Abstract
Background:
Urinary catheters are an important armamentarium of urologic practice. Several indications for their use exist. A good knowledge of the details surrounding every urinary catheter inserted is necessary for the proper management of the patients. Inadequate documentation can lead to complications such as urinary tract infection or even forgotten catheters.
Objectives:
This study aimed at auditing the practice of documentation of urinary catheter parameters in our hospital as a means to improving the standard of care and aligning with international best practices with respect to the use of urinary catheters in our hospital.
Materials and Methods:
This study was a 3-month audit on the quality of documentation on the parameters of each urinary catheter use in Alex Ekwueme Federal University Teaching Hospital, Abakaliki, Ebonyi State, Nigeria. The parameters included the indication for catheterisation, route of catheterisation, staff who catheterised, size of catheter, type of catheter, volume of water used for inflating catheter balloon, volume of urine drained, if aseptic technique was followed during catheterisation, informed consent and complications encountered. Data were summarised as frequencies and means. Statistical significance was pegged at P < 0.05.
Results:
Seventy-four patients were men, whereas two were women. The mean age of the patients was 67.29 ± 15.17 years. Overall, sex (76 [100%]), age (76 [100%]) and route of catheterisation (68 [89.5%]) were the three most commonly documented information. The documentation on complications and volume of fluid instilled to inflate the catheter balloon were the least-documented parameters (6 [7.9%] and 11 [14.5%], respectively). The following parameters were better documented in the SPC arm: The staff who passed the catheter p = 0.000), the type of catheter passed (p = 0.004), asepsis (p = 0.001) and acquisition of informed consent (p = 0.043).
Conclusions:
Documentation following urinary catheter use was noted to be poor in this study. Documentation of catheter parameters was noted to be higher in patients who had SPC than those who had urethral catheterisation.
Keywords: Catheter care, documentation, Nigeria, records, urinary catheter
Introduction
Urinary catheters are an important armamentarium of urologic practice. Several indications for its use exist.[1] A good knowledge and documentation of the details surrounding the catheter inserted in each patient is necessary for the proper management of the patients with this device. As basic as a urinary catheter is, improper use can result in far-reaching consequences. Urinary catheter use in hospitalised patients is a recognised risk factor for urinary tract infection.[2] Other complications include urethral strictures and forgotten catheters.[3,4]
The huge burden of urinary retention in this sub-region requires that proper documentation on the use of this device is paramount if complications associated with its use are to be avoided.[5,6,7,8,9]. Data on the documentation of catheter parameters and guidelines on urinary catheter are sparse in our environment. In developed climes, there is detailed documentation on every urinary catheter inserted and a catheter plan put in place.[10]
The aim of this audit was to describe the quality of documentation of urinary catheter parameters as it relates to patient and catheter parameters. This would serve as a template for improving the practice of medical care and outcome in our hospital.
Materials and Methods
This study was a retrospective 3-month audit (from September 2022 to November 2022) on the quality of documentation of urinary catheter use in Alex Ekwueme Federal University Teaching Hospital, Abakaliki, Ebonyi State, Nigeria. Ethical approval was obtained from the hospital ethics committee (Protocol no. AE-FUTHA/REC/VOL3/2022/138). The hospital is the only referral hospital in the state and serves neighbuoring states of Enugu, Benue, Imo and Abia. It is a 720-bedded multi-specialist tertiary hospital. Patients who were admitted into the emergency department and who were catheterised were included in the study. The case notes of these patients were retrieved for analysis. Data collected included documentation on the age, sex, indication for catheterisation, route of catheterisation, staff who catheterised, size of catheter, type of catheter, volume of water used for inflating catheter balloon, volume of urine drained, if aseptic technique was followed during catheterisation, informed consent and complications encountered. Data were analysed using IBM SPSS Statistics for Windows, version 26.0 (IBM, Armonk, New York). Categorical data were summarized as frequency, whereas continuous data were presented as means and standard deviation. Chi-square test was used to compare categorical data. Statistical significance was pegged at P < 0.05.
Results
A total of 100 patients had a catheter passed during the period of study. Twenty-four patients were excluded due to incomplete data, leaving 76 patients for analysis. Seventy-four patients (97.4%) were men, whereas two (2.6%) were women. The mean age of the patients was 67.29 ± 15.17 years. Overall, sex (76 [100%]), route of catheterisation (68 [89.5%]) and staff who passed the catheter (61 [80.3%]) were the most commonly documented information as shown in Tables 1 and 2. In contrast, the documentation on the volume of fluid used to inflate the balloon in 11 (14.5%) and complications encountered were the least-documented parameters 6 (7.9%), as shown in Tables 1 and 2. Of the complications, five (83.3%) were bleeding with three (60%) of bleeding occurring in patients who had suprapubic cystostomy (SPC), as shown in Figure 1.
Table 1.
Distribution of documentation of catheter parameters
| Catheter | Yes | No |
|---|---|---|
|
| ||
| Parameters | N (%) | N (%) |
| Route of catheterisation | 68 (89.5) | 8 (10.5) |
| Urethral catheter | 52 (68.4) | |
| Suprapubic catheter | 16 (21.1) | |
| Type of catheter | 51 (67.1) | 25 (32.9) |
| Latex | 27 (35.5) | |
| Silicone | 24 (31.6) | |
| Size of urethral catheter | 38 (50) | 38 (50) |
| volume of fluid instilled to inflate the | 11 (14.5) | 65 (85.5) |
| catheter balloon | ||
| Volume of urine drained | 17 (22.4) | 59 (77.6) |
| Asepsis documentation | 14 (18.4) | 62 (81.6) |
| Informed consent | 14 (18.4) | 62 (81.6) |
| Complications | 6 (7.9) | 70 (92.1) |
Table 2.
Documentation on staff who inserted the catheter
| Parameter | N (%) |
|---|---|
| Doctor | 53 (69.7) |
| Nurse | 8 (10.5) |
| No documentation | 15 (19.7) |
Figure 1.
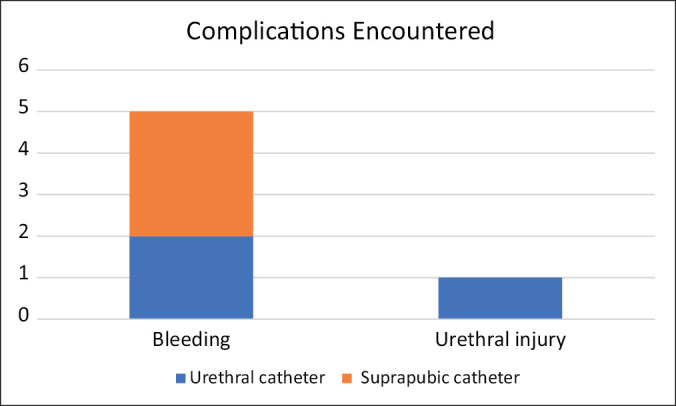
Bar chart showing the complications documented (n = 6)
The indications were documented in 65.8% of patients who were catheterised with benign prostatic enlargement being the most common indication as shown in Table 3. Patients who had SPC had most of the parameters documented as compared with the patients who had urethral catheterization, and these were statistically significant; The following parameters were better documented in the SPC arm: The staff who passed the catheter (p = 0.000), the type of catheter passed (p = 0.004), asepsis (p = 0.001) and acquisition of informed consent (p = 0.043).
Table 3.
Indications for catheter use
| Indications | N (%) |
|---|---|
| Benign prostate enlargement | 21 (27.6) |
| Urethral stricture disease | 7 (9.21) |
| Incontinence | 1 (1.3) |
| Cancer of the prostate | 21 (27.6) |
| No documentation | 26 (34.2) |
Discussion
Urinary catheters have varied uses and come in handy when urinary diversion is needed. If used wrongly, complications may arise.[11] Documentation on their use ensures that these catheters are appropriately used and that information about the catheter being worn by a patient can be safely communicated to the next managing physician.[12] In addition, documentation also helps in identifying faulty urethral catheter brands or batches, and when this occurs, these brands can be withdrawn from use.
All patients in this study had the data on gender and age already documented. This was notably so because the data were already documented by the health records in the process of registering the patients.
Approximately 55% of the documented indications for urinary catheterisation in this study were urinary retention due to prostate-related pathologies. This finding lays credence to the high prevalence of urinary retention due to prostate diseases in this sub-region reported by earlier authors.[5,8] This huge burden of urinary retention underscores the importance of proper documentation of details surrounding the insertion of urinary catheters.
The volume of urine drained and volume of water used to inflate the catheter balloon were the least recorded. Tijani et al.[13] in Lagos also noted a low rate on the documentation on the volume of water used to inflate catheter balloon and informed consent of their study population. The urinary catheters available in Nigeria do not come with the easy-peel-off sticky labels that usually contain catheter details; this may explain the paucity of documentation. Another reason for this may revolve around the lack of manpower, too many patients to cater for and other regional challenges bedevilling the healthcare system in this region.[14,15] Poor documentational practice on the part of the healthcare workers in this subregion is yet another reason.[16] The reverse is the case in developed countries. In these countries, all catheters passed are well documented and a catheter care plan is instituted.[10] A study in the United Kingdom found a catheter documentation rate of 89% for all catheter parameters with catheter care plan in place for approximately 98% of the patients who were catheterized[17]. This was in contrast to our study, in which none of these patients had a catheter care plan in place. Patients who had SPC had the majority of the parameters documented in their case notes. The reason may be related to the ample time spent in preparing these patients and the use of the theatre where the surgeon is required to fill the details of his procedure into the theatre logs and operation notes, which are usually attached to the case notes.
Complications following urinary catheter use could be long or short term.[18] In this study, all the documented complications were short-term complications. Bleeding was the most common complication, accounting for more than 80% of documented complications. Haematuria after SPC tends to be minimal; however, in some cases, it may become massive and require clot evacuation.[18,19] The degree of the bleeding in this study was not quantified.
Advocacy is needed for urinary catheter manufacturers to add easy-to-peel sticky labels to the catheters, so that these labels will be readily available in the emergency departments and wards such that at catheter insertion, the staff who insert catheters can easily tick the options available. Continuing medical education regarding the importance of the documentation of urinary catheterisation will bring about attitudinal change on the part of the healthcare workers and will play a significant role in correcting this anomaly. The governments and other hospital owners on their part need to invest in electronic medical records to make the documentation of these catheter details easier and faster.
Conclusion
This study highlights poor documentational practice on the use of urinary catheters in our institution. Suprapubic catheterisation was noted to have a high documentation rate compared with urethral catheterisation.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Ahluwalia A, Rossiter D, Menezes P. Urinary catheterisation: Indications, technique and managing failure. InnovAiT: Education and inspiration for general practice. 2018;11:29–34. [Google Scholar]
- 2.Nicolle LE. Catheter associated urinary tract infections. Antimicrob Resist Infect Control. 2014;3:23. doi: 10.1186/2047-2994-3-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bendaña EE, Trivedi D, Marshall J, Messing E. Lost and now found: Retained straight catheter for 20 years. Urology. 2011;77:73–4. doi: 10.1016/j.urology.2010.01.063. [DOI] [PubMed] [Google Scholar]
- 4.Popoola AA, Oseni I, Bamgbola KT, Babata AL. Toxic catheters and urethral strictures: A concern about types of catheters used in resource-poor countries. Afr J Urol. 2012;18:157–60. [Google Scholar]
- 5.Okeke CJ, Obi AO, Odoemene CA, Ojewola RW, Afogu EN, Odo C, et al. Urological emergencies in a Nigerian teaching hospital: Epidemiology and treatment. Niger J Clin Pract. 2021;24:400–5. doi: 10.4103/njcp.njcp_393_20. [DOI] [PubMed] [Google Scholar]
- 6.Fall B, Diao B, Fall PA, Diallo Y, Sow Y, Ondongo AAM, et al. Urological emergencies at the Dakar University Teaching Hospital: Epidemiological, clinical and therapeutic features. Prog Urol. 2008;18:650–3. doi: 10.1016/j.purol.2008.04.004. [DOI] [PubMed] [Google Scholar]
- 7.Atim T, Obiatuegwu K, Eniola S, Ajibola H, Aisuodionoa-Shedrach O, Dakum N. Urological emergencies at the university of Abuja Teaching Hospital Gwagwalada, Nigeria: Spectrum and initial outcome. Niger J Med. 2017;26:235–9. [Google Scholar]
- 8.Salako A, Badmus T, Babalola R, Igbokwe M, David R, Onyeze C, et al. Urologic emergencies in a low-resource setting: A 10-year review from South-Western Nigeria. Niger J Med. 2020;29:291–4. [Google Scholar]
- 9.Yenli EMT, Aboah K, Gyasi-Sarpong CK, Azorliade R, Arhin AA. Acute and chronic urine retention among adults at the urology section of the accident and emergency unit of Komfo Anokye Teaching Hospital, Kumasi, Ghana. Afr J Urol. 2015;21:129–36. [Google Scholar]
- 10.Miles G, Schroeder J. An evidence-based approach to urinary catheter changes. Br J Community Nurs. 2009;14:182–7. doi: 10.12968/bjcn.2009.14.5.42075. [DOI] [PubMed] [Google Scholar]
- 11.Hollingsworth JM, Rogers MAM, Krein SL, Hickner A, Kuhn L, Cheng A, et al. Determining the noninfectious complications of indwelling urethral catheters a systematic review and meta-analysis [Internet] Ann Intern Med. 2013;159:401–10. doi: 10.7326/0003-4819-159-6-201309170-00006. [DOI] [PubMed] [Google Scholar]
- 12.Manojlovich M, Ameling JM, Forman J, Judkins S, Quinn M, Meddings J. Contextual barriers to communication between physicians and nurses about appropriate catheter use. Am J Crit Care. 2019;28:290–8. doi: 10.4037/ajcc2019372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tijani KH, Lawal AO, Ojewola R, Badmus T. Quality of documentation of urethral catheterization in a Nigerian teaching hospital. Nig Q J Hosp Med. 2010;20:177–80. [PubMed] [Google Scholar]
- 14.Williams PB, Omishakin MA. Major barriers to effective delivery of health services in Nigeria. Int Q Community Health Educ. 1983;4:5–16. doi: 10.2190/0MJ5-FCP1-TD34-5BGC. [DOI] [PubMed] [Google Scholar]
- 15.Oleribe OO, Momoh J, Uzochukwu BSC, Mbofana F, Adebiyi A, Barbera T, et al. Identifying key challenges facing healthcare systems in Africa and potential solutions. Int J Gen Med. 2019;12:395–403. doi: 10.2147/IJGM.S223882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ko I, Adamu A, Jiya FB, Yusuf T, Sani UM, Jiya NM, et al. Quality of hospital admission documentation: A study in an emergency paediatric unit of a tertiary hospital in Nigeria. Afr J Med Health Sci. 2019;18:25–30. [Google Scholar]
- 17.Bhardwaj R, Pickard R, Rees J. Documented adherence to standards and guidelines: An audit. Br J Nurs. 2010;19:S26–30. doi: 10.12968/bjon.2010.19.Sup8.79066. [DOI] [PubMed] [Google Scholar]
- 18.Igawa Y, Wyndaele JJ, Nishizawa O. Catheterization: Possible complications and their prevention and treatment. Int J Urol. 2008;15:481–5. doi: 10.1111/j.1442-2042.2008.02075.x. [DOI] [PubMed] [Google Scholar]
- 19.Yip SK, Leung TY, Chart CK. Hematuria and Clot Retention after Burch colposuspension and cystofix suprapubic catheterization: Suprapubic cystotomy as an Alternative suprapubic drainage method. Int Urogynecol J Pelvic Floor Dysfunct. 1998;9:122–4. doi: 10.1007/BF01982223. [DOI] [PubMed] [Google Scholar]


