Abstract
Background
The oral cavity is a unique environment where wound healing needs to occur in the presence of heavily contaminated oral fluid often leading to infections at the suture site. Topical antimicrobial agents have proven to be effective in controlling intraoral infections. One such antimicrobial combination is Metronidazole-Chlorhexidine which has commonly been used to treat oral ulcers and gingival inflammation; however, there are no studies of its use in the healing of oral incisions.
Methodology
This split-mouth study comprised of 15 participants who received 30 intraoral incisions. Incisions were placed either simultaneously (Group 1) or at spaced intervals (Group 2) for various minor and major surgical procedures. Metronidazole -Chlorhexidine gel was applied to the study sites while the control sites were allowed to heal naturally. Pain, inflammation, and healing were assessed using visual analogue scale and healing index by Landry et al.
Results
The study sites showed better wound healing and decreased postoperative inflammation. There was a statistically significant decrease in post-operative pain in the study site in Group 1 but not in Group 2.
Conclusion
Metronidazole-Chlorhexidine combination gel is a cost-effective, readily available, and safe medicament to improve healing of intraoral incisions and reduce post-operative inflammation and pain.
Keywords: Metronidazole-Chlorhexidine gel, Intraoral incisions, Healing, Pain, Inflammation, Topical antibiotics
Introduction
Oral incisions used in various maxillofacial surgeries are susceptible to contamination due to the presence of saliva, plaque, microbes, and food debris in the oral cavity [1]. Following intraoral incisions for various major and minor surgical procedures, the administration of systemic antibiotics and anti-inflammatory agents is a common practice in oral surgery. However, the use of systemic antibiotics for the prevention of post-operative complications of the surgical site during minor surgical procedure like third molar surgery is also controversial and debated. [2]
Given the difficulty of postoperative oral hygiene maintenance after oral surgery, topical antibiotics are recommended to improve wound healing by reducing plaque buildup and postoperative pain and inflammation. Topical antibiotics also help overcome the demerits of systemic antibiotic therapy such as microbial resistance and side effects of the drug. Various antimicrobial agents, particularly chlorhexidine(CHX) and metronidazole(MTZ), have been studied in the search for an agent that could prevent post-operative infection of oral wounds. [3]
Both CHX and MTZ have shown to be effective against various Gram positive and Gram negative bacteria. CHX, a cationic biguanide has a bactericidal action- [4] increasing the vulnerability of the bacterial cell membrane and changing the protein characteristics, resulting in the dispersion of macromolecules into the cytoplasm and ultimately cell death owing to bacterial cell or fungal lysis [5]. It has a substantivity up to 12 h and is considered the gold standard for plaque control. [1]
MTZ on the other hand is an antibiotic that primarily affects Gram-positive and Gram-negative obligate anaerobes [6]. Anaerobic bacteria degrade metronidazole's nitro group to produce nitroso-containing intermediates. These bind to DNA covalently, cleave spiral DNA strands, inhibit bacterial nucleic acid synthesis, and eventually kill the bacterial cells. It has anti-trichomonal, antimicrobial, anthelmintic, xenobiotic, and anti-amoebic properties [7]. MTZ has excellent oral absorption and bioavailability (> 90%), with tissue concentrations that are generally similar to or slightly lower than serum concentrations. [8]
Although systemic metronidazole has shown good results [9], studies have shown that topical antibiotic therapy using metronidazole and tetracycline is superior in controlling oral infections compared with systemic therapy.
The combination of MTZ and CHX in gel form has been commonly used for oral ulcers and gingival inflammation, there are no studies of its use in the healing of oral incisions. This is the rationale for this study.
Methodology
The study was approved by the institutional ethics committee and was performed in accordance with the ethical standards laid down in the Declaration of Helsinki. Informed consent was obtained for all participants.
This split-mouth case–control study comprised of 15 participants who received 30 intraoral incisions (15 control sites and 15 study sites). The sample size was calculated based on 10% level of significance, 80% power and an effect size of 0.8
The participants included in the study were of the age group 15–50 years, belonging to ASA I and II, requiring more than one intraoral incision either simultaneously or at spaced intervals for one of the following procedures: surgical removal of impacted third molars, open reduction, and internal fixation of maxillofacial trauma, alveoloplasty or orthognathic surgery. Patients with pre-existing lacerations of oral mucosa, extensive soft tissue loss at the surgical site, contaminated wounds, history of chemotherapy or radiation therapy, ASA III and ASA IV, patients on immunosuppressive drugs or drugs that affect healing and pregnant patients were excluded from the study. The participants were divided into two groups- Group 1 (incisions placed simultaneously) and Group 2 (incisions placed at spaced intervals) by convenience sampling. All procedures were performed by a single operator.
In Group 1, the incisions placed on the left side and/or incisions placed in the mandibular mucosa were considered as study sites and received Metrogyl DG gel forte (Chlorhexidine 0.5% W/W + Metronidazole 1.5% W/W) whereas incisions placed on the right side and /or incisions placed in the maxillary vestibule were considered as control sites and were allowed to heal naturally. In Group 2, the incision on the left side was considered the study site and the incision on the right was the control site. Pre-operative and post-operative antibiotics (Cefotaxim IV/PO) and post-operative analgesics (Tab Diclofenac 50 mg TID) and anti-inflammatory drugs (Inj Dexamethasone 8 mg IV) were prescribed when indicated. Group 2 patients received the same medications during both procedures. The objective assessment of soft tissue healing, redness and inflammation was performed by an independent observer who was blinded to the study.
Study site: Metrogyl DG gel forte was applied on the gauze and placed over the sutured intraoral incision for 20 min from the 1st post-op day, three times a day for 5 days.
Control site: No antimicrobial gel was applied to the control site and the sutured incisions were allowed to heal naturally. In Group 1, the control site was covered with gauze to prevent flow of the gel from the study site.
The parameters assessed were:
Pain intensity on day 2, day 5, day 7, and day 15 evaluated by 10 level Visual Analogue Scale (VAS) with the patient placing a mark on the scale to indicate an intensity range which was categorized into four levels: none (0) = 0; mild (1–3) = 1; moderate (4–6) = 2; severe (7–10) = 3.
Soft tissue healing was assessed by the healing index of Landry, Turnbull, and Howley on days 2, 5, 7, and 15 and was categorized into 5 levels: 1 = Very Poor;2 = Poor; 3 = Good; 4 = Very Good; 5 = Excellent.
Redness / Inflammation was marked on day 2, day 5, day 7, day 15 as present or absent for both study and control sites.
Results
Fifteen patients (30 intraoral incisions) were considered for the procedure. Group 1 comprised of 7 patients who received simultaneously placed incisions for open reduction and internal fixation of one or a combination of the following- Mandibular fractures, midface fractures, and zygomatico-maxillary complex fractures or alveoloplasty involving more than one segment. Group 2 comprised of 8 patients who received incisions at the spaced intervals for minor surgical procedures which included surgical removal of the bilateral impacted teeth. Out of the 15 patients, 4 were female and 11 were male with a mean age of 26 years (range 17–42 years).
The data were analyzed using SPSS (Statistical Package for Social Science Program) version 23. Mann Whitney test was done to compare the pain, healing, and inflammation in Group 1 and Group 2.
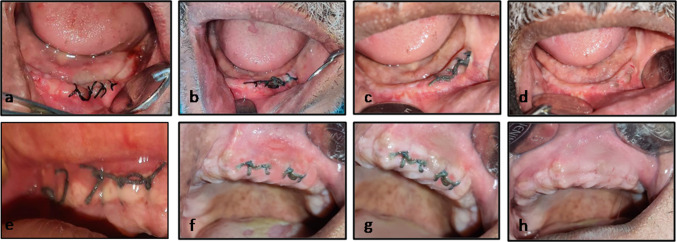
As seen in Table 1, pain on days 2 and 5 in Group 1 showed a lesser mean rank value as compared to the control site whereas by day 7 and 15 both the sites showed a similar mean rank value. Even though healing with a higher mean rank value was noted in the study site on days 2, 5, 7, and 15 (Fig. 1), it was statistically insignificant. Inflammation with a lower mean rank value was noted in the study site on days 2 and 5 while by days 7 and 15 the mean rank value was similar for both the sites deeming it statistically insignificant.
Table 1.
Comparison of Pain, Healing and Inflammation between study and control sites in Group 1
| Parameter | Day | Site (n = 7) | Mean Rank | p value |
|---|---|---|---|---|
| PAIN | Day 2 | Study | 7.00 | 0.710 |
| Control | 8.00 | |||
| Day 5 | Study | 7.00 | 0.710 | |
| Control | 8.00 | |||
| Day 7 | Study | 7.50 | 1.000 | |
| Control | 7.50 | |||
| Day 15 | Study | 7.50 | 1.000 | |
| Control | 7.50 | |||
| HEALING INDEX | Day 2 | Study | 9.50 | 0.073 |
| Control | 5.50 | |||
| Day 5 | Study | 8.50 | 0.383 | |
| Control | 6.50 | |||
| Day 7 | Study | 7.86 | 0.805 | |
| Control | 7.14 | |||
| Day 15 | Study | 8.00 | 0.710 | |
| Control | 7.00 | |||
| INFLAMMATION | Day 2 | Study | 6.00 | 0.209 |
| Control | 9.00 | |||
| Day 5 | Study | 7.00 | 0.710 | |
| Control | 8.00 | |||
| Day 7 | Study | 7.50 | 1.000 | |
| Control | 7.50 | |||
| Day 15 | Study | 7.50 | 1.000 | |
| Control | 7.50 |
p-value based on Mann–Whitney Test. * = Statistically Significant (p < 0.05)
Fig. 1.
Alveoloplasty in a 42-year-old male patient. Fig (a–d) shows the healing and inflammation at the study site noted on days 2,5,7,15 respectively. Fig (e–h) shows the healing and inflammation at the control site noted on days 2, 5,7,15 respectively
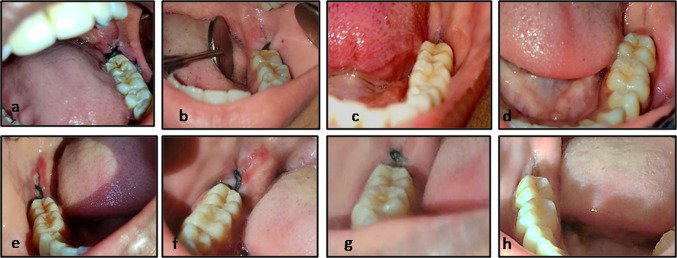
Similarly, Table 2 shows the comparison between sites in Group 2. Statistically, significant pain values were noted in day 2 and day 5 with lesser mean rank values in study sites whereas even though days 7 and 15 showed lesser mean rank values for pain, the values were statistically insignificant. Healing showed higher mean rank value in the study site for all the evaluated days, and inflammation showed a lesser mean rank value on days 2, 5 and 7 with similar values by day 15 (Fig. 2). However, both parameters were not statistically significant.
Table 2.
Comparison of Pain, Healing, and Inflammation between study and control sites in Group 2(Incisions placed at spaced intervals)
| Parameter | Day | Site (n = 8) | Mean Rank | p-value |
|---|---|---|---|---|
| PAIN | Day 2 | Study | 6.00 | 0.038* |
| Control | 11.00 | |||
| Day 5 | Study | 4.94 | 0.001* | |
| Control | 12.06 | |||
| Day 7 | Study | 6.75 | 0.161 | |
| Control | 10.25 | |||
| Day 15 | Study | 8.50 | 1.000 | |
| Control | 8.50 | |||
| HEALING INDEX | Day 2 | Study | 10.50 | 0.105 |
| Control | 6.50 | |||
| Day 5 | Study | 10.25 | 0.161 | |
| Control | 6.75 | |||
| Day 7 | Study | 10.00 | 0.234 | |
| Control | 7.00 | |||
| Day 15 | Study | 9.81 | 0.279 | |
| Control | 7.19 | |||
| INFLAMMATION | Day 2 | Study | 6.50 | 0.105 |
| Control | 10.50 | |||
| Day 5 | Study | 6.50 | 0.105 | |
| Control | 10.50 | |||
| Day 7 | Study | 7.50 | 0.442 | |
| Control | 9.50 | |||
| Day 15 | Study | 8.50 | 1.000 | |
| Control | 8.50 |
p value based on Mann–Whitney Test. * = Statistically Significant (p < 0.05)
Fig. 2.
Surgical extraction of 38 (study) and 48 (control) in a 26-year-old male patient. Fig (a–d) shows the healing and inflammation noted at the study site on days 2,5,7,15 respectively. Fig (e–h) shows the healing and inflammation noted at the control site on days 2, 5,7,15 respectively
Discussion
Wound healing in the oral cavity takes place in a saliva-filled environment harboring a multitude of microorganisms, which is a unique and extraordinary situation [10]. Contamination is a major cause of postoperative wound dehiscence, infection, and discomfort in intraoral wounds. As a result, safeguarding the intraoral wound becomes quite difficult [11]. The wound re-epithelialization process depends on keratinocyte migration, proliferation, and survival. Restoration of an intact epidermal barrier via re-epithelialization—an important aspect of oral healing, may be complicated by infection. [12].
Various methods have been used to control post-operative plaque and pain, and promote healing, such as mouth rinse with chlorhexidine, povidone-iodine solutions, intraoral suctioning, and intraoral dressings such as resopac, coepac, and others. Even though oral and oropharyngeal irrigation has shown to significantly reduce oral bacteria levels, the impact only lasted 3 h. [12] Thus, the use of antimicrobial agents to prevent contamination of oral wounds becomes important to promote and accelerate repair and allow a reduction in the patient’s postoperative discomfort due to pain and edema. [13].
Antimicrobials applied locally seem to attenuate several of the downsides of general antibiotic therapy, like microorganism resistance, superinfections, hypersensitivity, toxicity, and pharmaceutical interactions [13]. Topical antimicrobials deliver high concentration of the drug at reduced doses making them beneficial in orofacial infections. [8]
Bergamaschi et al. (2013) tested metronidazole concentrations in human plasma and saliva after tablet or gel administration and concluded that metronidazole gel had comparable bioavailability in plasma and saliva as metronidazole tablets. [8]
Torres-Lagares et al. (2006) investigated the efficacy of a 0.2 percent CHX gel in the treatment of alveolar osteitis and found a reduced incidence of osteitis by 63.33% [14]. When used in the form of a gel or paste, the product has a longer contact time with the operated area, contributing to more favorable outcomes [15]. However, because of its local adverse effects in the long-term, short- and medium-term therapeutic use should be considered. [16].
The integration of chlorhexidine and metronidazole has shown to be effective in the treatment of dry socket and in periodontal surgery. The CHX and MTZ gel utilized in this study has a higher viscosity compared to the liquid kind, causing the drugs to remain in contact with the tissue for longer and be removed slowly from the mouth, resulting in a superior pharmacotherapeutic impact. [8]
Kaur, J et al. (2017) found that interalveolar administration of a gel containing 0.2 percent chlorhexidine and 10gm metronidazole decreased the incidence of dry socket and adverse reactions following removal of impacted third molars. [9]
Mariano et al. (2015) explored the role of a 2% chlorhexidine and metronidazole paste application on the healing of palatal wounds in rats (n = 27). The combination paste demonstrated clinically promising results in terms of tissue repair. On day 6, the majority of the specimens had histologically premature wound closure. [16].
Perinetti et al. (2004) concluded that subgingival injection of 1% metronidazole gel and 1% chlorhexidine gel significantly reduced periodontopathic microorganisms in cases of chronic periodontitis and could help alleviate persistent pockets. [17].
A meta-analysis by Yusri et al. (2021) concluded that locally delivered antibiotics such as metronidazole and doxycycline, following periodontal surgery resulted in post-surgical improvement in terms of pocket depth, attachment level and bleeding on probing [18]. This was in agreement with the findings of Sander et al. (1994) who reported beneficial effects of locally applied metronidazole gel on healing of vertical periodontal defects following guided tissue regeneration. [19].
In our study, the patients reported less amount of pain at the study site on day 2 and day 5 especially in Group 2 as opposed to the control site, which was statistically significant. Healing observed clinically on day 2 and day 5 in Group 2 was superior at the study sites, however by day 15 both study and control sites showed similar healing. Though clinically less inflammation was seen in the study site on day 2, inflammation at both sites decreased by day 5 in most of the patients and the difference was statistically insignificant. Similarly, in Group 1, despite a clinically evidenced decrease in inflammation and pain and improved healing on day 2 and day 5, the differences were not statistically significant and by days 7 and 15 there was no difference in the parameters in both the sites. The statistically insignificant results in Group 1 could be attributed to the post-operative use of intravenous antibiotics, decreased oral contamination due to nasogastric feeding, intraoral irrigation and the probable saliva mediated transfer of the medicaments in the gel to the control site.
Conclusion
The MTZ-CHX gel improves healing of intraoral incisions and reduces post-operative inflammation and pain in the first five days post-operatively. It also has the advantage of being cost-effective and easily available. The study included systemically healthy individuals with the intention of providing baseline evidence to the scientific community regarding the efficacy of this topical antimicrobial combination in the healing of intraoral incisions. The results may be more conclusive when extended to a larger population, including patients with compromised wound healing. Another limitation of the study is that all the patients received systemic antibiotics following the surgery. Topical application of the test drugs may not provide significant additional benefit when systemic antibiotics are given orally. Further studies comparing topical and systemic antibiotics in patients undergoing oral surgical procedures may indicate whether topical antibiotics can substitute the invariably and often inadvertently prescribed systemic antibiotics for the prevention of post-operative infections.
Funding
Nil.
Declarations
Conflict of interest
The authors have no financial or proprietary interest in any material discussed in this article.
Ethical approval
Obtained from the Yenepoya Ethics Committee-2(YEC2/485), Yenepoya (Deemed to be University). Informed consent obtained for publication of patient data and photographs.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hammad HM, Hammad MM, Abdelhadi IN, Khalifeh MS. Effects of topically applied agents on intra-oral wound healing in a rat model: a clinical and histomorphometric study. Int J Dental Hygiene. 2011;9(1):9–16. doi: 10.1111/j.1601-5037.2009.00410.x. [DOI] [PubMed] [Google Scholar]
- 2.Cervino G, Cicciù M, Biondi A, Bocchieri S, Herford AS, Laino L, Fiorillo L. Antibiotic prophylaxis on third molar extraction: systematic review of recent data. Antibiotics. 2019;8(2):53. doi: 10.3390/antibiotics8020053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.en Bakae GS, Strahan JD. Effects of a 1% chlorhexidine gel during the healing phase after inverse bevel mucogingival flap surgery. J Clin Periodontol. 1980;7:20–5. doi: 10.1111/j.1600-051X.1980.tb01945.x. [DOI] [PubMed] [Google Scholar]
- 4.Denton GW, Chlorhexidine (1991) In: Block SS, ed. disinfection, sterilization, and preservation. philadelphia, Lea, and Febiger, 274–289
- 5.Fiorillo L. Chlorhexidine gel use in the oral district: a systematic review. Gels. 2019;5(2):31. doi: 10.3390/gels5020031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pradeep AR, Kumari M, Priyanka N, Naik SB. Efficacy of chlorhexidine, metronidazole, and combination gel in the treatment of gingivitis–a randomized clinical trial. J Int Acad Periodontol. 2012;14(4):91–96. [PubMed] [Google Scholar]
- 7.National Center for Biotechnology Information. PubChem Compound Summary for CID 4173, Metronidazole. https://pubchem.ncbi.nlm.nih.gov/compound/Metronidazole.
- 8.De C, Bergamaschi C, Berto LA, Venâncio PC, Cogo K, Franz-Montan M, Motta RH, Santamaria MP, Groppo FC. Concentrations of metronidazole in human plasma and saliva after tablet or gel administration. J Pharm Pharmacol. 2014;66(1):40–47. doi: 10.1111/jphp.12161. [DOI] [PubMed] [Google Scholar]
- 9.Kaur J, Raval R, Bansal A, Kumawat V. Repercussions of interalveolar placement of a combination of 0.2% chlorhexidine & 10 Mg metronidazole gel on the occurrence of dry sockets- A randomized control trial. J Clin Exp Dent. 2017;9(2):e284–e288. doi: 10.4317/jced.53262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shah R, Domah F, Shah N, Domah J. Surgical wound healing in the oral cavity: a review. Dent Update. 2020;47(2):135–143. doi: 10.12968/denu.2020.47.2.135. [DOI] [Google Scholar]
- 11.Raghavan SL, Panneerselvam E, Mudigonda SK, Raja KKVB. Protection of an intraoral surgical wound with a new dressing: a randomised controlled clinical trial. Br J Oral Maxillofac Surg. 2020;58(7):766–770. doi: 10.1016/j.bjoms.2020.03.017. [DOI] [PubMed] [Google Scholar]
- 12.Bhattacharya R, Xu F, Dong G, Li S, Tian C, Ponugoti B, Graves DT. Effect of bacteria on the wound healing behavior of oral epithelial cells. PLoS ONE. 2014;9(2):e89475. doi: 10.1371/journal.pone.0089475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Funahara M, Yamamoto S, Ueda M, Suzuki T, Ota Y, Nishimaki F, et al. Prevention of surgical site infection after oral cancer surgery by topical tetracycline: Results of a multicenter randomized control trial. Medicine. 2017;96(48):e8891. doi: 10.1097/MD.0000000000008891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Torres-Lagares D, Gutierrez-Perez JL, Infante-Cossio P, Garcia-Calderon M, Romero-Ruiz MM, Serrera-Figallo MA. Randomized, double-blind study on the effectiveness of intra-alveolar chlorhexidine gel in reducing the incidence of alveolar osteitis in mandibular third molar surgery. Int J Oral Maxillofac Surg. 2006;35:348–351. doi: 10.1016/j.ijom.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 15.da Silveira TD, de Figueiredo MA, Cherubini K, de Oliveira SD, Salum FG. The topical effect of chlorhexidine and povidone-iodine in the repair of oral wounds. A review Stomatologija. 2019;21(2):35–41. [PubMed] [Google Scholar]
- 16.Mariano RC, Oliveira MR, Silva LC, Ferreira S, Garcia Júnior IR, de Carvalho SA. Effect of topical application of chlorhexidine and metronidazole on the tissue repair of palatal wounds of rats: a clinical and histomorphometric study. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015;119(5):505–513. doi: 10.1016/j.oooo.2014.12.023. [DOI] [PubMed] [Google Scholar]
- 17.Perinetti G, Paolantonio M, Cordella C, D'Ercole S, Serra E, Piccolomini R. Clinical and microbiological effects of subgingival administration of two active gels on persistent pockets of chronic periodontitis patients. J Clin Periodontol. 2004;31(4):273–281. doi: 10.1111/j.1600-051x.2004.00481. [DOI] [PubMed] [Google Scholar]
- 18.Yusri S, Elfana A, Elbattawy W, Fawzy El-Sayed KM. Effect of locally delivered adjunctive antibiotics during surgical periodontal therapy: a systematic review and meta-analysis. Clin Oral Investig. 2021;25(9):5127–5138. doi: 10.1007/s00784-021-04056-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sander L, Frandsen EV, Arnbjerg D, Warrer K, Karring T. Effect of local metronidazole application on periodontal healing following guided tissue regeneration. Clinical findings J Periodontol. 1994;65(10):914–920. doi: 10.1902/jop.1994.65.10.914. [DOI] [PubMed] [Google Scholar]