Abstract
Aim: We examined the association between the carotid intima medica thickness (cIMT) and risk factors for atherosclerosis based on the Japan Atherosclerosis Society 2022 Atherosclerosis Prevention Guideline.
Methods: Using data from the Tohoku Medical Megabank Community-based Cohort Study, we performed a cross-sectional study that enrolled 13,366 participants (age ≥ 20 years) with an analysis of covariance to assess associations between cIMT and risk factors for atherosclerosis. The maximum common carotid artery was measured using high-resolution B-mode ultrasound. Analysis was conducted in the model adjusted for age, sex, smoking status, drinking status, body mass index (BMI), systolic blood pressure (SBP), glycated hemoglobin (HbA1c), high-density lipoprotein-cholesterol (HDL-C), non-high-density lipoprotein-cholesterol (non-HDL-C), and height.
Results: In this study cohort, the average age and cIMT were 57.3 (13.8) years and 0.61 (0.13) mm, respectively, which included 3,988 males (29.8%). Males had a higher cIMT than did the females. Age, height, BMI, SBP, HbA1c, and non-HDL-C were positively associated with cIMT. HDL-C was inversely associated with cIMT. Compared with never drinkers, current drinkers (≥ 46.0 g/day) had a significantly decreased cIMT.
Conclusions: The cIMT was associated with atherosclerosis risk factors including age, sex, BMI, SBP, HbA1c, non-HDL-C, and HDL-C, and adequate control of risks in high-risk individuals might be required to prevent atherosclerotic cardiovascular diseases.
Keywords: Atherosclerosis, Carotid intima media thickness, Risk factor, Epidemiology
Introduction
The 2022 Japan Atherosclerosis Society (JAS) Guideline for Prevention of Atherosclerotic Cardiovascular Diseases indicated several risk factors for atherosclerosis, such as aging, smoking, dyslipidemia, hypertension, and diabetes 1) . In the JAS guideline, intima media thickness (IMT) is shown as one of the methods to assess subclinical atherosclerosis to prevent atherosclerotic cardiovascular disease (CVD) 1) . Carotid intima media thickness (cIMT) is not only a strong predictor of future CVD but is also associated with atherosclerosis risk factors 2 - 14) . Previous studies in Japan showed that cIMT was associated with age, body mass index (BMI), systolic blood pressure (SBP), fasting blood glucose, smoking, total cholesterol (TC), and high-density lipoprotein-cholesterol (HDL-C) 4 , 7) . In addition, cIMT has been shown to be mainly affected by age and blood pressure 3 , 6) . However, previous studies had limited sample sizes, and large population studies are required to better understand the contribution of atherosclerotic risk factors in cIMT.
The Tohoku Medical Megabank (TMM) Project conducted by the Tohoku University Tohoku Medical Megabank Organization and Iwate Medical University Iwate Tohoku Medical Megabank Organization has been launched to realize creative reconstruction and to solve medical problems in the aftermath of the Great East Japan Earthquake (GEJE) 15) . In this project, we established two large-scale prospective cohorts: the TMM Birth and Three-Generation Cohort Study 16) , and the TMM Community-based Cohort Study (TMM CommCohort Study) 17) . In these studies, we obtained and analyzed data on lifestyle, blood, and urinary parameters. For some participants, we conducted further detailed measurements, including cIMT.
The large data set obtained from the abovementioned studies has enabled a detailed reconfirmation of the relationship between risk factors for atherosclerosis, which was proposed by the JAS Guideline for Prevention of Atherosclerotic Cardiovascular Diseases, and cIMT 1) . Moreover, the data from these studies have facilitated a comparison of the attribution of risk factors for cIMT.
Aim
We examined the association between cIMT and the risk factors for atherosclerosis, including age, sex, BMI, SBP, non-HDL-C, HDL-C, glycated hemoglobin (HbA1c), and smoking status in a Japanese population.
Methods
Study Design and Population
We conducted a cross-sectional study using data from the TMM CommCohort Study, which has been described elsewhere 15 , 17) . It assessed the long-term impact of GEJE on disaster victims and genomic and omics research that lead to the implementation of personalized healthcare and medicine in the affected area in the near future for which many genomic and epidemiological studies have been conducted 15 - 26) . The source population for the survey comprised males and females aged ≥ 20 years who were living in Miyagi prefecture, in northeastern Japan. All participants were recruited between May 2013 and March 2016 using the following three approaches. The Type 1 survey (40,433 participants) was conducted in specific municipal health check-up sites. The Type 1 additional survey (664 participants) was conducted on different dates during specific municipal health check-ups. The Type 2 survey (13,855 participants) was conducted in an assessment center. All surveys used a questionnaire, gathered data from blood and urine tests, and collected basic information from municipal health check-ups. Furthermore, several physiological measurements (carotid ultrasound imaging, body composition, respiratory function test, bone density measurement, etc.) were obtained only in the Type 2 survey 17) . Informed consent was obtained from a total of 54,952 participants. This study was approved by the Institutional Review Board of the TMM Organization (approval number: 2022-4-047, approval date: June 30, 2022).
To be included in the analysis, participants had to undergo several physiological measurements. Thus, we enrolled only those who participated in the Type 2 survey (n=13,855). From these 13,855 participants, we excluded 489 participants for the following reasons: (1) those who withdrew from the study by October 5, 2021, failed to return the self-reported questionnaire, or did not undergo physiological measurements (n=196); and (2) had data missing on height, weight, SBP, diastolic blood pressure (DBP), non-fasting blood glucose, HbA1c, TC, triglyceride (TG), HDL-C, and cIMT (n=293). Therefore, 13,366 participants were included in the analysis dataset of this study.
Anthropometry
Height was measured to the nearest 0.1 cm using a stadiometer (AD-6400; A&D Co, Ltd, Tokyo, Japan). Weight was measured using a body composition analyzer (InBody720; Biospace Co, Ltd, Seoul, Republic of Korea). Weight was measured in increments of 0.1 kg, and 1.0 kg was subtracted to account for the weight of the participant’s clothing. BMI was calculated as the weight (kg) divided by height squared (m2).
Carotid Intima Media Thickness
Ultrasound imaging (GM-72P00A; Panasonic Healthcare, Co, Ltd, Japan) was used to measure right and left cIMT at the common carotid artery. The left and right cIMT were measured at a plaque-free site situated 10 mm proximal to the carotid bifurcation. The Cardiovascular Health Study used the maximum cIMT as a parameter because this parameter is more closely associated with cardiovascular risk factors compared with the mean cIMT 27) . The Shiga Epidemiological Study of Subclinical Atherosclerosis showed that the mean cIMT of maximum values had stronger associations with coronary calcium, a manifestation of coronary atherosclerosis and a strong surrogate marker for coronary heart disease 28) . Thus, we measured the thickness of the left and right maximum common carotid arteries. The analysis used the average of the maximum IMT values of the left and right IMT.
Measurements
We collected information on the participants’ demographic characteristics, smoking status, and drinking status using a self-reported questionnaire. Age was determined at the time of the visit to the community support center. Smoking status was classified into six categories: never smoker (had smoked <100 cigarettes in their lifetime), ex-smoker (had smoked ≥ 100 cigarettes in their lifetime but were not current smokers), current smoker (1–9, 10–19, or ≥ 20 cigarettes a day), and unknown 29) . Drinking status was classified into six categories: never drinker (had consumed little or no alcohol or were constitutionally incapable of alcohol consumption), ex-drinker (had stopped drinking alcohol), current drinker (<23, 23.0–45.9, or ≥ 46.0 g/day), and unknown. Based on previous studies 18 - 21) that calculated the amount of ethanol consumed, the alcohol consumed was classified into six categories: sake, distilled spirits, shochu-based beverage, beer, whiskey, and wine. Furthermore, the alcohol intake frequency was classified into the following six categories: almost never, 1–3 days/month, 1–2 days/week, 3–4 days/week, 5–6 days/week, or daily. The amount of ethanol consumed was calculated by multiplying the type of alcohol by the frequency and amount of consumption. We set the cutoff value at 23 g, as this is the most common unit in Japan for measuring the amount of alcohol consumed 20 , 30) .
After resting in a sitting position for ≥ 2 min, blood pressure was measured twice in the upper right arm using a digital automatic blood pressure monitor (HEM-9000AI; Omron Healthcare Co, Ltd, Kyoto, Japan). We collected non-fasting blood samples, and non-fasting blood glucose levels were measured using the hexokinase method. HbA1c levels were measured using the latex agglutination turbidimetry method. TC was measured using the Ultraviolet-End method with cholesterol dehydrogenase. TG was measured using an enzymatic method. HDL-C levels were measured using the direct method. The non-HDL-C level was calculated by subtracting the HDL-C levels from the TC.
Statistical Analysis
Data are presented as the mean (standard deviation (SD)) or median (interquartile range) for continuous variables and as the number (percentage) for categorical variables. An analysis of covariance (ANCOVA) was used to examine the association between risk factors for atherosclerosis and cIMT. The least square (LS) means of cIMT and corresponding 95% confidence intervals (CI) are presented. The multivariable-adjusted models included age (per 1-year increase), sex, height (per 10-cm increase), smoking status (never smoker, ex-smoker, current smoker [1–9, 10–19, or ≥ 20 cigarettes a day] and unknown), BMI (per 1-kg/m2), SBP (per 10 mmHg), HbA1c (<5.5%, 5.5%–6.4%, and ≥ 6.5%), HDL-C (per 10 mg/dL), non-HDL-C (per10 mg/dL), and drinking status (never drinker, ex-drinker, and current drinker [<23, 23.0–45.9, or ≥ 46.0 g/day] and unknown). The results were compared for each independent variable by analysis using Dunnett’s test with the following categories as references: age <30 years, height <150 cm, never smoker, BMI <16.0 kg/m2, SBP <100 mmHg, HbA1c <5.5%, HDL-C <40 mg/dL, non-HDL-C <90 mg/dL, and never drinker. For continuous variables such as age, height, BMI, SBP, HbA1c, HDL-C, and non-HDL-C, we further calculated the p-values for the linear trend analysis by scoring the categories and entering the number as a continuous term in the regression model.
To compare the attribution of atherosclerosis risk factors for cIMT, we performed multivariable logistic regression analysis and calculated the area under the receiver operating characteristics curve (AUROC) and 95% CI by using the value of the third quartile of the cIMT measured for the entire cohort as the cutoff point of high cIMT. We compared the AUROC of the full model (age, sex, height, smoking status, BMI, SBP, HbA1c, HDL-C, non-HDL-C, and drinking status) and the AUROC without each independent variable.
Statistical significance was set at two-tailed p<0.05. All analyses were performed using SAS version 9.4 for Windows (SAS Inc, Cary, NC, USA).
Results
Characteristics of the Study Population
In the entire study cohort, the mean (SD) values for age, cIMT, SBP, HbA1c, HDL-C, and non-HDL-C were 57.3 (13.8) years, 0.61 (0.13) mm, 128.4 (17.7) mmHg, 5.5 (0.5)%, 64.5 (16.6) mg/dL, and 144.5 (35.0) mg/dL, respectively. The proportion (%) of males, current drinkers, and current smokers were 29.8%, 55.4%, and 11.3%, respectively ( Table 1 ) in this study cohort.
Table 1. Characteristics of participants.
| Number | 13366 | |
|---|---|---|
| Age, years | 57.3 | (13.8) |
| Men,% | 3988 | (29.8) |
| cIMT, mm | 0.61 | (0.13) |
| Height, cm | 159.3 | (8.0) |
| Weight, cm | 57.9 | (11.0) |
| BMI, kg/m2 | 22.7 | (3.4) |
| SBP, mmHg | 128.4 | (17.7) |
| DBP, mmHg | 77.8 | (10.8) |
| Glucose, mg/dL | 88.6 | (16.9) |
| HbA1c,% | 5.5 | (0.5) |
| TC, mg/dL | 208.9 | (35.7) |
| TG, mg/dL | 85.0 | (61.0-122.0) |
| HDL-C, mg/dL | 64.5 | (16.6) |
| non-HDL-C, mg/dL | 144.5 | (35.0) |
| Drinking status | ||
| Never drinker | 4863 | (36.4) |
| Ex-drinker | 333 | (2.5) |
| <23 g/day | 6207 | (46.4) |
| 23g–45.9 g/day | 673 | (5.0) |
| >46.0 g/day | 518 | (3.9) |
| Unknown | 772 | (5.8) |
| Smoking status | ||
| Never smoker | 8532 | (63.8) |
| Ex-smoker | 3280 | (24.5) |
| 1–9 cigarettes/day | 312 | (2.3) |
| 10–19 cigarettes/day | 634 | (4.7) |
| >20 cigarettes/day | 563 | (4.2) |
| Unknown | 45 | (0.3) |
Values are expressed as mean (standard deviation) or median (interquartile range) for continuous variables or as number (percentage) for categorical variables.
BMI, body mass index; cIMT, carotid intima media thickness; DBP, diastolic blood pressure; HbA1c, glycated hemoglobin; HDL-C, high-density lipoprotein-cholesterol; non-HDL-C, non-high-density lipoprotein-cholesterol; Q, quartile; SBP, systolic blood pressure; TC, total cholesterol; TG, triglyceride
Associations between Risk Factor of Atherosclerosis and cIMT
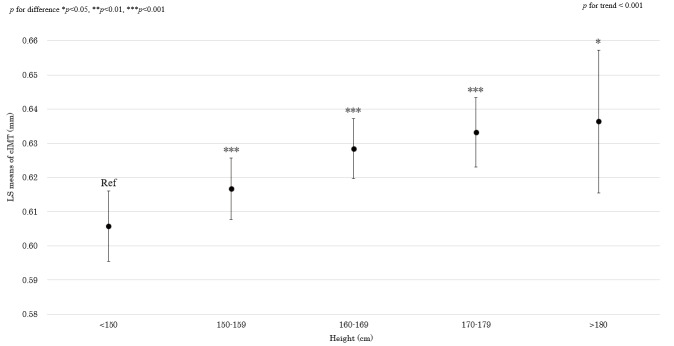
Males had a slightly higher cIMT (0.63 [0.62–0.64] mm) as compared with that of females (0.63 [0.61–0.64] mm) after multivariable adjustment. Age was clearly and linearly associated with an increase in the cIMT, even after adjusted for atherosclerosis risk factors (P for linear trend <0.001). Similarly, height and SBP were linearly associated with increased cIMT ( Figs.1 and 2 ) . BMI and non-HDL-C showed a positive linear trend with cIMT (P for linear trend <0.001; Figs.3 and 4 ). HbA1c was positively associated with cIMT. The LS means (95% CI) were 0.62 mm (0.61–0.63) for HbA1c <5.5%, 0.62 mm (0.61–0.63) for HbA1c 5.5%–6.4%, and 0.64 mm (0.62–0.65) for HbA1c ≥ 6.5% (P for linear trend <0.01). The cIMT was significantly higher when HbA1c ≥ 6.5%, compared with HbA1c <5.5% (P for difference <0.001). Conversely, HDL-C was inversely associated with the cIMT ( Fig.5 ) . Compared with never smokers, ex-smokers had significantly increased cIMT (The LS means (95%CI) were 0.62 mm (0.61–0.63) for never smokers and 0.63 mm (0.62–0.64) for ex-smoker); however, there was no significant difference in the cIMT between current smokers and never smokers (The LS means (95%CI) were 0.63 mm (0.61–0.64) for current smokers who smoked 1–9 cigarettes a day, 0.62 mm (0.61–0.64) for current smokers who smoked 10–19 cigarettes a day, 0.63 mm (0.62–0.64) for current smokers who smoked ≥ 20 cigarettes a day, and 0.61 mm (0.58–0.64) for unknown). With regard to the drinking status, the cIMT LS means (95%CI) were 0.63 mm (0.62–0.64) for never drinkers, 0.64 mm (0.62–0.65) for ex-drinkers, 0.62 mm (0.62–0.63) for current drinkers who consumed <23.0 g alcohol/day, 0.62 mm (0.61–0.63) for current drinkers who consumed 23.0–45.9 g alcohol/day, 0.61 mm (0.59–0.62) for current drinkers who consumed ≥ 46.0 g alcohol/day, and 0.63 mm (0.62–0.64) for unknown. Compared with never drinkers, those who consumed ≥ 46.0 g ethanol/day were significantly associated with lower cIMT values.
Fig.1. Association between height and cIMT (in the model adjusted for age, sex, smoking status, BMI, SBP, HbA1c, HDL-C, non-HDL-C, and drinking status).
p for difference was derived from Dunnett’s test using height<150 cm as the reference. Bars represent 95% confidence intervals. p for difference showed as following: *p<0.05, **p<0.01, ***p<0.001. p for trend was calculated by scoring the height categories and entering the number as a continuous term in the regression model. Abbreviations: BMI, body mass index; cIMT, carotid intima media thickness; HbA1c, glycated hemoglobin; HDL-C, high-density lipoprotein-cholesterol; LS, least square; non-HDL-C, non-high-density lipoprotein-cholesterol; SBP, systolic blood pressure.
Fig.2. Association between SBP and cIMT (in the model adjusted for age, sex, smoking status, BMI, HbA1c, HDL-C, non-HDL-C, drinking status, and height).
p for difference was derived from Dunnett’s test using SBP<100 mmHg as the reference. Bars represent 95% confidence intervals. p for difference showed as following: *p<0.05, **p<0.01, ***p<0.001. p for trend was calculated by scoring the SBP categories and entering the number as a continuous term in the regression model. Abbreviations: BMI, body mass index; cIMT, carotid intima media thickness; HbA1c, glycated hemoglobin; HDL-C, high-density lipoprotein-cholesterol; LS, least square; non-HDL-C, non-high-density lipoprotein-cholesterol; SBP, systolic blood pressure.
Fig.3. Association between BMI and cIMT (in the model adjusted for age, sex, smoking status, SBP, HbA1c, HDL-C, non-HDL-C, drinking status, and height).
p for difference was derived from Dunnett’s test using BMI<16.0 kg/m2 as the reference. Bars represent 95% confidence intervals. p for difference showed as following: *p<0.05, **p<0.01, ***p<0.001. p for trend was calculated by scoring the BMI categories and entering the number as a continuous term in the regression model. Abbreviations: BMI, body mass index; cIMT, carotid intima media thickness; HbA1c, glycated hemoglobin; HDL-C, high-density lipoprotein-cholesterol; LS, least square; non-HDL-C, non-high-density lipoprotein-cholesterol; SBP, systolic blood pressure.
Fig.4. Association between non-HDL-C and cIMT (in the model adjusted for age, sex, smoking status, BMI, SBP, HbA1c, HDL-C, drinking status, and height).
p for difference was derived from Dunnett’s test using non-HDL<90 mg/dl as the reference. Bars represent 95% confidence intervals. p for difference showed as following: *p<0.05, **p<0.01, ***p<0.001. p for trend was calculated by scoring the non-HDL-C categories and entering the number as a continuous term in the regression model. Abbreviations: BMI, body mass index; cIMT, carotid intima media thickness; HbA1c, glycated hemoglobin; HDL-C, high-density lipoprotein-cholesterol; LS, least square; non-HDL-C, non-high-density lipoprotein-cholesterol; SBP, systolic blood pressure.
Fig.5. Association between HDL-C and cIMT (in the model adjusted for age, sex, smoking status, BMI, SBP, HbA1c, non-HDL-C, drinking status, and height).
p for difference was derived from Dunnett’s test using HDL-C<40 mg/dl as the reference. Bars represent 95% confidence intervals. p for difference showed as following: *p<0.05, **p<0.01, ***p<0.001. p for trend was calculated by scoring the HDL-C categories and entering the number as a continuous term in the regression model. Abbreviations: BMI, body mass index; cIMT, carotid intima media thickness; HbA1c, glycated hemoglobin; HDL-C, high-density lipoprotein-cholesterol; LS, least square; non-HDL-C, non-high-density lipoprotein-cholesterol; SBP, systolic blood pressure.
Attribution of Atherosclerosis Risk Factors for cIMT
The AUROC of the full model (age, sex, height, smoking status, BMI, SBP, HbA1c, HDL-C, non-HDL-C, and drinking status) for the third quartile value of the cIMT as the cutoff value and the AUROC without each independent variable are shown in Table 2 . The AUROC of the full model was 0.826 (0.819–0.833) in this study, and the AUROC of the adjusted model, after excluding sex, HbA1c, HDL-C, and smoking status, was the same as that of the full model. The difference between the AUROCs of the full model and age-excluded model was largest (0.744 [0.735–0.753] and −0.082 for difference), followed by that of the SBP-excluded model (0.820 [0.812–0.827] and −0.006 for difference), the non-HDL-C-excluded model (0.824 [0.816–0.831] and −0.002 for difference), the BMI- and height-excluded model (0.825 [0.817–0.832] and −0.001 for difference), and the drinking status-excluded model (0.825 [0.818–0.833] and −0.001 for difference).
Table 2. Area under the ROC curve for atherosclerosis risk factors.
| Area under the receiver operating characteristic curve (95% CI) | |||||
|---|---|---|---|---|---|
| Variable | Full modela | Without corresponding variables | Difference between full model and without corresponding variables | ||
| Age, years | 0.826 | (0.819-0.833) | 0.744 | (0.735-0.753) | -0.082 |
| SBP, mmHg | 0.820 | (0.812-0.827) | -0.006 | ||
| Non-HDL-C | 0.824 | (0.816-0.831) | -0.002 | ||
| BMI, kg/m2 | 0.825 | (0.817-0.832) | -0.001 | ||
| Height | 0.825 | (0.817-0.832) | -0.001 | ||
| Drinking status | 0.825 | (0.818-0.833) | -0.001 | ||
| Sex | 0.826 | (0.818-0.833) | 0 | ||
| HbA1c | 0.826 | (0.818-0.833) | 0 | ||
| HDL-C | 0.826 | (0.818-0.833) | 0 | ||
| Smoking status | 0.826 | (0.818-0.833) | 0 | ||
The area under the receiver operating characteristics curve and 95% CI were calculated by the multivariable logistic regression analysis using the third quartile value of cIMT as a cutoff point in the entire cohort.
a Adjusted for age, sex, height, smoking status, BMI, SBP, HbA1c, HDL-C, non-HDL-C, and drinking status
BMI, body mass index; cIMT, carotid intima media thickness; DBP, diastolic blood pressure; HbA1c, glycated hemoglobin A1c; HDL-C, high- density lipoprotein-cholesterol; non-HDL-C, non-high-density lipoprotein-cholesterol; Q, quartile; SBP, systolic blood pressure; TC, total cholesterol; TG, triglyceride
Discussion
In this cross-sectional study, we analyzed data from 13,366 Japanese participants (aged ≥ 20 years) to investigate the association between risk factors for atherosclerosis and cIMT. We found that higher values for age, height, BMI, SBP, HbA1c, and non-HDL-C were positively associated with cIMT, whereas an inverse relationship was observed between HDL-C and the cIMT. Detailed figures can clarify that the relationship of the risk factors and cIMT essentially did not have a threshold. Males had a higher cIMT than did the females. Compared with never drinkers, current drinkers who consumed ≥ 46.0 g ethanol /day had lower cIMT. Moreover, we compared the contribution of risk factors for cIMT using AUROC, and the largest AUROC difference was owing to the exclusion of age, SBP, non-HDL-C, BMI, height, and alcohol status.
Several risk factors for atherosclerosis, such as aging, male sex, hypertension, dyslipidemia, and diabetes, have been identified in numerous epidemiological studies 31) . The 2022 JAS guideline recommends the management and treatment of the abovementioned risk factors to prevent progression of atherosclerosis 1) . The cIMT is used as a surrogate marker of subclinical atherosclerosis and is associated with risk factors for atherosclerosis as well as a future risk of CVD 2 - 14) . We observed that risk factors for atherosclerosis, including age, BMI, SBP, HbA1c, and non-HDL-C, were positively associated with the cIMT, whereas HDL-C was inversely associated with the cIMT, which is in accordance with the 2022 JAS guideline 1) . Although many previous studies have investigated the association between cIMT and alcohol consumption, the results were inconsistent: some studies showed a protective effect of light and moderate drinking 32 - 41) , others found that alcohol is positively associated with cIMT 42 - 45) , and yet others suggested that there was no association 46 - 51) . An inverse relationship between alcohol consumption and the cIMT was previously reported in three large epidemiological studies (n>4000) in the Korean and European populations 38 , 40 , 41) , and our findings concur with those of these previous studies. However, alcohol consumption may induce an increase in blood pressure and lead to the consequent increase in the cIMT. As we adjusted for blood pressure in our analysis, this may have caused an over-adjustment. Further studies are warranted to clarify the association between alcohol consumption and the cIMT and this mechanism.
There is a positive association between height and cIMT 52 - 54) . The China Kadoorie Biobank study showed that height was associated with a higher cIMT 54) . In the present study, height was positively associated with the cIMT, and this result is consistent with that of previous studies 52 - 54) . A potential mechanism underlying this association may be that, for geometric reasons, both arterial diameter and wall thickness need to adapt to maintain or increase the blood flow through the lengthening arterial tree 52) . Therefore, the cIMT may reflect not only atherosclerosis but also the physiological adaptation in hemodynamics, such as arterial diameter and thickening of the vascular wall, due to increased blood flow. Thus, height might need to be considered in risk factor analysis that includes the cIMT.
We compared the AUROC of the risk factors for atherosclerosis with that of the value of the third quartile of the cIMT as the cutoff value, and the AUROC without each atherosclerosis risk factors was used to compare the contribution of the risk factors for atherosclerosis to the increase in the cIMT. We found that the largest AUROC difference was due to the exclusion of age, SBP, non-HDL-C, BMI, height, or drinking status. Previous studies have shown that age and hypertension are strongly associated with an increase in the cIMT 3 , 6) . Our findings are consistent with the results of previous studies and suggest that control of blood pressure might be a priority for the prevention of atherosclerosis. Additionally, as per the 2022 JAS guideline, non-HDL-C is possibly a useful indicator for predicting the risk of coronary artery disease, and obesity promotes atherosclerosis via hyperlipidemia, hyperglycemia, and hypertension or directly through the action of adipocytokines 1) . Therefore, lipid level management and maintenance of an appropriate body weight are important to prevent atherosclerosis.
The strength of this study is that we describe the association between the risk factors for atherosclerosis and cIMT because this study enrolled a large population of approximately 13,000 participants. However, our study had limitations. First, the presence of plaque is considered a marker of atherosclerosis and has a stronger significance in disease prediction compared with cIMT 3 , 55 , 56) . However, as our study did not measure plaque, we were only able to examine the association between the risk factors for atherosclerosis and cIMT. Second, this study had a cross-sectional design and could not definitively establish a causal relationship. However, previous studies have reported the direction of either or both relationships and causality between risk factors for atherosclerosis and cIMT 5 , 8 - 10) .
In conclusion, the cIMT, as assessed using ultrasonography, is associated with the risk factors for atherosclerosis described in the 2022 JAS guideline. High-risk individuals require targeted interventions to adequately control their risk and to prevent atherosclerotic CVD.
Acknowledgements
The authors thank the members of the Tohoku Medical Megabank Organization, including the Genome Medical Research Coordinators and the office and administrative personnel for their assistance. A complete list of members is available at A complete list of members is available at https://www.megabank.tohoku.ac.jp/english/a220901/. We also thank Fuko Kisara for her analytical supports.
Funding
This work was supported by grants from the Japanese Society for the Promotion of Science [JSPS; Grant-in-Aid for Science Research (C), number 19K10637], Tohoku Medical Megabank Project from the Ministry of Education, Culture, Sports, Science, and Technology (MEXT), the Japan Agency for Medical Research and Development [AMED; JP22tm0124005] and JST SPRING, [Grant number JPMJSP2114].
Conflicts of Interest
There are no conflicts of interest.
References
- 1).Japan Atherosclerosis Society (JAS) Guidelines for Prevention of Atherosclerotic Cardiovascular Diseases 2022. Accessed November 24,2022. https: //www.j-athero.org/jp/wp-content/uploads/publications/pdf/GL2022_s/jas_gl2022_2_220926.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2).O’Leary DH, Polak JF, Kronmal RA, Manolio TA, Burke GL, and Wolfson SK: Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. Cardiovascular Health Study Collaborative Research Group. N Engl J Med, 1999; 340: 14-22 [DOI] [PubMed] [Google Scholar]
- 3).Nezu T, Hosomi N, Aoki S, and Matsumoto M: Carotid intima-media thickness for atherosclerosis. J Atheroscler Thromb, 2016; 23: 18-31 [DOI] [PubMed] [Google Scholar]
- 4).Mannami T, Konishi M, Baba S, Nishi N, Terao A: Prevalence of asymptomatic carotid atherosclerotic lesions detected by high-resolution ultrasonography and its relation to cardiovascular risk factors in the general population of a Japanese city: the Suita study. Stroke, 1997; 28: 518-525 [DOI] [PubMed] [Google Scholar]
- 5).van der Meer IM, Iglesias del Sol A, Hak AE, Bots ML, Hofman A, and Witteman JC: Risk factors for progression of atherosclerosis measured at multiple sites in the arterial tree: the Rotterdam Study. Stroke, 2003; 34: 2374-2379 [DOI] [PubMed] [Google Scholar]
- 6).Al-Shali K, House AA, Hanley AJ, Khan HM, Harris SB, Mamakeesick M, Zinman B, Fenster A, Spence JD, Hegele RA: Differences between carotid wall morphological phenotypes measured by ultrasound in one, two and three dimensions. Atherosclerosis, 2005; 178: 319-325 [DOI] [PubMed] [Google Scholar]
- 7).Naya T, Hosomi N, Ohyama H, Ichihara S, Ban CR, Takahashi T, Taminato T, Feng A, Kohno M, Koziol JA: Smoking, fasting serum insulin, and obesity are the predictors of carotid atherosclerosis in relatively young subjects. Angiology, 2008; 58: 677-684 [DOI] [PubMed] [Google Scholar]
- 8).Koskinen J, Kähönen M, Viikari JS, Taittonen L, Laitinen T, Rönnemaa T, Lehtimäki T, Hutri-Kähönen N, Pietikäinen M, Jokinen E, Helenius H, Mattsson N, Raitakari OT, and Juonala M: Conventional cardiovascular risk factors and metabolic syndrome in predicting carotid intima-media thickness progression in young adults: the cardiovascular risk in young Finns study. Circulation, 2009; 120: 229-236 [DOI] [PubMed] [Google Scholar]
- 9).Herder M, Johnsen SH, Arntzen KA, and Mathiesen EB: Risk factors for progression of carotid intima-media thickness and total plaque area: a 13-year follow-up study: the Tromsø Study. Stroke, 2012; 43: 1818-1823 [DOI] [PubMed] [Google Scholar]
- 10).Rosvall M, Persson M, Östling G, Nilsson PM, Melander O, Hedblad B, and Engström G: Risk factors for the progression of carotid intima-media thickness over a 16-year follow-up period: the Malmö Diet and Cancer Study. Atherosclerosis, 2015; 239: 615-621 [DOI] [PubMed] [Google Scholar]
- 11).Lorenz MW, Markus HS, Bots ML, Rosvall M, and Sitzer M: Prediction of clinical cardiovascular events with carotid intima-media thickness: a systematic review and meta-analysis. Circulation, 2007; 115: 459-467 [DOI] [PubMed] [Google Scholar]
- 12).Polak JF, Pencina MJ, Pencina KM, O’Donnell CJ, Wolf PA, and D’Agostino RB: Carotid-wall intima-media thickness and cardiovascular events. N Engl J Med, 2011; 365: 213-221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13).Kitamura A, Iso H, Imano H, Ohira T, Okada T, Sato S, Kiyama M, Tanigawa T, Yamagishi K, and Shimamoto T: Carotid intima-media thickness and plaque characteristics as a risk factor for stroke in Japanese elderly men. Stroke, 2004; 35: 2788-2794 [DOI] [PubMed] [Google Scholar]
- 14).Shimoda S, Kitamura A, Imano H, Cui R, Muraki I, Yamagishi K, Umesawa M, Sankai T, Hayama-Terada M, Kubota Y, Shimizu Y, Okada T, Kiyama M, and Iso H: Associations of carotid intima-media thickness and plaque heterogeneity with the risks of stroke subtypes and coronary artery disease in the Japanese general population: The Circulatory Risk in Communities Study. J Am Heart Assoc, 2020; 9: e017020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15).Kuriyama S, Yaegashi N, Nagami F, Arai T, Kawaguchi Y, Osumi N, Sakaida M, Suzuki Y, Nakayama K, Hashizume H, Tamiya G, Kawame H, Suzuki K, Hozawa A, Nakaya N, Kikuya M, Metoki H, Tsuji I, Fuse N, Kiyomoto H, Sugawara J, Tsuboi A, Egawa S, Ito K, Chida K, Ishii T, Tomita H, Taki Y, Minegishi N, Ishii N, Yasuda J, Igarashi K, Shimizu R, Nagasaki M, Koshiba S, Kinoshita K, Ogishima S, Takai-Igarashi T, Tominaga T, Tanabe O, Ohuchi N, Shimosegawa T, Kure S, Tanaka H, Ito S, Hitomi J, Tanno K, Nakamura M, Ogasawara K, Kobayashi S, Sakata K, Satoh M, Shimizu A, Sasaki M, Endo R, Sobue K, Tohoku Medical Megabank Project Study Group T, and Yamamoto M: The Tohoku Medical Megabank Project: Design and mission. J Epidemiol, 2016; 26: 493-511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16).Kuriyama S, Metoki H, Kikuya M, Obara T, Ishikuro M, Yamanaka C, Nagai M, Matsubara H, Kobayashi T, Sugawara J, Tamiya G, Hozawa A, Nakaya N, Tsuchiya N, Nakamura T, Narita A, Kogure M, Hirata T, Tsuji I, Nagami F, Fuse N, Arai T, Kawaguchi Y, Higuchi S, Sakaida M, Suzuki Y, Osumi N, Nakayama K, Ito K, Egawa S, Chida K, Kodama E, Kiyomoto H, Ishii T, Tsuboi A, Tomita H, Taki Y, Kawame H, Suzuki K, Ishii N, Ogishima S, Mizuno S, Takai-Igarashi T, Minegishi N, Yasuda J, Igarashi K, Shimizu R, Nagasaki M, Tanabe O, Koshiba S, Hashizume H, Motohashi H, Tominaga T, Ito S, Tanno K, Sakata K, Shimizu A, Hitomi J, Sasaki M, Kinoshita K, Tanaka H, Kobayashi T, Kure S, Yaegashi N, and Yamamoto M: Cohort Profile: Tohoku Medical Megabank Project Birth and Three-Generation Cohort Study (TMM BirThree Cohort Study): rationale, progress and perspective. Int J Epidemiol, 2020; 49: 18-19m [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17).Hozawa A, Tanno K, Nakaya N, Nakamura T, Tsuchiya N, Hirata T, Narita A, Kogure M, Nochioka K, Sasaki R, Takanashi N, Otsuka K, Sakata K, Kuriyama S, Kikuya M, Tanabe O, Sugawara J, Suzuki K, Suzuki Y, Kodama EN, Fuse N, Kiyomoto H, Tomita H, Uruno A, Hamanaka Y, Metoki H, Ishikuro M, Obara T, Kobayashi T, Kitatani K, Takai-Igarashi T, Ogishima S, Satoh M, Ohmomo H, Tsuboi A, Egawa S, Ishii T, Ito K, Ito S, Taki Y, Minegishi N, Ishii N, Nagasaki M, Igarashi K, Koshiba S, Shimizu R, Tamiya G, Nakayama K, Motohashi H, Yasuda J, Shimizu A, Hachiya T, Shiwa Y, Tominaga T, Tanaka H, Oyama K, Tanaka R, Kawame H, Fukushima A, Ishigaki Y, Tokutomi T, Osumi N, Kobayashi T, Nagami F, Hashizume H, Arai T, Kawaguchi Y, Higuchi S, Sakaida M, Endo R, Nishizuka S, Tsuji I, Hitomi J, Nakamura M, Ogasawara K, Yaegashi N, Kinoshita K, Kure S, Sakai A, Kobayashi S, Sobue K, Sasaki M, and Yamamoto M: Study profile of the Tohoku Medical Megabank Community-based Cohort Study. J Epidemiol, 2021; 31: 65-76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18).Takase M, Nakamura T, Tsuchiya N, Kogure M, Itabashi F, Narita A, Hirata T, Nakaya N, Hamanaka Y, Sugawara J, Suzuki K, Fuse N, Uruno A, Kodama EN, Kuriyama S, Tsuji I, Kure S, and Hozawa A: Association between the combined fat mass and fat-free mass index and hypertension: The Tohoku Medical Megabank Community-based Cohort Study. Clin Exp Hypertens, 2021; 43: 610-621 [DOI] [PubMed] [Google Scholar]
- 19).Takase M, Nakamura T, Hirata T, Tsuchiya N, Kogure M, Itabashi F, Nakaya N, Hamanaka Y, Sugawara J, Suzuki K, Fuse N, Uruno A, Kodama EN, Kuriyama S, Tsuji I, Kure S, and Hozawa A: Association between fat mass index, fat-free mass index and hemoglobin A1c in a Japanese population: The Tohoku Medical Megabank Community-based Cohort Study. J Diabetes Investig, 2022; 13: 858-867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20).Kogure M, Hirata T, Nakaya N, Tsuchiya N, Nakamura T, Narita A, Miyagawa K, Koshimizu H, Obara T, Metoki H, Uruno A, Kikuya M, Sugawara J, Kuriyama S, Tsuji I, Kure S, and Hozawa A: Multiple measurements of the urinary sodium-to-potassium ratio strongly related home hypertension: TMM Cohort Study. Hypertens Res, 2020; 43: 62-71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21).Itabashi F, Hirata T, Kogure M, Narita A, Tsuchiya N, Nakamura T, Nakaya N, Sasaki R, Takanashi N, Sakata K, Tanno K, Sugawara J, Kuriyama S, Tsuji I, Kure S, and Hozawa A: Combined associations of liver enzymes and obesity with diabetes mellitus prevalence: The Tohoku Medical Megabank Community-based Cohort Study. J Epidemiol, 2022; 32: 221-227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22).Nakaya N, Xie T, Scheerder B, Tsuchiya N, Narita A, Nakamura T, Metoki H, Obara T, Ishikuro M, Hozawa A, Snieder H, and Kuriyama S: Spousal similarities in cardiometabolic risk factors: A cross-sectional comparison between Dutch and Japanese data from two large biobank studies. Atherosclerosis, 2021; 334: 85-92 [DOI] [PubMed] [Google Scholar]
- 23).Kanno I, Hasegawa K, Nakamura T, Kogure M, Itabashi F, Narita A, Tsuchiya N, Hirata T, Nakaya N, Sugawara J, Kuriyama S, Tsuji I, Kure S, and Hozawa A: Relationship between the housing coldness/warmth evaluation by CASBEE Housing Health Checklist and psychological distress based on TMM Community-Based Cohort Study: a cross-sectional analysis. Public Health, 2022; 208: 98-104 [DOI] [PubMed] [Google Scholar]
- 24).Yamada M, Motoike IN, Kojima K, Fuse N, Hozawa A, Kuriyama S, Katsuoka F, Tadaka S, Shirota M, Sakurai M, Nakamura T, Hamanaka Y, Suzuki K, Sugawara J, Ogishima S, Uruno A, Kodama EN, Fujino N, Numakura T, Ichikawa T, Mitsune A, Ohe T, Kinoshita K, Ichinose M, Sugiura H, and Yamamoto M: Genetic loci for lung function in Japanese adults with adjustment for exhaled nitric oxide levels as airway inflammation indicator. Commun Biol, 2021; 4: 1288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25).Takase M, Nakamura T, Nakaya N, Kogure M, Hatanaka R, Nakaya K, Kanno I, Nochioka K, Tsuchiya N, Hirata T, Hamanaka Y, Sugawara J, Suzuki K, Fuse N, Uruno A, Kodama EN, Kuriyama S, Tsuji I, Kure S, and Hozawa A: Associations between the combined fat mass index and fat-free mass index with carotid intima-media thickness in a Japanese population: The Tohoku Medical Megabank Community-Based Cohort Study. J Atheroscler Thromb, 2022; 10.5551/jat.63523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26).Takase M, Yamada M, Nakamura T, Nakaya N, Kogure M, Hatanaka R, Nakaya K, Kanno I, Nochioka K, Tsuchiya N, Hirata T, Hamanaka Y, Sugawara J, Kobayashi T, Fuse N, Uruno A, Kodama EN, Kuriyama S, Tsuji I, Hozawa A: The Association of Lung Function and Carotid Intima-Media Thickness in a Japanese Population: The Tohoku Medical Megabank Community-Based Cohort Study. J Atheroscler Thromb, 2022; 10.5551/jat.63826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27).O’Leary DH, Polak JF, Kronmal RA, Manolio TA, Burke GL, and Wolfson SK: Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. Cardiovascular Health Study Collaborative Research Group. N Engl J Med, 1999; 340: 14-22 [DOI] [PubMed] [Google Scholar]
- 28).Zaid M, Fujiyoshi A, Hisamatsu T, Kadota A, Kadowaki S, Satoh A, Sekikawa A, Barinas-Mitchell E, Horie M, Miura K, Ueshima H: A Comparison of Segment-Specific and Composite Measures of Carotid Intima-Media Thickness and their Relationships with Coronary Calcium. J Atheroscler Thromb, 2022; 29: 282-295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29).Hamilton CM, Strader LC, Pratt JG, Maiese D, Hendershot T, Kwok RK, Hammond JA, Huggins W, Jackman D, Pan H, Nettles DS, Beaty TH, Farrer LA, Kraft P, Marazita ML, Ordovas JM, Pato CN, Spitz MR, Wagener D, Williams M, Junkins HA, Harlan WR, Ramos EM, and Haines J: The PhenX Toolkit: get the most from your measures. Am J Epidemiol, 2011; 174: 253-260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30).Inoue M, Nagata C, Tsuji I, Sugawara Y, Wakai K, Tamakoshi A, Matsuo K, Mizoue T, Tanaka K, Sasazuki S, Tsugane S, Tsugane S, Inoue M, Sasazuki S, Iwasaki M, Otani T, Sawada N, Shimazu T, Yamaji T, Tsuji I, Tsubono Y, Nishino Y, Wakai K, Matsuo K, Nagata C, Mizoue T, Tanaka K, and Tamakoshi A: Impact of alcohol intake on total mortality and mortality from major causes in Japan: a pooled analysis of six large-scale cohort studies. J Epidemiol Community Health, 2012; 66: 448-456 [DOI] [PubMed] [Google Scholar]
- 31).Herrington W, Lacey B, Sherliker P, Armitage J, and Lewington S: Epidemiology of Atherosclerosis and the potential to reduce the global burden of atherothrombotic disease. [DOI] [PubMed] [Google Scholar]
- 32).Ferrières J, Elias A, Ruidavets JB, Cantet C, Bongard V, Fauvel J, and Boccalon H: Carotid intima-media thickness and coronary heart disease risk factors in a low-risk population. J Hypertens, 1999; 17: 743-748 [DOI] [PubMed] [Google Scholar]
- 33).Kiechl S, Willeit J, Rungger G, Egger G, Oberhollenzer F, and Bonora E: Alcohol consumption and atherosclerosis: what is the relation? Prospective results from the Bruneck Study. Stroke, 1998; 29: 900-907 [DOI] [PubMed] [Google Scholar]
- 34).Jerrard-Dunne P, Sitzer M, Risley P, Steckel DA, Buehler A, von Kegler S, and Markus HS: Interleukin-6 promoter polymorphism modulates the effects of heavy alcohol consumption on early carotid artery atherosclerosis: the Carotid Atherosclerosis Progression Study (CAPS). Stroke, 2003; 34: 402-407 [DOI] [PubMed] [Google Scholar]
- 35).Knoflach M, Kiechl S, Kind M, Said M, Sief R, Gisinger M, van der Zee R, Gaston H, Jarosch E, Willeit J, and Wick G: Cardiovascular risk factors and atherosclerosis in young males: ARMY study (Atherosclerosis Risk-Factors in Male Youngsters). Circulation, 2003; 108: 1064-1069 [DOI] [PubMed] [Google Scholar]
- 36).Mukamal KJ, Kronmal RA, Mittleman MA, O’Leary DH, Polak JF, Cushman M, and Siscovick DS: Alcohol consumption and carotid atherosclerosis in older adults: the Cardiovascular Health Study. Arterioscler Thromb Vasc Biol, 2003; 23: 2252-2259 [DOI] [PubMed] [Google Scholar]
- 37).Schminke U, Luedemann J, Berger K, Alte D, Mitusch R, Wood WG, Jaschinski A, Barnow S, John U, and Kessler C: Association between alcohol consumption and subclinical carotid atherosclerosis: the Study of Health in Pomerania. Stroke, 2005; 36: 1746-1752 [DOI] [PubMed] [Google Scholar]
- 38).Lee YH, Shin MH, Kweon SS, Choi SW, Kim HY, Ryu SY, Kim BH, Rhee JA, and Choi JS: Alcohol consumption and carotid artery structure in Korean adults aged 50 years and older. BMC Public Health, 2009; 9: 358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39).Xie X, Ma YT, Yang YN, Fu ZY, Ma X, Huang D, Li XM, Chen BD, Liu F, Huang Y, Liu C, Zhang XL, Zheng YY, Baituola G, Wang BZ, Du L, and Gao X: Alcohol consumption and carotid atherosclerosis in China: the Cardiovascular Risk Survey. Eur J Prev Cardiol, 2012; 19: 314-321 [DOI] [PubMed] [Google Scholar]
- 40).Kim MK, Shin J, Kweon SS, Shin DH, Lee YH, Chun BY, and Choi BY: Harmful and beneficial relationships between alcohol consumption and subclinical atherosclerosis. Nutr Metab Cardiovasc Dis, 2014; 24: 767-776 [DOI] [PubMed] [Google Scholar]
- 41).Laguzzi F, Baldassarre D, Veglia F, Strawbridge RJ, Humphries SE, Rauramaa R, Smit AJ, Giral P, Silveira A, Tremoli E, Hamsten A, de Faire U, Frumento P, Leander K, Sirtori CR, Castelnuovo S, Amato M, Frigerio B, Ravani A, Sansaro D, Tedesco C, Coggi D, Bonomi A, Eriksson MJ, Cooper J, Acharya J, Huttunen K, Rauramaa E, Pekkarinen H, Penttila IM, Törrönen J, van Gessel AI, van Roon AM, Teune GC, Kuipers WD, Bruin M, Nicolai A, Haarsma-Jorritsma P, Mulder DJ, Bilo HJG, Smeets GH, Beaudeux JL, Kahn JF, Carreau V, Kontush A, Karppi J, Nurmi T, Nyyssönen K, Salonen R, Tuomainen TP, Tuomainen J, Kauhanen J, Vaudo G, Alaeddin A, Siepi D, Lupattelli G, and Mannarino E: Alcohol consumption in relation to carotid subclinical atherosclerosis and its progression: results from a European longitudinal multicentre study. Eur J Nutr, 2021; 60: 123-134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42).Kauhanen J, Kaplan GA, Goldberg DE, Salonen R, and Salonen JT: Pattern of alcohol drinking and progression of atherosclerosis. Arterioscler Thromb Vasc Biol, 1999; 19: 3001-3006 [DOI] [PubMed] [Google Scholar]
- 43).Juonala M, Viikari JS, Kähönen M, Laitinen T, Taittonen L, Loo BM, Jula A, Marniemi J, Räsänen L, Rönnemaa T, and Raitakari OT: Alcohol consumption is directly associated with carotid intima-media thickness in Finnish young adults: the Cardiovascular Risk in Young Finns Study. Atherosclerosis, 2009; 204: e93-98 [DOI] [PubMed] [Google Scholar]
- 44).Rantakömi SH, Laukkanen JA, Kurl S, and Kauhanen J: Binge drinking and the progression of atherosclerosis in middle-aged men: an 11-year follow-up. Atherosclerosis, 2009; 205: 266-271 [DOI] [PubMed] [Google Scholar]
- 45).Zyriax BC, Lau K, Klähn T, Boeing H, Völzke H, and Windler E: Association between alcohol consumption and carotid intima-media thickness in a healthy population: data of the STRATEGY study (Stress, Atherosclerosis and ECG Study). Eur J Clin Nutr, 2010; 64: 1199-1206 [DOI] [PubMed] [Google Scholar]
- 46).Demirovic J, Nabulsi A, Folsom AR, Carpenter MA, Szklo M, Sorlie PD, and Barnes RW: Alcohol consumption and ultrasonographically assessed carotid artery wall thickness and distensibility. The Atherosclerosis Risk in Communities (ARIC) Study Investigators. Circulation, 1993; 88: 2787-2793 [DOI] [PubMed] [Google Scholar]
- 47).Markus RA, Mack WJ, Azen SP, and Hodis HN: Influence of lifestyle modification on atherosclerotic progression determined by ultrasonographic change in the common carotid intima-media thickness. Am J Clin Nutr, 1997; 65: 1000-1004 [DOI] [PubMed] [Google Scholar]
- 48).Djoussé L, Myers RH, Province MA, Hunt SC, Eckfeldt JH, Evans G, Peacock JM, and Ellison RC: Influence of apolipoprotein E, smoking, and alcohol intake on carotid atherosclerosis: National Heart, Lung, and Blood Institute Family Heart Study. Stroke, 2002; 33: 1357-1361 [DOI] [PubMed] [Google Scholar]
- 49).Zureik M, Gariépy J, Courbon D, Dartigues JF, Ritchie K, Tzourio C, Alpérovitch A, Simon A, and Ducimetière P: Alcohol consumption and carotid artery structure in older French adults: the Three-City Study. Stroke, 2004; 35: 2770-2775 [DOI] [PubMed] [Google Scholar]
- 50).Spring B, Moller AC, Colangelo LA, Siddique J, Roehrig M, Daviglus ML, Polak JF, Reis JP, Sidney S, and Liu K: Healthy lifestyle change and subclinical atherosclerosis in young adults: Coronary Artery Risk Development in Young Adults (CARDIA) study. Circulation, 2014; 130: 10-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51).Britton AR, Grobbee DE, den Ruijter HM, Anderson TJ, Desvarieux M, Engström G, Evans GW, Hedblad B, Kauhanen J, Kurl S, Lonn EM, Mathiesen EB, Polak JF, Price JF, Rembold CM, Rosvall M, Rundek T, Salonen JT, Stehouwer C, Tuomainen TP, and Bots ML: Alcohol Consumption and Common Carotid Intima-Media Thickness: The USE-IMT Study. Alcohol Alcohol, 2017; 52: 483-486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52).Jourdan C, Wühl E, Litwin M, Fahr K, Trelewicz J, Jobs K, Schenk JP, Grenda R, Mehls O, Tröger J, and Schaefer F: Normative values for intima-media thickness and distensibility of large arteries in healthy adolescents. J Hypertens, 2005; 23: 1707-1715 [DOI] [PubMed] [Google Scholar]
- 53).Doyon A, Kracht D, Bayazit AK, Deveci M, Duzova A, Krmar RT, Litwin M, Niemirska A, Oguz B, Schmidt BM, Sözeri B, Querfeld U, Melk A, Schaefer F, and Wühl E: Carotid artery intima-media thickness and distensibility in children and adolescents: reference values and role of body dimensions. Hypertension, 2013; 62: 550-556 [DOI] [PubMed] [Google Scholar]
- 54).Arnold M, Linden A, Clarke R, Guo Y, Du H, Bian Z, Wan E, Yang M, Wang L, Chen Y, Chen J, Long H, Gu Q, Collins R, Li L, Chen Z, and Parish S: Carotid intima-media thickness but not carotid artery plaque in healthy individuals is linked to lean body mass. J Am Heart Assoc, 2019; 8: e011919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55).Störk S, van den Beld AW, von Schacky C, Angermann CE, Lamberts SW, Grobbee DE, Bots ML: Carotid artery plaque burden, stiffness, and mortality risk in elderly men: a prospective, population-based cohort study. Circulation, 2004; 110: 344-348 [DOI] [PubMed] [Google Scholar]
- 56).Belcaro G, Nicolaides AN, Ramaswami G, Cesarone MR, De Sanctis M, Incandela L, Ferrari P, Geroulakos G, Barsotti A, Griffin M, Dhanjil S, Sabetai M, Bucci M, Martines G: Carotid and femoral ultrasound morphology screening and cardiovascular events in low risk subjects: a 10-year follow-up study (the CAFES-CAVE study(1)). Atherosclerosis, 2001; 156: 379-387 [DOI] [PubMed] [Google Scholar]