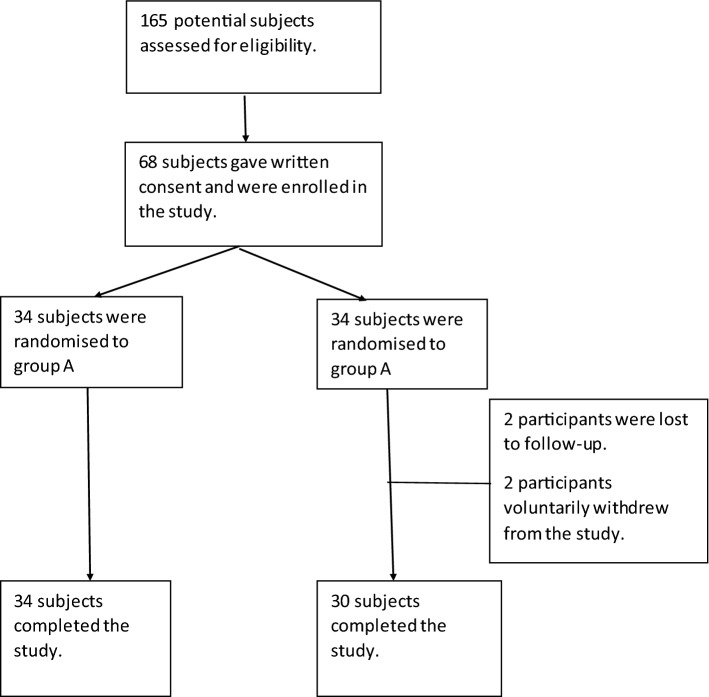
A total of 68 subjects who satisfied the inclusion criteria participated in the study, with 34 subjects randomised to each group (Fig. 3). A drop-out rate of 5.9% (n = 4) was observed in the study, with 2 participants lost to follow-up and 2 voluntarily withdrawing before the 6th month of follow-up. No case of pulpal exposure (failed partial coronectomy) was recorded during the first stage.
Fig. 3.
Flow chart of study subjects
Demographic Information
There were 33 (48.5%) males and 35 (51.5%) females with a male-to-female ratio of 1:1.1. The age range of subjects in the study was 18–57 years, with a mean age of 28.07 years (± 8.37). The mean age of subjects in group A was 29.6 ± 17.4 years (range, 18–57 years), while group B was 27.2 ± 6.7 years (range, 18–51 years). Mesioangular and horizontal impactions accounted for 46 (67.6%) and 22 (32.4%) respectively (Table 1).
Table 1.
Comparison of pre-operative variables between group A and B
| Variables | Control n = 34 (%) | Case n = 34 (%) | p-Value |
|---|---|---|---|
| Age (in years) | |||
| Mean (SD) | 29.59 (9.27) | 26.56 (7.18) | 0.14 |
| Gender | |||
| Male | 17 (50.0) | 16 (47.0) | 0.81 |
| Female | 17 (50.0) | 18 (53.0) | |
| Type of impaction | |||
| Mesioangular | 25 (73.5) | 21 (61.8) | 0.44 |
| Horizontal | 9 (26.5) | 13 (38.2) | |
| Position of Impaction§ | |||
| A | 10 (29.4) | 2 (5.9) | 0.01 |
| B | 19 (55.9) | 32 (94.1) | |
| C | 5 (14.7) | 0 (0) | |
| Class of Impaction§ | |||
| I | 1 (2.9) | 2 (5.9) | 0.79 |
| II | 29 (85.3) | 29 (85.3) | |
| III | 4 (11.8) | 3 (8.8) | |
| Morphology of root | |||
| Conical | 2 (5.9) | 4 (11.8) | |
| Club | 12 (35.3) | 7 (20.6) | 0.33 |
| Divergent | 20 (58.8) | 23 (67.6) | |
| Relationship of root with IAN canal | |||
| Deflection of the roots | 2 (5.9) | 2 (5.9) | 0.19 |
| Narrowing of the roots | 3 (8.8) | 1 (2.9) | |
| Darkening of roots | 12 (35.3) | 11 (32.4) | |
| Deviation of the canal | 4 (11.8) | 2 (5.9) | |
| Loss of tramelines of the canal | 12 (35.3) | 12 (35.3) | |
| Narrowing of the canal | 1 (2.9) | 6 (17.6) | |
| Duration of migration (in months) | |||
| Mean duration of root migration (range) | 6 (4–9) | ||
| Median duration of root migration (IQR) | 6 (6–8) | ||
§Position of impaction (A, B, C) and Class of Impaction (I, II, III) were based on Pell and Gregory’s classification
Recurrent pericoronitis 35 (51.5%) accounted for the major reason for extraction. Table 1 shows the comparison of pre-operative variables between group A and B. Similarly, the difference in the relationships of the roots of the IMTM with the inferior dental canal between the 2 groups was not statistically significant (p > 0.05).
The most common radiographic sign demonstrating the proximity of the IMTM roots to the IAN canal were darkening and the loss of tramline, which accounted for the majority with 35.3%, respectively, in group A, and 32.4 and 38.2% respectively, in group B p = 0.10) (Table 1). Regarding the root morphology of the IMTMs, divergent roots accounted for 63.2%, closely followed by club roots (27.9%) and conical root (8.8%). There was no statistically significant difference in the morphology of the roots between the two groups (p: 0.33).
Neurosensory Deficits
Neurosensory deficit of IAN in the form of altered sensation was observed in 7.8% (n = 5) of the study population. All 5 subjects with neurosensory deficit were observed in group A, and there was a statistically significant difference in the incidence of IAN neurosensory deficit between the two groups (p = 0.03) (Table 2).
Table 2.
Chi2 analysis assessing the relationship between surgical technique (one-stage vs two-stage) and incidence of neurosensory deficit
| Variables | One-stage n (%) | Two-stage n (%) | X2 | p-Value |
|---|---|---|---|---|
| 34 (100) | 30 (100) | |||
| Neurosensory deficit present | 5 (14.7) | 0 (0) | 4.79 | 0.03* |
| Neurosensory deficit absent | 29 (85.3) | 30 (100) |
*p-Value < 0.05
Table 3 shows a univariable and multivariable logistic regression model. Age, sex, weight, type of impaction, surgical difficulty, operation time and root morphology were not significantly associated with the onset of neurosensory deficit. However, there was increased odds for every 1 kg increase in weight in study participants (OR: 1.06; 95% CI: 1.00, 1.12; p: 0.04). On the multivariable logistic regression model, only weight remained significantly associated with the onset of a neurosensory deficit in participants after adjusting for age, sex, type of impaction, surgical difficulty and operation time (OR: 1.30; 95% CI: 1.03,1.62; p: 0.03).
Table 3.
Logistic regression demonstrating association between surgical technique and incidence of neurosensory deficit after adjusting for demographic and operative factors
| Variables | OR [95% CI] | p-Value | aOR [95% CI] | p-Value |
|---|---|---|---|---|
| Age | 0.92 [0.78, 1.07] | 0.29 | 0.74 [0.54, 1.02] | 0.07 |
| Gender | ||||
| Female | 1 [reference] | 1 [reference] | ||
| Male | 0.56 [0.09, 3.62] | 0.55 | 0.01 [0.00, 8.42] | 0.19 |
| Weight (in Kg) | 1.06 [1.00, 1.12] | 0.04* | 1.30 [1.03, 1.62] | 0.03* |
| Type of impaction | ||||
| Mesioangular | 1 [reference] | 1 [reference] | ||
| Horizontal | 1.79 [0.27, 11.73] | 0.54 | 2.08 [0.05, 79.09] | 0.69 |
| Surgical difficulty (Pederson’s index) | 1.77 [0.63, 4.95] | 0.28 | 2.20 [0.16, 29.92] | 0.55 |
| Duration of Operation (in minutes) | 1.03 [0.99, 1.07] | 0.16 | 1.06 [0.97, 1.15] | 0.18 |
| Morphology of root | ||||
| Conical shaped | 1 [reference] | |||
| Club shaped | 0.42 [0.04, 4.82] | 0.48 | ||
| Divergent roots | 0.28 [0.02, 5.27] | 0.39 | ||
OR Odds ratio, aOR adjusted odds ratio; adjusted for age, sex, weight, type of impaction, surgical difficulty (1–7), and duration of operation, 95% CI 95% confidence interval
*p-Value < 0.05
Pain
Using the VAS scale, the mean pain score for postoperative days 1, 3 and 7 in the partial coronectomy group was 4.27 [SD, 1.78], 2.57 [SD, 1.52] and 0.63 [SD, 0.76] compared to the complete extraction group with scores 4.06 [SD, 1.56], 2.44 [SD, 1.21], 0.53 [SD, 0.71] (Table 4). This demonstrates slightly higher mean pain scores in the partial coronectomy group compared with the one-stage complete extraction group. However, there was no statistically significant difference in pain scores between both study groups (Table 4).
Table 4.
Descriptive analysis of pain VAS scores and Univariable logistic regression of Pain scores by Study group
| One-stage complete extraction n (%) | Two-stage Coronectomy n (%) | |
|---|---|---|
| Day 1 | ||
| Mean pain score [± SD] | 4.06 [± 1.56] | 4.27 [± 1.78] |
| Median pain score [IQR] | 4.00 [3–5] | 4.00 [3–6] |
| Day 2 | ||
| Mean pain score [± SD] | 2.44 [± 1.21] | 2.57 [± 1.52] |
| Median pain score [IQR] | 2.00 [2–3] | 2.00 [1–4] |
| Day 3 | ||
| Mean pain score [± SD] | 0.53 [± 0.71] | 0.63 [± 0.76] |
| Median pain score [IQR] | 0.00 [0–1] | 0.00 [0–1] |
| Univariable logistic regression of Pain scores by Study group | ||
|---|---|---|
| OR [95% CI] | p Value | |
| Pain Day 1 | 1.06 [0.75, 1.49] | 0.75 |
| Pain Day 3 | 0.98 [0.61, 1.59] | 0.95 |
| Pain Day 7 | 1.18 [0.51, 2.75] | 0.70 |
SD Standard deviation, IQR interquartile range [25–75%], 95% CI 95% confidence interval
The mean duration to the second extraction for subjects in Group B was 6 months (range, 4–9 months). Three cases were extracted without ostectomy after migration (Table 1).
Discussion
The findings from this study suggest a lower incidence of IAN neurosensory deficit following partial coronectomy compared with a one-stage complete surgical extraction. Our findings validate the case series reported by Landi et al. [14], who first described this novel approach (now called partial coronectomy) to extracting IMTMs with intimate contact with the mandibular canal. Further, systematic reviews and meta-analysis studies [9, 17–19] all corroborate the effectiveness of the coronectomy procedure in reducing the risk of a neurosensory deficit from IAN injury compared with a complete surgical extraction. The advantage of partial coronectomy over complete extraction can be explained by the eruption of the root away from the nerve during the interval between the first and second operation, thereby reducing the potential of nerve injury during the second operation [12].
An overall incidence of 7.8% was recorded in the current study, with all cases of neurosensory deficit (14.7%) identified in the one-stage complete surgical extraction group. Our findings agree with other studies that report no incidence of IAN injury with partial or total coronectomy [12, 14, 20] and between 5 and 19% in cases of complete surgical extraction [12, 16]. In addition, our reported rate of IAN injury is higher than prior literature from Nigeria (2.6%) [8]. This relatively high incidence may be due to the inclusion of only mandibular third molars with an intimate relationship with the IAN in this study. Further, all cases of IAN injury in the current study presented with a transient postsurgical IAN neurosensory deficit, possibly due to apical pressure during surgery on the IAN, resulting in neuropraxia [12]. Thus, our findings corroborate the current literature that staged coronectomy (total and partial) surgical technique may be a safer surgical alternative to complete extraction when the roots of the IMTM are in an intimate relationship with the IAN nerve.
Several authors [9, 21] have reported an increased risk of nerve injury with increased depth of impaction of mandibular third molars. Nonetheless, the current study found no significant association between type and depth of impaction, as well as the pre-operative assessment of surgical difficulty with the onset of IAN injury. On the other hand, we observed that weight was a significant factor in predicting IAN injury after the one-stage complete surgical extraction. Participants with higher body weight had increased odds of developing neurosensory deficit from IAN injury after surgical extraction. Prior studies have linked increased weight to more difficult surgical procedures [22, 23]. This difficulty may be due to the reduced visibility of the surgical area in overweight patients due to excess soft tissue. The reduced visibility due to excess tissue may, in turn, result in iatrogenic nerve damage intraoperatively.
About 10–20% of cases who have coronectomy done experience pain in the first week [6]. Our findings on the effect of coronectomy on postoperative pain detail similar pain levels on days 1, 3 and 7, compared with one-stage complete extraction. These findings are similar to Long et al. [19], who reported that the risk ratios of pain at one week after surgery were similar between coronectomy and complete extraction. Other studies [17] have also demonstrated increased pain in patients who had coronectomy compared to those with complete extraction. On the other hand, Leung et al. [16] stated in a randomised trial that fewer subjects complained of pain in the coronectomy group than in the control group. These contradictory findings were corroborated by other authors [7, 12]. Further, none of the studies reported statistically significant differences in pain levels between the coronectomy and complete extraction groups [7, 12, 16]. The diverse findings reported in the studies above may be influenced by the mean age of participants and the use of antibiotics in the study population [19]. Antibiotic use can reduce the discomfort associated with postoperative inflammation and pain following surgical extraction of IMTMs [1].
A limitation of this study was the use of 2-dimensional (2D) imaging techniques (panoramic and periapical radiographs), which hampered a more objective assessment of the relationships of the roots of the IMTM with the inferior dental canal. Nonetheless, the 2D views provided a reasonable assessment and may be a valuable option in centres where 3-dimensional (3D) imaging tools such as Computed Tomography (CT) and Cone Beam Computed Tomography (CBCT) are not accessible, as in most settings in Nigeria. The current study validates the effectiveness of the novel surgical approach described by Landi et al. [14] and suggests the superiority of partial coronectomy over complete surgical extraction in cases of intimate contact between the IMTM roots and the IAN canal. Partial coronectomy may also reduce operating time and preserve the pulp chamber during the first stage, compared to total coronectomy (partial odontectomy) [12, 13, 16, 20, 24, 25].
Conclusion
This study shows that two-stage partial coronectomy of IMTMs was associated with a lower incidence of IAN injury when compared with the one-stage complete extraction technique. Postoperative pain was not significantly different on days 1, 3 and 7 between the partial coronectomy and complete extraction groups. Therefore, partial coronectomy may be considered an alternative to complete one-stage in cases where the IMTMs are in intimate contact with the IAN canal, and the nerve is at risk of injury during surgical extraction. Further studies using a CBCT may investigate the degree of migration of the root complex over prolonged periods beyond 12 months following total compared with partial coronectomy.
Funding
This research was funded through the TETFund Institutional-based Research Grant, University of Lagos (2015).
Availability of Data and Material (Data Transparency)
Data and manuscript material available.
Declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethics Approval
This study was approved by the Lagos University Teaching Hospital Health Research and Ethics Committee (ADM/DCST/HREC/APP/1307), and written informed consent was obtained from the participants.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Renton T. Surgical management of third molars. In: Andersson L, Kahnberg K-E, Pogrel MA, editors. Oral and maxillofacial surgery. 13. West Sussex: Wiley-Blackwell; 2010. pp. 219–254. [Google Scholar]
- 2.Susarla SM, Blaeser BF, Magalnick D. Third molar surgery and associated complications. Oral Maxillofac Surg Clin North Am. 2003;15(2):177–186. doi: 10.1016/S1042-3699(02)00102-4. [DOI] [PubMed] [Google Scholar]
- 3.Adeyemi MO, James O, Lawal AO, Fadeyibi SO. Iatrogenic displacement of impacted mandibular third molar into the submandibular space complicated by submasseteric abscess. Afr J Trauma. 2016;5:19–22. doi: 10.4103/1597-1112.192845. [DOI] [Google Scholar]
- 4.Blondeau F, Daniel NG. Extraction of impacted mandibular third molars: postoperative complications and their risk factors. J Can Dent Assoc. 2007;73(4):325–235e. [PubMed] [Google Scholar]
- 5.Valmaseda-Castellón E, Berini-Aytés L, Gay-Escoda C. Lingual nerve damage after third lower molar surgical extraction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90(5):567–573. doi: 10.1067/moe.2000.110034. [DOI] [PubMed] [Google Scholar]
- 6.Martin A, Perinetti G, Costantinides F, Maglione M. Coronectomy as a surgical approach to impacted mandibular third molars: a systematic review. Head Face Med. 2015;11:9. doi: 10.1186/s13005-015-0068-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cheung LK, Leung YY, Chow LK, Wong MCM, Chan EKK, Fok YH. Incidence of neurosensory deficits and recovery after lower third molar surgery: a prospective clinical study of 4338 cases. Int J Oral Maxillofac Surg. 2010;39(4):320–326. doi: 10.1016/j.ijom.2009.11.010. [DOI] [PubMed] [Google Scholar]
- 8.Olojede A, Gbotolorun O, Adeyemo W, Arotiba G, Akinwande J, Ladeinde A. Sensory nerve injury following impacted mandibular third molar extraction. Niger Dent J. 2008;16(1):10–13. [Google Scholar]
- 9.Leung YY, Cheung LK. Risk factors of neurosensory deficits in lower third molar surgery: A literature review of prospective studies. Int J Oral Maxillofac Surg. 2011;40(1):1–10. doi: 10.1016/j.ijom.2010.09.005. [DOI] [PubMed] [Google Scholar]
- 10.Renton T. Oral surgery: part 4 . Minimising and managing nerve injuries and other complications. Br Dent J. 2013;215(8):393–9. PMID: 24157759. 10.1038/sj.bdj.2013.993 [DOI] [PubMed]
- 11.Bonetti GA, Bendandi M, Laino L, Checchi V, Checchi L. Orthodontic Extraction: The Riskless Extraction Of the Impacted Lower Third Molars Close to the Mandibular Canal. J Oral Maxillofac Surg. 2007;65:2580–6. PMID: 18022488. 10.1016/j.joms.2007.06.686 [DOI] [PubMed]
- 12.Renton T, Hankins M, Sproate C, McGurk M. A randomised controlled clinical trial to compare the incidence of injury to the inferior alveolar nerve as a result of coronectomy and removal of mandibular third molars. Br J Oral Maxillofac Surg. 2005;43(1):7–12. PMID: 15620767. 10.1016/j.bjoms.2004.09.002 [DOI] [PubMed]
- 13.Pedersen MH, Bak J, Matzen LH, Hartlev J, Bindslev J, Schou S, Nørholt SE. Coronectomy of mandibular third molars: a clinical and radiological study of 231 cases with a mean follow-up period of 5.7 years. Int. J. Oral Maxillofac. Surg. 2018;47: 1596–1603. [DOI] [PubMed]
- 14.Landi L, Manicone PF, Piccinelli S, Raia A, Raia R. A Novel Surgical Approach to Impacted Mandibular Third Molars to Reduce the Risk of Paresthesia: A Case Series. J Oral Maxillofac Surg. 2010;68(5):969–74. PMID: 20156664. 10.1016/j.joms.2009.09.097 [DOI] [PubMed]
- 15.Rood JP, Shehab BA. The radiological prediction of inferior alveolar nerve injury during third molar surgery. Br J Oral Maxillofac Surg. 1990;28(1):20–5. PMID: 2322523. 10.1016/0266-4356(90)90005-6 [DOI] [PubMed]
- 16.Leung YY, Cheung LK. Safety of coronectomy versus excision of wisdom teeth: A randomised controlled trial. Oral Surgery, Oral Med Oral Pathol Oral Radiol Endodontology. 2009;108(6):821–7. PMID: 19782621. 10.1016/j.tripleo.2009.07.004 [DOI] [PubMed]
- 17.Cervera-Espert J, Pérez-Martínez S, Cervera-Ballester J, Peñarrocha-Oltra D, Peñarrocha-Diago M. Coronectomy of impacted mandibular third molars: a meta-analysis and systematic review of the literature. Med Oral Patol Oral Cir Bucal. 2016;21(4):e505–e513. doi: 10.4317/medoral.21074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pitros P, O'Connor N, Tryfonos A, Lopes V. A systematic review of the complications of high-risk third molar removal and coronectomy: development of a decision tree model and preliminary health economic analysis to assist in treatment planning. Br J Oral Maxillofac Surg. 2020;58(9):e16–e24. doi: 10.1016/j.bjoms.2020.07.015. [DOI] [PubMed] [Google Scholar]
- 19.Long H, Zhou Y, Liao L, Pyakurel U, Wang Y and Lai W. Coronectomy vs. Total Removal for Third Molar Extraction: A Systematic Review. J Dent Res 2012; 91(7):659–665 [DOI] [PubMed]
- 20.Monaco G, de Santis G, Gatto MRA, Corinaldesi G, Marchetti C. Coronectomy. JADA. 2012;143(4):363–369. doi: 10.14219/jada.archive.2012.0178. [DOI] [PubMed] [Google Scholar]
- 21.Jerjes W, Swinson B, Moles DR, El-Maaytah M, Banu B, Upile T, et al. Permanent sensory nerve impairment following third molar surgery: a prospective study. Oral Surgery, Oral Med Oral Pathol Oral Radiol Endodontology. 2006;102(4):e1–7. doi: 10.1016/j.tripleo.2006.01.016. [DOI] [PubMed] [Google Scholar]
- 22.Gbotolorun OM, Arotiba GT, Ladeinde AL. Assessment of factors associated with surgical difficulty in impacted mandibular third molar extraction. J Oral Maxillofac Surg. 2007;65(10):1977–1983. doi: 10.1016/j.joms.2006.11.030. [DOI] [PubMed] [Google Scholar]
- 23.Susarla SM, Dodson TB. Estimating Third Molar Extraction Difficulty: A Comparison of Subjective and Objective Factors. J Oral Maxillofac Surg. 2005;63:427–434. doi: 10.1016/j.joms.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 24.Garcia-Garcia A. Coronectomy: a questionable procedure. J Oral Maxillofac Surg. 2005;63:723–725. doi: 10.1016/j.joms.2005.01.013. [DOI] [PubMed] [Google Scholar]
- 25.Pogrel MA, Lee JS, Muff DF. Coronectomy: a technique to protect the inferior alveolar nerve. J Oral Maxillofac Surg. 2004;62(12):1447–1452. doi: 10.1016/j.joms.2004.08.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data and manuscript material available.