Abstract
Purpose
There has been no report of sex-specific, pediatric age-adjusted shock index (PASI) for pediatric trauma patients in previous studies. We aimed to determine the association between the PASI and in-hospital mortality of pediatric trauma patients and whether this association differs depending on sex.
Materials and Methods
This is a prospective, multinational, and multicenter cohort study using the Pan-Asian Trauma Outcome Study (PATOS) registry in the Asia-Pacific region, conducted in pediatric patients who visited the participating hospitals. The main exposure of our study was abnormal (elevated) PASI measured in an emergency department. The main outcome was in-hospital mortality. We performed a multivariable logistic regression analysis to estimate the association between abnormal PASI and study outcomes after adjusting for potential confounders. An interaction analysis between PASI and sex was also conducted.
Results
Of 6280 pediatric trauma patients, 10.9% (686) of the patients had abnormal PASI. In multivariable logistic regression analysis, abnormal PASI was significantly associated with increased in-hospital mortality [adjusted odds ratios (aOR), 1.74; 95% confidence interval (CI), 1.13–2.47]. Abnormal PASI had interaction effects with sex for in-hospital mortality (aOR, 1.86; 95% CI, 1.19–2.91 and aOR, 1.38; 95% CI, 0.58–2.99 for male and female, respectively) (p<0.01).
Conclusion
Abnormal PASI is associated with increased in-hospital mortality in pediatric trauma patients. The prediction power of PASI for in-hospital mortality was maintained only in male patients.
Keywords: Trauma, pediatrics, shock index, sex
INTRODUCTION
Traumatic injury is leading cause of mortality and morbidity in pediatric patients worldwide.1 While the burden of pediatric trauma has shown substantial geographic differences and the Asian region accounts for a significant number of pediatric trauma-related mortality worldwide, there are very limited studies on pediatric trauma in the Asian region.2
Rapid and accurate identification of severe trauma patients and appropriate triage are important in reducing mortality.3 In recent years, research studies have focused on evidence-based criteria for determining trauma team activation or treatment direction of trauma patients; these criteria help optimize the classification of such patients and efficiently distribute trauma-related resources.4
The shock index (SI), defined as the heart rate (HR) divided by systolic blood pressure (SBP), has been used to predict mortality and the need for massive transfusions, even in the presence of severe trauma.5,6,7 However, as limitations have been reported in applying the SI equally to all age groups, the pediatric age-adjusted shock index (PASI) values have subsequently been defined to account for variations in physiologically normal ranges displayed in pediatric populations.3 The PASI has been validated in pediatric trauma patients by demonstrating its utility in predicting the severity of injury, need for blood transfusion, surgical procedures, and mortality.3,8,9
Although there are no reports of sex-specific SI or PASI, a previous report on the sex-specific normal value of SI stated that the SI of females patients tended to be higher than those of male patients of all ages.10 Therefore, the changing patterns of physiological indicators, including SBP and HR after trauma, may differ according to age and sex.11
Studies on the prediction utility of PASI are limited in pediatric trauma patients, and no study has considered physiological differences according to sex. Therefore, we hypothesized that the PASI can predict the mortality of pediatric trauma patients, and that these prediction utilities would differ according to sex.
Our study aimed to determine the association between the PASI and mortality in pediatric trauma patients and whether this association differs depending on sex.
MATERIALS AND METHODS
Study design and setting
This study was a cross-sectional study using a prospective multicenter trauma registry from the Pan-Asian Trauma Outcomes Study (PATOS) database in the Asia-Pacific region from January 2015 to December 2020.12
The PATOS, a unique, self-funded, low-cost model of the collaborative clinical research network, was first launched in 2013 to build a multicenter registry for injured patients in Asia-Pacific countries. The 85 centers voluntarily participating in this network are from China, India, Japan, Korea, Laos, Malaysia, Philippines, Singapore, Taiwan, Thailand, the UAE, and Vietnam. The age-standardized mortality rate per 100000 injured population in the participating countries varies from 25.8 in Japan to 91.4 in India.12 There are many differences in trauma systems in Asia-Pacific countries, including emergency medical service (EMS) systems.13 The operation of the EMS system varies between different countries: fire-based in four countries, volunteer-based in two countries, and public health-based in one country. The highest level of EMS providers is doctors in five countries, intermediate emergency medical technician (EMT) in four countries, EMT paramedic in one country, EMT basic in one country, and multiple levels in one country. Regarding the national trauma registry, a registry system has not been established in most low- and middle-income countries; and even if such a registry system exists, the registry is often rudimentary and incomplete.14
Data sources
The PATOS database is a multicenter trauma registry compiled by the Asia-Pacific clinical research network. This study reports on injured patients transferred to the emergency departments (ED) of participating hospitals by EMS and various other vehicles in developing countries. Information on patients who visit the ED is entered into the registry system within 1 week. Only patients related to traffic accidents, falls, poisoning, burns, and violence (self-inflicted violence, assault, or acts of war),15 which are the case definition of the trauma by the World Health Organization, were included. Prehospital information was collected from the ambulance run sheet and EMS dispatch records, and hospital information was obtained from the in-hospital discharge record. Information on long-term outcomes was collected at 6 and 12 months after hospital discharge through a telephone survey by investigators. All variable definitions and coding instructions are contained in the data dictionary and distributed to participating hospitals. The data are then collected using an electronic data capture system (http://epatos.org), and the collected data are managed and cleaned by the PATOS Data Quality Management Committee (QMC) to address incomplete and/or invalid entries. All sites respond to the PATOS data QMC within 2 weeks of receiving data verification requests.
Study population
The population of our study consisted of pediatric patients with traumatic injury aged <18 years who visited the participating hospitals between January 2015 and December 2020. Patients aged <3 years (36 months after birth) were excluded as the normal range of vital signs varies drastically by month, and the normal range of PASI values in this population was not clearly categorized in previous studies. Cases with unknown information on SBP, HR, and clinical outcomes at hospital discharge were also excluded.
Variables and measurements
The main exposure of our study was elevated PASI, defined as SI greater than the maximum age-adjusted SI. Cut-offs included SI >1.22 (age, 4–6), >1.0 (7–12), and >0.9 (13–18). Maximum age-adjusted SI was based on published normal ranges compiled from two pediatric textbooks and the U.S. Department of Health and Human Services Pediatric Basic and Advanced Life Support Guidelines.16,17 We collected data on patients’ demographics (country of residence, age, and sex), injury characteristics (intentionality, place of injury, activity at the time of injury, and mechanism of injury), prehospital care (EMS use, fluid resuscitation, and immobilization), ED and hospital care (injury area and vital signs at ED arrival including SBP, HR, and Glasgow Coma Scale), and New Injury Severity Score (NISS). NISS was defined as the sum of the squares of the Abbreviated Injury Scale score in each of the patient’s three most severely injured body region and clinical outcomes at the time of hospital discharge.12
Main outcomes
The primary outcome measure was mortality at hospital discharge, and the secondary outcome measure was poor functional recovery at hospital discharge, measured by the modified Rankin Scale (mRS); poor functional recovery was defined by mRS scores of 4 (moderately severe disability), 5 (severe disability), and 6 (death).
Statistical analysis
We compared the characteristics of patients according to the PASI measure in the ED just after hospital arrival using the chi-square test for categorical variables and the Wilcoxon rank-sum test for nonparametrically distributed continuous variables.
Multivariable logistic regression analyses were performed to estimate the effect size of PASI for in-hospital mortality and poor functional recovery after adjusting for potential confounders (age, sex, comorbidities, intentionality, place of injury, activity, and mechanism of injury). Adjusted odds ratios (aORs) with 95% confidence intervals (CIs) were calculated. Finally, to calculate the prediction power of PASI according to sex, we used multivariable logistic regression model with an interaction term (PASI×sex) as the final model for the outcomes.
All statistical analyses were performed using SAS version 9.4 (SAS institute Inc., Cary, NC, USA). All p-values were two-tailed, and p<0.05 was considered statistically significant.
Ethics statement
This study complies with the Declaration of Helsinki. This study was approved by the Institutional Review Board (IRB) of Seoul National University Hospital and the PATOS Research Coordinating Centre (IRB No. SNUH-1509-045-702), and the requirement for informed consent was waived due to the retrospective nature of this study.
RESULTS
Demographic findings
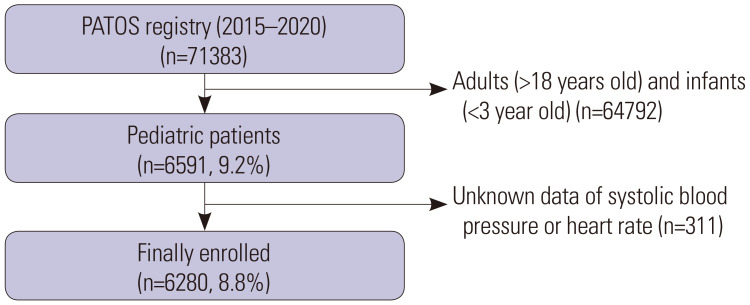
A total of 6280 pediatric trauma patients were finally enrolled in the study. We excluded patients aged >18 years and <3 years and patients with unknown data on SBP and HR (Fig. 1).
Fig. 1. Study population. PATOS, Pan-Asian Trauma Outcome Study.
The characteristics of the study population according to PASI are shown in Table 1. Of the 6280 pediatric patients, 10.9% (686) had abnormal PASI. In-hospital mortality was 3.2% (198) of the entire study population, of which it was 2.9% (164) in the normal PASI group and 5.0% (34) in the abnormal (elevated) PASI group (p<0.01). The rate of poor functional outcome was 5.3% (334): 4.4% (247) in the normal PASI group and 12.7% (87) in the abnormal (elevated) PASI group (p<0.01).
Table 1. Characteristics of the Study Population according to the Pediatric Age-Adjusted SI.
| Variables | All (n=6280) | Normal (n=5594) | Abnormal (n=686) | p value | |
|---|---|---|---|---|---|
| Country | <0.01 | ||||
| Korea | 3419 (54.4) | 3107 (55.5) | 312 (45.5) | ||
| Vietnam | 710 (11.3) | 636 (11.4) | 74 (10.8) | ||
| Malaysia | 1834 (29.2) | 1582 (28.3) | 252 (36.7) | ||
| Other | 317 (5.0) | 269 (4.8) | 48 (7.0) | ||
| Age, yr | 13 (7–16) | 13 (8–16) | 10 (5–15) | <0.01 | |
| Sex, female | 1787 (28.5) | 1536 (27.5) | 251 (36.6) | <0.01 | |
| Intentionality, yes | 257 (4.1) | 214 (3.8) | 43 (6.3) | <0.01 | |
| Place of injury | <0.01 | ||||
| Home | 1505 (24.0) | 1321 (23.6) | 184 (26.8) | ||
| Street | 3197 (50.9) | 2844 (50.8) | 353 (51.5) | ||
| School | 572 (9.1) | 522 (9.3) | 50 (7.3) | ||
| Sports and athletics area | 264 (4.2) | 242 (4.3) | 22 (3.2) | ||
| Other | 742 (11.8) | 665 (11.9) | 77 (11.2) | ||
| Activity | 0.16 | ||||
| Travel | 1357 (21.6) | 1209 (21.6) | 148 (21.6) | ||
| Sports and leisure | 1484 (23.6) | 1334 (23.8) | 150 (21.9) | ||
| Education or work | 578 (9.2) | 520 (9.3) | 58 (8.5) | ||
| Other | 2861 (45.6) | 2531 (45.2) | 330 (48.1) | ||
| Mechanism | 0.06 | ||||
| Traffic accident | 2933 (46.7) | 2612 (46.7) | 321 (46.8) | ||
| Fall-down | 1649 (26.3) | 1468 (26.2) | 181 (26.4) | ||
| Other | 1698 (27.0) | 1514 (27.1) | 184 (26.8) | ||
| Mode of arrival, EMS | 4918 (78.3) | 4435 (79.3) | 483 (70.4) | 0.03 | |
| Prehospital treatment | |||||
| Fluid resuscitation | 261 (4.2) | 217 (3.9) | 44 (6.4) | <0.01 | |
| Immobilization | 1780 (28.3) | 1613 (28.8) | 167 (24.3) | 0.95 | |
| Injury area | |||||
| Head | 1893 (30.1) | 1664 (29.7) | 229 (33.4) | 0.14 | |
| Neck and face | 1905 (30.3) | 1716 (30.7) | 189 (27.6) | <0.01 | |
| Chest | 374 (6.0) | 308 (5.5) | 66 (9.6) | <0.01 | |
| Abdomen | 349 (5.6) | 281 (5.0) | 68 (9.9) | <0.01 | |
| Spine | 134 (2.1) | 114 (2.0) | 20 (2.9) | <0.01 | |
| Extremity | 3364 (53.6) | 3015 (53.9) | 349 (50.9) | <0.01 | |
| Other | 590 (9.4) | 496 (8.9) | 94 (13.7) | <0.01 | |
| SBP, mm Hg | 123 (111–142) | 124 (113–143) | 116 (100–139) | <0.01 | |
| HR, beats/minute | 94 (81–111) | 92 (80–106) | 110 (92–125) | <0.01 | |
| GCS | <0.01 | ||||
| 15 | 5442 (86.7) | 4896 (87.5) | 546 (79.6) | ||
| 13–14 | 133 (2.1) | 111 (2.0) | 22 (3.2) | ||
| 9–12 | 72 (1.1) | 51 (0.9) | 21 (3.1) | ||
| 3–8 | 633 (10.1) | 536 (9.6) | 97 (14.1) | ||
| Severity of trauma (NISS) | <0.01 | ||||
| 1–8 | 4642 (73.9) | 4224 (75.5) | 418 (60.9) | ||
| 9–15 | 526 (8.4) | 434 (7.8) | 92 (13.4) | ||
| 16–24 | 172 (2.7) | 137 (2.4) | 35 (5.1) | ||
| 25–75 | 940 (15.0) | 799 (14.3) | 141 (20.6) | ||
| Clinical outcomes | |||||
| Poor functional outcome | 334 (5.3) | 247 (4.4) | 87 (12.7) | <0.01 | |
| In-hospital mortality | 198 (3.2) | 164 (2.9) | 34 (5.0) | <0.01 | |
SI, shock index; IQR, interquartile range; EMS, emergency medical service; SBP, systolic blood pressure; HR, heart rate; GCS, Glasgow Coma Scale; NISS, new injury severity score.
Data are presented as median (IQR) or n (%).
The characteristics of the study population according to sex are shown in Table 2. Of the 6280 patients, 71.5% (4493) were male and 28.5% (1787) were female. In-hospital mortality and poor functional outcomes in the two groups did not differ significantly.
Table 2. Characteristics of the Study Population according to Sex.
| Variables | All (n=6280) | Male (n=4493) | Female (n=1787) | p value | |
|---|---|---|---|---|---|
| Country | <0.01 | ||||
| Korea | 3419 (54.4) | 2374 (52.8) | 1045 (58.5) | ||
| Vietnam | 710 (11.3) | 472 (10.5) | 238 (13.3) | ||
| Malaysia | 1834 (29.2) | 1428 (31.8) | 406 (22.7) | ||
| Other | 317 (5.0) | 219 (4.9) | 98 (5.5) | ||
| Age, yr | 13 (7–16) | 13 (8–16) | 11 (6–16) | <0.01 | |
| Intentionality, yes | 257 (4.1) | 164 (3.7) | 93 (5.2) | <0.01 | |
| Place of injury | <0.01 | ||||
| Home | 1505 (24.0) | 941 (20.9) | 564 (31.6) | ||
| Street | 3197 (50.9) | 2391 (53.2) | 806 (45.1) | ||
| School | 572 (9.1) | 424 (9.4) | 148 (8.3) | ||
| Sports and athletics area | 264 (4.2) | 210 (4.7) | 54 (3.0) | ||
| Other | 742 (11.8) | 527 (11.7) | 215 (12.0) | ||
| Activity | <0.01 | ||||
| Travel | 1357 (21.6) | 1010 (22.5) | 347 (19.4) | ||
| Sports and leisure | 1484 (23.6) | 1175 (26.2) | 309 (17.3) | ||
| Education or work | 578 (9.2) | 414 (9.2) | 164 (9.2) | ||
| Other | 2861 (45.6) | 1894 (42.2) | 967 (54.1) | ||
| Mechanism | <0.01 | ||||
| Traffic accident | 2933 (46.7) | 2192 (48.8) | 741 (41.5) | ||
| Fall-down | 1649 (26.3) | 1138 (25.3) | 511 (28.6) | ||
| Other | 1698 (27.0) | 1163 (25.9) | 535 (29.9) | ||
| Mode of arrival, EMS | 4918 (78.3) | 3542 (78.8) | 1376 (77.0) | 0.11 | |
| Prehospital treatment | |||||
| Fluid resuscitation | 261 (4.2) | 218 (4.9) | 43 (2.4) | <0.01 | |
| Immobilization | 1780 (28.3) | 1373 (30.6) | 407 (22.8) | <0.01 | |
| Injury area | |||||
| Head | 1893 (30.1) | 1411 (31.4) | 482 (27.0) | 0.67 | |
| Neck and face | 1905 (30.3) | 1370 (30.5) | 535 (29.9) | <0.01 | |
| Chest | 374 (6.0) | 300 (6.7) | 74 (4.1) | 0.05 | |
| Abdomen | 349 (5.6) | 266 (5.9) | 83 (4.6) | 0.45 | |
| Spine | 134 (2.1) | 92 (2.0) | 42 (2.4) | <0.01 | |
| Extremity | 3364 (53.6) | 2458 (54.7) | 906 (50.7) | 0.44 | |
| Other | 590 (9.4) | 414 (9.2) | 176 (9.8) | ||
| SBP, mm Hg | 123 (111–142) | 124 (112–142) | 120 (110–141) | <0.01 | |
| HR, beats/minute | 94 (81–111) | 93 (80–108) | 98 (85–118) | <0.01 | |
| GCS | 0.45 | ||||
| 15 | 5442 (86.7) | 3877 (86.3) | 1565 (87.6) | ||
| 13–14 | 133 (2.1) | 94 (2.1) | 39 (2.2) | ||
| 9–12 | 72 (1.1) | 55 (1.2) | 17 (1.0) | ||
| 3–8 | 633 (10.1) | 467 (10.4) | 166 (9.3) | ||
| Severity of trauma (NISS) | <0.01 | ||||
| 1–8 | 4642 (73.9) | 3292 (73.3) | 1350 (75.5) | ||
| 9–15 | 526 (8.4) | 409 (9.1) | 117 (6.5) | ||
| 16–24 | 172 (2.7) | 142 (3.2) | 30 (1.7) | ||
| 25–75 | 940 (15.0) | 650 (14.5) | 290 (16.2) | ||
| Clinical outcomes | |||||
| Poor functional outcome | 334 (5.3) | 255 (5.7) | 79 (4.4) | 0.05 | |
| In-hospital mortality | 198 (3.2) | 153 (3.4) | 45 (2.5) | 0.07 | |
IQR, interquartile range; EMS, emergency medical service; SBP, systolic blood pressure; HR, heart rate; GCS, Glasgow Coma Scale; NISS, new injury severity score.
Data are presented as median (IQR) or n (%).
Main outcomes
In multivariable logistic regression analysis, abnormal PASI was significantly associated with increased in-hospital mortality (aOR, 1.74; 95% CI, 1.13–2.47) and poor functional outcome (aOR, 3.43; 95% CI, 2.51–4.26) after adjusting for potential confounders (Table 3).
Table 3. Multivariable Logistic Regression Analysis on Study Outcomes by the PASI and SI.
| Total (n) | Outcome n (%) | Model 1 | Model 2 | ||
|---|---|---|---|---|---|
| aOR (95% CI) | aOR (95% CI) | ||||
| In-hospital mortality | |||||
| Total population | 6280 | 198 (3.2) | |||
| Normal SI | 4880 | 147 (3.0) | ref. | ref. | |
| Abnormal SI | 1400 | 51 (3.6) | 1.61 (1.13–2.30) | 1.51 (1.06–2.17) | |
| Normal PASI | 5594 | 164 (2.9) | ref. | ref. | |
| Abnormal PASI | 686 | 34 (5.0) | 1.90 (1.29–2.79) | 1.74 (1.13–2.47) | |
| Poor functional outcome | |||||
| Total population | 6280 | 334 (5.3) | |||
| Normal SI | 4880 | 229 (4.7) | ref. | ref. | |
| Abnormal SI | 1400 | 105 (7.5) | 2.71 (2.08–3.54) | 2.64 (2.01–3.44) | |
| Normal PASI | 5594 | 247 (4.4) | ref. | ref. | |
| Abnormal PASI | 686 | 87 (12.7) | 3.47 (2.66–4.53) | 3.43 (2.51–4.26) | |
SI, shock index; PASI, pediatric age-adjusted shock index; aOR, adjusted odds ratio; CI, confidence interval.
Model 1 adjusted for age and sex. Model 2 adjusted for variables in Model 1 and intentionality, place of injury, activity, mechanism of injury, and severity of injury.
Interaction analysis
Interaction analysis was used to assess whether the study outcomes of PASI varied according to sex. The ORs for in-hospital mortality differed according to the sex of the injured patients (p<0.01). The association of PASI with in-hospital mortality was maintained only in males (aOR, 1.86; 95% CI, 1.19–2.91), but not in females (aOR, 1.38; 95% CI, 0.58–2.99) (Table 4).
Table 4. Interaction Analysis between the PASI/SI and Sex on Study Outcome.
| PASI/SI | Sex | ||||||
|---|---|---|---|---|---|---|---|
| Normal SI | Abnormal SI | p for interaction | Normal PASI | Abnormal PASI | p for interaction | ||
| aOR (95% CI) | aOR (95% CI) | aOR (95% CI) | aOR (95% CI) | ||||
| In-hospital mortality | 0.66 | <0.01 | |||||
| Male | ref. | 1.32 (0.92–2.02) | ref. | 1.86 (1.19–2.91) | |||
| Female | ref. | 1.55 (0.82–2.99) | ref. | 1.38 (0.58–2.99) | |||
| Poor functional outcome | 0.34 | 0.11 | |||||
| Male | ref. | 2.33 (1.69–3.20) | ref. | 3.72 (2.24–6.05) | |||
| Female | ref. | 2.54 (1.56–4.13) | ref. | 2.76 (1.91–3.23) | |||
SI, shock index; PASI, pediatric age-adjusted shock index; aOR, adjusted odds ratio; CI, confidence interval.
DISCUSSION
Using a prospective international multicenter registry of injury in the Asia-Pacific region, the results of this study showed that elevated PASI was associated with a higher probability of in-hospital mortality and poor functional recovery in pediatric trauma patients. In the interaction analysis, elevated PASI was associated with increased in-hospital mortality only in males, but not in females. This research contributes to a better understanding of the usefulness of PASI in predicting the clinical outcome of pediatric trauma patients who visit the ED. Furthermore, it shows a limit to applying the previously suggested cut-off value of PASI to predict mortality regardless of sex.
SI predicts hemodynamic instability more sensitively than traditional vital signs, such as SBP and HR. In a prospective study evaluating hypovolemia detection, SI was a more accurate predictor of acute changes in the blood volume compared to SBP or HR alone.18 Furthermore, in studies of geriatric patients, SI predicted the overall mortality better compared to the traditional vital signs.19 A study of pediatric patients with sepsis reported a higher mortality risk with increasing SI, although there was no clear cut-off value.20 Studies to predict mortality in adult trauma patients have used abnormal SI, defined as SI >0.9 to 1, as a cut-off value for mortality prediction.21 However, it is not ideal to apply the cut-off value of adult physiological indicators to pediatric patients due to their unique anatomy and physiological differences compared to adults. Furthermore, the pattern and degree of changes in vital signs, such as SBP and HR, when bleeding from trauma occurs in pediatric patients are different from those in adults.22
To increase the ability of SI to predict clinical outcomes in pediatric trauma patients, age-specific SI was applied to pediatric trauma patients in several studies.23,24,25 PASI was found to be a good predictor of mechanical ventilation or blood transfusion needs, increased intensive care unit hospitalization, and longer in-hospital stays.23,24,25 However, previous studies on PASI mainly focused on blunt injured pediatric patients; hence, studies on the generalizability of PASI to indicate negative clinical outcomes and the need for increased resources for pediatric patients who sustain injuries other than blunt injury are limited.
Our study targeted all pediatric trauma patients, and, to our knowledge, is the first study to suggest the association between SI and functional outcome of pediatric trauma patients. In our study, although elevated SI and elevated PASI were associated with worse clinical outcomes, the associations with PASI in predicting worse clinical outcomes were stronger, similar to the findings in previous studies.
In the interaction analysis of our study, elevated PASI was associated with in-hospital mortality in males, but not in females. However, regardless of sex, the SI of non-survivors was higher than that of survivors, suggesting that setting of the cut-off point requires sex-specific adjustment, and is not a functional limitation of the SI itself.
In previous studies, the SI of females was higher than that of males in all age groups; and in regards to SI components, while SBP did not show a clear difference according to sex, it has been reported that the HR is generally higher in females than in males.10,26 Although no study has reported sex-specific differences in changes in vital signs, including SBP and HR, after trauma, it can be expected that the male group with a low baseline SI would show a generally decreasing trend even after trauma. Hence, elevated PASI in males indicates a poorer physiological state compared to females, which eventually leads to worse clinical results.
In our study, as in previous studies, the normal cut-off values for SI were 1.22, 1.0, and 0.9 for ages 4–6 years, 7–12 years, and 13–18 years, respectively. However, based on the results of our study, it would be more appropriate for the female cut-off value to be higher than the current value.
Although PASI is an important predictor of in-hospital mortality and poor functional recovery in pediatric trauma patients, the results of our study, which have different predictive powers according to sex, provide a theoretical basis that sex-specific and age-specific normal values of SI may be more effective in screening for trauma severity than a single-value threshold.
This study has several limitations that need to be addressed. First, although intentionality, activity at the time of the injury, location, and mechanism of injury were adjusted in the multivariable logistic regression analysis, due to nature of observational study, the potential for unmeasured confounding still exists, which may have caused some bias in our study results. Second, pediatric patients may have inaccurate measurements of vital signs at ED compared to adults, possibly affecting the study results. Third, although several age-specific cut-off values for SI have been suggested in previous studies, one of the values was taken and used in our study, which may have resulted in a bias. Fourth, investigators in the PATOS registry were not blinded to the study hypothesis, which could have led to biased data collection. Finally, since this was not a randomized controlled trial, there could have been some potential biases that were not controlled.
Abnormal PASI is associated with increased in-hospital mortality and poor functional recovery in pediatric trauma patients; however, the prediction power of mortality is significant only in male patients. Further studies on sex- and age-specific cut-off value of SI are warranted to predict clinical outcomes in pediatric trauma patients.
Footnotes
The authors have no potential conflicts of interest to disclose.
- Conceptualization: Sang Do Shin.
- Data curation: Young Sun Ro and Eujene Jung.
- Formal analysis: Hyun Ho Ryu and Eujene Jung.
- Funding acquisition: Sang Do Shin.
- Investigation: Kentaro Kajino.
- Methodology: Hyun Ho Ryu and Eujene Jung.
- Project administration: Sang Do Shin and Kentaro Kajino.
- Resources: Sang Do Shin and Eujene Jung.
- Software: Young Sun Ro and Eujene Jung.
- Supervision: Hyun Ho Ryu.
- Validation: Eujene Jung.
- Visualization: Kentaro Kajino.
- Writing—original draft: Eujene Jung.
- Writing—review & editing: Hyun Ho Ryu.
- Approval of final manuscript: all authors.
References
- 1.Ott R, Krämer R, Martus P, Bussenius-Kammerer M, Carbon R, Rupprecht H. Prognostic value of trauma scores in pediatric patients with multiple injuries. J Trauma. 2000;49:729–736. doi: 10.1097/00005373-200010000-00023. [DOI] [PubMed] [Google Scholar]
- 2.Peden M, McGee K, Sharma G. The injury chart book: a graphical overview of the global burden of injuries. Geneva: World Health Organization; 2002. [Google Scholar]
- 3.Acker SN, Ross JT, Partrick DA, Tong S, Bensard DD. Pediatric specific shock index accurately identifies severely injured children. J Pediatr Surg. 2015;50:331–334. doi: 10.1016/j.jpedsurg.2014.08.009. [DOI] [PubMed] [Google Scholar]
- 4.Arshad A, Polcari AM, Pinto NP, Slidell MB. Trauma patients in the pediatric ICU: rational use of a limited resource. Curr Opin Pediatr. 2020;32:837–842. doi: 10.1097/MOP.0000000000000958. [DOI] [PubMed] [Google Scholar]
- 5.Vandromme MJ, Griffin RL, Kerby JD, McGwin G, Jr, Rue LW, 3rd, Weinberg JA. Identifying risk for massive transfusion in the relatively normotensive patient: utility of the prehospital shock index. J Trauma. 2011;70:384–388. doi: 10.1097/TA.0b013e3182095a0a. discussion 388-90. [DOI] [PubMed] [Google Scholar]
- 6.Mutschler M, Nienaber U, Münzberg M, Wölfl C, Schoechl H, Paffrath T, et al. The shock index revisited-a fast guide to transfusion requirement? A retrospective analysis on 21,853 patients derived from the TraumaRegister DGU. Crit Care. 2013;17:R172. doi: 10.1186/cc12851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fröhlich M, Driessen A, Böhmer A, Nienaber U, Igressa A, Probst C, et al. Is the shock index based classification of hypovolemic shock applicable in multiple injured patients with severe traumatic brain injury?-an analysis of the TraumaRegister DGU®. Scand J Trauma Resusc Emerg Med. 2016;24:148. doi: 10.1186/s13049-016-0340-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cuenca CM, Borgman MA, April MD, Fisher AD, Schauer SG. Validation of the age-adjusted shock index for pediatric casualties in Iraq and Afghanistan. Mil Med Res. 2020;7:33. doi: 10.1186/s40779-020-00262-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marenco CW, Do WS, Lammers DT, Horton JD, Azarow K, Eckert MJ. Validation of shock index pediatric-adjusted for children injured in warzones. J Trauma Acute Care Surg. 2020;89:642–648. doi: 10.1097/TA.0000000000002655. [DOI] [PubMed] [Google Scholar]
- 10.Rappaport LD, Deakyne S, Carcillo JA, McFann K, Sills MR. Age- and sex-specific normal values for shock index in national health and nutrition examination survey 1999-2008 for ages 8 years and older. Am J Emerg Med. 2013;31:838–842. doi: 10.1016/j.ajem.2013.01.014. [DOI] [PubMed] [Google Scholar]
- 11.Clarke WR, Schrott HG, Leaverton PE, Connor WE, Lauer RM. Tracking of blood lipids and blood pressures in school age children: the Muscatine study. Circulation. 1978;58:626–634. doi: 10.1161/01.cir.58.4.626. [DOI] [PubMed] [Google Scholar]
- 12.Kong SY, Shin SD, Tanaka H, Kimura A, Song KJ, Shaun GE, et al. Pan-Asian Trauma Outcomes Study (PATOS): rationale and methodology of an international and multicenter trauma registry. Prehosp Emerg Care. 2018;22:58–83. doi: 10.1080/10903127.2017.1347224. [DOI] [PubMed] [Google Scholar]
- 13.Ong ME, Shin SD, De Souza NN, Tanaka H, Nishiuchi T, Song KJ, et al. Outcomes for out-of-hospital cardiac arrests across 7 countries in Asia: the Pan Asian Resuscitation Outcomes Study (PAROS) Resuscitation. 2015;96:100–108. doi: 10.1016/j.resuscitation.2015.07.026. [DOI] [PubMed] [Google Scholar]
- 14.Nwomeh BC, Lowell W, Kable R, Haley K, Ameh EA. History and development of trauma registry: lessons from developed to developing countries. World J Emerg Surg. 2006;1:32. doi: 10.1186/1749-7922-1-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Berdowski J, Berg RA, Tijssen JG, Koster RW. Global incidences of out-of-hospital cardiac arrest and survival rates: systematic review of 67 prospective studies. Resuscitation. 2010;81:1479–1487. doi: 10.1016/j.resuscitation.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 16.Behrman RE, Kliegman RM, Jenson HB. Nelson textbook of pediatrics. 17th ed. Philadelphia, PA: Saunders; 2004. [Google Scholar]
- 17.Dehn A, Snedden P. Acute pre-hospital medicine: perspectives of an emergency medicine fellow and critical care paramedic. Emerg Med Australas. 2020;32:670–671. doi: 10.1111/1742-6723.13574. [DOI] [PubMed] [Google Scholar]
- 18.Naghibi T, Mohajeri M, Dobakhti F. Inflammation and outcome in traumatic brain injury: does gender effect on survival and prognosis? J Clin Diagn Res. 2017;11:PC06–PC09. doi: 10.7860/JCDR/2017/19132.9198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rousseaux J, Grandbastien B, Dorkenoo A, Lampin ME, Leteurtre S, Leclerc F. Prognostic value of shock index in children with septic shock. Pediatr Emerg Care. 2013;29:1055–1059. doi: 10.1097/PEC.0b013e3182a5c99c. [DOI] [PubMed] [Google Scholar]
- 20.Yasaka Y, Khemani RG, Markovitz BP. Is shock index associated with outcome in children with sepsis/septic shock?*. Pediatr Crit Care Med. 2013;14:e372–e379. doi: 10.1097/PCC.0b013e3182975eee. [DOI] [PubMed] [Google Scholar]
- 21.Bruijns SR, Guly HR, Bouamra O, Lecky F, Lee WA. The value of traditional vital signs, shock index, and age-based markers in predicting trauma mortality. J Trauma Acute Care Surg. 2013;74:1432–1437. doi: 10.1097/TA.0b013e31829246c7. [DOI] [PubMed] [Google Scholar]
- 22.Avarello JT, Cantor RM. Pediatric major trauma: an approach to evaluation and management. Emerg Med Clin North Am. 2007;25:803–836. x. doi: 10.1016/j.emc.2007.06.013. [DOI] [PubMed] [Google Scholar]
- 23.Keller MS, Fendya DG, Weber TR. Glasgow coma scale predicts coagulopathy in pediatric trauma patients. Semin Pediatr Surg. 2001;10:12–16. doi: 10.1053/spsu.2001.19381. [DOI] [PubMed] [Google Scholar]
- 24.Spinella PC, Holcomb JB. Resuscitation and transfusion principles for traumatic hemorrhagic shock. Blood Rev. 2009;23:231–240. doi: 10.1016/j.blre.2009.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Arbuthnot M, Armstrong LB, Mooney DP. Can we safely decrease intensive care unit admissions for children with high grade isolated solid organ injuries? Using the shock index, pediatric age-adjusted and hematocrit to modify APSA admission guidelines. J Pediatr Surg. 2017;52:989–992. doi: 10.1016/j.jpedsurg.2017.03.025. [DOI] [PubMed] [Google Scholar]
- 26.Rapsomaniki E, Timmis A, George J, Pujades-Rodriguez M, Shah AD, Denaxas S, et al. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1·25 million people. Lancet. 2014;383:1899–1911. doi: 10.1016/S0140-6736(14)60685-1. [DOI] [PMC free article] [PubMed] [Google Scholar]