Abstract
Background
We previously developed risk models predicting stroke, coronary heart disease (CHD), and cardiovascular disease (CVD) among Japanese people from the Suita Study. Yet, applying these models at the national level was challenging because some of the included risk factors differed from those collected in the Japanese governmental health check-ups, such as Tokutei-Kenshin. We, therefore, conducted this study to develop new risk models for stroke, CHD, and atherosclerotic CVD (ASCVD), based on data from the Suita Study. The new models used traditional cardiovascular risk factors similar to those in the Japanese governmental health check-ups.
Methods
We included 7,413 participants, aged 30–84 years, initially free from stroke and CHD. All participants received baseline health examinations, including a questionnaire assessing their lifestyle and medical history, medical examination, and blood and urine analysis. The risk factors of stroke, CHD, and ASCVD (cerebral infarction or CHD) were determined using the multivariable-adjusted Cox regression. The models’ performance was assessed using the C-statistics for discrimination and the Hosmer-Lemeshow for calibration. We also developed three simple scores (zero to 100) that could predict the 10-year incidence of stroke, CHD, and ASCVD.
Results
Within 110,428 person-years (median follow-up = 16.6 years), 410 stroke events, 288 CHD events, and 527 ASCVD events were diagnosed. Age, smoking, hypertension, and diabetes were associated with stroke, CHD, and ASCVD risk. Men and those with decreased high-density lipoproteins or increased low-density lipoproteins showed a higher risk of CHD and ASCVD. Urinary proteins were associated with an increased risk of stroke and ASCVD. The C-statistic values of the risk models were >0.750 and the p-values of goodness-of-fit were >0.30. The 10-year incidence of stroke, CVD, and ASCVD events was 3.8%, 3.5%, and 5.7% for scores 45–54, 10.3%, 11.8%, and 19.6% for scores 65–74, and 27.7%, 23.5%, and 60.5% for scores ≥85, respectively.
Conclusions
We developed new Suita risk models for stroke, CHD, and ASCVD using variables similar to those in the Japanese governmental health check-ups. We also developed new risk scores to predict incident stroke, CHD, and ASCVD within 10 years.
Supplementary information
The online version contains supplementary material available at https://doi.org/10.1265/ehpm.23-00099.
Keywords: Risk scores, Prediction models, Stroke, Coronary heart disease
1. Introduction
Cardiovascular disease (CVD), especially stroke and coronary heart disease (CHD), remains the leading cause of morbidity and mortality in Japan and globally [1]. Determining people at elevated risk of developing CVD is essential for risk prevention [2, 3].
In this context, we previously developed risk models predicting stroke [4], CHD [5], and CVD [6] using data from the Suita Study, a prospective cohort study representing the general population in urban Japan. Despite being used for health counseling in many Japanese health settings, applying the Suita risk models at the national level was challenging for two main reasons. First, some included risk factors, such as arrhythmia, cardiac murmurs, and chronic kidney disease (CKD), are not regularly assessed in the health check-ups conducted in local municipalities by the Japanese Government, such as Tokutei-Kenshin. In contrast, other risk factors, such as urinary proteins, are regularly assessed in these health check-ups but were not included in the Suita risk models [7], because CKD was used instead. Second, previous Suita risk models utilized different categorizations and scoring systems [4–6], making it difficult to compare them and inconvenient for practical application.
Hence, based on data from the Suita Study, we developed new risk models and scores for stroke, CHD, and atherosclerotic CVD (ASCVD) using risk factors similar to those that are regularly assessed in Japanese governmental health check-ups.
2. Methods
2.1. Participants
The Suita population (n = 8,360) included two cohorts randomly selected by sex and 10-year age category from the urban city of Suita (recruited between 1989 and 1998) and a volunteer group (recruited between 1992 and 2006). The first cohort included 12,200 participants (6,485 participants were eligible), the second cohort included 3,000 participants (1,329 participants were eligible), and the volunteer group included 546 participants. The baseline assessment was held at the National Cerebral Cardiovascular Centre (NCVC) in Suita. It included data collection about lifestyle, blood and urine sampling, clinical and fundus examinations, and electrocardiography (ECG). Participants were encouraged to return every two years for follow-up. In this study, we excluded participants who had a positive history of stroke or CHD (n = 367), lacked baseline data about weight, height, waist circumference (WC), smoking behavior, alcohol consumption, blood pressure (BP), blood glucose, low- or high-density lipoprotein-cholesterol (LDL-c or HDL-c), or urinary proteins (n = 131), or were lost to follow-up (n = 449). Eventually, 7,413 participants, aged 30–84 years, were included for analysis. All participants were followed up from the date of baseline assessment until the date of stroke or CHD event, death, leaving the study, or the end of follow-up (December 31, 2013), whichever came first.
2.2. Assessment of outcomes
The health status of participants was examined during the follow-up check-ups conducted every two years in addition to the annual follow-ups in the form of self-administered questionnaires sent by mail or telephone interviews. Besides, registered physicians, who were blind to participants’ baseline data, revised their medical records. Stroke was diagnosed per the US National Survey of Stroke criteria based on computed tomographic scans and magnetic resonance images [8]. CHD included myocardial infarctions, defined per the criteria of the World Health Organization Multinational MONItoring of Trends and Determinants in CArdiovascular Disease (WHO MONICA) Project [9], percutaneous coronary intervention, coronary artery bypass grafting, and sudden cardiac death within 24 hours. ASCVD included cerebral infarction and CHD.
2.3. Assessment of risk factors
Data about risk factors were collected during the baseline examination. Lifestyle factors, such as smoking and alcohol consumption, and clinical histories were self-reported. Well-trained nurses revised the health and medical records of participants. Weight and height were measured for body mass index (BMI) calculation (weight in Kg/height in m2). WC was measured in a standing position at the umbilical level to the nearest one cm without skin compression after instructing participants to breathe out. Participants wore light clothes for weight and WC assessment. BP was measured three times and the average of the last two measurements was used for analysis. Blood samples were collected and centrifuged before routine blood examinations, including blood glucose, LDL-c, HDL-c, and creatinine. Urine samples were also collected and analyzed. Besides, participants underwent a standard 12-lead ECG examination for three minutes. After revising the Tokutei-Kenshin questionnaire [7], previous Suita CVD risk models [4–6], and Japanese guidelines for obesity, hypertension, diabetes, and dyslipidemia [10–12], the following variables were included: sex, age (30–39, 40–44, 45–49, 50–54, 55–59, 60–64, 65–69, 70–74, and ≥75 years), BMI: (<18.5, 18.5–24.9, or ≥25 kg/m2), WC (<85 cm in men / <90 cm in women [normal] or ≥85 cm in men / ≥90 cm in women [high]), smoking (never, former, or current), alcohol consumption (never, former, or current), BP (<120/80 mmHg [optimal BP], 120–139/80–89 mmHg [high-normal or elevated BP], or ≥140/90 mmHg / receiving medications [hypertension]), blood glucose (fasting blood glucose (FBG) <100 mg/dL / HbA1c ≤5.5% [normal], FBG 100–125 mg/dL / HbA1c 5.6–6.4% [impaired], or FBG ≥126 mg/dL / HbA1c ≥6.5% / receiving medication [diabetes]), LDL-c (<100, 100–159 or ≥160 mg/dL), HDL-c (<40 or ≥40 mg/dL), and urinary proteins (− or ≥+1). In further analyses, we added variables that have been performed in the Japanese governmental health check-ups for high-risk individuals only. These variables included CKD, defined as an estimated glomerular filtration rate <60 mL/min/1.73 m2 (yes or no), hypertensive retinopathy diagnosed using the Keith–Wagener–Barker classification [13], and ECG findings per the Minnesota codes for atrioventricular conduction defect (6-codes), high-amplitude R (3-codes), ST-T abnormalities (4-codes and 5-codes), and atrial fibrillation or flutter (8-3-1 to 4) (yes or no, each).
2.4. Statistical analysis
First, we described the proportions of the baseline personal and clinical characteristics of participants by the outcome: no events, stroke, CHD, and ASCVD (Table 1). Then, we conducted age-and sex-adjusted Cox proportional hazard models to detect potential risk factors for stroke, CHD, and ASCVD. Among participants who developed both cerebral infarction and CHD, the follow-up in the ASCVD analysis was censored when the earlier event occurred. Factors that showed statistically significant associations in the age-and sex-adjusted models (p < 0.10) were included in multivariable-adjusted models, and variables that showed statistically significant associations in the later models (p < 0.05) were considered the final risk models (Table 2). Then, weights were assigned based on the β-coefficient of significant variables in the final risk model, and these weights were translated into risk scores ranging between zero and 100 (Table 3). We tested the final risk models in terms of discriminative ability using the C-statistics (Table 4) [14] and calibration using the Hosmer-Lemeshow statistics by comparing the observed and expected incident events by decile of risk (Fig. 1) [15]. We also calculated the 10-year incidence of stroke, CHD, and ASCVD by their risk scores (Table 5). The interaction of sex in the association between other potential risk factors and stroke, CHD, and ASCVD was examined as well (Supplementary Table 1). We repeated the analysis after adding the following variables one by one: CKD, hypertensive retinopathy, atrioventricular conduction defect, high-amplitude R, ST-T abnormalities, and atrial fibrillation or flutter (Supplementary Table 2). SAS version 9.4 software (SAS Institute Inc, Cary, NC) was used for statistical analysis.
Table 1.
Traditional cardiovascular disease risk factors at baseline
| Risk factors | No events | Stroke | Coronary heart disease | Atherosclerotic cardiovascular disease | |
| Number of participants | 6,715 | 410 | 288 | 527 | |
| Sex, % | Men | 45.6 | 54.9 | 67.0 | 63.2 |
| Women | 54.4 | 45.1 | 33.0 | 36.8 | |
| Age (years), % | 30–39 | 16.9 | 1.2 | 3.5 | 2.1 |
| 40–44 | 10.0 | 2.7 | 3.8 | 3.0 | |
| 45–49 | 10.0 | 5.1 | 6.3 | 5.3 | |
| 50–54 | 11.7 | 7.3 | 9.0 | 8.5 | |
| 55–59 | 12.0 | 12.2 | 11.8 | 11.8 | |
| 60–64 | 13.7 | 17.1 | 21.5 | 21.1 | |
| 65–69 | 9.6 | 19.0 | 16.3 | 18.0 | |
| 70–74 | 10.0 | 21.0 | 17.4 | 18.8 | |
| ≥75 | 6.1 | 14.4 | 10.4 | 11.4 | |
| Body mass index (kg/m2), % | <18.5 | 8.5 | 6.8 | 3.8 | 4.7 |
| 18.5–24.9 | 72.1 | 68.3 | 69.1 | 69.1 | |
| ≥25 | 19.4 | 24.9 | 27.1 | 26.2 | |
| Waist circumference (cm), % | Normal | 74.7 | 62.7 | 61.8 | 60.3 |
| High | 25.3 | 37.3 | 38.2 | 39.7 | |
| Smoking, % | Never | 55.0 | 46.6 | 38.5 | 40.4 |
| Former | 15.7 | 20.0 | 25.7 | 24.5 | |
| Current | 29.3 | 33.4 | 35.8 | 35.1 | |
| Alcohol drinking, % | Never | 45.5 | 42.9 | 47.2 | 44.4 |
| Former | 2.3 | 3.7 | 3.5 | 3.2 | |
| Current | 52.2 | 53.4 | 49.3 | 52.4 | |
| Blood pressure (mmHg), % | Optimal | 38.0 | 17.8 | 13.9 | 14.2 |
| High-normal | 32.7 | 27.8 | 29.2 | 28.1 | |
| Hypertension | 29.3 | 54.4 | 56.9 | 57.7 | |
| Blood glucose (mg/dL), % | Normal | 67.7 | 51.7 | 46.5 | 48.2 |
| Impaired | 27.5 | 36.8 | 41.3 | 38.9 | |
| Diabetes | 4.8 | 11.5 | 12.2 | 12.9 | |
| High-density lipoprotein-cholesterol (mg/dL), % | <40 | 13.4 | 18.0 | 27.1 | 24.3 |
| ≥40 | 86.6 | 82.0 | 72.9 | 75.7 | |
| Low-density lipoprotein-cholesterol (mg/dL), % | <100 | 20.2 | 17.1 | 10.8 | 14.6 |
| 100–159 | 62.8 | 63.9 | 57.6 | 60.0 | |
| ≥160 | 17.0 | 19.0 | 31.6 | 25.4 | |
| Urinary proteins, % | − | 82.5 | 72.2 | 77.4 | 75.3 |
| ≥+1 | 17.5 | 27.8 | 22.6 | 24.7 | |
Table 2.
Risk models of stroke, coronary heart disease, and atherosclerotic cardiovascular disease
| Risk factors | Stroke | Coronary heart disease |
Atherosclerotic
cardiovascular disease |
||||
|
| |||||||
| β1 | β2 | β1 | β2 | β1 | β2 | ||
| Sex | Men | 0.419* | 0.107 | 0.921* | 0.911* | 0.742* | 0.429* |
| Women | Ref | Ref | Ref | Ref | Ref | Ref | |
| Age (years) | 30–39 | Ref | Ref | Ref | Ref | Ref | Ref |
| 40–44 | 1.186* | 1.131* | 0.507* | 0.317 | 0.775* | 0.619* | |
| 45–49 | 1.842* | 1.773* | 1.025* | 0.779* | 1.344* | 1.151* | |
| 50–54 | 2.055* | 1.858* | 1.230* | 0.778* | 1.661* | 1.275* | |
| 55–59 | 2.630* | 2.424* | 1.583* | 1.016* | 2.052* | 1.625* | |
| 60–64 | 2.865* | 2.581* | 2.050* | 1.344* | 2.500* | 1.967* | |
| 65–69 | 3.418* | 3.143* | 2.259* | 1.533* | 2.803* | 2.263* | |
| 70–74 | 3.674* | 3.417* | 2.483* | 1.763* | 2.995* | 2.483* | |
| ≥75 | 4.050* | 3.768* | 2.761* | 2.002* | 3.238* | 2.695* | |
| Body mass index (Kg/m2) | <18.5 | −0.075 | 0.024 | −0.590* | −0.297 | −0.397* | −0.147 |
| 18.5–24.9 | Ref | Ref | Ref | Ref | Ref | Ref | |
| ≥25 | 0.268* | 0.010 | 0.350* | 0.104 | 0.308* | 0.020 | |
| Waist circumference | Normal | Ref | Ref | Ref | Ref | Ref | Ref |
| High | 0.311* | 0.171 | 0.239* | −0.125 | 0.328* | 0.069 | |
| Smoking | Never | Ref | Ref | Ref | Ref | Ref | Ref |
| Former | 0.088 | 0.077 | 0.197 | 0.233 | 0.222 | 0.197 | |
| Current | 0.460* | 0.527* | 0.330* | 0.471* | 0.409* | 0.474* | |
| Alcohol drinking | Never | Ref | Ref | Ref | Ref | Ref | Ref |
| Former | 0.310 | — | −0.139 | −0.268 | −0.078 | — | |
| Current | 0.169 | — | −0.431* | −0.465* | −0.152 | — | |
| Blood pressure (mmHg) | Optimal | Ref | Ref | Ref | Ref | Ref | Ref |
| High-normal | 0.152 | 0.134 | 0.547* | 0.535* | 0.424* | 0.390* | |
| Hypertension | 0.707* | 0.632* | 1.203* | 1.179* | 1.067* | 0.987* | |
| Blood glucose (mg/dL) | Normal | Ref | Ref | Ref | Ref | Ref | Ref |
| Impaired | 0.274* | 0.187 | 0.469* | 0.318* | 0.359* | 0.233* | |
| Diabetes | 0.871* | 0.667* | 0.999* | 0.892* | 0.979* | 0.778* | |
| High-density lipoprotein-cholesterol (mg/dL) | <40 | 0.167 | — | 0.563* | 0.511* | 0.447* | 0.401* |
| ≥40 | Ref | Ref | Ref | Ref | Ref | Ref | |
| Low-density lipoprotein-cholesterol (mg/dL) | <100 | Ref | Ref | Ref | Ref | Ref | Ref |
| 100–159 | −0.072 | — | 0.408* | 0.491* | 0.099 | 0.182 | |
| ≥160 | 0.135 | — | 1.064* | 1.056* | 0.434* | 0.445* | |
| Urinary proteins | − | Ref | Ref | Ref | Ref | Ref | Ref |
| ≥+1 | 0.587* | 0.430* | 0.282* | 0.069 | 0.386* | 0.198* | |
β1: adjusted for age and sex
β2: adjusted for age, sex, and significant variables in β1
*P-value < 0.10 in β1 and <0.05 in β2
Table 3.
Risk scores of stroke, coronary heart disease, and atherosclerotic cardiovascular disease
| Risk factors | Stroke | Coronary heart disease | Atherosclerotic cardiovascular disease | |
| Men | 0 | 13 | 7 | |
| Age | 40–44 years | 19 | 0 | 10 |
| 45–49 years | 29 | 11 | 18 | |
| 50–54 years | 31 | 11 | 20 | |
| 55–59 years | 40 | 14 | 25 | |
| 60–64 years | 43 | 19 | 31 | |
| 65–69 years | 52 | 22 | 35 | |
| 70–74 years | 57 | 25 | 39 | |
| ≥75 years | 63 | 28 | 42 | |
| Current smoking | 9 | 7 | 7 | |
| Current alcohol drinking | 0 | −6 | 0 | |
| Blood pressure | High-normal | 0 | 8 | 6 |
| Hypertension | 10 | 17 | 16 | |
| Blood glucose | Impaired | 0 | 5 | 4 |
| Diabetes | 11 | 13 | 12 | |
| HDL-c <40 mg/dL | 0 | 7 | 6 | |
| LDL-c (mg/dL) | 100–159 mg/dL | 0 | 7 | 0 |
| ≥160 mg/dL | 0 | 15 | 7 | |
| Urinary proteins ≥+1 | 7 | 0 | 3 | |
Table 4.
C-statistics of the risk scores after adding other risk factors
| Stroke | Coronary heart diseases | Atherosclerotic cardiovascular disease | |
| Primary risk model | 0.754 | 0.782 | 0.762 |
| +Chronic kidney disease | 0.755 | 0.782 | 0.762 |
| +Hypertensive retinopathy | 0.755 | 0.784 | 0.763 |
| +ECG findings | |||
| +Atrioventricular conduction defect | 0.755 | 0.782 | 0.763 |
| +High-amplitude R | 0.756 | 0.786 | 0.765 |
| +ST-T abnormalities | 0.756 | 0.782 | 0.763 |
| +Atrial fibrillation or flutter | 0.755 | 0.782 | 0.763 |
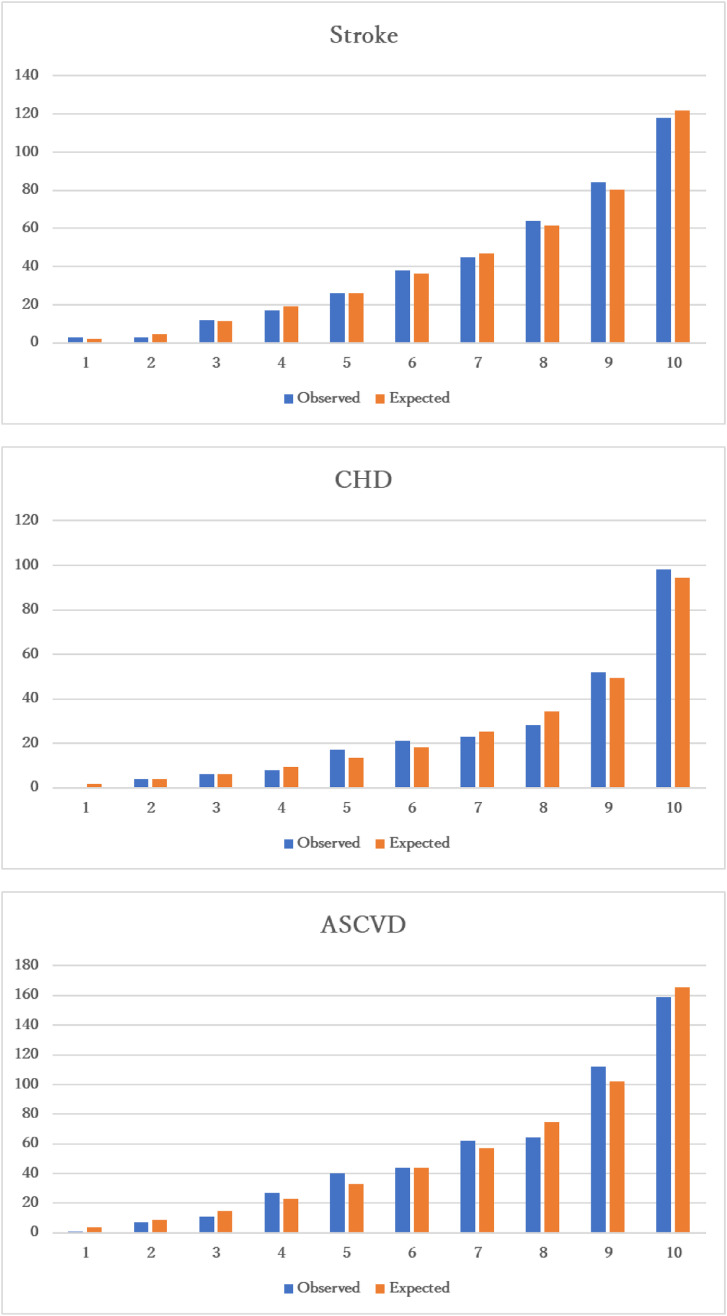
Fig. 1.
Hosmer-Lameshow goodness-of-fit test
P-values of goodness-of-fit were 0.981 for stroke, 0.746 for coronary heart disease (CHD), and 0.326 for atherosclerotic cardiovascular disease (ASCVD)
Table 5.
Incidence of cardiovascular diseases within 10 years by their risk scores
| Scores | Stroke, % | Coronary heart disease, % | Atherosclerotic cardiovascular disease, % |
| <15 | 0.2 | 0.3 | 0.2 |
| 15–24 | 0.4 | 0.3 | 0.8 |
| 25–34 | 1.0 | 0.7 | 1.2 |
| 35–44 | 2.2 | 2.2 | 3.5 |
| 45–54 | 3.8 | 3.5 | 5.7 |
| 55–64 | 7.3 | 8.2 | 9.6 |
| 65–74 | 10.3 | 11.8 | 19.6 |
| 75–84 | 18.0 | 13.2 | 21.5 |
| ≥85 | 27.7 | 23.5 | 60.5 |
N.B. The maximum risk score is 100.
3. Results
Participants who developed ASCVD had higher proportions of men, older adults, obesity, current smoking, hypertension, diabetes, decreased HDL-c, increased LDL-c, and urinary proteins (Table 1).
Within 110,428 person-years (median follow-up = 16.6 years), 410 stroke events (261 cerebral infarction, 73 intracerebral hemorrhage, 35 subarachnoid hemorrhage, and 41 unspecified types), 288 CHD events (83 confirmed myocardial infarction, 93 potential myocardial infarction, 108 percutaneous coronary intervention or coronary artery bypass grafting, and 4 sudden cardiac deaths), and 527 ASCVD events were diagnosed (22 participants developed both cerebral infarction and CHD).
In the multivariable-adjusted model, age, smoking, hypertension, and diabetes were associated with stroke, CHD, and ASCVD risk. The risk of CHD and ASCVD was higher among men than women. Decreased HDL-c and increased LDL-c were associated with higher CHD and ASCVD risk. Urinary proteins were associated with higher stroke and ASCVD risk. Alcohol consumption was inversely associated with CHD risk (Table 2). P-values for sex interaction were provided (Supplementary Table 1). The risk scores of variables contributing to stroke, CHD, and ASCVD risk were described (Table 3). The C-statistic values were 0.754 for stroke, 0.782 for CHD, and 0.762 for ASCVD (Table 4). The p-values of the goodness-of-fit were 0.981 for stroke, 0.746 for CHD, and 0.326 for ASCVD (Fig. 1). The 10-year incidence of stroke, CVD, and ASCVD events was 0.2%, 0.3%, and 0.2% for scores <15, 3.8%, 3.5%, and 5.7% for scores 45–54, 10.3%, 11.8%, and 19.6% for scores 65–74, and 27.7%, 23.5%, and 60.5% for scores ≥85, respectively (Table 5). The age- and sex-adjusted associations with CKD, hypertensive retinopathy, and other ECG findings were provided (Supplementary Table 2). Adding these variables to the final risk models did not improve the C-statistics (Table 4).
4. Discussion
This study indicated new Suita risk models for stroke, CHD, and ASCVD using risk factors similar to those collected in the Japanese governmental health check-ups. Within a median follow-up of 16.6 years, age, smoking, hypertension, and diabetes were associated with stroke, CHD, and ASCVD risk. Men had a higher risk of developing CHD and ASCVD than women. Decreased HDL-c and increased LDL-c were associated with higher CHD and ASCVD risk. Urinary proteins were associated with higher stroke and ASCVD risk. Alcohol consumption was inversely associated with CHD risk. The three risk models performed well in terms of discrimination and calibration. We also developed three simple risk scores ranging between zero and 100 and calculated the 10-year incidence of stroke, CHD, and ASCVD per these scores for potential health education purposes.
Our results aligned with other national risk models [16–21]. For example, the Hisayama study suggested a model, including age, sex, smoking, Systolic BP (SBP), diabetes, HDL-c, and LDL-c, to predict CVD. Later, they added urinary protein and physical activity to create a new model predicting ASCVD [16, 17]. Two risk models were extracted from the Japan Public Health Center-Based Prospective Study (JPHC); one for stroke [18] and the other one for CHD [19]. Both models included age, sex, smoking, SBP, antihypertensive medication use, and diabetes. In addition, the stroke model included BMI and the CHD model included HDL-c and non-HDL-c [18, 19]. In the Japan Arteriosclerosis Longitudinal Study (JALS), age, sex, smoking, hypertension, and diabetes predicted stroke and myocardial infarction. HDL-c and non-HDL-c were associated with myocardial infarction but not stroke [20]. In the Jichi Medical School (JMS) Cohort Study, age, sex, smoking, SBP, and diabetes were associated with stroke and cerebral infarction risk [21]. Using the IQVIA Japan Claims Database, the risk factors for stroke were age and SBP, while those for CHD were age, sex, SBP, HDL-c, LDL-c, and total cholesterol [22]. The annual check-ups of Ibaraki prefecture showed that age, being underweight, smoking, SBP, hypertension medication, diabetes, HDL-c, total cholesterol, and urinary proteins were risk factors for CVD mortality [23]. A summary of the featured Japanese CVD prediction models is provided (Supplementary Table 3).
Compared to the previous Suita risk scores, the current scores showed some differences. For example, the maximum scores of previous Suita risk scores were 26 for stroke, 104 for CHD, and 65 for CVD [4–6], compared to 100 in the current risk scores, making the current risk scores easier for calculation and comparisons. Additionally, previous Suita risk scores included variables that are not regularly assessed in the Japanese governmental health check-ups, such as CKD in the Stroke and CHD risk scores, atrial fibrillation in the Stroke and CVD risk scores, and left ventricular hypertrophy in the CVD risk score [4–6]. Thus, the previous Suita risk scores could not be implemented in the Japanese governmental health check-ups. These variables were not included in the current risk scores.
Our study had several strengths, such as the prospective design, long follow-up period, representativeness of the study population for urban people in Japan, ascertaining stroke, CHD, and their risk factors using standardized methods, the long follow-up period, and the development of simple risk scores. However, this study is not without limitations. First, we assessed the risk factors during baseline only. Participants with chronic diseases might have received close monitoring which minimized their contribution to ASCVD risk. Alike, around 50% of smokers at baseline quit smoking during follow-up, suggesting that the risk of smoking in this study could be underestimated. Second, the previous Suita risk models [4–6] were internally validated; therefore, we did not repeat this process in the current study. However, none of the previous or new Suita risk models were externally validated. Third, while the age of participants ranged between 30 and 84 years, Tokutei-Kenshin check-ups are conducted for those between 40–74 years. However, when we limited our analysis to this age group, the risk models did not materially change (data are not shown). By including data for those under the age of 40 years and those aged 75 and over, it is possible to evaluate the risk of ASCVD in age groups not included in Tokutei-Kenshin. Fourth, we created a prediction model limited to specific medical check-up items. Therefore, lifestyle habits, such as physical activity and diet, were not examined. Both factors can significantly influence ASCVD risk [2, 3]. Fifth, because of the low statistical power, we could not assess the risk by subtypes of cerebral infarction (atherothrombotic, lacunar, and cardioembolic infarction) and hemorrhagic stroke (intracerebral and subarachnoid hemorrhage). Sixth, lifestyle habits that may impact ASCVD, such as diet and sleep, are not often assessed in Japanese governmental health check-ups. Thus, they were not included in our models.
In conclusion, using traditional CVD risk factors from the Suita Study, we developed new risk models to predict stroke, CHD, and ASCVD in Japanese people. Among the suggested risk factors, current smoking, hypertension, diabetes, reduced HDL-c, elevated LDL-c, and urinary proteins are modifiable, suggesting that early detection and management of these health conditions can potentially reduce the risk of ASCVD. Compared to the previous Suita models, the new models can be more practical on the national level because they include factors like those in the Japanese governmental health check-ups. Besides, the risk scores in the current models are easier to calculate, and consequently more convenient to be used for health guidance. From a preventive medical point of view, developing a risk tool that can evaluate other lifestyle habits that increase the contribution rate of the risk score is still required.
Abbreviations
- ASCVD
Atherosclerotic cardiovascular disease
- BMI
Body mass index
- BP
Blood pressure
- CHD
Coronary heart disease
- CKD
Chronic kidney disease
- ECG
Electrocardiography
- FBG
Fasting blood glucose
- HDL-c
High-density lipoprotein-cholesterol
- JALS
Japan Arteriosclerosis Longitudinal Study
- JMS
Jichi Medical School
- LDL-c
Low-density lipoprotein-cholesterol
- NCVC
National Cerebral Cardiovascular Centre
- SBP
Systolic blood pressure
- WHO MONICA
World Health Organization Multinational MONItoring of Trends and Determinants in CArdiovascular Disease
Supplementary information
Additional file 1: Supplementary Table 1: P-values for sex interaction with potential risk factors. Supplementary Table 2: Associations between potential risk factors (added one by one to the risk models) and cardiovascular disease risk. Supplementary Table 3: Summary of Japanese cardiovascular disease prediction models.
Declarations
Ethical approval and consent to participate
The Suita Study protocol was approved by the Institutional Review Board of the NCVC (R21024). We conducted the study according to the Declaration of Helsinki. All participants signed their informed consent forms.
Consent for publication
We obtained consent from patients to publish their findings while keeping their details anonymous and all authors accepted the final version of the manuscript.
Acknowledgment
We would like to thank the Suita Medical Association, the Suita City Health Center, the Preventive Cardiology and Preventive Healthcare Departments, and all cohort members. We would like to thank Dr. Kawanishi and Dr. Misaki, the former and current presidents of the Suita City Medical Association.
Competing interests
None to declare.
Funding
This study was supported by the Intramural Research Fund for the cardiovascular diseases of the NCVC (20-4-9), Japan Health Research Promotion Bureau (2019-(1)-1), Japan Science and Technology Agency (JPMJPF2018), the Health and Labour Sciences Research Grants of the Ministry of Health, Labour, and Welfare of Japan (20FA1002), and the Meiji Yasuda Health Insurance Company and Research Institute.
Availability of data and materials
Available upon reasonable request.
Authors’ contributions
AA (draft writing, review literature, and data analysis), YK (resources, funding acquisition, and supervision), and all authors (visualization, revision, and editing).
References
- 1.Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 Study. J Am Coll Cardiol. 2020;76(25):2982–3021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Arafa A, Lee HH, Eshak ES, Shirai K, Liu K, Li J, et al. Modifiable risk factors for cardiovascular disease in Korea and Japan. Korean Circ J. 2021;51(8):643–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Arafa A, Kokubo Y, Kashima R, Teramoto M, Sakai Y, Nosaka S, et al. The Lifelong Health Support 10: a Japanese prescription for a long and healthy life. Environ Health Prev Med. 2022;27:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arafa A, Kokubo Y, Sheerah HA, Sakai Y, Watanabe E, Li J, et al. Developing a stroke risk prediction model using cardiovascular risk factors: the Suita Study. Cerebrovasc Dis. 2022;51(3):323–30. [DOI] [PubMed] [Google Scholar]
- 5.Nishimura K, Okamura T, Watanabe M, Nakai M, Takegami M, Higashiyama A, et al. Predicting coronary heart disease using risk factor categories for a Japanese urban population, and comparison with the Framingham risk score: the Suita Study. J Atheroscler Thromb. 2014;21(8):784–98. [DOI] [PubMed] [Google Scholar]
- 6.Nakai M, Watanabe M, Kokubo Y, Nishimura K, Higashiyama A, Takegami M, et al. Development of a cardiovascular disease risk prediction model using the Suita Study, a population-based prospective cohort study in Japan. J Atheroscler Thromb. 2020;27(11):1160–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Specific health checkups and specific health guidance. Health and medical services. Ministry of Health, Labour, and Welfare of Japan. https://www.mhlw.go.jp/english/wp/wp-hw3/dl/2-007.pdf. Accessed on the 5th of February, 2023.
- 8.Walker AE, Robins M, Weinfeld FD. The National Survey of Stroke. Clinical findings. Stroke. 1981;12(2 Pt 2 Suppl 1):I13–44. [PubMed] [Google Scholar]
- 9.The World Health Organization MONICA Project (monitoring trends and determinants in cardiovascular disease): a major international collaboration. WHO MONICA Project Principal Investigators. J Clin Epidemiol. 1988;41(2):105–14. [DOI] [PubMed] [Google Scholar]
- 10.Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens Res. 2019;42(9):1235–481. [DOI] [PubMed] [Google Scholar]
- 11.Araki E, Goto A, Kondo T, Noda M, Noto H, Origasa H, et al. Japanese Clinical Practice Guideline for Diabetes 2019. J Diabetes Investig. 2020;11(4):1020–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kinoshita M, Yokote K, Arai H, Iida M, Ishigaki Y, Ishibashi S, et al. Japan Atherosclerosis Society (JAS) Guidelines for Prevention of Atherosclerotic Cardiovascular Diseases 2017. J Atheroscler Thromb. 2018;25(9):846–984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Keith NM, Wagener HP, Barker NW. Some different types of essential hypertension: their course and prognosis. Am J Med Sci. 1974;268(6):336–45. [DOI] [PubMed] [Google Scholar]
- 14.Harrell FE Jr, Lee KL, Mark DB. Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med. 1996;15(4):361–87. [DOI] [PubMed] [Google Scholar]
- 15.Hosmer DW, Lemeshow S. A goodness-of-fit test for the multiple logistic regression model. Commun Stat. 1980;(A10):1043–69. [Google Scholar]
- 16.Arima H, Yonemoto K, Doi Y, Ninomiya T, Hata J, Tanizaki Y, et al. Development and validation of a cardiovascular risk prediction model for Japanese: the Hisayama study. Hypertens Res. 2009;32(12):1119–22. [DOI] [PubMed] [Google Scholar]
- 17.Honda T, Chen S, Hata J, Yoshida D, Hirakawa Y, Furuta Y, et al. Development and validation of a risk prediction model for atherosclerotic cardiovascular disease in Japanese adults: the Hisayama Study. J Atheroscler Thromb. 2022;29(3):345–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yatsuya H, Iso H, Yamagishi K, Kokubo Y, Saito I, Suzuki K, et al. Development of a point-based prediction model for the incidence of total stroke: Japan public health center study. Stroke. 2013;44(5):1295–302. [DOI] [PubMed] [Google Scholar]
- 19.Yatsuya H, Iso H, Li Y, Yamagishi K, Kokubo Y, Saito I, et al. Development of a risk equation for the incidence of coronary artery disease and ischemic stroke for middle-aged Japanese - Japan Public Health Center-Based Prospective Study. Circ J. 2016;80(6):1386–95. [DOI] [PubMed] [Google Scholar]
- 20.Harada A, Ueshima H, Kinoshita Y, Miura K, Ohkubo T, Asayama K, et al. Absolute risk score for stroke, myocardial infarction, and all cardiovascular disease: Japan Arteriosclerosis Longitudinal Study. Hypertens Res. 2019;42(4):567–79. [DOI] [PubMed] [Google Scholar]
- 21.Ishikawa S, Matsumoto M, Kayaba K, Gotoh T, Nago N, Tsutsumi A, et al. Risk charts illustrating the 10-year risk of stroke among residents of Japanese rural communities: the JMS Cohort Study. J Epidemiol. 2009;19(2):101–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yoshida S, Tanaka S, Okada M, Ohki T, Yamagishi K, Okuno Y. Development and validation of ischemic heart disease and stroke prognostic models using large-scale real-world data from Japan. Environ Health Prev Med. 2023;28:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Noda H, Iso H, Sairenchi T, Irie F, Fukasawa N, Toriyama Y, et al. [Prediction of stroke, coronary heart disease, cardiovascular disease, cancer, and total death based on results of annual health checkups]. Nihon Koshu Eisei Zasshi. 2006;53(4):265–76. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Supplementary Table 1: P-values for sex interaction with potential risk factors. Supplementary Table 2: Associations between potential risk factors (added one by one to the risk models) and cardiovascular disease risk. Supplementary Table 3: Summary of Japanese cardiovascular disease prediction models.
Data Availability Statement
Available upon reasonable request.