Background:
Many studies had shown that with global warming, heat waves may increase the mortality risk of Chinese populations. However, these findings are not consistent. Therefore, we elucidated the associations by meta-analysis and quantified the magnitude of these risks, as well as the underlying factors.
Methods:
We searched the China National Knowledge Infrastructure (CNKI), Wanfang database, PubMed, EMBASE, and Web of Science for literature screening up to Nov 10, 2022, to analyze the effect of heat waves on mortality in the Chinese population. Literature screening and data extraction were performed independently by two researchers and the data were merged by meta-analysis. In addition, we conducted subgroup analysis by sex, age, years of education, region, and number of events to explore the source of heterogeneity.
Results:
Fifteen related studies on the impact on heat waves of the death of Chinese people were included in this study. The results of the meta-analysis showed that heat waves were significantly associated with increased mortality from non-accidental deaths, cardiovascular diseases, stroke, respiratory diseases, and circulatory diseases in the Chinese population: non-accidental mortality (RR = 1.19, 95% CI: 1.13–1.27, P < .01), cardiovascular diseases (RR = 1.25, 95% CI: 1.14–1.38), stroke (RR = 1.11, 95% CI: 1.03–1.20), respiratory diseases (RR = 1.18, 95% CI: 1.09–1.28), and circulatory diseases (RR = 1.11, 95% CI: 1.06–1.17). Subgroup analyses showed that heat waves had a higher risk of non-accidental death for those with <6 years of education than for those with ≥6 years of education. Meta-regression analysis showed that the contribution of the study year to the inter studied heterogeneity was 50.57%. The sensitivity analysis showed that the exclusion of any single study did not materially alter the overall combined effect. The meta-analysis method indicated no obvious evidence of publication bias.
Conclusions:
The results of the review indicated that heat waves were associated with increased mortality in the Chinese population, that attention should be paid to high-risk groups, and that public health policies and strategies should be implemented to more effectively respond to and adapt to climate change.
Keywords: Chinese population, heat waves, meta-analysis, mortality, systematic review
1. Introduction
In recent years, the global climate has continued to warm,[1,2] heat waves have occurred frequently,[3] and harm to human health has aroused widespread concern around the world.[4] When exposed to high temperatures, the body’s thermoregulatory system counteracts the adverse effects of high temperatures on the human body.[5,6] However, once high temperatures exceed a certain limit, there is a risk of illness, and the number of deaths increases substantially on the day of exposure.[7] Sustain extreme heat, known as heatwave weather, is harmful to health.[8] The heatwave that affected Europe in the summer of 2003 resulted in 22,080 excess deaths.[9] The latest study puts these numbers at an unprecedented 70,000 excess deaths.[10] France alone experienced 14,800 deaths in 9 days, with one-third of the deaths attributed to heatstroke, which is a fatal disease that causes extensive multi-organ tissue damage.[11]
Heat waves may pose a greater threat to China owing to an aging population and are closely linked to human health and well-being.[12] In July 2013 in China, a record-breaking sustained high temperature occurred in Jianghuai, Jiangnan, Chongqing, and other places, posing a huge threat to the health of the population.[13] Several population-based observational studies have investigated the effect of heat waves on Chinese population mortality.[14,15] To date, there have been few systematic reviews of these associations.
At present, the definitions of heat waves are inconsistent in the world.[16] The China Meteorological Administration has a clear definition of heat waves: the daily maximum temperature is greater than or equal to 35°C, and the duration is not less than 3 days.[17] However, owing to the large climatic differences in various regions of the country, there is a large spatial heterogeneity, and the research results of a single article cannot provide a reliable basis for the formulation of prevention and control measures. Previous studies have also been inconsistent regarding the relationship between heatwaves and mortality. We pooled previous studies through a meta-analysis to provide a comprehensive and quantitative assessment of the association between heat waves and mortality in China.
Therefore, the aim of this study was to employ a meta-analysis to identify and review the epidemiological evidence associated with heat waves and mortality in Chinese populations, quantify the magnitude of these effects, and identify potential factors while identifying sensitive populations.
2. Materials and methods
2.1. Ethical approval
This meta-analysis was based entirely on previous published studies which had declared ethical approvals and no original clinical raw data was collected or utilized, thereby ethical approval was not required for this study.
2.2. Literature search
According to the Preferred Reporting Items of the Systematic Reviews and Meta-analyses (PRISMA) checklist, a systematic search was conducted in China National Knowledge Infrastructure (CNKI), Wanfang Database, PubMed, Embase and Web of Science databases for articles published in both English and Chinese until November 2022. The search terms were “Chinese population OR Chinese region OR China,” “heat waves OR extreme temperature OR high temperature” and “death OR mortality OR death rate.” In addition, supplemented by a manual search and literature tracing methods, more relevant literature was collected. The details of the search strategy were provided in File 1, Supplemental Digital Content, http://links.lww.com/MD/I694.
2.3. Inclusion and exclusion criteria of literature
The inclusion criteria for this study were: research on the relationship between heatwaves and Chinese population mortality; original research; have a clear definition of heatwaves; and provide clear outcome measures such as RR and its 95% CI. The exclusion criteria were as follows: literature review or health education; non-Chinese population; inability to obtain original data; and duplicate publications or low-quality literature. Two authors (R.-R.P. and M.X.) independently searched all references, and all authors resolved discrepancies between the included studies by vote.
2.4. Data extraction
Two authors (R.-R.P and M.X.) independently performed the data extraction, discussed again, and resolved any disagreements by consensus. The following information was collected from each eligible study: first author’s surname, year of publication, study region, number of events, study design, lag days, definition of heat waves, characteristics of the study population, and type of effect estimate (RR).
2.5. Statistical analysis
The risk ratio (RR) and 95% confidence interval (CI) is commonly used to measure the association between heatwaves and population mortality. Heterogeneity among the studies was estimated using the I²and Q statistics. For the Q statistics, P < .10 indicated statistically significant heterogeneity and the I2 values of < 25%, 25% to 50%, 50% to 75%, and >75% indicated no, small, moderate, and significant heterogeneity, respectively.[18] Pooled RRs were obtained using either a fixed-effects model (I2 ≤ 50%) or a random-effects model (I2 > 50%).[19,20] In addition, we performed subgroup analyses using region, sex, age, number of events, and years of education to explore potential heterogeneity.
We used funnel plots, Egger’s linear regression test, and the prune and fill method to evaluate publication bias for outcome measures in more than 10 articles.[20–22] Sensitivity analyses were performed by excluding each study and analyzing the data. We also performed meta-regression analyses to examine the effect of the study period and the number of events on the association between heat waves and mortality in the Chinese population. All statistical analyses were performed using Stata version 17.0 (Stata Corp., College Station, TX). Significance was set at P < .05, except for heterogeneity estimation, and all statistical tests were two-sided.
3. Results
3.1. Literature search
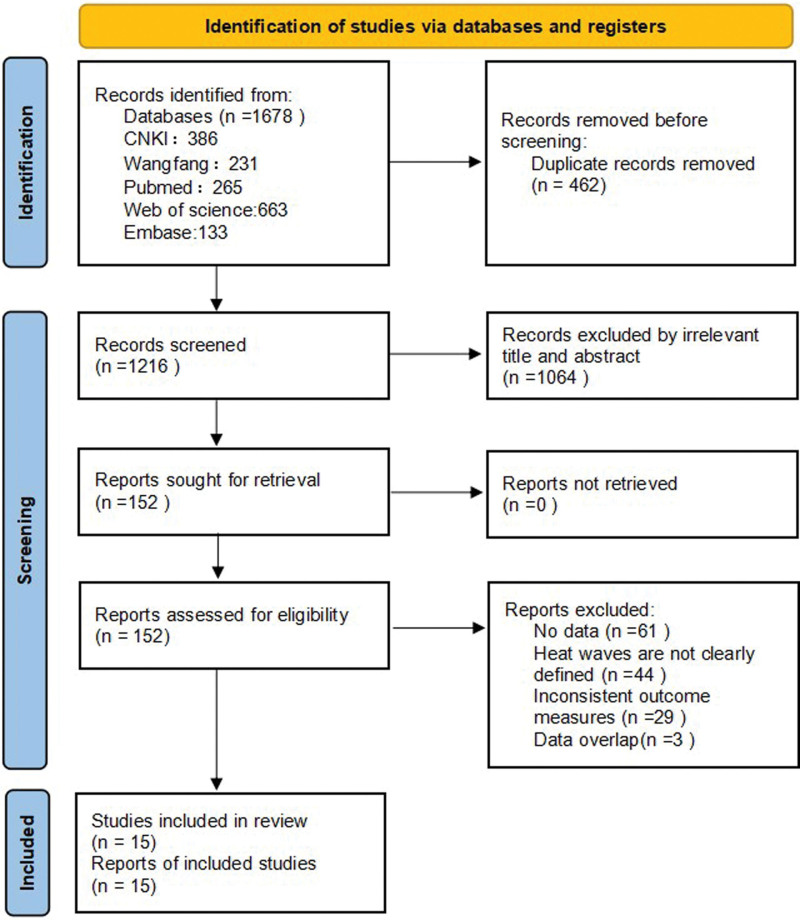
The database search identified 1678 studies on heat waves and the risk of mortality in Chinese populations, of these, 1663 were excluded for a range of reasons (462 duplicate articles, 1216 articles were screened by title and abstract, resulting in the exclusion of 1064 unrelated studies. Thereafter, 152 articles underwent full-text review, which resulted in the exclusion of 61 articles that did not provide an index of the available data, 44 did not report the definition of heat waves, and 29 articles that did not relate to outcomes, 3 data were reused.), resulted in the inclusion of 15 studies in the meta-analysis. The details of the literature search are shown in Figure 1.
Figure 1.
Flowchart of the study procedure. CNKI = China National Knowledge Infrastructure.
3.2. Study characteristics
The characteristics of the 15 included studies are summarized in Table 1. The studies were published between 2012 and 2022. Ten studies used distributed lag non-linear models, one used a case crossover study, three used generalized additive models, and one used Poisson regulation models. Seven studies were conducted in cities in southern China and six studies were conducted in cities in northern China. Eleven studies reported lag days, eight studies had event numbers above 10,000, four studies had event numbers below 10,000, and three studies remained unreported. Twelve studies reported the association between heat wave and non-accidental mortality, of which seven studies had event numbers above 10,000, three studies had event numbers below 10,000, and two studies remained unreported. Each study had a clear definition of a heat wave, of which seven were defined as the daily maximum temperature above 35°C for three consecutive days, two were defined as the daily maximum temperature of P95, one was defined as the mean temperature per day of P98, and four were defined as the mean temperature per day of P99.
Table 1.
Characteristics of 15 studies included in the meta-analysis.
| Author | Publication year | Study location | No. of events | Study design | Lag (d) | Definition of heat waves weather |
|---|---|---|---|---|---|---|
| Yang jun et al[23] | 2019 | Harbin, Changchun, Beijing, Shenyang, Tianjin,Shijiazhuang, Jinan, Zhengzhou, Shanghai,Nanjing, Chengdu, Chongqing, Changsha,Kunming and Guangzhou | 1,936,116 | Poisson regression models, distributed lag non-linear model (DLNM) | Lag 0–10 d | The daily maximum temperature was above 35°C for three consecutive days |
| Li lan et al[24] | 2012 | Harbin | 442 | Distributed lag non-linear model (DLNM) | NA | The mean temperature per day was higher than the maximum daily temperature of P98 |
| Zhang yuanquan et al[25] | 2017 | Hubei province | 146,676 | Distributed lag non-linear model (DLNM) | Lag 0–14 d | For three consecutive days above the daily maximum temperature of P99 |
| Bao junzhe et al[26] | 2016 | Wuhan, Changsha, Guilin, Haikou | NA | Distributed lag non-linear model (DLNM) | Lag 3, 7, 21 d | For three consecutive days above the daily maximum temperature of P99 |
| Wang cuicui et al[27] | 2014 | Suzhou | 49,984 | Poisson regression models, distributed lag non-linear model (DLNM) | Lag 0–14 d | least 7 consecutive days with daily maximum temperature above 35.0°C and daily average temperatures above the 97th percentile |
| Wang xuying et al[28] | 2015 | Beijing | NA | Distributed lag non-linear model (DLNM) | Lag 0–14 d | The mean temperature per day was higher than the maximum daily temperature of P99 |
| Zhang lingyan et al[12] | 2017 | Beijing Tianjin Hebei Region, Yangtze River Delta, Pearl River Delta | 477,240 | Distributed lag non-linear model (DLNM) | NA | The mean temperature per day was higher than the maximum daily temperature of P95 |
| Chen yichen et al[29] | 2020 | Shanghai | 93,040 | Distributed lag non-linear model (DLNM) | Lag 0–7 d | The daily maximum temperature was above 35°C for three consecutive days |
| Han jing et al[30] | 2019 | Jinan | 152,150 | Poisson regression models | Lag 7–14d | For three consecutive days above the daily maximum temperature of P95 |
| Luan guijie et al[31] | 2015 | Beijing | 558 | Case-crossover study | NA | The daily maximum temperature was above 35°C for three consecutive days |
| Wu kai et al[32] | 2015 | Wuhan | 2633 | Poisson generalized additive model (GAM) | Lag 0–7 d | The daily maximum temperature was above 35°C for three consecutive days |
| Zhang anran et al[33] | 2015 | Jinan | 1615 | Generalized additive model (GAM) | Lag 0–10 d | The daily maximum temperature was above 35°C for three consecutive days |
| Xu dandan et al[34] | 2017 | Shanghai | NA | Poisson generalized additive model (GAM) | NA | The daily maximum temperature was above 35°C for three consecutive days |
| Niu yanlin et al[35] | 2022 | Beijing | 192,568 | Distributed lag non-linear model (DLNM) | Lag 0–7 d | The daily maximum temperature was above 35°C for three consecutive days |
| Gu shaohua et al[36] | 2021 | Ningbo | 102,954 | Generalized linear model (GLM) and Distributed lag non-linear model (DLNM) | Lag 0–14 d | For three consecutive days above the daily maximum temperature of P99 |
NA = not available.
3.3. Influence of heat waves on the non-accidental mortality in China
Figure 2 shows the overall analysis of the mortality risk of non-accidental deaths in China due to heat waves. We observed high heterogeneity in the results of these studies (Q = 127.17, P < .01, I2 = 91.3%). And the random-effects model was applied, the summary RR for 12 studies showed that heatwave was associated with a 1.19-fold increased risk of non-accidental death population in China (RR = 1.19, 95% CI = 1.13–1.27, P < .01).
Figure 2.
Influence of heat waves on the non-accidental mortality in China. CI = confidence interval, RR = risk ratio.
3.4. Influence of heat waves on death of people with cardiovascular disease, stroke, respiratory disease and circulatory disease in China
The impact of heatwaves on the mortality risk of Chinese patients with CVD was explored for nine studies. The heterogeneity test results showed significant heterogeneity among these studies (Q = 92.67, P < .001, I2 = 91.4%). Applying random effects models, nine studies were summarized to show that heat waves increase the risk of death in Chinese patients with CVD (RR = 1.25, 95% CI: 1.14–1.38) (Fig. 3).
Figure 3.
Influence of heat waves on death of people with cardiovascular disease in China. CI = confidence interval, RR = risk ratio.
Five studies investigated the effect of heat waves on mortality risk of stroke patients in China. The heterogeneity test results showed significant heterogeneity among these studies (Q = 11.11, P = .025, I2 = 64.0%). By applying random effects models, five studies were summarized to show that heat waves increase the risk of death in Chinese patients with stroke (RR = 1.11, 95% CI: 1.03–1.20) (Fig. 4).
Figure 4.
Influence of heat waves on death of people with stroke in China. CI = confidence interval, RR = risk ratio.
Eight studies reported the impact of heat waves on mortality among patients with respiratory diseases in China. The heterogeneity test results showed significant heterogeneity among these studies (Q = 18.44, P = .010, I2 = 62.0%). By applying random effects models, eight studies were summarized to show that heat waves increase the risk of death in Chinese patients with respiratory disease (RR = 1.18, 95% CI: 1.09–1.28) (Fig. 5).
Figure 5.
Influence of heat waves on death of people with respiratory disease in China. CI = confidence interval, RR = risk ratio.
Two studies examined the effect of heat waves on mortality risk in patients with circulatory diseases in China. The heterogeneity test results showed no significant heterogeneity among these studies (Q = 0.0, P = .487, I2 = 0.0%). Applying fixed–effects models, two studies were summarized to show that heat waves increase the risk of death in Chinese patients with circulatory disease (RR = 1.11, 95% CI: 1.06–1.17) (Fig. 6).
Figure 6.
Influence of heat waves on death of people with circulatory disease in China. CI = confidence interval, RR = risk ratio.
3.5. Subgroup analyses
To further explore the potential heterogeneity of the association between heatwaves and non-unexpected mortality in China, we conducted a subgroup analysis. The results showed that individuals with ˂6 years of education had a higher risk of non-accidental death from heat waves than those with ≥ 6 years of education, years of education ≤ 6: (RR = 1.24, 95% CI: 1.11–1.39); years of Education > 6 (RR = 1.07, 95% CI: 1.00–1.15); When it was conducted by region sex and age, there was no significant difference in south and north, the increased risk was observed both in south (RR = 1.20, 95% CI: 1.11–1.32) and in north (RR = 1.26, 95% CI: 1.11–1.43), the increased risk was observed both in male (RR = 1.10, 95% CI: 1.05–1.14),and in female (RR = 1.17, 95% CI: 1.10–1.24); age with 0 to 64 years (RR = 1.13, 95% CI: 1.02–1.26), age with 65 to 74 years (RR = 1.07, 95% CI: 1.01–1.13) and age ≥ 75 years (RR = 1.15, 95% CI: 1.11–1.19).
Again, we reached a consistent conclusion based on the number of events (number of events ˂ 10,000: RR = 1.49, 95% CI: 1.15–1.94; number of events ≥ 10,000: RR = 1.13, 95% CI: 1.06–1.20) (Table 2).
Table 2.
Subgroup analysis of the association between heat waves and non-accidental mortality in China.
| Subgroups | No. of Studies | Heterogeneity test | RR | 95% CI | Z | P value | ||
|---|---|---|---|---|---|---|---|---|
| I2 (%) | Q | P value | ||||||
| Region | ||||||||
| South | 5 | 88.1 | 33.65 | <.001 | 1.20 | 1.11–1.32 | 3.91 | <.001 |
| North | 5 | 95.2 | 83.17 | <.001 | 1.26 | 1.11–1.43 | 3.96 | <.001 |
| Sex | ||||||||
| Male | 7 | 50.9 | 12.22 | .057 | 1.10 | 1.05–1.14 | 4.50 | <.001 |
| Female | 7 | 65.1 | 17.19 | .009 | 1.17 | 1.10–1.24 | 5.31 | <.001 |
| Age (yr) | ||||||||
| 0–64 | 5 | 66.2 | 11.83 | .019 | 1.13 | 1.02–1.26 | 2.40 | .017 |
| 65–74 | 3 | 3.1 | 2.06 | .356 | 1.07 | 1.01–1.13 | 2.33 | .020 |
| ≥75 | 6 | 30.1 | 7.15 | .210 | 1.15 | 1.11–1.19 | 7.54 | <.001 |
| Number of events | ||||||||
| <10,000 | 3 | 91.4 | 23.30 | <.001 | 1.49 | 1.15–1.94 | 3.01 | .003 |
| ≥10,000 | 7 | 89.8 | 58.96 | <.001 | 1.13 | 1.06–1.20 | 4.02 | <.001 |
| Years of education | ||||||||
| <6 | 5 | 81.2 | 21.28 | <.001 | 1.24 | 1.11–1.39 | 3.87 | <.001 |
| ≥6 | 5 | 57.7 | 9.46 | .051 | 1.07 | 1.00–1.15 | 2.09 | .037 |
CI = confidence interval, RR = risk ratio.
3.6. Meta regression
The results of the meta-regression analysis showed that increasing years had a significant effect on the association between heatwaves and deaths in the Chinese non accidental mortality population (coefficient = −0.040, P = .027), which could explain 50.57% of the heterogeneity (Fig. 7). However, the number of events (P = .316) did not significantly affect the association between heatwaves and non-accidental mortality (Fig. 8).
Figure 7.
Random-effects meta-regression analysis to explore the effect of year on association between heat waves and non-accidental mortality in China. RR = risk ratio.
Figure 8.
Random-effects meta-regression analysis to explore the effect of number of events on association between heat waves and non-accidental mortality in China. RR = risk ratio.
3.7. Sensitivity analysis and publication bias
The results of the sensitivity analysis showed that Han’s study inclusion and exclusion significantly affected the magnitude of the heterogeneity associated with the pooled RR. After excluding this study, the pooled RR was reduced but was still statistically significant (RR = 1.21, 95% CI: 1.14–1.29) and the heterogeneity was reduced (I2 = 3.6%). Additionally, the pooled results remained statistically significant after excluding one study at a time (Figure S1, Supplemental Digital Content, http://links.lww.com/MD/I695).
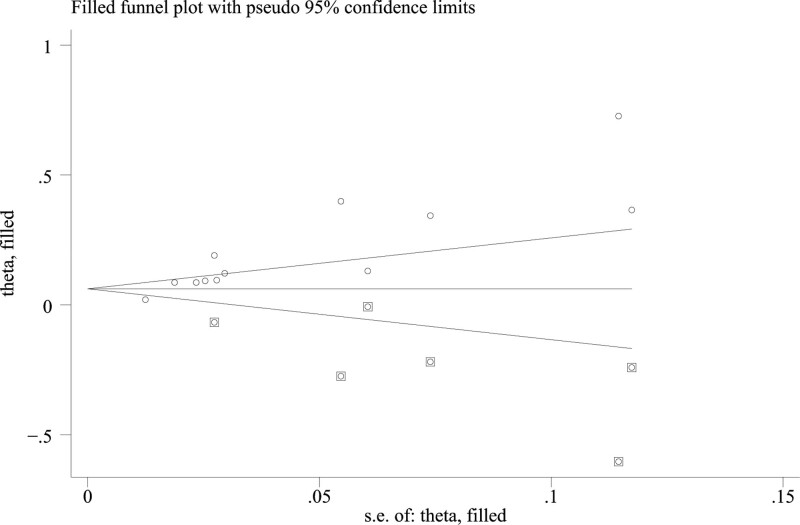
Funnel plots, Egger’s test, and the trimmed fill method were used to detect publication bias. The results from both methods (Egger’s test: P < .01, funnel plot: Figure S2, Supplemental Digital Content, http://links.lww.com/MD/I696) indicated possible publication bias. Before the trimmed fill, the combined RR of the heatwave and non-accidental death population in China was 1.19 (95% CI: 1.13–1.27, P < .01). After three iterations using the linear method, the number of missing studies was estimated to be six. Six studies were added to the shear compensation method and a meta-analysis was conducted for all studies. The results showed that the heterogeneity test yielded Q = 254.153, P < .01. The random effects model was used to combine the effect indicators, and the result was RR = 1.073 (95% CI: 1.009–1.141, P = .025). The results before and after the metric were stable and statistically significant, which means that the publication bias of this study can be ignored (Fig. 9).
Figure 9.
Funnel plot was used to evaluate the publication bias of meta-analysis.
4. Discussion
The present results, combined with the RRs from 15 articles, show that heat waves were associated with increased mortality risk in the Chinese population. This relationship was also consistent in subgroup analyses by study region, sex, age, years of education, and number of events. Thus, this meta-analysis is probably the best available evidence on the consistency and strength of the association between heat wave exposure and increased risk of mortality in the Chinese population. The human body is in a high-temperature environment, and it dissipates heat through conduction, radiation, and evaporation to maintain the balance of the body mechanism.[37,38] However, the process of heat dissipation can easily cause the loss of water in the human body,[39] the blood is relatively concentrated, and the viscosity increase, which affects the supply of visceral blood, increases the burden on the cardiovascular system,[40] and also affects the neural activity and movement coordination of the human body.[41]
This study found that heat waves significantly increased the risks of non-accidental deaths, deaths caused by cardiovascular diseases, stroke, respiratory diseases and circulatory diseases in China. The 19% increase in risk of non-accidental mortality due to heatwaves in China was higher than that in Sweden (10%)[42] and the United States (11%),[43] However, it was lower than India (43.1%)[44] and Pakistan (166.8%).[45] Developed regions, such as the United States, have a high economic level and more abundant healthcare resources, while developing countries, such as India, have a large population, relatively low economic level, lack of medical resources, and low public awareness of heat-related risks, resulting in differences in the impact of heatwaves on mortality.
Heat waves could lead to an accelerated heart rate, vasodilation, water and electrolyte loss, and increased blood viscosity in the human circulatory system, ultimately resulting in a higher risk of death among patients with cardiovascular disease.[46,47] Patients with preexisting chronic lung diseases are more vulnerable to heat-induced illnesses during heat waves.[48] The reason for this was the physiological impairment of the core temperature regulation in a hot environment. In addition, they are less able to dissipate excess heat, which increases their risk of suffering from heat stress conditions, such as dehydration and heatstroke.[49] Heat waves increase the risk of mortality in the Chinese circulatory population because blood flow must be redistributed to the periphery (vasodilation) away from the core organs during heat waves and increased sweat production.[50] Patients with preexisting circulatory disease have impaired mechanisms to adequately increase cardiac output, resulting in inadequate skin blood flow as the core temperature rises.[50] As the body’s core temperature increases, dehydration occurs, which affects the heart and other organs.[51]
Another interesting finding was that the risk of non-accidental death during heat waves was higher among people with ˂6 years of education than among those with ≥ 6 years of education, consistent with Ghumman and Horney.[45] It may be that those with fewer years of education are more likely to engage in outdoor work and lack health-related knowledge. Meta-regression results showed that increasing years had a significant effect on the association between heat waves and non-accidental mortality in China. In recent decades, significant reductions in mortality risks associated with heat waves have also been observed in the USA[52] and other developed regions of the world.[53,54] These are primarily related to improved healthcare, greater public awareness of heat-related risks, and increased use of air conditioning. The significant decline was mainly attributed to China’s substantial socioeconomic development and improvements in quality of life (including more effective health care and lifestyle changes).
Our study had significant strengths. First, this is the first meta-analysis and systematic review to explore the association between heatwaves and mortality in the Chinese population. Second, although most of the results showed significant heterogeneity, we performed a meta-regression analysis on the year and number of events to identify sources, which could explain 50.57% of the inter study heterogeneity. Third, the sample size of most of the included studies was > 10,000. A meta-analysis with a large sample size provided relatively strong statistical power to test the correlation.
Although this meta-analysis included 15 studies to examine the association between ring heat waves and mortality in the Chinese population, it has several limitations. First, the study was highly heterogeneous, although the use of subgroup analyses and meta-regression to explore the sources of heterogeneity explains some of this heterogeneity. Second, the research methods used in the included studies were not consistent, ten studies used distributed lag non-linear models, one used case crossover studies, three used generalized additive models, and one used Poisson regulation models. Third, most of the included studies tended to report the largest effect estimate, and the effect estimate for different lag days could not be fully used in the analysis. We ignored the lag effect and selected the largest effect estimate for meta-analysis, which also led to heterogeneity. Fourth, although we accounted for this issue by the trimmed fill method, our study was subject to publication bias. The relevance of our findings, although exciting, requires further investigation using larger population samples and subgroup analyses.
5. Conclusion
In summary, the present meta-analysis provides strong evidence that heat waves are significantly associated with an increased risk of death in the Chinese population, especially among residents with low education levels. Therefore, high-risk populations should be the focus of public health policies, and prevention strategies should be developed and implemented to effectively reduce the public health harm caused by extreme temperature events.
Acknowledgments
We thank the original studies for their contributions in conducting our meta-analysis.
Author contributions
Conceptualization: Ranran Pan, Mengxiang Chen, Junhua Zhou.
Data curation: Ranran Pan, Ming Xie, Yannan Zhang.
Formal analysis: Ranran Pan, Yannan Zhang.
Funding acquisition: Ranran Pan, Junhua Zhou.
Investigation: Ranran Pan, Ming Xie, Yannan Zhang.
Methodology: Ranran Pan, Ming Xie, Yannan Zhang.
Project administration: Ranran Pan, Ming Xie, Mengxiang Chen, Junhua Zhou.
Resources: Ranran Pan, Mengxiang Chen.
Software: Ranran Pan, Ming Xie, Mengxiang Chen, Jian Ma.
Supervision: Ranran Pan, Ming Xie, Jian Ma, Junhua Zhou.
Validation: Mengxiang Chen, Yannan Zhang.
Visualization: Mengxiang Chen, Jian Ma.
Writing – original draft: Ranran Pan.
Writing – review & editing: Mengxiang Chen, Yannan Zhang, Jian Ma.
Supplementary Material
Abbreviations:
- CI
- confidence interval
- RR
- risk ratio
This study was supported by the Natural Science Foundation Project of Hunan Province (no: 2020JJ5387).
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are publicly available.
Supplemental Digital Content is available for this article.
How to cite this article: Pan R, Xie M, Chen M, Zhang Y, Ma J, Zhou J. The impact of heat waves on the mortality of Chinese population: A systematic review and meta-analysis. Medicine 2023;102:13(e33345).
Contributor Information
Ranran Pan, Email: blingran@163.com.
Ming Xie, Email: xieming1125@126.com.
Mengxiang Chen, Email: 1509608279@qq.com.
Yannan Zhang, Email: 2536625470@qq.com.
Junhua Zhou, Email: zhoujunhua@hunnu.edu.cn.
References
- [1].Chaseling GK, Iglesies-Grau J, Juneau M, et al. Extreme heat and cardiovascular health: what a cardiovascular health professional should know. Can J Cardiol. 2021;37:1828–36. [DOI] [PubMed] [Google Scholar]
- [2].Keller CF. Global warming 2007. An update to global warming: the balance of evidence and its policy implications. ScientificWorldJournal. 2007;7:381–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Royé D, Codesido R, Tobías A, et al. Heat wave intensity and daily mortality in four of the largest cities of Spain. Environ Res. 2020;182:109027. [DOI] [PubMed] [Google Scholar]
- [4].Parks RM, Bennett JE, Tamura-Wicks H, et al. Anomalously warm temperatures are associated with increased injury deaths. Nat Med. 2020;26:65–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Cheshire WP, Jr. Thermoregulatory disorders and illness related to heat and cold stress. Auton Neurosci. 2016;196:91–104. [DOI] [PubMed] [Google Scholar]
- [6].Balli S, Shumway KR, Sharan S. Physiology, Fever. In: StatPearls. Treasure Island, FL: StatPearls Publishing; September 11, 2022. [PubMed] [Google Scholar]
- [7].D’Ippoliti D, Michelozzi P, Marino C, et al. The impact of heat waves on mortality in 9 European cities: results from the EuroHEAT project. Environ Health. 2010;9:37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Wang XY, Guo Y, FitzGerald G, et al. The impacts of heatwaves on mortality differ with different study periods: a multi-city time series investigation. PLoS One. 2015;10:e0134233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Kosatsky T. The 2003 European heat waves. Euro Surveill. 2005;10:148–9. [PubMed] [Google Scholar]
- [10].Patz JA, Campbell-Lendrum D, Holloway T, et al. Impact of regional climate change on human health. Nature. 2005;438:310–7. [DOI] [PubMed] [Google Scholar]
- [11].Fouillet A, Rey G, Wagner V, et al. Has the impact of heat waves on mortality changed in France since the European heat wave of summer 2003? A study of the 2006 heat wave. Int J Epidemiol. 2008;37:309–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Zhang L, Zhang Z, Ye T, et al. Mortality effects of heat waves vary by age and area: a multi-area study in China. Environ Health. 2018;17:54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Gu S, Huang C, Bai L, et al. Heat-related illness in China, summer of 2013. Int J Biometeorol. 2016;60:131–7. [DOI] [PubMed] [Google Scholar]
- [14].Sun Z, Chen C, Yan M, et al. Heat wave characteristics, mortality and effect modification by temperature zones: a time-series study in 130 counties of China. Int J Epidemiol. 2021;49:1813–22. [DOI] [PubMed] [Google Scholar]
- [15].Pu X, Wang TJ, Huang X, et al. Enhanced surface ozone during the heat wave of 2013 in Yangtze River Delta region, China. Sci Total Environ. 2017;603-604:807–16. [DOI] [PubMed] [Google Scholar]
- [16].Kanti FS, Alari A, Chaix B, et al. Comparison of various heat waves definitions and the burden of heat-related mortality in France: implications for existing early warning systems. Environ Res. 2022;215:114359. [DOI] [PubMed] [Google Scholar]
- [17].Huang Z, Chen H, Tian H. Research on indicators of heat wave. Meteorol J. 2011;37:345–51. [Google Scholar]
- [18].Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58. [DOI] [PubMed] [Google Scholar]
- [20].Higgins JP, Thompson SG, Spiegelhalter DJ. A re-evaluation of random-effects meta-analysis. J R Stat Soc Ser A Stat Soc. 2009;172:137–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–101. [PubMed] [Google Scholar]
- [23].Yang J, Yin P, Sun J, et al. Heatwave and mortality in 31 major Chinese cities: definition, vulnerability and implications. Sci Total Environ. 2019;649:695–702. [DOI] [PubMed] [Google Scholar]
- [24].Lan L, Cui G, Yang C, et al. Increased mortality during the 2010 heat wave in Harbin, China. Ecohealth. 2012;9:310–4. [DOI] [PubMed] [Google Scholar]
- [25].Zhang Y, Yu C, Bao J, et al. Impact of temperature on mortality in Hubei, China: a multi-county time series analysis. Sci Rep. 2017;7:45093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Bao J, Wang Z, Yu C, et al. The influence of temperature on mortality and its Lag effect: a study in four Chinese cities with different latitudes. BMC Public Health. 2016;16:375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Wang C, Chen R, Kuang X, et al. Temperature and daily mortality in Suzhou, China: a time series analysis. Sci Total Environ. 2014;466-467:985–90. [DOI] [PubMed] [Google Scholar]
- [28].Wang X, Li G, Liu L, et al. Effects of extreme temperatures on cause-specific cardiovascular mortality in China. Int J Environ Res Public Health. 2015;12:16136–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Chen Y, Peng L, Zhou Y, et al. Impact of heat wave on daily mortality and disease burden in Pudong New Area of Shanghai: a case-crossover study. Environ Occupational Med. 2020;5:657–63. [Google Scholar]
- [30].Han J, Fang Q, Zhou L, et al. Effects of extreme air temperature on non-accidental mortality and major cause-specific mortality in Ji ‘nan. China Public Health. 2019;35:1242–4. [Google Scholar]
- [31].Luan G, Li T, Yin P, et al. The impact of heat wave on deaths in Beijing in 2010. Environ Hyg. 2015;5:525–9. [Google Scholar]
- [32].Wu K, Zhang Y, Zhu C, et al. Association between heat wave and stroke mortality in Jiang ‘an district of Wuhan, China: a time-series analysis. Chin J Cardiol. 2015;43:1092–6. [PubMed] [Google Scholar]
- [33].Zhang A, Hu W, Li J, et al. A case-crossover study on the impact of heat waves on mortality from circulatory diseases. J Shandong Univ (Med Ed). 2018;56:56–62. [Google Scholar]
- [34].Xu D, Ban J, Chen C, et al. The impact of the high temperature and heat wave incident in Shanghai from 2013 to 2015 on the risk of death among people. J Environ Health. 2017;34:991–5. [Google Scholar]
- [35].Niu Y, Yang J, Lin H, et al. Additive effect of heat wave on mortality in Beijing. Chin J Public Health. 2021;38:344–50. [Google Scholar]
- [36].Gu S, Lu B, Wang Y, et al. Research on meteorological indicators for high temperature health risk early warning. Prev Med. 2022;34:803–08 + 15. [Google Scholar]
- [37].Liu C, Yavar Z, Sun Q. Cardiovascular response to thermoregulatory challenges. Am J Physiol Heart Circ Physiol. 2015;309:H1793–812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Zheng G, Wang Y, Li C, et al. Real-time quantification of human physiological state in high temperature environments based on variable weight theory. J Therm Biol. 2020;89:102531. [DOI] [PubMed] [Google Scholar]
- [39].Périard JD, Travers GJS, Racinais S, et al. Cardiovascular adaptations supporting human exercise-heat acclimation. Auton Neurosci. 2016;196:52–62. [DOI] [PubMed] [Google Scholar]
- [40].Cramer MN, Jay O. Biophysical aspects of human thermoregulation during heat stress. Auton Neurosci. 2016;196:3–13. [DOI] [PubMed] [Google Scholar]
- [41].Mizunuma M, Takahashi N, Usami A, et al. High-temperature, but not high-pressure, conditions alter neuronal activity. J Pharmacol Sci. 2009;110:117–21. [DOI] [PubMed] [Google Scholar]
- [42].Oudin Åström D, Åström C, Forsberg B, et al. Heat wave-related mortality in Sweden: a case-crossover study investigating effect modification by neighbourhood deprivation. Scand J Public Health. 2020;48:428–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Matte TD, Lane K, Ito K. Excess mortality attributable to extreme heat in New York City, 1997-2013. Health Secur. 2016;14:64–70. [DOI] [PubMed] [Google Scholar]
- [44].Azhar GS, Mavalankar D, Nori-Sarma A, et al.; Ahmedabad HeatClimate Study Group. Heat-related mortality in India: excess all-cause mortality associated with the 2010 Ahmedabad heat wave. PLoS One. 2014;9:e91831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Ghumman U, Horney J. Characterizing the impact of extreme heat on mortality, Karachi, Pakistan, June 2015. Prehosp Disaster Med. 2016;31:263–6. [DOI] [PubMed] [Google Scholar]
- [46].Yin Q, Wang J. The association between consecutive days’ heat wave and cardiovascular disease mortality in Beijing, China. BMC Public Health. 2017;17:223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Wainwright SH, Buchanan SD, Mainzer HM, et al. Cardiovascular mortality--the hidden peril of heat waves. Prehosp Disaster Med. 1999;14:222–31. [PubMed] [Google Scholar]
- [48].Kenny GP, Yardley J, Brown C, et al. Heat stress in older individuals and patients with common chronic diseases. CMAJ. 2010;182:1053–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].De Sario M, Katsouyanni K, Michelozzi P. Climate change, extreme weather events, air pollution and respiratory health in Europe. Eur Respir J. 2013;42:826–43. [DOI] [PubMed] [Google Scholar]
- [50].Bouchama A, Knochel JP. Heat stroke. N Engl J Med. 2002;346:1978–88. [DOI] [PubMed] [Google Scholar]
- [51].Cui J, Arbab-Zadeh A, Prasad A, et al. Effects of heat stress on thermoregulatory responses in congestive heart failure patients. Circulation. 2005;112:2286–92. [DOI] [PubMed] [Google Scholar]
- [52].Davis RE, Knappenberger PC, Novicoff WM, et al. Decadal changes in summer mortality in U.S. cities. Int J Biometeorol. 2003;47:166–75. [DOI] [PubMed] [Google Scholar]
- [53].Gasparrini A, Guo Y, Hashizume M, et al. Temporal variation in heat-mortality associations: a multi country study. Environ Health Perspect. 2015;123:1200–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Matzarakis A, Muthers S, Koch E. Human biometeorological evaluation of heat-related mortality in Vienna. Theor Appl Climatol. 2011;105:1–10. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.