Abstract
Objective
health care workers (HCWs) represent a vulnerable group in the COVID-19 pandemic, given the exposure to greater risk and higher levels of work-related stress. Neurofeedback (NF) has shown to be effective in the treatment of stress-related symptoms. We aimed to assess the effectiveness of an alpha-increase NF protocol for the treatment of acute stress symptoms in HCWs exposed to the COVID-19 pandemic.
Method
eighteen medical doctors on duty during the COVID-19 health emergency underwent an intensive NF alpha-increase protocol. The mean alpha wave values were recorded at the beginning (T0) and at the last day of stimulation (T1). Rapid Stress Assessment: Italian version; Copenhagen Burnout Inventory (CBI); Pittsburgh Sleep Quality Index (PSQI), and Brief-COPE were administered as psychometric assessment.
Results
a significant increase in alpha wave values and a significant reduction of the PSQI scores from T0 to T1 were found.
Conclusions
NF alpha-increase protocol showed promising results in terms of stress modulation, sleep quality improvement, and safety in a pilot sample of HCWs.
Keywords: neurofeedback, alpha-increase protocol, sleep quality, health care workers, stress, Covid-19
Introduction
From December 2019, the COVID-19 pandemic has rapidly spread worldwide, being identified as a health emergency of global interest (WHO, 2020). Among the at-risk individuals, health workers represent a particularly vulnerable group, given the greater risk of exposure and the higher levels of work-related stress (Mak et al., 2010; Liu et al., 2020)
As previously observed during past health emergencies, major consequences among the health workers involved include increased rates of burnout, anxious and depressive symptoms up to the development of a post-traumatic stress disorder, both during the epidemic and in the following months and years (WHO, 2020; Mak et al., 2009; Au et al., 2004).
Severe acute respiratory syndrome (SARS) was the first massive infectious disease outbreak in the 21st century, with a psychological impact comparable to other major disasters. Previous studies showed that 10%–35% of SARS survivors reported having features of anxiety, depression, or both at 1 month after discharge (Au et al., 2004; Wu et al., 2005; Hawryluck et al., 2004) and revealed that post-traumatic stress disorder (PTSD) was the most prevalent long-term psychiatric condition. This condition was present in 47.8% of patients, while 25.5% continue to meet PTSD criteria at 30 months post-SARS (Mak et al., 2009). In addition, those who had been isolated worked in high-risk workplaces such as SARS wards or had close relatives who contracted SARS were two to three times more likely to develop high levels of Posttraumatic Stress Symptoms (PTSS) than those who were not exposed to the virus (Wu et al., 2009).
Also, psychiatric symptoms of PTSD, depression, and anxiety have been described among health care workers during the SARS epidemic (Lin et al., 2007) and 2 years (Lancee, Maunder & Goldbloom, 2008) after the end of the epidemic.
Aware of the experience of the latest massive epidemic, several studies have investigated the impact of the Covid-19 epidemic on mental health. Two studies investigated mental health issues in COVID-19 patients finding a high level of PTSD (96.2%) (Bo, 2020) and significantly higher levels of depressive symptoms (29.2%) (Zhang et al., 2020).
Health care workers (HCWs) may be particularly hit by the psychological consequences of COVID-19. Research on HCWs has revealed that approximately 50% of physicians have reported poor sleep quality during the pandemic, which may be attributed to the contagious nature of COVID-19 (Zhang et al., 2020; Qiu, Yu, Li, Li & Xiao, 2020) and the emergency nature of their work (Zhang et al., 2020). Moreover, several studies have reported that depressive symptoms, anxiety and sleep disorders were increased in HCWs (Lu et al., 2020; Xue et al., 2020; Zhang et al., 2020). Significantly higher mean levels of fear, anxiety and depression were found among medical staff compared to administrative staff (Xue et al., 2020; Li et al., 2020). Moreover, frontline workers in particular, who are directly involved in management of patients with COVID-19, had a higher risk of insomnia and somatization compared to non-health workers (Xue et al., 2020; Zhang et a., 2020).
Furthermore, another stressor for HCWs is the “well-being” of their families (Shanafelt, Ripp, & Trockel, 2020). An online survey conducted by University of Arkansas for Medical Sciences to assess and ensure “well-being” of their physicians found that the primary worry of all HCWs was the safety of their families during the COVID-19 pandemic, which was regarded as a major anxiety stress factor (Berg, 2020). The lack of adequate personal protective equipment (PPE), which poses a threat to self as well as the family of HCWs, was another significant factor associated with higher levels of anxiety and poor sleep outcomes. In a significant number of HCWs the unavailability of adequate PPE highly correlated with poor sleep scores and moderate-to-severe anxiety levels on the 7-item anxiety scale (GAD-7) (Spitzer, Kroenke, Williams & Löwe, 2006). In addition, poor sleep outcomes have been reported particularly among female participants (Jahrami et al., 2020; ter Horst, de Kloet, Schächinger & Oitzl MS, 2012).
Although the psychological impact of health emergencies on health professionals is well known, the prevention protocols and management of psychiatric symptoms in at-risk populations are still under evaluation.
Neurofeedback (NF), a safe and non-invasive technique, has shown to be effective in several psychiatric disorders. NF consists of a brain neuromodulation technique with the target of training participants in the self-regulation of neural substrates underlying specific behaviours or pathologies (Demos, 2005; Coben & Evans, 2022).
In particular, alpha waves of the brain are associated with the process of relaxation, so protocols based on the increase of those frequencies are used for the add-on treatment of various diseases, including stress and anxiety related symptoms and sleep disturbances (Marzbani, Marateb & Mansourian, 2016; Panisch & Hai, 2020), showing decreased symptoms of depression and anxiety from pre-to post-training (Wang et al., 2019; Mennella, Patron & Palomba, 2017).
The aim of the present study was to assess safety, feasibility, and effectiveness of an alpha-increase NF protocol in healthcare workers involved in the COVID-19 health emergency in Milan, a city particularly hit by the pandemic.
Methods
Eighteen medical doctors on duty during the COVID-19 health emergency and belonging to the Psychiatry 2 Unit of ASST Fatebenefratelli-Sacco, Milan, Italy were recruited and underwent an intensive 10 sessions NF alpha-increase protocol during two consecutive weeks, between 1st June and 30th June 2020.
The inclusion criteria for this study were (1) male and female HCWs; (2) full-time practicing doctors, nurses, and paramedic staff directly involved in providing any kind of patient-related care; (3) age ≥18 years.
All procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. All participants involved in the study provided written informed consent for research purposes.
The sessions were carried out by trained professionals at the end of health workers' work shifts in a dedicated quiet space. The mean values of the alpha waves were recorded during each session. More in detail, each of the scheduled 10 sessions consisted of:
a preparation phase: a screen-printed cap was placed on the subject's head, followed by occipital cephalic areas (Oz) and neutral (ground - on the subject's arm) electrodes positioning. To promote better conductivity an abrasive cream and an electroconductive gel were applied to subjects’ skin before electrode positioning.
NF protocol: 20 minutes of stimulation with a 4-channels Rehacor T stimulator (Medicom MTD Ltd) consisting of visual and auditory scenarios, mainly: diagrams, geometric figures, graphic arts, images, slides, videos, linear distortions, slides, and video changes; different audio fragments, sounds of nature, voice information, noisy distortions. During the protocol, participants received feedback regarding their training scores both with audio and visual messages.
Final phase: electrodes and cap removal.
In order to measure the main psychometric features of stress-related disorders, subjects were assessed at the beginning (T0) and on the last day of stimulation (T1- fourteen days after T0), with the following self-administered psychometric questionnaires: Rapid Stress Assessment: Italian version (Tarsitani & Biondi, 1999); Copenhagen Burnout Inventory (CBI) (Kristensen, Borritz, Villadsen & Christensen, 2005); Pittsburgh Sleep Quality Index (PSQI) (Buysse et al., 1989); Brief-COPE (Carver, 1997).
Statistical analyses were performed with paired samples t-test for continuous variables. Both the overmentioned scale scores values and the mean values of alpha frequencies were compared at T0 and T1. Moreover, we performed an additional comparison of the values of alpha frequencies at the beginning (B) and at the end (E) of the T0 and T1 sessions for each participant.
All analyses were performed using Statistical Package for the Social Sciences (SPSS) 25.0 software for Windows (SPSS Inc, Chicago, IL, USA). The statistical significance level was set at p < 0.05.
Results
The sample included 18 medical doctors with a 77.8% female rate and a mean age of 32.22 ± 8.14 years (min 27- max 57 years old). Subjects did not report past or present psychiatric disorders or psychiatric family history. Moreover, no medical comorbidities were reported. After the conclusion of the NF alpha increase protocol, none of the participants experienced side effects.
A paired-samples t-test was conducted to evaluate alpha waves frequencies values between T0 and T1 registration phases (beginning –B - and end – E). Comparison of alpha waves frequencies values between T0 and T1 registration phases are provided in table 1. A statistically significant decrease in alpha wave values emerged between B and E phases at T0 (22.75 ± 13.18 vs 28.72 ± 12.27, t(17)=-2.54; p<0.05). The eta squared statistic is .60 which in Cohen’s terms indicated a large effect size (Cohen, 1998).
Table 1.
Comparison of alpha waves between neurofeedback registration phases
| Alpha waves | T0 | T1 | ||||
|---|---|---|---|---|---|---|
| m | sd | m | sd | P value | Cohen’s d | |
| B-phase alpha | 22.75 | 13.18 | 29.36 | 12.96 | .046 | -.506 |
| E-phase alpha | 28.72 | 12.27 | 25.75 | 10.24 | .267 | -.60033 |
| P value | .021 | .066 | ||||
Notes. Data presented as mean and standard deviations. Abbreviations. m, mean; sd, standard deviation; B-phase: beginning of neurofeedback session; E-phase: end of neurofeedback session.
In addition, a significant increase in alpha wave values was found comparing B phases between T0 and T1 (22.75 ± 13.18 vs 29.36 ± 12.96, t(17)= -2.14; p<0.05; see figure 1). The eta squared statistic (.50) indicated a medium effect size (Cohen, 1998).
Figure 1.
Comparison of alpha waves between registration phases
Notes. NF: neurofeedback. Boldface indicates parameters with statistically significant differences between the two subgroups; **p<0.005 *p<0.05.
As regards mean alpha frequencies values comparison between T0 and T1, no statistically significant differences emerged.
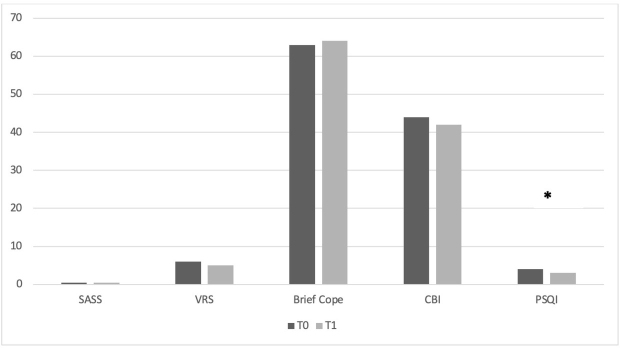
Concerning self-administered psychometric questionnaires, a significant reduction in PSQI test scores between T0 and T1 was observed (4.25 ± 2.01 vs 3.68 ± 2.02, t(15)=2.52 ; p<0.05; see figure 2). The eta squared statistic (.60) indicated a large effect size (Cohen, 1998). No significant differences emerged for Rapid Stress Assessment, Copenhagen Burnout Inventory (CBI), and Brief-Cope questionnaires between T0 and T1 (see table 2).
Figure 2.
Comparison of psychometric questionnaires between T0 and T1
Notes. NF: neurofeedback. Boldface indicates parameters with statistically significant differences between the two subgroups; **p<0.005 *p<0.05.
Table 2.
Comparison of psychometric questionnaires between T0 and T1
| T0 | T1 | |||||
|---|---|---|---|---|---|---|
| m | sd | m | sd | P value | Cohen’s d | |
| Rapid Stress Assessment | 6.50 | 4.0 | 5.56 | 3.09 | .279 | .2649 |
| Brief Cope | 63.5 | 6.38 | 64.18 | 6.19 | .467 | -.176 |
| CBI | 44.56 | 8.09 | 42.68 | 8.92 | .131 | .377 |
| PSQI | 4.25 | 2.01 | 3.68 | 2.02 | .023 | .5944 |
Notes. Data presented as mean and standard deviations. Abbreviations. CBI, Copenhagen Burnout Inventory; PSQI, Pittsburgh Sleep Quality Index; m, mean; sd, standard deviation.
Discussion
The present study examined the effectiveness of an alpha-increase NF protocol for the treatment of stress-related symptoms in healthcare workers exposed to the COVID-19 pandemic.
Our data showed a significant increase in alpha waves both between B and E phases at T0 and in the B phase between T0 and T1. Alpha waves are usually associated with alert relaxation (Evans & Abarbanel, 1999). Therefore, this result may indicate that NF alpha-increase protocol could modulate stress and anxiety in health care workers exposed to the COVID-19 pandemic. Wang et al. investigated the effects of alpha asymmetry and high-beta down-training neurofeedback for patients with major depressive disorder and anxiety symptoms, finding an improvement in symptoms of depression and anxiety in both neurofeedback groups (Wang et al., 2019).
In particular, alpha frequencies are implicated in the process of relaxation eventually leading to sleep (Marzbani et al., 2016). This is consistent with our results. In fact, when considering self-administrated psychometric questionnaires, we found a significant reduction in PSQI test scores, potentially indicating that NF could improve sleep quality. This finding could support the use of NF in healthcare workers exposed to Covid-19-related stress as sleep disorders represent one of the main disorders in this population (Lu et al., 2020; Xue et al., 2020). As noted, approximately 50% of HCWs have reported poor sleep quality during the pandemic period (Zhang et al., 2020; Qiu, Yu, Li, Li & Xiao, 2020).
No significant improvements emerged when considering other assessed psychometrics questionnaires such as VRS, CBI, and Brief-Cope, however this result could be related to the small sample size or to higher resilience features of the selected sample.
Finally, it has to be noticed that none of the participants experienced side effects, confirming the safety of NF technique, which could represent a rapid, straightforward, and non-invasive brain technique modulating potential risk factors for anxiety-related symptoms in healthcare workers.
The limitation of this study is the small sample size, which should be expanded to better assess the role of neurofeedback on stress modulation and sleep quality and the selected sample of healthcare workers. Further studies with larger samples and longitudinal follow-up are therefore warranted to confirm our preliminary results. Involvement of other departments may also be crucial.
References
- Au A, Chan I, Li P, Chan J, Chan YH, Ng F. Correlates of psychological distress in discharged patients recovering from acute respiratory syndrome in Hong Kong. The International Journal of Psychosocial Rehabilitation. 2004;8:41–51. [Google Scholar]
- Berg S. Survey: Doctors’ big COVID-19 worry is keeping their families safe. AMA - Physician Health. 2020. May. https://www.ama-assn.org/practice-management/physician-health/survey-doctors-big-covid-19-worry-keeping-their-families-safe
- Bo, H. X., Li, W., Yang, Y., Wang, Y., Zhang, Q., Cheung, T., Wu, X., & Xiang, Y. T. (2021). Posttraumatic stress symptoms and attitude toward crisis mental health services among clinically stable patients with COVID-19 in China. Psychological medicine, 51(6), 1052–1053. 10.1017/S0033291720000999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buysse, D. J., Reynolds, C. F., 3rd, Monk, T. H., Berman, S. R., & Kupfer, D. J. (1989). The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry research, 28(2), 193–213. 10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- Carver C. S. (1997). You want to measure coping but your protocol's too long: consider the brief COPE. International journal of behavioral medicine, 4(1), 92–100. 10.1207/s15327558ijbm0401_6 [DOI] [PubMed] [Google Scholar]
- Coben, R., Evans, J.R. (2011). Neurofeedback and Neuromodulation Techniques and Applications. London: Elsevier. [Google Scholar]
- Cohen, J. W. (1988). Statistical power analysis for the behavioral sciences (2nd edn). Hillsdale, NJ: Lawrence Erlbaum Associates. [Google Scholar]
- Demos, J. N. Getting started with neurofeedback (2005). New York: W. W. Norton [Google Scholar]
- Evans, J. R., Abarbanel, A. (1999). Introduction to quantitative EEG and neurofeedback. APA Academic Press. [Google Scholar]
- Hawryluck, L., Gold, W. L., Robinson, S., Pogorski, S., Galea, S., & Styra, R. (2004). SARS control and psychological effects of quarantine, Toronto, Canada. Emerging infectious diseases, 10(7), 1206–1212. 10.3201/eid1007.030703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jahrami, H., BaHammam, A. S., AlGahtani, H., Ebrahim, A., Faris, M., AlEid, K., Saif, Z., Haji, E., Dhahi, A., Marzooq, H., Hubail, S., & Hasan, Z. (2021). The examination of sleep quality for frontline healthcare workers during the outbreak of COVID-19. Sleep & breathing = Schlaf & Atmung, 25(1), 503–511. 10.1007/s11325-020-02135-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline C. (2013). Encyclopedie of Behavioral Medicine. Gellman MD, Turner JR editors. New York: Springer. [Google Scholar]
- Kristensen, T.S., Borritz M., Villadsen, E., Christensen, K.B. (2005). The Copenhagen Burnout Inventory: a new tool for the assessment of burnout. Work Stress. 19:192‐207. [Google Scholar]
- Lancee, W. J., Maunder, R. G., Goldbloom, D. S., & Coauthors for the Impact of SARS Study (2008). Prevalence of psychiatric disorders among Toronto hospital workers one to two years after the SARS outbreak. Psychiatric services (Washington, D.C.), 59(1), 91–95. 10.1176/ps.2008.59.1.91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, X., Yu, H., Bian, G., Hu, Z., Liu, X., Zhou, Q., Yu, C., Wu, X., Yuan, T. F., & Zhou, D. (2020). Prevalence, risk factors, and clinical correlates of insomnia in volunteer and at home medical staff during the COVID-19. Brain, behavior, and immunity, 87, 140–141. 10.1016/j.bbi.2020.05.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin, C. Y., Peng, Y. C., Wu, Y. H., Chang, J., Chan, C. H., & Yang, D. Y. (2007). The psychological effect of severe acute respiratory syndrome on emergency department staff. Emergency medicine journal : EMJ, 24(1), 12–17. 10.1136/emj.2006.035089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, N., Zhang, F., Wei, C., Jia, Y., Shang, Z., Sun, L., Wu, L., Sun, Z., Zhou, Y., Wang, Y., & Liu, W. (2020). Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: Gender differences matter. Psychiatry research, 287, 112921. 10.1016/j.psychres.2020.112921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu W, Wang H, Lin Y, Li L. Psychological status of medical workforce during the COVID-19 pandemic: A cross-sectional study. Psychiatry Res. 2020; 288:112936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mak, I. W., Chu, C. M., Pan, P. C., Yiu, M. G., & Chan, V. L. (2009). Long-term psychiatric morbidities among SARS survivors. General hospital psychiatry, 31(4), 318–326. 10.1016/j.genhosppsych.2009.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mak, I. W., Chu, C. M., Pan, P. C., Yiu, M. G., Ho, S. C., & Chan, V. L. (2010). Risk factors for chronic post-traumatic stress disorder (PTSD) in SARS survivors. General hospital psychiatry, 32(6), 590–598. 10.1016/j.genhosppsych.2010.07.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marzbani, H., Marateb, H. R., & Mansourian, M. (2016). Neurofeedback: A Comprehensive Review on System Design, Methodology and Clinical Applications. Basic and clinical neuroscience, 7(2), 143–158. 10.15412/J.BCN.03070208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mennella, R., Patron, E., & Palomba, D. (2017). Frontal alpha asymmetry neurofeedback for the reduction of negative affect and anxiety. Behaviour research and therapy, 92, 32–40. 10.1016/j.brat.2017.02.002 [DOI] [PubMed] [Google Scholar]
- Panisch, L. S., & Hai, A. H. (2020). The Efectiveness of Using Neurofeedback in the Treatment of Post-Traumatic Stress Disorder: A Systematic Review. Trauma, violence & abuse, 21(3), 541–550. 10.1177/1524838018781103 [DOI] [PubMed] [Google Scholar]
- Qiu, D., Yu, Y., Li, R. Q., Li, Y. L., & Xiao, S. Y. (2020). Prevalence of sleep disturbances in Chinese healthcare professionals: a systematic review and meta-analysis. Sleep medicine, 67, 258–266. 10.1016/j.sleep.2019.01.047 [DOI] [PubMed] [Google Scholar]
- Shanafelt, T., Ripp, J., & Trockel, M. (2020). Understanding and Addressing Sources of Anxiety Among Health Care Professionals During the COVID-19 Pandemic. JAMA, 323(21), 2133–2134. 10.1001/jama.2020.5893 [DOI] [PubMed] [Google Scholar]
- Spitzer, R. L., Kroenke, K., Williams, J. B., & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: the GAD-7. Archives of internal medicine, 166(10), 1092–1097. 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- Tarsitani, L., Biondi, M. (1999). Development and validation of the VRS, a rating scale for rapid stress assessment. Medicina Psicosomatica. 44:163-177. [Google Scholar]
- ter Horst, J. P., de Kloet, E. R., Schächinger, H., & Oitzl, M. S. (2012). Relevance of stress and female sex hormones for emotion and cognition. Cellular and molecular neurobiology, 32(5), 725–735. 10.1007/s10571-011-9774-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, S. Y., Lin, I. M., Fan, S. Y., Tsai, Y. C., Yen, C. F., Yeh, Y. C., Huang, M. F., Lee, Y., Chiu, N. M., Hung, C. F., Wang, P. W., Liu, T. L., & Lin, H. C. (2019). The effects of alpha asymmetry and high-beta down-training neurofeedback for patients with the major depressive disorder and anxiety symptoms. Journal of affective disorders, 257, 287–296. 10.1016/j.jad.2019.07.026 [DOI] [PubMed] [Google Scholar]
- WHO. Director-General’s opening remarks at the media briefing on COVID19, 2020. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19-11-march-2020. Accessed 15 Jan 2021
- Wu, K. K., Chan, S. K., & Ma, T. M. (2005). Posttraumatic stress, anxiety, and depression in survivors of severe acute respiratory syndrome (SARS). Journal of traumatic stress, 18(1), 39–42. 10.1002/jts.20004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu, P., Fang, Y., Guan, Z., Fan, B., Kong, J., Yao, Z., Liu, X., Fuller, C. J., Susser, E., Lu, J., & Hoven, C. W. (2009). The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Canadian journal of psychiatry. Revue canadienne de psychiatrie, 54(5), 302–311. 10.1177/070674370905400504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xue, Z., Lin, L., Zhang, S., Gong, J., Liu, J., & Lu, J. (2020). Sleep problems and medical isolation during the SARS-CoV-2 outbreak. Sleep medicine, 70, 112–115. 10.1016/j.sleep.2020.04.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, C., Yang, L., Liu, S., Ma, S., Wang, Y., Cai, Z., Du, H., Li, R., Kang, L., Su, M., Zhang, J., Liu, Z., & Zhang, B. (2020). Survey of Insomnia and Related Social Psychological Factors Among Medical Staff Involved in the 2019 Novel Coronavirus Disease Outbreak. Frontiers in psychiatry, 11, 306. 10.3389/fpsyt.2020.00306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, J., Lu, H., Zeng, H., Zhang, S., Du, Q., Jiang, T., & Du, B. (2020). The differential psychological distress of populations affected by the COVID-19 pandemic. Brain, behavior, and immunity, 87, 49–50. 10.1016/j.bbi.2020.04.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, W. R., Wang, K., Yin, L., Zhao, W. F., Xue, Q., Peng, M., Min, B. Q., Tian, Q., Leng, H. X., Du, J. L., Chang, H., Yang, Y., Li, W., Shangguan, F. F., Yan, T. Y., Dong, H. Q., Han, Y., Wang, Y. P., Cosci, F., & Wang, H. X. (2020). Mental Health and Psychosocial Problems of Medical Health Workers during the COVID-19 Epidemic in China. Psychotherapy and psychosomatics, 89(4), 242–250. 10.1159/000507639 [DOI] [PMC free article] [PubMed] [Google Scholar]