Abstract
Objective:
To report 8-year outcomes from a randomized controlled trial (RCT) comparing bilateral lateral rectus muscle recessions (BLRc) with unilateral recess-resect (R&R) for childhood intermittent exotropia (IXT).
Design:
Eight-year follow-up of RCT cohort
Participants:
123 of 197 randomized participants agreed to continue follow-up after the 3-year outcome visit (baseline age 3 to <11 years with basic-type IXT 15-40 prism diopters (Δ) by prism and alternate cover test (PACT), baseline stereoacuity of 400 arcsec or better, no prior surgery)
Methods:
Following the RCT primary outcome at 3 years, annual follow-up from 4 through 8 years with treatment at investigator discretion.
Main Outcome Measures:
Suboptimal surgical outcome by 8 years after randomization, defined as any of the following at any visit: exotropia ≥10Δ by simultaneous prism cover test (SPCT) at distance or near; constant esotropia (ET) ≥6Δ by SPCT at distance or near; loss of near stereoacuity by ≥0.6 log arcsec from baseline; or reoperation. Secondary outcomes included 1) reoperation by 8 years and 2) complete or near-complete resolution at 8 years: exodeviation <10Δ by SPCT and PACT at distance and near and ≥10Δ reduction from baseline PACT at distance and near; ET <6Δ at distance and near; no decrease in stereoacuity by ≥0.6 log arcsec from baseline; no reoperation or nonsurgical treatment for IXT.
Results:
The Kaplan-Meier cumulative probability of suboptimal surgical outcome through 8 years was 68% (55 events among 101 at risk) for BLRc and 53% (42 events among 96 at risk) for R&R (difference = 15%, 95% CI: −2% to 32%, P = 0.08). Complete or near-complete resolution at 8 years occurred in 14% (6/42) for BLRc and 37% (16/43) for R&R (difference = −22%, 95% CI: −44% to −0.1%, P = 0.049). The cumulative probability of reoperation was 30% for BLRc and 11% for R&R (difference = 19%, 95% CI=2% to 36%, P = 0.049).
Conclusions:
Despite no significant difference at primary outcome, the 95% CI did not exclude a moderate benefit of R&R, which together with secondary outcomes, suggests that unilateral R&R followed by usual care may yield better long-term outcomes than BLRc followed by usual care, for basic-type childhood IXT, using our surgical doses.
Precis:
Over eight years following surgery and usual care, differences in suboptimal outcomes for recess-resect versus bilateral recessions for childhood intermittent exotropia were not statistically significant, but secondary outcomes suggested benefit of recess-resect.
Intermittent exotropia (IXT) is a common form of childhood-onset strabismus1 for which surgical correction is often performed.2-4 One unresolved question is whether post-operative outcomes differ with bilateral lateral rectus recessions (BLRc) versus unilateral lateral rectus muscle recession with medial rectus muscle resection (R&R). We previously reported the results of an RCT5 comparing BLRc and R&R procedures for basic type IXT in children 3 to <11 years old, in which we found no statistically significant difference in sub-optimal outcome by 3 years postoperatively (46% in BLRc and 37% in R&R; difference = 9%; 95% confidence interval (CI): −6% to 23%).5 We are aware of three other RCTs that have addressed this question. Both Kushner6 and Somer et al7 reported higher success rates at one year after surgery with R&R vs. BLRc, whereas Zhang et al8 reported that both groups had similar success rates over the same period. Given the propensity of IXT to recur over time,9,10 longer-term effectiveness of surgical approaches should also be evaluated. The purpose of the present study was to evaluate long-term outcomes 8 years after surgery in the PEDIG RCT for which 3-year outcomes have been previously reported.5
Methods
The study was funded by the National Eye Institute of the National Institutes of Health and conducted according to the tenets of the Declaration of Helsinki by the Pediatric Eye Disease Investigator Group (PEDIG) at 35 academic and community-based clinical sites. The protocol and Health Insurance Portability and Accountability Act (HIPAA)-compliant informed consent forms were approved by institutional review boards for each site, and a parent or guardian of each study participant gave written informed consent. The study is listed on www.clinicaltrials.gov (clinicalcaltrials.gov identifier: NCT01032603);11 the full protocol is available at www.pedig.net (accessed 2/6/23).
Original 3-year Randomized Controlled Trial
We enrolled 197 children, age 3 to <11 years, with basic-type IXT, 15 to 40Δ (largest deviation at near, distance, or remote distance) by prism and alternate cover test (PACT), and near stereoacuity of at least 400 arc-seconds using the Randot® Preschool Stereoacuity test (Stereo Optical Co., Inc., Chicago, IL). Participants were randomly assigned to one of two surgical procedures: BLRc or R&R. Follow-up visits occurred every six months after surgery for 3 years. Reoperation was permitted only after suboptimal surgical outcome criteria were met and confirmed by a retest. Additional details of the protocol and results have been published previously.5,12
4 to 8-Years Post-Randomized Trial Follow-up (Extension Study)
The extension study (4-to-8-year follow-up) was implemented in February 2015. The parent or guardian for each randomized participant was asked to reconsent to extended follow-up, regardless of whether they were still active, had completed, or had withdrawn from the 3-year RCT. Participants who consented to the extension study had follow-up visits at 4, 5, 6, 7, and 8 years (±2 months) from randomization. At each follow-up visit, an examiner masked to the participant’s treatment group measured near stereoacuity using the Randot® Preschool Stereoacuity test, exotropia control using the IXT Office Control Scale 13,14 (Table S1) (mean of 3 measures [beginning, middle, and end of the masked exam) at distance and near, cover-uncover test, simultaneous prism and cover test (SPCT), and PACT at distance and near. At the 8-year visit, the Intermittent Exotropia Questionnaire (IXTQ) was administered to the child and parent to measure IXT-related quality of life and the Diplopia Questionnaire15 was administered to the child to assess the presence and frequency of diplopia in specific gaze positions.
Statistical Methods
In parallel with the previously reported 3-year outcomes, the primary outcome for the current analysis was suboptimal surgical outcome by 8 years was defined as any of the following at any follow-up examination from 6 months to 8 years: 1) ≥10Δ exotropia by SPCT at distance or near; 2) constant esotropia of ≥6Δ by SPCT; 3) loss of ≥0.6 log arcsec stereoacuity compared with baseline; or 4) reoperation without meeting any other criteria. Suboptimal surgical outcome had to be confirmed by a retest during the 3-year RCT; however, retesting was not performed during the 4-to-8-year follow-up to streamline visits and reduce participant testing burden.
For the primary analysis, the cumulative proportion of participants meeting criteria for suboptimal surgical outcome by 8 years was obtained using the Kaplan-Meier method and compared between treatment groups using the Z test. Assessment of suboptimal surgical outcome by 8 years included all participants originally enrolled in the RCT regardless of their participation in the extension study. Data for participants who did not meet suboptimal surgical outcome criteria were censored at the time of their last completed study visit.
Several secondary outcomes were analyzed. The cumulative proportion of reoperation by 8 years was compared between treatment groups using the same statistical methods used for the primary analysis. Additional secondary analyses were treatment group comparisons of outcomes at the 8-year visit (from participants who completed the 8-year visit within the analysis window of 7.5 to <9 years from randomization). At 8 years, the proportions of participants with: 1) suboptimal surgical outcome, 2) complete or near-complete resolution criteria, 3) spontaneous exotropia during the examination or average control score of 3 or higher at distance or near, and 4) a decrease in Randot Preschool stereoacuity of ≥0.6 log arcsec from enrollment, were compared between treatment groups using Barnard’s unconditional exact test. Suboptimal surgical outcome at 8 years was defined as meeting any of the three suboptimal surgical outcome criteria at the 8-year follow-up visit (regardless of whether any criterion had been met at an earlier visit) or undergoing reoperation at any time before completing the 8-year visit. Complete or near-complete resolution at 8 years was defined as meeting all of the following at the 8-year visit: 1) exodeviation <10 Δ (tropia or phoria) by both SPCT and PACT at distance and near and ≥10 Δ reduction in PACT magnitude from both the distance and near angles at enrollment if the exodeviation was ≥10 Δ at baseline (and reduction to 0 if the exodeviation was <10 Δ at baseline), 2) esotropia <6 Δ at distance and near by SPCT, 3) no decrease in Randot Preschool stereoacuity of ≥0.6 log arcsec from the enrollment stereoacuity or to nil, 4) no reoperation or treatment with botulinum toxin, and 5) no non-surgical treatment for a recurrent or residual exodeviation. In addition, distance and near control, distance and near PACT, and Randot Preschool stereoacuity at the 8-year visit were compared between treatment groups using analysis of covariance (ANCOVA), adjusting for the corresponding measurement at enrollment. In the ANCOVA models, for the participants who underwent reoperation during the 8-year follow-up, their data at the last visit before reoperation were used for analyses. The type I error rate for all secondary outcomes was controlled using the adaptive false discovery rate (FDR)16,17 approach to account for multiplicity, with the FDR controlled at the 5% probability level.
As exploratory analyses, we compared the mean Rasch-based HRQOL scores for the child IXTQ, each of the three parent IXTQ subscales, and the Diplopia Questionnaire scores15 at 8 years between treatment groups using the Wilcoxon rank-sum test and Hodges-Lehmann estimator without adjustment for multiplicity.
All treatment-group differences were calculated as the BLRc group minus the R&R group. Analyses were conducted using SAS version 9.4 (SAS Institute Inc. Cary, NC).
Results
Baseline Characteristics
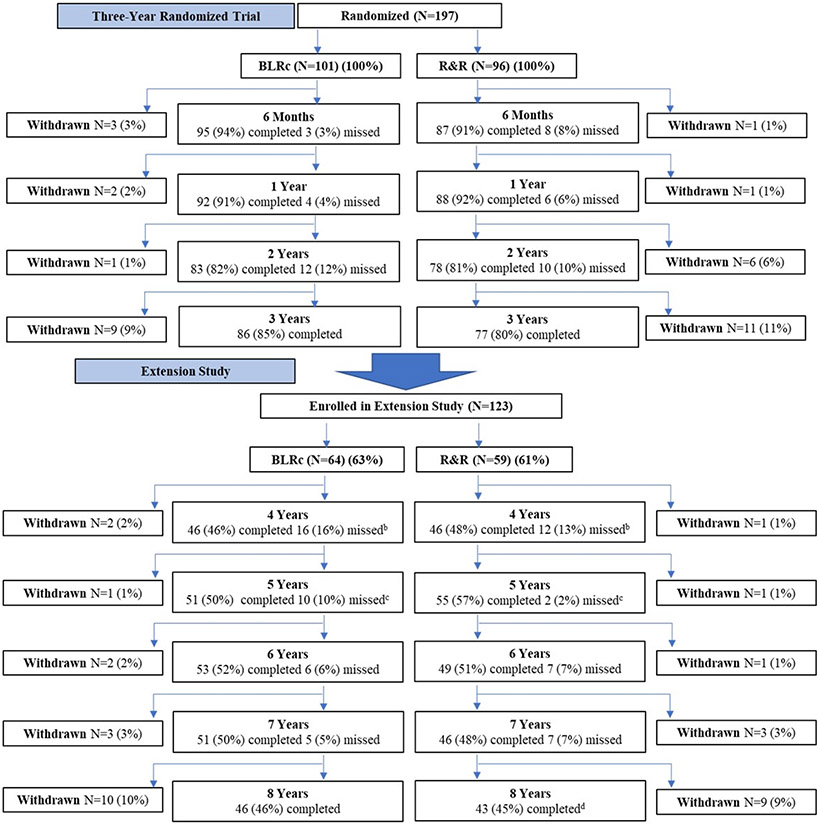
In the original 3-year RCT, 197 children were enrolled at 34 clinical sites with 101 assigned to the BLRc group and 96 assigned to the R&R (Figure 1); 123 (62%) elected to participate in the present extension study (64 from BLRc group and 59 from R&R group). In the BLRc and R&R groups, respectively, 46 (46% of 101 randomized; 72% of 64 enrolled in the extension) and 43 (45% of 96 randomized; 73% of 59 enrolled in the extension) of participants completed the 8-year visit. There did not appear to be meaningful differences in demographic and clinical characteristics at baseline between those who completed the 8-year visit and those who did not (either did not participate in the extension or were dropped during the extension) (Table S1).
Figure 1. Flow of Participants through Study.
BLRc = bilateral lateral rectus muscle recession; R&R = unilateral lateral rectus recession combined with a medial rectus resection in same eye.
Primary Outcome – Suboptimal Surgical Outcome by 8 Years
The Kaplan-Meier cumulative probability of suboptimal surgical outcome at any time point through 8 years was 68% (55 events among 101 at risk) in the BLRc group and 53% (42 events among 96 at risk) in the R&R group; the difference between BLRc and R&R was 15% (95% CI = −2% to 32%, P = 0.08) (Table 2, Figure 2). The most common reason for suboptimal surgical outcome was a residual or recurrent exotropia (34 of 55 [62%] in the BLRc group and 27 of 42 [64%] in the R&R group) (Table 2).
Table 2.
Suboptimal Surgical Outcome at Follow-up Visits
| Randomized Trial Period | Extension Study Period | Total | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 to 1 Year | >1 Year to 2 Years |
>2 Years to 3 Years |
>3 Years to 4 Years |
>4 Years to 5 Years |
>5 Years to 6 Years |
>6 Years to 7 Years |
>7 Years to 8 Years |
|||||||||||
| BLRc | R&R | BLRc | R&R | BLRc | R&R | BLRc | R&R | BLRc | R&R | BLRc | R&R | BLRc | R&R | BLRc | R&R | BLRc | R&R | |
| N at risk | 101 | 96 | 71 | 75 | 58 | 57 | 48 | 50 | 31 | 39 | 25 | 37 | 22 | 29 | 21 | 25 | N/A | N/A |
| N with suboptimal surgical outcome | 26 | 24 | 13 | 5 | 4 | 4 | 2 | 1 | 6 | 6 | 1 | . | 1 | 1 | 2 | 1 | 55 | 42 |
| XTa | 17 | 12 | 9 | 5 | 3 | 4 | 1 | . | 1 | 5 | . | . | 1 | 1 | 2 | . | 34 | 27 |
| Constant ETb | 1 | 2 | . | . | . | . | . | . | . | . | . | . | . | . | . | . | 1 | 2 |
| Stereo lossc | 4 | 4 | 4 | . | 1 | . | . | 1 | 2 | 1 | 1 | . | . | . | . | 1 | 12 | 7 |
| Stereo loss and XT | 1 | . | . | . | . | . | 1 | . | . | . | . | . | . | . | . | . | 2 | . |
| Stereo loss and constant ET | 2 | 5 | . | . | . | . | . | . | . | . | . | . | . | . | . | . | 2 | 5 |
| Reoperated without meeting suboptimal surgical outcome | 1 | 1 | . | . | . | . | . | . | 3 | . | . | . | . | . | . | . | 4 | 1 |
| Cumulative probability of meeting suboptimal surgical outcome | 27% | 26% | 41% | 32% | 46% | 37% | 49% | 39% | 60% | 49% | 62% | 49% | 64% | 51% | 68% | 53% | N/A | N/A |
Abbreviations: BLRc = Bilateral lateral rectus muscle recession, R&R = Unilateral lateral rectus muscle recess-medial rectus muscle resection.
XT = exotropia ≥10Δ by SPCT at distance or near.
Constant ET = constant esotropia ≥6Δ by SPCT at distance or near.
Stereo loss = decrease in Preschool Randot near stereoacuity ≥0.6 log arcsec from enrollment, or to nil.
Figure 2. Suboptimal Surgical Outcome By 8 Years.
Cumulative probability (and 95% confidence interval) of suboptimal surgical outcome over 8 years from Kaplan-Meier analysis. BLRc = bilateral lateral rectus muscle recession; R&R = unilateral lateral rectus muscle recession combined with a medial rectus muscle resection in same eye
Secondary Outcome – Reoperation by 8 Years
The cumulative probability of reoperation by 8 years was 30% (20 events among 101 at risk) with BLRc and 11% (7 events among 96 at risk) with R&R; the difference between BLRc and R&R was 19% (95% CI = 2% to 36%, P = 0.049) (Figure 3). Among participants who met suboptimal surgical outcome criteria, reoperation was performed for 30% (16 of 51) in the BLRc group and 14% (6 of 41) in the R&R group. In the BLRc group, 18 (90%) of 20 reoperations were for residual-recurrent exotropia, 1 (5%) was for consecutive esotropia, and 1 (5%) was for oblique muscle dysfunction; in the R&R group, 4 (57%) of 7 reoperations were for residual or recurrent exotropia and 3 (43%) were for consecutive esotropia.
Figure 3: Reoperation by 8 Years.
Cumulative probability (and 95% confidence interval) of reoperation over 8 years from Kaplan-Meier analysis. BLRc = bilateral lateral rectus muscle recession; R&R = unilateral lateral rectus recession combined with a medial rectus resection in same eye. Among the reoperations occurred during the 8-year follow-up, in the BLRc and R&R groups, respectively, 90% (18 of 20) and 57% (4 of 7) were to correct residual or recurrent exotropia, 5% (1 of 20) and 43% (3 of 7) were to correct consecutive esotropia, and 5% (1 of 20) and 0% (0 of 7) were to correct inferior oblique over-action.
Secondary Outcomes – Surgical Outcomes at the 8-Year Visit
Suboptimal surgical outcome at the 8-year visit was more likely with BLRc [48% (22 of 46)] than R&R [23% (10 of 43)] (difference = 25%; 95% CI = 0.2% to 50%, P = 0.049). Complete or near-complete resolution at the 8-year visit was less likely with BLRc [15% (7 of 46)] than with R&R [37% (16 of 43)] (difference = −22%; 95% CI = −44% to −0.1%, P = 0.049). Among participants completing the 8-year visit, reoperation was performed before 8 years in 14 of 46 (30%) in BLRc participants and 5 of 43 (12%) R&R participants. Most participants who had reoperation before the 8-year visit (13 of 14 in BLRc and 4 of 5 in R&R) also failed to meet at least one additional criterion for complete or near-complete resolution at 8 years.
Secondary Outcomes – Change in Exotropia Control PACT Magnitude, and Stereoacuity at 8 Years
The mean (standard deviation) distance exotropia control score at 8 years was 1.6 (1.8) in the BLRc group and 0.8 (1.1) in the R&R group (adjusted difference = 0.8; 95% CI = 0.0 to 1.5, P = 0.049). There were no statistically significant differences in means between the BLRc and R&R groups for near exotropia control, distance or near PACT magnitude, and near stereoacuity at the 8-year visit (Table 3).
Table 3.
Exotropia Control, PACT Magnitude and Near Stereo Outcomes at 8 Years
| BLRc (N = 46) |
R&R (N = 43) |
Treatment-Group Difference (BLRc – R&R)a |
|||||
|---|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Difference | 95% Confidence Interval |
P | |||
| Control at Distance (0 to 5) | 1.6 | (1.8) | 0.8 | (1.1) | 0.8 | (0.0 to 1.5) | 0.049 |
| Control at Near (0 to 5) | 1.1 | (1.5) | 0.6 | (1.1) | 0.5 | (−0.2 to 1.1) | 0.21 |
| PACT at Distance (Δ) | 11.6 | (8.7) | 9.3 | (11.5) | 2.3 | (−2.6 to 7.1) | 0.41 |
| PACT at Near (Δ) | 12.2 | (10.5) | 8.5 | (13.1) | 3.6 | (−2.1 to 9.3) | 0.25 |
| Near Stereoacuity (logArcSec)b | 2.0 | (0.5) | 1.9 | (0.4) | 0.1 | (−0.1 to 0.3) | 0.44 |
| N | (%) | N | (%) | Difference | 95% Confidence Interval |
P | |
| Participants with spontaneous exotropia during the examination or average control score of 3 or higher at distance or near | 17 | (37%) | 12 | (28%) | 9% | (−13% to 32%) | 0.53 |
| Participants with decrease in near stereoacuity ≥0.6 log arcsec from baseline b | 7 | (15%) | 4 | (9%) | 6% | (−10% to 22%) | 0.53 |
Abbreviations: BLRc = Bilateral lateral rectus muscle recession, PACT = Prism and alternate cover test, R&R = Unilateral lateral rectus muscle recess-medial rectus muscle resection in same eye SD = standard deviation.
The confidence intervals and P values were adjusted using the adaptive false discovery rate (FDR) approach to account for multiplicity, with the overall FDR controlled at the 5% probability level. The analyses of control at distance, control at near, PACT at distance, PACT at near, and near stereoacuity were adjusted for corresponding measure at baseline.
The near stereoacuity at 8 years was not available for 1 participant in the R&R group.
Exploratory Outcomes – IXT-related Quality of Life and Diplopia at 8 Years
There were no substantial differences between the BLRc and R&R treatment groups in the distribution of the mean Rasch-based HRQOL scores for the child IXTQ and each of the three parent IXTQ domains (Tables 4, S5, and S6). On the Diplopia Questionnaire, diplopia in any direction in the past week was reported in 8 of 46 participants (17%) from the BLRc group and in 4 of 41 participants (10%) from the R&R group. For those four R&R participants who reported diplopia, 2 reported diplopia in side gaze, 1 in the direction of the non-operated eye (in the field of action of the operated medial rectus muscle), 1 in both the right and left gaze. Mean Diplopia Questionnaire scores at 8 years also did not differ substantially between treatment groups (Tables 4 and S7).
Table 4.
Child Intermittent Exotropia Questionnaire (IXTQ), Parent IXTQ, and Diplopia Questionnaire Scores at 8 Years
| BLRc | R&R | Treatment-Group Difference (BLRc – R&R) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| N | Median | Interquartile Range |
N | Median | Interquartile Range |
Hodges-Lehmann Estimatora |
95% Confidence Interval |
Pb | |
| IXTQ Domain Scores | |||||||||
| Child | 46 | 86 | (77 to 95) | 41 | 91 | (77 to 100) | 0.0 | (−9.1 to 4.6) | 0.54 |
| Parent Psychosocial Domain | 42 | 97 | (86 to 100) | 40 | 98 | (81 to 100) | 0.0 | (0.0 to 3.1) | 0.86 |
| Parent Function Domain | 42 | 88 | (78 to 94) | 40 | 89 | (78 to 97) | 0.0 | (−5.6 to 2.8) | 0.67 |
| Parent Surgery Domain | 42 | 92 | (69 to 100) | 40 | 100 | (83 to 100) | 0.0 | (−8.4 to 0.0) | 0.45 |
| Diplopia Questionnaire Scores | 46 | 0 | (0 to 0) | 41 | 0 | (0 to 0) | 0.0 | (0.0 to 0.0) | 0.26 |
Abbreviations: BLRc = Bilateral lateral rectus muscle recession, R&R = Unilateral recess-resect, PACT = Prism and alternate cover test, IXTQ: Intermittent Exotropia Questionnaire.
The Hodges-Lehmann estimator is the median of all paired differences.
Wilcoxon Rank-Sum Test.
Postoperative Nonsurgical Treatment
During 8 years of follow-up, postoperative nonsurgical treatment was prescribed in 26% (26 of 101) of participants in the BLRc group and in 44% (42 of 96) in the R&R group (Table S8). Patching (alone or with other treatments) was prescribed for 4 (4%) and 26 (27%) of those in the BLRc and R&R groups, respectively. This difference was primarily due to more patching for esotropia being prescribed in the R&R group early in the post-operative course rather than patching for recurrent or residual exotropia. Orthoptic exercises (alone or with other treatments) were prescribed for 10 (10%) and 10 (10%) of participants in the BLRc and R&R groups, respectively; (Table S8).
Discussion
The IXT1 randomized clinical trial was designed to compare suboptimal surgical outcomes after BLRc versus R&R procedures, followed by usual care, for children with basic-type IXT. We now report that the cumulative incidence of suboptimal surgical outcome by 8 years was not significantly different between groups (68% in BLRc vs. 53% R&R: difference = 15%; 95% CI −2% to 32%); however, the 95% CI of the estimated difference did not exclude a possible moderate benefit of R&R, but it did exclude a moderate benefit of BLRc. This result is consistent with our previous report5 of this cohort after three years of follow-up, in which the cumulative incidence of suboptimal surgical outcome was not statistically different between the two groups (46% in BLRc vs. 37% in R&R; difference = 9%; 95% CI = −6% to 23%), and the 95% CI did not exclude a possible moderate benefit of R&R but did exclude a moderate benefit of BLRc. It is noteworthy that four of our secondary outcomes (reoperation by 8 years, and complete or near-complete resolution, suboptimal surgical outcome at 8 years, and IXT distance control score at 8 years) also suggested a statistically significant benefit of R&R over BLRc, consistent with the trend observed in the primary outcome.
We are unaware of any previous studies that compare long-term outcomes between BLRc and R&R procedures for childhood IXT. Nevertheless, our data which suggest a benefit of R&R over BLRc for IXT are consistent with two previous RCTs reporting shorter-term outcomes. Kushner et al6 found a benefit at 12 months of R&R versus BLRc for basic IXT (82% success for R&R vs. 52% for BLRc; N=17 and 19, respectively). Kushner hypothesized that the restrictive effect created by the medial rectus resection tethers the eye in place decreasing the tendency for an outward drift and recurrence. Kushner’s hypothesis is consistent with our finding that the primary reason for reoperation was residual or recurrent exodeviation, particularly when the initial surgery was BLRc, and that the reoperation rate over 8 years was significantly lower when the initial surgery was R&R. Similarly, Somer et al7 reported 1-year success rates of 77% in 26 patients who underwent R&R and 48% in 21 patents who underwent BLRc. Conversely, Zhang et al8 found no difference in 1-year success rates of 89% and 79% in patients who underwent R&R and BLRc, respectively (N = 58 in both groups), and the 3-year outcomes from the current RCT5 did not indicate a statistically significant difference between R&R and BLRc in suboptimal surgical outcome by 3 years or reoperation by 3 years. Our report of 8-year surgical outcomes may be useful to patients, families, and clinicians by providing data regarding long-term alignment.
Another hypothesis consistent with the suggestion that BLRc results in worse long-term postoperative outcomes is that the dose tables used for the present study were insufficient for BLRc. It is noteworthy that while the original IXT1 protocol was in development, Lee and coauthors reported a case series that suggested better results with augmented bilateral lateral rectus muscle recessions.18 It is possible that our study results may have differed from the current results had augmented surgery tables been used.
Although some might consider the rates of suboptimal surgical outcomes high, we suggest that our a priori definition of suboptimal surgical outcome was fairly liberal and our definition of complete or near-complete resolution was fairly strict. The severity of childhood intermittent exotropia is often judged by the parent and the provider as the level of control. Recent IXT treatment trials have used control as the primary outcome measure.19,20 In the current RCT, if we consider an outcome measure that reflects control, it is noteworthy that at the final 8-year visit, 63% of the BLRc group and 72% of the R&R group did not have a spontaneous tropia during the examination or an average control score of 3 or higher at distance or near. These data suggest that the overall impact of strabismus surgery for childhood IXT, followed by usual care, appears to be more favorable than when judged using the study’s primary outcome measure.
Our study has some limitations. First, we obtained 8-year outcome data in about half of our randomized cohort, and therefore we cannot rule out potential selection bias in our analysis. However, we found no appreciable differences in baseline characteristics between those who completed follow-up and those who did not. Second, reoperation was at investigator discretion after suboptimal surgical outcome for the first 3 years and at any time between 4 and 8 years. It is possible that the decision by the parent, child, and treating provider to reoperate might have been biased by the type of initial surgery.
In summary, we found that the cumulative incidence of a suboptimal surgical outcome by 8 years was not significantly different between BLRc and R&R, followed by usual care, for childhood basic-type IXT. Nevertheless, the 95% CI of the estimated difference did not exclude a possible moderate benefit of R&R whereas it did exclude a moderate benefit of BLRc. Taking this finding together with important secondary outcomes (including complete or near-complete resolution at 8 years and reoperation rate by 8 years) suggests that R&R may result in better long-term outcomes than BLRc using the surgical doses chosen for the present study. Overall, the results of surgery followed by usual care were somewhat disappointing, and therefore we need additional studies of alternative surgical and non-surgical treatments.
Supplementary Material
Funding/Support:
Supported by National Eye Institute of National Institutes of Health, Department of Health and Human Services EY011751, EY023198, EY018810 and EY024333. The funding organization had no role in the design or conduct of this research.
Appendix
*Writing Committee: Sean P. Donahue, MD, PhD1; Danielle L. Chandler, MSPH2; Rui Wu, MS2; Justin D. Marsh, MD3; Christine Law, MD4; Raymond G. Areaux Jr., MD5; Fatema F. Ghasia, MD6; Zhuokai Li, PhD2; Raymond T. Kraker, MSPH2; Susan A. Cotter, OD, MS7; Jonathan M. Holmes, BM, BCh8; On behalf of the Pediatric Eye Disease Investigator Group
1Vanderbilt University Medical Center, Nashville, TN
2Jaeb Center for Health Research, Tampa, FL
3Eye Physicians of Central Florida, Maitland, FL
4Queen’s University, Kingston, Ontario
5Minnesota Lions Children's Eye Clinic, Minneapolis, MN
6Cole Eye Institute, Cleveland, OH
7Southern California College of Optometry at Marshall B. Ketchum University, Fullerton, CA
8University of Arizona, Tucson, AZ
Participating members of the Pediatric Eye Disease Investigator Group can be found in the collaborators document.
Footnotes
Conflict of Interest: No conflicting relationships exist for any authors.
- Association of Research in Vision and Ophthalmology Annual Meeting, Denver, Colorado, May 3, 2022. (Oral Presentation)
- American Association for Pediatric Ophthalmology and Strabismus Annual Meeting, New York City, New York, April 1, 2023. (Oral Presentation)
References:
- 1.Govindan M, Mohney BG, Diehl NN, Burke JP. Incidence and types of childhood exotropia: A population-based study. Ophthalmology. Jan 2005;112(1):104–108. [DOI] [PubMed] [Google Scholar]
- 2.Von Noorden GK, Campos EC. Exodeviations. In: Lampert R, Cox K, Burke D, eds. Binocular Vision and Ocular Motility: Theory and Management of Strabismus. 6th ed. Mosby; 2002:356–376. [Google Scholar]
- 3.Wright KW. Exotropia. In: Wright KW, ed. Pediatric Ophthalmology and Strabismus. Mosby-Year Book, Inc.; 1995:195–202. [Google Scholar]
- 4.Mitchell PR, Parks MM. Concomitant Exodeviations. In: Tasman WS, ed. Duane's Clinical Ophthalmology. Lippincott Williams & Wilkins; 2000:1–17:chap 13. [Google Scholar]
- 5.Pediatric Eye Disease Investigator Group. A randomized trial comparing bilateral lateral rectus recession versus unilateral recess and resect for basic-type intermittent exotropia. Ophthalmology. 2019;126(2):305–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kushner BJ. Selective surgery for intermittent exotropia based on distance/near differences. Arch Ophthalmol. 1998;116:324–8. [DOI] [PubMed] [Google Scholar]
- 7.Somer D, Demirci S, Cinar FG, Duman S. Accommodative ability in exotropia: predictive value of surgical success. J AAPOS. Oct 2007;11(5):460–4. doi: 10.1016/j.jaapos.2007.01.123 [DOI] [PubMed] [Google Scholar]
- 8.Zhang M, Lu S, Liu H, Yuan N. Comparison of surgical outcomes of intermittent exotropia with different surgery. Chin J Pract Ophthalmol 2011;29(4):396–398. doi: 10.3760/cma.j.issn.1006-4443.2011.04.031 [DOI] [Google Scholar]
- 9.Pineles SL, Ela-Dalman N, Zvansky AG, Yu F, Rosenbaum AL. Long-term results of the surgical management of intermittent exotropia. J AAPOS. Aug 2010;14(4):298–304. [DOI] [PubMed] [Google Scholar]
- 10.Holmes JM, Hatt SR, Leske DA. Is intermittent exotropia a curable condition? Eye (Lond). 2015;29(2):171–6. doi:0.1038/eye.2014.268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.ClinicalTrials.gov. Bilateral Lateral Rectus Recession Versus Unilateral Recess-Resect for Intermittent Exotropia (IXT1). ClinicalTrials.govidentifierNCT01032603. Updated 11-5-2021. Accessed 1-24-2022, https://clinicaltrials.gov/ct2/show/NCT01032603
- 12.Repka MX, Chandler DL, Holmes JM, et al. The Relationship of Age and Other Baseline Factors to Outcome of Initial Surgery for Intermittent Exotropia. Am J Ophthalmol. Dec 17 2020;212:153–161. doi: 10.1016/j.ajo.2019.12.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mohney BG, Holmes JM. An office-based scale for assessing control in intermittent exotropia. Strabismus. Sep 2006;14(3):147–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hatt SR, Mohney BG, Leske DA, Holmes JM. Variability of control in intermittent exotropia. Ophthalmology. Feb 2008;115(2):371–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Holmes JM, Liebermann L, Hatt SR, Smith SJ, Leske DA. Quantifying diplopia with a questionnaire. Ophthalmology. Jul 2013;120(7):1492–6. doi: 10.1016/j.ophtha.2012.12.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Statist Soc B. 1995;57(1):289–300. [Google Scholar]
- 17.Benjamini Y, Hochberg Y. On the Adaptive Control of the False Discovery Rate in Multiple Testing With Independent Statistics. J Educ Behav Stat. 2000;25(1):60–83. doi: 10.3102/10769986025001060 [DOI] [Google Scholar]
- 18.Lee SY, Hyun Kim J, Thacker NM. Augmented bilateral lateral rectus recessions in basic intermittent exotropia. J AAPOS. Jun 2007;11(3):266–8. doi: 10.1016/j.jaapos.2007.02.014 [DOI] [PubMed] [Google Scholar]
- 19.Pediatric Eye Disease Investigator Group. A randomized trial evaluating short-term effectiveness of overminus lenses in children 3 to 6 years of age with intermittent exotropia. Ophthalmology. Aug 6 2016;123(10):2127–2136. doi: 10.1016/j.ophtha.2016.06.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen AM, Erzurum SA, Chandler DL, et al. Overminus lens therapy for children 3 to 10 years of age with intermittent exotropia: A randomized clinical trial. JAMA Ophthalmol. 2021;139(4):464–476. doi: 10.1001/jamaophthalmol.2021.0082 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.