Abstract
Metabolic syndrome X has been known to be a risk factor for the development of cardiovascular dysfunction. Insulin resistance, diabetes mellitus and serum lipid abnormalities, which are all seen in metabolic syndrome X, have been found to negatively impact heart function, leading to heart failure in particular. Heart failure is a condition resulting when the heart is unable to perform its function of providing sufficient blood flow to meet the body’s requirements. The treatment of heart failure in metabolic syndrome X varies based on the various components of metabolic syndrome X, which include obesity, hyperglycemia, hypertension and dyslipidemia. Obesity is regarded as one of the derangements seen in patients with metabolic syndrome X. It is a significant risk factor in the development of cardiovascular disease, which may eventually lead to heart failure. However, the obesity paradox suggests that obesity provides a higher chance of survival in patients with metabolic syndrome and heart failure. This review article focuses on the pathophysiology of heart failure in patients who already have metabolic syndrome X, as well as the therapeutic management complexity of the two conditions taking into consideration the protective role provided by obesity.
Keywords: Metabolic syndrome, insulin resistance, obesity paradox, heart failure, obesity.
SUMMARY
1. Introduction
2. Prevalence and incidence
3. Morbidity and mortality
4. Association of heart failure and metabolic syndrome X
5. Pathogenesis of heart failure in metabolic syndrome X patients
6. Diagnosis
7. Heart failure’s treatment in metabolic syndrome X
8. Prognosis
9. Conclusion
1. Introduction
Metabolic syndrome, also known as insulin resistance syndrome or metabolic syndrome X, is a multifactorial syndrome affecting men more than women, and is mainly influenced by hormonal, genetic, and lifestyle factors1. It is a steadily increasing metabolic abnormality, affecting 34% of the general population and may lead to glucose abnormality and significant cardiovascular complications such as high blood pressure and dyslipidemia that may increase the risk of heart failure, affecting both therapeutics and follow-up management plan2,3. Heart failure (HF) is a chronic, progressive condition in which the heart muscle is incapable of pumping enough blood to meet the body’s needs for blood and oxygen. Heart failure is a major health concern that has been a subject of interest since it was designated as an emerging epidemic in 19974,5. Since then, the total number of cases has evolved and become a major cause of mortality, hospitalization, and health care expenses among patients older than 65 years6. The presence of heart failure along with other comorbidities significantly affects the long-term morbidity and mortality of symptomatic and asymptomatic patients.
Moreover, metabolic syndrome may cause obesity, which is an established risk of heart failure, but recently it has been published that such a relationship may result in a better prognosis. This is called the obesity paradox. Obesity has been found to increase short and medium-term prognosis in association with the cardiorespiratory capacity of the patients. Several therapeutic effects including better physical activity and diet resulted in better outcomes in heart failure patients7. To date, the exact mechanism of metabolic syndrome and its association with heart failure and the obesity paradox are still not well understood. In this review article, we aim to highlight current knowledge regarding the impact of metabolic syndrome on heart failure development in relation to the obesity paradox.
2. Prevalence and incidence
The prevalence of metabolic syndrome has significantly increased over the years. According to the national health and nutrition examination Survey (NHANES), the prevalence has increased from 36.3% in 2011-2012 to 38.2% in 2017-2018 in the USA8. Furthermore, older studies have supported this finding as well, the prevalence was 23.1 % which increased to 27 % in 1999-20009. As per the national cholesterol education program (NCEP) criteria, metabolic syndrome is so common in the US that 43.5% of the total over 50 years of age population have it10.
The increasing prevalence of metabolic syndrome also leads to a growing prevalence of the global pandemic, heart failure, which affects around 26 million people in the whole world11. Metabolic syndrome is a risk factor for other cardiovascular conditions as well, which contributes to the increase in their prevalence.
According to a systematic review and meta-analysis that were done in Iran, metabolic syndrome was present in 34.2% of a total of 44,735 cardiovascular patients12. Moreover, a study of heart transplant patients showed that 42.3% patients had metabolic syndrome along with ischemic heart disease before the transplant13. One study suggested that the prevalence of metabolic syndrome was 49.5% among 200 coronary artery disease (CAD) patients who had undergone coronary angiography14. The population with an age of more than 50 years in NHANES was divided into two groups depending on the presence of the metabolic syndrome and the group with metabolic syndrome showed the highest prevalence of coronary heart disease (CHD)15.
Similar to other cardiovascular diseases, the prevalence of the metabolic syndrome is also high in heart failure patients. Various studies have shown similar findings. One single-center study showed that out of 865 patients with indigent heart failure, 40% had metabolic syndrome16. A Japanese study with 3603 patients enrolled with chronic heart failure showed the presence of metabolic syndrome in 49 % of males and 19 % of females, which was higher than double than the general population. Another study with 4762 HF patients had metabolic syndrome prevalence of 41.3%17.
3. Morbidity and mortality
The presence of comorbidities significantly affects long-term morbidity and mortality of symptomatic and asymptomatic heart failure patients18. Population studies have shown that metabolic syndrome increases the risk of developing heart failure and this effect is mediated by insulin resistance. However, obesity is a key component in metabolic syndrome and a customary partner of insulin resistance because it is protective in patients with established heart failure, although insulin resistance confers an increased risk of dying from heart failure. This phenomenon is called the "obesity paradox" accounting for the complexity of the heart failure-metabolic syndrome relationship6. Metabolic syndrome has a prevalence in the general population of 27% and is associated with increased mortality. In a cohort of hospitalized patients with heart failure, the prevalence of metabolic syndrome was 68%, exceeding that of the general population. However, unlike the general population, metabolic syndrome is associated with lower mortality in heart failure patients, establishing that mortality was lower in those with metabolic syndrome (44%) compared to those without (58%, unadjusted HR 0.67). Finally, in a fully adjusted model, there was a significantly lower risk of mortality in those with metabolic syndrome (adjusted, HR 0.73)19. Therefore, physicians treating patients with heart failure need to address the present metabolic syndrome epidemic.
4. Association of heart failure and metabolic syndrome X
For more than 50 years, there has been a correlation between obesity and atherosclerotic heart disease. The obesity pandemic has made this aspect of the population's risk for cardiovascular disease more important and evident20. Though generally known, the link between obesity and congestive heart failure is still not fully understood. Obstructive sleep apnea and systemic and pulmonary hypertension were thought to be the primary causes of this illness, which was formerly known as "obesity cardiomyopathy”21,22.
Numerous studies show that diabetes mellitus and insulin resistance are not the only risk factors for heart failure. They are also associated with a more severe form of left ventricular dysfunction and higher mortality rates than people without diabetes mellitus or insulin resistance or heart failure23. In individuals with heart failure, insulin resistance is very common (up to 60%), and there is a complex pathophysiological interplay between these two disorders since insulin resistance may be both a cause and an effect of heart failure. Similar to heart failure patients, diabetes mellitus is widespread among them, with prevalence rates in hospitalized patients ranging from 10% to 40%24.Several functional, metabolic, and anatomical changes brought on by insulin resistance and diabetes mellitus ultimately lead to heart failure.
Hypertension affects 6 to 10 percent of heart failure patients. According to the model put forth by Vasan and Levy, hypertension is not known to affect LV function in the early stages. A chronic increase in pressure load caused by mechanical stress leads to a rise in the level of cytokines, neurohormones and growth factors which progress to the development of concentric LV hypertrophy, leading to symptomatic heart failure with normal or abnormal LV function25. The lipid abnormalities mentioned in the definition of metabolic syndrome include low plasma levels of high-density lipoprotein (HDL) and high plasma levels of triglycerides. Velagaleti et al. found that low HDL plasma levels were linked to a 40% higher risk of developing heart failure over a 26-year follow-up in a population analysis from the Framingham cohort. Consequently, lipid buildup in the heart leads to heart failure26.
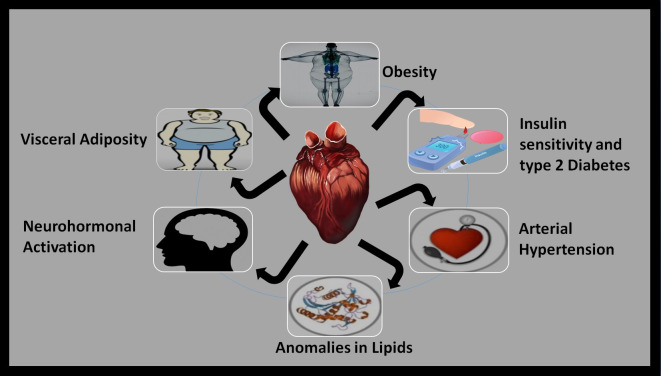
According to Jackson's heart research, visceral obesity is linked to an increased risk of developing heart failure in the black population27. The homozygous TT genotype of the aminopeptidase M1 (apM1) gene, which was identified in abundance in adipose tissue, was linked to a greater risk of metabolic syndrome. Adiponectin, a protein that resembles collagen, was also encoded by the apM1 gene28. Persistent activation of the sympathetic nervous system and renin-angiotensin-aldosterone system were the processes involved in metabolic syndrome29. Inability to adapt the results of these processes in cardiomyocyte hypertrophy, which, if the problem persists, could cause remodeling and finally result in heart failure30. The association between heart failure and metabolic syndrome has been illustrated in Figure 1.
Figure 1. Association between heart failure and metabolic syndrome X.
5. Pathogenesis of heart failure in metabolic syndrome X patients
Adipose tissue is classified according to its location: subcutaneous or visceral. However, it was found that visceral adiposity was independently associated with the incidence of hospitalized patients with heart failure with preserved ejection fraction (HFpEF). Obesity and in particular central adiposity directly correlates with increased left ventricular stiffness, which contributes to the diastolic dysfunction in HFpEF. Visceral adipose tissue (VAT), which is stored in the abdominal cavity and accounts for 20% of adipose tissue, is pro-inflammatory and increases cardiovascular risk by promoting metabolic diseases such as diabetes mellitus, dyslipidemia, and hypertension. Obesity-related biomarkers such as adipokines also have prognostic value in heart failure risk but it is unknown if these biomarkers better predict heart failure than anthropometrics and CT-measured adiposity31.
Thus, chronic inflammation also plays an important role in heart failure associated with metabolic syndrome. Serum IL-6 and TNF-α levels are high in patients with metabolic syndrome and elevated proinflammatory cytokines such as tumor necrosis factor (TNF)-α, interleukin (IL)-1, IL-6, galectin 3, soluble TNF receptor 1, and soluble TNF receptor 2 can be detected both in heart failure with reduced ejection fraction (HFrEF) and HFpEF. TNF provokes cardiomyocyte hypertrophy and impairs cardiac contractile function. TNF also induces dilation of the left ventricle as a result of extracellular matrix degradation. Several studies have also suggested the role of IL-6 in the progression of heart failure including its interaction with the vasculature and neurohormonal system to promote cardiac HF31.
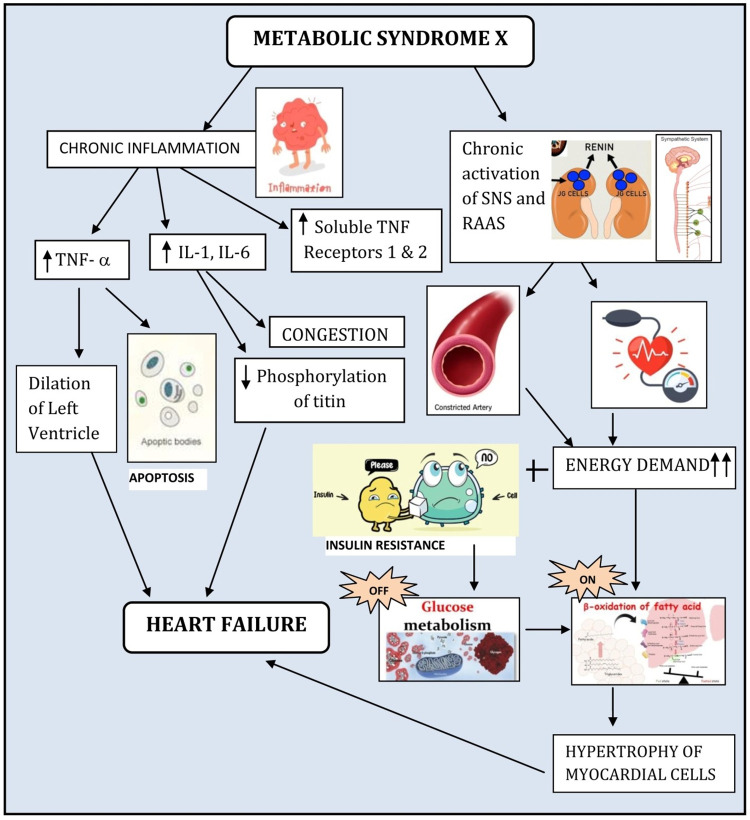
Overnutrition increases the levels of circulating free fatty acids and triglycerides, resulting in an increased accumulation of lipids and fatty acids in the myocardial cells by increased uptake. Activation of kinases results in increased serine phosphorylation of Insulin receptor substrate 1 (IRS-1)32. Insulin resistance occurs as a response to multiple stimuli leading to activation of s6 kinase. The response induced myocardial hypertrophy, cardiac fibrosis, impaired myocardial-endothelial signaling, and death of myocardial and endothelial cells. A study correlated a higher risk of heart failure incidence was related to a higher fasting insulin level. Prolonged Insulin resistance by the body can cause an increase in left atrial size, left ventricular mass, and alterations in transmitral velocity33. Hyperinsulinemia resulting from insulin resistance, along with an increase in adipokine levels and alterations of baroreceptor heart rate reflex are some key factors that give rise to chronic activation of the sympathetic autonomic nervous system. This leads to peripheral vasoconstriction and tachycardia. Although the metabolic demand of the heart increases in sympathetic stimulation, the metabolic supply to the tissues is decreased due to the transition from glycolysis pathway to fatty acid oxidation. The development of hypertrophy of cardiac myocytes results as a compensatory mechanism and failure to address the condition can thereby proceed to heart failure31 (Figure 2).
Figure 2. The mechanisms of heart failure in metabolic syndrome X patients.
There is a paradoxical relationship between obesity and heart failure, especially in those with BMI 30-35. The mechanism of this still remains unclear, however, the increased lean mass that obese individuals have could play a critical role in improving long-term outcomes. Excess lean mass allows a higher cardiorespiratory fitness, which in turn improves heart failure prognosis; furthermore, the exact mechanism is unknown34.
6. Diagnosis
The diagnosis of heart failure begins with a thorough assessment of the patient's history and physical. Classic signs and symptoms of heart failure, such as dyspnea, dyspnea on exertion, orthopnea, peripheral edema, pathologic S3 and S4 heart sounds, crackles/rales at the lung bases, and jugular venous distention raise clinical suspicion of heart failure. It is of note that the history and physical examination provide low specificity and sensitivity to the diagnosis of heart failure35.
Electrocardiography (ECG), Chest X-ray, and Laboratory evaluation are initial diagnostic evaluations for patients who are suspected to have heart failure. ECG is particularly useful in patients that have HFrEF. These patients have significant ECG abnormalities, and the ECG provides high sensitivity and limited specificity for identifying HFrEF in these patients36. HFpEF on the other hand, displays a normal 12 lead ECG, though the presence of atrial fibrillation or paced rhythm increases the probability that HFpEF is present. A normal ECG makes left ventricle systolic dysfunction unlikely with a 98% negative predictive value37.
Chest radiographs are useful especially for patients presenting with dyspnea because they can provide information that helps differentiate heart failure from a primary pulmonary disease38-40. Cardiomegaly, Kerley-B lines, pleural effusion, and cephalization of the pulmonary vessels are findings suggestive of heart failure. Redistribution and cardiomegaly are the best predictors of increased preload and reduced ejection fraction, but neither is sufficient to definitively diagnose heart failure. alveolar edema, interstitial edema, and cephalization all have high specificity for HFrEF, but only cardiomegaly had a sensitivity of over 50 percent39. Chest X-rays are more limited in providing diagnostic value for patients with HFpEF where the sensitivity of cardiomegaly is 24 percent and pleural effusion is only 9 percent41.
It is recommended that the clinician obtain a complete blood count, urinalysis, serum electrolytes, blood urea nitrogen, serum creatinine, glucose, fasting lipid panel, liver function test, iron studies, assays for BNP or NT-proBNP, and thyroid-stimulating hormone levels for patients who are suspected to have heart failure. These laboratory studies provide essential information with regard to patients’ comorbidities, treatment approach, and potential causes or confounders of heart failure. In the context of the correct clinical presentation, BNP or NT-proBNP levels provide immense value to the diagnosis of heart failure, but should not be used in isolation to diagnose or exclude heart failure42. BNP or NT-proBNP levels have sensitivities of 93 percent and a specificity of 74 and 65 percent respectively for the diagnosis of heart failure36.
Once the clinician develops high suspicion of heart failure, echocardiography becomes key to the diagnosis. Left ventricular ejection fraction (LVEF), a measure of heart function collected by echocardiography, is used to diagnose and categorize heart failure into either HFpEF or HFrEF. If the LVEF is less than 50 percent, the patient is diagnosed with HFrEF, and if the LVEF is over or equal to 50 percent then the patient is diagnosed with HFpEF. While echocardiography is essential to the diagnosis of heart failure, it alone does not establish or exclude heart failure. Thus, a conclusive diagnosis cannot be made without considering the signs, symptoms, clinical features, laboratory values, chest radiography, and ECG of the patient being evaluated35 (Table 1).
Table 1. Overall accuracy of the clinical features of heart failure.
Clinical features with high sensitivity can help us rule out the disease when a patient has a negative result. Whereas clinical features with high specificity are useful when ruling in a patient's disease37,43.
| Clinical features | Sensitivity (%) | Specificity (%) |
|---|---|---|
| History of MI | 26 | 89 |
| Dyspnea | 87 | 51 |
| Orthopnea | 44 | 89 |
| Peripheral edema | 53 | 72 |
| Lung crepatation | 51 | 81 |
| Elevated jugular venous pressure/ jugular venous distention | 52 | 70 |
| Cardiomegaly | 27 | 85 |
| Pathologic S3 or S4 heart sounds | 11 | 99 |
| Hepatomegaly | 17 | 97 |
| ECG in HFrEF | 89 | 56 |
| BNP | 93 | 74 |
| NT-proBNP | 93 | 65 |
| Chest radiograph | 68 | 83 |
| Echocardiography in HFpEF | 85 | 96 |
| Echocardiography in HFrEF | 96 | 80 |
Metabolic syndrome X is diagnosed when the patient has central obesity with two or more of the following; raised triglycerides or specific treatment for this lipid abnormality, reduced HDL cholesterol or specific treatment for this lipid abnormality, raised blood pressure or treatment of previously diagnosed hypertension, and raised fasting plasma glucose or previously diagnosed type 2 diabetes. Metabolic Syndrome X is the most dangerous heart attack risk factor as patients with metabolic syndrome X are three times as likely to have a heart attack or stroke compared to people without the syndrome. It is imperative to diagnose and identify individuals with metabolic syndrome early, so that lifestyle interventions and treatment may prevent the development of diabetes mellitus and/or cardiovascular disease44.
7. Heart failure’s treatment in metabolic syndrome X
The treatment for heart failure in metabolic syndrome X is multifactorial and mainly targets the different components of metabolic syndrome X: obesity, hyperglycemia, hypertension, and dyslipidemia. These components can be treated using lifestyle modifications or pharmaceutical agents.
According to current guidelines, in patients with metabolic syndrome X and heart failure, the blood pressure should be less than 130/80 mmHg, cholesterol should be less than 100 mg/dL, and glycosylated hemoglobin levels should be less than 7 percent45. Lifestyle modifications like weight loss, exercise, or dietary changes can be beneficial in managing both heart failure and metabolic syndrome X. For example, aerobic exercise has been shown to have anti-hypertensive effects since it decreases systolic and diastolic blood pressure. Furthermore, it also decreases fasting blood glucose, triglycerides, and low-density protein concentrations. On the other hand, combined exercise has been shown to decrease diastolic blood pressure with minor improvements in high-density lipoprotein levels43. Moreover, a low carbohydrate, low fat, or Mediterranean diet helps improve the different components of metabolic syndrome X46. Yet, it is important to note that all of the above treatment options not only have a favorable effect on weight loss, but also on central obesity. It is essential to mention that even though obesity paradox exists, where obese and overweight patients with heart failure have a better prognosis than average weighted people with heart failure, there is little known about it. Therefore, the most acceptable and widely used therapy protocol still remains weight loss.
The pharmaceutical approach, much like lifestyle modifications, also targets the individual components of metabolic syndrome X. For hyperglycemia, the drug of choice is metformin. It is known to be a cardioprotective drug that is associated with better survival in patients with heart failure and diabetes mellitus. Moreover, it is safe to use in patients with diabetes mellitus and HFrEF, whereas insulin had a negative impact47. For patients with insulin resistance, medications like thiazolidinediones (TZDs), alpha-glucosidase inhibitors, and sulfonylureas have been effective. Interestingly, both metformin and TZDs have been shown to reduce levels of inflammatory markers like PAI-I and hs-CRP48. This is important because according to some studies, there is a possible correlation between inflammatory cytokines, heart failure, and metabolic syndrome X18. Therefore, both of these medications may prove to be beneficial in this regard too.
Angiotensin-converting enzyme inhibitors (ACE-I) and angiotensin receptor blockers (ARBs) are the mainstay of therapy for hypertension because they are cardioprotective drugs that can be used to treat patients with HFrEF. However, it is important to recognize that inotropic calcium channel blockers are contraindicated in this patient population. Furthermore, B-blockers, hydralazine, diuretics, and amlodipine can be used to treat systolic HF31.
For the treatment of dyslipidemia, the medication of choice is statins. Statins, like atorvastatin and simvastatin, have been associated with a reduction in HF-related hospitalizations in patients with pre-existing heart failure. But it is important to recognize that rosuvastatin, also a statin drug, has not been associated with decreasing cardiovascular events45. Hence to effectively treat heart failure in metabolic syndrome X, it is crucial to target the underlying components of metabolic syndrome using either lifestyle changes or medications.
8. Prognosis
Clinicians have long known that there is a direct correlation between patients with metabolic X and an increased risk of cardiovascular morbidity. The counterintuitive association between obesity and a declining prevalence of heart failure still raises questions. The paradox that overweight and obese people with established heart failure had a better short- and medium-term prognosis than leaner patients was well-documented in many epidemiologic studies in large heart failure cohorts. This association and the degree of cardiorespiratory fitness were related7.
Although sternal infections, supraventricular arrhythmias, and bleedings are more common, moderate obesity has not been demonstrated to be associated with perioperative morbidity and death49. Research has revealed that BMI (Body Mass Index) is ineffective at differentiating between metabolically healthy and unhealthy obesity and hence cannot be extrapolated to quantify the risk of cardiovascular morbidity50.
Although there is no doubt that weight loss enhances heart structure and function and lessens heart failure symptoms, no significant research has been done on how weight loss affects clinical events in heart failure. As a result, there are no recommendations for individuals with heart failure regarding the ideal body composition51.
Metabolically healthy obesity (MHO) and the "fat but fit" phenomena are terms used to describe patients who have been given an obese diagnosis based on BMI but who also have higher Cardiorespiratory fitness (CRF) and few metabolic abnormalities. Finally, we suggest that obese patients who present with an excess of body fat but no metabolic abnormalities should still be considered a population that is "at risk" and as such, they should be advised on how to change their lifestyle to improve their CRF and stop the onset of other cardiovascular disease risk factors like diabetes mellitus and impaired fasting glucose. This is known as primary prevention52.
9. Conclusion
The connection between heart failure and metabolic syndrome X is succinctly summarized in this study, with a focus on the pathophysiology, risk factors, diagnosis, therapy, and prognosis of the illness. It is well established that metabolic syndrome X is associated with an increased risk of cardiovascular morbidity and mortality. Therefore, the treatment of metabolic syndrome X remains to be a challenge in patients with heart failure. We have also mentioned the “obesity paradox” which explains that obesity can be a positive prognostic factor. Since it is not still well understood, the Obesity Paradox provides a gray area for future researchers as it can dramatically alter the course of treatment for heart failure in association with metabolic syndrome X.
Acknowledgments
This review study received no grant from any funding agency in the public, commercial or not-for-profit sectors. Ethical approval was not required for this study. PO conceptualized the research idea and framed the title. She determined the exclusion and inclusion criteria for the papers used by the other authors in writing the sections of the article. She wrote the abstract. GNEH wrote the introduction and was in charge of compiling the data, reviewing, supervising and preparing the manuscript. GNEH, RHA and SM were in charge of editing the content of the paper along with the other authors. AM, Apurva P, Aayushi P, SR and RHA made the diagrams and tables that are used in the article. All the authors significantly contributed to writing the sections of the article and approved the manuscript.
Footnotes
Conflict of interests: The authors declare no conflicts of interest.
Abbreviations: Heart failure (HF); Heart Failure with Reduced Ejection Fraction (HFrEF); Heart Failure with Preserved Ejection Fraction (HFpEF); Left Ventricular Ejection Fraction (LVEF); Thiazolidinediones (TZD); High Sensitivity C-Reactive Protein (hsCRP); Angiotensin-Converting Enzyme Inhibitors (ACE-I); Angiotensin Receptor Blockers (ARBS); Body Mass Index (BMI); Metabolically Healthy Obesity (MHO); Cardiorespiratory Fitness (CRF); Cardiovascular disease (CVD); Insulin Receptor Substrate-1 (ISR-1); Tumor Necrosis Factor (TNF); Interleukin (IL); Left Ventricular (LV); High-Density Lipoprotein (HDL); Aminopeptidase M1 (apM1); Visceral Adipose Tissue (VAT); National Health and Nutrition Examination Survey (NHANES); National Cholesterol Education Program (NCEP); Coronary Artery Disease (CAD); Coronary Heart Disease (CHD).
DISCOVERIES is a peer-reviewed, open access, online, multidisciplinary and integrative journal, publishing high impact and innovative manuscripts from all areas related to MEDICINE, BIOLOGY and CHEMISTRY
References
- 1.Metabolic syndrome X: a review. Timar O, Sestier F, Levy E. The Canadian journal of cardiology. 2000;16(6):779–89. [PubMed] [Google Scholar]
- 2.Prevalence of metabolic syndrome among adults 20 years of age and over, by sex, age, race and ethnicity, and body mass index: United States, 2003-2006. Ervin R Bethene. National health statistics reports. 2009;(13):1–7. [PubMed] [Google Scholar]
- 3.The metabolic syndrome predicts incident congestive heart failure: a 20-year follow-up study of elderly Finns. Wang Jianjun, Sarnola Katriina, Ruotsalainen Sanna, Moilanen Leena, Lepistö Päivi, Laakso Markku, Kuusisto Johanna. Atherosclerosis. 2010;210(1):237–42. doi: 10.1016/j.atherosclerosis.2009.10.042. [DOI] [PubMed] [Google Scholar]
- 4.Epidemiology of heart failure. Groenewegen Amy, Rutten Frans H., Mosterd Arend, Hoes Arno W. European Journal of Heart Failure. 2020;22(8):1342-1356. doi: 10.1002/ejhf.1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Epidemiology of Heart Failure: A Contemporary Perspective. Roger Véronique L. Circulation research. 2021;128(10):1421–1434. doi: 10.1161/CIRCRESAHA.121.318172. [DOI] [PubMed] [Google Scholar]
- 6.Metabolic Syndrome in Heart Failure. Arcopinto Michele, Schiavo Alessandra, Salzano Andrea, Bossone Eduardo, D’Assante Roberta, Marsico Fabio, Demelo-Rodriguez Pablo, Baliga Ragavendra R., Cittadini Antonio, Marra Alberto M. Heart Failure Clinics. 2019;15(3):349-358. doi: 10.1016/j.hfc.2019.02.004. [DOI] [PubMed] [Google Scholar]
- 7.The Impact of Obesity in Heart Failure. Carbone Salvatore, Lavie Carl J, Elagizi Andrew, Arena Ross, Ventura Hector O. Cardiology clinics. 2022;40(2):209–218. doi: 10.1016/j.ccl.2021.12.009. [DOI] [PubMed] [Google Scholar]
- 8.Prevalence of Metabolic Syndrome in the United States National Health and Nutrition Examination Survey (NHANES) 2011-2018. Liang Xiaopeng, Or Benjamin, Tsoi Man Fung, Cheung Ching Lung, Cheung Bernard MY. 2021 doi: 10.1093/postmj/qgad008. [DOI] [PubMed] [Google Scholar]
- 9.Increasing Prevalence of the Metabolic Syndrome Among U.S. Adults. Ford Earl S., Giles Wayne H., Mokdad Ali H. Diabetes Care. 2004;27(10):2444-2449. doi: 10.2337/diacare.27.10.2444. [DOI] [PubMed] [Google Scholar]
- 10.NCEP-defined metabolic syndrome, diabetes, and prevalence of coronary heart disease among NHANES III participants age 50 years and older. Alexander Charles M, Landsman Pamela B, Teutsch Steven M, Haffner Steven M. Diabetes. 2003;52(5):1210–4. doi: 10.2337/diabetes.52.5.1210. [DOI] [PubMed] [Google Scholar]
- 11.Global Public Health Burden of Heart Failure. Savarese Gianluigi, Lund Lars H. Cardiac failure review. 2017;3(1):7–11. doi: 10.15420/cfr.2016:25:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.The prevalence of metabolic syndrome in cardiovascular patients in Iran: a systematic review and meta-analysis. Salari Nader, Doulatyari Peyman Kaikhosro, Daneshkhah Alireza, Vaisi-Raygani Aliakbar, Jalali Rostam, Jamshidi Parnian Kord, Abdi Alireza, Mohammadi Masoud, Kazeminia Mohsen. Diabetology & metabolic syndrome. 2020;12(1):96. doi: 10.1186/s13098-020-00605-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Prevalence of metabolic syndrome in heart transplant patients: role of previous cardiopathy and years since the procedure--the TRACA study. Cordero Fort Alberto, Gavira Juan José, Alegría-Barrero Eduardo, Castaño Sara, Martín Ana, Ubilla Matías, Mastrobuoni Stefano, Alegría Ezquerra Eduardo, Herreros Jesús, Rábago Gregorio. The Journal of heart and lung transplantation : the official publication of the International Society for Heart Transplantation. 2006;25(10):1192–8. doi: 10.1016/j.healun.2006.06.012. [DOI] [PubMed] [Google Scholar]
- 14.The Prevalence of Metabolic Syndrome in Coronary Artery Disease Patients. Montazerifar Farzaneh, Bolouri Ahmad, Mahmoudi Mozaffar Milad, Karajibani Mansour. Cardiology research. 2016;7(6):202–208. doi: 10.14740/cr507w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.CHD Prevalence in Americans Age 50 Years and Older Using NCEP and WHO Definitions of Metabolic Syndrome. Alexander Charles M., Landsman Pamela B., Nag Soma S., Teutsch Steven M., Haffner Steven M. Clinical Research and Regulatory Affairs. 2004;21(3-4):179-190. [Google Scholar]
- 16.Metabolic Syndrome Increases Mortality in Heart Failure. Tamariz Leonardo, Hassan Benjamin, Palacio Ana, Arcement Lee, Horswell Ron, Hebert Kathy. Clinical Cardiology. 2009;32(6):327-331. doi: 10.1002/clc.20496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Prevalence and Clinical Implication of Metabolic Syndrome in Chronic Heart Failure - Report From MetS-CHF Study - Miura Yutaka, Fukumoto Yoshihiro, Shiba Nobuyuki, Miura Toshiro, Shimada Kazunori, Iwama Yoshitaka, Takagi Atsutoshi, Matsusaka Hidenori, Tsutsumi Takaki, Yamada Akira, Kinugawa Shintaro, Asakura Masanori, Okamatsu Shuichi, Tsutsui Hiroyuki, Daida Hiroyuki, Matsuzaki Masunori, Tomoike Hitonobu, Shimokawa Hiroaki. Circulation Journal. 2010;74(12):2612-2621. doi: 10.1253/circj.cj-10-0677. [DOI] [PubMed] [Google Scholar]
- 18.The metabolic syndrome in heart failure: insights to specific mechanisms. Gargiulo Paola, Marsico Fabio, Renga Francesco, Dell’Aversana Simona, Esposito Immacolata, Marciano Caterina, Dellegrottaglie Santo, Perrone-Filardi Pasquale, Paolillo Stefania. Heart Failure Reviews. 2019;25(1):1-7. doi: 10.1007/s10741-019-09838-6. [DOI] [PubMed] [Google Scholar]
- 19.The Metabolic Syndrome and Mortality in an Ethnically Diverse Heart Failure Population. Hassan Saamir A., Deswal Anita, Bozkurt Biykem, Aguilar David, Mann Douglas L., Pritchett Allison M. Journal of Cardiac Failure. 2008;14(7):590-595. doi: 10.1016/j.cardfail.2008.03.004. [DOI] [PubMed] [Google Scholar]
- 20.Obesity as an independent risk factor for cardiovascular disease: a 26-year follow-up of participants in the Framingham Heart Study. Hubert H B, Feinleib M, McNamara P M, Castelli W P. Circulation. 1983;67(5):968-977. doi: 10.1161/01.cir.67.5.968. [DOI] [PubMed] [Google Scholar]
- 21.Obesity Cardiomyopathy: Pathophysiology and Evolution of the Clinical Syndrome. Alpert Martin A. The American Journal of the Medical Sciences. 2001;321(4):225-236. doi: 10.1097/00000441-200104000-00003. [DOI] [PubMed] [Google Scholar]
- 22.Obesity and the Heart. Alpert Martin A., Hashimi M. Wail. The American Journal of the Medical Sciences. 1993;306(2):117-123. doi: 10.1097/00000441-199308000-00011. [DOI] [PubMed] [Google Scholar]
- 23.Non-HDL Cholesterol as a Predictor of Cardiovascular Disease in Type 2 Diabetes. Lu Weiquan, Resnick Helaine E., Jablonski Kathleen A., Jones Kristina L., Jain Arvind K., Howard Wm. James, Robbins David C., Howard Barbara V. Diabetes Care. 2003;26(1):16-23. doi: 10.2337/diacare.26.1.16. [DOI] [PubMed] [Google Scholar]
- 24.Scova N. Automation in analytical chemistry. White Plains, NY: Mediad Inc. (2nd ed.); 1968. [Google Scholar]
- 25.A Case-Crossover Analysis of Out-of-Hospital Coronary Deaths and Air Pollution in Rome, Italy. Forastiere Francesco, Stafoggia Massimo, Picciotto Sally, Bellander Tom, D'Ippoliti Daniela, Lanki Timo, von Klot Stephanie, Nyberg Fredrik, Paatero Pentti, Peters Annette, Pekkanen Juha, Sunyer Jordi, Perucci Carlo A. American Journal of Respiratory and Critical Care Medicine. 2005;172(12):1549-1555. doi: 10.1164/rccm.200412-1726OC. [DOI] [PubMed] [Google Scholar]
- 26.The predictive value of cardiac troponin T measurements in subjects on regular haemodialysis. Stolear Jean Claude, Georges Bernard, Shita Ali, Verbeelen Dierik. Nephrology Dialysis Transplantation. 1999;14(8):1961-1967. doi: 10.1093/ndt/14.8.1961. [DOI] [PubMed] [Google Scholar]
- 27.Association Between Regional Adipose Tissue Distribution and Risk of Heart Failure Among Blacks. Pandey Ambarish, Kondamudi Nitin, Patel Kershaw V., Ayers Colby, Simek Shawn, Hall Michael E., Musani Solomon K., Blackshear Chad, Mentz Robert J., Khan Hassan, Terry James G., Correa Adolfo, Butler Javed, Neeland Ian J., Berry Jarett D. Circulation: Heart Failure. 2018;11(11) doi: 10.1161/CIRCHEARTFAILURE.118.005629. [DOI] [PubMed] [Google Scholar]
- 28.Polymorphism Of The APM1 Gene In Subjects With Central Obesity Related To Lower High-Density Lipoprotein Cholesterol. Barliana Melisa I, Yolanda Poppy D, Rostinawati Tina, Ng Henry, Alfian Sofa D, Abdulah Rizky, Diantini Ajeng. Diabetes, metabolic syndrome and obesity : targets and therapy. 2019;12:2317–2324. doi: 10.2147/DMSO.S220050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Obesity, kidney dysfunction and hypertension: mechanistic links. Hall John E, do Carmo Jussara M, da Silva Alexandre A, Wang Zhen, Hall Michael E. Nature reviews. Nephrology. 2019;15(6):367–385. doi: 10.1038/s41581-019-0145-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Renal function and cardiac adrenergic impairment in patients affected by heart failure. Marsico Fabio, Paolillo Stefania, Gargiulo Paola, Parisi Valentina, Nappi Carmela, Assante Roberta, Dell'Aversana Simona, Esposito Immacolata, Renga Francesco, Esposito Luca, Bardi Luca, Rengo Giuseppe, Dellegrottaglie Santo, Marciano Caterina, Leosco Dario, Cuocolo Alberto, Filardi Pasquale Perrone. Journal of nuclear cardiology : official publication of the American Society of Nuclear Cardiology. 2021;28(5):2112–2122. doi: 10.1007/s12350-019-01975-7. [DOI] [PubMed] [Google Scholar]
- 31.Metabolic syndrome and heart failure: mechanism and management. Purwowiyoto Sidhi Laksono, Prawara Ananta Siddhi. Medicine and pharmacy reports. 2021;94(1):15–21. doi: 10.15386/mpr-1884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Insulin resistance and heart failure: molecular mechanisms. Aroor Annayya R, Mandavia Chirag H, Sowers James R. Heart failure clinics. 2012;8(4):609–17. doi: 10.1016/j.hfc.2012.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Insulin resistance and risk of incident heart failure: Cardiovascular Health Study. Banerjee Dipanjan, Biggs Mary L, Mercer Laina, Mukamal Kenneth, Kaplan Robert, Barzilay Joshua, Kuller Lewis, Kizer Jorge R, Djousse Luc, Tracy Russell, Zieman Susan, Lloyd-Jones Donald, Siscovick David, Carnethon Mercedes. Circulation. Heart failure. 2013;6(3):364–70. doi: 10.1161/CIRCHEARTFAILURE.112.000022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Obesity paradox in cardiovascular disease: where do we stand? Carbone Salvatore, Canada Justin M, Billingsley Hayley E, Siddiqui Mohammad S, Elagizi Andrew, Lavie Carl J. Vascular health and risk management. 2019;15:89–100. doi: 10.2147/VHRM.S168946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Diagnosing and managing acute heart failure in the emergency department. Kuo Dick C, Peacock W Frank. Clinical and experimental emergency medicine. 2015;2(3):141–149. doi: 10.15441/ceem.15.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Systematic review and individual patient data meta-analysis of diagnosis of heart failure, with modelling of implications of different diagnostic strategies in primary care. Mant J, Doust J, Roalfe A, Barton P, Cowie M R, Glasziou P, Mant D, McManus R J, Holder R, Deeks J, Fletcher K, Qume M, Sohanpal S, Sanders S, Hobbs F D R. Health technology assessment (Winchester, England) 2009;13(32):1–207, iii. doi: 10.3310/hta13320. [DOI] [PubMed] [Google Scholar]
- 37.Value of the electrocardiogram in identifying heart failure due to left ventricular systolic dysfunction. Davie A P, Francis C M, Love M P, Caruana L, Starkey I R, Shaw T R, Sutherland G R, McMurray J J. BMJ (Clinical research ed.) 1996;312(7025):222. doi: 10.1136/bmj.312.7025.222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.How well can the chest radiograph diagnose left ventricular dysfunction? Badgett R G, Mulrow C D, Otto P M, Ramírez G. Journal of general internal medicine. 1996;11(10):625–34. doi: 10.1007/BF02599031. [DOI] [PubMed] [Google Scholar]
- 39.Diagnostic value of B-Type natriuretic peptide and chest radiographic findings in patients with acute dyspnea. Knudsen Cathrine W, Omland Torbjørn, Clopton Paul, Westheim Arne, Abraham William T, Storrow Alan B, McCord James, Nowak Richard M, Aumont Marie-Claude, Duc Philippe, Hollander Judd E, Wu Alan H B, McCullough Peter A, Maisel Alan S. The American journal of medicine. 2004;116(6):363–8. doi: 10.1016/j.amjmed.2003.10.028. [DOI] [PubMed] [Google Scholar]
- 40.Cross sectional study of contribution of clinical assessment and simple cardiac investigations to diagnosis of left ventricular systolic dysfunction in patients admitted with acute dyspnoea. Gillespie N D, McNeill G, Pringle T, Ogston S, Struthers A D, Pringle S D. BMJ (Clinical research ed.) 1997;314(7085):936–40. doi: 10.1136/bmj.314.7085.936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.A Simple, Evidence-Based Approach to Help Guide Diagnosis of Heart Failure With Preserved Ejection Fraction. Reddy Yogesh N V, Carter Rickey E, Obokata Masaru, Redfield Margaret M, Borlaug Barry A. Circulation. 2018;138(9):861–870. doi: 10.1161/CIRCULATIONAHA.118.034646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.2013 ACCF/AHA Guideline for the Management of Heart Failure. Yancy Clyde W., Jessup Mariell, Bozkurt Biykem, Butler Javed, Casey Donald E., Drazner Mark H., Fonarow Gregg C., Geraci Stephen A., Horwich Tamara, Januzzi James L., Johnson Maryl R., Kasper Edward K., Levy Wayne C., Masoudi Frederick A., McBride Patrick E., McMurray John J.V., Mitchell Judith E., Peterson Pamela N., Riegel Barbara, Sam Flora, Stevenson Lynne W., Tang W.H. Wilson, Tsai Emily J., Wilkoff Bruce L. Circulation. 2013;128(16) doi: 10.1161/CIR.0b013e31829e8776. [DOI] [PubMed] [Google Scholar]
- 43.The effect of exercise training on clinical outcomes in patients with the metabolic syndrome: a systematic review and meta-analysis. Ostman C., Smart N. A., Morcos D., Duller A., Ridley W., Jewiss D. Cardiovascular Diabetology. 2017;16(1) doi: 10.1186/s12933-017-0590-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.The IDF consensus worldwide definition of the metabolic syndrome. - - Obesity and metabolism. 2005;2(3):47-49. [Google Scholar]
- 45.Metabolic Syndrome and Heart Failure—The Risk, Paradox, and Treatment. Gaddam Krishna K., Ventura Hector O., Lavie Carl J. Current Hypertension Reports. 2011;13(2):142-148. doi: 10.1007/s11906-011-0179-x. [DOI] [PubMed] [Google Scholar]
- 46.Dietary therapy in heart failure with preserved ejection fraction and/or left ventricular diastolic dysfunction in patients with metabolic syndrome. von Bibra Helene, Ströhle Alexander, St. John Sutton Martin, Worm Nicolai. International Journal of Cardiology. 2017;234:7-15. doi: 10.1016/j.ijcard.2017.01.003. [DOI] [PubMed] [Google Scholar]
- 47.Contributory Risk and Management of Comorbidities of Hypertension, Obesity, Diabetes Mellitus, Hyperlipidemia, and Metabolic Syndrome in Chronic Heart Failure: A Scientific Statement From the American Heart Association. Bozkurt Biykem, Aguilar David, Deswal Anita, Dunbar Sandra B., Francis Gary S., Horwich Tamara, Jessup Mariell, Kosiborod Mikhail, Pritchett Allison M., Ramasubbu Kumudha, Rosendorff Clive, Yancy Clyde. Circulation. 2016;134(23) doi: 10.1161/CIR.0000000000000450. [DOI] [PubMed] [Google Scholar]
- 48.Metabolic Syndrome and Heart Failure. Thethi Tina, Bratcher Christina, Fonseca Vivian. Heart Failure Clinics. 2006;2(1):1-11. doi: 10.1016/j.hfc.2005.11.006. [DOI] [PubMed] [Google Scholar]
- 49.Obesity and cardiovascular disease: expected and unexpected relationship. Pedone Chiara, Urbinati Stefano, Pallotti Maria Giovanna, Pinelli Giuseppe. Monaldi Archives for Chest Disease. 2005;64(1) doi: 10.4081/monaldi.2005.610. [DOI] [PubMed] [Google Scholar]
- 50.Obesity paradox and heart failure. Donataccio Maria Pia, Vanzo Angiola, Bosello Ottavio. Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity. 2020;26(6):1697-1707. doi: 10.1007/s40519-020-00982-9. [DOI] [PubMed] [Google Scholar]
- 51.Update on Obesity and Obesity Paradox in Heart Failure. Lavie Carl J., Sharma Abhishek, Alpert Martin A., De Schutter Alban, Lopez-Jimenez Francisco, Milani Richard V., Ventura Hector O. Progress in Cardiovascular Diseases. 2016;58(4):393-400. doi: 10.1016/j.pcad.2015.12.003. [DOI] [PubMed] [Google Scholar]
- 52.An Overview and Update on Obesity and the Obesity Paradox in Cardiovascular Diseases. Elagizi Andrew, Kachur Sergey, Lavie Carl J., Carbone Salvatore, Pandey Ambarish, Ortega Francisco B., Milani Richard V. Progress in Cardiovascular Diseases. 2018;61(2):142-150. doi: 10.1016/j.pcad.2018.07.003. [DOI] [PubMed] [Google Scholar]