Background.
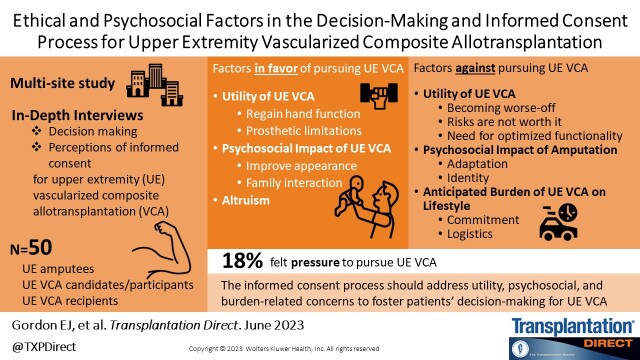
Although upper extremity (UE) vascularized composite allotransplantation (VCA) aims to improve quality of life, relatively few have been performed worldwide to support evidence-based treatment and informed decision-making.
Methods.
We qualitatively examined factors contributing to anticipated and actual decision-making about UE VCA and perceptions of the elements of informed consent among people with UE amputations, and UE VCA candidates, participants, and recipients through in-depth interviews. Thematic analysis was used to analyze qualitative data.
Results.
Fifty individuals participated; most were male (78%) and had a mean age of 45 y and a unilateral amputation (84%). One-third (35%) were “a lot” or “completely” willing to pursue UE VCA. UE VCA decision-making themes included the utility of UE VCA, psychosocial impact of UE VCA and amputation on individuals’ lives, altruism, and anticipated burden of UE VCA on lifestyle. Most respondents who underwent UE VCA evaluation (n = 8/10) perceived having no reasonable treatment alternatives. Generally, respondents (n = 50) recognized the potential for familial, societal, cultural, medical, and self-driven pressures to pursue UE VCA among individuals with amputations. Some (n = 9/50, 18%) reported personally feeling “a little,” “somewhat,” “a lot,” or “completely” pressured to pursue UE VCA. Respondents recommended that individuals be informed about the option of UE VCA near the amputation date.
Conclusions.
Our study identified psychosocial and other factors affecting decision-making about UE VCA, which should be addressed to enhance informed consent. Study participants’ perceptions and preferences about UE VCA suggest re-examination of assumptions guiding the UE VCA clinical evaluation process.
Many of the more than 41 000 service members, Veterans, and civilians with major upper extremity (UE) amputations experience functional, physical, and psychological deficits.1–4 Conventional treatment options, including prosthetics and reconstructive surgery, remain imperfect.5,6 UE vascularized composite allotransplantation (VCA) is a life-enhancing treatment that can restore motor and sensory function and enhance quality of life, self-image, independence, and social integration.7–9 UE VCA is the second most prevalent type of VCA, with 56 performed in the United States.10 Although functional outcomes are sound, limited data on psychosocial outcomes7,8,11 and lack of educational materials on UE VCA12 may undermine informed decision-making about UE VCA.9,11,13
Although VCA can be viewed as having recently transitioned from being a highly experimental research option to a standard clinical option, vestiges of its experimental status (eg, institutional review board oversight) remain in some transplant programs, suggesting otherwise.14,15 VCA’s full transition is ultimately contingent on the attainment of standardized, validated outcome measures (including patient-reported outcome measures), needed to generate the robust outcomes data to support this designation. However, the present lack of such outcomes data restricts full claim of transition. The ethical implications of this shifting treatment status are paramount with regard to informed consent. The blurred distinction between clinical care and research for VCA, and surgical innovations in general, generates ambiguity in disclosure standards used for informed consent.16
The limited data on UE VCA recipient outcomes may make it difficult for patients to make an informed decision about UE VCA, that is, express their self-determination (autonomy). We found that individuals with UE limb loss desired information about the success rate of UE VCA to inform treatment decision-making.17 This ethical concern arises commonly within the broader context of surgical innovation characterized by novel techniques and new technologies for which little is known about patient outcomes and its concomitant uncertainty.18,19 Research documents that surgical patients strongly desired information about the novelty of the procedure, the surgeon’s experience performing the procedure, and procedure volume and outcome to make informed decisions.20 However, despite good intentions, surgeons often fall short of disclosing that procedures were innovative and had uncertain outcomes.21
The UE VCA procedure provides significant potential benefits as well as serious medical and psychological risks and burdens, which require adequate understanding in order for candidates to make an informed decision about whether UE VCA is right for them. Additionally, VCA candidates can be considered “especially vulnerable” because they are willing to undergo considerable risks and burdens for an elective, non–life-saving treatment with uncertain long-term outcomes.15 Such vulnerability is also a common experience among patients undergoing innovative surgical procedures for which alternative standard treatments are either ineffective or nonexistent.19
Because of these ethical considerations, it is essential that patients and their transplant team engage in comprehensive communication for patients to provide meaningful informed consent. Although it is not feasible for patients to grant “full” informed consent (as patients cannot know the full extent of clinical information about the treatment), enabling patients to provide meaningful informed consent is achievable. Toward this end, systematic reviews show that informed consent for surgical/medical clinical procedures can be enhanced through a combination of modalities including digital health technologies (ie, interactive websites, question prompt lists, and specialized consent forms).22–24
Individuals with UE amputations commonly report receiving little information and engaging in limited communication with healthcare providers about treatment options.25–28 Assessing patient experiences in decision-making and informed consent is important for quality improvements in VCA.15 A few studies have examined factors influencing interest in UE VCA, albeit using small samples.29–31 No research has examined how individuals make decisions about whether to pursue UE VCA or patients’ perceptions of informed consent for UE VCA.
This study assessed factors influencing patients’ decision-making and anticipated and actual perceptions of the elements of informed consent about UE VCA. Assessing factors affecting decision-making about UE VCA is important for identifying opportunities to enhance the informed consent process. Our intent was to leverage our findings to help advance UE VCA clinical practice, broaden ethical understanding of UE VCA, and inform the development of educational materials to support the UE VCA informed consent process.
MATERIALS AND METHODS
Research Design
We conducted a cross-sectional convergent mixed-methods ethnographic study to examine perceptions, decision-making, and informed consent processes regarding UE VCA among people with UE amputations.32 The mixed-methods design involving in-depth, semistructured interviews and closed-ended questions, afforded a comprehensive analysis. Ethnography aims to understand human behaviors from the “insider’s point of view,” reveal culturally embedded norms or tacit assumptions shared among members of a group, and view phenomena in their political, social, economic, and historical contexts.33 Interview questions were guided by the ethical principle of respect for persons, which requires that individuals provide informed consent through information disclosure, comprehension, and voluntariness.34 We used the Consolidated Criteria for Reporting Qualitative Research for quality reporting.35
Setting
The study was conducted at Northwestern University (NU) and Shirley Ryan AbilityLab in Chicago, IL; David Rotter Prosthetics in Joliet, IL; Johns Hopkins University (JHU) in Baltimore, MD; and Walter Reed National Military Medical Center (WRNMMC) in Bethesda, MD, from October 2019 to April 2022. JHU was the only study site that performed UE VCA. Institutional Review Boards at NU (STU00209718), JHU (00225728), and WRNMMC (WRNMMC-EDO-2020-0432) approved the study. NU served as the Institutional Review Board of record for WRNMMC.
Sample Population and Recruitment
Eligible study participants were age 18–65 y, English-speaking, military personnel and civilians, and had an acquired UE amputation, including: those who never contacted a transplant center, UE VCA “candidates” (who contacted a transplant center to express interest but did not move forward with signing informed consent for UE VCA evaluation), UE VCA “participants” (who signed informed consent and began the UE VCA evaluation process), and UE VCA recipients. People who had finger/palm loss only, congenital limb loss, neurological causes of amputation, and/or were cognitively impaired were excluded.
Given challenges previously experienced recruiting people with UE amputations, we used purposive homogeneous sampling (ie, people with UE amputations) to ensure a representative sample from our target population36,37 and purposive maximum variation sampling to include diverse subgroups (ie, individuals with unilateral and bilateral amputations who had their amputations for different amounts of time).37 We targeted a sample size of n = 50 to achieve theoretical saturation of the overall sample, as a range of 30 - 60 is recommended,38–40 and to enable nonparametric statistics38 of amputation characteristics relevant to patients’ perceptions of UE VCA as found in other research.29
We sent recruitment letters via mail and email to patients from each site’s hand surgery outpatient clinics and JHU’s UE VCA program. Research staff called patients thereafter to assess interest and schedule interviews. Study fliers were shared by providers at other sites, the WRNMMC rehabilitation clinic, 3 online amputee listservs and newsletters, and 304 amputee support groups via email and social media platforms. Study participants were screened via phone and provided verbal informed consent.
Data Collection
We conducted in-depth telephone interviews from July 2020 to April 2022 to assess decision-making and perceptions of the elements of informed consent about UE VCA. Interviews were conducted by female and male research staff (B.R.K., K.B.V., M.D., and M.J.N.) trained by E.J.G., a seasoned social scientist, using standardized approaches41 (ie, interview guide), which were guided by the elements of informed consent.34 We developed the interview guide in collaboration with our interdisciplinary research team, including UE VCA clinicians and surgeons, and scientific advisory board. Interviewers had no prior relationship with study participants.
Open-ended questions assessed participants’ awareness and perceptions of UE VCA, actual and hypothetical willingness to consider UE VCA, factors informing decision-making about UE VCA, opinions about the optimal time to inform patients about UE VCA as an option, perceptions of elements of informed consent for UE VCA (ie, information disclosure, information needs, alternatives, comprehension, voluntariness). Analysis of participants’ information needs about UE VCA were reported elsewhere.17 The interview guide included 59 open-ended questions, with 23 additional questions tailored to UE VCA candidates, participants, and recipients (Supplemental File 1, http://links.lww.com/TXD/A556). Closed-ended questions included yes/no and Likert questions assessing willingness to receive UE VCA, perceived undue influence to pursue UE VCA, and likelihood of using educational materials about UE VCA. Interviews concluded with demographic and clinical questions (eg, age, amputation level and type, date of amputation), and health literacy (“How often do you need to have someone help you when you read instructions, pamphlets, or other written material from your doctor or pharmacy?” anchored by “Never” and “Always”; “Never” and “Rarely” responses were considered literate).42 Interviews lasted an average of 78 min (range: 37–140), were audio-recorded, and transcribed. Research staff took field notes during and after interviews. Cognitive telephone interviews were conducted initially with 5 participants using standard “think aloud” procedures to ensure interview questions were interpreted as intended and improve question wording.43,44 All study participants were compensated with a $35 gift card.
Analysis
Qualitative Analysis
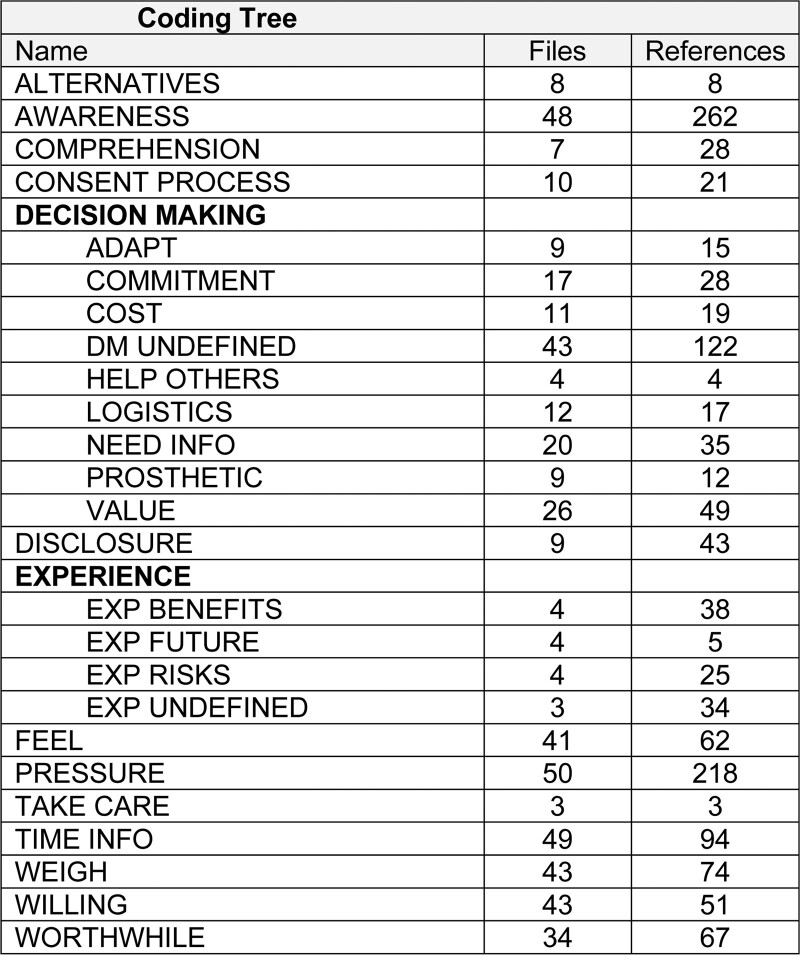
Verbatim transcriptions of audio-recorded interviews were analyzed for themes emergent from the data.45 As data were collected, we debriefed responses and refined the interview guide by adding probes until reaching thematic saturation.46,47 We first developed deductive codes from interview guide topics.48 In an iterative, constant comparative process,49 the research staff independently reviewed and coded 1–5 transcripts at each study site to develop inductive codes reflecting new themes emergent from the data (Figure 1). After coding each transcript, the research team held analytic retreats to resolve discrepancies in coding, and refine the codebook. After finalizing the codebook, research staff independently coded 3–5 transcripts per site using NVivo (Release 1.6.1, QSR International) until establishing inter-rater reliability (Kappa > 0.80).50 Thereafter, 2 research staff per site coded all transcripts at each site, resolving any discrepancies via discussion until reaching consensus. Teams of 2 research staff reviewed coded segments across participants to identify themes and wrote code summaries.51
FIGURE 1.
Coding tree.
Quantitative Analysis
We assessed the frequency, mean, and distribution of dichotomous and Likert interview responses across participants using IBM SPSS Statistics (Version 27). Fisher’s exact test, Spearman’s ρ, and t-tests were used to compare Likert scale responses (“not at all,” “a little,” and “somewhat” likely versus “very” and “completely” likely) by time since amputation and amputation type (ie, unilateral or bilateral). A P value of <0.05 was considered statistically significant.
RESULTS
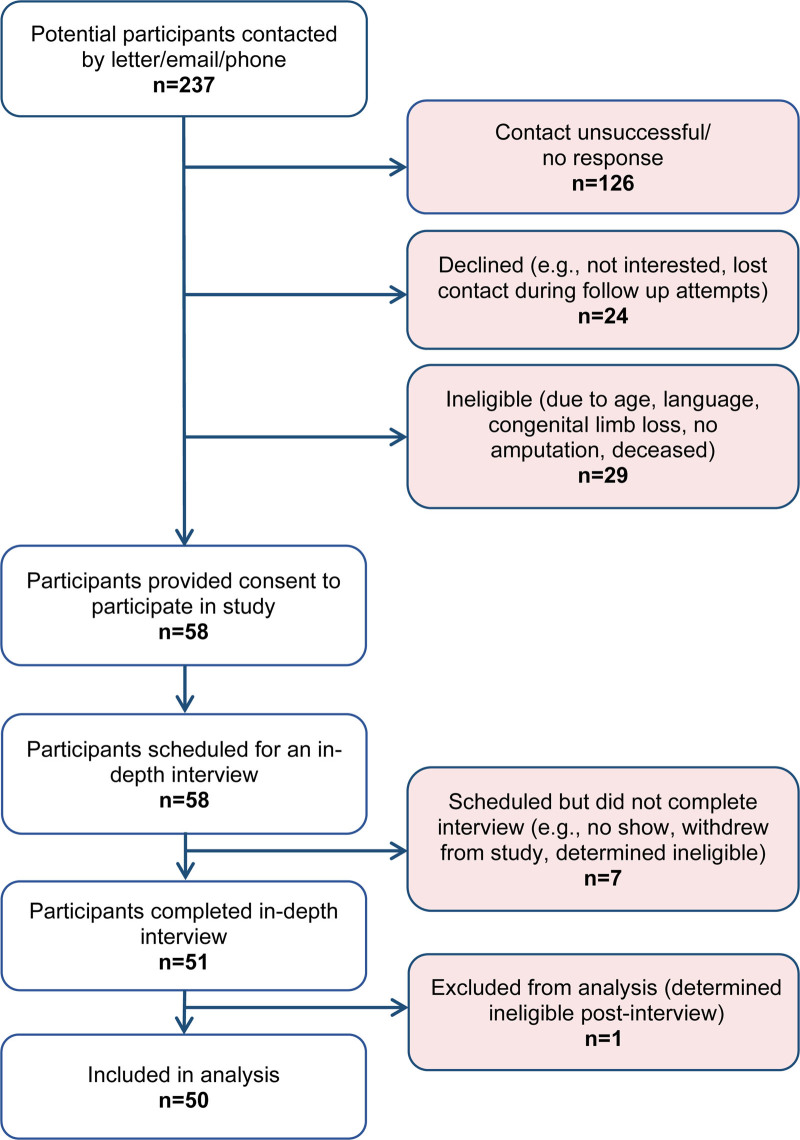
Demographics
Fifty participants completed an interview (64% participation rate; Figure 2). Twenty-two refused to participate or dropped out before or after providing consent because they were not interested, lost contact, or did not show up for their scheduled interview. Most participants were male (78%), White (72%), on average 45 y, and had a unilateral amputation (84%) (Table 1). Study participants included individuals with UE amputations (80%, n = 40), UE VCA candidates (4%, n = 2), UE VCA participants (8%, n = 4), and UE VCA recipients (8%, n = 4). Average time (at interview) since amputation was 9.9 y.
FIGURE 2.
Consort diagram.
TABLE 1.
Participants’ sociodemographic and clinical characteristics, N = 50
| Variable | Total N = 50 n (%) | UE amputees n = 40 n (%) | UE VCA candidates, participants N = 6 n (%) | UE VCA recipients n = 4 n (%) |
|---|---|---|---|---|
| Age, y, mean [SD] (range) | 45.3 [11.6] (19-65) | 45.8 [12.2] (19-65) |
44.8 [10.1] (37-63) |
40.8 [7.9] (34-52) |
| Gender | ||||
| Male | 39 (78.0) | 32 (80.0) | 3 (50.0) | 4 (100) |
| Female | 11 (22.0) | 8 (20.0) | 3 (50.0) | 0 (0) |
| Race | ||||
| White | 36 (72.0) | 28 (70.0) | 4 (66.7) | 4 (100) |
| Black or African American | 10 (20.0) | 8 (20.0) | 2 (33.3) | 0 (0) |
| Othera | 4 (8.0) | 4 (10.0) | 0 (0) | 0 (0) |
| Ethnicity | ||||
| Not Hispanic or Latino | 42 (84.0) | 32 (80.0) | 6 (100) | 4 (100) |
| Hispanic or Latino | 8 (16.0) | 8 (20.0) | 0 (0) | 0 (0) |
| Marital status | ||||
| Married/domestic partner or civil union | 33 (66.0) | 28 (70.0) | 4 (66.7) | 1 (25.0) |
| Never married/single | 10 (20.0) | 7 (17.5) | 1 (16.7) | 2 (50.0) |
| Separated or divorced | 7 (14.0) | 5 (12.5) | 1 (16.7) | 1 (25.0) |
| Education | ||||
| Less than high school graduate | 1 (2.0) | 1 (2.5) | 0 (0) | 0 (0) |
| High school graduate | 9 (18.0) | 7 (17.5) | 2 (33.3) | 0 (0) |
| Some college | 18 (36.0) | 15 (37.5) | 1 (16.7) | 2 (50.0) |
| College graduate | 15 (30.0) | 13 (32.5) | 1 (16.7) | 1 (25.0) |
| Post-graduate degree | 7 (14.0) | 4 (10.0) | 2 (33.3) | 1 (25.0) |
| Employment status | ||||
| Employed full time | 20 (40.0) | 15 (37.5) | 3 (50.0) | 2 (50.0) |
| Retired | 12 (24.0) | 11 (27.5) | 0 (0.0) | 1 (25.0) |
| Disabled | 11 (22.0) | 9 (22.5) | 2 (33.3) | 0 (0.0) |
| Not employed | 3 (6.0) | 1 (2.5) | 1 (16.7) | 1 (25.0) |
| Homemaker | 2 (4.0) | 2 (5.0) | 0 (0) | 0 (0) |
| Student | 1 (2.0) | 1 (2.5) | 0 (0) | 0 (0) |
| Income | ||||
| Less than $15 000 | 4 (8.0) | 3 (7.5) | 1 (16.7) | 0 (0) |
| Between $15 000 and $34 999 | 3 (6.0) | 1 (2.5) | 1 (16.7) | 1 (25.0) |
| Between $35 000 and $54 999 | 5 (10.0) | 5 (12.5) | 0 (0) | 0 (0) |
| Between $55 000 and $74 999 | 9 (18.0) | 7 (17.5) | 1 (16.7) | 1 (25.0) |
| Between $75 000 and $94 999 | 6 (12.0) | 6 (15.0) | 0 (0) | 0 (0) |
| More than $95 000 | 19 (38.0) | 16 (40.0) | 1 (16.7) | 0 (0) |
| Prefer not to answer | 4 (8.0) | 2 (5.0) | 2 (33.3) | 2 (50.0) |
| Primary health insuranceb | ||||
| Private | 23 (46.0) | 19 (47.5) | 3 (50.0) | 1 (25.0) |
| Medicaid or Medicare | 26 (52.0) | 20 (50.0) | 3 (50.0) | 3 (75.0) |
| Uniformed Services Health Insurance Program (Tricare) | 13 (26.0) | 10 (25.0) | 1 (16.7) | 2 (50.0) |
| Other (specify) | 1 (2.0) | 0 (0) | 0 (0) | 1 (25.0) |
| Health literacy, adequate | 47 (94.0) | 37 (92.5) | 6 (100) | 4 (100) |
| Health statusc | ||||
| Excellent | 12 (24.0) | 8 (20.0) | 2 (33.3) | 2 (50.0) |
| Very good | 20 (40.0) | 15 (37.5) | 3 (50.0) | 2 (50.0) |
| Good | 14 (28.0) | 13 (32.5) | 1 (16.7) | 0 (0) |
| Fair | 3 (6.0) | 3 (7.5) | 0 (0) | 0 (0) |
| Poor | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Dominant hand before amputationc | ||||
| Right | 46 (92.0) | 38 (95.0) | 5 (83.3) | 3 (75.0) |
| Left | 2 (4.0) | 1 (2.5) | 1 (16.7) | 1 (25.0) |
| Upper limb amputatedc | ||||
| Right | 22 (44.0) | 19 (47.5) | 3 (50.0) | 3 (75.0) |
| Left | 19 (38.0) | 16 (40.0) | 2 (33.3) | 1 (25.0) |
| Both | 8 (16.0) | 4 (10.0) | 1 (16.7) | 0 (0) |
| Amputation type | ||||
| Unilateral | 42 (84.0) | 36 (90.0) | 5 (83.3) | 1 (25.0) |
| Bilateral | 8 (16.0) | 4 (10.0) | 1 (16.7) | 3 (75.0) |
| Amputation level | ||||
| Below elbow | 23 (46.0) | 19 (47.5) | 3 (50.0) | 1 (25.0) |
| Above elbow | 26 (52.0) | 21 (52.5) | 3 (50.0) | 2 (50.0) |
| Both below and above elbow | 1 (2.0) | 0 (0) | 0 (0) | 1 (25.0) |
| Current prosthesis typeb | ||||
| Mechanic | 21 (42.0) | 20 (50.0) | 1 (16.7) | 0 (0) |
| Myoelectric | 20 (40.0) | 18 (45.0) | 2 (33.3) | 0 (0) |
| Cosmetic | 2 (4.0) | 2 (5.0) | 0 (0) | 0 (0) |
| None | 17 (34.0) | 9 (22.5) | 4 (66.7) | 4 (100) |
| Other | 1 (2.0) | 1 (2.5) | 0 (0) | 0 (0) |
| Years since firstd amputation mean [SD] (range) | 9.86 [8.2] (<1–41) | 10.05 [9.0] (<1–41) | 8.59 [4.4] (3–14) | 9.80 [2.6] (6–12) |
| <2 y | 9 (18.0) | 9 (22.5) | 0 (0) | 0 (0) |
| 3–5 y | 10 (20.0) | 8 (20.0) | 2 (33.3) | 6 (0) |
| 6–9 y | 12 (24.0) | 8 (20.0) | 2 (33.3) | 2 (50.0) |
| 10–15 y | 13 (26.0) | 9 (22.5) | 2 (33.3) | 2 (50.0) |
| >15 y | 6 (15.0) | 6 (15.0) | 0 (0) | 0 (0) |
| Study sitee | ||||
| NU | 16 (32.0) | 15 (30.0) | 1 (16.7) | 0 (0) |
| JHU | 17 (34.0) | 8 (16.0) | 5 (83.3) | 4 (100) |
| WRNMMC | 17 (34.0) | 17 (34.0) | 0 (0) | 0 (0) |
a “Other” included people who identified as Hispanic or Mexican (n =3), did not specify (n = 1).
b Percentages add up to greater than 100 due to more than one response from some participants.
c Percentages do not add up to 100 because some participants did not respond.
d Some participants had multiple surgeries for their amputation or multiple amputations, therefore, we used the time between the date of the first amputation surgery and the date of the interview for analysis.
e UE VCA candidates and participants from non-study site VCA programs who contacted the NU team were analyzed as NU study participants.
JHU, Johns Hopkins University; NU, Northwestern University; UE, upper extremity; VCA, vascularized composite allotransplantation; WRNMMC, Walter Reed National Military Medical Center.
Awareness and Perceptions of UE VCA
Among participants with UE amputations who had not pursued UE VCA (n = 40), most were aware of it (67%) and had considered getting an UE VCA (51%) before the research study. Most participants had positive impressions of UE VCA. Some participants were enthusiastic given the procedure’s potential to help individuals regain functionality and its associated benefits. Others were neutral, stating “I feel like it’s a good idea for those who want it, who feel that they need it, and I love that it’s an option for them. Personally, I don’t think so” (C-008).
Willingness to Receive UE VCA
UE amputees and UE VCA candidates and participants varied in their willingness to receive a transplant: 17.4% were “not at all willing,” 21.7% were “a little willing,” 26.1% were “somewhat willing,” 10.9% were “a lot willing,” and 23.9% were “completely willing.” Willingness to pursue UE VCA was unrelated to time since amputation and amputation type.
Decision-Making About UE VCA
Themes that emerged about factors contributing to UE VCA decision-making included the utility of UE VCA, psychosocial impact of UE VCA and amputation on individuals’ lives, altruism, and anticipated burden of UE VCA on lifestyle. Table 2 presents illustrative representative quotations.
TABLE 2.
Representative illustrative quotations about decision making by major theme and subthemea
| Themes Subthemes |
Quotations |
|---|---|
| Decision In Favor of Pursuing UE VCA | |
| Utility of UE VCA | |
| Regain Hand Function | “… The level of amputations that I was at, this was not working. I guess I wanted to do more. I wanted to--I didn’t really know what more was, but I do now because I went through it. … I wanted to have a better quality of life. I mean… picture in your mind what it would be like having a left hand and a right forearm and trying to do things you’re doing now. That was motivation enough, I think.... So, I needed this. I needed to do this because … it gave me hope that I could do things, whatever it was, whatever it is. I don’t let a lot hold me back.” (C-001-R) |
| Prosthetic Limitations | “I mean, a lot of the guys that talk to you that wear the prosthetics, we all have the same issues at the time, the fitting, the mechanics of it, how often they break down, so I’m sure a lot of guys lose patience with those myoelectric prosthetics because they’re always in the shop…. I’d rather have this transplant and work the kinks out in that instead of consistently dealing with that and dealing with the insurance company. So that’s motivating me to want to get this transplant.” (C-002-C/P) |
| Psychosocial Impact of UE VCA | |
| Improve Appearance | “Well, to get my hand back. To feel somewhat normal again, without having-I don’t care if people look, but it’s when they stare and they give you that look-you know which one I’m talking about? The awh look. That, that’s the biggest thing that would cause me to get it, besides having my hand back.” (A-016-A)“Okay, first of all, I wanted to be made full… I wanted to be made full, I wanted to not be broken into pieces. … I was an entrepreneur, I had a bunch of people who worked for me, I had all this stuff, and I was also a body builder and I loved all this, I loved having my arms and the idea that I could get one back was the most amazing thing.” (C-005-R)“OK. Because I think that if I had my arm, if I had the transplant, my life would be whole again. You know, even without my sight, my life would be whole again. I could do things that I can’t do, things that I have to ask someone to help me with. That’s the hardest part for me is that I have to wait and ask someone to do this. Even though they’re willing to do it, I have to wait until they get ready to do it.” (B-017-A) |
| Family Interaction | “What’s motivating me is my kids. You know, they see me, well they see pictures before the accident, and they’re like, ‘Oh, you had two hands?’ … they’ve only known me with one hand, so they’re like, ‘How cool will it be!’ Like, ‘You’ll be able to teach us how to swim,’ because, like I said, I have to depend on other people, and that’s just something that I don’t like to do. Like, depending on other people has really, I mean it’s taught me patience, but it’s motivated me to want to keep pursuing this because other people are not always dependable.” (B-015-C/P) |
| Altruism | “I’ve seen younger soldiers with amputations, and they need to see somebody that’s thriving in a program like that to encourage them and to show them that, hey, this technology is out there. Hey, I am living proof that this does work. You’re going to have to work hard for it, and that motivates me to do that because I’ve seen a group of young men that truly needs someone that can motivate them to that next level and I think getting that transplant and seeing somebody get it, actually making it functional, and living a normal life, that’s something that motivates me is to help others to get to that process.” (C-002-C/P) |
| Decision Against Pursuing UE VCA | |
| Utility of UE VCA | |
| Becoming Worse-off | “I would just really be concerned about the body rejecting it and then having to remove the arm and do another surgery to get rid of the arm. The hand not gaining as much strength in the nerves. Also, yeah, it could end up being more of a nuisance if the arm doesn’t work well and it just – I’ve known people in the past where they’ve had amputations where they had nerve damage in the arm and they’re just like get rid of their arm because it’s just hanging there and it has no strength. So, those are all concerns.” (A-008-A) |
| Risks are not worthwhile | “…getting my arm back to like lose my kidney is like not… and the risk of being on dialysis three days a week, right--three times a week, to me, is worse than not having an arm.” (C-010-C/P)“Yeah, it’s like the risks and the time seemed more negative to me than the pro of having it since there’s no guarantee that it’s gonna work, work properly. I don’t feel like I would want to take that risk.” (C-008-A) |
| Need for optimized functionality | “I would say it would have to be like—it would have to be like 95% success—like functional like I was before. Because as functional as I am with my prosthetic, to give that functionality up, it better damn well be perfect.” (A-033-A) |
| Psychosocial Impact of Amputation | |
| Adaptation | “Some of the things that would make it hard for me is—it’s interesting—I have incorporated the prosthetic into my body image. So I think about myself, I had dreamed about myself with prosthetics. And so I underwent like one revision to what my perception of my body. It would be something difficult, I think, to do that again and to choose to do it. I never chose to be an amputee. I didn’t have—it was not elective, right. It was not like I had cancer and a 6-mo lead up and there was a potential for it. I just blacked out and woke up and was one.” (A-007-A) |
| Identity | “Uh, me personally, I just couldn’t get past the portion of wearing – in my head, I like look at it as wearing somebody else’s arm, like a cadaver arm. Like let’s say even if my dad is a perfect match, and he has a perfectly good arm. And like me to wear somebody else’s arm is like the biggest identity issue I have had with transplants.” (A-002-A) |
| Anticipated Burden of UE VCA on Patient’s Lifestyle | |
| Commitment | “Okay, so it’s the rejection, and it’s that I’ve heard that a lot of work goes into making the hand work and getting the feeling and for it to function in a way that you would want it to. I also heard that it’s very hard. It’s hard work to get it to do that, and it’s not the way that it was before in terms of it working, yeah, and it’s a very long process, and I just don’t have--I’m really not interested in going through such a long process of--I have a family. The importance of getting it is not as important as being present in my life.” (C-008-A) |
| Logistics | “At first, I was considering it, but they told me that I would have to be away from my home for over a year and that it all could, it all boils down to if my system and my limbs would take to the limbs that were donated… I thought about it, but the away from home and time considering it to heal and to adapt was way too long for me.” (B-017-A) |
| Undecided | |
| Desire information on how UE VCA compares to a prosthetic | “What would motivate me would really be, again, to know how does it work differently than a prosthetic, how is it going to enhance my life, my lifestyle. … Like basically, what am I going to get back that my prosthetic cannot give to me or do for me? You know—and this sounds very strange—but something as little as like, I miss washing my hair with two hands. You know? So when I go get my hair done, it’s a treat to have the gentleman shampoo my head with two hands.” (B-022-A) |
| Evidence of successful outcomes | “If I came across someone who was a huge, like they love their arm transplant and were high functioning and it made all their needs as good as they thought or better than they were expecting. They could not (for lack of a better word) talk me into it, but, but push me in that direction. Because if I see that they’re excited about it and successful, then I’m more inclined to get more information and talk to medical staff about it. Instead of just doing solo search on my own.” (A-003-A) |
| Research studies | “I think if there was enough studies done or if there was enough research done and I was given some concrete information of what I am to expect.” (B-025-A) |
| Costs | “I also question the cost of such a thing, if that would be out of pocket, or if that’s an insurance thing. I don’t know. I don’t have any idea about that. And if it is an out-of-pocket thing, it would be beyond my financial abilities, so that would be a consideration also.” (B-011-A) |
| Good candidate | “First would be physically, am I a candidate of it? … I have a very short residual limb, and, physically, could this, is this an option for me? And secondly, … my thought process would be is it worth it? You know, at this stage of my life—I’m 46 y into the game as an amputee or a person with limb loss—and, you know, thinking of, ‘OK, I’m going to go a year—I don’t know, six months, I’m thinking six months to a year before I kind of have limited function of a transplanted limb—and is it worth it at this stage of the game, 46 y later?’ And the third thing is, do I want to make that commitment to that at this stage of the game? And fourth is do I want to change my life to make this happen, to make this a reality?” (B-019-A) |
a To protect participants’ privacy, we anonymized the study sites to A, B, or C, which appear at the beginning of the respondent’s ID#. Respondents with an amputation are designated as (A), or who were either a candidate or participant are designated as (CP), or who were VCA recipients are designated as (R) at the end of their ID#.
UE, upper extremity; VCA, vascularized composite allotransplantation.
Factors in Favor of Pursuing UE VCA
Individuals’ decisions in favor of pursuing UE VCA organized by theme included (1) utility of UE VCA (regaining hand function through UE VCA and the desire to avoid prosthetic limitations); (2) psychosocial impact of UE VCA (on improving appearance, gaining confidence in social settings, and increasing family interactions); and (3) altruism.
- 1. Utility of UE VCA
- A. Regain hand function: Participants hoped the transplanted limb would function “just like your old hand.” Participants specified activities they desired engaging in “bodybuilding,” “washing my hair,” “[picking] up a glass of wine,” and “[holding] the telephone.” Through regained function, individuals would anticipate renewed independence.
-
B.Prosthetic limitations: Study participants perceived that UE VCA would address limitations experienced with using prosthetics, including pain and discomfort. Additionally, participants expected that UE VCA would bypass the challenges of daily prosthetic maintenance (eg, donning and doffing, charging, frequent repairs). Furthermore, participants expected that UE VCA would work better than prosthetics.
- 2. Psychosocial impact of UE VCA
- A. Improve appearance: Some participants reckoned that UE VCA would improve their appearance, identity, and help with social reintegration. Some wanted a transplanted limb for their body “to be made full” or “complete.” Improved appearance would help them to “deal with people in public,” “identify with people,” and feel more confident.
- B. Family interaction: Some participants were motivated by the prospect of engaging in more activities with their child, which is currently challenging or impossible for them. Participants related how the new limb would enable them to “play with my kids,” “hold my kids,” and “teach them how to swim.”
- Altruism
- 3. A few participants were motivated to pursue UE VCA to help other people, particularly children and Service members, and help “to get the word out [that] this thing really works.” Participants desired to serve as a role model so that others know that UE VCA is available and feasible.
Factors Against Pursuing UE VCA
Decisions against pursuing UE VCA organized by theme included concerns about the utility of UE VCA, psychosocial impact of having adapted to amputation and identity concerns, and anticipated burden of UE VCA on lifestyle by commitment to rehabilitation and life-long immunosuppression and logistical barriers to UE VCA transplantation and rehabilitation.
- Utility of UE VCA
- 1. Respondents expressed doubts about the utility, functionality, or potential benefit of an UE VCA. Specifically, some feared that UE VCA would render them “worse off” in terms of losing more of their residual limb because of rejection and re-amputation surgeries. Others stated that the elevated risks of infection, immunosuppression, rejection, pain, and complications for the uncertain benefits would not be worth the effort. Some stated that they would not want to “jeopardize” their current level of functioning or risk going “backwards” because of health problems from UE VCA.
- A. Psychosocial impact of amputation
- Adaptation: Adaptation to life with prosthetics or without an upper limb(s) was a key factor that reduced some participants’ enthusiasm about UE VCA. Adaptation meant that participants had already learned to maintain “a decent way of life” after amputation, incorporated the prosthetic into their body image, and/or were satisfied with their function.
- B. Identity: A few conveyed that “wearing somebody else’s arm” would be “strange.” Participants expressed the challenge of overcoming perceptions of a transformed identity likened to “Frankenstein.”
- 3. Anticipated burden of UE VCA on lifestyle
- A. Commitment: Another factor dissuading respondents from considering UE VCA was the “big commitment” to prolonged rehabilitation and life-long immunosuppressants. Specifically, the extensive (2+ y) time investment and rigorous rehabilitation were not aligned with their life’s priorities. Some recognized that such a commitment would affect their relationships with others, including being away from family and needing support from employers for long-term time off from work. Several participants reflected on their past experiences of recovering from amputation surgery(ies) that involved investing emotional, mental, and physical energy toward healing and were averse to reliving that process and facing the “setback from my current level of independence,” especially given the “question of how functional it would be and how much risk would be involved.” Moreover, UE VCA would introduce new health concerns that respondents did not want to deal with “Because now you’re having to worry about your everyday health.”
- B. Logistics: Respondents reported that the distance between their home and the transplant center would factor negatively into their decision-making. Traveling the distance to the transplant center and/or the frequency of visits would be “burdensome” and “extraordinarily difficult.” A few respondents bemoaned the idea of moving away from their homes to live near the transplant center, displacing family members during and after the procedure.
Undecided
Some respondents needed more information before deciding, including the benefits, risks, eligibility, costs, and UE VCA research advancements. Many reported wanting to know how UE VCA function compares to prosthetic’s function (eg, percentage of function regained, fine motor skill capabilities, and wrist rotation). Others related that learning about research advancements in UE VCA and their eligibility as candidates would provide assurance about pursuing it.
Optimal Time to Inform Patients About UE VCA
Participants commented on the optimal time for people with UE amputations to be informed about UE VCA as a treatment option in relation to their amputation surgery (Table 3). Many respondents reported that the best time is “as soon as possible” (eg, before a scheduled amputation surgery or within days or weeks post-amputation) because “every person should be given the option for how they want to live their life…” (C-009-A) and to give “hope.” Some acknowledged that the earliest practical time would be after patients recovered physically and psychologically; being off pain medication could help them “think clearly.” Others suggested that UE VCA and prosthetic information should be provided concurrently and early so that patients know all their options.
TABLE 3.
Representative illustrative quotations about optimal time to inform patients about UE VCA and informed consent elements by major theme and subthemea
| Themes Subthemes | Illustrative Quotations |
|---|---|
| Optimal Time to Inform | |
| As soon as possible, after healing | “As soon as possible. As soon as possible. And I know, myself, feel like it’s a lot of pressure on an amputee because they just had an amputation and their mind is literally—they’re literally going crazy in their head. But, I would think after they recover from the amputation … and before they get discharged from the hospital, give them that information. … For one, I guess the psychological portion of it is the amputee could say ‘okay wait a minute, I lost my hand. You know they did tell me about this process and…’ So, there’s hope, you know, there’s hope, there is options. Instead of someone setting you up with prosthetic appointment and you go in there and you don’t know what the hell you’re looking at—it’s more depressing. That’s the worst. Like ‘Okay, I’ll wear a prosthetic the rest of my life’ or like, ‘Wait a minute, what about this hand transplant’. … I think they need to do as soon as possible.” (A-017-A) |
| At the same time as informing patients about prosthetics | “And I think it has to go hand in hand with the discussion about prosthetics. [laughter] … If a prosthetist is coming into the patient’s room at the hospital, why can’t a limb transplant doc come into the patient’s room and say, you know, ‘I know that you’ve talked about prosthetics. Well, here are your options for limb transplant as well.’ It should happen at the same time. Why not?” (B-019-A) |
| A few months to a year | “Honestly, I think as soon as they’re ready. In my experience, I think I was told pretty fairly early on, maybe like, six months to a year after my amputations. I had no issue with that. It was an easy thing to consider. Honestly, if I was further along with my therapy and rehab, I think maybe it would have been a more difficult decision, if I was more settled in. But I’m not sure, because I’m sure I wouldn’t have liked prosthetics still, because I didn’t like them throughout my whole time using them.” (C-004-R) |
| 1–2 y post-amputation | [laughter] “I’m kind of leaning immediate postop, but I wouldn’t want to give the person false hope, so I’m hesitant to say that. I feel like the patient should experience and then reject current technology prosthetically. So probably a year to two years post amputation, so that they’ve had time to learn the limitations of the prosthetics and still have that internal drive to want more. If I were to wake up post-surgical amputation and someone go, ‘Hey, yeah! We can bolt another arm onto you,’ I might be like, ‘Oh, yeah! Let’s do that!’ But not fully comprehend what that entails and what it involves. So I think a year to two post amputation, and having that experience of trying and not being successful or trying and wanting more prosthetically.” (B-021-A) |
| Informed Consent Elements | “I had a meeting with the team of doctors and representatives from, at the time, Pittsburgh and they pretty much laid everything out for me as the possibilities of what could happen and the goal of basically rebuilding me and giving me that independence that I desperately needed, and it was very nice.” (C-004-R) |
| Disclosure | “Honestly, I think it all was very important. I think you really have to prepare for what you’re about to go through and how much it’s going to take out of you at the time. It’s a major surgery and I don’t think you can have enough information about it.” (C-004-R)“But just basing it off of my knowledge I feel that it was very informed. They explained everything in detail. And I know that my dad was with me, and we had some questions, and it was basically questions that really wasn’t pertaining to the transplant. It was more about like what about this guy’s fingerprints. What if he was, you know, criminal or whatever? And, they actually answered all those questions. So those were probably the hardest questions or hardest answers okay to make--especially for the doctors, but they had the answers.” (C-001-R) |
| Alternatives | “Alternatives? Just, to me, nothing. I don’t want to get a prosthetic arm. I just didn’t have good luck. It’s spending a lot of money for something that didn’t end up working.” (C-006-C/P) |
| Voluntariness | “I mean, my girl, or my fiancée, like, doesn’t, like, want me to get it done, but like I do and my parents do, and so it’s kind of like two, like, you know, a couple want me to get it done, I want to get it done, my fiancée doesn’t, so it’s, there’s like, kind of like a conflict there...” (B-012-A) |
a To protect participants’ privacy, we anonymized the study sites to A, B, or C, which appear at the beginning of the respondent’s ID#. Respondents with an amputation are designated as (A), or who were either a candidate or participant are designated as (CP), or who were VCA recipients are designated as (R) at the end of their ID#.
UE, upper extremity; VCA, vascularized composite allotransplantation.
By contrast, all UE VCA recipients and several others reported that UE VCA information should be provided a few months to 1-y post-amputation to “give the person time to adjust, cope, and deal with their new normal” (B-011-A). Some emphasized 1–2 y post-amputation so that patients have “a chance to try out prosthetic devices,” time to “grieve” their limb loss, and “process what they are going through.” Otherwise, if patients are informed too early, a few cautioned against making an “impulse decision” they may regret in the long term.
Informed Consent Elements
Among the 10 UE VCA candidates, participants, and recipients who underwent the UE VCA informed consent process, 6 who commented reported a positive experience: “I can’t see anything that I could have asked for them to do better” (C-002-CP). Table 3 presents illustrative representative quotations of perceptions of informed consent.
Disclosure
All 8 UE VCA participants and recipients commenting about the disclosure process valued the information the transplant team disclosed. No one perceived the information as not important. Four commented that the transplant team was “very open,” “very detailed,” and respondents felt “very informed” about UE VCA.
Information was most commonly provided in pamphlets, verbally, and by email. Respondents disliked paper packets due to difficulty “turning pages,” or found information “overwhelming.” Instead, they suggested providing information in a “digital form,” such as a website, and in “little sections” to prevent overwhelming patients.
Alternatives
Among the 8 UE VCA candidates, participants, and recipients who discussed alternatives to UE VCA, all identified prosthetics, or no treatment, as alternatives to transplantation. Some expressed discontent with prosthetics because of their poor functionality, lack of sensation, and high cost. Accordingly, respondents did not consider prosthetics as acceptable treatment options for individuals with UE amputations.
Comprehension
UE VCA candidates, participants, and recipients expressed no challenges with comprehending disclosed information. Among 7 respondents, all reported that the transplant team checked their understanding during the consent process. Strategies used by the team included asking questions to confirm comprehension, “testing” the patient: “[they] would say things that were incorrect to see if I pick up on it… almost like a quiz,” meeting multiple times, and the psychiatrist meeting with the patient to confirm understanding of psychological aspects of UE VCA.
Voluntariness
Among all study participants, 18% (n = 9/50, including 1 recipient, 1 participant, 1 candidate, and 6 individuals with UE limb loss) reported personally feeling “a little,” “somewhat,” “a lot,” or “completely” pressured to pursue UE VCA (Table 4). These 9 individuals experiencing pressure recognized external and self-driven factors as sources of pressure. Study participants also identified sources of potential pressure to pursue UE VCA that other individuals with UE amputations may encounter. For example, people may feel pressure from family to look “normal” or become independent; and societal pressure to “fit in,” maintain a body image with 2 upper limbs, and avoid being labeled as disabled. Study participants acknowledged that the medical community might exert pressure on individuals to advance the field of VCA and increase the number of procedures performed. Moreover, study participants identified that some may experience personal pressures to restore a sense of wholeness, be independent, not be a burden to others, and continue their careers. Conversely, others reported pressure to not pursue VCA. For example, 2 individuals wanted to pursue UE VCA, but their family did not agree; to avoid conflict, participants decided against this treatment option.
TABLE 4.
Voluntariness of decision to pursue UE VCA
| Variable | Total N = 50 N (%) | UE amputees N = 40 n (%) | UE VCA candidates/participants N = 6 n (%) | UE VCA recipients N = 4 n (%) |
|---|---|---|---|---|
| Pressure to get UE VCA | ||||
| Not at all | 41 (82.0) | 34 (95.0) | 4 (66.7) | 3 (75.0) |
| A little | 2 (4.0) | 1 (2.5) | 0 (0.0) | 1 (25.0) |
| Somewhat | 4 (8.0) | 3 (10.0) | 1 (16.7) | 0 (0.0) |
| A lot | 2 (4.0) | 2 (5.0) | 0 (0.0) | 0 (0.0) |
| Completely | 1 (2.0) | 0 (0.0) | 1 (16.7) | 0 (0.0) |
UE, upper extremity; VCA, vascularized composite allotransplantation.
Likelihood of Using Educational Materials About UE VCA
Among respondents asked, most reported being “a lot” or “completely” likely to use a website (95.7% n = 45/47) and watch a video (93.5% n = 43/46) about UE VCA if they were considering the procedure.
DISCUSSION
In this multisite qualitative study, we identified myriad psychosocial and ethical factors influencing decision-making and perceptions of elements of informed consent about UE VCA. A major theme representing decisions about pursuing UE VCA pertained to utility associated with regaining hand function and overcoming prosthetic limitations, as other research found.30 Conversely, respondents not considering UE VCA reported doubts about UE VCA’s functionality and benefits (eg, fear of becoming worse-off). Other research similarly identified concerns with rejection and subsequent amputation.30
Another key theme pertained to psychosocial factors. Although those in favor of UE VCA were compelled by UE VCA’s promise of improved appearance and increased family interaction, others were less enthusiastic after having adapted to limb loss, consistent with previous research.30 We found that willingness to pursue UE VCA was statistically unrelated to time since amputation. Talbot and colleagues found an inverse relationship between patients’ interest in UE VCA and adjustment time since amputation.31 Patients also reported identity concerns of transforming into “Frankenstein”52 through VCA, as found elsewhere.53
Other study participants desired further information before deciding,17 including about costs and insurance coverage, as documented elsewhere.30 Consistent with previous research, a key finding was limited knowledge about UE VCA among individuals with UE amputations.30
Transplant providers’ shared decision-making process with potential UE VCA recipients should address the psychosocial factors pertaining to the pre-transplant course that our respondents identified to enhance the informed consent process. Toward this end, transplant providers could structure their shared decision-making discussion according to the elements of informed consent. Specifically, providers should disclose information about UE VCA, as reported herein and elsewhere,17 regarding the UE VCA eligibility criteria; risks; potential benefits; timeline of transplant evaluation steps and recovery; rehabilitation process and role of caregivers; and the potential impact of UE VCA on patient’s identity, family, finances, and lifestyle, among other topics. A discussion of the patients’ perceptions of viable alternatives to UE VCA would provide insight into their motivation to pursue UE VCA and perceived voluntariness. Throughout the discussion, providers should assess patient comprehension; use of the teach back method can be used to ascertain patients’ level of understanding. Additionally, the multidisciplinary team should be prepared to engage in shared decision-making post-transplant among transplant recipients about exit strategies in case of graft failure (ie, amputation of the transplanted hand(s) or re-transplantation).54 Future research that assesses patients’ exit strategy preferences could inform this discussion.
We found that although most individuals with UE amputations believed that the best time to be informed about UE VCA is as soon as possible, all UE VCA recipients preferred a few months to 1-y post-amputation. As respect for dignity requires a “thorough exploration of alternatives,”15 whenever possible, healthcare providers should discuss all treatment options prior to amputation. By gauging patient interest in UE VCA over time, providers may better accommodate variation in preferences for disclosure. We acknowledge that some transplant clinicians believe that a conservative and thoughtful approach to UE VCA requires failure of prosthetics as an eligibility criterion.55 The disconnection between patient and clinician preferences may be cause for reassessment of assumptions underlying clinical practice decisions regarding patient selection, as is occurring across organs.56,57
Some respondents pursuing UE VCA did not perceive having reasonable treatment options because of prosthetic challenges and resulting limited independence, as ethical analyses have acknowledged.15 Without perceived alternatives, individuals with UE amputations may be more inclined to pursue UE VCA, as our study participants indicated.
The method of information disclosure presented challenges unique to this population. Transplant programs should use digital platforms (eg, websites with voice-over applications) to provide information in a culturally tailored medium to avoid providing information in paper pamphlets, which can be difficult to handle for individuals with UE amputations. Our team developed a neutral, ADA-compliant, culturally sensitive website, Within Reach [www.withinreach.info], to help individuals and families make informed decisions about UE VCA.58 Most respondents reported being likely to review a website if they were considering UE VCA. Future research should assess how Within Reach affects informed decision-making and expectation management for UE VCA.
A noteworthy finding was that 18% of respondents reported experiencing some level of pressure to pursue UE VCA. It is unclear whether this proportion is ethically acceptable or alarming. Study participants identified sources of potential pressure to pursue UE VCA, including from the medical community. Transplant clinicians should maintain caution and neutrality when informing individuals about UE VCA given patients’ vulnerability to succumb to such pressures due to their UE amputation(s), which can interfere with autonomous treatment decision-making. Study participants recognized that physicians may be motivated to offer UE VCA to advance the field, which may not align with patients’ preferences. The Brocher Bioethics Working Group confirmed this finding, acknowledging that VCA transplant programs may exert pressure on providers to meet milestones in federally funded grants or be the first in the field to achieve novel outcomes.15 Independent patient advocates may protect patients from potential duress.15
Our findings may inform the development of the U.S. Organ Procurement and Transplant Network guidelines to standardize information disclosed to UE VCA candidates in the informed consent process.59 We recommend incorporating metrics of informed consent (eg, perceptions of information needs being addressed, information comprehended, making a voluntary decision) as patient-reported outcome measures to foster standardization of the informed consent process.
Study strengths include recruitment of individuals with UE amputation and UE VCA candidates, participants, and recipients, across different geographic regions, amputation types, and durations of time since amputation, which increase the transferability of our study findings across diverse UE populations. Varied knowledge about UE VCA also supports transferability. Although our sample population was comprised of primarily male and White individuals with unilateral amputation(s), it is comparable to individuals with UE amputations nationally by gender, race, age, and amputation type.60,61
We recognize that some VCA clinicians believe that individuals with unilateral amputation are generally not ideal candidates for UE VCA because they can do most of what a person with 2 arms can do, which may not justify the risks of immunosuppression. We found that some individuals with unilateral amputation still desired UE VCA. This disconnection between patient and clinician preferences raises the question of optimal candidate selection and reassessing clinical assumptions may foster clarity on this matter.
This study has limitations. Nearly all UE VCA candidates, participants, and recipients were recruited from one UE VCA transplant program, which may limit generalizability to other UE VCA programs. Although some respondents’ replies may not reflect actual decisions, their thought processes likely reflect factors that UE VCA candidates consider. Our results were unlikely to have been influenced by selection bias because our sample expressed factors in favor of and against UE VCA. We did not offer information about UE VCA before interviews because it did not coincide with study goals, consistent with other VCA research practices.62 Further research should assess international perceptions of UE VCA decision-making and informed consent.
Our study identified novel psychosocial and other factors driving decision-making, and perceptions of elements of informed consent for UE VCA, which may impact patients’ autonomous treatment decision-making. The informed consent process should address utility, psychosocial, and burden-related concerns to support patients’ informed decision-making. Information disclosed to patients should address their UE VCA concerns to instill realistic expectations, put patients at ease, and make them feel prepared for the procedure.
ACKNOWLEDGMENTS
We thank Withney Altema, Shannon Fichter, and Michelle Luken for their research assistance. We also thank our scientific advisory board members: James DuBois, Edmund Howe, Ana Iltis, and Richard Sharp. Research Electronic Data Capture, a secure online data capture application, is supported at the Feinberg School of Medicine by the NU Clinical and Translational Science Institute. Research reported in this publication was supported in part by the NIH’s National Center for Advancing Translational Sciences, grant UL1TR001422. This work was also supported in part by the Northwestern Medicine Enterprise Data Warehouse.
Supplementary Material
Footnotes
The authors declare no conflicts of interest.
This study was supported by the Department of Defense through the Congressionally Directed Medical Research Program (CDMRP) Reconstructive Transplant Research Program (RTRP) grant awards: Initiating Principal Investigator: E.J.G. (Grant No. W81XWH-19-2-0033); Partnering Principal Investigators: M.L. (Grant No. W81XWH-19-2-0034); G.B. (Grant No. W81XWH-19-2-0035), S.T. (Grant W81XWH1920036). The opinions and assertions expressed herein are those of the authors and do not necessarily reflect the official policy or position of the Uniformed Services University or the Department of Defense. The opinions and assertions expressed herein are those of the authors and do not necessarily reflect the official policy or position of the Henry M. Jackson Foundation for the Advancement of Military Medicine. The views expressed in this manuscript are those of the author(s) and do not necessarily reflect the official policy of the Department of Defense or the U.S. Government. The identification of specific products and scientific instrumentation does not constitute endorsement or implied endorsement on part of the authors, DOD or any component agency. The funders had no role in study design; collection, analysis, and interpretation of data; writing the report; and the decision to submit the report for publication.
The following authors have made substantial contributions to the conception or design of the work: E.J.G.; the acquisition, analysis, or interpretation of data: E.J.G., J.G.-S., B.R.K., M.D., K.B.V., M.J.N., T.R., S.J., and C.M.C.; drafted the work or substantively revised it: E.J.G.; provided access to their patient populations for study recruitment: G.B., S.T., and G.D. All authors have approved the submitted version and have agreed both to be personally accountable for the author’s own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
The data sets generated during and/or analyzed during the current study are not publicly available due to lack of available funding but are available from the corresponding author on reasonable request.
Supplemental digital content (SDC) is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal’s Web site (www.transplantationdirect.com).
REFERENCES
- 1.Ostlie K, Franklin RJ, Skjeldal OH, et al. Assessing physical function in adult acquired major upper-limb amputees by combining the Disabilities of the Arm, Shoulder and Hand (DASH) Outcome Questionnaire and clinical examination. Arch Phys Med Rehabil. 2011;92:1636–1645. [DOI] [PubMed] [Google Scholar]
- 2.Belon HP, Vigoda DF. Emotional adaptation to limb loss. Phys Med Rehabil Clin N Am. 2014;25:53–74. [DOI] [PubMed] [Google Scholar]
- 3.Sheehan TP, Gondo GC. Impact of limb loss in the United States. Phys Med Rehabil Clin N Am. 2014;25:9–28. [DOI] [PubMed] [Google Scholar]
- 4.Ziegler-Graham K, MacKenzie EJ, Ephraim PL, et al. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Arch Phys Med Rehabil. 2008;89:422–429. [DOI] [PubMed] [Google Scholar]
- 5.Biddiss EA, Chau TT. Upper limb prosthesis use and abandonment: a survey of the last 25 years. Prosthet Orthot Int. 2007;31:236–257. [DOI] [PubMed] [Google Scholar]
- 6.Ostlie K, Lesjo IM, Franklin RJ, et al. Prosthesis rejection in acquired major upper-limb amputees: a population-based survey. Disabil Rehabil Assist Technol. 2012;7:294–303. [DOI] [PubMed] [Google Scholar]
- 7.Shores JT, Malek V, Lee WPA, et al. Outcomes after hand and upper extremity transplantation. J Mater Sci Mater Med. 2017;28:72. [DOI] [PubMed] [Google Scholar]
- 8.Dean WK, Talbot SG. Vascularized composite allotransplantation at a Crossroad: adopting lessons from technology innovation to novel clinical applications. Transplantation. 2017;101:452–456. [DOI] [PubMed] [Google Scholar]
- 9.Jowsey-Gregoire SG, Kumnig M, Morelon E, et al. The Chauvet 2014 Meeting Report: psychiatric and psychosocial evaluation and outcomes of upper extremity grafted patients. Transplantation. 2016;100:1453–1459. [DOI] [PubMed] [Google Scholar]
- 10.Wainright JL, Booker SE, Cherikh WS, et al. Vascularized composite allograft transplantation in the United States: current state of the field and future challenges. Transplantation. 2022;106:2093–2096. [DOI] [PubMed] [Google Scholar]
- 11.Breidenbach WC, 3rd, Tobin GR, 2nd, Gorantla VS, et al. A position statement in support of hand transplantation. J Hand Surg Am. 2002;27:760–770. [DOI] [PubMed] [Google Scholar]
- 12.Van Pilsum Rasmussen SE, Uriarte J, Anderson N, et al. Public education materials about vascular composite allotransplantation and donation in the United States: current scope and limitations. Clin Transplant. 2020;34:e14066. [DOI] [PubMed] [Google Scholar]
- 13.Cooney CM, Siotos C, Aston JW, et al. The ethics of hand transplantation: a systematic review. J Hand Surg Am. 2018;43:84.e1–84.e15. [DOI] [PubMed] [Google Scholar]
- 14.Caplan AL, Parent B, Kahn J, et al. Emerging ethical challenges raised by the evolution of vascularized composite allotransplantation. Transplantation. 2019;103:1240–1246. [DOI] [PubMed] [Google Scholar]
- 15.Magill G, Benedict J, Plock JA, et al. ; Brocher Working Group on VCA. Existing and evolving bioethical dilemmas, challenges, and controversies in vascularized composite allotransplantation: an international perspective from the Brocher bioethics working group. Transplantation. 2019;103:1746–1751. [DOI] [PubMed] [Google Scholar]
- 16.Bracken-Roche D, Bell E, Karpowicz L, et al. Disclosure, consent, and the exercise of patient autonomy in surgical innovation: a systematic content analysis of the conceptual literature. Account Res. 2014;21:331–352. [DOI] [PubMed] [Google Scholar]
- 17.Gacki-Smith J, Kuramitsu BR, Downey M, et al. Information needs and development of a question prompt sheet for upper extremity vascularized composite allotransplantation: a mixed methods study. Front Psychol. 2022;13:960373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Miller ME, Siegler M, Angelos P. Ethical issues in surgical innovation. World J Surg. 2014;38:1638–1643. [DOI] [PubMed] [Google Scholar]
- 19.Broekman ML, Carrière ME, Bredenoord AL. Surgical innovation: the ethical agenda: a systematic review. Medicine (Baltim). 2016;95:e3790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee Char SJ, Hills NK, Lo B, et al. Informed consent for innovative surgery: a survey of patients and surgeons. Surgery. 2013;153:473–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Elliott D, Ochieng CA, Zahra J, et al. What are patients told about innovative surgical procedures? a qualitative synthesis of seven case studies in the UK. Ann Surg. [Epub ahead of print]. 2022. doi: 10.1097/sla.0000000000005714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gesualdo F, Daverio M, Palazzani L, et al. Digital tools in the informed consent process: a systematic review. BMC Med Ethics. 2021;22:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shlobin NA, Sheldon M, Lam S. Informed consent in neurosurgery: a systematic review. Neurosurg Focus. 2020;49:E6. [DOI] [PubMed] [Google Scholar]
- 24.Glaser J, Nouri S, Fernandez A, et al. Interventions to improve patient comprehension in informed consent for medical and surgical procedures: an updated systematic review. Med Decis Making. 2020;40:119–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bennett J. Limb loss: the unspoken psychological aspect. J Vasc Nurs. 2016;34:128–130. [DOI] [PubMed] [Google Scholar]
- 26.Nielsen C. A survey of amputees: functional level and life satisfaction, information needs, and the prosthetist’s role. JPO Journal of Prosthetics & Orthotics. 1991;3:125–129. [Google Scholar]
- 27.Pedlow H, Cormier A, Provost M, et al. Patient perspectives on information needs for amputation secondary to vascular surgery: what, when, why, and how much? J Vasc Nurs. 2014;32:88–98. [DOI] [PubMed] [Google Scholar]
- 28.Pasquina CP, Carvalho AJ, Sheehan TP. Ethics in rehabilitation: access to prosthetics and quality care following amputation. AMA J Ethics. 2015;17:535–546. [DOI] [PubMed] [Google Scholar]
- 29.Jensen SE, Butt Z, Heinemann AW, et al. Perceptions of the risks and benefits of upper limb transplantation among individuals with upper limb amputations. Plast Reconstr Surg. 2014;134:979–987. [DOI] [PubMed] [Google Scholar]
- 30.Finnie D, Griffin JM, Kennedy CC, et al. Education for patients with limb loss or absence: aging, overuse concerns, and patient treatment knowledge gaps. Front Psychol. 2022;13:953113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Talbot SG, Carty MJ, Jensen SE, et al. Adjustment to amputation and interest in upper limb transplantation. SAGE Open Med. 2019;7:2050312119858248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Creswell J, Plano Clark V. Designing and Conducting Mixed Methods Research. Sage Publications; 2007. [Google Scholar]
- 33.Gordon EJ, Levin BW. Contextualizing Ethical Dilemmas: Ethnographic Methods in Bioethics. In: Jacoby L, Siminoff L, eds. Empirical Methods for Bioethics: A Primer (Advances in Bioethics, Volume 11). Elsevier; 2008:83–116. [Google Scholar]
- 34.The National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research. The Belmont Report. 1978. Available at https://www.hhs.gov/ohrp/regulations-and-policy/belmont-report/index.html. Accessed June 21, 2023.
- 35.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19:349–357. [DOI] [PubMed] [Google Scholar]
- 36.Coyne IT. Sampling in qualitative research. Purposeful and theoretical sampling; merging or clear boundaries? J Adv Nurs. 1997;26:623–630. [DOI] [PubMed] [Google Scholar]
- 37.Patton M. Qualitative Research & Evaluation Methods, 4th ed. Sage Publications; 2015. [Google Scholar]
- 38.Morse A. Analytic strategies and sample size. Qual Health Res. 2015;25:1317–1318. [DOI] [PubMed] [Google Scholar]
- 39.Morse J. Determining sample size. Qual Health Res. 2000;10:3–5. [Google Scholar]
- 40.Bernard H. Social Research Methods. Sage Publications; 2000. [Google Scholar]
- 41.Siminoff LA, Seltzer D. Semi-Structured Interviewing: A Guide to Survey Techniques and Procedures. Western Reserve University; 1994. [Google Scholar]
- 42.Morris NS, MacLean CD, Chew LD, et al. The Single Item Literacy Screener: evaluation of a brief instrument to identify limited reading ability. BMC Fam Pract. 2006;7:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Schwarz N, Sudman S, eds. Answering Questions: Methodology for Determining Cognitive and Communicative Processes in Survey Research. Jossey-Bass; 1996. [Google Scholar]
- 44.Singleton R, Straits B. Approaches to Social Research, 4th ed. Oxford University Press; 2005. [Google Scholar]
- 45.Bernard H, Ryan G. Text Analysis: Qualitative and Quantitative Methods. In: Bernard H, ed. Handbook of Methods in Cultural Anthropology. Altamira Press; 1998:595–646. [Google Scholar]
- 46.Miles M, Huberman A. Qualitative Data Analysis: An Expanded Sourcebook, 2nd ed. Sage Publications; 1994. [Google Scholar]
- 47.Giacomini M, Cook D. Users’ guides to the medical literature: XXIII. qualitative research in health care A. Are the results of the study valid? Evidence-Based Medicine Working Group. JAMA. 2000;284:357–362. [DOI] [PubMed] [Google Scholar]
- 48.Bradley E, Curry L, Devers K. Qualitative data analysis for health services research: developing taxonomy, themes, and theory. Health Services Res. 2007;42:1758–1772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lincoln Y, Guba E. Naturalistic Inquiry. Sage Publications; 1985. [Google Scholar]
- 50.Guest G, MacQueen K, Namey E. Applied Thematic Analysis. Sage Publishers; 2012. [Google Scholar]
- 51.Keith RE, Crosson JC, O’Malley AS, et al. Using the Consolidated Framework for Implementation Research (CFIR) to produce actionable findings: a rapid-cycle evaluation approach to improving implementation. Implement Sci. 2017;12:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Shelley M. Frankenstein. Penguin Classics; 2012. [Google Scholar]
- 53.Ferzola A, Uriarte J, Sung HC, et al. Public perceptions and information needs of VCA transplantation and donation: a mixed methods study. Transpl Int. 2022;35:10752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kumnig M, Jowsey-Gregoire SG, Gordon EJ, et al. Psychosocial and bioethical challenges and developments for the future of vascularized composite allotransplantation: a scoping review and viewpoint of recent developments and clinical experiences in the field of vascularized composite allotransplantation. Front Psychol. 2022;13:1045144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Shores JT. Recipient screening and selection: who is the right candidate for hand transplantation. Hand Clin. 2011;27:539–543, x. [DOI] [PubMed] [Google Scholar]
- 56.Strauss AT, Sidoti CN, Purnell TS, et al. Multicenter study of racial and ethnic inequities in liver transplantation evaluation: understanding mechanisms and identifying solutions. Liver Transpl. 2022;28:1841–1856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ladin K, Emerson J, Berry K, et al. Excluding patients from transplant due to social support: results from a national survey of transplant providers. Am J Transplant. 2019;19:193–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Vanterpool K, J G-S, Kuramitsu B, et al. A patient-centered website (within reach) to foster informed decision-making about upper extremity vascularized composite allotransplantation: development and usability study. JMIR Form Res. 2023;7: e44144 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Rose J, Cooney CM, Kaufman C, et al. Evolving ethics, policy and reimbursement issues of vascularized composite allotransplantation: symposium summary. SAGE Open Med. 2019;7:2050312119866944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Inkellis E, Low EE, Langhammer C, et al. Incidence and characterization of major upper-extremity amputations in the National Trauma Data Bank. JB JS Open Access. 2018;3:e0038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.U.S. Department of Health and Human Services, Organ Procurement and Transplant Network. Transplants in the U.S. by Recipient Ethnicity, U.S. Transplants Performed: January 1, 1988 - February 28, 2023, For Organ = Upper Limb: Bilateral, and Unilateral. Based on OPTN data as of March 23, 2023. Available at: https://optn.transplant.hrsa.gov/data/view-data-reports/national-data/#. Accessed March 25, 2023.
- 62.Jensen S, Butt Z, Heinemann A, et al. Adjustment to amputation and attitudes toward upper limb transplantation: Implications for patient selection. 2014. AAHS (American Association for Hand Surgery) Annual Meeting. Available at: https://meeting.handsurgery.org/abstracts/2014/36.cgi. Accessed June 21, 2023. [Google Scholar]