Abstract
Epiploic appendagitis (EA) is an uncommon cause of acute abdominal pain that may mimic other causes of acute abdomen. Epiploic appendages are outpouching of fat tissue located on the external wall of the colon, being more numerous in the descending and sigmoid colon that account for up to 80% of EA cases.
We present the case of a 59-year-old woman with right upper quadrant pain. Abdominal ultrasound and contrast-enhanced computed tomography suggested the diagnosis of epiploic appendagitis of the right colonic flexure.
Our case highlights the fact that epiploic appendagitis may occur in unusual locations and must be included in the differential diagnosis of acute abdominal pain, in order to avoid unnecessary medical and surgical treatment.
Keywords: Epiploic appendagitis, Ultrasound, Acute abdomen, Emergency radiology, Computed tomography
Introduction
Epiploic appendages are pediculated outpouchings of fat located along the wall of the large bowel from the cecum to the sigmoid colon.
Their pediculated structure causes high mobility and makes them prone to torsion and infarction.
Primary epiploic appendagitis (EA) refers to spontaneous torsion, ischemia, and inflammation of the epiploic appendages, whereas secondary EA is caused by spreading of inflammation from adjacent organs as occurs in diverticulitis, appendicitis, or cholecystitis.
The most common sites of EA are the ileo-cecal region and the descending/sigmoid colon.
EA is usually a self-limiting condition that may mimic other conditions causing acute abdomens such as omental infarction, appendicitis, and diverticulitis [1], [2], [3], [4].
Case report
A 59-year-old woman was admitted to our Emergency Department for right hypocondrium pain and fever (maximum peak 37.8°C). Physical examination revealed signs of peritoneal irritation in the right upper quadrant.
Laboratory tests were unremarkable.
Abdominal Ultrasound (US) showed normal liver, gallbladder, and bile ducts. The appendix was not visible. In the subhepatic region, US revealed a 4 cm noncompressible heterogeneous hyperechoic mass with a thin hypoechoic rim, with no signs of blood flow at color-Doppler (Fig 1).
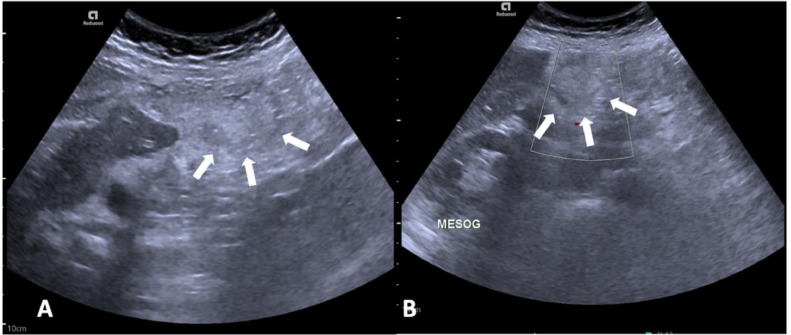
Fig. 1.
Abdominal US showing a hyperechoic rounded mass in the right hypocondrium adjacent to the lower margin of IVb hepatic segment close to the ascending colon (white arrows in A and B). The mass is surrounded by a hypoechoic rim. Color Doppler US shows absent internal blood flow (B).
Contrast-enhanced CT was performed to clarify US findings. CT revealed a formation of 43 × 33 × 56 mm located between the right colic flexure and the lower border of IVb hepatic segment (Fig 2).
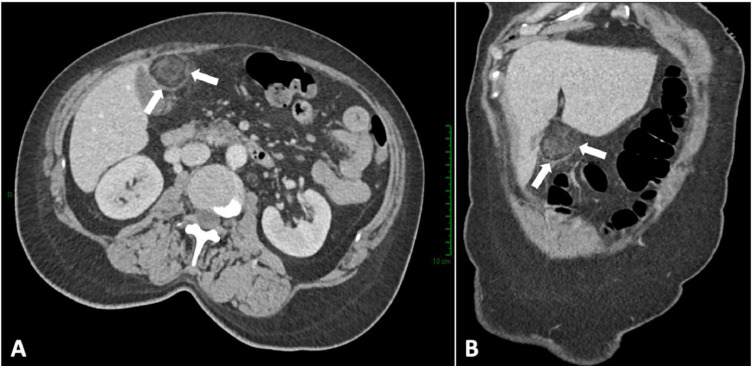
Fig. 2.
Axial (A) and coronal (B) contrast-enhanced CT demonstrating a formation with heterogeneous adipose matrix and peripheral dense rim (white arrows in A and B) adjacent to the right colic flexure. The findings were consistent with epiploic appendagitis.
The formation had an adipose matrix with dense internal branches and was surrounded by a hyperdense-enhancing rim.
The findings were consistent with epiploic appendagitis. No other significant CT findings were visible.
The patient underwent pharmacological therapy with intravenous Ketorolac. Abdominal pain and fever progressively disappeared and the patient was discharged in good clinical condition after 2 days.
Discussion
Epiploic appendagitis (EA) is a rare inflammation of the small fatty outpouchings located on the external colonic surface, occurring most frequently in the descending–sigmoid colon and the ileocecal region.
Epiploic appendages are usually undetectable by current imaging techniques unless inflammation occurs.
Abdominal Ultrasound may reveal a rounded, noncompressible, hyperechoic mass, without internal vascularity surrounded by a hypoechoic line in the zone of maximal abdominal tenderness, typically 2-4 cm in maximum diameter [5,6]. Color-Doppler evaluation shows absent or weak internal blood flow, in contrast to the hypervascularity observed in appendicitis or diverticulitis [3]. CEUS may demonstrate a central nonenhancing area with a peripheral enhancing rim [7].
Compute tomography shows a fat-density ovoid formation adjacent to the colon, usually 1.5-3.5 cm in diameter with thin (1-3 mm) high-density rim (hyperattenuating ring sign), surrounding fat stranding and thickening of the adjacent peritoneum [3,4].
Magnetic resonance, even though not routinely performed, may show a fat-containing mass with a peripheral enhancing rim [8].
Common differential diagnoses include omental infarction, diverticulitis, mesenteric panniculitis, and omental neoplasms.
Although omental infarction may have a very similar appearance to epiploic appendagitis, it usually lacks the hyperdense rim and appears attached to the parietal peritoneum, showing no movement during respiratory excursions (tethered fat sign) [9].
In diverticulitis, colon diverticula and thickened bowel wall are demonstrated [10].
Mesenteric panniculitis is a chronic inflammation involving the adipose tissue of the bowel mesentery. US may show distortion and thickening of the root of the mesentery, which appears hyperechoic, with a halo of hypoechoic fat around vessels (fat halo sign) [11].
Liposarcomas show a more prominent mass effect with indistinct margins and areas of hypervascularity [12].
Epiploic appendagitis is usually a self-limiting condition and conservative management with oral anti-inflammatory medications is considered the best treatment option. Surgery is performed in case when there is no improvement with conservative treatment or in patients who develop complications such as adhesions, abscess formation, peritonitis, bowel obstruction and intussusception [13,14].
Conclusions
Even though several cases of EA have been described, only few present with right upper quadrant abdominal pain. Epiploic appendagitis of the hepatic flexure is an uncommon self-limiting condition that should be included in the differential diagnoses in a patient with right upper quadrant abdominal pain, in order to avoid unnecessary hospitalization and invasive treatment.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Patient consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Acknowledgments: The authors received no financial support for the research, authorship, and/or publication of this article.
Competing Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Boardman J, Kaplan KJ, Hollcraft C, Bui-Mansfield LT. Radiologic-pathologic conference of Keller Army Community Hospital at West Point, the United States Military Academy: torsion of the epiploic appendage. AJR Am J Roentgenol. 2003;180(3):748. doi: 10.2214/ajr.180.3.1800748. [DOI] [PubMed] [Google Scholar]
- 2.Gaur S, Jawahar RP, Prasad R, Prabakaran M. Epiploic appendagitis - a rare cause of acute lower abdominal pain. Radiol Case Rep. 2021;16(5):1144–1147. doi: 10.1016/j.radcr.2021.02.026. Erratum in: Radiol Case Rep. 2022 Sep 29;17(12):4933. PMID: 33747330; PMCID: PMC7960494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Singh AK, Gervais DA, Hahn PF, Sagar P, Mueller PR, Novelline RA. Acute epiploic appendagitis and its mimics. Radiographics. 2005;25(6):1521–1534. doi: 10.1148/rg.256055030. [DOI] [PubMed] [Google Scholar]
- 4.Almeida AT, Melão L, Viamonte B, Cunha R, Pereira JM. Epiploic appendagitis: an entity frequently unknown to clinicians–diagnostic imaging, pitfalls, and look-alikes. AJR Am J Roentgenol. 2009;193(5):1243–1251. doi: 10.2214/AJR.08.2071. [DOI] [PubMed] [Google Scholar]
- 5.Trovato P, Simonetti I, Verde F, Lomoro P, Vinci G, Tarotto L, et al. Acute epiploic appendagitis: ultrasound and computed tomography findings of a rare case of acute abdominal pain and the role of other imaging techniques. Pol J Radiol. 2020;85:e178–e182. doi: 10.5114/pjr.2020.94335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rioux M, Langis P. Primary epiploic appendagitis: clinical, US, and CT findings in 14 cases. Radiology. 1994;191(2):523–526. doi: 10.1148/radiology.191.2.8153333. [DOI] [PubMed] [Google Scholar]
- 7.Görg C, Egbring J, Bert T. Contrast-enhanced ultrasound of epiploic appendagitis. Ultraschall Med. 2009;30(2):163–167. doi: 10.1055/s-2008-1027891. [DOI] [PubMed] [Google Scholar]
- 8.Sirvanci M, Tekelioğlu MH, Duran C, Yardimci H, Onat L, Ozer K. Primary epiploic appendagitis: CT manifestations. Clin Imaging. 2000;24(6):357–361. doi: 10.1016/s0899-7071(00)00236-9. [DOI] [PubMed] [Google Scholar]
- 9.Esposito F, Ferrara D, Schillirò ML, Grillo A, Diplomatico M, Tomà P. Tethered Fat Sign": the sonographic sign of omental infarction. Ultrasound Med Biol. 2020;46(5):1105–1110. doi: 10.1016/j.ultrasmedbio.2020.01.003. Epub 2020 Feb 5. PMID: 32035686. [DOI] [PubMed] [Google Scholar]
- 10.Mazzei MA, Cioffi Squitieri N, Guerrini S, Stabile Ianora AA, Cagini L, Macarini L, et al. Sigmoid diverticulitis: US findings. Crit Ultrasound J. 2013;(Suppl 1):S5. doi: 10.1186/2036-7902-5-S1-S5. 5 Suppl 1Epub 2013 Jul 15. PMID: 23902791; PMCID: PMC3711739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Horton KM, Lawler LP, Fishman EK. CT findings in sclerosing mesenteritis (panniculitis): spectrum of disease. Radiographics. 2003;23(6):1561–1567. doi: 10.1148/rg.1103035010. [DOI] [PubMed] [Google Scholar]
- 12.Craig WD, Fanburg-Smith JC, Henry LR, Guerrero R, Barton JH. Fat-containing lesions of the retroperitoneum: radiologic-pathologic correlation. Radiographics. 2009;29(1):261–290. doi: 10.1148/rg.291085203. [DOI] [PubMed] [Google Scholar]
- 13.Dongmo S., Tambe J., Onana Y., Ntongwetape N., Weledji E., Guegang E. Ultrasound diagnosis of primary epiploic appendagitis: a case report. Open J Med Imag. 2023;13:1–10. doi: 10.4236/ojmi.2023.131001. [DOI] [Google Scholar]
- 14.Chu EA, Kaminer E. Epiploic appendagitis: a rare cause of acute abdomen. Radiol Case Rep. 2018;13(3):599–601. doi: 10.1016/j.radcr.2018.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]