Abstract
Purpose
To investigate the association of meal timing with body composition and cardiometabolic risk factors in young adults.
Methods
In this cross-sectional study participated 118 young adults (82 women; 22 ± 2 years old; BMI: 25.1 ± 4.6 kg/m2). Meal timing was determined via three non-consecutive 24-h dietary recalls. Sleep outcomes were objectively assessed using accelerometry. The eating window (time between first and last caloric intake), caloric midpoint (local time at which ≥ 50% of daily calories are consumed), eating jetlag (variability of the eating midpoint between non-working and working days), time from the midsleep point to first food intake, and time from last food intake to midsleep point were calculated. Body composition was determined by DXA. Blood pressure and fasting cardiometabolic risk factors (i.e., triglycerides, total cholesterol, high-density lipoprotein-cholesterol, low-density lipoprotein-cholesterol, and insulin resistance) were measured.
Results
Meal timing was not associated with body composition (p > 0.05). The eating window was negatively related to HOMA-IR and cardiometabolic risk score in men (R2 = 0.348, β = − 0.605; R2 = 0.234, β = − 0.508; all p ≤ 0.003). The time from midsleep point to first food intake was positively related to HOMA-IR and cardiometabolic risk score in men (R2 = 0.212, β = 0.485; R2 = 0.228, β = 0.502; all p = 0.003). These associations remained after adjusting for confounders and multiplicity (all p ≤ 0.011).
Conclusions
Meal timing seems unrelated to body composition in young adults. However, a longer daily eating window and a shorter time from midsleep point to first food intake (i.e., earlier first food intake in a 24 h cycle) are associated with better cardiometabolic health in young men.
Clinical trial registration
NCT02365129 (https://www.clinicaltrials.gov/ct2/show/NCT02365129?term=ACTIBATE&draw=2&rank=1).
Supplementary Information
The online version contains supplementary material available at 10.1007/s00394-023-03141-9.
Keywords: Chrononutrition, Circadian rhythms, Timing of food intake, Intermittent fasting, Fat mass, Insulin resistance
Introduction
The obesity epidemic is one of the leading contributors to the global burden of cardiometabolic diseases and disability, resulting in a significant economic impact on health care systems [1, 2]. However, despite the known consequences of excess body weight, the prevalence of obesity continues to rise, and currently there are more than 1.9 billion adults with overweight or obesity worldwide [1]. Body weight regulation and obesity are highly influenced by several factors such as genetics, physiology, and socioeconomic factors [3]. For instance, in recent years, emerging evidence has shown that the timing of food intake may be a relevant risk factor for obesity and cardiometabolic diseases [4, 5].
The importance of when we eat is tied to our circadian system, which temporally orchestrates numerous metabolic processes across the body over a 24 h period [6, 7]. The circadian system is constituted by a central clock located in the suprachiasmatic nuclei of the hypothalamus and a series of peripheral clocks placed in virtually all cells and tissues of the body [6, 7]. The central clock is primarily controlled by external light via direct connection to the retina, whereas peripheral clocks are regulated by the central clock and external time cues, such as eating, physical activity and sleep among other behavioural tasks [6, 7]. Since different stimuli impact the central and peripheral clocks, the two clock systems become misaligned whenever their respective time cues are out of synchrony [6, 7]. The modern lifestyle promotes this circadian misalignment by allowing exposure to artificial light at night and by allowing access to food all day long [6–8].
Epidemiological data have shown that eating late in the day is associated with greater energy intake, adiposity and worst cardiometabolic health [9–16]. Furthermore, considerable variability in meal timing between non-working days and working days, coined eating jet lag, has been linked to higher body mass index (BMI) [17]. Clinical trials have also revealed that reducing the daily eating window (i.e., the period of time between the first and the last caloric intake) and/or shifting dietary energy intake earlier in the day results in body weight loss or optimized cardiometabolic health in adults with overweight or obesity [9, 18–22]. Nonetheless, one of the main limitations of meal timing studies is the use of clock time to illustrate the timing of food intake, which fails to correctly characterize meal timing in relation to the internal circadian time [10, 23]. Because obtaining measures of dim-light melatonin is not practical in large clinical trials, it has been proposed that the timing of food intake should be assessed in relation to the sleep/wake cycle as a proxy of circadian time [10, 23, 24]. Only a few studies have followed this methodology, indicating that a longer time period from dinner to midsleep point or bedtime is associated with lower adiposity and BMI, respectively [10, 23]. However, these studies also present important limitations, such as the self-reported assessment of sleep timing, solely including anthropometric variables or fat mass measured by non-state-of-the-art methods and the absence of various cardiometabolic risk. Moreover, although sex is known to influence several aspects of biology, physiology and psychology previous studies have not investigated if there are sex differences in the relationship between meal timing with body composition and cardiometabolic risk factors.
Our study was aimed at elucidating the association of meal timing [i.e., eating window, caloric midpoint (the time at which ≥ 50% of daily calories are consumed), eating jet lag, time from midsleep point to first food intake, and time from last food intake to midsleep point] with anthropometry [i.e., body weight, BMI and waist circumference], body composition [i.e., fat mass, lean mass, and visceral adipose tissue (VAT) mass] and cardiometabolic risk factors [i.e., blood pressure, triglycerides, total cholesterol, high-density lipoprotein-cholesterol (HDL-C), low-density lipoprotein-cholesterol (LDL-C), insulin resistance] in young adults. Special attention was paid to the influence of sex on these associations. We hypothesized that a shorter daily eating window, earlier food intake schedule and less variability in meal timing between non-working days and working days would be associated with healthier body composition and cardiometabolic risk factors.
Materials/subjects and methods
Participants
A total of 118 young adults (n = 82 women; see Flow Chart, Figure S1) took part in this cross-sectional study which includes the baseline measurements of the ACTIBATE study (ClinicalTrials.gov NCT02365129) [25] and follows the STROBE-nut guidelines (Table S1) [26]. All assessments were performed in Granada (Spain) during September-December in 2015 and 2016. The inclusion/exclusion criteria included the following: (i) being 18–25 years, (ii) having a BMI ranging from 18 to 35 kg/m2, (iii) being non-smokers, (iv) not being enrolled in a weight loss program, (iii) having a stable body weight (body weight changes < 3 kg over 3 months), (iv) not being physically active (< 20 min on < 3 days/week), (v) not taking any medication or drugs, and (vi) not suffering from any acute or chronic illness.
Outcome measurements
Anthropometry and body composition
Body weight and height were determined with participants wearing light clothing and without shoes using a SECA scale and stadiometer (model 799; Electronic Column Scale, Seca GmbH, Hamburg, Germany). The BMI was calculated as weight (kilograms) divided by height squared (square meters). Waist circumference (centimetres) was assessed midway between the lowest rib and the top of the iliac crest. Alternatively, when participants showed abdominal obesity, waist circumference was determined in a horizontal plane above the umbilicus after exhalation.
Body composition was measured by dual-energy X-ray absorptiometry (DiscoveryWi; Hologic, Inc., Marlborough, MA, USA) strictly following the manufacturer’s instructions, obtaining fat mass, lean mass, and VAT mass. The lean mass index was calculated as lean mass (kilograms) divided by height squared (square meters).
Cardiometabolic profile
The systolic and diastolic blood pressure were measured on three different days with an automatic monitor (Omron Healthcare Europe B.V. Hoofddorp, The Netherlands), and the average was used in later analyses. We calculated the mean blood pressure as diastolic blood pressure + 1/3(systolic blood pressure − diastolic blood pressure). Blood samples were collected from the antecubital area in the morning after fasting for > 10 h. All samples were centrifuged, and aliquots of serum were stored at − 80 °C until analysis. All participants were requested to abstain from drugs and caffeine and to avoid moderate-intensity physical activity and vigorous-intensity activity for 24 and 48 h before testing, respectively. Serum glucose, total cholesterol, HDL-C and triglycerides were assessed following standard methods using an AU5832 automated analyzer (Beckman Coulter Inc., Brea CA, USA). LDL-C was then estimated [27]. Serum insulin was measured using the Access Ultrasensitive Insulin Chemiluminescent Immunoassay Kit (Beckman Coulter Inc., Brea, CA, USA). The homeostasis model assessment of insulin resistance (HOMA-IR) was calculated.
Cardiometabolic risk scores were calculated for each sex based on variables included in the diagnosis of Metabolic Syndrome [28]: waist circumference, blood pressure, plasma glucose, HDL-C, and triglyceride concentrations. A Z-score was calculated for each variable. The HDL-C standardized values were multiplied by − 1 to be directly proportional to the cardiometabolic risk. The final score was determined as the average of the 5 Z-scores. Thus, the cardiometabolic risk score is a continuous variable with a mean of 0 and a standard deviation of 1; higher scores indicating higher risk.
Sleep parameters, sedentary time and physical activity assessment
Participants were instructed to wear a triaxial accelerometer (ActiGraph GT3X+, Pensacola, FL, USA) on the non-dominant wrist 24 h a day for seven consecutive days, removing them only when swimming or bathing, and to record information on sleep onset and wakeup times each day in a sleep diary. The midsleep point and other sleep-related outcomes were objectively assessed using an algorithm guided by the participants' reported times. The raw data were processed in R [version 3.1.2, https://www.R-project.org/] using the GGIR package [version 1.5-12, https://cran.r-project.org/web/packages/GGIR/]. Actigraphy recordings were used to determine: (i) sleep onset (time at which the subject fell asleep); (ii) sleep offset (time at which the subject woke up); and (iii) sleep duration (time between falling asleep and waking up). Daytime naps were not considered. Those participants registering less than 16 h/day of wear time for more than 4 days and/or not having data from at least one weekend day were excluded from the final analysis. We used these sleep variables to calculate the midsleep point (the middle time point between sleep onset and sleep offset) as follows: midsleep point (local time) = (sleep duration/2) + sleep onset [24]. We determined the midsleep point for non-working days and working days separately. Subsequently, the midsleep point for the week was calculated as a weighted mean, which was used in later analyses. Last, we computed social jetlag (a proxy of the discrepancy between social and biological time) by subtracting each participant’s midsleep point for working days from non-working days [24].
We estimated the time spent in sedentary behavior and different physical activity intensities (i.e., light, moderate, vigorous, and moderate to vigorous) using age-specific cut points [29].
Dietary assessment and meal timing
Dietary intake and meal timing were recorded using three non-consecutive 24 h dietary recalls (one of them for a non-working day) distributed over three weeks with the participants unaware of when their diets were going to be recorded. In face-to-face interviews performed by trained dietitians, participants were asked to recall all food consumed on the previous day, using photographs of portion sizes [30], as well as the time of the meal event. Data recorded in the interviews were independently introduced by two dieticians in the EvalFINUT® software When the coefficient of variance between the two datasets was > 5%, a third dietician reintroduced the data obtained from the 24-h recalls in the EvalFINUT® software and the mean of the two datasets with the best agreement (i.e., lower coefficient of variance) was used. From these data, we calculated the following meal timing variables:
The eating window (i.e., the period of time between the first and the last caloric intake) was calculated for each day [31]. The caloric midpoint is defined as the time at which ≥ 50% of daily calories are consumed and is expressed in local time [12]. We determined the eating window and the caloric midpoint for non-working days and working days. Subsequently, the value for the week was calculated as a weighted mean, which was used in later analyses. Eating jetlag (i.e., the variability of the eating midpoint between non-working days and working days) was determined as [24]: eating midpoint for non-working days − eating midpoint for working days. The time from the midsleep point to first food intake and the time from last food intake to the midsleep point were also calculated.
Dietary patterns and quality were determined by analysing the participants' data from the 24 h recalls and a validated food frequency questionnaire [32]. Three The following Mediterranean dietary patterns [33–35] were computed: the a priori Mediterranean dietary pattern [33], the Mediterranean diet score, and the dietary quality index for a Mediterranean diet [34, 35]. Adherence to the Dietary Approaches to Stop Hypertension guidelines was also calculated. The diet quality index [36] and the dietary inflammatory index [37], were also determined. Breakfast consumers were defined as consuming breakfast in all of the three non-consecutive 24 h dietary recalls, whereas breakfast skippers were defined as not consuming breakfast on at least one of the three non-consecutive 24 h dietary recalls.
Statistical analyses
The distribution of the variables was verified using the Shapiro–Wilk test, skewness and kurtosis values, visual checking of histograms, and Q–Q and box plots. The descriptive parameters are reported as mean and standard deviation when normally distributed, or medians (interquartile range) when a Gaussian distribution was not found. Triglycerides, total cholesterol, HDL-C, LDL-C, and HOMA-IR were log10-transformed to bring their distributions closer to normal and used in subsequent analyses. A one-way analysis of variance was used to compare baseline characteristics between men and women. We conducted simple linear regression models to examine the association of meal timing (i.e., eating window, caloric midpoint, eating jetlag, time from midsleep point to first food intake, and time from last food intake to midsleep point) with anthropometry (i.e., weight, BMI and waist circumference), body composition (i.e., fat mass percentage, lean mass index, and VAT mass) and cardiometabolic risk factors (i.e., mean blood pressure, triglycerides, total cholesterol, HDL-C, LDL-C, HOMA-IR, and cardiometabolic risk score). We also conducted multiple linear regression models to examine these associations adjusting for potential confounders (i.e., sex, a priori Mediterranean diet pattern, light physical activity, midsleep point or sleep duration, and BMI). Differences between breakfast skippers and consumers in anthropometry, body composition, cardiometabolic risk factors and potential confounders were determined by the Welch's t test. Some statistical differences were observed; therefore, additional analyses were performed. Concretely, the simple linear regression models were repeated to examine the association of meal timing with anthropometry, body composition and cardiometabolic risk factors only in breakfast consumers.
The main analyses were corrected for multiple comparison errors (familywise error rate [Hochberg procedure]) [38]. The Statistical Package for the Social Sciences (SPSS) v.25.0 (IBM Corporation, Chicago, IL, USA) was used for all analyses. GraphPad Prism 8 (GraphPad Software, San Diego, CA, USA) was used for plots. Significance was set at p < 0.05.
Results
Table 1 shows the main characteristics of the study participants.
Table 1.
Descriptive characteristics of participants
| All | Men | Women | ||||
|---|---|---|---|---|---|---|
| Age (years) | 118 | 22.2 (2.2) | 36 | 22.5 (2.3) | 82 | 22.1 (2.1) |
| Height (cm) | 116 | 168.0 (8.5)* | 34 | 176.3 (6.4) | 82 | 164.5 (6.7) |
| Weight (kg) | 116 | 71.2 (16.8)* | 34 | 85.5 (18.5) | 82 | 65.2 (11.7) |
| Body composition | ||||||
| Body mass index (kg/m2) | 116 | 25.1 (4.6)* | 34 | 27.4 (5.4) | 82 | 24.1 (3.9) |
| Fat mass (kg) | 116 | 25.6 (9.0) | 34 | 27.0 (11.6) | 82 | 25.0 (7.6) |
| Fat mass (%) | 116 | 36.4 (7.3)* | 34 | 31.1 (7.7) | 82 | 38.6 (5.9) |
| Lean mass (kg) | 116 | 41.6 (9.8)* | 34 | 53.7 (7.5) | 82 | 36.6 (5.0) |
| Lean mass index (kg/m2) | 116 | 14.6 (2.4)* | 34 | 17.3 (2.2) | 82 | 13.5 (1.4) |
| Visceral adipose tissue mass (g) | 116 | 346.0 (187.3)* | 34 | 446.7 (188.7) | 82 | 304.3 (171.2) |
| Waist circumference (cm) | 114 | 80.8 (14.5)* | 34 | 91.4 (16.4) | 80 | 76.3 (10.9) |
| Cardiometabolic risk factors | ||||||
| Systolic blood pressure (mmHg) | 116 | 116.2 (12.4)* | 36 | 126.0 (12.5) | 80 | 111.8 (9.6) |
| Diastolic blood pressure (mmHg) | 116 | 70.7 (7.9)* | 36 | 73.0 (10.1) | 80 | 69.7 (6.6) |
| Mean blood pressure (mmHg) | 116 | 85.9 (8.1)* | 36 | 90.7 (8.8) | 80 | 83.7 (6.7) |
| Triglycerides (mg/dl) | 117 | 70.0 (52.5, 97.5) | 36 | 74.0 (57.8, 105.8) | 81 | 68.0 (52.0, 89.5) |
| Total cholesterol (mg/dl) | 117 | 158.0 (143.0, 179.0) | 36 | 153.0 (140.0, 174.8) | 81 | 164.0 (143.0, 183.5) |
| High-density lipoprotein cholesterol (mg/dl) | 117 | 51.0 (45.5, 58.0)* | 36 | 46.5 (39.3, 51.0) | 81 | 53.0 (47.5, 63.0) |
| Low-density lipoprotein cholesterol (mg/dl) | 117 | 92.0 (78.5, 109.0) | 36 | 91.0 (81.3, 108.8) | 81 | 92.0 (75.5, 109.0) |
| Glucose (mg/dl) | 117 | 87.0 (83.0, 92.0)* | 36 | 89.5 (82.3, 97.0) | 81 | 86.0 (83.0, 90.0) |
| Insulin (μIU/ml) | 117 | 7.2 (5.5, 10.1) | 36 | 7.3 (5.2, 11.4) | 81 | 7.1 (5.5, 9.8) |
| HOMA-IR | 117 | 1.5 (1.1, 2.2)* | 36 | 1.6 (1.2, 2.5) | 81 | 1.5 (1.1, 2.1) |
| Chronobiology | ||||||
| Sleep onset (hh:mm)a | 113 | 01:13 (01:13) | 34 | 01:15 (01:20) | 79 | 01:12 (01:10) |
| Sleep offset (hh:mm)a | 113 | 08:52 (01:02) | 34 | 09:00 (01:12) | 79 | 08:48 (00:57) |
| Sleep duration (h)b | 113 | 7.85 (1.2) | 34 | 7.98 (1.25) | 79 | 7.8 (1.17)) |
| Midsleep point (hh:mm)a | 113 | 05:04 (01:05) | 34 | 05:10 (01:15) | 79 | 05:02 (01:00) |
| Social jetlag (h)b | 113 | 1.42 (1.23) | 34 | 1.40 (1.10) | 79 | 1.42 (1.30) |
| Meal timing | ||||||
| Eating window (h)b | 117 | 12.10 (1.5) | 36 | 12.00 (1.70) | 81 | 12.20 (1.40) |
| Caloric midpoint (hh:mm)a | 117 | 15:54 (01:36) | 36 | 15:48 (01:36) | 81 | 15:54 (01:42) |
| Eating jetlag (h)b | 117 | 1.20 (1.10) | 36 | 1.20 (1.33) | 81 | 1.20 (1.00) |
| Time from midsleep point to first food intake (h)b | 113 | 4.87 (1.40) | 34 | 4.87 (1.72) | 79 | 4.87 (1.23) |
| Time from last food intake to midsleep point (h)b | 113 | 7.05 (1.08) | 34 | 7.22 (1.23) | 79 | 6.97 (1.02) |
Data are presented as sample size, mean (standard deviation) when normally distributed, or medians (interquartile range) when not
HOMA-IR homeostasis model assessment of insulin resistance
*p ≤ 0.05 for sex comparisons by a one-way analysis of variance (all cardiometabolic risk factors except for blood pressure variables were log10-transformed to bring their distributions closer to normal)
aTime shown in local time
bTime shown in decimal format
Meal timing and anthropometry/body composition
The caloric midpoint was negatively associated with fat mass percentage in men (R2 = 0.089, β = − 0.342, p = 0.048; Table 2), but became non-significant after adjusting for multiplicity (p > 0.05). No further associations were found between meal timing and anthropometry/body composition (all p ≥ 0.068; Table 2).
Table 2.
Association of meal timing with body composition in young adults
| Body composition | All | Men | Women | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | R2 | β | p value | N | R2 | β | p value | N | R2 | β | p value | |
| Body mass index (kg/m2) | ||||||||||||
| Eating window (h) | 116 | − 0.004 | − 0.070 | 0.452 | 34 | 0.030 | − 0.243 | 0.166 | 82 | − 0.005 | 0.088 | 0.433 |
| Caloric midpoint (h) | 116 | − 0.008 | 0.029 | 0.759 | 34 | − 0.009 | − 0.146 | 0.410 | 82 | 0.008 | 0.143 | 0.201 |
| Eating jetlag (h) | 116 | − 0.009 | − 0.007 | 0.945 | 34 | − 0.026 | − 0.073 | 0.681 | 82 | − 0.012 | 0.012 | 0.917 |
| Time from midsleep point to first food intake (h) | 113 | − 0.001 | 0.091 | 0.339 | 34 | 0.030 | 0.243 | 0.166 | 79 | − 0.012 | − 0.024 | 0.833 |
| Time from last food intake to midsleep point (h) | 113 | − 0.008 | − 0.032 | 0.737 | 34 | − 0.031 | − 0.010 | 0.956 | 79 | − 0.001 | − 0.110 | 0.334 |
| Fat mass (%) | ||||||||||||
| Eating window (h) | 116 | − 0.009 | 0.003 | 0.979 | 34 | − 0.015 | − 0.125 | 0.482 | 82 | − 0.012 | 0.016 | 0.886 |
| Caloric midpoint (h) | 116 | − 0.007 | − 0.037 | 0.691 | 34 | 0.089 | − 0.342 | 0.048 | 82 | − 0.006 | 0.083 | 0.460 |
| Eating jetlag (h) | 116 | − 0.006 | − 0.054 | 0.563 | 34 | − 0.031 | − 0.013 | 0.943 | 82 | − 0.009 | − 0.055 | 0.625 |
| Time from midsleep point to first food intake (h) | 113 | − 0.006 | 0.053 | 0.578 | 34 | − 0.013 | 0.131 | 0.459 | 79 | − 0.013 | 0.005 | 0.968 |
| Time from last food intake to midsleep point (h) | 113 | − 0.002 | − 0.082 | 0.390 | 34 | − 0.031 | − 0.014 | 0.938 | 79 | − 0.010 | − 0.054 | 0.634 |
| Lean mass index (kg/m2) | ||||||||||||
| Eating window (h) | 116 | 0.001 | − 0.099 | 0.289 | 34 | 0.072 | − 0.316 | 0.068 | 82 | 0.004 | 0.128 | 0.250 |
| Caloric midpoint (h) | 116 | − 0.007 | 0.041 | 0.659 | 34 | − 0.031 | 0.022 | 0.901 | 82 | 0.006 | 0.135 | 0.228 |
| Eating jetlag (h) | 116 | − 0.008 | 0.027 | 0.776 | 34 | − 0.023 | − 0.087 | 0.625 | 82 | − 0.010 | 0.052 | 0.642 |
| Time from midsleep point to first food intake (h) | 113 | − 0.003 | 0.074 | 0.434 | 34 | 0.054 | 0.287 | 0.100 | 79 | − 0.010 | − 0.052 | 0.651 |
| Time from last food intake to midsleep point (h) | 113 | − 0.008 | 0.034 | 0.724 | 34 | − 0.030 | 0.029 | 0.873 | 79 | 0.002 | − 0.120 | 0.292 |
| Visceral adipose tissue mass (g) | ||||||||||||
| Eating window (h) | 116 | 0.004 | − 0.111 | 0.236 | 34 | 0.037 | − 0.257 | 0.142 | 82 | − 0.012 | 0.002 | 0.989 |
| Caloric midpoint (h) | 116 | − 0.008 | 0.027 | 0.771 | 34 | − 0.014 | − 0.130 | 0.464 | 82 | 0.000 | 0.112 | 0.315 |
| Eating jetlag (h) | 116 | − 0.006 | − 0.049 | 0.600 | 34 | − 0.030 | − 0.034 | 0.848 | 82 | − 0.005 | − 0.087 | 0.440 |
| Time from midsleep point to first food intake (h) | 113 | 0.002 | 0.107 | 0.261 | 34 | 0.051 | 0.282 | 0.106 | 79 | − 0.013 | 0.006 | 0.960 |
| Time from last food intake to midsleep point (h) | 113 | − 0.009 | 0.002 | 0.982 | 34 | − 0.029 | − 0.046 | 0.798 | 79 | − 0.012 | − 0.028 | 0.809 |
| Waist circumference (cm) | ||||||||||||
| Eating window (h) | 114 | − 0.001 | − 0.088 | 0.352 | 34 | 0.049 | − 0.279 | 0.111 | 80 | − 0.001 | 0.109 | 0.337 |
| Caloric midpoint (h) | 114 | − 0.008 | − 0.028 | 0.770 | 34 | 0.020 | − 0.224 | 0.203 | 80 | − 0.003 | 0.101 | 0.375 |
| Eating jetlag (h) | 114 | − 0.005 | − 0.065 | 0.491 | 34 | − 0.022 | − 0.095 | 0.594 | 80 | − 0.002 | − 0.105 | 0.352 |
| Time from midsleep point to first food intake (h) | 111 | − 0.004 | 0.072 | 0.450 | 34 | 0.007 | 0.192 | 0.277 | 77 | − 0.013 | − 0.018 | 0.876 |
| Time from last food intake to midsleep point (h) | 111 | − 0.009 | 0.016 | 0.866 | 34 | − 0.019 | 0.110 | 0.536 | 77 | 0.008 | − 0.147 | 0.203 |
Adjusted R2, β standardized regression coefficients and p values are obtained from single linear regressions. Neither association remained statistically significant after applying false discovery rate correction (Benjamini–Hochberg)
Bold font is used to indicate statistically significant p-values (p < 0.05)
Meal timing and cardiometabolic risk factors
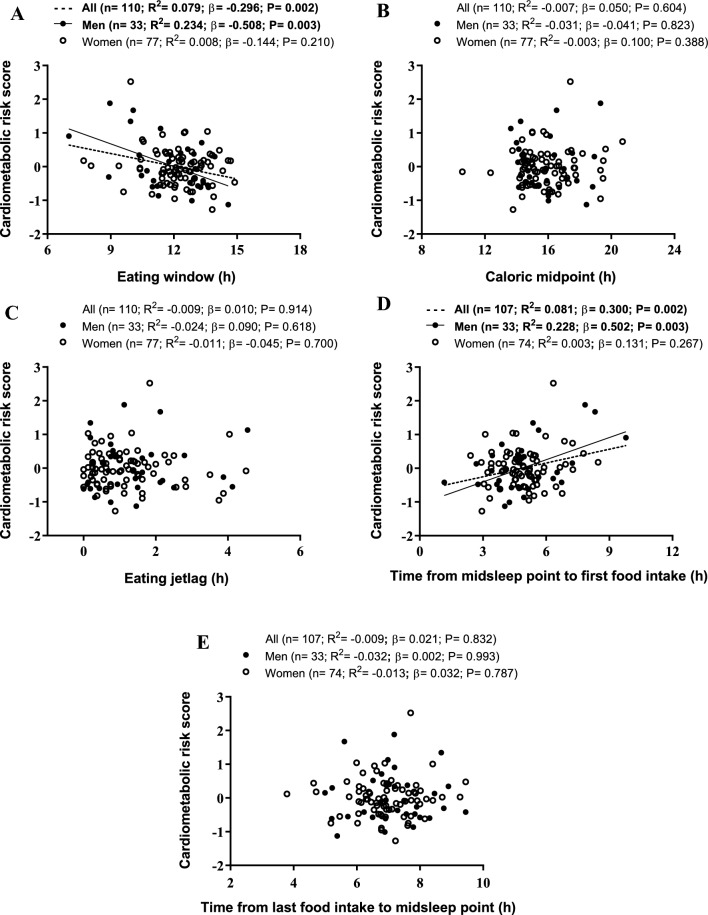
The eating window was negatively related to HOMA-IR in all participants and in men (R2 = 0.100, β = − 0.328; R2 = 0.348, β = − 0.605, respectively; all p ≤ 0.001; Table 3, Fig. 1 and S2). The eating window was also negatively associated with cardiometabolic risk score in all participants and in men (R2 = 0.079, β = − 0.296; R2 = 0.234, β = − 0.508, respectively; all p ≤ 0.003; Table 3, Fig. 1 and S2). A negative association between the eating window and triglycerides was observed in all participants (R2 = 0.044, β = − 0.229, p = 0.013; Table 3 and figure S2). The eating window was positively related to HDL-C in all participants and in men (R2 = 0.048, β = 0.238; R2 = 0.162, β = 0.431, respectively; all p ≤ 0.010; Table 3 and figure S2). No associations were found between caloric midpoint and eating jetlag with cardiometabolic risk factors (all p ≥ 0.150; Table 3). The time from midsleep point to first food intake was positively related to HOMA-IR in all participants and in men (R2 = 0.078, β = 0.294; R2 = 0.212, β = 0.485, respectively; all p ≤ 0.003; Table 3, Fig. 1 and S2). The time from midsleep point to first food intake was also positively associated with cardiometabolic risk score in all participants and in men (R2 = 0.081, β = 0.300; R2 = 0.228, β = 0.502, respectively; all p ≤ 0.003; Table 3, Fig. 1 and S2). A positive association between the time from midsleep point to first food intake and mean blood pressure was found in all participants (R2 = 0.030, β = 0.197, p = 0.037; Table 3 and figure S2). The time from midsleep point to first food intake was negatively associated with HDL-C in all participants and in men (R2 = 0.045, β = − 0.231; R2 = 0.137, β = − 0.403, respectively; all p ≤ 0.016; Table 3 and figure S2). A significant positive association between the time from last food intake to midsleep point and triglycerides was found in women (R2 = 0.087, β = 0.314, p = 0.005; Table 3). Several variables of meal timing were significantly associated with potential confounders such as a priori Mediterranean diet pattern, light physical activity and midsleep point (all p ≤ 0.05; figure S3). Of note is that only the associations of eating window and time from midsleep point to first food intake with HOMA-IR and cardiometabolic risk score—in all participants and men—remained after adjusting for potential confounders and false discovery rate (all p ≤ 0.011; Table 2, 3 and S2–S3).
Table 3.
Association of meal timing with cardiometabolic risk factors in young adults
| Cardiometabolic risk factors | All | Men | Women | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | R2 | β | P value | N | R2 | β | P value | N | R2 | β | P value | |
| Mean blood pressure (mmHg) | ||||||||||||
| Eating window (h) | 116 | 0.015 | − 0.153 | 0.100 | 36 | 0.051 | − 0.280 | 0.099 | 80 | − 0.011 | − 0.036 | 0.749 |
| Caloric midpoint (h) | 116 | − 0.006 | 0.054 | 0.562 | 36 | − 0.007 | 0.149 | 0.387 | 80 | − 0.012 | 0.033 | 0.773 |
| Eating jetlag (h) | 116 | − 0.009 | − 0.015 | 0.871 | 36 | − 0.029 | − 0.013 | 0.940 | 80 | − 0.010 | − 0.056 | 0.624 |
| Time from midsleep point to first food intake (h) | 112 | 0.030 | 0.197 | 0.037 | 35 | 0.031 | 0.245 | 0.156 | 77 | 0.021 | 0.185 | 0.107 |
| Time from last food intake to midsleep point (h) | 112 | − 0.006 | − 0.052 | 0.585 | 35 | − 0.030 | 0.006 | 0.973 | 77 | 0.017 | − 0.174 | 0.129 |
| Triglycerides | ||||||||||||
| Eating window (h) | 117 | 0.044 | − 0.229 | 0.013 | 36 | 0.040 | − 0.259 | 0.127 | 81 | 0.030 | − 0.204 | 0.068 |
| Caloric midpoint (h) | 117 | − 0.008 | 0.032 | 0.730 | 36 | − 0.005 | 0.154 | 0.371 | 81 | − 0.012 | − 0.022 | 0.844 |
| Eating jetlag (h) | 117 | − 0.005 | 0.063 | 0.502 | 36 | 0.032 | 0.245 | 0.150 | 81 | − 0.010 | − 0.051 | 0.650 |
| Time from midsleep point to first food intake (h) | 113 | 0.005 | 0.119 | 0.209 | 35 | 0.072 | 0.315 | 0.066 | 78 | − 0.012 | − 0.026 | 0.823 |
| Time from last food intake to midsleep point (h) | 113 | 0.015 | 0.154 | 0.103 | 35 | − 0.017 | − 0.113 | 0.516 | 78 | 0.087 | 0.314 | 0.005 |
| Total cholesterol | ||||||||||||
| Eating window (h) | 117 | − 0.006 | − 0.052 | 0.577 | 36 | − 0.012 | − 0.130 | 0.451 | 81 | − 0.012 | − 0.017 | 0.878 |
| Caloric midpoint (h) | 117 | − 0.009 | − 0.013 | 0.892 | 36 | − 0.020 | 0.096 | 0.579 | 81 | − 0.007 | − 0.073 | 0.516 |
| Eating jetlag (h) | 117 | − 0.001 | 0.088 | 0.346 | 36 | − 0.009 | 0.142 | 0.409 | 81 | − 0.009 | 0.058 | 0.604 |
| Time from midsleep point to first food intake (h) | 113 | − 0.005 | 0.063 | 0.505 | 35 | 0.057 | 0.291 | 0.090 | 78 | − 0.003 | − 0.101 | 0.380 |
| Time from last food intake to midsleep point (h) | 113 | − 0.009 | 0.008 | 0.936 | 35 | − 0.003 | − 0.164 | 0.347 | 78 | 0.007 | 0.141 | 0.218 |
| High-density lipoprotein cholesterol | ||||||||||||
| Eating window (h) | 117 | 0.048 | 0.238 | 0.010 | 36 | 0.162 | 0.431 | 0.009 | 81 | 0.008 | 0.141 | 0.208 |
| Caloric midpoint (h) | 117 | − 0.006 | 0.054 | 0.560 | 36 | 0.013 | 0.202 | 0.237 | 81 | − 0.012 | − 0.021 | 0.855 |
| Eating jetlag (h) | 117 | − 0.009 | 0.004 | 0.964 | 36 | 0.004 | − 0.179 | 0.296 | 81 | − 0.003 | 0.099 | 0.379 |
| Time from midsleep point to first food intake (h) | 113 | 0.045 | − 0.231 | 0.014 | 35 | 0.137 | − 0.403 | 0.016 | 78 | 0.021 | − 0.184 | 0.106 |
| Time from last food intake to midsleep point (h) | 113 | − 0.008 | − 0.027 | 0.774 | 35 | − 0.030 | − 0.007 | 0.966 | 78 | − 0.011 | 0.041 | 0.721 |
| Low-density lipoprotein cholesterol | ||||||||||||
| Eating window (h) | 117 | − 0.001 | − 0.088 | 0.345 | 36 | − 0.001 | − 0.167 | 0.329 | 81 | − 0.011 | − 0.039 | 0.730 |
| Caloric midpoint (h) | 117 | − 0.008 | − 0.020 | 0.830 | 36 | − 0.029 | − 0.008 | 0.963 | 81 | − 0.012 | − 0.027 | 0.812 |
| Eating jetlag (h) | 117 | 0.000 | 0.094 | 0.313 | 36 | − 0.003 | 0.161 | 0.349 | 81 | − 0.010 | 0.053 | 0.637 |
| Time from midsleep point to first food intake (h) | 113 | 0.011 | 0.140 | 0.139 | 35 | 0.077 | 0.323 | 0.058 | 78 | − 0.013 | 0.007 | 0.953 |
| Time from last food intake to midsleep point (h) | 113 | − 0.007 | − 0.041 | 0.665 | 35 | − 0.008 | − 0.146 | 0.401 | 78 | − 0.012 | 0.032 | 0.784 |
| HOMA-IR | ||||||||||||
| Eating window (h) | 117 | 0.100 | − 0.328 | < 0.001* | 36 | 0.348 | − 0.605 | < 0.001* | 81 | − 0.002 | − 0.101 | 0.369 |
| Caloric midpoint (h) | 117 | − 0.002 | 0.079 | 0.399 | 36 | − 0.029 | 0.015 | 0.935 | 81 | 0.005 | 0.131 | 0.245 |
| Eating jetlag (h) | 117 | − 0.002 | 0.080 | 0.393 | 36 | − 0.022 | 0.085 | 0.623 | 81 | − 0.007 | 0.076 | 0.499 |
| Time from midsleep point to first food intake (h) | 113 | 0.078 | 0.294 | 0.002* | 35 | 0.212 | 0.485 | 0.003 | 78 | 0.003 | 0.126 | 0.271 |
| Time from last food intake to midsleep point (h) | 113 | − 0.006 | 0.053 | 0.579 | 35 | − 0.017 | 0.115 | 0.511 | 78 | − 0.013 | − 0.019 | 0.867 |
| Cardiometabolic risk score | ||||||||||||
| Eating window (h) | 110 | 0.079 | − 0.296 | 0.002* | 33 | 0.234 | − 0.508 | 0.003* | 77 | 0.008 | − 0.144 | 0.210 |
| Caloric midpoint (h) | 110 | − 0.007 | 0.050 | 0.604 | 33 | − 0.031 | − 0.041 | 0.823 | 77 | − 0.003 | 0.100 | 0.388 |
| Eating jetlag (h) | 110 | − 0.009 | 0.010 | 0.914 | 33 | − 0.024 | 0.090 | 0.618 | 77 | − 0.011 | − 0.045 | 0.700 |
| Time from midsleep point to first food intake (h) | 107 | 0.081 | 0.300 | 0.002* | 33 | 0.228 | 0.502 | 0.003* | 74 | 0.003 | 0.131 | 0.267 |
| Time from last food intake to midsleep point (h) | 107 | − 0.009 | 0.021 | 0.832 | 33 | − 0.032 | 0.002 | 0.993 | 74 | − 0.013 | 0.032 | 0.787 |
Adjusted R2, β standardized regression coefficients and p values are obtained from single linear regressions. All cardiometabolic risk factors (except for mean blood pressure and cardiometabolic risk score) were log10-transformed to bring their distributions closer to normal. Cardiometabolic risk score was calculated for each sex based on waist circumference, blood pressure, plasma glucose, high-density lipoprotein cholesterol, and triglyceride concentrations (see methods for further details). Symbol * these associations remained statistically significant after applying false discovery rate correction (Benjamini–Hochberg)
Bold font is used to indicate statistically significant p-values (p < 0.05)
HOMA-IR homeostasis model assessment of insulin resistance
Fig. 1.
Scatterplots of the associations of meal timing with cardiometabolic risk score (calculated for each sex based on waist circumference, blood pressure, plasma glucose, high-density lipoprotein cholesterol, and triglyceride concentrations, see methods for further details) in young adults. Adjusted R2, β standardized regression coefficients and p values are obtained from single linear regressions
Differences between breakfast skipper and consumer
Significant differences between breakfast skipper and consumer were found for fasting blood glucose, midsleep point, dietary patterns and quality, eating window, caloric midpoint, eating jetlag, and time from midsleep point to first food intake (all p ≤ 0.045; table S4). Breakfast consumption influenced the relationship between meal timing and body composition in women observing that the eating window was positively associated with BMI and VAT mass in women breakfast consumers (all p ≤ 0.036; figure S4). Breakfast consumption did not modify the relationship shown by meal timing with cardiometabolic risk factors (figure S5).
Discussion
Our findings suggest that meal timing is not related to anthropometry or body composition parameters in young adults. Similarly, caloric midpoint, eating jetlag and the time from last food intake to midsleep point are not associated with cardiometabolic risk factors. On the other hand, our results show that a longer daily eating window and a shorter time from midsleep point to first food intake (i.e., earlier first food intake in a 24 h cycle) are associated with a healthier cardiometabolic profile (i.e., lower HOMA-IR and cardiometabolic risk score) in young men. These results refute our previous hypothesis, by which a shorter eating window would be associated with a healthier status. However, these findings confirm previous evidence that eating early in alignment with circadian rhythms may play an important role in cardiometabolic health.
The habitual daily eating window in adults in modern societies is ≥ 12 h which is abnormal from an evolutionary perspective [4, 31]. The eating pattern of our hunter-gatherer ancestors was characterized by eating sporadically with inter-meal intervals that depend upon the availability of food sources which included extended fasting period [4]. Moreover, clinical trials have also revealed that reducing the daily eating window results in body weight loss and improvement in cardiometabolic health in adults with overweight or obesity [20–22]. Therefore, we hypothesized that a shorter daily eating window would be associated with better body composition and cardiometabolic health in our cohort of young adults. However, interpreting the cross-sectional relationship between meal timing and health status is a complex task, as it can be influenced by several factors. Indeed, contradictory findings have been reported [9–14, 17, 23, 31, 39, 40]. For instance, we found that the daily eating window is not related to body composition, which could be partly explained by the low variability (standard deviation of 1.5 h) of the daily eating window in our sample. Our results concur with other studies in young adults [12], middle-aged adults [31] and adults with prediabetes [39]. In contrast, others reported that a longer daily eating window is related to a lower BMI [40] and lower fat mass percentage in adults [11]. A confounding factor may be the consumption of breakfast; epidemiological data have constantly shown that breakfast consumption is associated with lower BMI and adiposity [41–43]. Greater energy intake, lower diet quality, lower physical activity levels and misalignment of circadian rhythms are thought to be the physiological mechanisms behind these associations [41–43]. In our cohort of young adults, we observed that adherence to the Mediterranean diet and Mediterranean diet quality was lower in breakfast skippers than in consumers in women. Furthermore, breakfast consumption influences the relationship between meal timing and body composition in women. Specifically, a longer daily eating window was associated with worst body composition (i.e., higher BMI and VAT mass) in women breakfast consumers which is in line with our previous hypothesis and with other study findings in middle-aged women [16] and in older adults [14].
The daily eating window does not take into account the time distribution of food intake, which may be a more important factor than its duration. Indeed, Xiao et al. [14] observed that when a short daily eating window occurs early in the day is associated with a reduced likelihood of being overweight or obese in older adults; while, when a short daily eating window occurs late in the day is related to a higher likelihood of being overweight or obese. For this reason, other meal timing variables have been proposed. One of them is the caloric midpoint, that links meal timing to clock time. A study conducted in Spanish middle-aged adults found that late eaters (i.e., caloric midpoint after 3 pm) had higher BMI, fat mass percentage and waist circumference than early eaters [9], findings that partially concur with those observed in Brazilian young adults [13]. In our study, the caloric midpoint was negatively associated with fat mass percentage in men but became non-significant after adjusting for multiplicity. Another meal-timing variable is eating jetlag, which indicates the variability of the eating midpoint between working and non-working days, being informative about the circadian misalignment. For example, Zerón-Rugerio et al. [17] showed that a greater eating jet lag is related to higher BMI in Spanish and Mexican young adults. Conversely, we observed no association between eating jetlag and body composition in our cohort of Spanish young adults.
Nonetheless, the caloric midpoint and eating jetlag use clock time to illustrate the timing of food intake, which fails to correctly characterize meal timing in relation to the internal circadian time [10, 23]. In this sense, McHill et al. [12] found that a long time from caloric midpoint to melatonin onset is associated with lower BMI and fat mass percentage. However, obtaining measures of dim-light melatonin is not practical in large clinical trials; thus, it has been proposed to measure the timing of food intake relative to the sleep/wake cycle as a proxy for circadian time [10, 23, 24]. Using this methodology, two studies observed that a longer time period from dinner to midsleep point or bedtime is associated with lower adiposity and BMI, respectively [10, 23]. In contrast, we found no relationship between the time from the midsleep point to first food intake or time from last food intake to midsleep point with anthropometry or body composition parameters, which concurs with another study [14]. These discrepancies could be partially explained by the sample size and the assessment of meal and sleep timing.
Regarding cardiometabolic health, we found that a longer daily eating window and a shorter time from midsleep point to first food intake are associated with healthier cardiometabolic profile in men, which agree with previous studies. Concretely, a longer daily eating window has been related to decreased insulin, total cholesterol, LDL-C and increased HDL-C in middle-aged adults [44]. In addition, in concordance with our results, previous studies have found that late eating is related to worst cardiometabolic health [9–16]. Circadian misalignment between the central clock (controlled by external light) and peripheral clocks (regulated by eating, physical activity and sleep among other factors) is one of the mechanisms that may explain these results [6, 7]. In addition, glucose tolerance is higher in the biological morning, which appear to be driven by diurnal variations in β-cell responsiveness, peripheral insulin sensitivity, insulin clearance, and glucose effectiveness [6, 7]. Skeletal muscle fatty acid oxidation and the thermic effect of food are also higher in the biological morning or around noon, which implicates earlier in the daytime is optimal for eating whereas night time is better for fasting and sleep [6, 7]. Our findings could also be partly explained by the consumption of breakfast; epidemiological data have systematically reported that breakfast skipping (i.e., shorter and later daily eating window) is associated with worst cardiometabolic health [41, 42]. As mentioned above, this association could be driven in part by lower diet quality and lower physical activity levels [41–43]. Indeed, in our cohort of young men, we observed that breakfast skippers had a more inflammatory diet and tended to be less physically active. Lastly, others [16] and we did not observe a relationship between meal timing and cardiometabolic risk factors in women, which is intriguing and requires further investigation.
Our findings should be interpreted with caution because the current study suffers from several limitations. Firstly, the cross-sectional design prevents establishing causal relationships. Secondly, we measured the clock timing of food intake via three non-consecutive 24 h recalls. Thirdly, the study population comprised young and healthy adults, limiting the generalizability of the results to older or metabolically compromised individuals. Lastly, the statistical power of the study may have been insufficient to comprehensively investigate potential sex differences in the relationship between meal timing with body composition and cardiometabolic risk factors. Despite these limitations, this study is one of the pioneers in investigating the relationship between meal timing (characterized relative to the sleep/wake cycle) and cardiometabolic risk factors. Further well-designed long-term prospective studies and randomized controlled trials are needed to elucidate the effects of meal timing on body composition and cardiometabolic health.
Conclusion
Meal timing is not related to either anthropometry or body composition parameters in young adults. Similarly, caloric midpoint, eating jetlag and the time from last food intake to midsleep point are not associated with cardiometabolic risk factors. Nonetheless, a longer daily eating window and a shorter time from midsleep point to first food intake are associated with better cardiometabolic health in men. These results confirm previous evidence that eating early in alignment with circadian rhythms may improve cardiometabolic health. Nutrition strategies aimed to improve cardiometabolic health may contemplate advancing the timing of food intake. Further well-designed studies are needed to confirm these findings and unravel potential mechanisms.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
This study is part of a Ph.D. Thesis conducted in the Biomedicine Doctoral Studies of the University of Granada, Spain.
Author contributions
MD-M: Formal analysis, Writing—Original Draft. FMA: Conceptualization, Methodology, Investigation, Writing—Review & Editing. GS-D: Conceptualization, Methodology, Investigation, Project administration, Writing—Review & Editing. EM-R: Investigation, Writing—Review & Editing. FJA-G: Investigation, Writing—Review & Editing. IL: Writing—Review & Editing. JRR: Conceptualization, Methodology, Supervision, Funding acquisition, Writing—Review & Editing.
Funding
Funding for open access publishing: Universidad de Granada/CBUA. This study was funded by the Spanish Ministry of Economy and Competitiveness via the Fondo de Investigación Sanitaria del Instituto de Salud Carlos III (PI13/01393) and PTA 12264-I, by Retos de la Sociedad (DEP2016-79512-R), European Regional Development Funds (ERDF), Spanish Ministry of Universities (FPU 13/03410, FPU14/04172 and FPU18/03357), the Fundación Iberoamericana de Nutrición (FINUT), the Redes Temáticas de Investigación Cooperativa RETIC network (Red SAMID RD16/0022), the AstraZeneca HealthCare Foundation, Junta de Andalucía, Consejería de Transformación económica, Industria, Conocimiento y Universidades (A-CTS-516-UGR20), the University of Granada's Plan Propio de Investigación 2016—Excellence actions: Unit of Excellence on Exercise and Health (UCEES), the Junta de Andalucía, Consejería de Conocimiento, Investigación y Universidades (ERDF, SOMM17/6107/UGR), and a postdoctoral grant from the Fundación Alfonso Martín Escudero.
Data availability
The deidentified participant data that support the findings of this study are available from the corresponding author upon reasonable request.
Declarations
Conflict of interest
The authors declared no conflict of interest.
Ethical standards
The study protocol and written informed consent procedures contemplated the latest revised Declaration of Helsinki (2013), and they were approved by the Human Research Ethics Committee of the University of Granada (Nº 924) and the Servicio Andaluz de Salud (CEI-Granada, nº 0838-N-2017). All participants provided written informed consent in order to be included in the study.
Footnotes
The original online version of this article was revised: The x-axis visualization is somewhat blurred or diffused in figure 1.
Change history
6/1/2023
A Correction to this paper has been published: 10.1007/s00394-023-03175-z
Contributor Information
Manuel Dote-Montero, Email: manueldote@ugr.es.
Jonatan R. Ruiz, Email: ruizj@ugr.es
References
- 1.Organization WH (2020) Obesity and overweight. World Health Organization. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. Accesed 15 Nov 2022
- 2.Finkelstein EA, Trogdon JG, Cohen JW, Dietz W. Annual medical spending attributable to obesity: payer-and service-specific estimates. Health Aff (Millwood) 2009;28(5):w822–w831. doi: 10.1377/hlthaff.28.5.w822. [DOI] [PubMed] [Google Scholar]
- 3.Hall KD, Farooqi IS, Friedman JM, Klein S, Loos RJF, Mangelsdorf DJ, O'Rahilly S, Ravussin E, Redman LM, Ryan DH, Speakman JR, Tobias DK. The energy balance model of obesity: beyond calories in, calories out. Am J Clin Nutr. 2022;115(5):1243–1254. doi: 10.1093/ajcn/nqac031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mattson MP, Allison DB, Fontana L, Harvie M, Longo VD, Malaisse WJ, Mosley M, Notterpek L, Ravussin E, Scheer FAJL, Seyfried TN, Varady KA, Panda S. Meal frequency and timing in health and disease. Proc Natl Acad Sci USA. 2014;111(47):16647. doi: 10.1073/pnas.1413965111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dashti HS, Scheer F, Saxena R, Garaulet M. Timing of food intake: identifying contributing factors to design effective interventions. Adv Nutr. 2019;10(4):606–620. doi: 10.1093/advances/nmy131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lewis P, Oster H, Korf HW, Foster RG, Erren TC. Food as a circadian time cue—evidence from human studies. Nat Rev Endocrinol. 2020;16(4):213–223. doi: 10.1038/s41574-020-0318-z. [DOI] [PubMed] [Google Scholar]
- 7.Poggiogalle E, Jamshed H, Peterson CM. Circadian regulation of glucose, lipid, and energy metabolism in humans. Metabolism. 2018;84:11–27. doi: 10.1016/j.metabol.2017.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zerón-Rugerio MF, Díez-Noguera A, Izquierdo-Pulido M, Cambras T. Higher eating frequency is associated with lower adiposity and robust circadian rhythms: a cross-sectional study. Am J Clin Nutr. 2021;113(1):17–27. doi: 10.1093/ajcn/nqaa282. [DOI] [PubMed] [Google Scholar]
- 9.Dashti HS, Gómez-Abellán P, Qian J, Esteban A, Morales E, Scheer F, Garaulet M. Late eating is associated with cardiometabolic risk traits, obesogenic behaviors, and impaired weight loss. Am J Clin Nutr. 2020;113(1):154–161. doi: 10.1093/ajcn/nqaa264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xiao Q, Garaulet M, Scheer F. Meal timing and obesity: interactions with macronutrient intake and chronotype. Int J Obes (Lond) 2019;43(9):1701–1711. doi: 10.1038/s41366-018-0284-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thomas EA, Zaman A, Cornier MA, Catenacci VA, Tussey EJ, Grau L, Arbet J, Broussard JL, Rynders CA. Later meal and sleep timing predicts higher percent body fat. Nutrients. 2020;13(1):73. doi: 10.3390/nu13010073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McHill AW, Phillips AJ, Czeisler CA, Keating L, Yee K, Barger LK, Garaulet M, Scheer FA, Klerman EB. Later circadian timing of food intake is associated with increased body fat. Am J Clin Nutr. 2017;106(5):1213–1219. doi: 10.3945/ajcn.117.161588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Teixeira GP, Barreto ACF, Mota MC, Crispim CA. Caloric midpoint is associated with total calorie and macronutrient intake and body mass index in undergraduate students. Chronobiol Int. 2019;36(10):1418–1428. doi: 10.1080/07420528.2019.1652830. [DOI] [PubMed] [Google Scholar]
- 14.Xiao Q, Bauer C, Layne T, Playdon M. The association between overnight fasting and body mass index in older adults: the interaction between duration and timing. Int J Obes (Lond) 2021;45(3):555–564. doi: 10.1038/s41366-020-00715-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Quist JS, Blond MB, Faerch K, Ewers B. Late-evening food intake is highly prevalent among individuals with type 2 diabetes. Nutr Res. 2021;81:91–96. doi: 10.1016/j.nutres.2020.12.015. [DOI] [PubMed] [Google Scholar]
- 16.Taetzsch A, Roberts SB, Bukhari A, Lichtenstein AH, Gilhooly CH, Martin E, Krauss AJ, Hatch-McChesney A, Das SK. Eating timing: associations with dietary intake and metabolic health. J Acad Nutr Diet. 2021;121(4):738–748. doi: 10.1016/j.jand.2020.10.001. [DOI] [PubMed] [Google Scholar]
- 17.Zerón-Rugerio MF, Hernáez Á, Porras-Loaiza AP, Cambras T, Izquierdo-Pulido M. Eating jet lag: a marker of the variability in meal timing and its association with body mass index. Nutrients. 2019;11(12):2980. doi: 10.3390/nu11122980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Madjd A, Taylor MA, Delavari A, Malekzadeh R, Macdonald IA, Farshchi HR. Effects of consuming later evening meal v. earlier evening meal on weight loss during a weight loss diet: a randomised clinical trial. Br J Nutr. 2021;126(4):632–640. doi: 10.1017/s0007114520004456. [DOI] [PubMed] [Google Scholar]
- 19.Madjd A, Taylor MA, Delavari A, Malekzadeh R, Macdonald IA, Farshchi HR. Beneficial effect of high energy intake at lunch rather than dinner on weight loss in healthy obese women in a weight-loss program: a randomized clinical trial. Am J Clin Nutr. 2016;104(4):982–989. doi: 10.3945/ajcn.116.134163. [DOI] [PubMed] [Google Scholar]
- 20.Sutton EF, Beyl R, Early KS, Cefalu WT, Ravussin E, Peterson CM. Early time-restricted feeding improves insulin sensitivity, blood pressure, and oxidative stress even without weight loss in men with prediabetes. Cell Metab. 2018;27(6):1212–21.e3. doi: 10.1016/j.cmet.2018.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cienfuegos S, Gabel K, Kalam F, Ezpeleta M, Wiseman E, Pavlou V, Lin S, Oliveira ML, Varady KA. Effects of 4- and 6-h time-restricted feeding on weight and cardiometabolic health: a randomized controlled trial in adults with obesity. Cell Metab. 2020;32(3):366–78.e3. doi: 10.1016/j.cmet.2020.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dote-Montero M, Sanchez-Delgado G, Ravussin E. Effects of intermittent fasting on cardiometabolic health: an energy metabolism perspective. Nutrients. 2022;14(3):489. doi: 10.3390/nu14030489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zerón-Rugerio MF, Longo-Silva G, Hernáez Á, Ortega-Regules AE, Cambras T, Izquierdo-Pulido M. The elapsed time between dinner and the midpoint of sleep is associated with adiposity in young women. Nutrients. 2020;12(2):410. doi: 10.3390/nu12020410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Roenneberg T, Pilz LK, Zerbini G, Winnebeck EC. Chronotype and social jetlag: a (self-) critical review. Biology (Basel) 2019;8(3):54. doi: 10.3390/biology8030054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sanchez-Delgado G, Martinez-Tellez B, Olza J, Aguilera CM, Labayen I, Ortega FB, Chillon P, Fernandez-Reguera C, Alcantara JMA, Martinez-Avila WD, Muñoz-Hernandez V, Acosta FM, Prados-Ruiz J, Amaro-Gahete FJ, Hidalgo-Garcia L, Rodriguez L, Ruiz YA-K, Ramirez-Navarro A, Muros-de Fuentes MA, García-Rivero Y, Sanchez-Sanchez R, de Dios Beas Jimenez J, de Teresa C, Navarrete S, Lozano R, Brea-Gomez E, Rubio-Lopez J, Ruiz MR, Cano-Nieto A, Llamas-Elvira JM, Jimenez Rios JA, Gil A, Ruiz JR. Activating brown adipose tissue through exercise (ACTIBATE) in young adults: rationale, design and methodology. Contemp Clin Trials. 2015;45:416–425. doi: 10.1016/j.cct.2015.11.004. [DOI] [PubMed] [Google Scholar]
- 26.Hörnell A, Berg C, Forsum E, Larsson C, Sonestedt E, Åkesson A, Lachat C, Hawwash D, Kolsteren P, Byrnes G, De Keyzer W, Van Camp J, Cade JE, Greenwood DC, Slimani N, Cevallos M, Egger M, Huybrechts I, Wirfält E. Perspective: an extension of the STROBE Statement for Observational Studies in Nutritional Epidemiology (STROBE-nut): explanation and elaboration. Adv Nutr. 2017;8(5):652–678. doi: 10.3945/an.117.015941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18(6):499–502. doi: 10.1093/clinchem/18.6.499. [DOI] [PubMed] [Google Scholar]
- 28.Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart JC, James WP, Loria CM, Smith SC., Jr Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120(16):1640–1645. doi: 10.1161/circulationaha.109.192644. [DOI] [PubMed] [Google Scholar]
- 29.Migueles JH, Cadenas-Sanchez C, Ekelund U, Delisle Nyström C, Mora-Gonzalez J, Löf M, Labayen I, Ruiz JR, Ortega FB. Accelerometer data collection and processing criteria to assess physical activity and other outcomes: a systematic review and practical considerations. Sports Med. 2017;47(9):1821–1845. doi: 10.1007/s40279-017-0716-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ruiz-López MD, Martín-Lagos RA (2010) Guía para estudios dietéticos: álbum fotográfico de alimentos: Editorial Universidad de Granada
- 31.Gill S, Panda S. A Smartphone App reveals erratic diurnal eating patterns in humans that can be modulated for health benefits. Cell Metab. 2015;22(5):789–798. doi: 10.1016/j.cmet.2015.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vioque J, Navarrete-Muñoz EM, Gimenez-Monzó D, García-de-la-Hera M, Granado F, Young IS, Ramón R, Ballester F, Murcia M, Rebagliato M, Iñiguez C. Reproducibility and validity of a food frequency questionnaire among pregnant women in a Mediterranean area. Nutr J. 2013;12:26. doi: 10.1186/1475-2891-12-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Martínez-González MA, Fernández-Jarne E, Serrano-Martínez M, Marti A, Martinez JA, Martín-Moreno JM. Mediterranean diet and reduction in the risk of a first acute myocardial infarction: an operational healthy dietary score. Eur J Nutr. 2002;41(4):153–160. doi: 10.1007/s00394-002-0370-6. [DOI] [PubMed] [Google Scholar]
- 34.Trichopoulou A, Costacou T, Bamia C, Trichopoulos D. Adherence to a Mediterranean diet and survival in a Greek population. N Engl J Med. 2003;348(26):2599–2608. doi: 10.1056/NEJMoa025039. [DOI] [PubMed] [Google Scholar]
- 35.Gerber M. Qualitative methods to evaluate Mediterranean diet in adults. Public Health Nutr. 2007;9(1a):147–151. doi: 10.1079/PHN2005937. [DOI] [PubMed] [Google Scholar]
- 36.Patterson RE, Haines PS, Popkin BM. Diet quality index: capturing a multidimensional behavior. J Am Diet Assoc. 1994;94(1):57–64. doi: 10.1016/0002-8223(94)92042-7. [DOI] [PubMed] [Google Scholar]
- 37.Shivappa N, Steck SE, Hurley TG, Hussey JR, Hébert JR. Designing and developing a literature-derived, population-based dietary inflammatory index. Public Health Nutr. 2014;17(8):1689–1696. doi: 10.1017/s1368980013002115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dmitrienko A, D'Agostino Sr RB, Huque MF. Key multiplicity issues in clinical drug development. Stat Med. 2013;32(7):1079–1111. doi: 10.1002/sim.5642. [DOI] [PubMed] [Google Scholar]
- 39.Mogensen CS, Faerch K, Bruhn L, Amadid H, Tetens I, Quist JS, Clemmensen KKB. Timing and frequency of daily energy intake in adults with prediabetes and overweight or obesity and their associations with body fat. Nutrients. 2020;12(11):3484. doi: 10.3390/nu12113484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.O'Connor SG, Reedy J, Graubard BI, Kant AK, Czajkowski SM, Berrigan D. Circadian timing of eating and BMI among adults in the American Time Use Survey. Int J Obes (Lond) 2022;46(2):287–296. doi: 10.1038/s41366-021-00983-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Deshmukh-Taskar P, Nicklas TA, Radcliffe JD, O'Neil CE, Liu Y. The relationship of breakfast skipping and type of breakfast consumed with overweight/obesity, abdominal obesity, other cardiometabolic risk factors and the metabolic syndrome in young adults. The National Health and Nutrition Examination Survey (NHANES): 1999–2006. Public Health Nutr. 2013;16(11):2073–2082. doi: 10.1017/s1368980012004296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.St-Onge MP, Ard J, Baskin ML, Chiuve SE, Johnson HM, Kris-Etherton P, Varady K. Meal timing and frequency: implications for cardiovascular disease prevention: a scientific statement from the American Heart Association. Circulation. 2017;135(9):e96–e121. doi: 10.1161/cir.0000000000000476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Horikawa C, Kodama S, Yachi Y, Heianza Y, Hirasawa R, Ibe Y, Saito K, Shimano H, Yamada N, Sone H. Skipping breakfast and prevalence of overweight and obesity in Asian and Pacific regions: a meta-analysis. Prev Med. 2011;53(4–5):260–267. doi: 10.1016/j.ypmed.2011.08.030. [DOI] [PubMed] [Google Scholar]
- 44.Wirth MD, Zhao L, Turner-McGrievy GM, Ortaglia A. Associations between fasting duration, timing of first and last meal, and cardiometabolic endpoints in the National Health and Nutrition Examination Survey. Nutrients. 2021;13(8):2686. doi: 10.3390/nu13082686. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The deidentified participant data that support the findings of this study are available from the corresponding author upon reasonable request.