ABSTRACT
Aim:
To find out the prevalence of OSMF and its Co-relation of clinical grading to various habit factors (time span of habit practiced in years, repetition of habit practiced per day, time of habit practiced in minutes per use).
Method:
This descriptive, cross-sectional survey was carried out and close ended questionnaire was used for data collection. Demographic details like gender & age and different tissue exploiting habits like, chewing gutkha, chewing areca nut, chewing panmasala with or without tobacco, plain tobacco, mawa, smoking, alcohol was recorded. Also, duration of habit in years, repetition of habit per day, time of habit per use & site of involvement was recorded.
Results:
Among 5297 patients examined at OPD, 120 were diagnosed with OSMF. The present study found no statistical relation between age, gender & OSMF. The present study concluded that majority 83 (69.17%) of the OSMF patients are guthka user and buccal mucosa was most affected site. OSMF was more prevalent in patients who practiced the habit for more than 15 years.
Conclusion:
Among the OSMF patients, guthka was most commonly practiced & buccal mucosa was most commonly involved. Duration and frequency of consumption were significantly associated with severity of OSMF.
KEYWORDS: Guthka, OSMF, Pindborg classification
INTRODUCTION
Blanching and stiffness of the oral mucosa is the most common clinical characteristic of oral submucous fibrosis. Histologically, the oral connective tissue becomes hyalinized and the overlying epithelium markedly atrophic.[1] Various studies have reported areca nut/betel quid to be the most important etiological factor for the causation of OSMF. Various epidemiological, observational, case control, experimental and interventional studies have strongly shown the association between OSMF and areca nut.[2-7] Collagen synthesis and proliferation of fibroblasts stimulated by the alkaloids and flavonoids (arecoline, arecaidine, tannins and catechins) can act both as a chemical and physical irritant to oral mucosa.
The most common initial symptoms are burning sensation due to dry mouth, blanched oral mucosa and frequent ulceration. Increased fibrosis in this condition results in blanching of mucosa and marble like appearance.
In the later stages, fibrous bands are formed which causes trismus, difficulty in mastication, speech, swallowing and maintaining oral hygiene. Long-term follow-up studies over a period of 17 years shows a rate of malignant transformation of OSMF in the range of 7–13%.[8,9]
While there are numerous prevalence studies on OSMF in this region of India, there are no studies to corelate the prevalence to clinical grading with various habit factors. Thus, keeping in view the morbidity & mortality of OSMF, the present survey was carried out to study the prevalence of OSMF & its co-relation of clinical grading to various Habit Factors among outdoor patients visiting Buddha Institute of Dental Sciences & Hospital, Patna.
MATERIAL AND METHODS
This descriptive, cross-sectional survey was carried out in the outpatient Department of Buddha Institute of Dental Sciences and Hospital, Patna. Ethical clearance (No. 72/BIDSH) was obtained by the ethical committee of Buddha Institute of Dental Sciences for this study. Among 5297 of regular patient visiting the OPD, 120 clinically diagnosed cases of OSMF were considered for the study. Patients with any other systemic disease and with any other white or red lesion except OSMF are excluded.
Selected patients were informed about the survey prior to data collection. Close- ended questionnaire was used for data collection during this survey. Demographic details like age & gender and different tissue exploiting habits like, chewing gutkha, chewing areca nut, chewing pan masala with or without tobacco, and habit of plain tobacco, mawa, smoking, alcohol was recorded. Also, timespan of habit in years, repetition of habit per day, time of habit per use & site of involvement was recorded
Clinical criteria described by Pinborg et al in 1984 for the diagnosis of OSMF was used for recording. Pindborg JJ classified OSMF in three stages according to clinical features.[3]
Stage 1: Stomatitis includes erythematous mucosa, vesicles, mucosal ulcers, melanotic mucosal pigmentation & mucosal petechiae
Stage 2: Fibrosis occurs in the healing vesicles & ulcers, which is the hallmark of this stage. blanching of the oral mucosa is the early sign of this lesion. Older lesions include circular & vertical palpebral band in the buccal mucosa & around the mouth opening or lips. This results in a mottled marble like appearance of the mucosa because of vertical thick fibrous bands in association with blanched mucosa. Reduction of mouth opening, stiff & small tongue, blanched & leathery floor of the mouth, fibrotic & depigmented gingiva, rubbery soft palate with decreased mobility, atrophic tonsils, shrunken bud like uvula & sunken cheeks not commensurate with age or nutritional status are the fixed set of finding associated to this lesion.
Stage 3: Leukoplakia is present in more than 25% of the individuals with OSMF. Involvement of tongue & eustachian tube can progress into speech and hearing difficulty.
Pearson’s Chi -Square test was used to analysed the collected data.
RESULTS
Among 5297 patients visiting the outpatient department of Buddha Institute of Dental Sciences & Hospital, 120 were diagnosed with OSMF, thus the prevalence of OSMF was 2.26%.
The present study found no statistical relation between age, gender & OSMF [Table 1]. Majority 83 (69.17%) of the OSMF patients in the study were guthka users followed by Pan and Areca (12.5%), Mawa (12.5%), Tobacco (2.5%), Smoking & pan masala (1.67%) and Alcohol & pan masala (1.67 %). In majority of patients, the lesion involved only one site, i.e., buccal mucosa (62.5%). In 17.5% of patients, three sites namely buccal mucosa, soft palate and tongue was involved followed by involvement of buccal mucosa and soft palate in 15.8% of patients.
Table 1.
Table showing relation between age, gender & prevalence of OSMF
| Age group | Gender | Total | |
|---|---|---|---|
|
| |||
| Male | Female | ||
| 11-20 | 11 | 0 | 11 |
| 100.0% | .0% | 100.0% | |
| 21-30 | 35 | 1 | 36 |
| 31-40 | 19 | 2 | 21 |
| 90.5% | 9.5% | 100.0% | |
| 41-50 | 12 | 1 | 13 |
| 92.3% | 7.7% | 100.0% | |
| >50 | 38 | 1 | 39 |
| 97.4% | 2.6% | 100.0% | |
| Total | 115 | 5 | 120 |
| 95.8% | 4.2% | 100.0% | |
P=0.589
The present study revealed that 52 (43.3%) patients were in Stage 1, 21 (17.5%) are in Stage 2a, 21 (17.5%) are in stage 2b and 26 (21.6%) are in stage 3 of OSMF according to Pindborg’s classification [Figure 1]. The present study reveals that among 26 (21.6%) patients in stage 3 OSMF, the majority (20.83%) practiced guthka. Guthka was significantly associated with severity of OSMF with P value = 0.011 [Table 2]. Among the 26 patients in Stage 3 of OSMF, 25 (20.83%) practiced the habit for more than 15 years while among the 52 (43.3%) patients in Stage 1 OSMF only 8 (6.6%) practiced the habit for more than 15 years. Thus, OSMF was significantly associated with increased duration of habit in years with P < 0.001 [Table 3]. Among the 26 patients in stage 3 of OSMF, 25 (20.83%) practiced the habit for more than 10 times/day while among the 52 (43.3%) patients in stage 1 of OSMF only 10 (8.3%) practiced the habit for more than 10 times/day. OSMF severity was significantly associated with frequency of habit practiced per day with P < 0.001 [Table 4].
Figure 1.
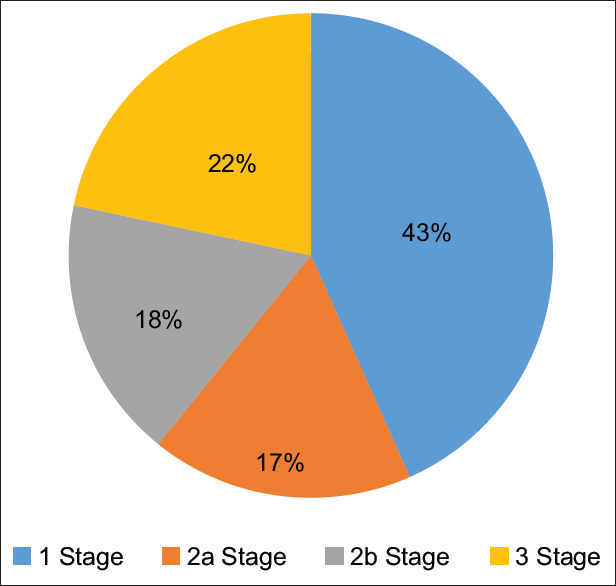
Distribution of OSMF according to Pindborg classification
Table 2.
Distribution of stages of OSMF according to type of habit
| Type of habit | Stage 1 | Stage 2a | Stage 2b | Stage 3 | Total |
|---|---|---|---|---|---|
| Guthka | 30 (25%) | 11 (9.1%) | 17 (14.16%) | 25 (20.83%) | 83 (69.16%) |
| Pan & Araeca nut | 9 (7.5%) | 6 (5%) | 0 (0%) | 0 (0%) | 15 (12.5%) |
| Smoking & pan masala | 0 (0%) | 0 (0%) | 1 (0.83%) | 1 (0.83%) | 2 (1.6%) |
| Alcohol & pan masala | 1 (0.83%) | 0 (0%) | 1 (0.83%) | 0 (0%) | 2 (1.6%) |
| Mawa | 10 (8.3%) | 4 (3.3%) | 1 (0.83%) | 0 (0%) | 15 (12.5%) |
| Tobacco | 2 (1.6%) | 0 (0%) | 1 (0.83%) | 0 (0%) | 3 (2.5%) |
| Total | 52 (43.3%) | 21 (17.5%) | 21 (17.5%) | 26 (21.6%) | 120 (100%) |
P=0.011
Table 3.
Distribution of OSMF according to duration of habit
| Duration of habit/year | Stage 1 | Stage 2a | Stage 2b | Stage 3 | Total |
|---|---|---|---|---|---|
| 0-5 years | 32 (26.6%) | 0 (0%) | 0 (0%) | 0 (0%) | 32 (26.6%) |
| 6-10 years | 5 (4.1%) | 4 (3.3%) | 1 (0.83%) | 0 (0%) | 10 (8.23%) |
| 10-15 years | 7 (5.8%) | 7 (5.8%) | 5 (4.1%) | 1 (0.83%) | 20 (16.6%) |
| >15 years | 8 (6.6%) | 10 (8.3%) | 15 (12.5%) | 25 (20.83%) | 58 (48.3%) |
| Total | 52 (43.3%) | 21 (17.5%) | 21 (17.5%) | 26 (21.6%) | 120 (100%) |
P <0.001
Table 4.
Distribution of OSMF according to frequency of habit
| Frequency of habit/day | Stage 1 | Stage 2a | Stage 2b | Stage 3 | Total |
|---|---|---|---|---|---|
| 1-3 times/day | 8 (6.6%) | (0%) | (0%) | (0%) | 8 (6.6%) |
| 3-6 times/day | 32 (26.6%) | (0%) | 1 (0.83%) | (0%) | 33 (27.5%) |
| 6-10 times/day | 2 (1.66%) | 11 (9.1%) | 3 (2.5%) | 1 (0.83%) | 17 (14.1%) |
| >10 times/day | 10 (8.3%) | 10 (8.3%) | 17 (14.5%) | 25 (20.83%) | 62 (51.6%) |
| Total | 52 (43.3%) | 21 (17.5%) | 21 (17.5%) | 26 (21.6%) | 120 (100%) |
DISCUSSION
OSMF is an insidious, chronic disease affecting mainly the buccal mucosa but sometimes may extend to soft palate and pharynx. It is characterized by localized or diffuse ulceration, burning sensation, fibrosis of oral tissues and trismus. The condition shows a strong confinement to Indians & South East Asians & strong predisposition to malignant transformation.[10-12]
The prevalence of OSMF in the present study is 2.26% which is in agreement with other study done by Rao et al.[9] Majority of the study population (32.5%) belongs to age group >50 years followed by 31–40 years age group which had 36 (30%) OSMF patients. In contrast other studies have reported that majority of OSMF patients affected are in the third decade age group. The present study shows male predisposition of OSMF which is same in other studies.[9-12]
The present study found guthka (pan masala) to be most commonly practiced by OSMF patients (69.17%) followed by pan & areca nut (12.5%) & mawa (12.5%). Guthka is a combination of areca nut, slaked lime, paraffin & katechu along with tobacco & marketed by name of pan masala. Study conducted by Ranganathan et al.[13] concluded that all areca nut products were associated with OSMF, with the risk being highest for guthka (pan masala).
It is because average betel quid (areca nut, tobacco, catechu & lime wrapped in betel leaf) approximately weighing 3.5–4 g has 70% moisture & dry weight of areca nut & tobacco is only 1.14 g whereas the guthka sachet weighing 3.5 gm has only 7% moisture & dry weight 3.26 g.[14] Since habitual chewers tend to consume more dry weight of areca nut & tobacco when they use guthka so they probably develop more fibrosis of oral mucosa. The present study did not observed tobacco, smoking or alcohol as the etiological factor for OSMF which is in accordance with other study.[6] The most common site to be affected in the present study is buccal mucosa among 62.5% patients which is in accordance to other studies.[11-13]
The present study concluded that as the duration of the habit in years increased, the severity of OSMF increased. Patients (20.83%) who were exposed to habit for more than 15 years had Stage 3 OSMF than patients who were exposed to habit for less than 5 years (0%) which is in accordance with other studies.[5]
CONCLUSION
Guthka has high tobacco ingredients like nitrosamine, areca nut & alkaloid arecoline and its absorbtion in patients depends upon frequency and duration of its use. The study suggests that gutkha is the most common cause of this premalignant lesion. As habit progressed with time, repetition of habit per day & time of persuing habit per use increased and this had significant correlation to severity of clinical grading. Promotion of these products by celebrities influence the people of all aged and such advertisement should be strictly banned on social platform.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Pindborg JJ, Sirasat Satyavati M. Oral submucous fibrosis. Oral Surg Oral Med Oral Pathol. 1966;22:764–9. doi: 10.1016/0030-4220(66)90367-7. [DOI] [PubMed] [Google Scholar]
- 2.Seedat HA, Van Wyk CW. Betel nut chewing and oral submucous fibrosis in Durban. S Afr Med J. 1988;74:572–5. [PubMed] [Google Scholar]
- 3.Pindborg JJ, Murti PR, Bhonsle RB, Gupta PC, Daftary DK, Metha FS. Oral submucous fibrosis as a precancerous condition. Scand J Dent Res. 1984;92:224–9. doi: 10.1111/j.1600-0722.1984.tb00883.x. [DOI] [PubMed] [Google Scholar]
- 4.Sinor PN, Gupta PC, Murti PR, Bhonsle RB, Daftary DK, Mehta FS, et al. A case-control study of oral submucous fibrosis with special reference to the aetiologic role of areca nut. J Oral Pathol Med. 1990;19:94–8. doi: 10.1111/j.1600-0714.1990.tb00804.x. [DOI] [PubMed] [Google Scholar]
- 5.Maher R, Lee AJ, Warnakulasuriya KA, Lewis JA, Johnson NW. Role of areca nut in the causation of oral submucous fibrosis:A case control study in Pakistan. J Oral Pathol Med. 1994;23:65–9. doi: 10.1111/j.1600-0714.1994.tb00258.x. [DOI] [PubMed] [Google Scholar]
- 6.Shah N, Sharma PP. Role of chewing and smoking habits in the aetiology of oral submucous fibrosis (OSF):A case control study. J Oral Pathol Med. 1998;27:475–9. doi: 10.1111/j.1600-0714.1998.tb01915.x. [DOI] [PubMed] [Google Scholar]
- 7.Ajit A, Rosin MP, Zhang L, Sumanth KN. Oral submucous fibrosis, a clinically benign but potentially malignant disease:Report of 3 cases and review of the literature. J Can Dent Assoc. 2008;74:735–40. [PubMed] [Google Scholar]
- 8.Ahher V, Ali FM, Bhushan P, Mudhol A, Prasant MC, Suryavanshi H. Oral submucous fibrosis:Comparing clinical grading with duration and frequency of habit among areca nut and its products chewers. J Cancer Res Ther. 2013;9:471–6. doi: 10.4103/0973-1482.119353. [DOI] [PubMed] [Google Scholar]
- 9.Rao RN, Villa A, More BC, Jayasinghe RD, Kerr AR, Johnson NW. Oral submucous fibrosis:A contemporary narrative review with a proposed inter-professional approach for an early diagnosis and clinical management. J Otolaryngol Head Neck Surg. 2020;49:3. doi: 10.1186/s40463-020-0399-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Srivastava R, Jyoti B, Pradhan D, Siddiqui Z. Prevalence of oral submucous fibrosis in patients visiting dental OPD of a dental college in Kanpur:A demographic study. J Family Mad Prim Care. 2019;8:2612–7. doi: 10.4103/jfmpc.jfmpc_465_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reddy V, Wanjari PV, Banda NR, Reddy P. Oral submucous fibrosis:Correlation of clinical grading to various habit factors. Int J Dent Clin. 2011;3:21–4. doi: 10.4103/jispcd.JISPCD_92_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ahmad MS, Ali SA, Ali AS, Chaubey KK. Epidemiological and etiological study of oral submucous fibrosis among guthka chewers of Patna. J Indian Soc Pedod Prev Dent. 2006;24:84–9. doi: 10.4103/0970-4388.26022. [DOI] [PubMed] [Google Scholar]
- 13.Ranganathan K, Devi MU, Joshua E, Kirankumar K, Saraswati R. Oral submucous fibrosis:A case control study. J Oral Pathol Med. 1998;27:475–9. doi: 10.1111/j.0904-2512.2004.00116.x. [DOI] [PubMed] [Google Scholar]
- 14.Babu S, Bhat RV, Kumar PU, Sesikaran B, Rao KV, Aruna P, et al. A comparative clinico-pathological study of oral submucous fibrosis in habitual chewers of pan masala and betelquid. J Toxicol Clin Toxicol. 1996;34:317–22. doi: 10.3109/15563659609013796. [DOI] [PubMed] [Google Scholar]


