Abstract
Background
The management of the oxygenator can be prolonged in the long-term procedures especially during extracorporeal membrane oxygenation (ECMO) for bridge to transplant or bridge to recovery. Long-term use often involves an overrun of the time of use with respect to certification of the oxygenating module of 14 days, for the maintenance of performance and efficiency of the oxygenator. The evaluation of the long-term oxygenator efficiency is complex and depends on the: patient pathology, ECMO configuration, the management of coagulation and anticoagulation, materials selection and circuit components, the structure, design and performance of the oxygenator. In this context we investgated the long-term performance of the A.L.ONE Eurosets ECMO oxygenator in relation to the parameters prodromal to replacement.
Methods
We retrospectively collected eight years data from Anthea Hospital GVM Care & Research, Bari, Italy on the long-term use exceeding 14 days of Eurosets A.L.ONE ECMO Adult oxygenator in Polymetylpentene fiber, for ECMO procedures, including the procedures: Veno Arterial (VA) ECMO post-cardiotomy or not, veno-venous (VV) ECMO. The primary end points were the evaluation of Gas Transfer: oxygen partial pressure (PO2) post oxygenator, Carbon dioxide partial pressure (PCO2) post oxygenator, the oxygen transfer across the oxygenator membrane V′O2, differential CO2 content across oxygenator; Pressure monitoring: oxygenator pressure Drop in relation to Blood flow rate (BFR) (ΔP); Hematologic values: Hemoglobin, Fibrinogen, Platelets, aPTT, D-Dimer, LDH.
Results
Nine VA ECMO patients who used the oxygenator for 18.5 days and two VV ECMO patients who used the oxygenators for 17.2 days on the seventeenth days reported average values PaO2 (267 ± 29 mmHg); PaCO2 (34 ± 4 mmHg) with gas blender values set to 3.8 ± 0.6 L/min of air and a FiO2 of 78 ± 5%; the transfer across the oxygenator membrane V′O2 was 189 ± 43 (ml/min/m2). The mean peak of partial pressure of carbon dioxide from the gas exhaust of oxygenator (PECO2) was 38 ± 4 mmHg; differential CO2 across the oxygenator “pre-oxygenator PCO2–post-oxygenator PCO2” (18 ± 6 mmHg); the mean blood flow rate (BFR) 4.5 ± 0.6 (L/minute); the pump revolution per minutes mean maximum rate was 4254 ± 345 (RPM); the mean pressure drop (ΔP) was 76 ± 12 mmHg; the mean peak of d-dimers (DDs) was 23.6 ± 0.8 mg / dL; the mean peak of LDH was 230 ± 55 (mg/dl); fibrinogen mean peak 223 ± 40 (mg/dl).
Conclusions
The performance of the Eurosets A.L.ONE ECMO Adult polymethylpentene fiber oxygenator in our experience has proven efficiency in terms of O2 uptake and CO2 removal, blood fluid dynamics, metabolic compensation and heat exchange in the long-term treatment. The device was safe without iatrogenic problems over a period of 14 days in the patients undergoing ECMO VA and in all patients undergoing VV ECMO with continuous administration of anticoagulation therapy.
Keywords: Polymethylpentene, Hollow fibers, Extracorporeal membrane oxygenator, Long term, Efficiency, Performance, Safety
Introduction
With improvements in circuit technology and expanding supportive evidence, extracorporeal membrane oxygenation (ECMO) use has grown rapidly over the past decade. The management of the oxygenator can be prolonged in the long-term procedures especially during extracorporeal membrane oxygenation (ECMO) for bridge to transplant or bridge to recovery. In this study, we present a classification of the short, medium, long term use of the oxygenating module in relation to its certification and validation [1]. Long-term use often involves an overrun of the time use respect to certification with only one oxygenating module. The evaluation of the long-term oxygenator efficiency is complex and depends on the type of: patient pathology, ECMO configuration, the management of coagulation or anticoagulation, materials selection; circuit components and design, the structure, design and performance of the oxygenator [2]. In this study we present a retrospective analysis about Eurosets A.L.ONE ECMO Adult Polymethylpentene fiber oxygenator a medical device validated and certified by the manufacturer (Eurosets SPA, Medolla, Italy) for ECMO procedures up to 14 days. In this context we wanted to investigate the long-term performance of the A.L.ONE Eurosets ECMO oxygenator in relation to the parameters prodromal to replacement: Hematologic profiles (Coagulopathy, Hemolysis) [1–3]; Pressure monitoring (Blood Flow, Pressure Drop); Gas Transfer (O2 uptake and CO2 removal) [4, 5].
Materials and methods
Extracorporeal membrane oxygenation settings
The ECMO circuit consists exclusively of commercially available components. By default, a Thoratec Centrimag centrifugal magnetic levitation pumps (Abbott) (Fig. 1) and ECMOLIFE centrifugal magnetic levitation pumps (Eurosets SPA, Medolla, Italy) (Fig. 2) were used, in synergy with Landing system for pressure monitoring (Blood Flow, Pressure Drop); Gas Transfer (O2 uptake and CO2 removal), (Eurosets SPA, Medolla, Italy). As a standard, the Eurosets A.L.ONE ECMO Adult oxygenator was used (Fig. 3). The tubing and the oxygenator were treated with phosphorylcholine-coated surface (Eurosets SPA, Medolla, Italy). The system has a priming volume of 500 ml and features connectors for other emergency extracorporeal devices, such as renal replacement devices or rapid infusion systems for advanced in-center intensive care treatment during further courses of therapy. The main determinants of cannula sizing in peripheral VA ECMO are anatomical considerations and the targeted flow rate. Generally, cannulas are chosen to support a flow equivalent to a cardiac index of 2.2–2.5 L/m2/min, which is considered full flow. Femoral Arterial cannulas that we used were 17–25 Fr and Femoral venous cannulas were usually 19–25 Fr Biomedicus (Medtronic, Minneapolis, USA). For Central VA ECMO Aortic Arterial cannulas were 20–24 Fr EOPA (Medtronic, Minneapolis, USA) and Atrial venous cannulas were 32/40–36/46 Fr (Medtronic, Minneapolis, USA). For Peripheral VV ECMO for Femoral venous cannulas were 19–25 Fr for reinfusion in jugular vein cannulas were 17–21 Fr Biomedicus (Medtronic, Minneapolis, USA) (Fig. 4).
Fig. 1.
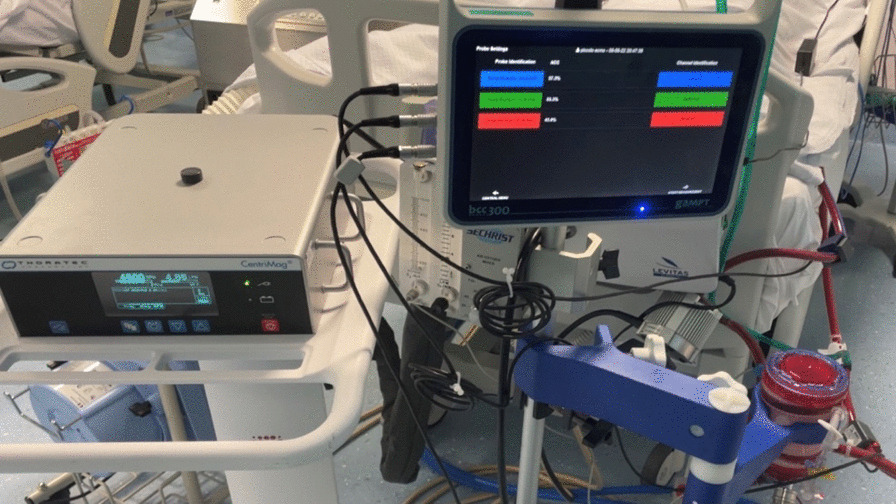
Adult A.L.ONE ECMO Oxygenator (Eurosets SPA, Medolla, Italy) configuration with Thoratec Centrimag, centrifugal magnetic levitation pumps (Abbott) during VA ECMO
Fig. 2.

Adult A.L.ONE ECMO Oxygenator configuration with ECMOLIFE, centrifugal magnetic levitation pump (Eurosets SPA, Medolla, Italy) during VA ECMO
Fig. 3.

Adult A.L.ONE ECMO Oxygenator (Eurosets SPA, Medolla, Italy)
Fig. 4.
Trend of PO2 and PCO2 out Oxygenator with and without continuous Heparin
Anticoagulation and blood product management
The ECMO patients are i our center are anticoagulated with a heparin infusion, with a goal activated partial thromboplastic time (aPTT) of 50–65 s unless the clinical setting (e.g., active bleeding) dictates otherwise. The heparin infusion is titrated with a nurse-managed nomogram, whereby the initial infusion dose is based on the patient’s weight. Six hours after the infusion begins, an aPTT is again drawn, and the rate of infusion is increased if subtherapeutic (< 50 s), decreased if supratherapeutic (> 65 s), or kept constant if within goal (50–65 s). Another aPTT is drawn in 6 h until the second consecutive aPTT is within target range, at which point the aPTT is checked daily. In our institution the usual practice is to transfuse platelets when counts fall below 80,000/μL, although several experienced centers use a more conservative approach and transfuse platelets only when they fall below 40,000–50,000/μL, or even as low as 20,000 in non- bleeding patients. The strategies in RBC transfusion depending on Hb level—restrictive when transfusion is performed at a Hb level of 7–9 g/dL, and liberal with a Hb level between 10 and 12 g/dl, in relation to Blood Flow (BF), Cardiac Output (CO) and Oxygen Delivery (DO2) [6].
Veno-arterial (VA) ECMO indication
ECMO was initiated for circulatory instability during or immediately after weaning from the cardiopulmonary bypass (CPB) in the primary cardiac procedure or for hemodynamic support for high risk interventional cardiology procedures. The clinical criteria for hemodynamic support included the following: left atrial pressure > 15 mmHg; central venous pressure > 12 mmHg; metabolic acidosis (i.e. pH < 7.3 with serum lactate > 3.0 mmol/L); end-organ hypoperfusion (urine output < 30 mL/h); cardiac index < 2.2 L/min/m2; and systolic blood pressure < 80 mmHg despite adequate filling volumes, use of multiple adrenergic agents (epinephrine > 0.1 µg/kg/min or dobutamine > 10 µg/kg/min, norepinephrine > 0.1 µg/kg/min), or an intra-aortic balloon pump (IABP). VA-ECMO support was initiated via peripheral cannulation through the femoral route with the semi-open method, and an additional 6 Fr catheter was systematically inserted distally into the femoral artery to prevent leg ischemia ECMO blood flow was adjusted on based on clinical assessments (e.g. pre-oxygenator venous oxygen saturation, evidence of hypoperfusion, resolution of hyperlactatemia, normalization of mean arterial pressure). ECMO-related complications were carefully monitored. ECMO weaning was performed in patients who fulfilled our published institutional weaning criteria and passed an ECMO weaning trial consisting in decreasing and clamping ECMO flow. In general, the patient should have a pulsatile arterial waveform for at least 24 h; be hemodynamically stable, with baseline mean arterial pressure greater than 60 mmHg with no or low doses of catecholamines; should have left ventricular ejection fraction (LVEF) of 35%, and an aortic velocity time integral (VTI) of ≥ 12 cm; and have recovered from major metabolic disturbances. Weaning was considered unsuccessful if ECMO re-cannulation was required within 2 days of decannulation [2–7].
Veno-venous (VV) ECMO indication
The indication for VV-ECMO are typically severely hypoxemic and/or hypercapnic and unresponsive to optimal medical management, including protective ventilation with low-tidal volumes and plateau pressure less than 28–30 cmH2O, high levels of PEEP, prone positioning, neuromuscular blockers and/or other adjunctive therapies, including nitrous oxide or almitrine. The recent literature suggests that a PaO2/FIO2 ratio of 70–80 mmHg, Murray score > 3, and pH < 7.2 provide a reasonable threshold for considering VV-ECMO in adults with ARDS. It is crucial to determine the acute nature of the pulmonary failure, exclude cardiac and/or other organ failure and verify that the respiratory failure cannot be improved with optimal ventilator management [8].
Indication and cut-off parameters used for oxygenator or circuit replacement
The polymethylpentene fiber oxygenator is responsible for oxygen uptake and carbon dioxide removal. The non-biologic surface of the oxygenator activates inflammatory and coagulation pathways with thrombus formation, fibrinolysis, and leukocyte activation leading to fiber dysfunction. Activation of coagulation and fibrinolysis can precipitate systemic coagulopathy or hemolysis, while clot deposition can obstruct blood flow. Additionally, moisture buildup in the gas phase and protein and cellular debris accumulation in the blood phase may contribute to shunt and dead-space physiology, respectively, impairing gas exchange. These three categories—hematologic abnormalities, mechanical obstruction, and inadequate gas exchange—prompt the majority of oxygenator exchanges. Principal Cut-off parameters for replacement the oxygenator or the circuit, Gas Transfer: Arterial oxygen partial pressure (PO2) post oxygenator (< 200 mmHg), Carbon dioxide partial pressure PCO2 (> 40 mmHg) post oxygenator, the oxygen transfer across the oxygenator membrane V′O2 (< 100–150 ml/min/m2),
where V′O2 = O2 transfer across the oxygenator (mL/min), BFR = blood flow rate (L/min), Cx O2 = O2 content of(pre-/post-oxygenator) blood (mL/L) for
where Hb = hemoglobin (g/dL), Sx O2 = O2 saturation of (pre-/post-ML) blood, Px O2 = O2 partial pressure of (pre-/post-oxygenator) blood (mmHg).
Measurement of V′O2 provides an objective measure of oxygen transfer and can confirm oxygenator dysfunction, when clinically indicated. Differential CO2 across the oxygenator “pre oxygenator PCO2–post oxygenator PCO2” (< 10 mmHg); Pressure monitoring: pressure Drop across the oxygenator “Pressure Pre oxygenator–Pressure Post oxygenator” (> 80 mmHg) in relation to Blood flow rate (BFR) (ΔP); Hematologic profiles: Fibrinogen (< 200 mg/dl), Platelets (< 80,000 109/L), aPTT (> 65 s), D-Dimer (> 25–30 ng/ml), LDH (> 250 mg/dl) [1].
Patients and data collection
We recruited retrospectively from January 2014 to May 2022 at Institution of Anthea Hospital GVM Care & Research, Bari, Italy, long-term ECMO procedures (exceeding 14 days) that use the Eurosets A.L.ONE ECMO Adult oxygenator. The procedures analyzed including: Veno-arterial (VA) ECMO post-cardiotomy or not, veno-venous (VV) ECMO. ECMO characteristics are described and presented as means with sd or medians with interquartile range. The primary end point was the substitution of oxygenator incidence in relation to the oxygenator performance were Gas Transfer: O2 uptake and CO2 removal were collected in relation to the blood flow rate (BFR), maximum rate per minute of pump (RPM), hemoglobin value (Hb), ventilation indices FiO2 (%)/ Air (L/min), PO2 post oxygenator (mmHg), PCO2 post oxygenator, the transfer across the oxygenator membrane V′O2 (ml/min/m2), Indexed Oxygen Delivery (iDO2) (ml/min/m2) only for VA ECMO patient, the partial pressure of carbon dioxide from the gas exhaust of oxygenator (PECO2) (mmHg), differential CO2 across the oxygenator (mmHg); Hematologic profiles: Fibrinogen (mg/dl), Platelets (109/L), aPTT (sec), D-Dimer (ng/ml), LDH (mg/dl), and incidence of Heparin‐induced thrombocytopenia (HIT) I, II, Temperature in arterial and venous line (°C) and Pressure monitoring: pressure Drop (ΔP) (mmHg).
Statistical analysis
Continuous data were expressed as mean ± standard deviation or a median with the interquartile range and categorical data as percentages. Cumulative survival was evaluated with the Kaplan–Meier method. All reported p-values were two-sided, and p-values of < 0.05 were considered to indicate statistical significance. All statistical analyses were performed with SPSS 22.0 (SPSS, Inc., Chicago, IL, USA).
Results
From January 2014 to May 2022 twenty-two ECMO procedures with Eurosets A.L.ONE ECMO Adult Polymethylpentene fiber oxygenator were retrospectively collected from the tertiary institution Anthea Hospital GVM Care & Research, Bari, Italy. Eight peripheral VA ECMOs were used as short-term hemodynamic support for interventional cardiology procedures, the medium time of use was less than 3 h. Twelve VA ECMOs were used as cardiocirculatory assistance, nine post cardiotomy of which: two with central cannulation, seven with peripheral cannulation and one peripheral after angioplasty. In nine oxygenators with continuous endo venous heparin treatment the average use time was 18.5 days. Only three oxygenators on post-cardiotomy VA ECMO procedures without continuous endo venous heparin treatment for patient bleeding were replaced on three patients between the sixth/seventh day of use for the performance decrease for previously mentioned cut-off (Table 1). in particular, the failure of the oxygenator was mainly caused by oxygenation (PO2 out the oxygenator < 120 mmHg with 100% FIO2 set to 10 L of gas flow), decapneization (PCO2 out the oxygenator > 45 mmHg with 10 L of gas flow and 100% FiO2) (Fig. 3), by the pressure drop (> 350 mmHg), by the reduction of the pump flow rate (< 2.4 l/min/m2) and by the visible formation of clots in the part corresponding to the purging of the oxygenator because an area with low vorticity which could have facilitated the halving of the platelet count (< 100,000 109/L). None of the patients reported incidence of HIT I and II. The use of a Phosphorylcholine-treated ECMO circuit versus a heparin circuit likely reduces heparin exposure by reducing the incidence of HIT [9]. Two oxygenators were used on Veno-Venous (VV) ECMO with continuous endo venous heparin treatment for the treatment of Acute Respiratory Distress Syndrome (ARDS) the average use time was 17.2 days. The 9 VA ECMO patients who used the oxygenator for 18.5 days and the two VV ECMO patients who used the oxygenators for 17.2 days on the seventeenth days reported average values of mean hemoglobin 8.9 ± 0.8; PO2 post oxygenator (267 ± 29 mmHg); PCO2 post oxygenator (34 ± 4 mmHg) with average values of gas blender set to Air 3.8 ± 0.6 L/min and a FiO2 of 78 ± 5%; the oxygen transfer across the oxygenator membrane V′O2 was 189 ± 43 (ml/min/m2); the mean peak of indexed oxygen delivery (iDO2) for only nine VA ECMO at seventeenth days was 340 ± 37 ml/min/m2. The mean peak of partial pressure of carbon dioxide from the gas exhaust of oxygenator (PECO2) was 20 ± 4 mmHg; differential CO2 across the oxygenator “pre-oxygenator PCO2–post-oxygenator PCO2” was 18 ± 6 (mmHg); the mean blood flow rate (BFR) was 4.5 ± 0.6 (L/minute); the pump revolution per minutes mean maximum rate was 4254 ± 345 (RPM); the mean pressure drop (ΔP) was 76 ± 12 mmHg; the mean arterial blood temperature was 36.5 ± 0.3 °C and in the venous line was 36.4 ± 0.2 °C; the mean peak of D-dimers (DDs) was 23.6 ± 0.8 mg/dL; the mean peak of LDH was 230 ± 55 (mg/dl); fibrinogen mean peak 223 ± 40 (mg/dl); PLT 150,000 ± 987 (109/L); aPTT 53 ± 4 (sec), the other hematologic values data prodromal to oxygenator replacement are presented in the Table 1.
Table 1.
Operative data, during long term versus medium term on Adult A.L.ONE ECMO Oxygenator
| Procedures nr = 14 | Long term VA (Nr = 9) and VV ECMO (Nr = 2) | Medium term VA ECMO(Nr = 3) | p-value |
|---|---|---|---|
| Parameters at seventeenth day | Parameters at sixth day | ||
| Period (days) | 17.8 | 6.8 | 0.003 |
| Hemoglobin (gr/dl) | 8.9 ± 0.8 | 7.3 ± 0.8 | 0.022 |
| PO2 post oxygenator (mmHg) | 267 ± 29 | 170 ± 23 | 0.002 |
| PCO2 post oxygenator (mmHg) | 34 ± 4 | 42 ± 8 | 0.034 |
| Air (L/min) /FiO2 (%) | 3.8 ± 0.6/78 ± 5 | 5.3 ± 0.9/100 ± 9 | 0.019 |
| V′O2 (ml/min/m2) | 189 ± 43 | 105 ± 28 | 0.017 |
| iDO2 (ml/min/m2) | 340 ± 37 | 245 ± 48 | 0.025 |
| PECO2 (mmHg) | 20 ± 4 | 10 ± 6 | 0.031 |
| Differential CO2 (mmHg) | 18 ± 6 | 8 ± 3 | 0.021 |
| BFR (L/min) | 4.5 ± 0.6 | 3.9 ± 0.9 | 0.041 |
| Pump revolution (RPM) | 4254 ± 345 | 5000 ± 445 | 0.023 |
| Pressure drop (ΔP) | 76 ± 12 | 246 ± 22 | 0.011 |
| Arterial blood temperature (°C) | 36.5 ± 0.3 | 36.2 ± 0.8 | 0.89 |
| Venous blood temperature (°C) | 36.4 ± 0.2 | 36.1 ± 0.5 | 0.91 |
| Continuous anticoagulation Use | Yes | No | |
| DDs (mg/dL) | 23.6 ± 0.8 | 42 ± 13 | 0.005 |
| LDH (mg/dL) | 230 ± 55 | 424 ± 38 | 0.004 |
| Fibrinogen (mg/dL) | 223 ± 40 | 176 ± 40 | 0.003 |
| PLT (109/L) | 150,000 ± 987 | 39,000 ± 778 | 0.033 |
| aPTT (sec) | 53 ± 4 | 69 ± 23 | 0.018 |
| Oxygenator replacement (nr) | 0 | 3 | 0.002 |
| Total oxygenator used (nr) | 11 | 6 | 0.033 |
| Red blood cells (units for patients) | 2 ± 1 | 2 ± 1 | 0.027 |
| Platelets (units for patients) | 3 ± 1 | 2 ± 1 | 0.027 |
Values are presented as n (%) or mean ± standard deviation
VA, Veno-Arterial; VV, Veno-venous; ECMO, extracorporeal membrane oxygenation; PO2, partial pressure of oxygen; PCO2, partial pressure of carbon dioxide; V′O2, the oxygen transfer across the oxygenator membrane; iDO2, indexed oxygen delivery; PECO2, partial pressure of carbon dioxide from the gas exhaust of oxygenator; BFR, blood flow rate; DDs, D-Dimers; LDH, lactate dehydrogenase; PLT, Platelets; aPTT, partial thromboplastin time
Discussion
The main limitation of this study is the fact that it is a single center retrospective investigation with a small number of ECMO cases. An advantage of a small sample size in this case may be to contain medical, technical, and nursing management skills compared to a multicenter study. Long-term oxygenator management during post-cardiotomy ECMO procedures in the literature is limited with a high incidence of replacement due in particular to post-procedures bleeding [10, 11]. In future perspective would be interesting to explore this issue further in a larger multicenter study.
In this study, we present a classification of the short, medium, long term use of the oxygenating module in relation to its certification and validation and demonstrate that the determinant that can impact the duration of the oxygenator and its failure in particular after cardiac surgery procedures does not depend exclusively on the model and design but mainly on the medical and technical management of the device in relation to the anticoagulant. The same model in this case it may have a different duration and need to be replaced depending on the suspension or continued use of heparin infusion [9]. Long-term use often involves an overrun of the time use respect to certification with only one oxygenating module. The evaluation of the long-term oxygenator efficiency is complex and depends on the type of: patient pathology, ECMO configuration, the management of coagulation or anticoagulation, materials selection; circuit components and design, the structure, design and performance of the oxygenator. Prompt recognition of oxygenator dysfunction is vital for safety, allowing for elective replacement in a controlled manner [10, 12]. On the other hand, replacement of an adequately functioning device requiring temporary cessation of ECMO support places the patient at unnecessary risk while consuming a limited and expensive resource. Based on the pathophysiology of the oxygenator, replacement may be required for one of three reasons: if there is (A) an associated hematologic abnormality, (B) an increasing obstruction to blood flow, or (C) inadequate gas exchange [1]. In our experience we report that the continuous anticoagulation and a good balance in aPTT management is protective for the oxygenators until long-term use respect to the group that suspend the anticoagulation strategy for bleeding.
Conclusions
The performance of the Eurosets A.L.ONE ECMO Adult polymethylpentene fiber oxygenator in our experience has proven efficiency in terms of O2 uptake and CO2 removal, blood fluid dynamics, metabolic compensation and heat exchange in the long-term treatment. The device was safe without iatrogenic problems over a period of 14 days in the patients undergoing ECMO VA and in all patients undergoing VV ECMO with continuous administration of anticoagulation therapy, oxygenator replacement was not reported in this group of patients, compared with three replacements in the group that did not do continuous heparin infusion for bleeding.
Author contributions
IC designed the research study and wrote the original draft; RL contributed to the interpretation of the results and supervised the project; GN and GS contributed to the interpretation of the results and supervised the project; All authors contributed to editorial changes in the manuscript. All authors read and approved the final manuscript.
Funding
None.
Availability of data and materials
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This study was conducted according to the guidelines of the Declaration of Helsinki. The GVM Care & Research review board approved the study (internal protocol; decision 13 August 2022) and need for patient consent was waived due to the retrospective nature of the study.
Informed consent
Informed consent was obtained from all subjects involved in the study.
Competing interests
Ignazio Condello is consultant for Eurosets SPA, Medolla (Italy).
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Zakhary B, Vercaemst L, Mason P, et al. How I approach membrane lung dysfunction in patients receiving ECMO. Crit Care. 2020;24:671. doi: 10.1186/s13054-020-03388-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Condello I, Lorusso R, Santarpino G, Di Bari N, Fiore F, Moscarelli M, Calafiore AM, Speziale G, Nasso G. Perioperative incidence of ECMO and IABP on 5901 mitral valve surgery procedures. J Cardiothorac Surg. 2022;17(1):38. doi: 10.1186/s13019-022-01790-1.PMID:35300722;PMCID:PMC8928683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dornia C, Philipp A, Bauer S, Lubnow M, Muller T, Lehle K, et al. Analysis of thrombotic deposits in extracorporeal membrane oxygenators by multidetector computed tomography. ASAIO J. 2014;60(6):652–656. doi: 10.1097/MAT.0000000000000133. [DOI] [PubMed] [Google Scholar]
- 4.Doyle AJ, Hunt BJ. Current understanding of how extracorporeal membrane oxygenators activate haemostasis and other blood components. Front Med (Lausanne) 2018;5:352. doi: 10.3389/fmed.2018.00352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lubnow M, Philipp A, Foltan M, Bull Enger T, Lunz D, Bein T, et al. Technical complications during veno-venous extracorporeal membrane oxygenation and their relevance predicting a system-exchange–retrospective analysis of 265 cases. PLoS ONE. 2014;9(12):e112316. doi: 10.1371/journal.pone.0112316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maul TM, Massicotte MP, Wearden PD. ECMO biocompatibility: surface coatings, anticoagulation, and coagulation monitoring. In: Firstenberg MS, editor. Extracorporeal membrane oxygenation: advances in therapy. Croatia: IntechOpen; 2016. pp. 30–35. [Google Scholar]
- 7.Hastings SM, Deshpande SR, Wagoner S, Maher K, Ku DN. Thrombosis in centrifugal pumps: location and composition in clinical and in vitrocircuits. Int J Artif Organs. 2016;39(4):200–204. doi: 10.5301/ijao.5000498. [DOI] [PubMed] [Google Scholar]
- 8.Lehle K, Philipp A, Gleich O, Holzamer A, Muller T, Bein T, et al. Efficiency inextracorporeal membrane oxygenation-cellular deposits on polymethylpentene membranes increase resistance to blood flow and reduce gas exchange capacity. ASAIO J. 2008;54(6):612–617. doi: 10.1097/MAT.0b013e318186a807. [DOI] [PubMed] [Google Scholar]
- 9.Epis F, Belliato M. Oxygenator performance and artificial-native lunginteraction. J Thorac Dis. 2018;10(Suppl 5):S596–605. doi: 10.21037/jtd.2017.10.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Extracorporeal Life Support Organization. ECLS registry report: international summary. https://www.elso.org/Registry/Statistics/InternationalSummary.aspx
- 11.Posluszny J, Engoren M, Napolitano LM, Rycus PT, Bartlett RH. Predicting survival of adult respiratory failure patients receiving prolonged (≥14 days) extracorporeal membrane oxygenation. ASAIO J. 2020;66:825–833. doi: 10.1097/MAT.0000000000001067. [DOI] [PubMed] [Google Scholar]
- 12.Zakhary B, Sheldrake J, Pellegrino V. Extracorporeal membrane oxygenation and V/Q ratios: an ex vivo analysis of CO2 clearance within the Maquet Quadrox-iD oxygenator. Perfusion. 2020;35(1):29–33. doi: 10.1177/0267659120906767. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets analyzed during the current study are available from the corresponding author on reasonable request.



