Abstract
Purpose
The COVID-19 pandemic has been associated with a decline in mental health of adolescents. The aim of this study was to analyze the rate of deliberate self-poisonings (DSPs) among adolescents reported to the Dutch Poisons Information Center before and during the COVID-19 pandemic.
Methods
A retrospective study from 2016 until 2021 was performed to characterize DSPs among adolescents, and to analyze trends in the number of DSPs. All DSPs among adolescents with the age of 13 up to and including 17 years were included. DSP characteristics included: age, gender, bodyweight, used substance, dose, and treatment advice. Trends in the number of DSPs were analyzed using time series decomposition and Seasonal Autoregressive Integrated Moving Average models.
Results
Six thousand nine hundred fifteen DSPs in adolescents were recorded from January first 2016 until December 31st 2021. Females were involved in 84% of adolescent DSPs. A strong increase in the number of DSPs was observed in 2021 (45% increase compared to 2020), which deviated from the predicted trend based on previous years. This increase was most prominent in 13-, 14-, and 15-year-old female adolescents. Commonly involved drugs were paracetamol, ibuprofen, methylphenidate, fluoxetine, and quetiapine. The contribution of paracetamol rose from 33% in 2019 to 40% in 2021.
Discussion
The strong increase in the number of DSPs during the second year of the COVID-19 pandemic suggests that long-term containment measures such as quarantines, lockdowns, and school closures may enhance self-harm behavior among adolescents, especially among younger females (13–15 years of age), with a preference for paracetamol as DSP substance.
Keywords: Adolescent, COVID-19, Deliberate, Intoxication, Overdose, Pandemic, Self-harm, Self-poisoning
Implications and Contribution.
The COVID-19 pandemic has been associated with a decline in mental health of adolescents. This study supports this association by showing a considerable increase in deliberate self-poisonings reported to the Dutch Poisons Information Center, predominantly among female adolescents, during the second year of the COVID-19 pandemic. This increase was especially prominent in younger adolescents (13–15 years). Over-the-counter analgesics paracetamol and ibuprofen were most often used in deliberate self-poisonings among adolescents.
The COVID-19 pandemic has been associated with a decline in mental health, in particular in adolescents and young adults. This may be due to measures taken to limit the spread of the SARS-CoV-2 virus, such as quarantines, lockdowns, and school closures. In the Netherlands, mitigation measures started in March 2020, with a general lockdown preventing children and adolescents to enter school, sport clubs, or other social gatherings. This was followed by strict and less strict measures alternating until the first quarter of 2022. Early studies showed a COVID-19 pandemic-related decrease in social interactions, and an increase in depression and anxiety in adolescents and young adults [1,2]. Such effects could translate into an increase in self-harm behavior, including deliberate self-poisonings (DSPs).
In Western society, DSP is the predominant method by which adolescents intentionally harm themselves [[3], [4], [5], [6], [7], [8], [9], [10], [11], [12], [13], [14]]. Over-the-counter (OTC) analgesics, in particular paracetamol and ibuprofen, are the predominant substances used for DSPs by adolescents, followed by antidepressants and sedatives/hypnotics [[6], [7], [8], [9],15]. The preferred DSP substances may differ between boys and girls, with girls predominantly using analgesics, and boys more prone to using sedatives, hypnotics and/or antipsychotics [9]. Several risk factors for DSPs among adolescents have been described: female gender [[7], [8], [9], [10], [11],[15], [16], [17]], older age [9,10,15], school terms/school pressure [7,15], and socio-economic deprivation [18].
Only a few reports have been published studying the effect of the COVID-19 pandemic on DSP rate among adolescents. In the United States, data from the Poisons Control Centers' National Poison Data System showed an increase in the proportion of adolescent intentional exposures with a suicide intent during the first 1.5 year of the COVID-19 pandemic compared to the prepandemic period, with a higher proportion of patients with moderate/major clinical effects and deaths [19]. The data of the French National Database of Poisonings showed a strong increase in DSPs among 12–24-year-olds starting halfway through the first year of the COVID-19 pandemic, particularly among females, although no distinction was made between adolescents and young adults [20]. In neither of these studies an adolescent-specific trend analysis including the first 2 years of the pandemic was performed, nor were specific age groups analyzed separately.
The aim of the present study was a) to analyze trends in the number of adolescent DSPs reported to the Dutch Poisons Information Center (DPIC), comparing the first 2 years of the COVID-19 pandemic (2020–2021) with the prepandemic years 2016–2019, and b) to further characterize these DSPs in terms of demographics and exposure type.
Materials and Methods
Study design and patient population
A retrospective analysis of adolescent DSPs reported to the DPIC from January first 2016 until December 31st 2021was performed, covering 2 years of the COVID-19 pandemic (In the Netherlands, March 11th 2020 is regarded as the starting date of the COVID-19 pandemic). Data were subtracted from the DPIC's database, which consists of inquiries received by telephone from Dutch health care professionals about acute intoxications. In this database, anonymous case information is recorded using a standard data format, to ensure uniform data collection. Inquiries involving adolescents (from 13 to and including 17 years old) who exposed themselves to substances with the (suspected) intent of self-harm were included. Exposures to drugs of abuse or alcohol with no clear intent of self-harm were excluded. Accidental exposures, for instance medication errors, were also excluded. Cases were assessed against the inclusion and exclusion criteria by three authors and any disagreements were resolved through consensus. For each DSP, the following parameters were registered: date and time of the inquiry, patient characteristics (age, gender, and bodyweight), exposure characteristics (involved substance, dose, route, day of exposure), intent (accidental/intentional), symptoms at the time of DPIC consultation, and treatment advice. Multiple inquiries regarding the same patient and same exposure(s) were analyzed as a single case. The monthly and yearly number of DSPs and the DSP rate (number of monthly adolescent DSPs relative to total monthly number of received inquiries about human intoxications) were determined. The DSP rate was included to rule out that possible trends among adolescents were caused by overall changes in the total number of inquiries to the DPIC (regardless of age). In addition, data regarding the total number of adolescents living in the Netherlands from 2016 until 2021 was obtained from the Central Office for Statistics [21] and was compared to trends in adolescent DSPs reported to the DPIC.
The Dutch Medical Research Involving Human Subjects Act did not apply to this retrospective cohort study, since the obtained information was anonymous and not traceable to personal data.
Statistical analyzes
Descriptive statistics (percentage, median, interquartile range) were used to provide an overview of patient characteristics (e.g., age, gender), exposure characteristics (e.g., type of exposures), and treatment advice. Analyzes were conducted using IBM SPSS Statistics (version 26.0.0.1; IBM, Armonk, NY) and R studio version 2022.12.0 for Windows (R version 4.2.2; Boston, MA). The DSP rate over time was considered as a time series with the “ts” function in R and decomposed into three components (“trend,” “seasonal,” and “random”). After removing the trend of the time series, we fitted a Seasonal Autoregressive Integrated Moving Average (SARIMA) model on prepandemic data in the Netherlands (2016–February 2020). Normality of the residuals and goodness of fit of the model were checked. This SARIMA model was used to predict what the DSP rate would have been in 2021–2022 without a pandemic (with 95% confidence intervals). Observed DSP rate and DSP rate predicted by the SARIMA model were compared. For further information, see the supplementary data. Further, we considered the time series of DSP rates separately for school days and weekend days. The average number of DSPs per school day (Monday–Friday) and weekend day (Saturday–Sunday) was calculated for each month. Since the pattern and seasonal effects were similar for the average number of DSPs during school days and weekend days, a paired t test was performed to compare both types of days. Finally, we also analyzed the time series of DSP rates separately for girls and boys. Chi-square tests (IBM SPSS 26.0.0.1) were performed in order to compare the DPIC's treatment advice between DSPs with and without paracetamol.
Dutch poisons information center procedure and definitions
The DPIC provides a 24/7 telephone service giving expert advice to Dutch health care professionals on the diagnosis and treatment of patients exposed to potentially toxic substances. Advice can be requested on a voluntary basis whenever needed. The term “exposure” is defined as an actual or suspected contact with any substance through ingestion, inhalation, absorption, application to, or injection into the body. A mono-intoxication is defined as contact with only one substance, whereas a multi-intoxication is defined as contact with two or more substances. Not all exposures reported to the DPIC result in toxic effects, since this depends on the dose the patient has been exposed to. For each patient, the DPIC performs a risk assessment, based on reported dose of exposure (mg/kg) and symptoms at the time of DPIC consultation, resulting in one of the following types of treatment advice (based on a pure medical toxicological point of view): observation at home (when estimated to be no or a mild intoxication) or further medical examination by a physician, followed by hospital observation if necessary (when estimated to be a potentially moderate/severe intoxication). Obviously, observation in a hospital or psychiatric institution could also be warranted because of psychiatric reasons; in the Netherlands, this judgment is made by the patient's physician (e.g., general practitioner or emergency physician).
Results
Patient characteristics and trend analysis
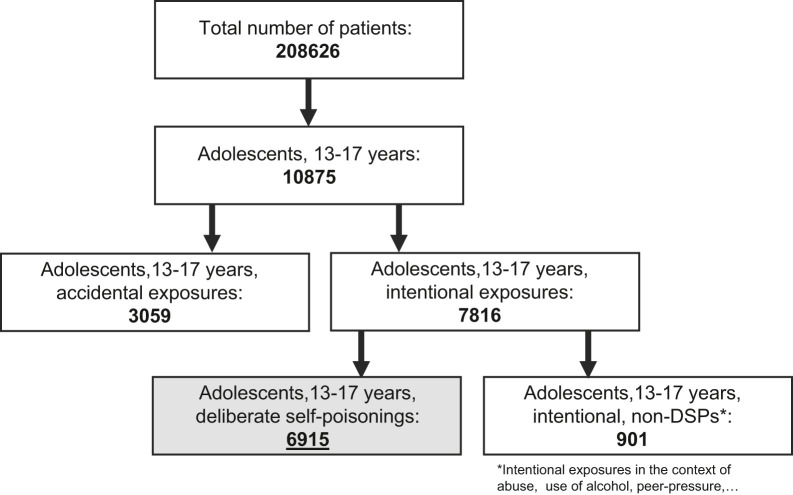
From January first 2016 until December 31st 2021 the DPIC received a total of 208,626 inquiries concerning acute human intoxications. A total number of 10,875 inquiries involved adolescents of 13 to and including 17 years of age, of which 6,915 were included as adolescent DSP (Figure 1 ). Eighty-four percent of the DSPs involved female adolescents (Table A1). The median age of both adolescent males and females was 16 years (interquartile range 15–17 years). The time series decomposition showed a general trend; the monthly number of DSPs slowly increased between 2016 and mid-2018, then decreased from 2019 to mid-2020, followed by an abrupt increase from mid-2020. The observed DSP rate well exceeded the 95% confidence interval of the DSP rate predicted by the SARIMA model in March and November 2021 (Figure 2 , Figure A1A). The number of DSPs increased with 45% in 2021 compared to 2020 (n = 1,512 vs. n = 1,044, respectively, Table A1). The increase in DSP rate was much higher among girls than among boys, with an increase of 50% for girls versus 20% for boys in 2021 compared to 2020 (Table A1 and Figure A1B). Hence, as further confirmed by the SARIMA model (data not shown), the overall increase in adolescent DSPs was mainly attributable to the increase in female adolescent DSPs. Moreover, the increase was most prominent among 13-, 14-, and 15-years olds (49%, 75%, and 77% increase (2021 vs. 2020) respectively), although the number of DSPs also increased among 16- and 17-year old adolescents (27% and 21% increase (2021 vs. 2020), respectively) (Table A1, Figures A1C and D). The total number of DPIC consultations (regardless of age) did not increase during this period (Figure A1C).
Figure 1.
Patient selection flowchart, covering all inclusions from January first 2016 until December 31st 2021.
Figure 2.
Trends in DSPs by adolescents. (A) SARIMA model of expected rate of DSPs in 2021. The red line represents the percentage of adolescent DSPs relative to the total number of patients reported to the DPIC, per month. The blue line represents the expected percentage of adolescent DSPs from March 2020 onward. CI = confidence interval. (B) DSP rates for girls and boys. Each dot represents the monthly DSP rate (percentage of male (gray circles) or female (black circles) adolescent DSPs in a particular month relative to the total number of patients reported to the DPIC in that month). Dotted lines represent fourth order polynomial trend lines.
Furthermore, a clear seasonal effect was observed, with lower numbers of DSPs in July and August. Interestingly, the number of DSPs was also dependent on the day of the week: throughout the study period, the frequency of DSPs during weekend days was generally lower than during school days (paired t test, p value < .001) (Figure A1E), with Monday displaying the highest frequency of DSPs and Saturday the lowest (Figure A1F). Taken together, our data show a strong increase in the number of adolescent DSPs starting in the second half of the first year of the COVID-19 pandemic, and continuing in the second year.
Characteristics of substances used in deliberate self-poisonings
Approximately two-thirds (n = 4,828, 70%) of DSPs involved exposure to a single substance (mono-intoxication) and one-third (n = 2,087, 30%) comprised DSPs with exposure to two or more substances (multi-intoxication) (Table A1). The most commonly used substances were paracetamol, ibuprofen, and methylphenidate, covering 36%, 14%, and 7% of all adolescent DSPs in 2016–2021 (Figure 3 A). The proportion of paracetamol involved in DSPs increased from 32% in 2019 to 40% in 2021 (Figure 3B). The ratio of the number of DSPs with single substance versus multi-substance exposure was age-dependent (Figure A2A). Younger adolescents (13 and 14 years of age) displayed a higher frequency of single substance exposures compared to older adolescents (16 and 17 years of age). Use of the various substances changed with age. For instance, the use of paracetamol in DSPs was highest among 13- and 14-year-old adolescents (42%), but decreased to 30% in 17-year-olds. Older adolescents tended to use prescription drugs more often (e.g., fluoxetine, sertraline, quetiapine, oxazepam, and lorazepam) compared to younger adolescents (Figure A2B), although paracetamol use was still dominant. In addition, the preference for the type of pharmaceutical differed between boys and girls. Paracetamol and ibuprofen were involved in 38% and 16% of all DSPs in females, respectively, compared to 25% and 8% of all DSPs in males (Figure A2C). In contrast, methylphenidate was used considerably more often in DSPs by boys (12% in boys, vs. 6% in girls).
Figure 3.
Substances used in DSPs by adolescents. (A) Fifteen most frequently used substances during 2016–2021 as percentage of the total number of DSPs in 2016–2021. (B) Annual contribution of the five most frequently used substances in DSPs as percentage of the total number of DSPs in a particular year.
Treatment advice
Since follow-up data are not routinely registered by the DPIC, it is not possible to report the clinical outcome and severity of the DSPs. As alternative, the treatment advice given by the DPIC, which is based on the estimated severity of the DSP, was further analyzed. During the period 2016–2021, 51% of adolescents were advised to be observed at home (estimated low risk for serious clinical effects), whereas in 49% of the cases medical examination or hospital observation was advised (estimated high risk for serious clinical effects). During the period 2016–2020, the annual proportion of patients with the advice “medical examination or hospital observation” varied between 46% and 50%. In 2021 this proportion increased to 54%, suggesting a larger share of DSPs with an estimated risk of serious clinical effects (Figure A1D). Moreover, DSPs with paracetamol were more likely to result in the advice “medical examination or hospital observation” compared to DSPs without paracetamol (Chi-square, df = 1, 82.28, p value < .001), suggesting that DSPs with paracetamol may have a higher risk of serious clinical effects.
Discussion
In this study, a strong increase in the number of adolescent DSPs was observed during the COVID-19 pandemic, starting halfway through the year 2020, particularly among young female adolescents (13–15 years old). Predominant substances used in DSPs were OTC analgesics (paracetamol, ibuprofen), of which paracetamol showed an increase in its contribution to DSPs in 2021. Moreover, the proportion of DSPs estimated to cause a more serious clinical course increased in 2021. These observations suggest a strong effect of the COVID-19 pandemic on self-harm behavior through self-poisoning, predominantly by young females.
An important but difficult to answer question is if there is a causal relation between the observed increase in adolescent DSPs, especially among females, and the COVID-19 pandemic. Similar to most parts of the world, several measures were taken in the Netherlands during the COVID-19 pandemic to mitigate the spread of the SARS-CoV-2 virus, including social distancing, general lockdowns, and curfews. Far-reaching socially isolating measures could have a profound effect on mental wellbeing of adolescents, although recent studies show conflicting results. Several studies have shown signs of deteriorating mental health among adolescents during the COVID-19 pandemic [20,[22], [23], [24], [25], [26], [27], [28], [29], [30], [31], [32]], whereas studies from the Netherlands, Sweden, and Canada showed no difference or even a decrease in the incidence of mental health problems in 2020 compared to pre-COVID-19 years in adolescents [[33], [34], [35], [36], [37]]. Since most of these studies were conducted within the first year of the COVID-19 pandemic, the study period could have been too short to observe robust changes in mental health. Moreover, country-specific differences in mitigation measures may also affect study outcomes. A large Dutch study conducted in October 2021–January 2022 among adolescents showed that the life satisfaction and emotional wellbeing had declined considerably, especially among girls, compared to the previous reference year 2017 [38]. This suggests that socially isolating measures that were prolonged up to the second year of the pandemic may have had more impact. Moreover, this study emphasizes that boys and girls may react differently on social and societal stressors.
Despite the unclear picture of the impact of the COVID-19 pandemic on adolescent mental health, a limited number of studies have shown a relation between the COVID-19 pandemic and increases in adolescent DSP rate. A recent study by Wang et al., in which prepandemic adolescent exposure calls received by US poison centers were compared with those of the first 1.5 years of the COVID-19 pandemic, showed a considerable increase in the proportion of intentional exposures with a suicide intent [19]. Moreover, there was an increase in the proportion of adolescents requiring hospital admission and in the proportion of moderate/major clinical effects and mortality. These data are in line with our data which show an increase in adolescent DSPs with a potentially more severe outcome (with the advice of further medical examination or hospital observation). Another similarity between this study and ours was the observation that the proportion of calls involving OTC analgesics increased during the pandemic. Two additional US studies, based on poison center calls during the first year of the COVID-19 pandemic, further confirmed the increase in DSPs among adolescents [39,40]. In Europe, limited data have been published regarding adolescent DSPs during the COVID-19 pandemic. In a study by Jollant et al., suicide attempts reported to French poison centers until 31st May 2022 were analyzed for different age groups, including 12–24 year olds [20]. French measures to mitigate the SARS-CoV-2 virus were comparable with Dutch measures, with a number of lengthy lockdowns and curfews, although the last curfew in France ended in June 2021, while the last lockdown in the Netherlands ended in February 2022. Especially among young females (12–24 years old) an increase in DSPs was observed in France, starting in the second half of 2020. This observation is in line with our data, although we further differentiated between different ages within the age group 13–17 years. This differentiation showed that the increase in DSPs was stronger among younger adolescents. As with the study of Jollant et al., our study showed gender-specific trends, with a strong increase in the number of female DSPs. This gender-specific effect is in line with the aforementioned study by Boer et al., which observed a decline in the mental wellbeing in 2021, mainly among girls 2021 [38]. Moreover, the general observation that girls are more often involved in DSPs than boys, has been shown previously [11,15]. The onset of the increase in DSP number (starting halfway 2020) was comparable between France and the Netherlands, which may be explained by the corresponding timing of measures taken to limit the spread of the SARS-CoV-2 virus.
A large share of OTC medication in DSPs among adolescents has been shown before [6,7,9,11,15,19]. Such drugs are easily accessible and are often available at home for general use. At therapeutic dose, paracetamol is regarded as a relatively safe analgesic with little adverse effects. However, acute and chronic overdose can result in (severe) liver damage, if not treated correctly [41]. Our data show that the proportion of adolescent DSPs involving paracetamol increased during the COVID-19 pandemic, probably due to the increase of younger adolescents involved in DSPs who predominantly use paracetamol. Moreover, our data suggest that DSPs with paracetamol may have a higher risk of serious clinical effects compared to DSPs without paracetamol. These observations raises the question whether m measures should be required to limit the access to paracetamol, but also other drugs involved in DSPs,. Preventive measures could include limiting dispensing of prescription medication to adolescents and restricting the sale of OTC medication to adolescents. In addition, indirect measures to prevent self-harm could be considered. For instance, early identification, assessment and treatment of adolescents with possible suicidal behavior may help to prevent DSPs. Practitioners, parents/caregivers, and teachers could be educated to pick up warning signs of suicidal behavior. Easy access to mental health care and losing the stigma associated with asking for mental care may be important as well [10]. Finally, societal stress factors underlying the general deterioration of mental wellbeing of adolescents may be addressed. In our study the frequency of DSPs was higher during schooldays and lower during the months of summer holidays, suggesting that school-related stress may be a risk factor for self-harm behavior. Programs to mitigate school-related stress, e.g., stress to perform or stress as result of bullying, may help to improve the mental wellbeing of adolescents.
Limitations
This retrospective study has a number of limitations. First, our data are subject to under-reporting. Health care professionals are not obliged to contact the DPIC in case of a DSP, resulting in an underestimation of the number of DSPs among adolescents in the Netherlands. Second, health care professionals may be more inclined to consult a Poison Control Center when they expect a more severe outcome of the DSP, which could lead to an overrepresentation of DSPs with the advice to medically examine or observe the patient in hospital. Third, the anamnesis regarding the exposure is usually based on self-reporting by the patient. Exposures are generally not analytically confirmed. Fourth, since patient data are anonymous, it is not possible to indicate whether individuals have been included in the study multiple times due to multiple DSPs. Fifth, in almost every case the final medical outcome of the DSP is unknown, since the DPIC does not routinely conduct follow up. Finally, in a small subset of cases (approximately 2%) the true intent of the patient was not clear. In these cases inclusion was based on exposure scenario.
Conclusion
The second year of the COVID-19 pandemic (2021) showed a strong increase in DSPs among adolescents, especially among girls and 13-, 14-, and 15- year-old children. Adolescent DSPs predominantly involved the OTC analgesics paracetamol and ibuprofen, of which the share of paracetamol showed a disproportional increase during the COVID-19 pandemic. Measures should be considered to limit access to OTC medication and prescription drugs. These measures may include restriction of the sale and dispensing of drugs to adolescents, or limiting the availability of these drugs at home. Our data suggest that social and societal stressors associated with pandemics may have an impact on self-poisoning behavior among adolescents, especially among younger girls.
Footnotes
Conflicts of interest: The authors have no conflicts of interest to disclose.
Supplementary data related to this article can be found at 10.1016/j.jadohealth.2023.02.041.
Supplementary Data
References
- 1.Giuntella O, Hyde K, Saccardo S, et al. Lifestyle and mental health disruptions during COVID-19. Proc Natl Acad Sci U S A. 2021:118. doi: 10.1073/pnas.2016632118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cohen ZP, Cosgrove KT, DeVille DC, et al. The impact of COVID-19 on adolescent mental health: Preliminary findings from a longitudinal sample of healthy and at-risk adolescents. Front Pediatr. 2021;9 doi: 10.3389/fped.2021.622608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Griffin E, McMahon E, McNicholas F, et al. Increasing rates of self-harm among children, adolescents and young adults: A 10-year national registry study 2007-2016. Soc Psychiatry Psychiatr Epidemiol. 2018;53:663–671. doi: 10.1007/s00127-018-1522-1. [DOI] [PubMed] [Google Scholar]
- 4.Beckman K, Mittendorfer-Rutz E, Waern M, et al. Method of self-harm in adolescents and young adults and risk of subsequent suicide. J Child Psychol Psychiatry. 2018;59:948–956. doi: 10.1111/jcpp.12883. [DOI] [PubMed] [Google Scholar]
- 5.Morgan C, Webb RT, Carr MJ, et al. Incidence, clinical management, and mortality risk following self harm among children and adolescents: Cohort study in primary care. BMJ. 2017;359:j4351. doi: 10.1136/bmj.j4351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cairns R, Karanges EA, Wong A, et al. Trends in self-poisoning and psychotropic drug use in people aged 5-19 years: A population-based retrospective cohort study in Australia. BMJ Open. 2019;9 doi: 10.1136/bmjopen-2018-026001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Froberg BA, Morton SJ, Mowry JB, et al. Temporal and geospatial trends of adolescent intentional overdoses with suspected suicidal intent reported to a state poison control center. Clin Toxicol (Phila) 2019;57:798–805. doi: 10.1080/15563650.2018.1554186. [DOI] [PubMed] [Google Scholar]
- 8.Gilley M, Sivilotti MLA, Juurlink DN, et al. Trends of intentional drug overdose among youth: A population-based cohort study. Clin Toxicol (Phila) 2020;58:711–715. doi: 10.1080/15563650.2019.1687900. [DOI] [PubMed] [Google Scholar]
- 9.Overall B, Hon SL, Jones A, et al. Intentional suspected suicide exposures by poisoning among adolescents from 2009 to 2018 reported to the Georgia Poison Center and compared nationally. Basic Clin Pharmacol Toxicol. 2021;128:699–708. doi: 10.1111/bcpt.13563. [DOI] [PubMed] [Google Scholar]
- 10.Spiller HA, Ackerman JP, Spiller NE, et al. Sex- and age-specific increases in suicide attempts by self-poisoning in the United States among youth and young adults from 2000 to 2018. J Pediatr. 2019;210:201–208. doi: 10.1016/j.jpeds.2019.02.045. [DOI] [PubMed] [Google Scholar]
- 11.Daly C, Griffin E, McMahon E, et al. Paracetamol-related intentional drug overdose among young people: A national registry study of characteristics, incidence and trends, 2007-2018. Soc Psychiatry Psychiatr Epidemiol. 2021;56:773–781. doi: 10.1007/s00127-020-01981-y. [DOI] [PubMed] [Google Scholar]
- 12.Toce MS, Hudgins JD, Yuskaitis CJ, et al. National assessment of anti-epileptic drug exposures among pre-teens and adolescents, 2000-2020. Clin Toxicol (Phila) 2022 doi: 10.1080/15563650.2021.2023747. [DOI] [PubMed] [Google Scholar]
- 13.Friedrich JM, Sun C, Geng X, et al. Child and adolescent benzodiazepine exposure and overdose in the United States: 16 years of poison center data. Clin Toxicol (Phila) 2020;58:725–731. doi: 10.1080/15563650.2019.1674321. [DOI] [PubMed] [Google Scholar]
- 14.Whitely M., Raven M., Jureidini J. Antidepressant Prescribing and suicide/self-harm by young Australians: Regulatory warnings, Contradictory advice, and long-term trends. Front Psychiatry. 2020;11:478. doi: 10.3389/fpsyt.2020.00478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Spiller HA, Ackerman JP, Smith GA, et al. Suicide attempts by self-poisoning in the United States among 10-25 year olds from 2000 to 2018: Substances used, temporal changes and demographics. Clin Toxicol (Phila) 2020;58:676–687. doi: 10.1080/15563650.2019.1665182. [DOI] [PubMed] [Google Scholar]
- 16.Tyrrell E.G., Orton E., Tata L.J. Changes in poisonings among adolescents in the UK between 1992 and 2012: A population based cohort study. Inj Prev. 2016;22:400–406. doi: 10.1136/injuryprev-2015-041901. [DOI] [PubMed] [Google Scholar]
- 17.Qin P, Sun S, Boe AS, et al. Injuries prior and subsequent to index poisoning with medication among adolescents: A national study based on Norwegian patient registry. BMC Psychiatry. 2018;18:200. doi: 10.1186/s12888-018-1778-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pawer S, Rajabali F, Zheng A, et al. Analyses of child and youth self-poisoning hospitalizations by substance and socioeconomic status. Int J Environ Res Public Health. 2021;18:7003. doi: 10.3390/ijerph18137003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang GS, Leonard J, Cornell A, et al. Adolescent US poison center exposure calls during the COVID-19 pandemic. J Adolesc Health. 2022;71:764–767. doi: 10.1016/j.jadohealth.2022.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jollant F, Blanc-Brisset I, Cellier M, et al. Temporal trends in calls for suicide attempts to poison control centers in France during the COVID-19 pandemic: A nationwide study. Eur J Epidemiol. 2022;37:901–913. doi: 10.1007/s10654-022-00907-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.CBS. Statistics Netherlands - Centraal Bureau voor de Statistiek (CBS). Available at: www.cbs.nl. Accessed October 4, 2022.
- 22.Bortoletto R, Di Gennaro G, Antolini G, et al. Sociodemographic and clinical changes in pediatric in-patient admissions for mental health emergencies during the COVID-19 pandemic: March 2020 to June 2021. Psychiatry Res Commun. 2022;2 doi: 10.1016/j.psycom.2022.100023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Leith T, Brieger K, Malas N, et al. Increased prevalence and severity of psychiatric illness in hospitalized youth during COVID-19. Clin Child Psychol Psychiatry. 2022;27:804–812. doi: 10.1177/13591045221076889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Saunders NR, Kurdyak P, Stukel TA, et al. Utilization of physician-based mental health care services among children and adolescents before and during the COVID-19 pandemic in Ontario, Canada. JAMA Pediatr. 2022;176 doi: 10.1001/jamapediatrics.2021.6298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Werling AM, Walitza S, Eliez S, et al. The impact of the COVID-19 pandemic on mental health care of children and adolescents in Switzerland: Results of a survey among mental health care professionals after one year of COVID-19. Int J Environ Res Public Health. 2022;19:3252. doi: 10.3390/ijerph19063252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Radhakrishnan L, Leeb RT, Bitsko RH, et al. Pediatric Emergency Department visits associated with mental health conditions before and during the COVID-19 pandemic - United States, January 2019-January 2022. MMWR Morb Mortal Wkly Rep. 2022;71:319–324. doi: 10.15585/mmwr.mm7108e2. [DOI] [PubMed] [Google Scholar]
- 27.Edgcomb JB, Benson NM, Tseng CH, et al. Mental health-related emergency department visits among children during the early COVID-19 pandemic. Psychiatr Res Clin Pract. 2022;4:4–11. doi: 10.1176/appi.prcp.20210036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kim MJ, Paek SH, Kwon JH, et al. Changes in suicide rate and characteristics according to age of suicide attempters before and after COVID-19. Children (Basel) 2022;9:151. doi: 10.3390/children9020151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Racine N, McArthur BA, Cooke JE, et al. Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: A meta-analysis. JAMA Pediatr. 2021;175:1142–1150. doi: 10.1001/jamapediatrics.2021.2482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.De France K, Hancock GR, Stack DM, et al. The mental health implications of COVID-19 for adolescents: Follow-up of a four-wave longitudinal study during the pandemic. Am Psychol. 2022;77:85–99. doi: 10.1037/amp0000838. [DOI] [PubMed] [Google Scholar]
- 31.Knowles G, Gayer-Anderson C, Turner A, et al. Covid-19, social restrictions, and mental distress among young people: A UK longitudinal, population-based study. J Child Psychol Psychiatry. 2022;63:1392–1404. doi: 10.1111/jcpp.13586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Theberath M, Bauer D, Chen W, et al. Effects of COVID-19 pandemic on mental health of children and adolescents: A systematic review of survey studies. SAGE Open Med. 2022;10 doi: 10.1177/20503121221086712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.van der Velden PG, van Bakel HJA, Das M. Mental health problems among Dutch adolescents of the general population before and 9 months after the COVID-19 outbreak: A longitudinal cohort study. Psychiatry Res. 2022;311 doi: 10.1016/j.psychres.2022.114528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chen Y, Osika W, Henriksson G, et al. Impact of COVID-19 pandemic on mental health and health behaviors in Swedish adolescents. Scand J Public Health. 2022;50:26–32. doi: 10.1177/14034948211021724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bouter DC, Zarchev M, de Neve-Enthoven NGM, et al. A longitudinal study of mental health in at-risk adolescents before and during the COVID-19 pandemic. Eur Child Adolesc Psychiatry. 2022 doi: 10.1007/s00787-021-01935-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ray JG, Austin PC, Aflaki K, et al. Comparison of self-harm or overdose among adolescents and young adults before vs during the COVID-19 pandemic in Ontario. JAMA Netw Open. 2022;5 doi: 10.1001/jamanetworkopen.2021.43144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.van Loon AWG, Creemers HE, Vogelaar S, et al. Trajectories of adolescent perceived stress and symptoms of depression and anxiety during the COVID-19 pandemic. Sci Rep. 2022;12:15957. doi: 10.1038/s41598-022-20344-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Boer M, Dorsselaer van S, Looze de M, et al. HBSC 2021: Gezondheid en welzijn van jongeren in Nederland. Netherlands: Health Behaviour in School-aged Children (HBSC) consortium. 2022. [Google Scholar]
- 39.Ciccotti HR, Spiller HA, Casavant MJ, et al. Pediatric poison exposures reported to United States poison centers before and during the COVID-19 pandemic. Clin Toxicol (Phila) 2022;60:1299–1308. doi: 10.1080/15563650.2022.2139714. [DOI] [PubMed] [Google Scholar]
- 40.Lelak KA, Vohra V, Neuman MI, et al. COVID-19 and pediatric ingestions. Pediatrics. 2021;148 doi: 10.1542/peds.2021-051001. [DOI] [PubMed] [Google Scholar]
- 41.Dear J., Bateman D. Paracetamol poisoning. Medicine. 2020;48:208–210. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.