Abstract
BACKGROUND
Minimizing contrast dose and radiation exposure while maintaining image quality during computed tomography angiography (CTA) for transcatheter aortic valve replacement (TAVR) is desirable, but not well established. This systematic review compares image quality for low contrast and low kV CTA versus conventional CTA in patients with aortic stenosis undergoing TAVR planning.
METHODS
We performed a systematic literature review to identify clinical studies comparing imaging strategies for patients with aortic stenosis undergoing TAVR planning. The primary outcomes of image quality as assessed by the signal-to-noise ratio (SNR) and contrast-to-noise ratio (CNR) were reported as random effects mean difference with 95% confidence interval (CI).
RESULTS
We included 6 studies reporting on 353 patients. There was no difference in cardiac SNR (mean difference, −1.42; 95% CI, −5.71 to 2.88; p = 0.52), cardiac CNR (mean difference, −3.83; 95% CI, −9.98 to 2.32; p = 0.22), aortic SNR (mean difference, −0.23; 95% CI, −7.83 to 7.37; p = 0.95), aortic CNR (mean difference, −3.95; 95% CI, −12.03 to 4.13; p = 0.34), and ileofemoral SNR (mean difference, −6.09; 95% CI, −13.80 to 1.62; p = 0.12) between the low dose and conventional protocols. There was a difference in ileofemoral CNR between the low dose and conventional protocols with a mean difference of −9.26 (95% CI, −15.06 to −3.46; p = 0.002). Overall, subjective image quality was similar between the 2 protocols.
CONCLUSIONS
This systematic review suggests that low contrast and low kV CTA for TAVR planning provides similar image quality to conventional CTA.
Keywords: Aortic valve, Contrast media, Heart valve prosthesis
INTRODUCTION
Transcatheter aortic valve replacement (TAVR) is an established treatment method for patients with symptomatic severe aortic stenosis regardless of their surgical risk.1) Computed tomography angiography (CTA) is often used for TAVR planning to comprehensively assess valve anatomy and vascular access to facilitate patient selection and prosthesis sizing.2),3) Patients undergoing TAVR are often elderly with multiple comorbidities including renal dysfunction.4) The use of iodinated contrast media in patients with renal dysfunction undergoing TAVR can cause acute kidney injury that is associated with increased morbidity and mortality.5) Therefore, reducing the amount of contrast media administered during CTA for TAVR planning is an active area of research.6) The use of radiation protection strategies by using low tube voltage settings has shown promise to reduce contrast media volumes for CTA.7) However, there is limited data on image quality using low contrast and low kV CTA for TAVR planning. The objective of this systematic review was to assess image quality for low contrast and low kV CTA versus conventional CTA in patients for TAVR planning.
METHODS
This study did not require ethical approval because only public published data was used. The reporting of this systematic review follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement.8) This review was submitted to PROSPERO for registration.
Search strategy
We performed a systematic literature review to identify randomized and nonrandomized clinical studies that reported qualitative and quantitative image outcomes using low contrast and low radiation CT protocols in patients before TAVR. Searches were limited to peer-reviewed articles published in English up to March 1st, 2022. This research involved human subjects and described image quality on patients undergoing CT for TAVR assessment. We developed the search strategy according to available guidance from the Cochrane Collaboration.
The search strategy in PubMed explored Medical Subject Heading (MeSH) terms related to patients undergoing low contrast and low kV CTA for TAVR assessment. The exact search strategy is available as a supplementary file. The articles found to be relevant during the search were stored in EndNote. References from full-text articles were also evaluated and considered for inclusion.
Study selection
Articles were selected for inclusion based on predefined criteria, which included low contrast and radiation dose CT protocols for TAVR assessment. The primary outcome was quantitative image quality as assessed by the signal-to-noise ratio (SNR) or contrast-to-noise ratio (CNR). We excluded feasibility studies, case series, studies that did not report on our primary outcome, and studies that did not have different contrast volumes between groups.
Two authors (SL, MB) independently completed literature searches and screened abstracts to choose potentially relevant articles. Selected articles underwent full evaluation to assess their potential inclusion in the systematic review.
Risk for bias
The risk for bias was assessed using the Cochrane tool for assessing the risk for bias in randomized controlled trials (RCTs).9) The risk of bias for non-randomized trials was evaluated using the ROBINS-I tool.10) The risk for bias was assessed by 2 independent reviewers (SL, MB).
Statistical analysis
Review Manager software 5.4 was used for data analysis. Pooled estimates were calculated using Mantel-Hansel methods. The DerSimonian and Laird11) approach was used for random effects model estimation. We preferred the random effects model to account for potential statistical heterogeneity. Pooled estimates were presented as mean difference with 95% confidence intervals (CI). A χ2 test of heterogeneity was calculated for each pooled analysis. The I2 measure of statistical heterogeneity was also estimated, with higher I2 values representing greater heterogeneity. All statistical tests were two-sided and p-values < 0.05 were considered significant.
RESULTS
Literature search
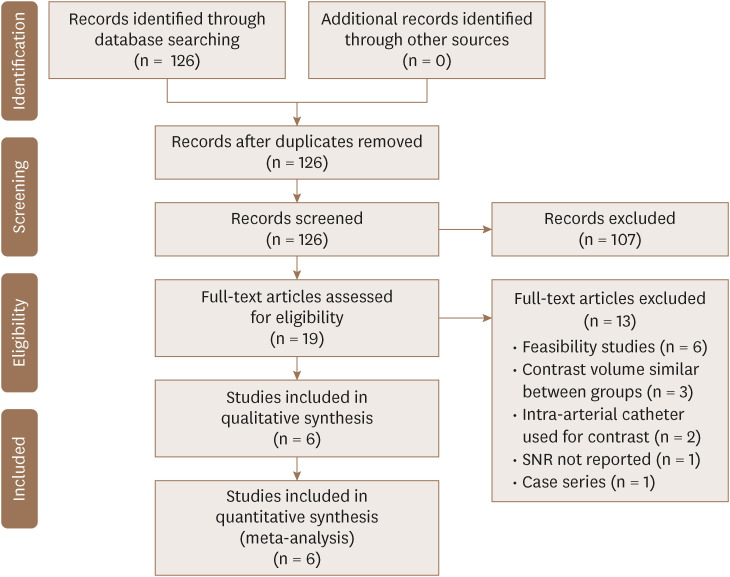
Our search yielded 126 abstracts. We excluded 107 studies at the abstract level and selected 19 full-text articles for detailed assessment; 6 studies were ultimately included in our systematic review. Figure 1 describes the flow-chart of included studies.
Figure 1. Flow chart of the included studies.
SNR: signal-to-noise ratio.
Baseline characteristics of the studies
Table 1 shows the baseline characteristics of the included studies. All studies were published between 2017 and 2020. The 6 studies included 353 patients and the median age of the participants was 82.5 years interquartile range (IQR) (80.4–83.8). The median percentage of men was 51.0 IQR (41.4–54.5). The median BMI for participants was 26.0 IQR (24.8–27.3). In the study by Felmy et al., 25% of the patients were in atrial fibrillation. While in the studies by Franzesi et al. and Ippolito et al., 100% of the patients were in sinus rhythm. In the study by Suchá et al., the low-dose group had significantly worse kidney function with median creatinine of 1.6 compare to median creatinine of 1.0 in the conventional group.
Table 1. Baseline characteristics of the included studies.
| Study, author, year | Location | Sample size | Group | Group size | Mean age, years | Men, % | BMI (kg/m2) | Atrial fibrillation (%) | Sinus rhythm (%) | HR (bpm) | LV EF (%) | Creatinine (mg/dL) | GFR (mL/min/1.73m2) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Felmly et al.,13) 2017 | SC, USA | 40 | Group B (low-dose) | 20 | 78.6 ± 7.6 | 75 | 28.1 ± 5.4 | 25 | NR | 62.6 ± 12.4 | 62.6 ± 17.1 | NR | NR |
| Group A (standard) | 20 | 81.8 ± 6.2 | 70 | 24.8 ± 3.8 | 25 | NR | 68.7 ± 11.2 | 58.3 ± 15.9 | NR | NR | |||
| Franzesi et al.,14) 2018 | Italy | 79 | Study group | 42 | 83.6 (79–89) | 45 | 24.8 ± 2.9 | NR | 100 | 73 ± 6.8 | NR | NR | NR |
| Control group | 37 | 84.3 (81–90) | 54 | 25.4 ± 3.8 | NR | 100 | 75 ± 8.7 | NR | NR | NR | |||
| Hachulla et al.,15) 2019 | Switzerland | 84 | Protocol 2: 60 mL contrast | 42 | 83 ± 6.8 | 52 | 27.2 ± 4.6 | NR | NR | 75.5 ± 11.0 | NR | NR | NR |
| Protocol 1: 120 mL contrast | 42 | 86.3 ± 6.5 | 43 | 26.5 ± 5.0 | NR | NR | 76.3 ± 12.2 | NR | NR | NR | |||
| Onoda et al.,16) 2019 | Japan | 40 | 70 kV group | 30 | 84.2 ± 5.8 | 37 | 20.3 ± 3.6 | NR | NR | NR | 62.4 ± 12.2 | 0.91 ± 0.44 | 61.4 ± 25.5 |
| 120/120 kV group | 10 | 83.5 ± 6.0 | 30 | 23.4 ± 4.8 | NR | NR | NR | 66.1 ± 5.4 | 0.67 ± 0.19 | 75.0 ± 28.4 | |||
| Ippolito et al.,17) 2020 | Italy | 60 | Study group | 32 | 73.32 (43–78) | 56 | NR | NR | 100 | 76 ± 6.05 | NR | NR | NR |
| Control group | 28 | 76.14 (56–88) | 50 | NR | NR | 100 | 75 ± 8.7 | NR | NR | NR | |||
| Suchá et al.,18) 2020 | CA, USA | 50 | Low-CM | 25 | 82 ± 7.9 | 52 | 27.3 ± 6.4 | NR | NR | NR | NR | 1.6 (1.5–1.9) | 36 (32–44) |
| Standard-CM | 25 | 81 ± 7.2 | 36 | 28.0 ± 5.1 | NR | NR | NR | NR | 1.0 (0.9–1.1) | 60 (51–86) |
Values are mean ± SD, median (interquartile range), or number (%).
BMI: body mass index, bpm: beats per minute, CA: California, GFR: glomerular filtration rate, HR: heart rate, LV EF: left ventricle ejection fraction, NR: not reported, SC: South Carolina, USA: United States of America.
Risk for bias
The risk for bias revealed adequate randomization and allocation concealment in the 1 RCT included in this study. Blinding for qualitative image assessment was not addressed in the RCT due to the nature of the study. The non-RCTs included in this study had appropriate selection and ascertainment approaches, while blinded assessments were deficient. Overall, the risk for bias in the measurement of the quantitative image outcomes was low.
Low contrast dose strategies for CTA for TAVR planning
The included studies reported image quality in patients undergoing low contrast CTA for TAVR planning as summarized in Table 2.12),13),14),15),16),17) Felmly et al.12) low-dose protocol consisted of a third-generation dual-source CT at 70 kW with 40 ml contrast compared to a conventional protocol with a second-generation dual-source CT at 100 kW and 60 mL contrast. Aortoiliac SNR was higher for the low-dose protocol (low dose: 15.4 ± 6.7, conventional: 13.1 ± 6.8, p = 0.0003), whereas cardiac SNR (conventional: 15.6 ± 9.0, low dose: 12.2 ± 4.5, p = 0.0003) and cardiac CNR (conventional: 20.2 ± 13.4, low dose: 15.3 ± 6.7, p = 0.0181) were higher for the conventional protocol. Subjective image quality was similar between the 2 groups for cardiac and aortoiliac attenuation and noise. However, there was significantly increased subjective image quality for aortoiliac image noise for the low dose protocol (low dose: 4.42 [IQR 4.0–5.0], conventional 4.12 [IQR 4.0–5.0], p = 0.037). All TAVR candidates were safely and effectively evaluated using the low-dose protocol.12) Franzesi et al.13) low-dose protocol consisted of 100 kV, 50 mL contrast, whole-body retrospective ECG-gating, and iterative reconstruction algorithm compared to a conventional protocol using 120 kV, 100 mL contrast, ECG-gating for chest, and Filtered back Projection reconstruction. All patients were examined with a 256-multidector CT. Higher mean attenuation values were achieved with the low-dose protocol compared to the conventional protocol. There was no significant difference in subjective image quality between the 2 groups.13) Hachulla et al.14) low-dose protocol consisted of 60 mL contrast compared to a conventional protocol using 120 mL contrast. All patients were examined with a 128-slice multidetector CT using automated 80-140 kV tube voltage. Although higher aortic mean attenuation was achieved with the conventional protocol, there was similar overall image quality between the 2 groups.14) Onoda et al.15) low-dose protocol consisted of a mean 31 mL contrast with 70 kV tube voltage compared to a conventional protocol with a mean 78 mL contrast with 120 or 100 kV tube voltage using a 192-slice dual-source CT. The low-dose protocol maintained adequate objective image quality.15) Ippolito et al.16) low-dose protocol consisted of 80 kV, 60 mL contrast, and iterative reconstruction compared to a conventional protocol using 100 kV, 80 mL contrast, and iDose4 reconstruction. All patients were examined with a 256-row multidetector CT. Higher mean attenuation values were achieved with the low-dose protocol and there were no significant differences in subjective image quality between the 2 groups.16) Suchá et al.17) low-dose protocol consisted of a median 69 mL contrast and 90 kV tube voltage compared to a conventional protocol with a median 116 mL contrast and 100 kV tube voltage. All patients were examined with dual-source CT. The low-dose protocol achieved good image quality. However, the conventional protocol was shown to have higher measurement reproducibility. Therefore, the authors recommended reserving low-dose protocols for patients at high risk for postcontrast acute kidney injury.17)
Table 2. Summary of study design, protocols, and outcomes for the included studies.
| Study, author, year | Sample size | Study design | Low-dose protocol | Conventional protocol | Image acquisition | Outcomes |
|---|---|---|---|---|---|---|
| Felmly et al.,13) 2017 | 40 | Prospective cohort | 3rd-gen. DSCT, 70 kV, 40 mL contrast, 2.5 mL/s flow rate, iodine: 10.8 g | 2nd-gen. DSCT, 100 kV, 60 mL contrast, 4.0 mL/s flow rate, iodine: 16.1 g | See protocols | Vascular attenuation, noise, SNR, CNR, image quality |
| Franzesi et al.,14) 2018 | 79 | Prospective cohort | 100 kV, whole-body retrospective ECG-gating, 50 mL contrast, iterative reconstruction algorithm, iodine: 350 mg/mL | 120 kV, ECG-gating for chest, 100 mL contrast, FBP reconstruction, iodine: 350 mg/mL | 256-MDCT | Image quality, vascular enhancement, radiation dose, image noise |
| Hachulla et al.,15) 2019 | 84 | Retrospective cohort | 60 mL contrast, iodine: 350 mg/mL | 120 mL contrast, iodine: 350 mg/mL | 128-slice MDCT automated 80–140 kV | Mean attenuation, image quality, SNR, CNR, CAD prediction |
| Onoda et al.,16) 2019 | 40 | Prospective cohort | 70 kV, mean 31 mL contrast, iodine: 300 mg/mL | 120/100 kV, mean 78 mL contrast, iodine: 300 mg/mL | 192-slice DSCT | Vascular attenuation, image noise, CNR, renal function |
| Ippolito et al.,17) 2020 | 60 | Randomized controlled trial | 80-kV ECG-gated, 60 mL contrast, IMR reconstruction, iodine: 350 mg/mL | 100 kV, 80 mL contrast, iDose4 reconstruction, iodine: 350 mg/mL | 256-row MDCT | Subjective and objective image quality, radiation dose |
| Suchá et al.,18) 2020 | 50 | Retrospective cohort | Median 69 mL contrast, 90 kV, iodine: 300 mg/mL | Median 116 ml contrast, 100 kV, iodine: 300 mg/ml | DSCT (Slice thickness/increment, mm: 0.75/0.7) | Image quality, pre-TAVR measurement interobserver variability, renal function change |
CNR: contrast-to-noise ratio, DSCT: dual-source CT, ECG: electrocardiogram, MDCT: multidetector CT, SNR: signal-to-noise ratio.
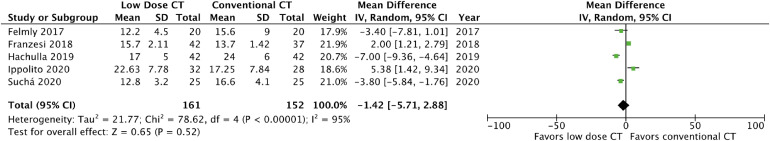
The average contrast volume (low dose 51.6 ± 14.2 mL, conventional 92.3 ± 23.6, p = 0.001) and tube voltage (low dose 82 ± 13.0 kV, conventional 108 ± 11.0 kV, p = 0.018) was decreased for the low dose protocols when compared to the conventional protocols as shown in Table 3. Pooled estimates of the included studies revealed no difference in cardiac SNR between the low dose and conventional protocols with a mean difference of −1.42 (95% CI, −5.71 to 2.88, p = 0.52). The forest plot for cardiac SNR is shown in Figure 2. There was no difference in cardiac CNR between the low dose and conventional protocols with a mean difference of −3.83 (95% CI, −9.98 to 2.32, p = 0.22). The forest plot for cardiac CNR is shown in Figure 3. The statistical heterogeneity was high for the reported cardiac SNR and CNR outcomes with I2 values of 95% and 93%, respectively. There was no difference in aortic SNR between the low dose and conventional protocols with a mean difference of −0.23 (95% CI, −7.83 to 7.37, p = 0.95). The forest plot for aortic SNR is shown in Supplementary Figure 1. There was no difference in aortic CNR between the low dose and conventional protocols with a mean difference of −3.95 (95% CI, −12.03 to 4.13, p = 0.34). The forest plot for aortic CNR is shown in Supplementary Figure 2. The statistical heterogeneity was high for the reported aortic SNR and CNR outcomes with I2 values of 95% and 93%, respectively. There was no difference in ileofemoral SNR between the low dose and conventional protocols with a mean difference of −6.09 (95% CI, −13.80 to 1.62, p = 0.12). The forest plot for ileofemoral SNR is shown in Supplementary Figure 3. There was a significant difference in ileofemoral CNR between the low dose and conventional protocols with a mean difference of −9.26 (95% CI, −15.06 to −3.46, p = 0.002). The forest plot for ileofemoral CNR is shown in Figure 4. The statistical heterogeneity was high for the reported ileofemoral SNR and CNR outcomes with I2 values of 85% and 80%, respectively.
Table 3. Average contrast volume and tube voltage for the included protocols.
| Measurement | Low-dose protocols | Conventional protocols | p-value |
|---|---|---|---|
| Average contrast volume (mL) | 51.6 ± 14.1 | 92.3 ± 23.6 | 0.001 |
| Average tube voltage (kV) | 82 ± 13.0 | 108 ± 10.9 | 0.018 |
Figure 2. Forest plot of cardiac signal-to-noise ratio in patients undergoing computed tomography angiography for transcatheter aortic valve replacement planning.
CI: confidence interval, CT: computed tomography, SD: standard deviation.
Figure 3. Forest plot of cardiac contrast-to-noise ratio in patients undergoing computed tomography angiography for transcatheter aortic valve replacement planning.
CI: confidence interval, CT: computed tomography, SD: standard deviation.
Figure 4. Forest plot of ileofemoral contrast-to-noise ratio in patients undergoing computed tomography angiography for transcatheter aortic valve replacement planning.
CI: confidence interval, CT: computed tomography, SD: standard deviation.
Qualitative image assessments were completed by the included studies as summarized in Table 4. Overall, qualitative image assessment was similar for the low dose protocols when compared to conventional protocols. Felmly et al.12) did report increased subjective image quality for aortoiliac noise for their low dose protocol when compared to the conventional protocol (low dose: 4.42 [IQR, 4.0–5.0], conventional 4.12 [IQR, 4.0–5.0], p = 0.037).
Table 4. Summary of qualitative image assessment for the included studies.
| Study | Parameter | Low-dose protocol | Conventional protocol | p-value |
|---|---|---|---|---|
| Felmly et al.,13) 2017 | Cardiac attenuation | 4.71 (IQR 5.0–5.0) | 4.67 (IQR 4.0–5.0) | 0.720 |
| Image noise | 4.08 (IQR 4.0–4.0) | 3.88 (IQR 4.0–4.0) | 0.238 | |
| Aortoiliac attenuation | 4.53 (IQR 4.0–5.0) | 4.33 (IQR 4.0–5.0) | 0.213 | |
| Aortoiliac noise | 4.42 (IQR 4.0–5.0) | 4.12 (IQR 4.0–5.0) | 0.037 | |
| Franzesi et al.,14) 2018 | Image quality, reader 1 | 3.48 ± 0.71 | 3.45 ± 0.67 | 0.378 |
| Image quality, reader 2 | 3.45 ± 0.67 | 3.41 ± 0.62 | 0.621 | |
| Hachulla et al.,15) 2019 | Global quality, excellent | 38/42 | 37/42 | NR |
| Global quality, moderate | 4/42 | 5/42 | NR | |
| Ippolito et al.,17) 2020 | Image quality, reader 1 | 3.44 ± 0.73 | 3.48 ± 0.71 | 0.840 |
| Image quality, reader 2 | 3.50 ± 0.53 | 3.45 ± 0.67 | 0.562 | |
| Suchá et al.,18) 2020 | Annular image quality | 3.0 (range 2–4) | 3.5 (range 2–4) | NR |
| Iliofemoral image quality | 3.5 (range 2–4) | 4.0 (range 2.5–4) | NR |
IQR: interquartile range, NR: not reported.
DISCUSSION
This systematic review suggests adequate image quality for low contrast and low kV CTA compared to conventional CTA for TAVR planning. Our findings are derived from 6 studies reporting on image quality in 353 patients with aortic stenosis undergoing CTA for TAVR planning. There was no difference in image quality as assessed by cardiac, aortic, and ileofemoral SNR and cardiac and aortic CNR between imaging protocols for this patient population. There was decreased ileofemoral CNR for the low dose protocols when compared to the conventional protocols. This is likely from improved CNR with higher contrast and kV amounts used in the conventional protocols at this specific anatomic location. Interestingly, Ippolito et al.16) were able to achieve significantly higher SNR and CNR with their low dose protocol combined with a model-based iterative reconstruction algorithm, specifically IMR.16) Overall subjective image quality was similar with high quality scores for both protocols. Image quality was acceptable for TAVR planning using the low dose protocols in all of the included studies.
These findings are consistent with additional studies that achieved adequate image quality using intra-arterial catheters to deliver low contrast volumes compared to conventional CTA for TAVR planning.18),19) Recently developed CT technology using virtual monoenergetic images at lower kV levels has been shown to result in better image quality at lower doses of contrast material.20),21) This is feasible since the K-edge of iodine at 33.3 kV is closer to lower x-ray energy spectra, therefore increased soft tissue contrast can be obtained at decreased keV levels.22),23) Cavallo et al.24) described a method of using 40 keV reconstruction with low contrast volume compared to conventional 120 kV images with the same contrast volume in patients undergoing TAVR planning. The 40 keV method with low dose contrast achieved better image quality as assessed by SNR and CNR. Mangold et al. developed another 40 keV virtual monoenergetic image reconstruction technique that obtained higher image quality when compared to a conventional protocol for TAVR planning.25) Several studies have also demonstrated the feasibility of low radiation and low contrast CTA for TAVR planning, although comparisons to conventional imaging were not made.26),27),28) These findings also support a recent expert consensus document that recommends optimizing scanning protocols to achieve lower overall contrast volumes.29)
This systematic review provides important insights on using a low contrast and low kV CTA strategy for patients undergoing TAVR planning that may inform decisions in clinical practice. Using low radiation through low-tube-voltage techniques maintains image quality at lower contrast volumes. Minimizing contrast volume can help make TAVR available to patients with renal dysfunction who would otherwise not be candidates since there is a dose-dependent association with contrast-induced nephropathy.30) As TAVR expands to younger patient populations, the reduced radiation dose used by this imaging strategy may also become a more relevant clinical benefit.
The limitations of this systematic review are influenced by the limitations of the included studies. The included studies had small sample sizes likely due to the complexity of image quality research for this patient population. One major limitation is the variability in the low dose and conventional protocols between studies. Various contrast amounts, tube voltages, and image acquisition techniques were used and severely limits the generalizability of the aggregate data. Variations in clinical settings, population characteristics, and imaging protocols are potential sources of heterogeneity. We used a random effects model to account for these variations. CIs for estimates were wide in spite of pooling likely due to high heterogeneity and low sample sizes.
In conclusion, this systematic review suggests that low contrast and low kV CTA for TAVR planning provides similar image quality to conventional CTA.
Footnotes
Conflict of Interest: The authors have no financial conflicts of interest.
- Conceptualization: Lacy S, Benjamin M, Syed M, Kinno M.
- Data curation: Lacy S.
- Formal analysis: Lacy S.
- Investigation: Lacy S.
- Methodology: Lacy S.
- Software: Lacy S.
- Supervision: Benjamin M, Syed M, Kinno M.
- Writing - original draft: Lacy S, Benjamin M.
- Writing - review & editing: Benjamin M, Osman M, Syed M, Kinno M.
SUPPLEMENTARY MATERIALS
Forest plot of aortic signal-to-noise ratio in patients undergoing computed tomography angiography for transcatheter aortic valve replacement planning.
Forest plot of aortic contrast-to-noise ratio in patients undergoing computed tomography angiography for transcatheter aortic valve replacement planning.
Forest plot of ileofemoral signal-to-noise ratio in patients undergoing computed tomography angiography for transcatheter aortic valve replacement planning.
References
- 1.Slomski A. TAVR vs surgery in low-risk patients. JAMA. 2019;321:1965. doi: 10.1001/jama.2019.5992. [DOI] [PubMed] [Google Scholar]
- 2.Achenbach S, Delgado V, Hausleiter J, Schoenhagen P, Min JK, Leipsic JA. SCCT expert consensus document on computed tomography imaging before transcatheter aortic valve implantation (TAVI)/transcatheter aortic valve replacement (TAVR) J Cardiovasc Comput Tomogr. 2012;6:366–380. doi: 10.1016/j.jcct.2012.11.002. [DOI] [PubMed] [Google Scholar]
- 3.Holmes DR, Jr, Mack MJ, Kaul S, et al. 2012 ACCF/AATS/SCAI/STS expert consensus document on transcatheter aortic valve replacement. J Am Coll Cardiol. 2012;59:1200–1254. doi: 10.1016/j.jacc.2012.01.001. [DOI] [PubMed] [Google Scholar]
- 4.Faggiano P, Frattini S, Zilioli V, et al. Prevalence of comorbidities and associated cardiac diseases in patients with valve aortic stenosis. Potential implications for the decision-making process. Int J Cardiol. 2012;159:94–99. doi: 10.1016/j.ijcard.2011.02.026. [DOI] [PubMed] [Google Scholar]
- 5.Bagur R, Webb JG, Nietlispach F, et al. Acute kidney injury following transcatheter aortic valve implantation: predictive factors, prognostic value, and comparison with surgical aortic valve replacement. Eur Heart J. 2010;31:865–874. doi: 10.1093/eurheartj/ehp552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Azzalini L, Abbara S, Ghoshhajra BB. Ultra-low contrast computed tomographic angiography (CTA) with 20-mL total dose for transcatheter aortic valve implantation (TAVI) planning. J Comput Assist Tomogr. 2014;38:105–109. doi: 10.1097/RCT.0b013e3182a14358. [DOI] [PubMed] [Google Scholar]
- 7.Meyer M, Haubenreisser H, Schoepf UJ, et al. Closing in on the K edge: coronary CT angiography at 100, 80, and 70 kV-initial comparison of a second- versus a third-generation dual-source CT system. Radiology. 2014;273:373–382. doi: 10.1148/radiol.14140244. [DOI] [PubMed] [Google Scholar]
- 8.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343(oct18 2):d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. doi: 10.1136/bmj.i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 12.Felmly LM, De Cecco CN, Schoepf UJ, et al. Low contrast medium-volume third-generation dual-source computed tomography angiography for transcatheter aortic valve replacement planning. Eur Radiol. 2017;27:1944–1953. doi: 10.1007/s00330-016-4537-6. [DOI] [PubMed] [Google Scholar]
- 13.Talei Franzesi CR, Ippolito D, Riva L, Fior D, Cangiotti C, Sironi S. Diagnostic value of iterative reconstruction algorithm in low kV CT angiography (CTA) with low contrast medium volume for transcatheter aortic valve implantation (TAVI) planning: image quality and radiation dose exposure. Br J Radiol. 2018;91:20170802. doi: 10.1259/bjr.20170802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hachulla AL, Noble S, Ronot M, et al. Low iodine contrast injection for CT acquisition prior to transcatheter aortic valve replacement: aorta assessment and screening for coronary artery disease. Acad Radiol. 2019;26:e150–e160. doi: 10.1016/j.acra.2018.06.016. [DOI] [PubMed] [Google Scholar]
- 15.Onoda H, Ueno H, Hashimoto M, Kuwahara H, Sobajima M, Kinugawa K. Clinical advantages of using low tube voltage in third-generation 192-slice dual-source computed tomographic angiography before transcatheter aortic valve implantation. Int Heart J. 2019;60:1091–1097. doi: 10.1536/ihj.18-693. [DOI] [PubMed] [Google Scholar]
- 16.Ippolito D, Riva L, Talei Franzesi C, et al. Computed tomography angiography combined with knowledge-based iterative algorithm for transcatheter aortic valve implantation planning: image quality and radiation dose exposure with low-kV and low-contrast-medium protocol. J Comput Assist Tomogr. 2020;44:13–19. doi: 10.1097/RCT.0000000000000965. [DOI] [PubMed] [Google Scholar]
- 17.Suchá D, Kino A, Bogart K, et al. Effect of low contrast medium-dose CTA on device sizing and access vessel assessment for TAVR. Eur J Radiol. 2020;124:108826. doi: 10.1016/j.ejrad.2020.108826. [DOI] [PubMed] [Google Scholar]
- 18.Zemedkun M, LaBounty TM, Bergman G, et al. Effectiveness of a low contrast load CT angiography protocol in octogenarians and nonagenarians being evaluated for transcatheter aortic valve replacement. Clin Imaging. 2015;39:815–819. doi: 10.1016/j.clinimag.2014.08.010. [DOI] [PubMed] [Google Scholar]
- 19.Truong VT, Choo J, McCoy L, et al. Low-volume contrast CT angiography via pulmonary artery injection for measurement of aortic annulus in patients undergoing transcatheter aortic valve replacement. J Invasive Cardiol. 2017;29:181–186. [PubMed] [Google Scholar]
- 20.McCollough CH, Leng S, Yu L, Fletcher JG. Dual- and multi-energy CT: principles, technical approaches, and clinical applications. Radiology. 2015;276:637–653. doi: 10.1148/radiol.2015142631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Patino M, Prochowski A, Agrawal MD, et al. Material separation using dual-energy CT: current and emerging applications. Radiographics. 2016;36:1087–1105. doi: 10.1148/rg.2016150220. [DOI] [PubMed] [Google Scholar]
- 22.Zopfs D, Lennartz S, Laukamp K, et al. Improved depiction of atherosclerotic carotid artery stenosis in virtual monoenergetic reconstructions of venous phase dual-layer computed tomography in comparison to polyenergetic reconstructions. Eur J Radiol. 2018;100:36–42. doi: 10.1016/j.ejrad.2018.01.008. [DOI] [PubMed] [Google Scholar]
- 23.Vlahos I, Godoy MC, Naidich DP. Dual-energy computed tomography imaging of the aorta. J Thorac Imaging. 2010;25:289–300. doi: 10.1097/RTI.0b013e3181dc2b4c. [DOI] [PubMed] [Google Scholar]
- 24.Cavallo AU, Patterson AJ, Thomas R, et al. Low dose contrast CT for transcatheter aortic valve replacement assessment: results from the prospective SPECTACULAR study (spectral CT assessment prior to TAVR) J Cardiovasc Comput Tomogr. 2020;14:68–74. doi: 10.1016/j.jcct.2019.06.015. [DOI] [PubMed] [Google Scholar]
- 25.Mangold D, Salatzki J, Riffel J, Kauczor HU, Weber TF. Dual-layer spectral CTA for TAVI planning using a split-phase protocol and low-keV virtual monoenergetic images: improved image quality in comparison with single-phase conventional CTA. RoFo Fortschr Geb Rontgenstr Nuklearmed. 2021;2021 doi: 10.1055/a-1717-2542. E-pub ahead of print. [DOI] [PubMed] [Google Scholar]
- 26.Bittner DO, Arnold M, Klinghammer L, et al. Contrast volume reduction using third generation dual source computed tomography for the evaluation of patients prior to transcatheter aortic valve implantation. Eur Radiol. 2016;26:4497–4504. doi: 10.1007/s00330-016-4320-8. [DOI] [PubMed] [Google Scholar]
- 27.Kok M, Turek J, Mihl C, et al. Low contrast media volume in pre-TAVI CT examinations. Eur Radiol. 2016;26:2426–2435. doi: 10.1007/s00330-015-4080-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dankerl P, Hammon M, Seuss H, et al. Computer-aided evaluation of low-dose and low-contrast agent third-generation dual-source CT angiography prior to transcatheter aortic valve implantation (TAVI) Int J CARS. 2017;12:795–802. doi: 10.1007/s11548-016-1470-8. [DOI] [PubMed] [Google Scholar]
- 29.Blanke P, Weir-McCall JR, Achenbach S, et al. Computed tomography imaging in the context of transcatheter aortic valve implantation (TAVI)/transcatheter aortic valve replacement (TAVR): an expert consensus document of the society of cardiovascular computed tomography. JACC Cardiovasc Imaging. 2019;12:1–24. doi: 10.1016/j.jcmg.2018.12.003. [DOI] [PubMed] [Google Scholar]
- 30.Toprak O. Conflicting and new risk factors for contrast induced nephropathy. J Urol. 2007;178:2277–2283. doi: 10.1016/j.juro.2007.08.054. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Forest plot of aortic signal-to-noise ratio in patients undergoing computed tomography angiography for transcatheter aortic valve replacement planning.
Forest plot of aortic contrast-to-noise ratio in patients undergoing computed tomography angiography for transcatheter aortic valve replacement planning.
Forest plot of ileofemoral signal-to-noise ratio in patients undergoing computed tomography angiography for transcatheter aortic valve replacement planning.