Highlights
-
•
The rate of DFS at 2 and 5 years was 89%, and the 5- year OS was 96%.
-
•
Early complications were grade 1–2 in 90% of cases. Late postoperative complications were seen in 15 patients (31.2%).
-
•
60.4% of patients intended to get pregnant. The pregnancy rate was 41.4%, and the live birth rate 88.2%.
Abstract
Objective
To report the surgical, oncological, and obstetrical outcomes of the different surgical techniques used for the fertility-sparing treatment of patients with early-stage cervical cancer.
Methods
We retrospectively analyzed all fertility-sparing procedures performed between 2004 and 2020. The study included patients desiring to preserve fertility who had squamous cell carcinoma, adenocarcinoma, and adenosquamous carcinoma histology, all grades, and FIGO 2009 stage IA2-IB1 tumors.
Results
48 patients met the inclusion criteria. Eight patients (16.7%) had stage IA2, and 40 (83.3%) had stage IB1 tumors. Conization with pelvic lymph node assessment was performed in 5 (10.4%) patients, an open radical trachelectomy in 21 (43.8%), and a laparoscopic radical trachelectomy in 22 (45.8%). No major intraoperative complications were registered. Two patients required surgery due to an early postoperative complication. Late postoperative complications were seen in 15 patients (31.2%), with cervical stenosis being the most frequent (60%). The rate of DFS at 2 and 5 years was 89% (95% CI, 76–95%), and the 5- year OS was 96% (95% CI, 83–98%). Univariate analysis demonstrated a relationship between tumor size and recurrence, but not for other prognostic tumor factors or surgical approach. One patient (4.8%) developed recurrent disease in the open radical trachelectomy group, and five (22.7%) in the laparoscopic radical trachelectomy group. The pregnancy rate was 41.4%, and the live birth rate 88.2%.
Conclusion
Fertility-sparing treatment for patients with early-stage cervical cancer is ever-evolving. This study adds information to the literature about the outcomes of these quite uncommon procedures, and allows a critical analysis of many of the topics which are under discussion.
1. Introduction
Cervical cancer is the fourth most frequently diagnosed cancer and the fourth leading cause of cancer death in women, with an estimated 604,000 new cases and 342,000 deaths worldwide in 2020. It is most frequently diagnosed among women aged 35–44, and its burden mainly affects women in low-and middle-income countries (Cancer of the Cervix Uteri - Cancer Stat Facts [Internet], 2022, Sung et al., 2020).
The standard recommendation for the treatment of patients with early-stage cervical cancer (stages IA2–IB1) is radical hysterectomy or, for those interested in preserving fertility, radical trachelectomy (National Comprehensive Cancer Network, 2022). Different approaches are described for this last surgery, and lately the debate has been focused on the possibility of performing more conservative procedures in certain scenarios, considering that radical trachelectomy results in excellent tumor control, but is associated with significant morbidity and obstetrical outcomes may also be compromised (Theofanakis et al., 2022, Plante et al., 2011). In addition, the usefulness of parametrial resection in women with early-stage cervical cancer and favorable pathologic characteristics has come under question after the publication of several studies reporting that < 1% of this population has parametrial involvement (Stegeman et al., 2007, Frumovitz et al., 2009).
Also, research has recently been carried out to compare oncological outcomes between minimally invasive and open radical trachelectomy following the publication of a randomized noninferiority trial showing worse oncologic outcomes after minimally invasive radical hysterectomy in stage I cervical cancer (Salvo et al., 2022, Smith et al., 2020, Ramirez et al., 2018). In one study, the 4.5-year disease-free survival rates after radical trachelectomy were 94.3% for open surgery and 91.5% for minimally invasive surgery (Salvo et al., 2022).
The aim of this study was to report the surgical, oncological, and obstetrical outcomes of the different surgical techniques used in our institution for the fertility-sparing treatment of patients with early-stage cervical cancer.
2. Methods
This is a retrospective cohort study, performed in a single, tertiary referral medical center. Approval was obtained from the institutional ethics committee. Information was obtained from patient electronic medical records. All conservative procedures for cervical cancer performed in our hospital by gynecologic oncologists of our department between January 1, 2004, and December 31, 2020, were analyzed. Inclusion criteria were: patients desiring to preserve fertility, squamous cell carcinoma, adenocarcinoma, and adenosquamous carcinoma histology, all grades, FIGO 2009 stage IA2-IB1 (Pecorelli, 2009) with no involvement of the upper endocervical canal, and follow-up information available for at least 12 months. Exclusion criteria were: neoadjuvant chemotherapy, pregnancy at diagnosis, and evidence or suspicion of lymph node involvement or distant metastasis by imaging.
Fertility conservative procedures included conization, laparoscopic radical trachelectomy (LRT), and open radical trachelectomy. Eligibility criteria to be candidates for conization were according to the ConCerv trial (as our hospital was a participating site) and included tumor size < 2 cm, squamous cell (any grade) or adenocarcinoma (grade 1 or 2 only) histology, no lymphovascular space invasion (LVSI), depth of invasion < 10 mm, and conization margins and endocervical curettage negative for malignancy and high-grade dysplasia. A negative margin was defined as non-invasive cancer within 1.0 mm of both the endocervical and ectocervical margins and no adenocarcinoma in situ, cervical intraepithelial neoplasia 2 or 3 at the inked or cauterized margin (Schmeler et al., 2021, Network and Clinical, 2022). The possibility of performing a conization if these criteria were met was considered since the beginning of this protocol in 2010. In cases in which a radical trachelectomy was performed, the surgical approach was at the discretion of the treating surgeon. Laparoscopic radical trachelectomies started to be performed in our institution in 2011, and was the most frequent approach until the publication of the LACC trial (Ramirez et al., 2018). Afterwards, it had to be done through an open approach. Uterine manipulator was used in laparoscopic procedures. An abdominal cerclage using a monofilament, nonabsorbable, polypropylene suture was placed during radical trachelectomies.
The size of the lesion was established by review of the loop electrocautery excision (leep)/cone specimen, MRI, and/or clinical examination. Nodal assessment was performed by pelvic lymphadenectomy and/or sentinel lymph node biopsy (in cases where the sentinel lymph node was clearly identified). Sentinel lymph node mapping was done using patent blue dye. Patients were followed with history and physical examination every 4 months for 2 years, every 6 months for another 3 years, and then annually. Annual cervical cytology was performed, and additional investigations as required according to symptoms or findings.
The primary objective of the study was to evaluate the disease free survival (DFS) and overall survival (OS) of patients with conservative surgery in our institution. DFS was measured from the date of surgery to the date of first recurrence (certified by biopsy) or last available follow-up visit. OS was measured from the date of surgery until death or last available follow- up visit. Secondary endpoints included the analysis of the surgical, fertility, and obstetrical outcomes. Surgical complications were graded according to the Clavien-Dindo Classification (Dindo et al., 2004). Continuous variables were described as mean with their respective standard deviation if they had a normal distribution, or as a median if the distribution was skewed with their respective interquartile ranges 25–75% (IQR) and were compared using a Student's t-test or a Mann-Whitney test, respectively. Categorical variables were reported as number or percentage and were compared using the Chi-square test. The DFS and OS were estimated at 2 and 5 years, with their respective confidence intervals, using the Kaplan-Meier method. Two-tailed p-values <0.05 were considered statistically significant. STATA version 13.1 software was used for statistical analysis.
3. Results
A total of 65 patients were evaluated, and 48 met the inclusion criteria (Fig. 1). Patient and tumor characteristics are summarized in Table 1. The median age was 31.5 (range 18–44). Thirty (62.5%) patients were nulliparous. Median tumor size was 15 mm (IQR 25–75 10–20). Eight patients (16.7%) had stage IA2, and 40 (83.3%) had stage IB1. The diagnostic procedure was a cervical biopsy in 20 (41.7%) cases, and an excisional procedure (leep/cone) in 28 (58.3%). Histological examination revealed squamous cell carcinoma in 27 cases, adenocarcinoma in 19, and adenosquamous carcinoma in 2. LVSI was seen in 9 (18.75%) patients, and deep stromal invasion (invasion of cervical stromal > 50%) in 5 (10.4%) cases. None of the final specimens had positive margins.
Fig. 1.
Flowchart of patient selection.
Table 1.
Patients’ and tumor characteristics (n = 48).
| Age at surgery (years) | |
|---|---|
|
31,5 (18–44) |
| Gravida, N (%) | |
|
30 (62,5%)18 (37,5%) |
| Stage*, N (%) | |
|
8 (16,7%)40 (83.3%) |
| Histology, N (%) | |
|
27 (56,2%)19 (39,6%)2 (4,2%) |
| Grade, N (%) | |
|
23 (47.9 %)22 (45.8%)3 (6.3%) |
| Stromal invasion, N (%) | |
|
43 (89.6%)5 (10.4%) |
| LVSI, N (%) | |
|
39 (81.25%)9 (18.75%) |
| Diagnostic procedure, N (%) | |
|
Cervical biopsy Excisional procedure |
20 (41.7%)28 (58.3%) |
| Tumor size (mm) Median |
15 (IQR 25–75 10–20) |
*FIGO 2009 classification (Pecorelli, 2009).
LVSI, lymphovascular space invasion.
Surgical outcomes are listed in Table 2. Conization was performed in 5 (10.4%) patients, an open radical trachelectomy in 21 (43.8%), and a laparoscopic radical trachelectomy in 22 (45.8%). There was no evidence of residual disease in 22 (45.8%) cases, and no evidence of parametrial disease in any of the radical trachelectomies. No major intraoperative complications were registered. Considering early postoperative complications (within 30 days after surgery), there were 21 complications, most of them (90.5%) were grade I and II, and 2 (9.5%) were grade III. These two last cases required surgery, one due to symptomatic lymphocyst, and the other to cervical necrosis and infection. Late postoperative complications were seen in 15 patients (31.2%), with cervical stenosis being the most frequent (60%). In patients who had undergone a conization with lymph node evaluation as definitive treatment, no early or late postoperative complications were identified.
Table 2.
Surgical outcomes.
| Type of surgery, N (%) | |
|---|---|
|
5 (10.4)21 (43.8)22 (45.8) |
| Estimated blood loss, N (%) | |
|
1 (2.1)8 (16.7)3 (6.2)1 (2.1)35 (72.9) |
| Number of lymph nodes removed | |
|
15 (IQR 25–75 13–19) |
| Operative time (minutes) Median |
282 (IQR 25–75 240–318) |
| Hospital stay, days Median |
3 (IQR 25–75 2–4) |
| Early postoperative complications*, N (%): | |
|
4 (8.3%)14 (29.2%)2 (4.2%) |
| Late postoperative complications*, N (%): | |
|
9 (18.75%)2 (4.2%)2 (4.2%)2 (4.2%) |
According to the Clavien-Dindo Classification.
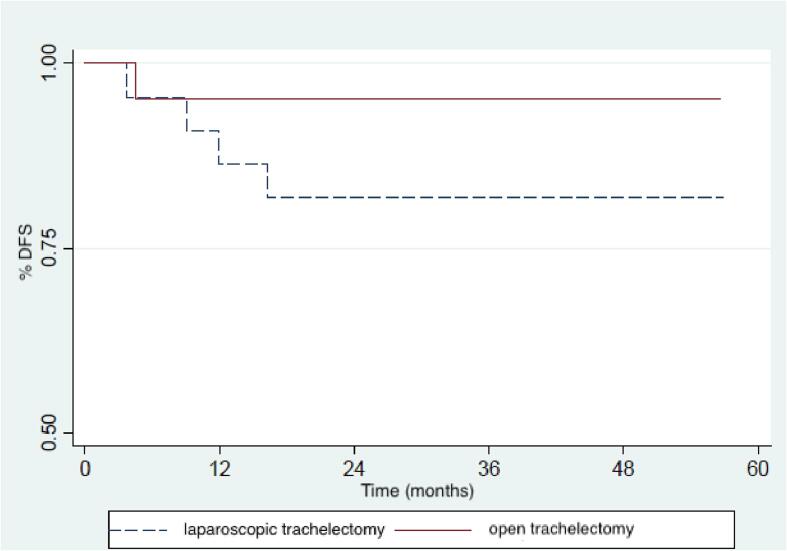
The median follow-up time was 66 months (IQR 25–75 40–107). Six patients (12.5%) developed a recurrence (95% confidence interval [CI], 2.7–22%), and 2 (4.2%) of them died of their disease. The rate of DFS at 2 and 5 years was 89% (95% CI, 76–95%) (Fig. 2). The 5- year OS was 96% (95% CI, 83–98%). Details of the cases with disease recurrence are presented in Table 3. All of them were initially classified as stage IB1 according to FIGO 2009 (Pecorelli, 2009), with a mean tumor size of 21.2 mm (17–25 mm). The tumor size in patients with recurrence was on average 6 mm greater than that of the patients who did not relapse (p < 0.001). Univariate analysis did not demonstrate a relationship between recurrence and other tumor prognostic factors such as histology, deep stromal invasion (DSI), and LVSI. Neither was there a significant difference in recurrences according to the surgical approach (Fig. 3).
Fig. 2.
Kaplan-Meier curve for disease-free survival.
Table 3.
Characteristics of recurrent cases.
| Case | Tumor size (mm) | Histology (size in mm) |
LVSI | DSI | Surgery | Time to recurrence | Recur site | Recur Tx | Outcome (after recurrence) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 20 (on CE) | SCC, G1 (10) |
Neg | Neg | LRT | 3 months | Cervix | CCRT | NED at 63 months |
| 2 | 17 (on MRI) | SCC, G2 (15) |
Neg | Neg | LRT | 16 months | Carcinomatosis | CT | DOD at 14 months |
| 3 | 23 (on MRI) | SCC, G2 (10) |
Neg | Pos | LRT | 8 months | Cervix | Sx + RT + BT | NED at 73 months |
| 4 | 22 (on MRI) | AC, G1 (7) |
Pos | Neg | LRT | 77 months | Cervix and ovary | Sx + CT | NED at 3 months |
| 5 | 20 (on EP) | AC, G1 (11) |
Neg | Neg | LRT | 12 months | Ovary | Sx + CT | NED at 51 months |
| 6 | 25 (on MRI) | AC, G1 (24) |
Neg | Neg | ORT | 5 months | Pelvis | CCRT | DOD at 14 months |
LVSI, lymphovascular space invasion; DSI, deep stromal invasion; Tx, treatment; CE, clinical examination; MRI, magnetic resonance imaging; EP, excisional procedure; SCC, squamous cell carcinoma; AC, adenocarcinoma; Neg, negative; POS, positive; LRT, laparoscopic radical trachelectomy; ORT, open radical trachelectomy; CCRT, concurrent chemoradiation; CT, chemotherapy; Sx, surgery; RT, radiotherapy; BT, brachytherapy.
Fig. 3.
Kaplan-Meier curves for disease-free survival according to the surgical approach.
Considering the diagnostic procedure, 28 patients were diagnosed after an excisional procedure (leep/cone). Of these, 12 and 16 had negative and positive surgical margins on the histopathological analysis, respectively. None of the 12 patients with negative margins had residual disease in the final specimen, while 6 of the 16 patients with positive margins did. None of the patients with no residual disease experienced a recurrence, while 1 of the 6 patients with residual disease had a recurrence 12 months after a LRT.
In terms of fertility outcomes, 29 (60.4%) patients intended to get pregnant. Of these, 12 (41.4%) actually got pregnant, for a total of 18 pregnancies. All were spontaneous pregnancies. The live birth rate was 88.2%, and 66.6% of the deliveries were after 34 weeks of gestation. Considering specifically the cases treated with a conization and lymph node assessment, 2 patients tried to get pregnant, and both had spontaneous conceptions, and a normal vaginal delivery at 36 and 40 weeks. All the other patients had cesarean sections. Of the patients who had cervical stenosis as late postoperative complication, all of them intended to become pregnant and only one was able to achieve a gestation, although 88.9% were evaluated by fertility specialists.
4. Discussion
This study showed that in patients with cervical cancer FIGO 2009 stage IA2-IB1 (Pecorelli, 2009) who were treated with fertility-sparing surgery in our institution, the rate of DFS at 2 and 5 years was 89% (95% CI, 76–95%), and the 5- year OS was 96% (95% CI, 83–98%). Comparing these results with the literature, a systematic review by Smith et al regarding radical trachelectomy for the treatment of early-stage cervical cancer published a median 5-year recurrence-free and OS of 94.6% (range 88–97.3%) and 97.4% (range 95–99%), respectively (Smith et al., 2020). In another systematic review, recurrent disease was seen in 4%, 5%, and 6% of the patients who had had a vaginal radical trachelectomy, an open radical trachelectomy, and a LRT, respectively (Bentivegna et al., 2016). In the IRTA study, in which the oncological results after an open vs a minimally invasive radical trachelectomy were compared, the 4.5-year disease-free survival rates were 94.3% (95% confidence interval, 91.6–97.0) for open surgery and 91.5% (95% confidence interval, 87.6–95.6) for minimally invasive surgery (Salvo et al., 2022). Most of the publications about this topic are limited to observational research, mainly retrospective case series and case reports, and oncologic results are varied, ranging from 5-year DFS rates of 84% to 99% (Park et al., 2014, Vieira et al., 2015). In addition, significant differences exist in the inclusion and exclusion criteria of the studies, some of them including patients with tumors FIGO 2009 (Pecorelli, 2009) stage IA1 with lymphovascular space invasion while others not, and some excluding tumors > 2 cm while others not.
Many aspects of cervical cancer treatment are currently under debate, including surgical approach, type of surgery depending on the size of the tumor, and the role of prior conization. In this context, the treatment of patients with early-stage cervical cancer who desire to preserve their fertility is an evolving paradigm. It is complicated to reach definitive conclusions due to the low incidence of early-stage disease, the good medical prognosis, and the low rate of recurrences in this scenario. Our series of 48 patients enables us to analyze many of the issues under discussion in this population.
In terms of surgical outcomes, no intraoperative complications were reported in this study, in agreement with the 0.7% intraoperative complication rate in open radical trachelectomy published in a systematic review performed by Pareja et al (Pareja et al., 2013), and is lower than the 5.6% rate reported for vaginal radical trachelectomy by Plante et al. (2011). Early postoperative complications were frequent (43.75%) in our series, but 90.5% of them were grade I and II of the Clavien-Dindo classification, as published in other series (Dindo et al., 2004, Vieira et al., 2015). The most frequent long-term morbidity was cervical stenosis (9%). No late postoperative complications were identified in the 5 patients treated with conization and pelvic lymph node evaluation, which is consistent with the theoretical benefits of a less radical surgery in this group of patients. In many other publications, cervical stenosis has been the most common sequelae with an incidence varying between 8.1% and 12% considering all types of approaches for radical trachelectomy (Plante et al., 2011, Vieira et al., 2015, Pareja et al., 2013, Li et al., 2011, Wethington et al., 2012). Indeed, it remained a significant problem in a study by Plante et al of 50 patients who underwent a simple vaginal trachelectomy/conization with laparoscopic sentinel lymph node mapping ± complete pelvic node dissection (Plante et al., 2020).
Regarding the analysis of recurrences in our series, univariate analysis demonstrated a relationship between tumor size and recurrence, but not for other prognostic tumor factors. Similarly, other studies had previously reported that a size of lesion > 2 cm was statistically associated with the risk of recurrence (Plante et al., 2011, Park et al., 2014, Nishio et al., 2009). In the study of Park et al, a depth of cervical stromal invasion>50% was also significantly associated with decreased DFS (Park et al., 2014). Interestingly, 3 of the patients that recurred in our series had a preoperative tumor size > 2 cm, but in the final pathology measurement none of the tumors of patients with recurrence were>2 cm. Tumor size being such an important variable according to the literature, it is surprising that many studies about cervical cancer determine the tumor size by preoperative estimates (Salvo et al., 2022, Plante et al., 2020), and others by final pathology measurements (Ramirez et al., 2018), making it difficult to draw conclusions with regards to tumor size. Even after the new 2018 FIGO cervical cancer staging, the determination of tumor size by clinical examination, pathology, or imaging results is still unresolved (Salvo et al., 2020). Furthermore most publications about conservative treatment in cervical cancer use the 2009 FIGO staging, and this may not reflect the actual tumor stage according to the 2018 FIGO classification (Bhatla et al., 2018).
With respect to the surgical approach, in this study there was no statistically significant difference in recurrences according to the type of procedure, which is consistent with the results of the IRTA Study, in which the 4.5-year disease-free survival rates after radical trachelectomy were 94.3% for open surgery and 91.5% for minimally invasive surgery (log-rank P = 0.37)(Salvo et al., 2022). However, in our series, the rate of recurrence after LRT and after open radical trachelectomy was 22.7% and 4.8%, respectively. It may be hypothesized that the absence of statistical significance may be due to the number of cases.
Another topic of interest when comparing surgical approaches is the pattern of recurrence. In this study, 5 out of 6 recurrences were in the pelvis, and the remaining one had carcinomatosis after a LRT. In a series of 61 women who had undergone open radical trachelectomy, there were 6 recurrences, all of them in the pelvis (Nishio et al., 2009). In the study of Park et al with 79 patients operated by a LRT, 9 patients had a recurrence, and one of them recurred in the abdomen (Park et al., 2014).
In our series, when analyzing patients who had an excisional procedure (leep/cone) at diagnosis, it is remarkable that 22 patients had no residual disease in the final specimen (9 had a LRT, 9 an open radical trachelectomy, and 4 a conization), and none of them experienced a recurrence. It should be noted that 1 of the 6 patients who had had residual disease in the final specimen experienced an ovarian recurrence 12 months after a LRT. Oncological results were better in this subgroup of patients, but logically all of them had initially microscopic tumors, and this may be one possible explanation for their outcomes.
Analyzing fertility outcomes, 29 (60.4%) patients intended to get pregnant. Although this number may seem low, previous series reported rates between 41% and 54%, and 38% in a systematic review by (Vieira et al., 2015, Pareja et al., 2013, Wethington et al., 2012). The pregnancy rate in our population was 41.4%, and is varied in the literature, ranging from 13.8% to 74% in retrospective series (Wethington et al., 2012, Nishio et al., 2009). In a recent updated systematic review, Morice et al published a pregnancy rate of 56.3%, 58.7%, 36%, and 50.8% after a simple trachelectomy/cone, a vaginal radical trachelectomy, an open radical trachelectomy, and a LRT, respectively (Bentivegna et al., 2016). In our series, 44.4% of the pregnancies were delivered at term, and remarkably, the live birth rate was 88.2%. Live birth rates reported in the systematic review mentioned above were 87%, 71%, 66.6%, and 66.6% after a simple trachelectomy/cone, a vaginal radical trachelectomy, an open radical trachelectomy, and a LRT, respectively (Bentivegna et al., 2016).
The strengths of our study include the fact that it is the first series of one center publishing its results in these 3 fertility-sparing surgical procedures in early-stage cervical cancer. In addition, we have not found a larger series of any other developing country, where the incidence of cervical cancer is the highest. Smith et al. highlighted the lack of information regarding treatment outcomes from this population.(9) Also, the median follow-up was 66 months, long enough in order to do more precise estimations of the oncological and obstetrical outcomes. Our study has several limitations, mainly due to its retrospective nature, which increases information bias. In addition, the time period of the study is wide, and the quality of the complementary exams has probably varied.
In conclusion, in our institution the rate of DFS at 2 and 5 years of patients with cervical cancer treated with conservative surgery was 89% (95% CI, 76–95%), and the 5- year overall survival was 96% (95% CI, 83–98%). Fertility-sparing treatment for patients with early-stage cervical cancer is ever-evolving. This series adds information to the literature about outcomes in these quite uncommon procedures, and allows a critical analysis of many of the topics which are under debate nowadays.
Author contribution
All the authors have contributed to the preparation of this article (design, planning, conduct, data analysis, and manuscript writing).
Financial support
No financial support was received for this study.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Bentivegna E., Maulard A., Pautier P., Chargari C., Gouy S., Morice P. Fertility results and pregnancy outcomes after conservative treatment of cervical cancer: a systematic review of the literature. Fertil. Steril. 2016;106(5) doi: 10.1016/j.fertnstert.2016.06.032. [DOI] [PubMed] [Google Scholar]
- Bentivegna E., Gouy S., Maulard A., Chargari C., Leary A., Morice P. Oncological outcomes after fertility-sparing surgery for cervical cancer: a systematic review. LancetOncol. 2016;17(6):e240–e253. doi: 10.1016/S1470-2045(16)30032-8. [DOI] [PubMed] [Google Scholar]
- Bhatla N., Aoki D., Sharma D.N., Sankaranarayanan R. Cancer of the cervix uteri. Int. J. Gynaecol. Obstet. 2018;143(Suppl 2):22–36. doi: 10.1002/ijgo.12611. [DOI] [PubMed] [Google Scholar]
- Cancer of the Cervix Uteri - Cancer Stat Facts [Internet]. SEER. [cited 2022 Jul 1]. Available from: https://seer.cancer.gov/statfacts/html/cervix.html.
- Dindo, D., Demartines, N., Clavien, P.A., 2004. Classification of surgical complications [Internet]. Vol. 240, Annals Surg. 2004. p. 205–13. Available from: Doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed]
- Frumovitz M, Sun CC, Schmeler KM, Deavers MT, dos Reis R, Levenback CF, et al. Parametrial Involvement in Radical Hysterectomy Specimens for Women With Early-Stage Cervical Cancer [Internet]. Vol. 114, Obstetrics & Gynecology. 2009. p. 93–9. Available from: Doi: 10.1097/aog.0b013e3181ab474d. [DOI] [PubMed]
- Li J., Li Z., Wang H., Zang R., Zhou Y., Ju X., et al. Radical abdominal trachelectomy for cervical malignancies: surgical, oncological and fertility outcomes in 62 patients. Gynecol. Oncol. 2011;121(3):565–570. doi: 10.1016/j.ygyno.2011.01.032. [DOI] [PubMed] [Google Scholar]
- National Comprehensive Cancer Network. NCCN Clinical practice guidelines in oncology (NCCN guidelines). 2022 [Internet]. 2023. Available from: https://www.nccn.org/professionals/physician_gls/pdf/cervical.pdf.
- Nishio H, Fujii T, Kameyama K, Susumu N, Nakamura M, Iwata T, et al. Abdominal radical trachelectomy as a fertility-sparing procedure in women with early-stage cervical cancer in a series of 61 women [Internet]. Vol. 115, Gynecologic Oncology. 2009. p. 51–5. Available from: Doi: 10.1016/j.ygyno.2009.06.036. [DOI] [PubMed]
- Pareja R., Rendón G.J., Sanz-Lomana C.M., Monzón O., Ramirez P.T. Surgical, oncological, and obstetrical outcomes after abdominal radical trachelectomy - a systematic literature review. Gynecol. Oncol. 2013;131(1):77–82. doi: 10.1016/j.ygyno.2013.06.010. [DOI] [PubMed] [Google Scholar]
- Park J.Y., Joo W.D., Chang S.J., Kim D.Y., Kim J.H., Kim Y.M., et al. Long-term outcomes after fertility-sparing laparoscopic radical trachelectomy in young women with early-stage cervical cancer: an Asan Gynecologic Cancer Group (AGCG) study. J. Surg. Oncol. 2014;110(3):252–257. doi: 10.1002/jso.23631. [DOI] [PubMed] [Google Scholar]
- Pecorelli S. Revised FIGO staging for carcinoma of the vulva, cervix, and endometrium. Int. J. Gynaecol. Obstet. 2009 May;105(2):103–104. doi: 10.1016/j.ijgo.2009.02.012. [DOI] [PubMed] [Google Scholar]
- Plante M, Grégoire J, Renaud M, Roy M. The vaginal radical trachelectomy: An update of a series of 125 cases and 106 pregnancies [Internet]. Vol. 120, Gynecologic Oncology. 2011. p. S29. Available from: Doi: 10.1016/j.ygyno.2010.12.072. [DOI] [PubMed]
- Plante M., Renaud M.C., Sebastianelli A., Gregoire J. Simple vaginal trachelectomy in women with early-stage low-risk cervical cancer who wish to preserve fertility: the new standard of care? Int. J. Gynecol. Cancer. 2020;30(7):981–986. doi: 10.1136/ijgc-2020-001432. [DOI] [PubMed] [Google Scholar]
- Ramirez P.T., Frumovitz M., Pareja R., Lopez A., Vieira M., Ribeiro R., et al. Minimally invasive versus abdominal radical hysterectomy for cervical cancer. N. Engl. J. Med. 2018;379(20):1895–1904. doi: 10.1056/NEJMoa1806395. [DOI] [PubMed] [Google Scholar]
- Salvo G., Odetto D., Pareja R., Frumovitz M., Ramirez P.T. Revised 2018 International Federation of Gynecology and Obstetrics (FIGO) cervical cancer staging: A review of gaps and questions that remain. Int. J. Gynecol. Cancer. 2020;30(6):873–878. doi: 10.1136/ijgc-2020-001257. [DOI] [PubMed] [Google Scholar]
- Salvo G., Ramirez P.T., Leitao M.M., Cibula D., Wu X., Falconer H., et al. Open vs minimally invasive radical trachelectomy in early-stage cervical cancer: International Radical Trachelectomy Assessment Study. Am. J. Obstet. Gynecol. 2022;226(1):97.e1–97.e16. doi: 10.1016/j.ajog.2021.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmeler K.M., Pareja R., Lopez Blanco A., Humberto Fregnani J., Lopes A., Perrotta M., et al. ConCerv: a prospective trial of conservative surgery for low-risk early-stage cervical cancer. Int. J. Gynecol. Cancer. 2021;31(10):1317–1325. doi: 10.1136/ijgc-2021-002921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith E.S., Moon A.S., O’Hanlon R., Leitao M.M., Jr, Sonoda Y., Abu-Rustum N.R., et al. Radical trachelectomy for the treatment of early-stage cervical cancer: a systematic review. Obstet Gynecol. 2020;136(3):533–542. doi: 10.1097/AOG.0000000000003952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stegeman M, Louwen M, van der Velden J, ten Kate FJW, den Bakker MA, Burger CW, et al. The incidence of parametrial tumor involvement in select patients with early cervix cancer is too low to justify parametrectomy [Internet]. Vol. 105, Gynecologic Oncology. 2007. p. 475–80. Available from: Doi: 10.1016/j.ygyno.2007.01.016. [DOI] [PubMed]
- Sung, H., Ferlay, J., Siegel, R.L., Laversanne, M., Soerjomataram, I., Jemal, A., et al., 2020. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries [Internet]. Vol. 71, CA: A Cancer J. Clin. 2021. p. 209–49. Available from: Doi: 10.3322/caac.21660. [DOI] [PubMed]
- Theofanakis, C., Koulakmanidis, A.M., Prodromidou, A., Haidopoulos, D., Rodolakis, A., Thomakos, N., 2022. Fertility-sparing treatment for young patients with early-stage cervical cancer: a dawn of a new era [Internet]. Vol. 9, Front. Surgery. 2022. Available from: Doi: 10.3389/fsurg.2022.867993. [DOI] [PMC free article] [PubMed]
- Vieira M.A., Rendón G.J., Munsell M., Echeverri L., Frumovitz M., Schmeler K.M., et al. Radical trachelectomy in early-stage cervical cancer: A comparison of laparotomy and minimally invasive surgery. Gynecol. Oncol. 2015;138(3):585–589. doi: 10.1016/j.ygyno.2015.06.023. [DOI] [PubMed] [Google Scholar]
- Wethington S.L., Cibula D., Duska L.R., Garrett L., Kim C.H., Chi D.S., et al. An international series on abdominal radical trachelectomy: 101 patients and 28 pregnancies. Int. J. Gynecol. Cancer. 2012;22(7):1251–1257. doi: 10.1097/IGC.0b013e318263eee2. [DOI] [PubMed] [Google Scholar]