Abstract
Background:
Surgical intervention is not typically used to treat symptoms after mild tibiofibular ligament injuries without ankle dislocation or subluxation.
Purpose:
To describe outcomes in patients arthroscopically treated for unique intra-articular lesions after sustaining syndesmosis injury of the ankle.
Study Design:
Case series; Level of evidence, 4.
Methods:
A total of 11 elite male rugby players with a mean age of 21.0 years (range, 17-28 years) were referred to our hospital for prolonged posterior ankle pain after a high ankle sprain during rugby football. The patients were examined using standing view radiography, computed tomography (CT) and magnetic resonance imaging (MRI) to determine the extent of ligament damage. Posterior ankle arthroscopy was performed to examine intra-articular lesions. The patients were evaluated using the American Orthopaedic Foot and Ankle Society (AOFAS) ankle/hindfoot rating scale and sports activity score of the Self-Administered Foot Evaluation Questionnaire (SAFE-Q).
Results:
The average reduced tibiofibular overlap on the standing mortise view was 1.2 mm (range, 0.5-2.0 mm) compared with the opposite ankles. Mason type 1 fracture was detected on CT in 6 patients, and ossification of the interosseous membrane was detected in 2 patients. A bone bruise in the posterior malleolus was observed on MRI in all but 1 patient. Intra-articular fragments located in the posterior ankle were observed and removed arthroscopically. Symptoms improved rapidly after arthroscopic treatment in all patients. All patients returned to rugby games at a median of 11 weeks postoperatively. The median AOFAS scores improved from 77 preoperatively to 100 postoperatively (P < .01), and the median SAFE-Q sports activity subscale score improved from 49.4 to 100 (P < .01).
Conclusion:
All unique intra-articular lesions that developed in rugby football players after syndesmosis injury were able to be treated arthroscopically. Patients returned to playing rugby football without syndesmosis reduction. Posterior ankle arthroscopy was effective in patients with residual symptoms after syndesmosis injury.
Keywords: ankle, cartilage, ligament, posterior ankle impingement syndrome, rugby, syndesmosis injury
Syndesmosis injuries of the ankle often occur in athletes participating in collision sports.6,20 The risk of high ankle sprain is 1.1 times higher in men's soccer and 2.42 times higher in men's football compared with the incidence in all the sports studied. 20 Unstable injuries accompanying the medial and/or lateral malleolar fracture(s) and/or the deltoid ligament rupture are managed operatively, although stable injuries are treated nonoperatively with a short-leg cast or brace as “ankle sprains.” 36
Ankle syndesmosis consists of the anterior, interosseous, and posterior talofibular ligaments. The posterior inferior tibiofibular ligament (PITFL) is thick and strongly inserted into the outer half of the posterior tibial malleolus, and injury to the PITFL often accompanies a fracture of the posterior tibial malleolus. Mason et al 19 classified posterior malleolar fractures into 4 types, reporting type 1 fractures as avulsion-type injuries. An ankle with type 1 fractures has syndesmosis disruption without exception and one-quarter of such injuries involve only the posterior syndesmosis.
The PITFL consists of superficial and deep layers, and the inferior border of the deep layer is attached to the posterior edge of the tibial plafond.13,18,28,33 The distal parts of the ligament fibers are inserted into the lower part of the posterior border of the tibial articular surface. 29 Detachment of the PITFL from the posterior edge of the tibial plafond causes avulsion fracture of the articular edge, which is a possible cause of posterior ankle impingement syndrome (PAIS).30,32,39
Ligament repair is generally necessary to treat residual symptoms after ligament injury. There is little information on how to treat persistent posterior ankle pain after a PITFL injury with mild instability. In this study, we report on whether arthroscopic excision of the lesion alone, without ligament repair, can improve symptoms in such cases.
Methods
Patients
Our institutional review board approved this study, and comprehensive agreement for the academic use of information on treatment progress or any other data acquired during treatments was obtained from the patients at the time of hospitalization. Between February 28, 2015, and December 31, 2021, 11 patients were referred to the Nara Prefecture General Medical Center for prolonged posterior ankle symptoms after a high ankle sprain that developed 6 to 26 weeks previously. All were elite male rugby players with a mean age of 21.0 years (range, 17-28 years). The patients experienced an ankle injury when tackled or involved in a ruck during a rugby game or practice.
Delayed healing of the syndesmosis injury or ankle-impingement syndrome triggered by the sprain was suspected. The patients were questioned regarding their ankle and hindfoot positions at injury, treatment before visiting our hospital by their team physicians or local doctors, history of ankle symptoms before the injury, playing position and category in rugby, and whether weightbearing worsened the symptoms. 20 Instability of the syndesmosis was examined using manual tests, such as the squeeze and cross-leg tests. Pain induction was also tested using forced plantar flexion and dorsiflexion of the ankle, which indicated impingement syndrome.
Patients were examined using standing ankle mortise view radiography (computed radiography [CT]); 320-row CT; and 3.0-T magnetic resonance imaging (MRI) using T1-weighted turbo spin-echo (TSE), T2-weighted TSE, and short tau inversion recovery (STIR) TSE sequence. Maximal tibiofibular overlap (TFO) on the standing ankle mortise view was measured from the medial border of the fibula to the lateral aspect of the anterior tibial tubercle. 31
Arthroscopic examination targeting the PAIS triggered by a high ankle sprain was performed at least 8 weeks after the injury. An additional 2 to 4 weeks of conservative treatment with an ankle brace was performed in 2 patients at the time of the first visit less than 8 weeks after the sprain. Posterior arthroscopy was performed in all patients, while anterior arthroscopy was additionally performed in 1 patient who had both anterior and posterior pain.
Arthroscopy
Posterior ankle arthroscopy was performed with the patient in the prone position, and the symptomatic ankle was elevated 10 cm with a small triangular support under the leg. The posterior approach with 2 portals as described by van Dijk et al 37 was used. A 2.7 mm–diameter 30° oblique arthroscope was inserted from the lateral portal and another instrument from the medial portal. An irrigation pump was used with an initial setting of 60 mm Hg pressure and 0.5 mL/s flow volume and adjusted according to the bleeding. If control of bleeding was difficult by the pump, 0.5 mg of adrenaline was added to 3000 mL of perfusate or 250 mm Hg air pressure was applied to the tourniquet attached to the proximal thigh. 30
A working space was created by shaving adipose and fibrous tissues just behind the posterior talar process, and the flexor hallucis longus tendon was identified. Inflamed synovium and fibrous scars at the posterior end of the ankle were removed and the arthroscope was introduced to the ankle joint space. The cartilage surface was probed carefully to examine any chondral or osteochondral lesions, and fragments in the joint space were removed using forceps or shaving instruments. In 1 patient who had anterior ankle symptoms, anterior arthroscopy was performed simultaneously after the prone-to-supine position change. A traction device was used during anterior arthroscopy.
Postoperative Treatment
A compression bandage was applied for 24 hours after the operation. The patients were allowed early range of motion immediately after surgery and were encouraged to walk without crutches the next day. They were allowed to jog 2 weeks after the operation and to subsequently increase their exercise intensity if they had no unbearable symptoms.
Clinical Evaluation and Follow-up
The mean follow-up period was 32 months (range, 7-72 months). The American Orthopaedic Foot and Ankle Society (AOFAS) ankle and hindfoot clinical rating scale and Self-Administered Foot Evaluation Questionnaire (SAFE-Q) were used to evaluate preoperative and postoperative ankle conditions. 22 All patients were asked about their postoperative activity level in rugby football along with the time required to resume training and return to participation in a game.
Histological Examination
The cartilaginous fragments removed using forceps in 5 patients were examined histologically with hematoxylin-eosin staining.
Statistical Analysis
Statistical analyses were performed using EZR (V.1.61; Saitama Medical Center, Jichi Medical University; based on R V.4.2.2). 14 The AOFAS and the SAFE-Q sports scores were assessed using the Wilcoxon signed-rank test. P < .05 was considered statistically significant in tests of statistical inference.
Results
Patient Characteristics
Details of the patients are summarized in Table 1. Seven patients had ankle injuries involving forced plantar flexion, 1 had eversion, and the other 3 could not remember the position of the ankle and hindfoot. The patients had been treated primarily conservatively for the acute phase of a “severe ankle sprain” by their team physicians or local physicians. Four patients treated with below-the-knee cast immobilization were inhibited from weightbearing for 3 weeks, and the other patients were treated with an ankle brace or taping.
Table 1.
Characteristics and Imaging Findings of Patients With Prolonged Symptoms After Syndesmosis Injury of the Ankle a
| Patient | Age, y | Playing Position/ Rugby Category | Ankle Position at Injury | Duration of Symptoms, wk | Reduced TFO, mm | Fracture or Ossification on CT | Bone Bruise in PM on MRI? | Detached Fragment(s)? |
|---|---|---|---|---|---|---|---|---|
| 1 | 21 | CTB/College elite | NA | 35 | 1.3 | Avulsion fracture | Yes | Yes |
| 2 | 21 | CTB/College elite | PF | 18 | 0.8 | Mason type 1 | Yes | Yes |
| 3 | 21 | WTB/College elite | NA | 15 | 1.5 | Mason type 1 (incomplete) | Yes | Yes |
| 4 | 28 | SH/National elite | NA | 18 | 0.5 | Avulsion fracture | Yes | Yes |
| 5 | 17 | HO/High school elite | PF | 19 | 1.9 | Avulsion fracture | Yes | Yes |
| 6 | 21 | No. 8/College elite | PF | 12 | 0.5 | Mason type 1 | Yes | Yes |
| 7 | 22 | No. 8/College elite | PF | 14 | 1.5 | None | No | Yes |
| 8 | 21 | SO/College elite | PF | 9 | 2.0 | Ossification of interosseous membrane | Yes | Yes |
| 9 | 18 | PR/College elite | PF | 8 | 0.6 | None | Yes | Yes |
| 10 | 20 | LO/College elite | Eversion | 14 | 1.3 | Ossification of interosseous membrane | Yes | Yes |
| 11 | 21 | PR/College elite | PF | 12 | 0.7 | None | Yes | Yes |
CT, computed tomography; CTB, center three-quarter back; HO, hooker; LO, lock; MRI, magnetic resonance imaging; NA, not available; PF, plantarflexion; PM, posterior malleolus; PR, prop; SH, scrum half; SO, standoff; TFO, tibiofibular overlap; WTB, wing three-quarter back.
During the first examination, the patients complained of posterior ankle pain during physical training and playing rugby with no disabilities in their daily activities. None of the patients had a history of ankle symptoms before the injury. The posterior ankle pain was induced by passive plantar flexion of the affected ankle in all patients, although active motion of the ankle was not restricted. Tenderness occurred posterior and lateral to the ankle in all patients, with more pain anterior and lateral to the ankle in 1 patient. The squeeze or cross-leg test, indicating instability of the syndesmosis, had negative results, and weightbearing did not worsen the symptoms. An additional conservative treatment performed in 2 patients less than 8 weeks after the sprain did not improve the symptoms.
Imaging
The reduction in the TFO distance compared with the opposite ankles no more than 2 mm (range, 0.5-2.0 mm). CT revealed Mason type 1 avulsion fractures in 6 ankles and ossification of the interosseous membrane in 2 ankles. The fracture lines did not involve the joint surface of the tibial plafond. Intramedullary high intensity of the posterior malleolus was detected on STIR TSE sequence of MRI in all but 1 of the ankles.
Arthroscopy
Arthroscopic examination was performed at a mean of 15.8 weeks after injury (range, 8-35 weeks). Fibrous, cartilaginous, or osteocartilaginous fragments intervening in the posterior and lateral parts of the ankle joint were detected in all patients using posterior ankle arthroscopy and were removed. These fragments were not free bodies and were retained in the posterior ankle space by soft fibrous stems (Figures 1D, 2C, and 3A). Cartilage defects at the intra-articular footprint of the PITFL were observed in 3 patients. In 1 patient, an inflamed synovium between the tibia and fibula, just behind the Bassett ligament, was observed and removed using anterior ankle arthroscopy.
Figure 1.
Examination results of a 28-year-old male rugby football player (patient 4). (A) Standing mortise radiographic view of the ankles. (B) Avulsion fracture of the posterior malleolus detected on axial view CT (arrow). (C) Lateral view STIR sequence MRI showing intramedullary edema of the posterior malleolus (large arrow) and lift of the posterior and distal periosteal membrane (small arrows). (D) A cartilaginous fragment (arrow) was observed in the posterior and lateral area of the ankle. CT, computed tomography; MRI, magnetic resonance imaging; STIR, short tau inversion recovery.
Figure 2.
Examination results of a 17-year-old male rugby player (patient 5). (A) Avulsion fracture (arrow) of the posterior malleolus and widening of the syndesmosis compared with contralateral ankle were detected on axial view CT. (B) Lateral view STIR sequence MRI showing intramedullary edema of the posterior malleolus (large arrow) and lifted posterior and distal periosteal membrane (small arrows). (C) Fragments (arrow) were impinged at the posterior and lateral area of the ankle. CT, computed tomography; MRI, magnetic resonance imaging; STIR, short tau inversion recovery.
Figure 3.

Examination results of a 21-year-old male rugby football player (patient 8). (A) Cartilaginous fragment observed at the posterior and lateral area of the ankle. (B) A chondral defect at the insertion of the PITFL is visible. (C) Histology of the fragment showing the structures of enthesis including collagen fibers, cartilage, and bone (hematoxylin and eosin staining; magnification, 40×). PITFL, posterior inferior tibiofibular ligament.
Histology
Histologically, these fragments were found to consist of articular hyaline cartilage, subchondral bone, and thick collagen bands attached to the fibrocartilage. No inflammatory or neoplastic changes were observed in the specimen (Figure 3B).
Return to Rugby
Patient symptoms improved promptly after the operation, and all 11 patients returned to their original rugby football activities. The median time required to restart athletic training was 4 weeks (range, 2-12 weeks), and the time to participate in rugby games was 11 weeks (range, 6-24 weeks) after the operation (Table 2). At the final follow-up, 10 patients had been playing rugby football at the elite level without any symptoms in the operated ankle. One patient was able to play rugby at an elite level with no postoperative problems but decided to play rugby on weekends at a local club and pursue a career outside of sports.
Table 2.
Return to Rugby and Clinical Outcomes a
| Patient | Return to Training, wk | Return to Games, wk | AOFAS Score | SAFE-Q Score | Follow-up, mo | ||
|---|---|---|---|---|---|---|---|
| Preop | Postop | Preop | Postop | ||||
| 1 | 4 | 7 | 77 | 100 | 89.4 | 88.3 | 67 |
| 2 | 12 | 24 | 77 | 100 | 53.6 | 100 | 60 |
| 3 | 4 | 8 | 77 | 100 | 74.4 | 100 | 58 |
| 4 | 3 | 12 | 77 | 100 | 23.9 | 100 | 53 |
| 5 | 2 | 6 | 77 | 100 | 43.3 | 100 | 30 |
| 6 | 3 | 13 | 72 | 100 | 36.1 | 100 | 24 |
| 7 | 4 | 10 | 72 | 100 | 50.0 | 100 | 18 |
| 8 | 4 | 12 | 72 | 100 | 24.4 | 100 | 16 |
| 9 | 4 | 11 | 78 | 100 | 49.4 | 100 | 13 |
| 10 | 5 | 12 | 88 | 100 | 55.0 | 100 | 8 |
| 11 | 4 | 8 | 77 | 100 | 37.8 | 100 | 7 |
AOFAS, American Orthopaedic Foot and Ankle Society; Postop, postoperative; Preop, preoperative; SAFE-Q, Self-Administered Foot Questionnaire.
Clinical Outcomes
The median AOFAS score improved from 77 (range, 72-88) to 100 (range, 100-100) postoperatively (P < .01), and the median SAFE-Q sports activity subscale score improved from 49.4 (range, 23.9-89.4) to 100 (range, 88.3-100) (P < .01). There were no cases of delayed healing, wound infection, or superficial nerve disturbances.
Case Presentations
Patient 4
A 28-year-old male rugby player sprained the left ankle when he was involved in a ruck during a seasonal match of the Japan Rugby Top League. The patient was examined by a team physician and treated conservatively for an ankle sprain. Physical training was resumed after a rest of 6 weeks, but the patient could not return to his original activity even 10 weeks after the injury because of posterior ankle pain while kicking a ball, and he was subsequently referred to our hospital. The reduction in the distance of the TFO on the standing radiographic view was less than 1 mm (Figure 1A); however, an avulsion fracture of the posterior malleolus was observed on CT (Figure 1B). MRI with STIR sequence showed bone marrow edema in the posterior malleolus, and the periosteum with the PITFL was lifted from the posterior malleolus (Figure 1C).
Posterior ankle arthroscopy was performed 4 months after injury. A small (3 × 3 × 1 mm) fragment of fibrocartilage-like tissue was observed with the PITFL in the posterior and lateral corner of the joint (Figure 1D). This mass was removed, but reduction and fixation of the syndesmosis were not performed. A compression bandage was applied to the ankle, and the patient was allowed to walk without crutches the day after surgery. The patient returned to physical training after 3 weeks and to practice matches 12 weeks after the operation. He was able to play in the official matches of the Japan Rugby Top League without any symptoms in the final follow-up.
Patient 5
A 17-year-old male high school rugby player sprained his left ankle with forced plantar flexion when he was involved in a ruck during a practice rugby match. The patient was treated conservatively for an ankle sprain by a local physician. The patient could not return to his original activity even 8 weeks after the injury and was referred to our hospital for posterior ankle pain during sports activities. Physical examination revealed mild swelling of the ankle and tenderness in both the anterior and posterior syndesmoses. An avulsion fracture of the posterior malleolus and widening of the syndesmosis compared with the contralateral ankle were detected on CT (Figure 2A). MRI with STIR TSE sequence showed bone marrow edema in the posterior malleolus, and the periosteum with the PITFL was lifted from the posterior malleolus (Figure 2B). Additional conservative treatments comprising rest, administration of nonsteroidal anti-inflammatory drugs, and external fixation with an ankle brace were applied for 4 weeks. However, the patient still complained of posterior ankle pain that was compatible with PAIS. Arthroscopic examination was performed 5 months after the injury.
A fibrocartilage-like fragment was observed at the intra-articular attachment of the PITFL (Figure 2C). The fragment and scarred tissues along the inferior margin of the PITFL were removed. Reduction and fixation of the syndesmosis were not performed. The patient was allowed to walk without crutches on the day after the operation. He returned to physical training 2 weeks later and rugby practice 4 weeks postoperatively. The patient is asymptomatic and has been playing on the Japanese college champion team without symptoms for 2 years after the injury.
Patient 8
A 21-year-old male college rugby player sprained his left ankle when he was involved in a ruck during a practice game. The patient was treated conservatively by a team physician with an ankle brace and rest. The patient was referred to our hospital 6 weeks after the injury because of prolonged posterior ankle pain.
The patient complained of pain in the posterior ankle during forced plantar flexion. An avulsion fracture was detected on routine radiography. The symptoms persisted, and arthroscopy was performed 9 weeks after the injury. Posterior ankle arthroscopy was performed, and an unstable small (8 × 4 × 3 mm) fragment was observed with a chondral defect at the intra-articular attachment of the PITFL to the tibia (Figure 3 A,B). Histologically, the fragment was shown to consist of articular hyaline cartilage, subchondral bone, and thick collagen bands attached to fibrocartilage (Figure 3C).
The patient was allowed to walk without crutches on the day after surgery. The patient complained of no symptoms and returned to rugby games 12 weeks after the operation.
Discussion
The patients in our series complained of posterior ankle pain after syndesmosis injury during rugby games or practice. Intra-articular lesions were observed on arthroscopy in all patients. There have been many reports of anterior intra-articular lesions after syndesmosis injury8-10,15,34,35 but only a few posterior lesions. Williams et al 38 previously reported rupture of the PITFL at the insertion of the tibia observed arthroscopically from the anterior portal, although they did not mention the symptoms caused by the lesion.
Hypertrophy of the intermalleolar ligament (IML) caused by repetitive compression injuries with forced plantar flexion is a possible cause of posterolateral soft tissue impingement.7-9 Lohrer and Arentz 17 reported a case of posterior meniscoid lesion of the ankle of a 25-year-old elite field hockey player that developed after pronounced plantar flexion of the foot. The meniscoid lesion consisted of scarred fibrous tissue that was successfully removed arthroscopically from the posterior portals.
The distal region of the PITFL is composed of a deep layer of ligaments that attaches to the posterior margin of the tibial plafond.16,18,24,33 There are various types of the PITFL, and the distal part is sometimes difficult to differentiate from the IML. 12 Ferkel 5 previously described the different types of PITFL and IML observed arthroscopically from the anterior portal, as well as variations in which the ligamentous fibers of the PITFL migrate into the articular cartilage of the ankle.
In our series, osteochondral fragments were detected arthroscopically. These fragments were not free bodies and were located in the insertion area of the PITFL. Histological examination of the 5 patients showed that the fragments contained cartilage bodies and collagen fibers. These findings are consistent with the findings of fragments from the ligament insertion. Arthroscopic excision of cartilage fragments resulted in a rapid improvement of symptoms, although the syndesmosis itself was not repaired or fixed. We strongly suspect that the PAIS developed from a fragment of the cartilage that was detached from the intra-articular insertion of the PITFL (Figure 4).
Figure 4.
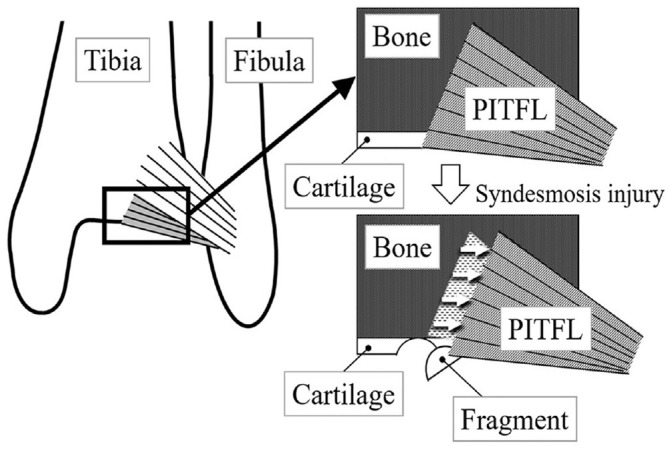
Mechanism of cartilage detachment from the tibia without becoming free at the posterior inferior margin of the tibia to which the PITFL attaches. PITFL, posterior inferior tibiofibular ligament.
Severe syndesmosis injuries with or without a posterior malleolar fracture usually occur in combination with other injuries, such as pilon fractures, spiral tibial shaft fractures, or bi- or trimalleolar ankle fractures.1,11,31 Isolated posterior malleolar fractures are uncommon and are often overlooked on plain radiographs.2,25,29
In our series of 11 patients, isolated avulsion fracture of the posterior malleolus was seen in 6 ankles, and ossification of the interosseous membrane in 2. Even in 2 ankles without a fracture or ossification of the interosseous membrane, MRI revealed periosteal and PITFL lifting from the posterior ankles. Acute repair of the disarticulation between the tibia and fibula could have prevented the impingement phenomenon caused by the cartilage fragments, but was not performed because the displacement was no more than 2 mm, and there were no medial or lateral fractures of the ankle joint or tears of the triangular ligament.21,23,26
Ogilvie-Harris et al 24 reported that resection of the torn interosseous ligament and cartilage lesions was successful in relieving prolonged symptoms after syndesmosis injury without restoring the ligament. The cartilage lesions were in the posterolateral corner of the tibial plafond. The cartilage lesions observed in our series were compatible with those in their report. However, the average duration between the injury and arthroscopic treatment was much earlier in our series (15.8 weeks) than that in their report (2 years). In our series, all patients complained of posterior ankle pain induced by forced plantar flexion. These symptoms were consistent with PAIS, which has gained wide clinical acceptance since van Dijk et al 37 introduced posterior ankle arthroscopy in 2000. Posterior arthroscopy allowed detailed observation of the posterior half of the ankle joint, including the medial and lateral gutter areas and the attachment of the PITFL to the posterior tibial rough surface with lower rate of iatrogenic chondral damage than the anterior approach. In addition, 10 of 11 patients showed bone bruise in the posterior tibial malleolus on fat suppression MRI scan and 6 patients had avulsion fracture of the posterior malleolus on CT. These objective findings suggested the presence of intra-articular lesions caused by syndesmosis injuries. There was no reason for us to delay performing a posterior ankle arthroscopy. We believe that the development of preoperative imaging techniques such as MRI and CT and the establishment of ankle arthroscopy have made it possible to treat these lesions in a minimally invasive manner, leading to early recovery of patients.
All patients injured their ankles when they were tackled or involved in a ruck during rugby football. Half remembered that their ankles were in plantar flexion with the hind feet in the eversion position at the time of injury. Players are more likely to experience syndesmosis injuries in collision sports such as rugby than in other sports,6,19,38 and most injuries are incurred by direct contact or by a posterior tackle.3,4 In a previous report, the mean number of days after radiologically detected syndesmosis injuries not treated with surgery in the English Premiership Rugby Union clubs was 30. 27
In our series of patients, it took 6 to 26 weeks after the ankle sprain for patients to be referred to our hospital. Signs indicating instability of the syndesmosis were not confirmed, but the patients did not resume rugby training due to residual symptoms compatible with PAIS. PAIS is usually caused by a bony element such as the os trigonum or a large posterior talar process, and ankle sprains sometimes cause fracture of the posterior process of the talus or loosen the fibrous union between the talus and the os trigonum. The os trigonum was present in 5 ankles, but MRI scans (STIR sequence) showed no intramedullary edema in the ossicles or the posterior part of the talus bone that abutted them, and arthroscopy did not reveal an impingement phenomenon caused by the os trigonum.
Limitations
The major limitations of this study were the small number of patients and the short-term follow-up periods (<2 years in 5 of 11 patients). However, the unique intra-articular lesions after syndesmosis injury of the ankle should be urgently brought to the attention of physicians treating athletes, especially those involved in collision sports. Although the arthroscopic debridement resulted in good medium- and short-term results, it is unclear how the lack of ligament repair will affect long-term results.
In our series of patients, information on the position of ankle and hindfoot at injury depended on patients’ memories. Video analysis at the time of injury might have made the hypothesis of injury mechanism more credible, but no video was obtained for this case group.
Conclusion
PAIS that developed in rugby players after syndesmosis injury could be treated arthroscopically. The patients returned to playing rugby football rapidly after arthroscopic excision of intra-articular lesions of the PITFL, without reduction of the syndesmosis. Posterior ankle arthroscopy was effective in patients with residual symptoms compatible with PAIS after syndesmosis injury.
Acknowledgments
The authors acknowledge the sports medicine staff of all the rugby football teams to which the study patients belonged.
Footnotes
Final revision submitted April 28, 2023; accepted May 19, 2023.
The authors have declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Nara Prefecture General Medical Center (No. 766).
References
- 1. Boggs LR. Isolated posterior malleolar fractures. Am J Emerg Med. 1986;4:334-336. [DOI] [PubMed] [Google Scholar]
- 2. Chang AL, Mandell JC. Syndesmotic ligaments of the ankle: anatomy, multimodality imaging, and patterns of injury. Curr Probl Diagn Radiol. 2020;49(6):452-459. [DOI] [PubMed] [Google Scholar]
- 3. Corte-Real N, Caetano J. Ankle and syndesmosis instability: consensus and controversies. EFFORT Open Rev. 2021;286(6):420-431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Delahunt E, Farrel G, Boylan A. Mechanism of acute ankle syndesmosis ligament injuries in professional male rugby union players: a systematic visual video analysis. Br J Sports Med. 2021;55(12):691-696. [DOI] [PubMed] [Google Scholar]
- 5. Ferkel RD. Diagnostic arthroscopic examination. In: Ferkel RD, ed. Arthroscopic Surgery: The Foot and Ankle. Lippincott; 1996:103-118. [Google Scholar]
- 6. Gerber JP, Williams GN, Scoville CR, Arciero RA, Taylor DC. Persistent disability associated with ankle sprains: a prospective examination of an athletic population. Foot Ankle Int. 1998;19(10):653-660. [DOI] [PubMed] [Google Scholar]
- 7. Giannini S, Buda R, Mosca M, Parma A, Di Caprio F. Posterior ankle impingement. Foot Ankle Int. 2013;34(3):459-465. [DOI] [PubMed] [Google Scholar]
- 8. Golanò P, Mariani PP, Rodríguez-Niedenfuhr M, Mariani PF, Ruano-Gil D. Arthroscopic anatomy of the posterior ankle ligaments. Arthroscopy. 2002;18(4):353-358. [DOI] [PubMed] [Google Scholar]
- 9. Golanó P, Vega J, Pérez-Carro L, Götzens V. Ankle anatomy for the arthroscopist. Part II: Role of the ankle ligaments in soft tissue impingement. Foot Ankle Clin. 2006;11(2):275-296. [DOI] [PubMed] [Google Scholar]
- 10. Han SH, Lee JW, Kim S, Suh JS, Choi YR. Chronic tibiotalar syndesmosis injury: the diagnosis efficacy of magnetic resonance and comparative analysis of operative treatment. Foot Ankle Int. 2007;28(3):336-342. [DOI] [PubMed] [Google Scholar]
- 11. Haraguchi N, Haruyama H, Toga H, Kato F. Pathoanatomy of posterior malleolar fractures of the ankle. J Bone Joint Surg Am. 2006;88(5):1085-1092. [DOI] [PubMed] [Google Scholar]
- 12. Hermans JJ, Beumer A, de Jong TAW, Kleinrensink JG. Anatomy of the distal tibiofibular syndesmosis in adults: a pictorial essay with a multimodality approach. J Anat. 2010;217(6):633-645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Jayatilaka MLT, Philpott MDG, Fisher A, Fisher L, Molloy A, Mason L. Anatomy of the insertion of the posterior inferior tibiofibular ligament and the posterior malleolar fracture. Foot Ankle Int. 2019;40(11):1319-1324. [DOI] [PubMed] [Google Scholar]
- 14. Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48(3):452-458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Koczy B, Pyda M, Stołtny T, et al. Affiliations expand arthroscopy for anterolateral soft tissue impingement of the ankle joint. Ortop Traumatol Rehabil. 2009;11(4):339-345. [PubMed] [Google Scholar]
- 16. Lilyquist M, Shaw A, Latz K, Bogener J, Wentz B. Cadaveric analysis of the distal tibiofibular syndesmosis. Foot Ankle Int. 2016;37(8):882-890. [DOI] [PubMed] [Google Scholar]
- 17. Lohrer H, Arentz S. Posterior approach for arthroscopic treatment of posterolateral impingement syndrome of the ankle in a top-level field hockey player. Arthroscopy. 2004;20(4):e15-e21. [DOI] [PubMed] [Google Scholar]
- 18. Martins CF, Miranda M, Cortegana IM, Sanchez MA, Harpe AG, Oliva XM. Posteroinferior tibiofibular ligament - a cadaveric study. Foot Ankle Surg. 2021;27(3):296-300. [DOI] [PubMed] [Google Scholar]
- 19. Mason LW, Marlow WJ, Widnall J, Molloy AP. Pathoanatomy and associated injuries of posterior malleolus fracture of the ankle. Foot Ankle Int. 2017;38(11):1229-1235. [DOI] [PubMed] [Google Scholar]
- 20. Mauntel TC, Wikstrom EA, Roos KG, Djoko A, Dompier TP, Kerr ZY. The epidemiology of high ankle sprains in National Collegiate Athletic Association sports. Am J Sports Med. 2017;45(9):2156-2163. [DOI] [PubMed] [Google Scholar]
- 21. Mulligan EP. Evaluation and management of ankle syndesmosis injuries. Phys Ther Sport. 2011;12;57-69. [DOI] [PubMed] [Google Scholar]
- 22. Niki H, Tatsunami S, Haraguchi N, et al. Validity and reliability of a self-administered foot evaluation questionnaire (SAFE-Q). J Orthop Sci. 2013;18(2):298-320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Odak S, Ahluwalia R, Unnikrishnan P, Hennessy M, Platt S. Management of posterior malleolar fractures: a systematic review. J Foot Ankle Surg. 2016;55:140-145. [DOI] [PubMed] [Google Scholar]
- 24. Ogilvie-Harris DJ, Reed SC, Hedman TP. Disruption of the ankle syndesmosis: biomechanical study of the ligamentous restraints. Arthroscopy. 1994;10(5):558-560. [DOI] [PubMed] [Google Scholar]
- 25. Özler T, Güven M, Önal A, Uluçay C, Beyzadeoğlu T, Altıntaş F. Missed isolated posterior malleolar fractures. Acta Orthop Traumatol Turc. 2014;48(3):249-252. [DOI] [PubMed] [Google Scholar]
- 26. Porter DA, Jaggers RR, Barnes AF, Rund AM. Optimal management of ankle syndesmosis injuries. Open Access J Sports Med. 2014:5(5):173-182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Sankey RA, Brooks JH, Kemp SP, Haddad FS. The epidemiology of ankle injuries in professional rugby union players. Am J Sports Med. 2008;36(12):2415-2424. [DOI] [PubMed] [Google Scholar]
- 28. Sarrafian K, Kelikian A. Syndesmology. In: Kelikian A, eds. Sarrafian’s Anatomy of the Foot and Ankle. 3rd ed. Lippincott; 2011:163-222. [Google Scholar]
- 29. Shah AS, Kadakia AR, Tan G, Karadsheh MS, Wolter TD, Sabb B. Radiographic evaluation of the normal distal tibiofibular syndesmosis. Foot Ankle Int. 2012;33(10):870-876. [DOI] [PubMed] [Google Scholar]
- 30. Shane AM, Reeves CL, Vazales R, Farley Z. Soft tissue impingement of the ankle. Pathophysiology, evaluation, and arthroscopic treatment. Clin Podiatr Med Surg. 2016;33:503-520. [DOI] [PubMed] [Google Scholar]
- 31. Smeeing DPJ, Houwert RM, Kruyt MC, Hietbrink F. The isolated posterior malleolar fracture and syndesmosis instability: a case report and review of the literature. Int J Surg Case Rep. 2017;41:360-365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Sugimoto K, Isomoto S, Samoto N, Matsui T, Tanaka Y. Arthroscopic treatment of posterior ankle impingement syndrome: mid-term clinical results and a learning curve. Arthrosc Sports Med Rehabil. 2021;3(4):e1077-e1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Tourné Y, Molinier F, Andrieu M, Porta J, Barbier G. Diagnosis and treatment of tibiofibular syndesmosis lesions. Orthop Traumatol Surg Res. 2019;105(8S):S275-S286. [DOI] [PubMed] [Google Scholar]
- 34. Turky M, Menon KV, Saeed K. Arthroscopic grading of injuries of the inferior tibiofibular syndesmosis. J Foot Ankle Surg. 2018;57:1125-1129. [DOI] [PubMed] [Google Scholar]
- 35. Van den Bekerom MPJ, Raven EEJ. The distal fascicle of the anterior inferior tibiofibular ligament as a cause of tibiotalar impingement syndrome: a current concepts review. Knee Surg Sports Traumatol Arthrosc. 2007;15(4):465-471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. van Dijk CN, Scholten PE, Krips R. A 2-portal endoscopic approach for diagnosis and treatment of posterior ankle pathology. Arthroscopy. 2000;16(8):871-876. [DOI] [PubMed] [Google Scholar]
- 37. van Dijk CN, Longo UG, Loppini M, et al. Classification and diagnosis of acute isolated syndesmosis injuries: ESSKA-AFAS consensus and guidelines. Knee Surg Sports Traumatol Arthrosc. 2016;24(4):1200-1216. [DOI] [PubMed] [Google Scholar]
- 38. Williams GN, Jones MH, Amendola A. Syndesmotic ankle sprains in athletes. Am J Sports Med. 2007;35(7):1197-1207. [DOI] [PubMed] [Google Scholar]
- 39. Zwiers R, Wiegerinck JI, Murawski CD, Smyth NA, Kennedy JG, van Dijk CN. Surgical treatment for posterior ankle impingement. Arthroscopy. 2013;29(7):1263-1270. [DOI] [PubMed] [Google Scholar]




