Abstract
Callosal agenesis is a complex condition with disruption in the steps such as cellular proliferation, migration, axonal growth, guidance, or glial patterning at the midline. Agenesis of the corpus callosum (AgCC) is associated with diverse midline craniofacial malformations affecting the frontal-cranial and midface skeleton. Diagnosing midline abnormalities prenatally can be challenging, especially in twin pregnancies, due to poor resolution of skull base structures on fetal MRI, basal cephalocele could be mistaken for fluid in the nasopharynx, motion limitation, and fetal positioning. Our case highlights the importance of evaluation for other associated midline anomalies when there is callosal agenesis.
Keywords: agenesis of the corpus callosum, frontonasal dysplasia, fetal MRI, morning glory syndrome
Case presentation
A 25-year-old primigravida with monozygotic (dichorionic, diamniotic) twin pregnancy was seen for a fetal neurologic consultation at 25 weeks gestation with a prenatal diagnosis of agenesis of corpus callosum (AgCC) in Twin B (Figure 1). There was no family history of any genetic or congenital malformations. There were no reported environmental exposures. The limitations of fetal MRI due to motion degradation and the spectrum of varied outcomes of AgCC were discussed with the family. Delivery was by planned cesarean section at 37 weeks. APGAR scores were 8 and 9 and required routine newborn care. Twin B was initially admitted to the neonatal intensive care unit (NICU) preemptively for one week to coordinate consults with Neurosurgery, Neurology, Ophthalmology, and Genetics. During the NICU stay, he was monitored for respiratory and feeding issues. The infant had a mild depression of the midface, a midline incomplete cleft lip, an alveolar cleft, and anomalous optic nerves, consistent with the frontonasal dysplasia syndrome (FND) spectrum, which was not appreciated on the prenatal imaging. The postnatal MRI on the second day of life demonstrated complete AgCC, a large defect along the inferior sella turcica, consistent with the craniopharyngeal canal, with herniation of the adenohypophysis into a cephalocele protruding into the nasopharynx and mild hypertelorism with bilateral optic disc anomalies (Figure 2). A fundoscopic exam confirmed morning glory disc anomalies (Figure 3). The neonate developed episodes of hypoxia, likely attributed to cephalocele obstructing the nasopharynx and underwent tracheostomy and had a prolonged hospitalization from 2 weeks to 6 months age. He was monitored clinically and by serial neuroimaging with a plan for surgery around 18–20 months later. At 17 months of age, he presented with a cerebrospinal fluid leak and underwent endoscopic endonasal surgery for excision of this lesion and repair. Genetic workup included chromosomal microarray and whole exome sequencing. They were non-diagnostic for pathogenic variants. He has developmental delay and walked at 19 months, and he continues to improve with therapies. He uses sign language to communicate and has several sounds with limitations in speech due to tracheostomy. He is social and interactive. The twin brother did not share the dysmorphic facial features, has normal motor development, and is closely monitored for his speech and language skills.
Figure 1.
Prenatal fetal MR: T2-weighted images in the axial (A), coronal (B), and sagittal (C) planes demonstrate a small focal T2 hyperintense signal (white arrows), which extends from the skull base to the nasopharynx, consistent with the cephalocele. Agenesis of the corpus callosum is also present (B).
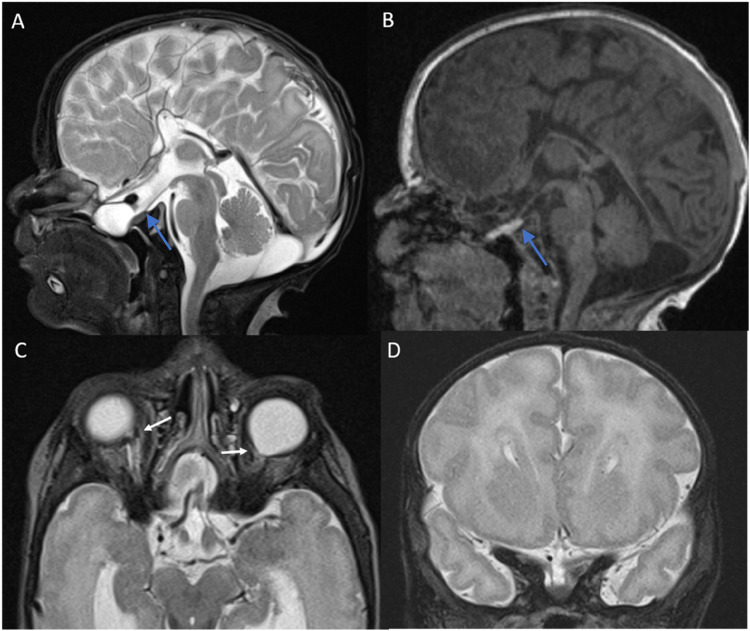
Figure 2.
Postnatal MR: sagittal T2 image (A) and sagittal T1 MPRAGE (B) show a large defect consistent with a craniopharyngeal canal, with herniation of the adenohypophysis into the defect, which protrudes into the nasopharynx (blue arrows). Bilateral optic disc anomalies (C, white arrows) and agenesis of the corpus callosum (D) are also present.
Figure 3.
Fundus examination revealed a normal optic disc within a slight staphyloma in the right eye as well as normal macula and vessels. In the left eye, there was a Morning Glory Disc (large and excavated with vessels leaving from the side with the absence of central vasculature) surrounded by pigmentation (black arrow) that extended to the macula. Please see online publication for color images.
Discussion
Callosal agenesis is a complex condition with disruption in cellular proliferation, migration, axonal growth, guidance, or glial patterning at the midline.1 The incidence of AgCC is 0.5 to 70 in 10000. The prevalence in children with developmental disabilities is about 230 in 10000 (2.3%).2 A study by Hetts and colleagues showed that midline anomalies such as primarily cysts, lipomas, and anomalies of the anterior or hippocampal commissures are the most common supratentorial abnormalities.3 AgCC is associated with diverse midline craniofacial malformations affecting the frontal-cranial and midface skeleton.4–6
FND is the hallmark of several syndromes that may have a variable phenotype due to defective embryological development, most likely during the early induction of the forebrain. FND results from anomalies involving the frontonasal process, midfacial structures, and the primordium of the eyes.4 Callosal agenesis, FND, basal encephalocele, and variable presentation of ocular and facial anomalies have been described under the morning glory syndrome (MGS).4,7 MGS is characterized by a funnel-shaped optic nerve head. It is a primary mesenchymal abnormality. Kindler reported ten cases of congenital optic disc anomaly; the optic nerve head was funnel-shaped; it had a central whitish fibrous tissue and was surrounded by a ring-shaped area of chorioretinal pigmentary disturbance. The retinal vessels originated as multiple straight narrow branches at the edge of the optic disc. He called it the morning glory disc because it resembled a morning glory flower.8,9
Neurodevelopmental outcomes are usually favorable in FND; some children have learning disabilities, behavioral issues, and/or speech and language impairments.4 Intrauterine MRI (iuMRI) or fetal brain MRI is a valuable complement to ultrasound (US) in investigating fetal brain malformations. The standard of care in most centers following an abnormal US study is to obtain fetal MRI to inform counseling and management decisions better. This has been backed by a multicenter, prospective cohort study at 16 fetal medicine centers in the UK.10 The literature regarding the prenatal diagnosis of AgCC associated with FND using fetal MRI and postnatal MRI confirmatory studies is lacking. The iuMRI has a sensitivity of about 90% in diagnosing midline anomalies (corpus callosum agenesis and cavum septum pellucidum).11 Another review by Sotiriadis et al included 132 cases in 16 studies; MRI detected additional cerebral abnormalities in 22.5% of apparently isolated AgCC cases.12 A recent study in 2021 from Turkey showed that cortical malformations were the main anomalies accompanying AgCC. Five of the 18 cases with AgCC had cortical malformation. The midline anomalies were found with a rate of 13.6% in the postnatal period, and the majority of midline anomalies were AgCC. In 32 (16.7%) cases, the prenatal US and fetal MRI were inconsistent with postnatal findings.13 Diagnosing midline abnormalities prenatally can be challenging, especially in twin pregnancy, due to poor resolution of skull base structures on fetal MR (Figure 1); basal cephalocele could be mistaken for fluid in the nasopharynx; motion limitation (Figure 1), and due to fetal positioning. Frick and colleagues evaluated the inter- and intraobserver reliability of different fetal MRI measurements in cases of fetal brain malformations and examined the concordance between ultrasonography (US) and MRI findings. Although the reliability of intrauterine iuMRI was high except for the measurements of the third and fourth ventricles and the corpus callosum.14 Timely recognition of associated syndromic midline anomalies (such as FND) is essential for counseling and planning of delivery and specialist availability for multidisciplinary care of the infant. Our case highlights the importance of evaluation for other associated midline anomalies when there is callosal agenesis.
Our institution does not require ethical approval for reporting individual cases or case series. Verbal informed consent was obtained from a legally authorized representative(s) for anonymized patient information to be published in this article.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Akash Virupakshaiah https://orcid.org/0000-0003-2624-9974
Sonika Agarwal https://orcid.org/0000-0002-0668-6897
Sara Reis Teixeira https://orcid.org/0000-0001-5845-058X
References
- 1.Paul LK, Brown WS, Adolphs R, et al. Agenesis of the corpus callosum: Genetic, developmental and functional aspects of connectivity. Nat Rev Neurosci. 2007;8(4):287-299. doi: 10.1038/nrn2107 [DOI] [PubMed] [Google Scholar]
- 2.Jeret JS, Serur D, Wisniewski K, Fisch C. Frequency of agenesis of the corpus callosum in the developmentally disabled population as determined by computerized tomography. Pediatr Neurosci. 1985;12(2):101-103. doi: 10.1159/000120229 [DOI] [PubMed] [Google Scholar]
- 3.Hetts SW, Sherr EH, Chao S, Gobuty S, Barkovich AJ. Anomalies of the corpus callosum: An MR analysis of the phenotypic spectrum of associated malformations. AJR Am J Roentgenol. 2006;187(5):1343-1348. doi: 10.2214/AJR.05.0146 [DOI] [PubMed] [Google Scholar]
- 4.Richieri-Costa A, Guion-Almeida ML. The syndrome of frontonasal dysplasia, callosal agenesis, basal encephalocele, and eye anomalies - phenotypic and aetiological considerations. Int J Med Sci. 2004;1(1):34-42. doi: 10.7150/ijms.1.34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Farlie PG, Baker NL, Yap P, Tan TY. Frontonasal dysplasia: Towards an understanding of molecular and developmental aetiology. Mol Syndromol. 2016;7(6):312-321. doi: 10.1159/000450533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abele TA, Salzman KL, Harnsberger HR, Glastonbury CM. Craniopharyngeal canal and its Spectrum of pathology. Am J Neuroradiol. 2014;35(4):772-777. doi: 10.3174/ajnr.A3745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nawratzki I, Schwartzenberg T, Zaubermann H, Yanko L. Bilateral morning glory syndrome with midline brain lesion in an autistic child. Metab Pediatr Syst Ophthalmol (1985). 1985;8(2-3):35-36. Accessed August 27, 2022. https://pubmed.ncbi.nlm.nih.gov/3870943/. [PubMed] [Google Scholar]
- 8.Chan RTY, Chan HHL, Collin HB. Morning glory syndrome. Clin Exp Optom. 2002;85(6):383-388. doi: 10.1111/J.1444-0938.2002.TB02390.X [DOI] [PubMed] [Google Scholar]
- 9.Kindler P. Morning glory syndrome: Unusual congenital optic disk anomaly. Am J Ophthalmol. 1970;69(3):376-384. doi: 10.1016/0002-9394(70)92269-5 [DOI] [PubMed] [Google Scholar]
- 10.Griffiths PD, Bradburn M, Campbell MJ, et al. Use of MRI in the diagnosis of fetal brain abnormalities in utero (MERIDIAN): A multicentre, prospective cohort study. Lancet. 2017;389(10068):538-546. doi: 10.1016/S0140-6736(16)31723-8 [DOI] [PubMed] [Google Scholar]
- 11.Manganaro L, Bernardo S, Antonelli A, Vinci V, Saldari M, Catalano C. Fetal MRI of the central nervous system: State-of-the-art. Eur J Radiol. 2017;93:273-283. doi: 10.1016/J.EJRAD.2017.06.004 [DOI] [PubMed] [Google Scholar]
- 12.Sotiriadis A, Makrydimas G. Neurodevelopment after prenatal diagnosis of isolated agenesis of the corpus callosum: An integrative review. Am J Obstet Gynecol. 2012;206(4):337.e1-337.e5. doi: 10.1016/J.AJOG.2011.12.024 [DOI] [PubMed] [Google Scholar]
- 13.Eyüboğlu İ, Dinç G. Fetal US and MRI in detection of craniospinal anomalies with postnatal correlation: Single-center experience. Turk J Med Sci. 2021;51(3):1211-1219. doi: 10.3906/sag-2011-122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Frick N, Fazelnia C, Kanzian K, et al. The reliability of fetal MRI in the assessment of brain malformations. Fetal Diagn Ther. 2015;37(2):93-101. doi: 10.1159/000363652 [DOI] [PubMed] [Google Scholar]