Abstract
Background A variety of internal and external fixation techniques have been described for the treatment of Rolando fractures, but the optimal fixation method has not been clearly defined.
Purpose The aim of the study was to describe the results and the long-term functional outcome of the application, under local anesthesia, of an external fixation system for the treatment of Rolando fractures.
Patients and Methods In total, 22 consecutive patients (16 men) underwent surgical treatment for Rolando fractures by using two pairs of pins external fixator. All procedures were performed under local anesthesia (Xylocaine 2%) and an image intensifier. Patients were evaluated at regular intervals postoperatively and contacted by phone for long-term follow-up. Functional outcome was assessed using the validated Quick Disabilities of the Arm, Shoulder, and Hand (Quick DASH) tool.
Results The mean age was 39.8 ± 14.2 years. The mean time from injury to surgery was 4.1 ± 2 days. The mean operative time was 16.3 ± 2.6 minutes. All fractures were healed and no loss of fracture reduction was observed postoperatively. One patient developed wound erythema at the proximal pins, without requiring early removal of the implant, and another one experienced temporary numbness at the distribution of the superficial radial nerve. In total, 20 out of the 22 patients who were available for long-term follow-up did not report any complaints and could perform the daily activities without restriction. The average follow-up was 6.5 ± 1.2 years, and the mean Quick DASH score was 1.8 ± 3.
Conclusion The two pairs of pins external fixator is a valuable option for the treatment of Rolando fractures and can be easily, quickly, and effectively applied under local anesthesia.
Keywords: Rolando fracture, trapeziometacarpal joint, thumb, metacarpal fractures, external fixation
Intra-articular fractures of the base of the thumb metacarpal account for 1.4% of all hand fractures. They usually occur after moderate trauma in active working population 1 and a proportion of 15 to 21% of them are of Rolando type. 2 3 4 Rolando fracture refers to a tripartite intra-articular T or Y fracture pattern that extends to the metaphyseal area and splits the base of the first metacarpal into dorsal and volar fragments. 4 5 It is usually a result of a compression axial force directed through a partially flexed metacarpal shaft. 6 7
Rolando-type fractures are considered unstable and failure to restore joint congruity may lead to pain, stiffness, functional impairment, and posttraumatic arthritis. 4 8 9 10 Even with successful closed initial reduction and immobilization, it is difficult to maintain the position of these fractures due to the deforming forces acting at the trapeziometacarpal joint region and, therefore, require close observation for several weeks. 9 11 12 Hence, these fractures are considered an indication for surgical intervention with closed or open fixation methods. In case of large fracture fragments, open reduction and internal fixation with lag screws, anatomical T- or L-type plates, and Kirschner wires (K-wires) may be applied to achieve anatomical alignment and stability. 13 14 However, open surgery may compromise ligament integrity and bone vascularization and can be associated with joint stiffness and malfunction. 15
To avoid the above-mentioned issues, closed reduction with traction and manipulation along with the application of percutaneous K-wire fixation or external fixation can be utilized. 1 4 5 6 10 12 15 16 17 K-wires alone cannot maintain distraction forces and their introduction through the base of the thumb metacarpal to the trapezium for preserving joint reduction and congruity can cause additional damage to the articular cartilage. 17 18 19 On the contrary, external fixators allow proper adjustment of the applying distraction forces that facilitate fracture reduction through the tension of the capsuloligamentous structures acting on the first trapeziometacarpal joint. Furthermore, they enable early mobilization of the adjacent joints and minimize the risk of postoperative stiffness. 12 20 So far, multiple types of external fixation have been used for the treatment of intra-articular fractures of the proximal thumb metacarpal including one or two pins inserted in the metacarpal and trapezium bone areas. Our aim is to describe the results and the long-term functional outcome of the application, under local anesthesia, of two pairs of pins external fixation system for the treatment of Rolando fractures.
Materials and Methods
Between 2012 and 2016, 22 consecutive patients over the age of 18 years underwent surgical treatment for Rolando-type fractures by using an external fixator. There were not any open fractures or simultaneous injuries/fractures at the ipsilateral hand and wrist. Fractures were assessed with anteroposterior and oblique hand X-rays.
The procedures were performed according to the ethical standards of the institutional committee on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. Preoperatively, all patients signed a written informed consent form for the use of their anonymized data for clinical research or trials. Institutional review board approval was obtained for the study.
All patients were evaluated at regular intervals postoperatively until fracture healing and restoration of normal function were achieved. They were also contacted by phone for long-term follow-up (>5 years) and asked questions about the operated hand performance and function. The functional outcome was assessed using the validated Quick Disabilities of the Arm, Shoulder, and Hand (Quick DASH) tool. 21 Descriptive statistics were calculated using the Statistical Package for the Social Sciences (SPSS, IBM) software version 24.
Surgical Technique
In all procedures performed by the senior author (P.K.G.), the operated hand was prepped with betadine and placed directly on the C-arm image intensifier. Tourniquet was applied and inflated 100 mm Hg above the systolic arterial pressure. Local anesthesia (Xylocaine 2%) was administered 10 minutes before tourniquet inflation at the proposed pin insertion sites over the dorsal first metacarpal and trapezium as well as proximally at the radial styloid area to block the superficial radial nerve. Afterward, two small dorsal skin incisions were utilized at the trapezium and proximal first metacarpal regions aiming to avoid the sensory branches of the radial nerve. Under fluoroscopy, two pairs of 2 mm bicortical half-threaded pins were inserted in the trapezium and first metacarpal shaft. Two clamps were applied over the pins and approximately 1cm far from the skin. A threaded bar was then attached to both clamps allowing compression and distraction using supplementary nuts. Axial traction was applied along the longitudinal axis of the thumb, and manipulation was additionally made to achieve the best fracture reduction image. At this point, the clamps and cams were locked, and the wires were trimmed such that 2 mm of each wire protruded from each clamp. A 4-0 Prolene suture was used to approximate the skin edges, and no cast or brace was applied ( Fig. 1 ). The external fixator was removed in outpatient clinic after 6 weeks, and range of motion exercises were immediately commenced. Radiologic evaluation of fracture reduction and progression of healing with hand X-Rays was performed at 6 and 12 weeks postoperatively.
Fig. 1.
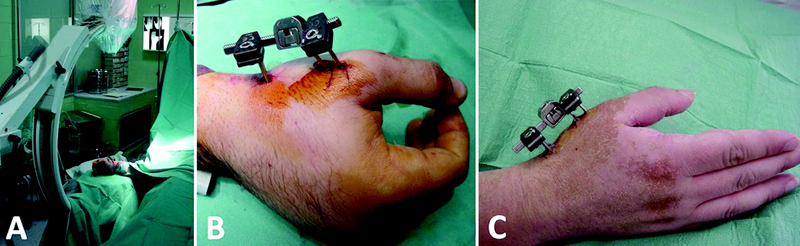
( A ) Intraoperative photo illustrates the setup of the operating room and the position of the operated hand over the image intensifier C-Arm. ( B ) Intraoperative and ( C ) postoperative (6 weeks) photographs show the position and location of external fixation.
Results
There were 16 men and 6 women with a mean age of 39.8 ± 14.2 years. The dominant hand was involved in 12 cases. The fracture occurred after fall in 11 patients, traffic accident in 8 patients, and during sports injury in 3 patients. The mean time from injury to surgery was 4.1 ± 2 days. The mean operative time was 16.3 ± 2.6 minutes ( Table 1 ). All fractures were healed, and no loss of intraoperation reduction was observed postoperatively ( Fig. 2 ).
Table 1. Patients' demographics and functional parameters.
| Patient no. | Gender | Age (years) | Fracture side | Injury mechanism | Interval from injury to surgery (days) | Operation time (minutes) | Follow-up (years) | QuickDASH |
|---|---|---|---|---|---|---|---|---|
| 1 | M | 59 | R | Fall | 5 | 20 | 8.6 | 0 |
| 2 | F | 43 | L | Fall | 2 | 12 | 8.5 | 2.3 |
| 3 | M | 38 | R | TA | 7 | 18 | 1.5 | N/R |
| 4 | M | 55 | L | Fall | 2 | 17 | 8.2 | 0 |
| 5 | M | 62 | R | TA | 2 | 15 | 8.0 | 0 |
| 6 | F | 34 | R | Fall | 3 | 20 | 7.7 | 0 |
| 7 | M | 42 | L | Fall | 1 | 15 | 6.9 | 4.5 |
| 8 | M | 64 | L | Fall | 6 | 19 | 6.8 | 0 |
| 9 | M | 33 | R | TA | 7 | 21 | 1.2 | N/R |
| 10 | M | 19 | R | SI | 6 | 15 | 6.7 | 2.3 |
| 11 | M | 29 | L | TA | 4 | 16 | 6.5 | 11.4 |
| 12 | M | 29 | R | SI | 7 | 13 | 6.2 | 0 |
| 13 | F | 36 | R | Fall | 3 | 15 | 6.1 | 0 |
| 14 | M | 24 | R | TA | 4 | 19 | 6.0 | 4.5 |
| 15 | M | 51 | L | Fall | 6 | 15 | 5.9 | 0 |
| 16 | M | 65 | R | Fall | 3 | 17 | 5.7 | 2.3 |
| 17 | F | 29 | L | TA | 5 | 14 | 5.5 | 6.8 |
| 18 | M | 31 | L | Fall | 4 | 14 | 5.4 | 0 |
| 19 | F | 28 | L | TA | 1 | 12 | 5.3 | 0 |
| 20 | F | 21 | R | TA | 2 | 17 | 5.2 | 0 |
| 21 | M | 48 | R | Fall | 7 | 15 | 5.0 | 0 |
| 22 | M | 36 | R | SI | 3 | 19 | 5.0 | 2.3 |
Abbreviations: DASH, disabilities of the arm, shoulder and hand; F, female; M, male; N/R, not reported; SI, sports injury; TA, traffic accident.
Fig. 2.

( A ) Anteroposterior X-ray of the right hand shows a Rolando fracture of the base of first metacarpal. ( B ) Intraoperative fluoroscopic view of fracture reduction and fixation with a two-pair pins external fixator. ( C ) Anteroposterior hand X-ray at 6 weeks postoperatively shows healing of the fracture. ( D ) Anteroposterior hand radiograph at 1 year postoperatively shows complete fracture union and no displacement or arthritis.
One patient developed wound erythema at the trapezium pins site that was treated with oral antibiotics and local wound care. However, early removal of the external fixator was not required. Another patient complained of temporary numbness in the distribution of the superficial radial nerve on the dorsum of the thumb, which was fully resolved at 10 weeks postoperatively.
Two patients could not be located during the latest phone call follow-up. The remaining 20 patients did not report any complaints, and they could perform daily activities without any restriction. The average follow-up was 6.5 ± 1.2 years, and the mean Quick DASH score was 1.8 ± 3. No further operations at the injury side were performed.
Discussion
External fixator for the treatment of intra-articular complex fractures of the base of the thumb metacarpal is a simple and effective technique leading to adequate fracture reduction, bone union, and excellent long-term functional result. Closed reduction of the fracture prevents soft-tissue damage, devascularization of the bone fragments, and development of fibrosis and tendon adhesion. 10 Although in the previous studies the technique was applied under general or regional anesthesia, we presented excellent patient tolerance by using only local anesthesia. Therefore, the operation can be done on an outpatient basis, and the patients can be discharged in an hour after surgery.
Apart from the external fixator, supplementary K-wires may be used to hold the intra-articular fragments and maintain reduction. Houshian and Jing 4 applied additional 1 mm or 1.25 mm K-wires to prevent shearing forces from causing fracture angulation and displacement. Their decision regarding the use of K-wires was based on intraoperative examination of the fracture stability under the image intensifier by passively moving the tip of the thumb to the base of the little finger. After a mean follow-up of 20 months, the authors reported a painless motion in 14 out of 16 patients. The remaining two patients had some residual pain, and they both had a comminuted Rolando fracture. In our series including exclusively Rolando-type fractures, the reduction was achieved with distraction and ligamentotaxis and no further implants or actions were deemed necessary. We believe that the strong ligaments of the thumb carpometacarpal joint can adequately reduce and stabilize the attached intra-articular bone fragments through continuous traction from the external fixator and ligamentotaxis. Consequently, percutaneous or mini-open K-wire application is not essential for accomplishing satisfactory articular congruity and alignment.
Fractures of the base of the thumb are considered unstable, and although they may be easily reduced, it is difficult to maintain their position. 11 12 The number of pins that should be used in an external fixator is still debated. Marsland et al 10 treated eight patients with a small external fixator inserting one pin in the first metacarpal shaft and another one in the trapezium. After 4 months, no significant joint incongruity or malunion was observed. According to these results, they advocated that additional pins to gain extra-rotational stability or construct stiffness were unnecessary. Kontakis et al 6 treated 11 Rolando fractures with a mini-external fixator and placed two pins distally in the first metacarpal and one pin in the trapezium. In 10 of 11 patients, the results were good or excellent. Considering the difficulty of inserting two pins in the trapezium, the authors concluded that insertion of only one pin proximally was easier and could provide sufficient stability and maintenance of fracture reduction. We believe that the application of two pairs of pins improves the performance and the strength of the external fixator. The main surgical tip is that trapezium pins should be introduced in the transverse plane using a semiopen approach to avoid accidental injury of the tendons and sensory branches of radial nerve crossing the anatomical snuffbox. Moreover, to enhance pin fixation and stability and minimize the possibility of secondary loosening and infection, the pins can be occasionally extended to the trapezoid.
Dynamic external fixator systems using K-wires have been also introduced for fixation of first metacarpal base fractures. 5 12 15 These systems may not be extended to the trapezium and, therefore, do not immobilize the thumb carpometacarpal joint. 12 15 Byrne et al 12 treated 10 complex fractures of the base of the thumb using an “S” Quattro external fixation constituting two pins inserted into first metacarpal shaft and two serpentine springs. Poor outcomes were reported in an elderly patient and in a patient with an open fracture. Wang et al 15 described a modification of a parallel K-wire fixation technique between the first and second metacarpals for the treatment of 20 proximal first metacarpal fractures. The ends of the K-wires were bent at 90° toward each other and then sheathed with a section of infusion tube and strapped with silk thread. That construct created a rectangular frame resembling an external fixator that offered a similar hand grip and function compared with the uninjured side in both the extra-articular and intra-articular fracture subgroups. However, it has not been yet clarified any superiority and clear advantage of the dynamic constructs over the simple static external fixation devices.
The current study has certain limitations. First, it represents a case series with a relatively small sample size and no control group. It is also a single institution's report, with scarce literature available to guide management and provide adequate comparison of data. However, it contains a specific fracture type treated with the same technique and protocol.
Footnotes
Conflict of Interest None declared.
References
- 1.Oc Y, Kilinc B E, Varol A, Kara A. A safe method for early rehabilitation of articular fracture at the base of thumb metacarpal bone. Adv Orthop. 2021;2021:6.632211E6. doi: 10.1155/2021/6632211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hove L M. Fractures of the hand. Distribution and relative incidence. Scand J Plast Reconstr Surg Hand Surg. 1993;27(04):317–319. [PubMed] [Google Scholar]
- 3.Surzur P, Rigault M, Charissoux J L, Mabit C, Arnaud J P. [Recent fractures of the base of the 1st metacarpal bone. A study of a series of 138 cases] Ann Chir Main Memb Super. 1994;13(02):122–134. doi: 10.1016/s0753-9053(05)80385-0. [DOI] [PubMed] [Google Scholar]
- 4.Houshian S, Jing S S. Treatment of Rolando fracture by capsuloligamentotaxis using mini external fixator: a report of 16 cases. Hand Surg. 2013;18(01):73–78. doi: 10.1142/S0218810413500147. [DOI] [PubMed] [Google Scholar]
- 5.El-Sharkawy A A, El-Mofty A O, Moharram A N, Abou Elatta M M, Asal F. Management of Rolando fracture by modified dynamic external fixation: a new technique. Tech Hand Up Extrem Surg. 2009;13(01):11–15. doi: 10.1097/BTH.0b013e3181847652. [DOI] [PubMed] [Google Scholar]
- 6.Kontakis G M, Katonis P G, Steriopoulos K A.Rolando's fracture treated by closed reduction and external fixation Arch Orthop Trauma Surg 1998117(1-2):84–85. [DOI] [PubMed] [Google Scholar]
- 7.Proubasta I R, Sanchez A. Rolando's fracture: treatment by closed reduction and external fixation. Tech Hand Up Extrem Surg. 2000;4(04):251–256. [PubMed] [Google Scholar]
- 8.Gedda K O. Studies on Bennett's fracture; anatomy, roentgenology, and therapy. Acta Chir Scand Suppl. 1954;193:1–114. [PubMed] [Google Scholar]
- 9.Soyer A D. Fractures of the base of the first metacarpal: current treatment options. J Am Acad Orthop Surg. 1999;7(06):403–412. doi: 10.5435/00124635-199911000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Marsland D, Sanghrajka A P, Goldie B. Static monolateral external fixation for the Rolando fracture: a simple solution for a complex fracture. Ann R Coll Surg Engl. 2012;94(02):112–115. doi: 10.1308/003588412X13171221501140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pollen A G. The conservative treatment of Bennett's fracture-subluxation of the thumb metacarpal. J Bone Joint Surg Br. 1968;50(01):91–101. [PubMed] [Google Scholar]
- 12.Byrne A M, Kearns S R, Morris S, Kelly E P. “S” Quattro external fixation for complex intra-articular thumb fractures. J Orthop Surg (Hong Kong) 2008;16(02):170–174. doi: 10.1177/230949900801600208. [DOI] [PubMed] [Google Scholar]
- 13.Foster R J, Hastings H., II Treatment of Bennett, Rolando, and vertical intraarticular trapezial fractures. Clin Orthop Relat Res. 1987;(214):121–129. [PubMed] [Google Scholar]
- 14.Langhoff O, Andersen K, Kjaer-Petersen K. Rolando's fracture. J Hand Surg [Br] 1991;16(04):454–459. doi: 10.1016/0266-7681(91)90027-l. [DOI] [PubMed] [Google Scholar]
- 15.Wang W, Zeng M, Yang J, Wang L, Xie J, Hu Y. Clinical efficacy of closed reduction and percutaneous parallel K-wire interlocking fixation of first metacarpal base fracture. J Orthop Surg Res. 2021;16(01):454. doi: 10.1186/s13018-021-02600-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Howard F M. Fractures of the basal joint of the thumb. Clin Orthop Relat Res. 1987;(220):46–51. [PubMed] [Google Scholar]
- 17.Greeven A PA, Alta T DW, Scholtens R EM, de Heer P, van der Linden F M. Closed reduction intermetacarpal Kirschner wire fixation in the treatment of unstable fractures of the base of the first metacarpal. Injury. 2012;43(02):246–251. doi: 10.1016/j.injury.2011.10.038. [DOI] [PubMed] [Google Scholar]
- 18.Kjaer-Petersen K, Langhoff O, Andersen K. Bennett's fracture. J Hand Surg [Br] 1990;15(01):58–61. doi: 10.1016/0266-7681_90_90049-a. [DOI] [PubMed] [Google Scholar]
- 19.Wagner C J. Method of treatment of Bennett's fracture dislocation. Am J Surg. 1950;80(02):230–231. doi: 10.1016/0002-9610(50)90537-x. [DOI] [PubMed] [Google Scholar]
- 20.Fahmy N R. The Stockport Serpentine Spring System for the treatment of displaced comminuted intra-articular phalangeal fractures. J Hand Surg [Br] 1990;15(03):303–311. doi: 10.1016/0266-7681_90_90009-s. [DOI] [PubMed] [Google Scholar]
- 21.Upper Extremity Collaborative Group . Beaton D E, Wright J G, Katz J N. Development of the QuickDASH: comparison of three item-reduction approaches. J Bone Joint Surg Am. 2005;87(05):1038–1046. doi: 10.2106/JBJS.D.02060. [DOI] [PubMed] [Google Scholar]


