Abstract
Aims:
To measure the independent consequences of community-level armed conflict beatings on alcohol use disorders (AUD) among males in Nepal during and after the 2000–2006 conflict.
Design:
A population-representative panel study from Nepal, with precise measures of community-level violent events and subsequent individual-level AUD in males. Females were not included because of low AUD prevalence.
Setting:
Chitwan, Nepal.
Participants:
4,876 males from 151 neighborhoods, systematically selected and representative of Western Chitwan. All residents aged 15–59 were eligible (response rate 93%).
Measurements:
Measures of beatings in the community during the conflict (2000–2006), including the date and distance away, were gathered through neighborhood reports, geo-location, and official resources, then linked to respondents’ life histories of AUD (collected in 2016–2018) using the Nepal-specific Composite International Diagnostic Interview with life history calendar. Beatings nearby predict the subsequent onset of AUD during and after the armed conflict. Data were analyzed in 2021–2022.
Findings:
Cohort-specific, discrete-time models revealed that within the youngest cohort (born 1992–2001), those living in neighborhoods where armed conflict beatings occurred were more likely to develop AUD compared with those in other neighborhoods (odds ratio=1.66; 95% confidence interval=1.02–2.71). In this cohort, a multilevel matching analysis designed to simulate a randomized trial showed the post-conflict incidence of AUD for those living in neighborhoods with any armed conflict beatings was 9.5% compared with 5.3% in the matched sample with no beatings.
Conclusions:
Among children living in Chitwan, Nepal during the 2000–2006 armed conflict, living in a neighborhood where armed conflict beatings occurred is associated with increased odds of developing subsequent alcohol use disorder. This association was independent of personal exposure to beatings and other mental disorders.
Keywords: armed conflict, alcohol use, alcohol use disorder (AUD), low-income setting, Nepal
INTRODUCTION
Rarely do we have an opportunity to estimate the independent consequences of living in a community with high levels of violence for an individual’s subsequent transition to the onset of alcohol use disorders (hereafter onset of AUD). There is strong evidence that links individual-level experiences of organized violence to the onset of AUD. In post-conflict areas in Northern Uganda, up to half of the men met the criteria for a current AUD (1). A report from the global World Mental Health survey initiative (N=65,165) showed that 13% of those who have had experiences with organized violence/war met criteria for lifetime AUD compared to 4% among those without this experience (2). But also, in non-conflict contexts there is a clear association between exposure to physical violence and problematic alcohol use, which is more frequently reported among women (3). Although the impact of personal exposure to violence appears to increase the risk of problematic alcohol consumption (4), less is known about whether living in a community experiencing violence has similar adverse effects. The Nepalese context, which experienced six years of medium-intensity armed conflict and related exposure to neighborhood violence between 2000–2006 (5), provides a valuable opportunity to address this question. If community exposure to violence (independent of individual-level victimization) leads to increased risk of the onset of AUD, this would support the hypothesis that interventions to reduce community-level violence may improve health outcomes.
Understanding how exposure to violence affects the extent to which individuals experience the onset of AUD in this setting will provide basic but essential health data that can guide governments and clinicians to proactively plan sustainable healthcare frameworks. It will also help address several limitations regarding the understanding of how community (and not personal) exposure to violence is associated with subsequent onset of AUD. Prior studies have typically combined personal experience and/or witnessing violence in examining the association with the onset of AUD (6), or investigated associations between dysfunctional proximal social networks (7) or social disadvantage (8) on the development of alcohol-related outcomes. Another limitation of prior research is the scarcity of longitudinal designs. Those studies that used such an approach limited their sample to younger respondents (9) and not the full age range of community-dwelling individuals.
It is also rare to have measures of AUD from a post-conflict setting that span a broad age-range to inform our understanding of how exposure to community violence may shape the risk of AUD differently depending on the age of that exposure to community violence. However, this is an important question. As data resources increase for the study of the post-armed conflict trajectory of mental health, there is recent evidence that childhood exposure to armed conflict can have stronger long-term consequences than adult exposure (10,11). This is important both for understanding the mechanisms producing this association and for designing effective interventions to minimize these adverse consequences.
The current study examines the role of living in a community characterized by violence and the subsequent onset of AUD. To address the limitations of prior studies, we use community-level data gathered during an armed conflict on exposure to neighborhood beatings in the Chitwan Valley Family Study (CVFS) in Nepal, linked directly to the age of onset of AUD. Building upon previous work documenting the processes leading to AUD in Nepal (12) and the association between neighborhood violence and depression in Nepal (11), this study is new in documenting the associations between community violence and AUD across cohorts who experienced the violence at different ages. More specifically, we aim to (a) estimate the onset of AUD as a function of living in violent neighborhoods; and (b) examine birth cohort differences in the association between neighborhood violence and AUD.
METHODS
Data sources and respondents
The CVFS—launched in 1995 with a representative sample of Western Chitwan, Nepal—is a rigorous multiple cohort panel study with low attrition (13). At launch, 151 similar-sized neighborhoods were selected with equal probability, using random selection within geographic strata. All individuals in the neighborhoods were included in the CVFS. All household members are followed and become eligible for interviews at age 15, and the sample is refreshed periodically to represent in-migrants. A key feature of the CVFS for the analyses reported here is that it was established before the armed conflict began, it followed both neighborhoods and individuals throughout the armed conflict with high success, and it measured both the timing and location of violent events as they happened during the armed conflict (2000–2006) (5). One decade after the armed conflict ended (2016–2018), CVFS added one of the most rigorous measures of lifetime history of AUD and other mental disorders, including timing, ever conducted in settings like Nepal (14,15). The specially designed CVFS mixed-method event history calendars provide the timing of AUD onset relative to other events (14,16–18), allowing us to estimate the association between violent events near the neighborhood during the armed conflict and subsequent onset of AUD, both during and after the armed conflict.
Another key feature of the CVFS is that it features the application of state-of-the-art survey methods for panel studies to the extremely cooperative study population, generating exceptionally low levels of item missing data, high response rates, and low levels of attrition (5). Data in this study include observational measures of violent events and neighborhood characteristics during the armed conflict (2000–2006) and clinically validates survey measures of lifetime reports of AUD onset gathered in 2016–2018, with no item missing data for key measures. Due to the low numbers of females experiencing lifetime AUD in this setting (i.e., only 31 female respondents (12)), we focus on males aged 15–59 (n=4,876, response rate 93%). Further details about the CVFS sample and methods are available elsewhere (13,14).
All procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975 (revised in 2008). All procedures involving human subjects were approved by the University of Michigan Health Sciences and Behavioral Sciences Institutional Review Board (HUM00104171); they were also approved by the Nepal Health Research Council (Reg. No. 323/2015). Written informed consent was obtained from all subjects.
Data availability
The data come from the CVFS, which are archived at the Inter-university Consortium for Political and Social Research (ICPSR) at https://doi.org/10.3886/ICPSR04538.v20. Data are available to the scientific community following ICPSR protocols for restricted-use data.
Outcome measure
Lifetime onset of alcohol use disorder (AUD)
The onset of AUD was measured retrospectively using the Nepal-specific, life history calendar enhanced, version of the World Mental Health–Composite International Diagnostic Interview (CIDI), 3rd version (14,19). For lifetime onset of AUD, the instrument measures whether the respondent met diagnostic criteria for DSM-IV lifetime alcohol abuse or alcohol dependence, as well as the age at which respondents first met diagnostic criteria. Abuse and dependence were combined into AUD. The CIDI was paired with a life history calendar that used existing measures of individual and community events to improve recall of the timing of the onset of the outcomes (14). For the hazards of our outcome measure, all person-years from age 15 onward, including person-years before the beginning of the armed conflict (2000) for respondents from the oldest cohorts.1 Note that exposure to neighborhood beatings, personal beatings, or other mental disorders in a specific year only predict the onset of AUD in the subsequent year for all persons analyzed.
Because we investigate the onset of AUD among respondents who already consumed alcohol, we assessed the first use of alcohol using responses to: “How old were you the very first time you ever drank an alcoholic beverage?”. The definition of alcoholic beverages included local alcoholic beverages (jad and rakshy), beer, wine, and hard liquors such as vodka, gin, or whiskey. This indicator was coded 0 for “never” and 1 if the respondent reported an age of onset. This question measuring first use is a standard question used in multiple studies and settings (20,21). We also test models of the onset of AUD among all respondents (see eTable 2).
Neighborhood-level exposure measure
Neighborhood exposure to beatings
The CVFS collected neighborhood-level measures of violent events from 2000–2006. We defined neighborhood exposure to beatings within the context of the armed conflict as violent acts of taking an individual or a group of individuals and physically hitting, slamming, binding, or thrashing repeatedly using hand, foot, stick, hard wood, or weapons. Each event was measured using Global Positioning System locations (which allowed us to document the locations of violent events within 30 m), and each event between 2000–2006 was measured through a combination of sources: the South Asia Terrorism Portal, district-level archival records from government security forces, human rights organizations, courts, and other news sources and verified through focus groups with community members, as well as direct observation (5). We also collected data on the timings of events, allowing us to gain accurate insight into both the locations and timing of the violent events. We used detailed measures of the timing of events to create time-varying covariates for 0 vs. 1 or more beatings within 1 km from the respondent’s neighborhood in each year throughout the armed conflict.
Neighborhood-level characteristics
Decades of prior research using the CVFS demonstrate that other neighborhood characteristics have independent consequences for important individual outcomes, including marriage timing, childbearing, and migration (22–25). Because these experiences are also potential predictors of mental health and AUD (26–28), we also control for the two neighborhood characteristics most strongly associated with these outcomes, schools nearby (schools within a 5-minute walk) and health services nearby (health services within a 5-minute walk).
Individual-level exposure measures
Personal exposure to beatings
We also assessed whether respondents personally experienced a beating using the CIDI Posttraumatic Stress Disorder module (14). Respondents were asked whether they had ever been beaten by anyone. We created a time-varying dichotomous measure of whether the respondent was ever personally beaten (= 1).
Lifetime mental disorders
Lifetime mental disorders were retrospectively measured using the Nepal-specific, life history calendar enhanced, version of the World Mental Health–Composite International Diagnostic Interview (CIDI), 3rd version (14,19), a fully structured diagnostic interview that evaluates lifetime and 12-month DSM-IV mental disorders (29). Respondents who met the criteria for a lifetime mental disorder (other than AUD) prior to the onset of AUD (i.e., major depressive disorder, bipolar disorder, panic disorder, generalized anxiety disorder, post-traumatic stress disorder, and intermittent explosive disorder) were classified as having ‘any other lifetime mental disorder’ (coded 0 vs. 1 for those who met these criteria).
Socio-demographic characteristics
We collected age (as a continuous measure) and birth cohort. Birth cohort is categorized into four groups consistent with prior CVFS studies of the substantial social and economic changes in Nepal, mental health, and AUD: 1957–1971, 1972–1981, 1982–1991, and 1992–2001 (11–13,28). Ethnicity is measured through a set of dichotomous variables: Brahmin/Chhetri, Hill Janajati, Newar, Terai Janajati, and Dalit. Educational attainment at the time of the interview was dichotomized into those who passed the School Leaving Certificate (SLC) vs. those who did not. The SLC is awarded to Nepali students upon successful completion of their secondary education (10th grade) and a standardized SLC exam, issued by the Ministry of Education, Science, and Technology. This measure was coded 0 vs. 1 for those who received an SLC.
Statistical analysis
We present four sets of findings and use two contrasting statistical methods to investigate the associations between neighborhood-level exposure to beatings nearby and the subsequent onset of AUD. First, in Table 1, we present descriptive statistics separately for the four different birth cohorts we investigate. All measures used in our analyses are included in these descriptive results.
Table 1:
Descriptive Sample Characteristics of Males in the Chitwan Valley Family Study by Birth Cohort
| Characteristic | Born 1992–2001, ages 5–14 in 2006 (N=1519; 31.2%) | Born 1982–1991, ages 15–24 in 2006 (N=1253; 25.7%) | Born 1972–1981, ages 25–34 in 2006 (N=1058; 21.7%) | Born 1957–1971, ages 35–49 in 2006 (N=1046; 21.5%) | ||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| N | % | N | % | N | % | N | % | |
|
| ||||||||
| Outcome measure | ||||||||
| Lifetime onset of alcohol use disorder (AUD) | ||||||||
| Lifetime alcohol abuse or alcohol dependence = 1 | 113 | 7.4% | 190 | 15.1% | 153 | 14.5% | 155 | 14.8% |
| Neighborhood-level exposure measure | ||||||||
| Neighborhood exposure to beatings | ||||||||
| Ever any beatings within 1 km = 1 | 264 | 17.4% | 326 | 26.0% | 264 | 25.0% | 255 | 26.5% |
| Neighborhood-level characteristics | ||||||||
| Schools nearby | ||||||||
| Schools within 5-minute walk (2006) = 1 | 826 | 54.4% | 682 | 54.4% | 609 | 57.6% | 629 | 60.1% |
| Health services nearby | ||||||||
| Health services within 5-minute walk (2006) = 1 | 735 | 48.4% | 667 | 53.2% | 546 | 51.6% | 558 | 53.4% |
| Individual-level exposure measures | ||||||||
| Personal exposure to beatings | ||||||||
| Ever personally beaten = 1 | 51 | 3.4% | 50 | 4.0% | 24 | 2.3% | 32 | 3.1% |
| Lifetime mental disorders (other than AUD prior to the onset of AUD) | ||||||||
| Any other lifetime mental disorder = 1 | 108 | 7.1% | 94 | 7.5% | 83 | 7.8% | 110 | 10.5% |
| Socio-demographic characteristics | ||||||||
| Ethnicity | ||||||||
| Brahmin-Chhetri | 602 | 39.6% | 547 | 43.7% | 476 | 45.0% | 494 | 47.2% |
| Hill Janajati | 308 | 20.3% | 260 | 20.8% | 219 | 20.7% | 181 | 17.3% |
| Dalit | 226 | 14.9% | 153 | 12.2% | 114 | 10.8% | 132 | 12.6% |
| Newar | 86 | 5.7% | 74 | 5.9% | 63 | 6.0% | 69 | 6.6% |
| Terai Janajati | 297 | 19.6% | 219 | 17.5% | 186 | 17.6% | 170 | 16.3% |
| Educational attainment | ||||||||
| School Leaving Certificate (SLC) = 1 | 815 | 53.7% | 609 | 48.6% | 330 | 31.2% | 234 | 22.4% |
Second, in Table 2, we present multilevel discrete-time hazard models (also called “survival analysis”) with person-years as the unit of analysis. Each person contributes years of exposure to the risk of transitioning to the onset of AUD from the time they become age 15 and have their first drink until the date of the interview measuring AUD (2016–2018), or the date that person first experiences AUD. This means individuals contribute different numbers of person-years. This discrete-time approach is not biased by multiple person-years per person, has many advantages relative to continuous-time hazard models, and is easily adjusted for the multilevel (neighborhood and individual) data we use (30,31). These multilevel, multivariable models are used to estimate the association between exposure to neighborhood beatings and the onset of AUD. Note that respondents with AUD before the armed conflict began were not removed from the analysis, but those who transitioned to the onset of AUD before the armed conflict were not exposed to the risk of AUD in response to beatings nearby the neighborhood.2 Per cohort, logistic regression models estimated associations of exposures to neighborhood beatings and AUD onset, with hazard coefficients presented as odds ratios (ORs) and 95% confidence intervals (95% CI), and adjustments for age, ethnicity, education, individual exposure to beatings, and lifetime mental disorders other than AUD. We used standard multilevel hazard modeling that adjusts for individuals clustered within neighborhoods (30). We also conducted sensitivity analyses to choose a distance threshold (1 km) to use for beatings nearby (results comparing this threshold to alternatives are presented in supplementary eTable 3).
Table 2:
Discrete-Time Hazard Models of the Transition to the Onset of AUD, Conditioned on Alcohol Consumption (Adjusted for Personal Exposure to Beatings, Other Lifetime Mental Disorders, and Other Covariates)
| Born 1992–2001 ages 5–14 in 2006 OR (95% CI) | Born 1982–1991 ages 15–24 in 2006 OR (95% CI) | Born 1972–1981 ages 25–34 in 2006 OR (95% CI) | Born 1957–1971 ages 35–49 in 2006 OR (95% CI) | |
|---|---|---|---|---|
|
| ||||
| Neighborhood-level exposure measure | ||||
| Neighborhood exposure to beatings | ||||
| Ever any beatings within 1 km = 1 | 1.66* | 0.90 | 1.34 | 0.99 |
| (REF: no beatings within 1 km) | (1.02–2.71) | (0.59–1.37) | (0.82–2.18) | (0.49–2.01) |
| Neighborhood-level characteristics | ||||
| Schools nearby | ||||
| Schools within 5-minute walk = 1 | 1.23 | 0.82 | 0.92 | 0.87 |
| (REF: no schools within 5-minute walk) | (0.83–1.82) | (0.61–1.10) | (0.65–1.29) | (0.63–1.22) |
| Health services nearby | ||||
| Health services within 5-minute walk = 1 | 0.79 | 1.39* | 0.87 | 1.44* |
| (REF: no health services within 5-minute walk) | (0.53–1.18) | (1.02–1.88) | (0.60–1.26) | (1.00–2.07) |
| Individual-level exposure measures | ||||
| Personal exposure to beatings | ||||
| Ever personally beaten = 1 | 3.21* | 2.85* | 5.34* | 1.30 |
| (REF: never personally beaten) | (1.65–6.24) | (1.69–4.79) | (2.74–10.42) | (0.60–2.79) |
| Lifetime mental disorders (other than AUD prior to AUD onset) | ||||
| Any other lifetime mental disorder = 1 | 2.57* | 2.23* | 1.76 | 2.16* |
| (REF: no lifetime mental disorder) | (1.37–4.83) | (1.35–3.68) | (0.88–3.50) | (1.25–3.73) |
| Socio-demographic characteristics | ||||
| Ethnicity (REF: Brahmin/Chhetri) | ||||
| Hill Janajati | 1.29 | 1.10 | 1.11 | 1.17 |
| (0.76–2.18) | (0.74–1.64) | (0.71–1.75) | (0.73–1.87) | |
| Dalit | 1.21 | 1.17 | 1.08 | 1.30 |
| (0.68–2.17) | (0.74–1.87) | (0.62–1.87) | (0.79–2.13) | |
| Newar | 0.52 | 0.95 | 0.81 | 0.91 |
| (0.15–1.74) | (0.49–1.88) | (0.38–1.75) | (0.45–1.84) | |
| Terai Janajati | 1.08 | 0.94 | 1.24 | 1.73* |
| (0.61–1.91) | (0.60–1.48) | (0.79–1.95) | (1.12–2.66) | |
| Educational attainment | ||||
| School Leaving Certificate (SLC) = 1 | 0.46* | 0.84 | 0.67 | 0.64 |
| (REF: no SLC) | (0.30–0.70) | (0.61–1.17) | (0.44–1.04) | (0.38–1.07) |
| Age | 18.65* | 1.96* | 1.35* | 1.26* |
| (7.40–47.02) | (1.56–2.45) | (1.16–1.56) | (1.15–1.38) | |
| Age Squared | 0.93* | 0.99* | 1.00* | 1.00* |
| (0.90–0.95) | (0.98–0.99) | (0.99–1.00) | (1.00–1.00) | |
|
| ||||
| Observations | 10,186 | 20,064 | 25,303 | 32,108 |
| LL | −541.7 | −1005 | −875.1 | −948.5 |
| Chi2 | 158.6 | 139.0 | 107.7 | 65.70 |
p<0.05
Third, we also used the results shown in Table 2 to estimate the annual predicted probability of transitioning to the onset of AUD in the observed years following the end of armed conflict (2006–2017) for the youngest cohort we studied. These annual predicted probabilities are displayed graphically in Figure 1.
Figure 1.
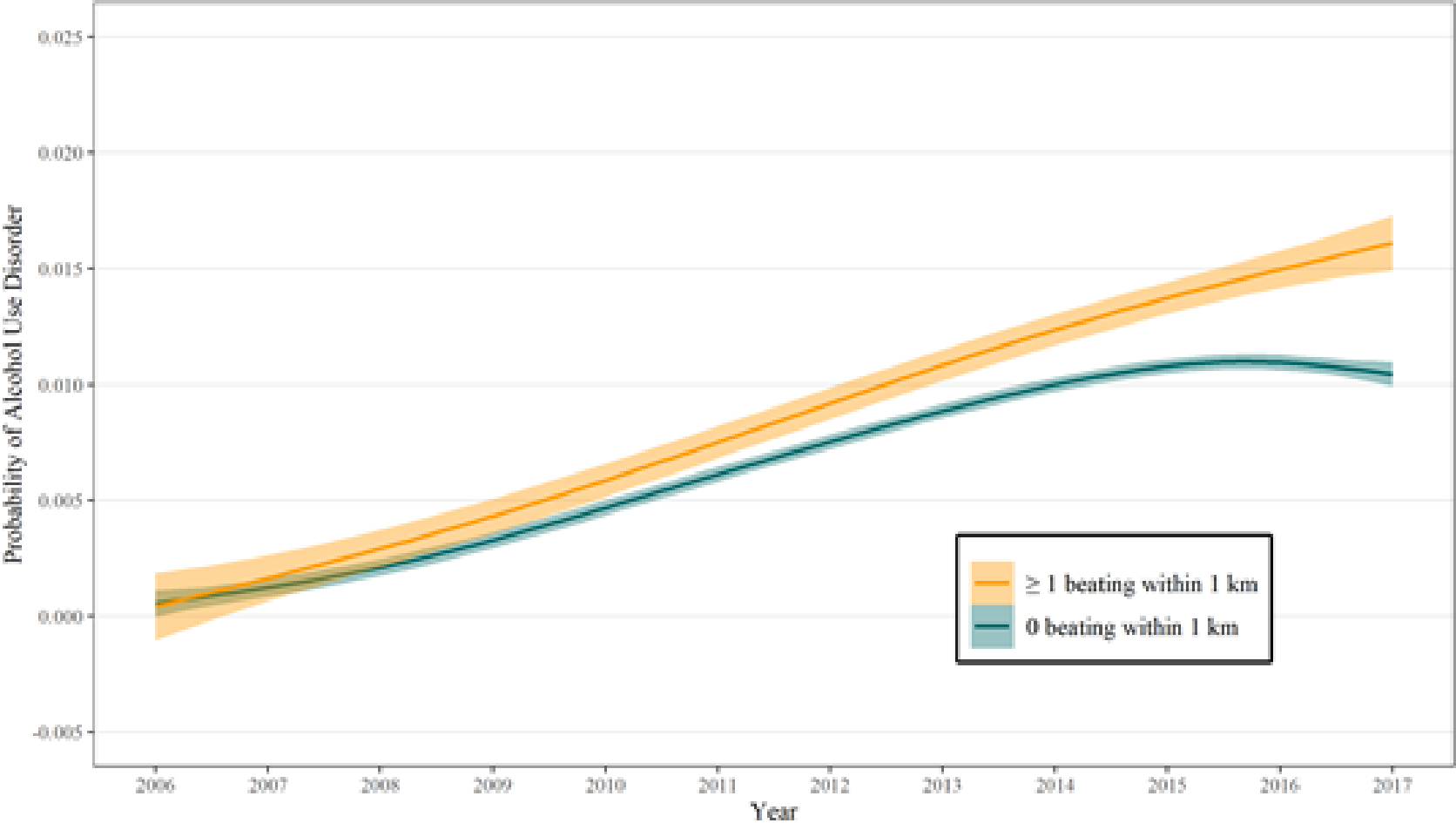
Estimated Time-Varying Probability of the Transition to the Onset of AUD 2006–2016 among those born 1992–2001 (ages 4–13 in 2006)
Finally, to contrast to our multilevel, multivariate hazard modelling approach, we used optimal multilevel matching methods to simulate an experimental design (32). For each cohort, the treatment-control matching process tested for the presence of a neighborhood-level treatment effect of 1 or more cumulative beatings within 1 km during the armed conflict (2000–2006), predicting the likelihood of transitioning to the onset of AUD in the decade following the armed conflict (2006–2016). This can be interpreted as testing the hypothesis of whether living in a neighborhood with any beating (as the exposure condition) results in a higher subsequent incidence of AUD compared to living in neighborhoods without the exposure variable (the control condition). Such methods are designed for observational data to approximate a randomized experiment (33). We started with cardinality matching, which simultaneously mean-balances and/or exact-matches on key covariates in their original form, without needing to estimate propensity scores or any other summary measure of the covariates (34). This resulted in 2 matched samples that were matched on male gender, ethnicity, and education. For ethnicity, we used a binary version of ethnicity (Brahmin-Chhetri and Newar [49.4% of the sample] or not) because of the key role this ethnic divide played in the Chitwan armed conflict and alcohol consumption (12). This within birth cohort approach to multilevel matching using the CVFS to study consequences of armed conflict has been used previously and is explained in detail elsewhere (33). Table 3 displays our results for all four birth cohorts with 95% confidence intervals. Unlike the hazard models, the matching analysis does not include exposure to AUD risk during the conflict period. Rather, the matching analyses focus on AUD during the decade directly following the armed conflict, just as in the predicted probabilities in Figure 1.
Table 3:
Multilevel Matching on Exposure to Neighborhood Violence (2000–2006) Predicting the Transition to the Onset of AUD (2006–2016), by Birth Cohort
| Born 1992–2001 ages 5–14 in 2006 Ever AUD | Born 1982–1991 ages 15–24 in 2006 Ever AUD | Born 1972–1981 ages 25–34 in 2006 Ever AUD | Born 1957–1971 ages 35–49 in 2006 Ever AUD | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No | Yes | No | Yes | No | Yes | No | Yes | |||||
|
| ||||||||||||
| Neighborhood exposure to beatings | ||||||||||||
| Ever any beatings within 1 km = 1 | ||||||||||||
| No | 94.7% | 5.3% | 86.2% | 13.8% | 86.0% | 14.0% | 84.5% | 15.5% | ||||
| 95% CI | (92.0–97.4) | (2.6–8.0) | (82.5–89.9) | (10.1–17.5) | (81.8–90.2) | (9.8–18.2) | (80.2–88.8) | (11.2–19.8) | ||||
| Yes | 90.5% | 9.5% | 84.7% | 15.3% | 86.0% | 14.0% | 84.5% | 15.5% | ||||
| 95% CI | (87.0–94.0) | (6.0–13.0) | (80.8–88.6) | (11.4–19.2) | (81.8–90.2) | (9.8–18.2) | (80.2–88.8) | (11.2–19.8) | ||||
| N in each arm of comparison | 264 | 326 | 264 | 277 | ||||||||
The analysis in the study was not pre-registered, therefore it should be considered exploratory.
RESULTS
Descriptive statistics
Table 1 presents the descriptive statistics for measures used in our analyses by birth cohort because we analyze each cohort separately. Birth cohort is categorized into four groups: those born between 1992–2001 (n=1,519; 31.2%), 1982–1991 (n=1,253; 25.7%), 1972–1981 (n=1,058; 21.7%), and 1957–1971 (n=1,046; 21.5%). Note that age is a time-varying covariate in our hazard models (Table 2), so we provide the age range in 2006 (end of the armed conflict) for each cohort. Rates of lifetime onset of AUD by cohort vary from 7.4% in the most recent birth cohort (born 1992–2001 and 15.1% in the next birth cohort (born 1982–1991). This pattern of increasing AUD prevalence with age (due to increased exposure to risk with age), along with increasing prevalence among the most recent birth cohorts as alcohol becomes more available in Nepal, has already been thoroughly documented using these same data sources (12).
Between 17.4% (born 1992–2001) and 26.5% (born 1957–1971) of respondents lived in a neighborhood where 1 or more beatings occurred within 1 km during the armed conflict and between 2.3% (born 1972–1981) and 4.0% (born 1982–1991) were exposed to personal beatings ever in their lives. Lifetime mental disorders occurred in 7.1% (born 1992–2001) and 10.5% (born 1957–1971) of the respondents (see Table 1).
Discrete-time hazard models of onset of AUD
A total of 4,876 male respondents contributed 224,357 person-years at risk of lifetime AUD before, during, and after the armed conflict. Note that the number of person-years contributed by each individual is different, depending upon when their first drink was reported and when they either experienced the onset of AUD or the date of the interview assessing AUD. In the discrete-time hazard models, three findings stand out. First, respondents with lifetime alcohol consumption who experienced beatings within 1 km had 66% increased odds of making the transition to the onset AUD (OR=1.66; 95% CI=1.02–2.71), but this increased risk was statistically significant only in the youngest cohort (i.e., those born between 1992–2001, see Table 2). Second, this association was independent of both the presence of either personal exposure to beatings or a mental disorder (other than AUD). Both of these factors are significant predictors of AUD across cohorts, with large effects in the youngest cohort (see Table 2). Note that the strength of the associations between neighborhood exposure to beatings and transition to the onset of AUD is similar before and after adjustment for personal exposure to beatings and other mental disorders (eTable 1). Third, respondents in the youngest cohort with an SLC had significantly lower odds of transitioning to the onset of AUD in models that controlled for personal beatings and other mental disorders (Table 2) and models that did not control for personal beatings and other mental disorders (eTable 1). In that cohort, having an SLC was associated with substantially lower odds of transition to the onset of AUD (OR=0.46, 95% CI=0.30–0.70). Finally, note that the significant association between exposure to beatings in the neighborhood and subsequent AUD is independent of all other covariates, including neighborhood resources, ethnicity, and age.
Figure 1 shows the time-varying odds of transitioning to the onset of AUD each year in the decade following the armed conflict for the youngest birth cohort only (those aged 5–14 in 2006 when the armed conflict ended). The top line (in yellow) shows that among those in this cohort, living in neighborhoods with 1 or more beatings nearby continues to increase the probability that they transition into AUD across their teenage years and young adulthood. By contrast, those who lived in neighborhoods with no beatings nearby increased in probability of transitioning to the onset of AUD through approximately 2014, and then the annual probability of transitioning to the onset of AUD leveled off. Note, these estimates come from the multivariable models presented in Table 2, controlling for age, age-squared, and all other covariates. The annual probability for those who experienced beatings nearby was consistently higher than the probability for those without that experience; this difference increased as respondents aged across the decade following the armed conflict.
Multivariable multilevel matching models of AUD by neighborhood beatings
Multivariable multilevel matching results were consistent with the discrete-time hazard models, finding an association between exposure to beatings nearby the neighborhood and subsequent AUD among respondents born in the most recent birth cohort (born 1992–2001). In this cohort, 264 respondents lived in neighborhoods with one or more beatings nearby. The proportion of respondents that made the transition to AUD was estimated at 9.5% among those exposed to community beatings and 5.3% among the matched unexposed sample (t=−1.86, p= 0.06). This finding was not present in any of the other birth cohorts (see Table 3).
DISCUSSION
This study is the first population-representative investigation of the effects of armed conflict neighborhood beatings on the subsequent development of AUD among male community-dwelling respondents. We used time-varying data on AUD as well as a validated structured psychiatric interview to investigate the extent to which living in neighborhoods with beatings are related to transitions into AUD. The most important finding is that living in a neighborhood with community beatings was associated with a statistically significant 66% increase in the odds of developing subsequent AUD among respondents who were born in the most recent birth cohort (i.e., the youngest at the time of the conflict). This result was independent of personal experience with beatings and other mental disorders. The result was consistent in analyses using an entirely different approach – multilevel matching to simulate an experimental design (33).
Our findings extend earlier work on the relationship between neighborhood disadvantage, violent neighborhoods, and AUD (35,36) by documenting that independent of personally experiencing beatings, living in a neighborhood where armed conflict beatings occurred nearby also increases subsequent AUD. In discussing the relationship between violence and AUD, many studies highlight the protective effect of education (37–40). Although we found that respondents with an SLC had lower odds of transitioning into AUD, our data highlight the independent association between community beating violence and the transition into AUD. In light of evidence that AUD itself contributes significantly to violent behaviors (41), identifying violent exposures that increase the risk of AUD may inform understanding of cross-generation and long-term perpetuation of violence.
Our data also extend knowledge in documenting that the association between neighborhood exposure to armed conflict violence and AUD is especially relevant to respondents who were young children at the time of the community-level exposure. This supports the hypothesis that childhood is a period during which individuals are particularly vulnerable to early life environmental exposures that confer risk for later problematic alcohol behaviors (42) and other mental disorders (11,43,44).
This study has several methodological strengths, including the large population sample nested within neighborhoods, longitudinal design, high response rate (93%), geo-located measures of violence exposure during the armed conflict, a follow-up period spanning a decade, and the statistical approach used to simulate an experimental design. At the same time, our results should be interpreted in light of four notable limitations. First, because of retrospective assessment, the onset of AUD is likely to be underreported and respondents’ reported ages of onset may be biased. Estimates of the age of onset tend to increase upon repeat assessment (i.e., as people age) (45). Currently, there is no gold standard in assessing alcohol-related outcomes; retrospective assessments are by definition biased in their accuracy of recalling, especially related to social desirability and memory biases. We attempted to reduce such bias using the CIDI which includes questions about both frequency of use and quantity of use. Such questions provide higher validity and reliability in estimates of alcohol use (46). Additionally, we estimated the timing of use using a calendar method (14) that provides more accurate estimates of the use of alcohol-related outcomes (47). Our measures of timing are also limited to annual precision to reduce the consequences of imprecise recall on our results and age-related recall bias is much less likely to be operating in the youngest cohort whose AUD onset would have happened quite recently (relative to assessment). In part, our confidence in these measures of relative timing comes from the success of the life history calendar approach to the measurement of the timing of symptom onset, as documented in a previously published large-scale randomized experiment (14,18). Second, we focus solely on neighborhood beatings. Beatings produce consequences for those living nearby because they were used explicitly to threaten people during the conflict, but other forms of violence (such as robbing, gunfights, or domestic violence) may also have important consequences (48). We do not control for all possible individual-level exposures that may increase transitions into AUD – an important limitation of the study reported here that deserves attention in future research. However, we do include a measure of personal experience of being beaten, which is a strong predictor of transitions into AUD. Third, we included only respondents up to 59 years, and thus we were not able to investigate associations for older individuals. This limits the generalizability of our findings. Finally, because rates of alcohol use are low among females in the population, making female experiences of AUD extremely rare (12), we only study AUD among males, leaving important questions about potential gender differences unaddressed.
The extent to which exposure to neighborhood violence confers risk for subsequent AUD has been unclear. In this large longitudinal study, we found that living in a neighborhood with community-level exposure to beatings was independently associated with increased subsequent rates of the onset of AUD, but only among those who were in their childhood or teenage years at the end of the exposure. Thus, our findings suggest that children exposed to neighborhood violence may be at increased risk of AUD onset, with health consequences lasting long after such violent conflicts have ended. This result is particularly important for understanding the potential long-term consequences of childhood exposure to armed conflict violence.
Supplementary Material
Acknowledgments:
The authors thank the survey staff of the Institute for Social and Environmental Research–Nepal for collecting the data reported here; the staff of the Survey Research Operations unit of the University of Michigan’s Survey Research Center for development and support of the technical systems that made the fieldwork in Nepal possible; the World Mental Health Consortium leadership and staff at Harvard University for their input into the design and all subsequent steps of collecting and analyzing the data reported here; and the respondents of the CVFS, whose generous contributions made this research possible. The authors alone remain responsible for any errors or omissions in this manuscript.
Primary Funding:
This work was supported by the National Institute of Mental Health (grant number R01MH110872) and the National Institute of Child Health and Human Development (NICHD) (grant number R01HD099135). The authors also gratefully acknowledge use of the services and facilities of the Population Studies Center at the University of Michigan, funded by an NICHD Center Grant (grant number P2CHD041028). These sponsors played no direct role in data collection, analysis, interpretation, or manuscript preparation.
Footnotes
Declaration of Interests: JWS is a member of the Leon Levy Foundation Neuroscience Advisory Board, the Scientific Advisory Board of Sensorium Therapeutics (with equity), and has received grant support from Biogen, Inc. He is PI of a collaborative study of the genetics of depression and bipolar disorder sponsored by 23andMe for which 23andMe provides analysis time as in-kind support but no payments. DJG is also the Director of the Institute for Social and Environmental Research in Nepal (ISER-N) that collected the data for the research reported here. His conflict of interest management plan is approved and monitored by the Regents of the University of Michigan.
The number of males in each birth cohort who had AUD before the armed conflict began is: born 1992–2001: n=6 (0.4%); born 1982–1991: n=4 (0.3%); born 1972–1981: n=27 (2.5%); born 1957–1971: n=80 (7.6%).
The number of males in each birth cohort who had AUD before the armed conflict began was, by cohort: born 1992–2001: n=6 (0.4%); born 1982–1991: n=4 (0.3%); born 1972–1981: n=27 (2.5%); born 1957–1971: n=80 (7.6%).
REFERENCES
- 1.Ertl V, Saile R, Neuner F, Catani C. Drinking to ease the burden: a cross-sectional study on trauma, alcohol abuse and psychopathology in a post-conflict context. BMC Psychiatry. 2016. Dec;16(1):202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Degenhardt L, Bharat C, Glantz MD, Bromet EJ, Alonso J, Bruffaerts R, et al. The associations between traumatic experiences and subsequent onset of a substance use disorder: Findings from the World Health Organization World Mental Health surveys. Drug Alcohol Depend. 2022. Nov 1;240:109574. [DOI] [PubMed] [Google Scholar]
- 3.Beardslee J, Schulenberg J, Simonton S. The Long-Term Associations Between Direct and Threatened Physical Violence in Adolescence and Symptoms of Substance Use Disorders During the Mid-30s. J Stud Alcohol Drugs. 2020. Mar;81(2):125–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kilpatrick DG, Ruggiero KJ, Acierno R, Saunders BE, Resnick HS, Best CL. Violence and risk of PTSD, major depression, substance abuse/dependence, and comorbidity: results from the National Survey of Adolescents. J Consult Clin Psychol. 2003. Aug;71(4):692–700. [DOI] [PubMed] [Google Scholar]
- 5.Axinn WG, Ghimire DJ, Williams NE. Collecting survey data during armed conflict. J Off Stat. 2012. Jun;28(2):153–71. [PMC free article] [PubMed] [Google Scholar]
- 6.Finkelhor D, Ormrod RK, Turner HA, Hamby SL. Measuring poly-victimization using the Juvenile Victimization Questionnaire. Child Abuse Negl. 2005. Nov;29(11):1297–312. [DOI] [PubMed] [Google Scholar]
- 7.Chartier KG, Karriker-Jaffe KJ, Cummings CR, Kendler KS. Review: Environmental influences on alcohol use: Informing research on the joint effects of genes and the environment in diverse U.S. populations: Environmental Influences on Alcohol Use. Am J Addict. 2017. Aug;26(5):446–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Orozco R, Benjet C, Ruiz Velasco-Acosta S, Moreno Altamirano L, Karriker-Jaffe KJ, Zemore S, et al. Area-level disadvantage and alcohol use disorder in northern Mexico. Drug Alcohol Depend. 2017. Jun;175:219–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Borges G, Benjet C, Orozco R, Medina-Mora ME. Traumatic life-events and alcohol and drug use disorders among Mexican adolescents: Bidirectional associations over 8 years. Drug Alcohol Depend. 2021. Nov;228:109051. [DOI] [PubMed] [Google Scholar]
- 10.Axinn WG, Bruffaerts R, Kessler TL, Frounfelker R, Aguilar-Gaxiola S, Alonso J, et al. Findings From the World Mental Health Surveys of Civil Violence Exposure and Its Association With Subsequent Onset and Persistence of Mental Disorders. JAMA Netw Open. 2023. Jun 20;6(6):e2318919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Benjet C, Axinn WG, Hermosilla S, Schulz P, Cole F, Sampson L, et al. Exposure to armed conflict in childhood vs older ages and subsequent onset of Major Depressive Disorder. JAMA Netw Open. 2020. Nov 13;3(11):e2019848–e2019848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cole F, Benjet C, Ghimire DJ, Axinn WG. Predictors of transitions across stages of alcohol use and disorders in an adult population with heterogeneous ethnic restrictions regarding drinking. Addiction. 2021. Apr 1;116(4):809–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Scott KM, Zhang Y, Chardoul S, Ghimire DJ, Smoller JW, Axinn WG. Resilience to mental disorders in a low-income, non-Westernized setting. Psychol Med. 2021;51(16):2825–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Axinn WG, Chardoul S, Gatny H, Ghimire DJ, Smoller JW, Zhang Y, et al. Using life history calendars to improve measurement of lifetime experience with mental disorders. Psychol Med. 2020;50(3):515–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ghimire DJ, Chardoul S, Kessler RC, Axinn WG, Adhikari BP. Modifying and validating the Composite International Diagnostic Interview (CIDI) for use in Nepal. Int J Methods Psychiatr Res. 2013;22(1):71–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Axinn WG, Pearce LD, Ghimire DJ. Innovations in life history calendar applications. Soc Sci Res. 1999;28(3):243–64. [Google Scholar]
- 17.Axinn WG, Pearce LD. Mixed method data collection strategies. New York, NY: Cambridge University Press; 2006. (New perspectives on anthropological and social demography). [Google Scholar]
- 18.Axinn WG, Chardoul S. Improving reports of health risks: Life history calendars and measurement of potentially traumatic experiences. Int J Methods Psychiatr Res. 2020. Sep 17;30(1):e1853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kessler RC, Üstün TB. The World Mental Health (WMH) survey initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). Int J Methods Psychiatr Res. 2004;13(2):93–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kalaydjian A, Swendsen J, Chiu WT, Dierker L, Degenhardt L, Glantz M, et al. Sociodemographic predictors of transitions across stages of alcohol use, disorders, and remission in the National Comorbidity Survey Replication. Compr Psychiatry. 2009. Jul 1;50(4):299–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee S, Guo WJ, Tsang A, He YL, Huang YQ, Zhang MY, et al. Associations of cohort and socio-demographic correlates with transitions from alcohol use to disorders and remission in metropolitan China. Addiction. 2009. Aug 1;104(8):1313–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Axinn WG, Yabiku ST. Social change, the social organization of families, and fertility limitation. Am J Sociol. 2001. Mar 1;106(5):1219–61. [Google Scholar]
- 23.Brauner-Otto SR, Axinn WG, Ghimire DJ. The spread of health services and fertility transition. Demography. 2007;44(4):747–70. [DOI] [PubMed] [Google Scholar]
- 24.Massey DS, Williams N, Axinn WG, Ghimire DJ. Community services and out-migration. Int Migr. 2010;48(3):1–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yabiku ST. Marriage timing in Nepal: Organizational effects and individual mechanisms. Soc Forces. 2004;83(2):559–86. [Google Scholar]
- 26.Zhang Y, Axinn WG. Marital experiences and depression in an arranged marriage setting. Am J Sociol. 2021. May 1;126(6):1439–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Axinn WG, Zhang Y, Ghimire DJ, Chardoul SA, Scott KM, Bruffaerts R. The association between marital transitions and the onset of major depressive disorder in a South Asian general population. J Affect Disord. 2020. Apr 1;266:165–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Axinn WG, Banchoff E, Cole F, Ghimire DJ, Smoller JW. The transition to parenthood, opportunity to drink, drinking, and alcohol use disorder. Drug Alcohol Depend. 2022. Dec 1;241:109697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. Fourth Edition. Washington, D.C: American Psychiatric Association; 1994. [Google Scholar]
- 30.Barber JS, Murphy SA, Axinn WG, Maples J. Discrete-time multilevel hazard analysis. Sociol Methodol. 2000;30(1):201–35. [Google Scholar]
- 31.Yamaguchi K Event history analysis. Vol. 28. Newbury Park, CA: Sage Publications; 1991. [Google Scholar]
- 32.Zubizarreta JR, Paredes RD, Rosenbaum PR. Matching for balance, pairing for heterogeneity in an observational study of the effectiveness of for-profit and not-for-profit high schools in Chile. Ann Appl Stat. 2014;8(1):204–31. [Google Scholar]
- 33.Niknam BA, Zubizarreta JR. Using cardinality matching to design balanced and representative samples for observational studies. JAMA. 2022. Jan 11;327(2):173–4. [DOI] [PubMed] [Google Scholar]
- 34.de los Angeles Resa M, Zubizarreta JR. Evaluation of subset matching methods and forms of covariate balance. Stat Med. 2016. Nov 30;35(27):4961–79. [DOI] [PubMed] [Google Scholar]
- 35.Martin-Storey A, Ruttle PL, Temcheff CE, Serbin LA, Stack DM, Ledingham JE, et al. Longitudinal and concurrent pathways to alcoholism: The importance of perception of neighborhood disorder. J Community Psychol. 2013. Mar;41(2):156–74. [Google Scholar]
- 36.Schiff M, Benbenishty R, McKay M, DeVoe E, Liu X, Hasin D. Exposure to Terrorism and Israeli Youths’ Psychological Distress and Alcohol Use: An Exploratory Study. Am J Addict. 2006. Jan;15(3):220–6. [DOI] [PubMed] [Google Scholar]
- 37.Lê F, Ahern J, Galea S. Neighborhood education inequality and drinking behavior. Drug Alcohol Depend. 2010. Nov 1;112(1–2):18–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mulia N, Karriker-Jaffe KJ. Interactive Influences of Neighborhood and Individual Socioeconomic Status on Alcohol Consumption and Problems. Alcohol Alcohol Oxf Oxfs. 2012. Mar;47(2):178–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Thor S, Karlsson P, Landberg J. Social Inequalities in Harmful Drinking and Alcohol-Related Problems Among Swedish Adolescents. Alcohol Alcohol Oxf Oxfs. 2019. Dec;54(5):532–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Norström T, Rossow I, Pape H. Social inequality in youth violence: The role of heavy episodic drinking. Drug Alcohol Rev. 2018. Feb;37(2):162–9. [DOI] [PubMed] [Google Scholar]
- 41.Friesen EL, Bailey J, Hyett S, Sedighi S, de Snoo ML, Williams K, et al. Hazardous alcohol use and alcohol-related harm in rural and remote communities: a scoping review. Lancet Public Health. 2022. Feb;7(2):e177–87. [DOI] [PubMed] [Google Scholar]
- 42.Guttmannova K, Bailey JA, Hill KG, Lee JO, Hawkins JD, Woods ML, et al. Sensitive Periods for Adolescent Alcohol Use Initiation: Predicting the Lifetime Occurrence and Chronicity of Alcohol Problems in Adulthood. J Stud Alcohol Drugs. 2011. Mar;72(2):221–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Scott KM, Lim CCW, Al-Hamzawi A, Alonso J. Intermittent explosive disorder. In: Scott KM, De Jonge P, Stein DJ, Kessler RC, editors. Mental disorders around the world: Facts and figures from the WHO World Mental Health Surveys. Cambridge: Cambridge Univeristy Press; 2018. p. 182–94. [Google Scholar]
- 44.Smith NDL, Cottler LB. The Epidemiology of Post-Traumatic Stress Disorder and Alcohol Use Disorder. Alcohol Res Curr Rev. 2018;39(2):113–20. [PMC free article] [PubMed] [Google Scholar]
- 45.Labouvie E, Bates ME, Pandina RJ. Age of first use: its reliability and predictive utility. J Stud Alcohol. 1997. Nov;58(6):638–43. [DOI] [PubMed] [Google Scholar]
- 46.McKenna H, Treanor C, O’Reilly D, Donnelly M. Evaluation of the psychometric properties of self-reported measures of alcohol consumption: a COSMIN systematic review. Subst Abuse Treat Prev Policy. 2018. Feb 2;13(1):6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bowling A Mode of questionnaire administration can have serious effects on data quality. J Public Health Oxf Engl. 2005. Sep;27(3):281–91. [DOI] [PubMed] [Google Scholar]
- 48.Wang X, Auchincloss AH, Barber S, Mayne SL, Griswold ME, Sims M, et al. Neighborhood social environment as risk factors to health behavior among African Americans: The Jackson Heart Study. Health Place. 2017. May;45:199–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data come from the CVFS, which are archived at the Inter-university Consortium for Political and Social Research (ICPSR) at https://doi.org/10.3886/ICPSR04538.v20. Data are available to the scientific community following ICPSR protocols for restricted-use data.


