PURPOSE
To compare the efficacy of tai ji quan versus strength training to prevent falls after chemotherapy in older, postmenopaual women.
METHODS
We conducted a three-arm, single-blind, randomized controlled trial where older (50+ years), postmenopausal women cancer survivors participated in one of three supervised group exercise programs (tai ji quan, strength training, or stretching control) twice weekly for 6 months and were followed up 6 months after training stopped. The primary outcome was the incidence of falls. Secondary outcomes included fall-related injuries, leg strength (1 repetition maximum; kg), and balance (sensory organization [equilibrium score] and limits of stability [LOS; %] tests).
RESULTS
Four hundred sixty-two women were enrolled (mean age, 62 ± 6.3 years). Retention was 93%, and adherence averaged 72.9%. In primary analysis, there was no difference in the incidence of falls between groups after 6 months of training, nor during 6-month follow-up. A post hoc analysis detected a significantly reduced incidence of fall-related injuries within the tai ji quan group over the first 6 months, dropping from 4.3 falls per 100 person-months (95% CI, 2.9 to 5.6) at baseline to 2.4 falls per person-months (95% CI, 1.2 to 3.5). No significant changes occurred during 6-month follow-up. Over the intervention period, leg strength significantly improved in the strength group and balance (LOS) improved in the tai ji quan group, compared with controls (P < .05).
CONCLUSION
We found no significant reduction in falls for tai ji quan or strength training relative to stretching control in postmenopausal women treated with chemotherapy.
Check out our JCO paper on one of the first clinical trials to test exercise for fall prevention in cancer survivors!
INTRODUCTION
Falls are a serious problem for aging cancer survivors, particularly women, that can lead to fractures and other life-threatening injuries, loss of independence, and increased health care costs.1-3 Chemotherapy accelerates aging and the development of frailty4 (ie, muscle loss, weakness, slowness, fatigue, and inactivity) and is associated with higher fall risk.5-8 It also damages central and peripheral nervous system integrity, leading to chemotherapy-induced peripheral neuropathy causing lower-extremity motor and sensory impairments, vestibular toxicity affecting postural control,9,10 and cognitive dysfunction altering gait.6,11-14 Given the impact of falls on morbidity and mortality on individuals and health care systems, clinicians need access to effective nonpharmacologic interventions to mitigate the neurotoxic effects of chemotherapy, including the prevention of falls.
CONTEXT
Key Objective
To test the efficacy of two different exercise-based fall prevention approaches (tai ji quan and strength training) against a stretching control group on falls and fall-related injuries in older (50+ years), postmenopausal women cancer survivors (n = 462; mean age, 62 ± 6.3 years).
Knowledge Generated
Despite evidence for intervention fidelity (eg, tai ji quan improved balance control and strength training increased lower body muscle strength), we did not find that 6 months of strength or balance-based training, compared with a stretching control, reduced fall and fall-related injuries after chemotherapy in a broad sample of postmenopausal cancer survivors. However, a post hoc analysis pointed to some promising data to suggest that high-risk patients with a history of falls may benefit from engaging in regular balance-based exercise regimens after finishing chemotherapy to mitigate injury risk related to treatment-related falls.
Relevance (S.B. Wheeler)
-
Exercise and strength training are increasingly recommended for cancer survivors, but limited data exist comparing different types of training regimens to each other. This comparative study examining tai ji quan balance-based training or strength training compared with stretching to reduce fall and fall-related injuries found no evidence of superior benefits of one approach over another in postmenopausal women cancer survivors.*
*Relevance section written by JCO Associate Editor Stephanie B. Wheeler, PhD, MPH.
Exercise is an effective fall prevention strategy, particularly programs emphasizing balance or functional movements with resistance exercise.15,16 For example, exercise has demonstrated over 30% reduction in falls, and balance training programs, such as tai ji quan,17 reduce falls among community-dwelling older adults.18-20 Yet, the evidence for exercise as a fall prevention strategy in cancer survivors is limited to a single, underpowered trial using a general strengthening program that demonstrated no clinical benefit in post-treatment breast cancer survivors.21 To address this knowledge gap and inform clinical practice, we designed the Group Exercise Training for Functional Improvement after Treatment (GET FIT) trial to compare the relative efficacy of two distinct types of prescribed exercise interventions, tai ji quan versus strength training, to reduce falls in older, postmenopausal women who received chemotherapy. We hypothesized that tai ji quan and strength training would each reduce the number of falls compared with a control group (stretch and relaxation). Secondary aims were to determine the impact of exercise on fall-related injuries, training-related mechanisms of fall reductions (eg, increased strength or balance), and sustainability of exercise benefits.
METHODS
Patient Population
The target population included women cancer survivors at risk for falls after chemotherapy. Inclusion criteria were a diagnosis of stage I-III cancer other than brain or spinal cord, chemotherapy completion ≥3 months before enrollment, age 50-75 years, postmenopausal status, physically underactive (<60 min/wk of self-reported moderate-intensity exercise),22 ability to provide consent, and absence of contraindications to moderate-intensity exercise (Clinicaltrials.gov identifier: NCT01635413). The published study Protocol21 was institutional review board–approved, and written informed consent was obtained from each participant. Women were enrolled from 2013 to 2018. Patients were recruited using mailings sent by the Oregon State Cancer Registry and direct referrals from Oregon Health and Science University (OHSU) and community clinicians. Staff screened and scheduled eligible participants who provided consent at baseline.
Study Design
This was a single-blind, parallel-group, randomized controlled trial. Participants were randomly assigned in a 1:1:1 ratio to one of three groups: (1) tai ji quan, (2) strength training, or (3) stretch and relaxation (control). Women participated in their assigned, supervised group training (10-15 participants/group) for 6 months, with 6 months of follow-up. Interventions were conducted at OHSU and community locations. Each participant received a sealed, opaque envelope containing her randomly assigned sequence number generated by a statistician (N.D.) using a random number generator in MS Excel after completion of baseline testing, including surveys, which ensured that measurement technicians responsible for data collection and coding were blinded to group allocation. Participants were not told whether or not their group represented the experimental or control groups.
Interventions
Each group attended supervised 1-hour classes led by a certified exercise instructor twice weekly for 6 months. Quality control procedures to minimize instructional differences across instructors have been previously described.23 All participants followed the same set of exercises unless individual modifications were required for safety. Physician clearance was obtained for every participant before starting classes.
Tai ji quan.
The intervention protocol was a set of eight purposeful and functional movement forms blended with practice variation and therapeutic moves designed to challenge balance control and train gait patterns, including movement exercises such as ankle sways, displacement of the body's center of mass over the base of support, trunk rotation/flexion, coordinated eye-hand movements, and multidirectional stepping.24 Training was progressive, with the number of forms doubling and repetitions increasing (approximately 2-4 each month for the first 3 months) and the forms' complexity gradually increasing thereafter.
Strength training.
This intervention protocol involved progressive lower-body strength training to improve neuromuscular function (strength, gait, and balance). This training program consisted of 1-3 sets of 8-10 exercises at a weight performed at 8-12 repetitions with a 1- to 2-minute rest between sets.25 Weighted vests and steps provided resistance, and starting intensity was tailored to each participant's initial capability. Planned progression increases were 1%-3% of body weight in weight vests per month up to a target of 15% by 6 months, depending on tolerance.
Stretching and relaxation control.
We chose a placebo exercise group over a nonexercise control group since exercise is recommended usual care for all cancer survivors.26 The protocol involved whole-body stretches from a seated or lying position to minimize weight-bearing forces that might increase muscle strength or postural control.27 The last 10-15 minutes of each session focused on progressive neuromuscular relaxation exercises.
6-Month Follow-Up
To evaluate the sustainability of supervised training, we followed participants for 6 months after formal training stopped. During this time, participants were encouraged to stay physically active and given a written copy of their exercise program without exercise equipment. Participants then reported their continued exercise frequency at the 12-month visit.
Study Outcomes and Assessments
Baseline demographic and clinical data were assessed by self-report, and height and weight by anthropometry (Table 1). Other measures included comorbidities (Functional Comorbidity Index28), physical function (Short Physical Performance Battery29), physical activity (Community Health Activity Model Program for Seniors questionnaire29), and fear of falling (Survey of Activities and Fear of Falling in the Elderly [SAFFE]30).
TABLE 1.
Demographics and Clinical Characteristics of the Full Sample and by Study Arm
Adherence, tolerance, and safety.
The exercise instructor recorded adherence (percent of prescribed sessions completed) in attendance logs. Tolerance to training was described as the percent of women who could perform at least 50% of the prescribed exercises without modification for more than 50% of the intervention period. Exercise-related adverse events (AEs; eg, fatigue, muscle soreness/pain, or musculoskeletal injuries) were tracked using monthly surveys and categorized by severity according to prespecified criteria.23
Primary and secondary outcomes were measured at baseline, 3 (midintervention), 6 (postintervention), and 12 months (6-month postintervention follow-up). The primary outcome of falls was operationally defined31 and assessed retrospectively at baseline through a 6-month recall and tracked prospectively during the study using a monthly calendar collected every 3 months. A fall was injurious if it resulted in fractures, head injuries, sprains, bruises, scrapes, serious joint injuries, or if the participant sought medical care.31 Secondary outcomes included measures of postural control (sensory organization test [SOT]32 and limits of stability [LOS] by computerized dynamic posturography [Clinical Research System, Neurocom Intl, Inc]),33 and muscle strength (leg press 1-repetition maximum [kg]).27 A measure of flexibility, the chair sit and reach test (cm), was included to assess fidelity of the control arm.34
Statistical Analysis
Statistical power analyses, detailed elsewhere,30 were based on expected reductions in fall incidence found in previous work35,36 and negative binomial regression to model overdispersed count data.37 Planned sample size was 456 participants (152 per group), accounting for 25% attrition. Negative binomial regression models tested the efficacy of tai ji quan versus control and strength training versus control in reducing the incidence of falls during the intervention, follow-up, and the full study period (0-12 months). Age, cancer type (breast or other), and time from chemotherapy completion were covariates. To account for differences in participant study (exposure) time, follow-up months were included as an offset in the model. Effect estimates are reported as incidence rate ratios and 95% CIs. The moderating effect of regular versus infrequent participation in exercise (≥1 v <1 session/wk) during the follow-up period was tested by including interactions with the intervention group. Planned mediation analyses were not conducted because of a lack of significant intervention effects on falls. The post hoc analyses tested for changes in fall incidence within each study arm using baseline fall history (ie, falls in prior 6 months) as a reference. Fall incidence densities (number of falls/number of person-months observed), scaled to reflect the number of falls per 100 person-months, were calculated to estimate the fall rate for each group.38 Incidence density ratios (IDRs) compared falls over each measurement interval with baseline fall history within each group. Analyses were repeated for fall-related injuries. Missing data on falls because of loss to follow-up were accounted for by adjusting for exposure time as discussed above. Intervention groups were compared on changes in secondary outcomes (strength, balance, and flexibility) using a piecewise linear mixed-effects (involving both fixed and random effects) modeling approach with a breakpoint at 6 months to allow for simultaneous estimation of change during the intervention and also during follow-up. Models included random intercepts and random slopes on the time variable and allow the use all available data. All analyses were completed in R39 and conducted as intention-to-treat (ITT) for two-sided tests and alpha = 0.05. Negative binomial regression models (estimated dispersion parameter estimate = 1) were estimated with the glm function from the base stats package R. Mixed-effects models used the lme function from the nlme package.40 R syntax for all models and calculations for incidence densities are provided in a Data Supplement, online only.
RESULTS
Study Sample
In response to recruitment efforts, 1,463 women expressed interest in the study and 462 of them were eligible and enrolled in the trial for a 31% accrual rate (Fig 1). Most women (mean age: 62.1 ± 6.3 years) had stage I or II disease (67%), breast cancer (71%), and were 5 years past chemotherapy completion (Table 1). Between random assignment and the start of training, 15 women did not receive the intervention (late screening failure (n = 7) or were unable to make class times (n = 8); consequently, they were not included in the ITT analysis. Groups did not differ on baseline demographic variables (Table 1). During the intervention, 30 women withdrew from the study and another three withdrew during follow-up, resulting in 93% retention (Fig 1).
FIG 1.

CONSORT diagram for the GET FIT trial. aExpressed interest but unable to connect. GET FIT, Group Exercise Training for Functional Improvement after Treatment.
Adherence, Tolerance, and Safety
Adherence to supervised training did not differ across groups (tai ji quan, 71.5% ± 22.0%; strength, 73.3% ± 20.9%; control, 73.8% ± 20.8%). During follow-up, the percent of women reporting continued participation in tai ji quan, strength, or stretching more than one time per week was 18%, 67%, and 70%, respectively (Appendix Table A1, online only). Women in tai ji quan and stretching groups tolerated the prescribed program, whereas 4% of women in the strength program (n = 6) required adjustments to improve tolerance. Final average vest weight in the strength group was 9% ± 3% of body weight, reaching 60% of the target intensity. There were 11 reports of AEs related or possibly related to exercise training (6 mild, 5 moderate, and 0 severe) and 5 AEs that were unrelated. Study related AEs were either pain-related exacerbations of existing knee or back pain or new-onset pain (Appendix Table A2, online only). Most AEs were from the strength group (n = 9) which led to program modification and withdrawal (n = 1) in the tai ji quan group.
Falls and Fall-Related Injuries
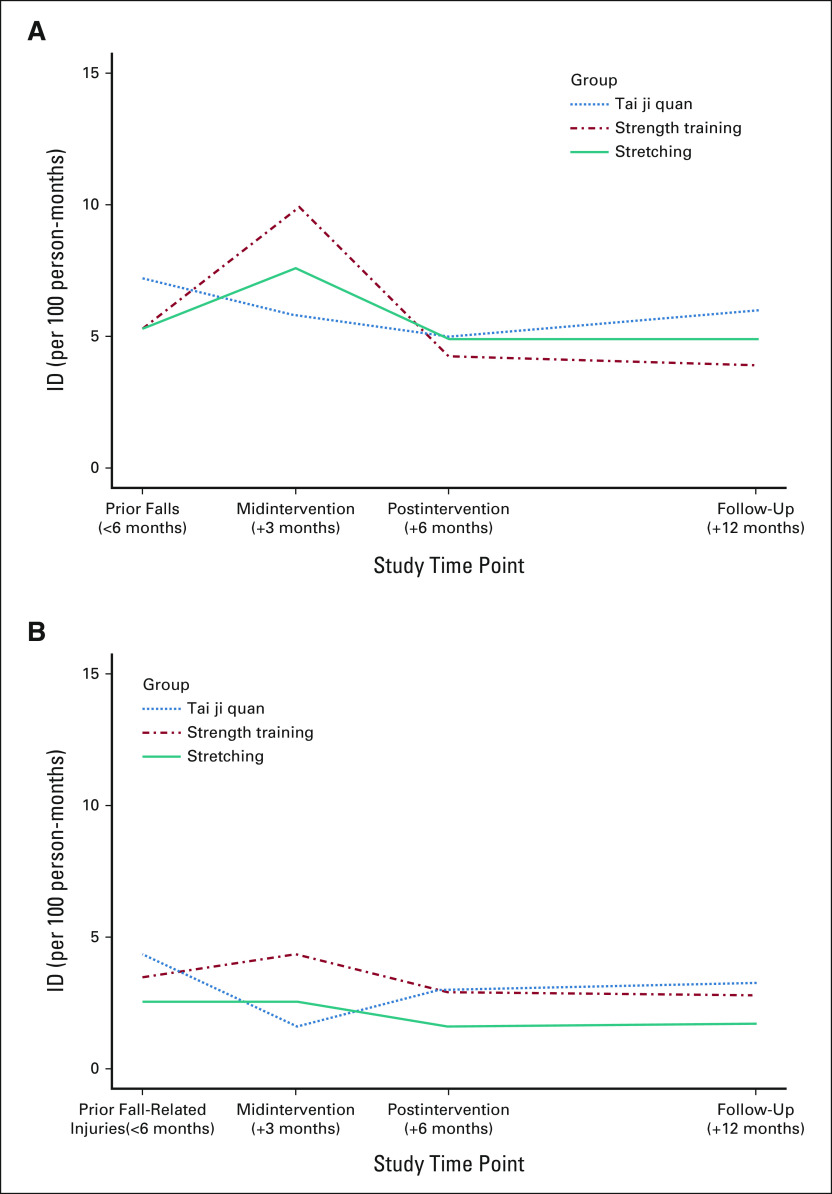
Over the 6 months before enrollment, 21% of the sample reported at least one fall, and 12% reported at least one fall injury (Table 1). During the 6-month intervention period, 26% had at least one fall, and 9% reported at least one fall-related injury; similarly, in the 6-month follow-up period, 27% experienced at least one fall, and 9% reported at least one fall-related injury. The most common injuries were bruises, scrapes, and sprains. In strength and control groups, total fall rates rose during the initial half of the intervention but fell below baseline by the end of supervised training and remained low during follow-up. Despite higher fall rates at baseline, the tai ji quan group had a steady decline in falls during the intervention and a slight increase during follow-up (Fig 2A).
FIG 2.
(A) IDRs comparing fall rates across the study period to prior fall history. (B)IDRs comparing fall-related injuries across the study period to prior history of fall injuries. ID, incidence density; IDRs, incidence density ratios.
In prespecified negative binomial analyses, there were no statistically significant differences in fall incidence rates or fall-related injuries comparing tai ji quan and strength with the stretching group over any study period (Table 2). Continued participation in the study exercise program did not moderate incidence rates for falls or fall-related injuries over follow-up.
TABLE 2.
IRRs for Falls Over the Intervention and Follow-Up Periods and Across the Full Study Period
In post hoc analyses using IDRs, there were no significant differences in falls or fall rates within each study group across time intervals (Table 3). However, there was a significantly reduced rate of fall-related injuries in tai ji quan compared with the baseline rate, dropping from 4.3 falls per 100 person-months (95% CI, 2.9 to 5.6) at baseline to 2.4 falls per person-months (95% CI, 1.2 to 3.5) at the end of training (Fig 2B). The reduction in fall-related injuries did not persist during the follow-up period. No difference was observed for fall-related injuries across any period in strength or control groups.
TABLE 3.
ID and IDRs for Falls and Fall-Related Injuries by Exercise Group and Study Assessment Interval
Strength, Balance, and Flexibility
Over the intervention period, strength training significantly increased maximal leg strength (+14.3 kg [95% CI, 11.4 to 17.1]; P = .002) versus stretching (+7.5 kg [95% CI, 4.6 to 10.4]; Table 4). Tai ji quan significantly improved LOS postural control (+2.42% [95% CI, 1.36 to 3.48]) compared with controls (+0.35% [95% CI, –0.69 to 1.38]; P = .007), but SOT scores were not significantly different. Stretching improved lower-body flexibility within the control group (+4.14 cm [95% CI, 3.00 to 5.28]), which was significantly greater than the tai ji quan group (+2.03 cm [95% CI, 0.86 to 3.20]; P = .012), but not strength (+3.03 cm [95% CI, 1.89 to 4.17]; P = .176; Table 4).
TABLE 4.
Changes in Secondary Outcomes and Fear of Falling From Baseline
Using the SAFFE scale, the strength group reported engaging in more activities during the intervention period that significantly differed from decreases reported by controls (P = .043; Table 4).
DISCUSSION
In this randomized controlled trial evaluating nonpharmacologic approaches to mitigate falls and related injuries in older, postmenopausal women who received chemotherapy, tai ji quan and strength training each showed evidence of training fidelity through improved postural control and increased leg strength compared with the control condition. In addition, at 6 months, both tai ji quan and strength training showed a promising downward trend, albeit statistically nonsignificant, in the incidence of falls, and fall rates were shown to be stay unchanged during follow-up. However, participants in the tai ji quan group experienced significantly fewer fall-related injuries over the intervention period compared with their injury rates before enrollment.
Several factors might explain why we did not detect significant reductions in falls from tai ji quan or strength training interventions. First, the study enrolled a younger cohort of women with a lower rate of falls than most fall prevention studies targeting adults older than 65 years and at risk for falling.15 On the basis of our prior work, we presumed women treated with chemotherapy would be at high risk of falls,41 but treatment history alone may be insufficient for identifying fall risk. Future intervention efforts should target older cancer survivors with established fall risk factors (eg, fall history and slow gait speed). Relatedly, a second reason may be that we powered the study to detect a 47% reduction in falls on the basis of our prior studies of tai ji quan in much older adults without cancer, not the 20%-30% reductions we observed in our sample with a lower fall history. However, a post hoc power analysis suggested that we had increased statistical precision (power) because of lower falls outcome dispersion than expected and a larger achieved sample size than planned (see the Data Supplement for details of this power analysis). A recent Cochrane review reported a 23% reduction in falls from exercise in older adults.20 Thus, our observations align with this expected effect size despite not being significant. Although a minimally clinically important reduction in fall rates has not been established for cancer survivors, a 25% reduction in fall rates is considered clinically important in other diseases, such as Parkinson's disease.42 Third, on the basis of the positive trends we observed, the 6-month dose of exercise implemented in this study may be insufficient. A higher frequency or longer duration of supervised training may lead to significantly lower falls, especially in our younger sample of cancer survivors who were relatively well functioning at baseline.19
Notably, although fall reductions were nonsignificant, women randomly assigned to tai ji quan had 45% fewer fall-related injuries during the intervention period, significantly less than baseline rates at study enrollment. Our study's tai ji quan program was specifically designed to challenge neuromuscular and sensory systems involved in postural control and has reduced falls in older adults with neurologic disease.35,43-45 Half of our patient cohort reported neuropathy symptoms at baseline. A secondary data analysis of these data showed that neuropathy symptoms were associated with greater postural sway and falls,46 which could increase risk for fall-related injuries, including hip fracture.47 As such, tai ji quan training appears to be a promising clinical countermeasure to treatment-induced balance impairments that has the potential to reduce injuries from falls among patients with cancer.
Contrary to our hypothesis, strength training did not reduce falls or fall injuries among women treated with chemotherapy. Women reported more falls during the first half of the intervention, yet, falls eventually declined below baseline rates by the end of supervised training and during follow-up. Women in the strength group, who were underactive at enrollment, reported engaging in more activities associated with fall risk over the intervention period. Therefore, they may have heightened their exposure to falling before exercise adaptations would occur.48 Our strength training program focused on functional movements that take 4-6 weeks to learn, while musculoskeletal adaptations take at least 8-12 weeks to manifest.25 Women may have placed themselves at a higher risk of falls before the exercise intervention could be protective. Wolf et al49 described this exercise adaption phenomenon in their study of tai ji quan where transitionally frail older adults who participated in a 12-month trial needed 3 months to learn and master forms before increasing intensity enough to elicit adaptations. Importantly, fall injuries did not increase simultaneously, suggesting that although more falls occurred, they were not serious. In addition, although our program improved leg strength, it is possible that to prevent falls and related injuries, greater improvements in strength from a higher or longer dose of training or possibly adding a balance component may be needed.
Our study has notable strengths that enhanced its rigor. To our knowledge, we are the first to test two evidence-based fall prevention programs to address known risk factors for falls in older adults and target a cancer population likely to have treatment-induced fall risk. Participants were blinded to the primary outcome and our study sample was sufficiently large. We also had high retention rates, adherence, and compliance to training, allowing us to test our hypotheses rigorously. Notwithstanding these strengths, our study had limitations. The choice of a placebo control group that exercised over a nonexercise control may have diminished our ability to detect intervention effects. We accepted this limitation, however, because ethically we could not withhold exercise altogether and it avoided confounding related to attention and social support. Stretching control conditions have had little effect on falls in other studies.21,50-53 Also, although an important finding in this study was a reduction in fall injuries in the tai ji quan arm, we were not powered to examine specific types of injuries. This limitation would be important to explore in future studies as hip and spine fractures are elevated in women with cancer,54 mostly related to falls,55 and are costly and deadly.56 This finding was also drawn from post hoc analysis using an alternative statistical approach than initially planned, so all conclusions must be tempered. Relatedly, it is possible that the higher fall-related injury rates in the tai ji quan group influenced these post hoc findings, which might suggest that the effect is limited to a high-risk group. To avoid this potential bias, future intervention trials should consider stratifying random assignment by baseline fall history.
In summary, despite evidence for fidelity, we did not find that strength or balance-based training, compared with a stretching control, reduced fall and fall-related injuries after chemotherapy in a broad sample of postmenopausal cancer survivors. However, there were some promising data to suggest that high-risk patients with a history of falls may benefit from engaging in regular balance-based exercise regimens after finishing chemotherapy to mitigate injury risk from treatment-related falls.
ACKNOWLEDGMENT
The authors thank all GET FIT participants for their time and effort. The authors would also like to thank Carolyn Guidarelli, Lauren Bumgartner, and Jessica Sitemba for their assistance with project management and data collection. The authors recognize the Oregon State Cancer Registry for their collaboration on recruitment for this trial. The Oregon State Cancer Registry is one of the participating registries funded by the National Program of Cancer Registries under the Centers for Disease Control and Prevention.
Appendix 1. Post hoc power analysis
A manuscript reviewer pointed out that our original a priori power analysis for the falls outcome was based on inaccurate assumptions about the model contrasts to be tested and other model parameters. We discovered that the original power analysis was, in fact, overly pessimistic in several ways. First, we had better recruitment and participant retention than originally estimated, resulting in n = 137-141 participants in each study arm. The original power analysis was based on the assumption of n = 114 in each group. Second, our analyses revealed that Phi (the overdispersion parameter) was best estimated to be 1.0 (making it equivalent to a Poisson regression). The original power analyses had assumed Phi = 2.5. Third, the baseline rate per 1-year exposure time was estimated to be 0.65. By incorporating all of these estimates, including that the primary hypotheses were tested using two separate two-group contrasts, we get the following results:
Power analysis results using PASS 2022.
Input/assumptions: response rate ratio = 0.53, baseline rate = 0.65, mean exposure time = 1, R-squared = 0.25, Phi = 1, distribution of X1 = binomial, proportion = 0.50.
Results: A Poisson regression of a dependent variable of counts on a binary independent variable with proportion = 0.5 using a sample of 200 observations achieves 84% power at a 0.05 significance level to detect a response rate ratio of at least 0.53 because of a one-unit change in the IV. The baseline rate is 0.65 and the mean exposure time is 1. The sample size was adjusted since a multiple regression of the covariate of interest on the other covariates in the Poisson regression is expected to have an R-squared of 0.25.
Thus, we would need n = 100 per group for each two-group hypothesis test to achieve slightly more than 80% power for the effect size used in the original analysis. Since our n per group is larger than this, we actually have more statistical power/precision than originally expected on the basis of the a priori power analysis.
TABLE A1.
Exercise Adherence During and After the Supervised Intervention Period
TABLE A2.
AEs Related or Possibly Related to Study Intervention (n = 11)
Kerri M. Winters-Stone
Consulting or Advisory Role: Bayer
Fay Horak
Employment: APDM-Clario
Research Funding: Pfizer and Biogen (Inst)
Eric J. Roeland
Consulting or Advisory Role: Napo Pharmaceuticals, AIM Specialty Health, Helsinn Therapeutics, Byomass, Veloxis, PRA Health, Actimed Therapeutics, Takeda, MeterHealth
Expert Testimony: Regents of the University of California
Travel, Accommodations, Expenses: Pfizer
No other potential conflicts of interest were reported.
DISCLAIMER
This report does not reflect the opinions of the Veterans Administration, nor those of the US Government.
SUPPORT
Supported by National Cancer Institute (R01CA163474).
CLINICAL TRIAL INFORMATION
AUTHOR CONTRIBUTIONS
Conception and design: Kerri M. Winters-Stone, Fay Horak, Nathan F. Dieckmann, Shiuh-Wen Luoh, Fuzhong Li
Provision of study materials or patients: Kerri M. Winters-Stone, Shiuh-Wen Luoh
Collection and assembly of data: Kerri M. Winters-Stone
Data analysis and interpretation: Kerri M. Winters-Stone, Nathan F. Dieckmann, Shiuh-Wen Luoh, Elizabeth Eckstrom, Sydnee A. Stoyles, Eric J. Roeland, Fuzhong Li
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
GET FIT: A Randomized Clinical Trial of Tai Ji Quan Versus Strength Training for Fall Prevention After Chemotherapy in Older, Postmenopausal Women Cancer Survivors
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/jco/authors/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Kerri M. Winters-Stone
Consulting or Advisory Role: Bayer
Fay Horak
Employment: APDM-Clario
Research Funding: Pfizer and Biogen (Inst)
Eric J. Roeland
Consulting or Advisory Role: Napo Pharmaceuticals, AIM Specialty Health, Helsinn Therapeutics, Byomass, Veloxis, PRA Health, Actimed Therapeutics, Takeda, MeterHealth
Expert Testimony: Regents of the University of California
Travel, Accommodations, Expenses: Pfizer
No other potential conflicts of interest were reported.
REFERENCES
- 1.Wildes TM, Dua P, Fowler SA, et al. : Systematic review of falls in older adults with cancer. J Geriatr Oncol 6:70-83, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Burns ER, Stevens JA, Lee R: The direct costs of fatal and non-fatal falls among older adults—United States. J Saf Res 58:99-103, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stevens JA, Sogolow ED: Gender differences for non-fatal unintentional fall related injuries among older adults. Inj Prev 11:115-119, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Irwin ML, Crumley D, McTiernan A, et al. : Physical activity levels before and after a diagnosis of breast carcinoma: The Health, Eating, Activity, and Lifestyle (HEAL) study. Cancer 97:1746-1757, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tofthagen C, Overcash J, Kip K: Falls in persons with chemotherapy-induced peripheral neuropathy. Supp Care Cancer 20:583-589, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang X, Sun M, Liu S, et al. : Risk factors for falls in older patients with cancer. BMJ Support Palliat Care 8:34-37, 2017 [DOI] [PubMed] [Google Scholar]
- 7.Huang MH, Blackwood J, Godoshian M, et al. : Factors associated with self-reported falls, balance or walking difficulty in older survivors of breast, colorectal, lung, or prostate cancer: Results from Surveillance, Epidemiology, and End Results-Medicare Health Outcomes Survey linkage. PLoS One 13:e0208573, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen TY, Janke MC: Predictors of falls among community-dwelling older adults with cancer: Results from the health and retirement study. Support Care Cancer 22:479-485, 2014 [DOI] [PubMed] [Google Scholar]
- 9.Black FO, Johnson JT, Effron MZ, et al. : Vestibular ototoxicity of prophylactic aminoglycoside antibiotics in head and neck cancer patients. Otolaryngol Head Neck Surg 90:349-354, 1982 [PubMed] [Google Scholar]
- 10.Black FO, Myers EN, Schramm VL, et al. : Cisplatin vestibular ototoxicity: Preliminary report. Laryngoscope 92:1363-1368, 1982 [PubMed] [Google Scholar]
- 11.Kuroi K, Shimozuma K: Neurotoxicity of taxanes: Symptoms and quality of life assessment. Breast Cancer 11:92-99, 2004 [DOI] [PubMed] [Google Scholar]
- 12.Gewandter JS, Fan L, Magnuson A, et al. : Falls and functional impairments in cancer survivors with chemotherapy-induced peripheral neuropathy (CIPN): A University of Rochester CCOP study. Support Care Cancer 21:2059-2066, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Winters-Stone KM, Horak F, Jacobs PG, et al. : Falls, functioning and disability among women with persistent symptoms of chemotherapy-induced peripheral neuropathy. J Clin Oncol 35:2604-2612, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang W, Low LF, Schwenk M, et al. : Review of gait, cognition, and fall risks with implications for fall prevention in older adults with dementia. Dement Geriatr Cogn Disord 48:17-29, 2019 [DOI] [PubMed] [Google Scholar]
- 15.Gillespie LD, Robertson MC, Gillespie WJ, et al. : Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev 15:CD007146, 2010 [DOI] [PubMed] [Google Scholar]
- 16.Panel on Prevention of Falls in Older Persons, American Geriatrics Society and British Geriatrics Society : Summary of the Updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc 59:148-157, 2011 [DOI] [PubMed] [Google Scholar]
- 17.Guo Y, Qiu P, Liu T: Tai ji quan: An overview of its history, health benefits, and cultural value. J Sport Health Sci 3:3-8, 2014 [Google Scholar]
- 18.Li F, Harmer P, Fitzgerald K, et al. : Effectiveness of a therapeutic tai ji quan intervention vs a multimodal exercise intervention to prevent falls among older adults at high risk of falling: A randomized clinical trial. JAMA Intern Med 178:1301-1310, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sherrington C, Fairhall N, Wallbank G, et al. : Exercise for preventing falls in older people living in the community: An abridged Cochrane systematic review. Br J Sports Med 54:885-891, 2020 [DOI] [PubMed] [Google Scholar]
- 20.Sherrington C, Fairhall NJ, Wallbank GK, et al. : Exercise for preventing falls in older people living in the community. Cochrane Database Syst Rev 1:CD012424, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Twiss JJ, Waltman NL, Berg K, et al. : An exercise intervention for breast cancer survivors with bone loss. J Nurs Scholarsh 41:20-27, 2009 [DOI] [PubMed] [Google Scholar]
- 22.Bennett JA, Winters-Stone K, Nail LM, et al. : Definitions of sedentary in physical-activity-intervention trials: A summary of the literature. J Aging Phys Act 14:456-477, 2006 [DOI] [PubMed] [Google Scholar]
- 23.Winters-Stone KM, Li F, Horak F, et al. : Comparison of Tai Chi vs. strength training for fall prevention among female cancer survivors: Study protocol for the GET FIT trial. BMC Cancer 12:577, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Li F, Harmer P, Eckstrom E, et al. : Effectiveness of tai ji quan vs multimodal and stretching exercise interventions for reducing injurious falls in older adults at high risk of falling: Follow-up analysis of a randomized clinical trial. JAMA Netw Open 2:e188280, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chodzko-Zajko WJ, Proctor DN, Fiatarone Singh MA, et al. : American College of Sports Medicine position stand: Exercise and physical activity for older adults. Med Sci Sports Exerc 41:1510-1530, 2009 [DOI] [PubMed] [Google Scholar]
- 26.Campbell KL, Winters-Stone KM, Wiskemann J, et al. : Exercise guidelines for cancer survivors: Consensus statement from international multidisciplinary roundtable. Med Sci Sports Exerc 51:2375-2390, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.American College of Sports Medicine : ACSM's Guildelines for Exercise Testing and Prescription (ed 7). Philadelphia, Lippincott Williams & Wilkins, 2006 [Google Scholar]
- 28.Groll DL, To T, Bombardier C, et al. : The development of a comorbidity index with physical function as the outcome. J Clin Epidemiol 58:595-602, 2005 [DOI] [PubMed] [Google Scholar]
- 29.Stewart AL, Mills KM, King AC, et al. : CHAMPS physical activity questionnaire for older adults: Outcomes for interventions. Med Sci Sports Exerc 33:1126-1141, 2001 [DOI] [PubMed] [Google Scholar]
- 30.Lachman ME, Howland J, Tennstedt S, et al. : Fear of falling and activity restriction: The survey of activities and fear of falling in the elderly (SAFE). J Gerontol B Psychol Sci Soc Sci 53B:P43-P50, 1998 [DOI] [PubMed] [Google Scholar]
- 31.Tinetti ME, Williams CS: Falls, injuries due to falls, and the risk of admission to a nursing home. N Engl J Med 337:1279-1284, 1997 [DOI] [PubMed] [Google Scholar]
- 32.Ford-Smith CD, Wyman JF, Elswick R Jr, et al. : Test-retest reliability of the sensory organization test in noninstitutionalized older adults. Arch Phys Med Rehabil 76:77-81, 1995 [DOI] [PubMed] [Google Scholar]
- 33.Juras G, Słomka K, Fredyk A, et al. : Evaluation of the limits of stability (LOS) balance test. J Hum Kinet 19:39-52, 2008 [Google Scholar]
- 34.Rikli RE, Jones CJ: Senior Fitness Test Manual. Champaign, IL, Human Kinetics, 2001 [Google Scholar]
- 35.Li F, Harmer P, Fisher KJ, et al. : Tai Chi and fall reductions in older adults: A randomized controlled trial. J Gerontol A Biol Sci Med Sci 60:187-194, 2005 [DOI] [PubMed] [Google Scholar]
- 36.Wolf SL, Barnhart HX, Kutner NG, et al. : Reducing frailty and falls in older persons: An investigation of Tai Chi and computerized balance training. Atlanta FICSIT Group. Frailty and injuries: Cooperative studies of intervention techniques. J Am Geriatr Soc 44:489-497, 1996 [DOI] [PubMed] [Google Scholar]
- 37.Signorini DF: Sample size for Poisson regression. Biometrika 78:446-450, 1991 [Google Scholar]
- 38.Oleckno WA: Epidemiology: Concepts and Methods. Long Grove, IL, Waveland Press, 2008 [Google Scholar]
- 39.R Core: A Language and Environment for Statistical Computing. https://CRAN.R-project.org/package=nlme [Google Scholar]
- 40.Pinheiro J, Bates D, DebRoy S, et al. : nlme: Linear and Nonlinear Mixed Effects Models. R Package Version 3.1-153, 2021 [Google Scholar]
- 41.Winters-Stone KM, Torgrimson B, Horak F, et al. : Identifying factors associated with falls in postmenopausal breast cancer survivors: A multi-disciplinary approach. Arch Phys Med Rehabil 92:646-652, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Henderson EJ, Morgan GS, Amin J, et al. : The minimum clinically important difference (MCID) for a falls intervention in Parkinson's: A Delphi study. Parkinsonism Relat Disord 61:106-110, 2019 [DOI] [PubMed] [Google Scholar]
- 43.Li F, Harmer P, Fisher KJ, et al. : Tai Chi: Improving functional balance and predicting subsequent falls in older persons. Med Sci Sports Exerc 36:2046-2052, 2004 [DOI] [PubMed] [Google Scholar]
- 44.Li F, Harmer P, Fitzgerald K, et al. : Tai Chi and postural stability in patients with Parkinson's disease. N Engl J Med 366:511-519, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Li F, Harmer P, Glasgow R, et al. : Translation of an effective Tai Chi intervention into a community-based falls-prevention program. Am J Public Health 98:1195-1198, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fino PC, Horak FB, El-Gohary M, et al. : Postural sway, falls, and self-reported neuropathy in aging female cancer survivors. Gait Posture 69:136-142, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yang Y, Mackey DC, Liu-Ambrose T, et al. : Risk factors for hip impact during real-life falls captured on video in long-term care. Osteoporos Int 27:537-547, 2016 [DOI] [PubMed] [Google Scholar]
- 48.Gregg EW, Cauley JA, Seeley DG, et al. : Physical activity and osteoporotic fracture risk in older women. Study of Osteoporotic Fractures Research Group. Ann Intern Med 129:81-88, 1998 [DOI] [PubMed] [Google Scholar]
- 49.Wolf SL, Sattin RW, Kutner M, et al. : Intense Tai Chi exercise training and fall occurrences in older, transitionally frail adults: A randomized, controlled trial. J Am Geriatr Soc 51:1693-1701, 2003 [DOI] [PubMed] [Google Scholar]
- 50.Brochu M, Savage P, Lee M, et al. : Effects of resistance training on physical function in older disabled women with coronary heart disease. J Appl Physiol 92:672-678, 2002 [DOI] [PubMed] [Google Scholar]
- 51.Alexander NB, Gross MM, Medell JL, et al. : Effects of functional ability and training on chair-rise biomechanics in older adults. J Gerontol A Biol Sci Med Sci 56:M538-M547, 2001 [DOI] [PubMed] [Google Scholar]
- 52.Brown M, Sinacore DR, Ehsani AA, et al. : Low-intensity exercise as a modifier of physical frailty in older adults. Arch Phys Med Rehabil 81:960-965, 2000 [DOI] [PubMed] [Google Scholar]
- 53.Barrett CJ, Smerdely P: A comparison of community-based resistance exercise and flexibility exercise for seniors. Aust J Physiother 48:215-219, 2002 [DOI] [PubMed] [Google Scholar]
- 54.Chen Z, Maricic M, Aragaki AK, et al. : Fracture risk increases after diagnosis of breast or other cancers in postmenopausal women: Results from the Women's Health Initiative. Osteoporos Int 20:527-536, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Berry SD, Miller RR: Falls: Epidemiology, pathophysiology, and relationship to fracture. Curr Osteoporos Rep 6:149-154, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Williams SA, Chastek B, Sundquist K, et al. : Economic burden of osteoporotic fractures in US managed care enrollees. Am J Manag Care 26:e142-e149, 2020 [DOI] [PubMed] [Google Scholar]