Abstract
Objectives
Insertion of a double-lumen endotracheal tube (DLT) is the most commonly used method for one-lung ventilation (OLV). This meta-analysis was aimed at investigating the performance of lung ultrasound in assessing the DLT position in OLV.
Methods
Electronic databases were searched for related trials from inception to October 2022. The primary outcome was the performance of ultrasound or clinical evaluation in confirming the correctness of the DLT position, using fiberoptic bronchoscopy or intraoperative direct visualization of lung collapse as the gold standard. The secondary outcome was the time required to confirm or adjust the DTL position.
Results
Five randomized controlled trials and three observational studies involving 771 patients were included in the meta-analysis. The pooled sensitivity and specificity of ultrasound were 0.93 (95% confidence interval [CI]: 0.79–0.98) and 0.61 (95% CI: 0.41–0.77), respectively, while those of clinical evaluation were 0.93 (95% CI: 0.73–0.99) and 0.35 (95% CI: 0.25–0.47), respectively. The pooled procedure duration was 122.27 s (95% CI: 20.85–223.69) with ultrasound and 112.03 s (95% CI: 95.30–128.76) with clinical evaluation. The area under the curve for discriminating the DLT position was 0.86 (95% CI: 0.82–0.88) for ultrasound and 0.52 (95% CI: 0.48–0.57) for clinical evaluation.
Conclusions
Compared to clinical evaluation, ultrasound has a similar sensitivity but a better specificity for confirming the correctness of the DLT position. Ultrasound is an acceptable imaging tool for assessing DTL placement in OLV.
Keywords: Anesthesia, Ultrasonography, Thoracic surgery, Auscultation, Double-lumen tube
1. Introduction
Perioperative one-lung ventilation (OLV) is indispensable in thoracic surgery for obtaining local operative access [1]. It can be provided via several airway devices, of which the double-lumen endotracheal tube (DLT) is the most commonly used [2], owing to its facilitation of total collapse of the operated lung. Additionally, air, blood, and secretions in the lungs can be aspirated through DLT during surgery. Recently, the video double-lumen tube (VDLT) has been developed for OLV with an embedded camera and light source between the tracheal and bronchial cuffs. VDLT enables the continuation of airway visualization during the insertion and positioning of the tube. Multiple studies have suggested that the intubation time of VDLT is significantly shorter than that of conventional DLT [3,4]. However, even with VDLT, malpositioning of DLT may still take place, causing failure of total collapse of the target lung or inadequate ventilation of the contralateral lung, leading to intraoperative hypoventilation and hypoxemia [5]. Therefore, optimal DLT positioning is essential for OLV, and several evaluation methods have been developed for its assessment.
Fiberoptic bronchoscopy (FOB) is the gold standard for confirming the DLT position in the trachea [6,7]. Placement of airway devices, such as the Univent tube or bronchial blocker, requires the assistance of FOB [6,8], making operating skills for it a prerequisite for anesthesiologists specializing in thoracic anesthesia. Although the attributable mortality rates during FOB remain low (<0.1%), practitioners should be aware of potential risks, such as bronchospasms and tracheal hemorrhage [9]. Moreover, FOB is expensive and increases the risk of cross-infection. Considering these limitations, clinical evaluation is the mainstream method for the initial assessment of the DLT position.
Clinical evaluation encompasses multiple methods, such as auscultation, inspection of chest movements, and manual ventilation, to examine lung compliance; however, their accuracy is questionable, and reliability is unsatisfactory [[10], [11], [12], [13]]. Furthermore, de Bellis et al. [11] found that 37% of DLTs, whose positions were initially determined by clinical evaluation, required repositioning using FOB afterwards. Therefore, anesthesiologists need a learning curve to be skillful in examining the DLT position using clinical evaluations [10,[13], [14], [15]].
Ultrasound [16], a noninvasive modality, has been widely applied to facilitate various types of airway managements [[17], [18], [19]]. Some sonographic signs found on imaging of the pleural interface can be used to assess lung ventilation. Ultrasound has been employed in several studies to observe the presence/absence of lung sliding to ensure OLV following DLT placement [14,20]. In addition, ultrasound scans can be saved for documentation. Therefore, ultrasound may substitute clinical evaluations for verifying the DLT position; however, summarized evidence is currently lacking. Therefore, this meta-analysis was aimed at investigating the diagnostic performance of lung ultrasound in confirming the accuracy of the DLT position for OLV.
2. Methods
2.1. Protocol registration
This systematic review and meta-analysis was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines. The protocol was registered on Inplasy.com (INPLASY2022100021).
2.2. Data sources and search strategy
Electronic databases, including PubMed, Scopus, and Web of Science, were systematically searched from inception to October 8, 2022, without language restrictions. Relevant studies were identified using the following algorithm: ((ultrasound) OR (sonography) OR (ultrasonography)) AND ((double lumen) OR (double-lumen) AND (thoracic surgery) OR (one-lung ventilation)). The reference lists of associated reviews were manually searched for potential studies. Supplementary Material shows the complete search strategy.
2.3. Inclusion and exclusion criteria
Inclusion criteria were: (1) clinical trials of sonography for confirming DLT positioning and (2) human studies. Articles were excluded if they (1) investigated surgeries for two-lung ventilation, (2) did not specify the lung isolation technique, (3) lacked a control group, or (4) were case reports/series, reviews, study protocols, letters to the editor, or commentaries.
2.4. Article selection and data extraction
Papers retrieved from the original database search underwent title and abstract screening, and potentially eligible papers were assessed for full text. Two authors (T.Y.-L. and I.M.-S.) independently performed article selection and, in case of disagreement, a final decision was made after discussion with the corresponding author.
2.5. Quality assessment
Two independent authors graded the quality of the included studies using the Quality Assessment of Diagnostic Accuracy Studies (QUADAS)-2 [21]. The tool addresses four key domains: (1) patient selection, (2) index test, (3) reference standard, and (4) flow and timing of the primary studies used in the meta-analysis. For each domain, the risk of bias was classified as high, low, or unclear, and applicability was rated in the same manner for the previous three domains. Any discrepancies in the quality assessment were resolved by consensus. In the present meta-analysis, the result of quality assessment was not served as the reason why a study was included or excluded. The inclusion and exclusion of an article was based on the aforementioned inclusion and exclusion criteria.
2.6. Statistical analysis
The main outcome was the performance of ultrasound or clinical evaluation for validating the correctness of the DLT position using FOB or direct intraoperative visualization of lung collapse as the gold standard. The relevant parameters were the sensitivity, specificity, positive/negative predictive value, and positive/negative likelihood ratio, which were pooled using the random-effects model. The summary receiver operating characteristics (sROC) analysis was used to compute the area under the curve (AUC) for the diagnostic examination, and heterogeneity was assessed using I2 statistics. Significant heterogeneity was assumed for an I2 > 50% [22]. Deeks’ funnel plot asymmetry test was used to address the publication bias [23].
The secondary outcome was the procedure duration for confirming the DLT position, represented by the weighted mean with standard error. A significant difference between two evaluation tools was assumed by non-overlap of their 95% confidence intervals (CIs). Stata (StataCorp 2015, Stata Statistical Software: Release 14, StataCorp LP, College Station, TX, USA) and Comprehensive Meta-Analysis Software, version 3 (Biostat, Englewood, NJ, USA) were used for statistical analyses, and statistical significance was set at p < 0.05.
3. Results
3.1. Literature search
A total of 261 studies were obtained from the database search. After removing duplicates and screening the titles and abstracts, 11 full-text papers were retrieved to verify eligibility. One study [24] was excluded because ultrasound examination was carried out after correct placement of DLT, and two [25,26] studies were excluded for not using ultrasound to assess the DLT position. Finally, eight studies [14,15,20,[27], [28], [29], [30], [31]] were included in the quantitative analysis (Fig. 1).
Fig. 1.
Flow diagram of the literature search based on the Preferred Reporting Items for Systematic Reviews and Meta Analyses (PRISMA) guidelines.
3.2. Study characteristics
Of the eight included studies, five were randomized controlled trials, while three were observational studies. In this meta-analysis, we enrolled 771 patients who had undergone elective thoracic surgery. The mean age ranged from 46.3 to 64.0 years. Five studies [14,15,20,28,29] targeted left-sided DLT placement; one study [30] inspected bilateral DLT intubation; and the remaining two studies [27,31] did not specify the type of DTL used, as the side of DLT was selected according to the judgement of anesthesiologists who performed the intubation. The diagnostic accuracy of lung ultrasound was compared with that of clinical evaluations in seven studies [14,15,20,27,28,30,31] and FOB in one study [29]. The tube position was determined by FOB [14,20,27,28,30,31] or visualization of lung collapse during surgery [15,29] (Table 1).
Table 1.
Characteristics of the included studies.
| Author, year | Country | Design | Enrolled Patient (M/F) | Mean age | Type of surgery | Type of DLT | Diagnostic tool used | Reference standard |
|---|---|---|---|---|---|---|---|---|
| Sustic et al., 2010 | Croatia | Prospective RCT | 50 (29/21) | 58.5 | Elective thoracic | Left | LUS: lung sliding sign; Clinical examination; chest wall movement | FOB |
| Álvarez-Díaz et al., 2014 | Spain | Prospective Observational study | 105 (N/A) | 53.7 | Elective thoracic | N/A | LUS: lung sliding sign; Clinical examination; chest wall movement and breathing sound | FOB |
| Parab et al., 2015 | India | Prospective Non-RCT | 70 (50/20) | 48.3 | Elective thoracic | Left | LUS: lung sliding sign; Clinical examination; chest wall movement | Visual confirmation |
| Hu et al., 2017 | China | Prospective Non-RCT | 103 (51/52) | 56.1 | Elective thoracic | Both | LUS: lung sliding sign; Auscultation; breathing sound | FOB |
| Parab et al., 2019 | India | Prospective RCT | 91 (69/22) | 50.6 | Elective thoracic | N/A | LUS: lung sliding sign; Auscultation; breathing sound | FOB |
| Chung et al., 2020 | Korea | Prospective RCT | 88 (36/52) | 64.0 | Elective thoracic | Left | LUS: lung sliding sign; Auscultation; breathing sound | FOB |
| Park et al., 2021 | Korea | Prospective RCT | 69 (15/54) | 46.3 | Elective thoracic | N/A | LUS: lung sliding sign; Auscultation; breathing sound | FOB |
| Kanavitoon et al., 2022 | Thailand | Prospective RCT | 195 (86/109) | 60.5 | Elective thoracic | Left | LUS: lung sliding sign; FOB; correct positioning | Visual confirmation |
M: male; F: female; DLT, double-lumen endotracheal tube; FOB, fiberoptic bronchoscopy; RCT: randomized controlled trial; LUS, lung ultrasound; N/A: not available.
3.3. Quality assessment
Table 2 shows the results of the quality assessment. Two studies failed item 1 because one [15] did not mention the allocation process, while the other [28] did not perform random patient enrollment. Sustic et al. [20] set different time limits for completing auscultation and ultrasound assessment, which posed a high risk of bias for item 2. Park et al. [27] did not clarify if physicians performing sonography and FOB were blinded to the auscultation results. Five studies [14,[28], [29], [30], [31]] reported low risks for all analyzed items.
Table 2.
The methological quality of the included studies assessed by QUADAS-2.
| Author, year | Risk of Bias |
Applicability Concerns |
|||||
|---|---|---|---|---|---|---|---|
| Patient Selection | Index Text | Reference Standard | Flow and Timing | Patient Selection | Index Text | Reference Standard | |
| Sustic et al., 2010 | Low | High | Low | Low | Low | Low | Low |
| Álvarez-Díaz et al., 2014 | Low | Low | Low | Low | Low | Low | Low |
| Parab et al., 2015 | High | Low | Low | Low | Low | Low | Low |
| Hu et al., 2017 | Low | Low | Low | Low | Low | Low | Low |
| Parab et al., 2019 | Low | Low | Low | Low | Low | Low | Low |
| Chung et al., 2020 | Low | Low | Low | Low | Low | Low | Low |
| Park et al., 2021 | High | Unclear | Unclear | Low | Low | Low | Low |
| Kanavitoon et al., 2022 | Low | Low | Low | Low | Low | Low | Low |
Abbreviations: QUADAS, Quality Assessment of Diagnostic Accuracy Studies.
4. Outcome
4.1. Diagnostic performance
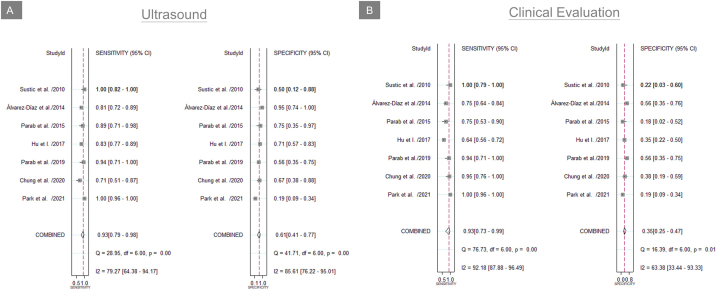
Among the eight included studies, seven reported data on diagnostic accuracy validated by FOB [14,20,[27], [28], [29], [30], [31]]. Ultrasound showed a pooled sensitivity of 0.93 (95% CI: 0.79–0.98; I2 = 79.27%), a specificity of 0.61 (95% CI: 0.41–0.77; I2 = 85.61%; Fig. 2A), accuracy of 78.6% (95% CI: 73.8%–82.7%; I2 = 33.97%), a pooled positive likelihood of 2.37 (95% CI: 1.56–3.59), a negative likelihood of 0.12 (95% CI: 0.05–0.30), a positive predictive value of 0.88 (95% CI: 0.77–0.99), and a negative predictive value of 0.69 (95% CI: 0.60–0.77). AUC in the sROC curve analysis was 0.86 (95% CI: 0.82–0.88; Fig. 3A). Deeks’ funnel plot asymmetry test showed no significant evidence of publication bias (p = 0.984; Fig. 4A).
Fig. 2.
Forest plot of the summarized sensitivity and specificity of (A) ultrasound imaging and (B) clinical evaluation for confirming the double-lumen tube position. CI, confidence interval.
Fig. 3.
The summary receiver operating curve (SROC) curve of (A) ultrasound imaging and (B) clinical evaluation for confirming the double-lumen tube position. AUC, area under the curve; SENS, sensitivity; SPEC, specificity; SROC, summary receiver operating curve.
Fig. 4.
Deek's Funnel Plot Asymmetry test for (A) ultrasound imaging and (B) clinical evaluation for confirming the double-lumen tube position.
Clinical evaluation for confirmation of the DLT position showed a sensitivity of 0.93 (95% CI: 0.73–0.99; I2 = 92.18%), a specificity of 0.35 (95% CI: 0.25–0.47; I2 = 63.38%; Fig. 2B), accuracy of 64.1% (95% CI: 56.2%–71.4%; I2 = 68.94%), a pooled positive likelihood of 1.44 (95% CI: 1.22–1.70), a negative likelihood of 0.19 (95% CI: 0.04–0.80), a positive predictive value of 0.83 (95% CI: 0.75–0.91), and a negative predictive value of 0.58 (95% CI: 0.54–0.63). The sROC curve analysis revealed an AUC of 0.52 (95% CI: 0.48–0.57; Fig. 3B). Finally, Deeks’ funnel plot asymmetry test revealed no significant evidence of publication bias (p = 0.812; Fig. 4B).
4.2. Time to confirm and adjust the DLT position
The time taken to confirm and adjust the DLT position was extracted from three studies [[28], [29], [30]]. The pooled values were 122.27 s (95% CI: 20.85–223.69; I2 = 99.95%) for ultrasound, 112.03 s (95% CI: 95.30–128.76; I2 = 87.59%) for clinical evaluation, and 240.30 s (95% CI: −70.43–551.05; I2 = 99.23%) for FOB (Fig. 5).
Fig. 5.
Forest plot for the procedure time for confirming the double-lumen position. CE, clinical evaluation; FOB, fiberoptic bronchoscopy; US, ultrasound.
5. Discussion
This meta-analysis yielded several important findings. First, ultrasound and clinical evaluation were similar in the sensitivity, positive predictive value, and positive likelihood ratio for confirming the DLT position. Second, the specificity, negative predictive value, and negative likelihood ratio were likely to be better with ultrasound than with clinical evaluation. Third, ultrasound and clinical evaluation did not differ in the procedure time required to confirm the DLT position.
This might be the first meta-analysis to evaluate the diagnostic performance of ultrasound to confirm the DLT position compared to clinical evaluation. The pooled sensitivity (0.93, 95% CI: 0.79–0.98) of ultrasound appeared similar to that of clinical evaluation (0.93, 95% CI: 0.73–0.99). These findings indicate that lung collapse after DLT insertion can be successfully recognized using ultrasonography or clinical evaluation. Nevertheless, ultrasound had significantly better specificity (0.61, 95% CI: 0.41–0.77) than clinical evaluation (0.35, 95% CI: 0.25–0.47), indicating that clinical evaluation was more likely to misrecognize the DLT position when the lung had not collapsed. The better specificity, negative predictive value, and negative likelihood ratio of ultrasound compared to clinical evaluation might be attributed to two factors. First, clinical evaluation is mainly based on auscultation, which depends on the intensity, frequency, and timbre of breath sounds [32]. Several factors, such as inadequate tidal volume, airway obstruction, bullae/hyperinflation of the lung, pneumothorax, pleural effusion/thickening, obesity, and stethoscope quality, can cause diminished or absent breathing sounds [32,33]. Second, by visualizing the presence/absence of pleural movements, lung collapse can be readily identified using point-of-care ultrasound. Moreover, AUC was 0.86 (95% CI: 0.82–0.88) for ultrasound and 0.52 (95% CI, 0.48–0.57) for clinical evaluation. Generally, an AUC of 0.5 indicates no discriminative value of the diagnostic test, while that of 0.8–0.9 denotes good to excellent discriminative power [34]. Accordingly, our meta-analysis was in favor of ultrasound rather than clinical evaluation for confirming the DLT position.
Based on the side of the main bronchus used for the distal opening of the DLT, DLTs can be right- or left-sided. The safe margin is higher for placement of left-sided DLTs than for right-sided DLTs because of the longer left main bronchus. The proximity of the bronchial opening of the right upper lung lobe into the carina (1.5–2 cm) makes the position of right-sided DLTs further challenging and demanding [35]. Right-sided DLTs are less commonly used than left-sided DLTs in clinical practice and only indicated in specific clinical situations, such as pneumonectomy and left lung transplantation [36]. This meta-analysis showed that left-sided DLTs had been used in all studies, except for Hu et al.‘s study [30], in which the accuracy of ultrasound was similar to that of clinical evaluation for confirming left- and right-sided DLTs. However, it was more time-consuming to validate the position of right-sided DLTs compared to that of left-sided DLTs using either method. However, whether or not ultrasound has different diagnostic performance when examining the location of right- or left-sided DLTs requires further investigation.
The patients’ posture may influence the accuracy of confirming the DLT position. In our meta-analysis, the patients might have been in the supine or lateral decubitus position during DLT placement. Hu et al. [30] showed decreased sensitivity with increased specificity under ultrasound assessment from the supine to the lateral decubitus position. However, Park et al. [27] reported that the specificity of ultrasound increased from the supine to lateral decubitus position without changes in its sensitivity. The discrepant outcomes might result from variations in the ultrasound scanning protocol. Furthermore, compared to the supine position, lung compliance would decline in the lateral decubitus position, which also affects the depth of DLT insertion and the results of the assessment.
In this meta-analysis, ultrasound was better than clinical evaluation for checking the DLT position as a potential substitute for FOB. Unlike ultrasonography, FOB can be used to guide the placement of right-sided DLTs to avoid blocking the right upper lobe orifice. Blood and secretions in the lung can be directly aspirated through FOB, which can also be used for intraoperative adjustment of the DLT. During the coronavirus disease pandemic, operators are at an increased risk of exposure to respiratory pathogens during FOB, which is not a concern for ultrasound [24]. Although ultrasound may not be employed to directly visualize the DLT position inside the trachea, it is helpful in evaluating pleural sliding in the ventilated lungs and pulse signs in the non-ventilated lungs. Kanavitoon et al. [29] showed that ultrasound was non-inferior to FOB for confirming the DLT position by inspecting lung collapse during thoracic surgery, which is the gold standard. Therefore, ultrasound was suggested to be included in a stepwise protocol for OLV, whereas FOB was only reserved for difficult or uncertain cases to save time and medical expenses [36]. However, data comparing the diagnostic performances of ultrasound and FOB were insufficient in our meta-analysis, necessitating more prospective trials.
This study has several limitations. First, the number of the studies included in this meta-analysis was small (only eight) and not all enrolled trials used a randomized controlled design. Second, we pooled data from both the supine and lateral decubitus positions in certain studies for the analysis, which might be a potential source of heterogeneity. Another cause of heterogeneity was whether or not there was a prior ultrasound examination before lung isolation. Considering the existence of significant heterogeneity across the included studies, the current meta-analytic result should be interpreted with caution [37]. Third, OLV could be obtained using other airway devices, such as bronchial blockers and univent tubes, but only studies using DLT were included in our meta-analysis [38]. The diagnostic performance of ultrasound over clinical evaluation in assessing the position of other airway devices requires further investigation. Fourth, our meta-analysis revealed that ultrasound assessment may not be less time-consuming than clinical evaluation. Accordingly, standardized, simple ultrasound scanning protocols should be developed to effectively reduce the procedure time. Fifth, in the present meta-analysis, the AUC was estimated by the sROC curve analysis using the parameters (sensitivity/specificity) estimated by the bivariate model [39]. Unlike other outcome variables (sensitivity/specificity), the overall AUC was not pooled from the values of the AUC of the individual studies, which were usually unavailable. It was understandable because the diagnosis of proper or improper positioning of the double lumen tube in the included trials was based on the predefined criteria instead of a sliding/changing threshold. Therefore, I2 for AUC, which needed the individual AUC to compute, could not be provided in our meta-analysis. Sixth, in the enrolled trials, some patients might have benefited from a double assessment, i.e. clinical and then ultrasound, especially in the non-randomized trials (three of the eight). As a result, the performance of ultrasound assessment might be overestimated (if the results of the clinical examination were already known).
6. Conclusion
Compared to clinical evaluation, ultrasound has similar sensitivity but better specificity for confirming the DLT position. Based on an AUC of 0.8–0.9, ultrasound appears to be an acceptable imaging tool for assessing DTL placement for OLV. Data comparing the diagnostic performances of ultrasound and FOB were insufficient in this meta-analysis, and FOB remains the gold standard assessment method for DLT positioning.
Author contribution statement
Po-Kai Wang; Ting-Yu Lin: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Wrote the paper.
I-Min Su; Wei-Ting Wu; Wei-Ting Wu: Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data.
Ke Vin Chang: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Data availability statement
Data included in article/supplementary material/referenced in article.
Funding statement
This work was funded by National Taiwan University Hospital, Bei-Hu Branch; Ministry of Science and Technology (MOST 106-2314-B-002-180-MY3 and 109-2314-B-002-114-MY3); and the Taiwan Society of Ultrasound in Medicine
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper. The authors declare the following financial interests/personal relationships which may be considered as potential competing interests.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.heliyon.2023.e15458.
Appendix A. Supplementary data
The following is the Supplementary data to this article.
References
- 1.Mehrotra M., Jain A. StatPearls. Treasure Island (FL) StatPearls Publishing Copyright © 2022, StatPearls Publishing LLC.; 2022. Single lung ventilation. [Google Scholar]
- 2.Hao D., Saddawi-Konefka D., Low S., Alfille P., Baker K. Placement of a double-lumen endotracheal tube. N. Engl. J. Med. 2021;385(16) doi: 10.1056/NEJMvcm2026684. [DOI] [PubMed] [Google Scholar]
- 3.Levy-Faber D., Malyanker Y., Nir R.R., Best L.A., Barak M. Comparison of VivaSight double-lumen tube with a conventional double-lumen tube in adult patients undergoing video-assisted thoracoscopic surgery. Anaesthesia. 2015;70(11):1259–1263. doi: 10.1111/anae.13177. [DOI] [PubMed] [Google Scholar]
- 4.Onifade A., Lemon-Riggs D., Smith A., et al. Comparing the rate of fiberoptic bronchoscopy use with a video double lumen tube versus a conventional double lumen tube-a randomized controlled trial. J. Thorac. Dis. 2020;12(11):6533–6541. doi: 10.21037/jtd-20-1595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Inoue S., Nishimine N., Kitaguchi K., Furuya H., Taniguchi S. Double lumen tube location predicts tube malposition and hypoxaemia during one lung ventilation. Br. J. Anaesth. 2004;92(2):195–201. doi: 10.1093/bja/aeh055. [DOI] [PubMed] [Google Scholar]
- 6.Cohen E. Double-lumen tube position should be confirmed by fiberoptic bronchoscopy. Curr. Opin. Anaesthesiol. 2004;17(1):1–6. doi: 10.1097/00001503-200402000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Klein U., Karzai W., Bloos F., et al. Role of fiberoptic bronchoscopy in conjunction with the use of double-lumen tubes for thoracic anesthesia: a prospective study. Anesthesiology. 1998;88(2):346–350. doi: 10.1097/00000542-199802000-00012. [DOI] [PubMed] [Google Scholar]
- 8.Brodsky J.B. Lung separation and the difficult airway. Br. J. Addiction: Br. J. Anaesth. 2009;103(suppl_1):i66–i75. doi: 10.1093/bja/aep262. [DOI] [PubMed] [Google Scholar]
- 9.Stahl D.L., Richard K.M., Papadimos T.J. Complications of bronchoscopy: a concise synopsis. Int J Crit Illn Inj Sci. 2015;5(3):189–195. doi: 10.4103/2229-5151.164995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smith G.B., Hirsch N.P., Ehrenwerth J. Placement of double-lumen endobronchial tubes. Correlation between clinical impressions and bronchoscopic findings. Br. J. Anaesth. 1986;58(11):1317–1320. doi: 10.1093/bja/58.11.1317. [DOI] [PubMed] [Google Scholar]
- 11.de Bellis M., Accardo R., Di Maio M., et al. Is flexible bronchoscopy necessary to confirm the position of double-lumen tubes before thoracic surgery? Eur. J. Cardio. Thorac. Surg. 2011;40(4):912–916. doi: 10.1016/j.ejcts.2011.01.070. [DOI] [PubMed] [Google Scholar]
- 12.Seo J.H., Bae J.Y., Kim H.J., Hong D.M., Jeon Y., Bahk J.H. Misplacement of left-sided double-lumen tubes into the right mainstem bronchus: incidence, risk factors and blind repositioning techniques. BMC Anesthesiol. 2015;15:157. doi: 10.1186/s12871-015-0138-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Boucek C.D., Landreneau R., Freeman J.A., Strollo D., Bircher N.G. A comparison of techniques for placement of double-lumen endobronchial tubes. J. Clin. Anesth. 1998;10(7):557–560. doi: 10.1016/s0952-8180(98)00081-6. [DOI] [PubMed] [Google Scholar]
- 14.Álvarez-Díaz N., Amador-García I., Fuentes-Hernández M., Dorta-Guerra R. Comparison between transthoracic lung ultrasound and a clinical method in confirming the position of double-lumen tube in thoracic anaesthesia. A pilot study. Rev. Esp. Anestesiol. Reanim. 2015;62(6):305–312. doi: 10.1016/j.redar.2014.06.005. [DOI] [PubMed] [Google Scholar]
- 15.Parab S.Y., Divatia J.V., Chogle A. A prospective comparative study to evaluate the utility of lung ultrasonography to improve the accuracy of traditional clinical methods to confirm position of left sided double lumen tube in elective thoracic surgeries. Indian J. Anaesth. 2015;59(8):476–481. doi: 10.4103/0019-5049.162983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chang K.V., Wu W.T., Han D.S., Özçakar L. Static and dynamic shoulder imaging to predict initial effectiveness and recurrence after ultrasound-guided subacromial corticosteroid injections. Arch. Phys. Med. Rehabil. 2017;98(10):1984–1994. doi: 10.1016/j.apmr.2017.01.022. [DOI] [PubMed] [Google Scholar]
- 17.Blaivas M., Tsung J.W. Point-of-care sonographic detection of left endobronchial main stem intubation and obstruction versus endotracheal intubation. J. Ultrasound Med. 2008;27(5):785–789. doi: 10.7863/jum.2008.27.5.785. [DOI] [PubMed] [Google Scholar]
- 18.Das S.K., Choupoo N.S., Haldar R., Lahkar A. Transtracheal ultrasound for verification of endotracheal tube placement: a systematic review and meta-analysis. Can. J. Anaesth. 2015;62(4):413–423. doi: 10.1007/s12630-014-0301-z. [DOI] [PubMed] [Google Scholar]
- 19.Farrokhi M., Yarmohammadi B., Mangouri A., et al. Screening performance characteristics of ultrasonography in confirmation of endotracheal intubation; a systematic review and meta-analysis. Arch Acad Emerg Med. 2021;9(1) doi: 10.22037/aaem.v9i1.1360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sustić A., Protić A., Cicvarić T., Zupan Z. The addition of a brief ultrasound examination to clinical assessment increases the ability to confirm placement of double-lumen endotracheal tubes. J. Clin. Anesth. 2010;22(4):246–249. doi: 10.1016/j.jclinane.2009.07.010. [DOI] [PubMed] [Google Scholar]
- 21.Whiting P.F., Rutjes A.W., Westwood M.E., et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann. Intern. Med. 2011;155(8):529–536. doi: 10.7326/0003-4819-155-8-201110180-00009. [DOI] [PubMed] [Google Scholar]
- 22.Borenstein M., Hedges L.V., Higgins J.P., Rothstein H.R. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res. Synth. Methods. 2010;1(2):97–111. doi: 10.1002/jrsm.12. [DOI] [PubMed] [Google Scholar]
- 23.Deeks J.J., Macaskill P., Irwig L. The performance of tests of publication bias and other sample size effects in systematic reviews of diagnostic test accuracy was assessed. J. Clin. Epidemiol. 2005;58(9):882–893. doi: 10.1016/j.jclinepi.2005.01.016. [DOI] [PubMed] [Google Scholar]
- 24.Saporito A., Lo Piccolo A., Franceschini D., Tomasetti R., Anselmi L. Thoracic ultrasound confirmation of correct lung exclusion before one-lung ventilation during thoracic surgery. J Ultrasound. 2013;16(4):195–199. doi: 10.1007/s40477-013-0050-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Coonar A.S., Hughes J.A., Walker S., et al. Implementation of real-time ultrasound in a thoracic surgery practice. Ann. Thorac. Surg. 2009;87(5):1577–1581. doi: 10.1016/j.athoracsur.2008.12.024. [DOI] [PubMed] [Google Scholar]
- 26.Lesser T.G. Significance of thoracic and lung ultrasound in thoracic surgery. Ultraschall der Med. 2017;38(6):592–605. doi: 10.1055/s-0043-119873. [DOI] [PubMed] [Google Scholar]
- 27.Park J.W., Jung K.T., Ki Y.J., Kim S.H. Diagnostic accuracy of auscultation and lung ultrasound in the assessment of adequate double lumen tube position for anesthetic trainee doctors-a single center, prospective study. Med. Biol. Sci. Eng. 2021;4(2):98–105. [Google Scholar]
- 28.Chung J.Y., Go Y., Jang Y.S., Lee B.J., Seo H. Lung sonography can improve the specificity of determination of left-sided double-lumen tracheal tube position in both novices and experts: a randomised prospective study. J. Int. Med. Res. 2020;48(10) doi: 10.1177/0300060520964369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kanavitoon S., Raksamani K., Troy M.P., et al. Lung ultrasound is non-inferior to bronchoscopy for confirmation of double-lumen endotracheal tube positioning: a randomized controlled noninferiority study. BMC Anesthesiol. 2022;22(1):168. doi: 10.1186/s12871-022-01707-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hu W.C., Xu L., Zhang Q., Wei L., Zhang W. Point-of-care ultrasound versus auscultation in determining the position of double-lumen tube. Medicine (Baltim.) 2018;97(13) doi: 10.1097/MD.0000000000009311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Parab S.Y., Kumar P., Divatia J.V., Sharma K. A prospective randomized controlled double-blind study comparing auscultation and lung ultrasonography in the assessment of double lumen tube position in elective thoracic surgeries involving one lung ventilation at a tertiary care cancer institute. Korean J Anesthesiol. 2019;72(1):24–31. doi: 10.4097/kja.d.17.00081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sarkar M., Madabhavi I., Niranjan N., Dogra M. Auscultation of the respiratory system. Ann. Thorac. Med. 2015;10(3):158–168. doi: 10.4103/1817-1737.160831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bohadana A., Azulai H., Jarjoui A., Kalak G., Izbicki G. Influence of observer preferences and auscultatory skill on the choice of terms to describe lung sounds: a survey of staff physicians, residents and medical students. BMJ Open Respir Res. 2020;7(1) doi: 10.1136/bmjresp-2020-000564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.El Khouli R.H., Macura K.J., Barker P.B., Habba M.R., Jacobs M.A., Bluemke D.A. Relationship of temporal resolution to diagnostic performance for dynamic contrast enhanced MRI of the breast. J. Magn. Reson. Imag. 2009;30(5):999–1004. doi: 10.1002/jmri.21947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Benumof J.L., Partridge B.L., Salvatierra C., Keating J. Margin of safety in positioning modern double-lumen endotracheal tubes. Anesthesiology. 1987;67(5):729–738. doi: 10.1097/00000542-198711000-00018. [DOI] [PubMed] [Google Scholar]
- 36.Ashok V., Francis J. A practical approach to adult one-lung ventilation. BJA Educ. 2018;18(3):69–74. doi: 10.1016/j.bjae.2017.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ioannidis J.P., Patsopoulos N.A., Evangelou E. Uncertainty in heterogeneity estimates in meta-analyses. BMJ. 2007;335(7626):914–916. doi: 10.1136/bmj.39343.408449.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Adler A.C. Extraluminal use of a pediatric bronchial blocker with confirmation by point-of-care ultrasound: a case report. In Pract. 2019;13(1):13–16. doi: 10.1213/XAA.0000000000000970. [DOI] [PubMed] [Google Scholar]
- 39.Dwamena B. 2009. MIDAS: Stata Module for Meta-Analytical Integration of Diagnostic Test Accuracy Studies. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data included in article/supplementary material/referenced in article.