Abstract
An aortico-left ventricular tunnel is a rare congenital heart disease, and its prenatal diagnosis is even rarer. This report describes a fetus diagnosed with an aortico-left ventricular tunnel at 26 weeks of gestation. After delivery, the infant exhibited cyanosis and cessation of breathing. After resuscitation, he was transferred to the neonatal intensive care unit. Echocardiography confirmed an aortico-left ventricular tunnel. The infant survived after surgical repair. An aortico-left ventricular tunnel can be diagnosed by antenatal ultrasound, and prompt neonatal management can help to prevent perinatal morbidity and mortality.
Keywords: Aortico-left ventricular tunnel, echocardiography, fetus, neonatal, case report, prenatal diagnosis
Introduction
An aortico-left ventricular tunnel is an extracardiac channel connecting the ascending aorta to the left or right ventricular cavity. 1 It was first reported by Edwards 2 in 1961 and named by Levy et al. 3 in 1963. An aortico-left ventricular tunnel is a rare congenital cardiac malformation accounting for approximately 0.001% of all congenital heart diseases. 1 Affected patients usually present with symptoms of congestive heart failure. Early surgical treatment is recommended to prevent complications. Prenatal diagnosis of this congenital cardiac defect is rare. The present report describes a fetus prenatally diagnosed with an aortico-left ventricular tunnel that was successfully repaired after birth.
Case report
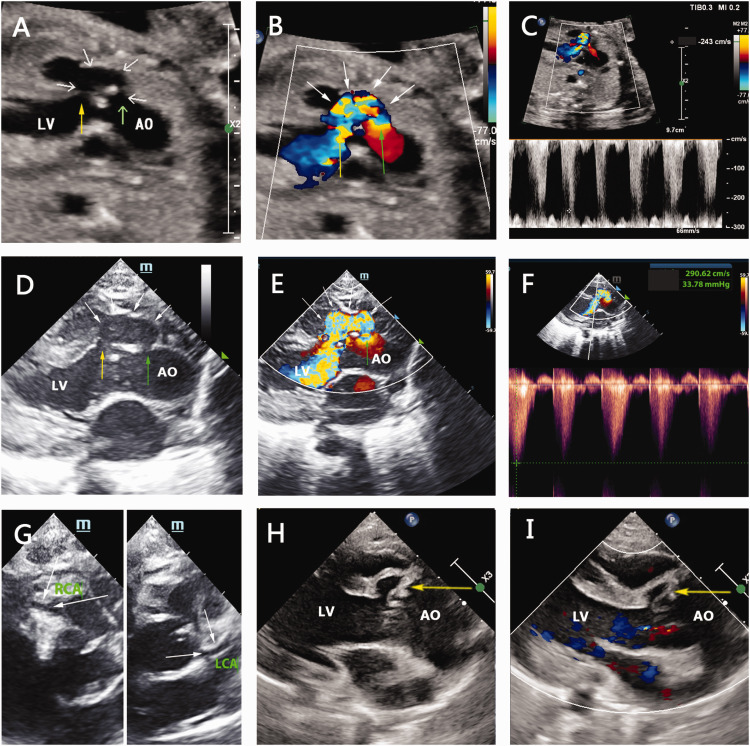
A 37-year-old woman, gravida 2 para 1 (healthy first child), with no history of congenital disabilities or other diseases, was admitted to the authors’ hospital at 26 weeks of gestation because her fetus had been diagnosed with left ventricular enlargement 1 week before. Fetal ultrasound revealed a normal heart position. However, the left ventricle was larger than the right ventricle, the cardiothoracic area ratio was 45%, the three-vessel view was abnormal, and the pulmonary artery was narrower than the aorta. In addition, the fetal aortic annulus diameter was 4.9 mm (normal range, 3.7–5.8 mm), and the pulmonary annulus diameter was 5.0 mm (normal range, 4.2–6.4 mm). The ascending aorta (7.6 mm) was wider than the pulmonary artery (5.1 mm), and the ratio of the pulmonary artery/ascending aorta was 0.67. The left ventricular ejection fraction was 59%. The left ventricular long-axis view showed an abnormal paravalvular C-shaped tunnel-like route originating from the ascending aorta, bypassing the aortic valve, and opening into the left ventricular cavity (Figure 1(a), Supplemental Online Video 1). The tunnel-like route had a width of 2.4 mm on both the side adjacent to the ascending aorta and the side adjacent to the left ventricular cavity. Color Doppler indicated that the blood flow from the aortic valve margins to the left ventricle was retrograde in the diastolic phase and orthodromic in the systolic phase (Figure 1(b), Supplemental Online Video 1). Continuous-wave Doppler showed a turbulent spectrum from the anomalous duct to the left ventricle in the diastolic phase; the peak systolic velocity was 2.4 m/s (Figure 1(c)). These findings suggested a diagnosis of an aortico-left ventricular tunnel.
Figure 1.
(a–c) Echocardiographic images of the fetus at 26 weeks of gestation. (a) Left ventricular long-axis view showing the opening of the tunnel on the left ventricle side (yellow arrow), the ascending aorta side (green arrow), and the tunnel body (white arrow) (see Supplemental Online Video 1). (b) Color Doppler flow imaging of the aortico-left ventricular tunnel. The blood flow from the aortic valve margins to the left ventricle was retrograde in the diastolic phase and orthodromic in the systolic phase (see Supplemental Online Video 1). (c) Blood flow spectrum in the duct. The spectrum from the anomalous duct to the left ventricle was turbulent in the diastolic phase. The peak systolic velocity was 2.4 m/s. (d–g) Echocardiographic images were obtained 1 day after birth. (d) The left ventricular long-axis view showed the opening of the tunnel on the left ventricle side (yellow arrow), the ascending aorta side (green arrow), and the tunnel body (white arrow). (e) Color Doppler flow imaging of the aortico-left ventricular tunnel. The blood flowed into the left ventricular outflow tract through this tunnel (see Supplemental Online Video 2). (f) Spectrum of blood flow in the duct. The peak systolic velocity was 2.9 m/s. (g) The right and left coronary arteries were normal (white arrow). (h–i) Echocardiographic images after surgery. (h) Left ventricular long-axis view showing the surgical patch in the tunnel (yellow arrow). (i) Color Doppler flow imaging indicated no abnormal blood flow signal through the tunnel (yellow arrow).
The patient underwent multiple fetal heart ultrasound examinations for 1 month, showing a stable fetal condition. At 33 weeks of gestation, the mother’s blood pressure increased to 155/99 mmHg, progressing to severe preeclampsia at 35+6 weeks. A boy was delivered by cesarean section. His Apgar scores were 8 and 10 at 1 and 5 minutes, respectively. The child’s birth weight was 2.58 kg. Eight minutes after delivery (09:10), the infant exhibited cyanosis and cessation of breathing. His temperature was 35.9°C, heart rate was 40 beats/minute, and SpO2 was 24%. After resuscitation, the child was transferred to the neonatal intensive care unit. He had a grade 3/4 systolic and diastolic murmur at the left intercostal margin. At 09:12, his blood pressure was 81/34 (48) mmHg, SpO2 was 75%, heart rate was 124 beats/minute, and respiration was 30 breaths/minute, and his cyanosis had improved. At 09:14, his SpO2 increased to 95% and his respiration increased to 42 breaths/minute. He was treated with continuous positive airway pressure. On the same day, echocardiography confirmed an aortico-left ventricular tunnel (Figure 1(d)). The width of the tunnel was 3.0 mm on the ascending aorta side and 3.0 mm on the left ventricle side. The width of the tunnel body was 5.9 mm. Color Doppler indicated that the blood flowed into the left ventricular outflow tract through this tunnel (Figure 1(e), Supplemental Online Video 2). The peak systolic velocity was 2.9 m/s (Figure 1(f)). The left ventricular ejection fraction was 64%. In the cardiac-base short-axis view of the aorta, the bilateral coronary arteries were normal (Figure 1(g)). Patent ductus arteriosus and an atrial septal defect with patent foramen ovale were observed.
The left ventricular ejection fraction on days 4, 8, 12, and 16 after delivery was 53%, 55%, 55%, and 59%, respectively. The patient underwent successful surgical patch closure of the defect. Echocardiography demonstrated the aortico-left ventricular tunnel had been successfully repaired, and the left ventricular ejection fraction was 75.7%. The infant had normal left ventricular function at discharge (Figure 1(h), (i); Supplemental Online Video 3), and his condition was stable.
Discussion
This case report suggests that an aortico-left ventricular tunnel might be diagnosed by antenatal ultrasound and that prompt neonatal management can help to prevent perinatal morbidity and mortality.
Angiography cannot differentiate an aortico-left ventricular tunnel from aortic regurgitation, and neonates can be easily misdiagnosed with other heart malformations.4,5 However, echocardiography can clearly show two-dimensional structures in real time, and color Doppler can display the blood flow. Echocardiography is an accurate, noninvasive, and effective way to show the inlet and inside of the channel structure. 4 Two-dimensional ultrasound scanning with color Doppler flow imaging is the gold standard for diagnosing aortico-left ventricular tunnel. 6
The clinical features of an aortico-left ventricular tunnel are similar to those of aortic insufficiency. 7 The most important feature is abnormal blood flow. Color Doppler flow imaging can show whether the aortico-left ventricular tunnel connects the ascending aorta with the left ventricle in a non-echo tube and whether the original blood flow of aortic insufficiency is derived from the aortic valve. Compared with aortic insufficiency, it is difficult to differentiate sinus of Valsalva aneurysm rupture and a coronary artery–left ventricular fistula from an aortico-left ventricular tunnel. 5 In patients with a ruptured sinus of Valsalva aneurysm, the rupture is below the annulus level, and an expansion of the Valsalva aneurysm is usually present. The two-dimensional image will display the interrupted sinus wall. Color Doppler usually shows that the blood flows into the left ventricular outflow tract through this tunnel. The aortico-left ventricular tunnel is often derived from above the opening of the coronary artery. In patients with a coronary artery–left ventricular fistula, two-dimensional ultrasound will reveal dilatation of the coronary artery, whereas patients with an aortico-left ventricular tunnel will show no abnormalities.
In the case reported herein, the aortico-left ventricular tunnel was diagnosed prenatally. It is essential to evaluate fetal heart function because it is closely related to the prognosis. 8 If the fetal cardiac function progressively deteriorates, a balance between the cardiac function and the gestational age should be achieved by timely delivery and surgical repair. In this case, the fetus had normal cardiac function during pregnancy, and early recognition of the aortico-left ventricular tunnel by antenatal ultrasound allowed for prompt neonatal management. 9 Fetuses at high risk require correct early diagnosis and continuous surveillance after delivery to prevent perinatal morbidity and mortality. Patients with an aortico-left ventricular tunnel usually develop congestive heart failure symptoms during their childhood, which is possibly related to ventricular volume overload. 10 Early surgical management is recommended to prevent complications. 11
Conclusion
Early recognition of an aortico-left ventricular tunnel by antenatal ultrasound allows prompt neonatal management and prevents perinatal morbidity and mortality.
Supplemental Material
Supplemental material, sj-mp4-1-imr-10.1177_03000605231207756 for Diagnosis of an aortico-left ventricular tunnel in a fetus: a case report by Yelin Lou, Yang Hu and Xiaoying Tao in Journal of International Medical Research
Supplemental material, sj-mp4-2-imr-10.1177_03000605231207756 for Diagnosis of an aortico-left ventricular tunnel in a fetus: a case report by Yelin Lou, Yang Hu and Xiaoying Tao in Journal of International Medical Research
Supplemental material, sj-mp4-3-imr-10.1177_03000605231207756 for Diagnosis of an aortico-left ventricular tunnel in a fetus: a case report by Yelin Lou, Yang Hu and Xiaoying Tao in Journal of International Medical Research
Acknowledgements
We wish to thank the patient’s family for sharing the patient’s medical record.
Authors’ contributions: Conceptualization: Y.H.; Methodology and investigation: X.T.; Writing – original draft preparation: Y.L.; Writing – review and editing: Y.H.; Funding: Y.H.
Funding: This work was supported by the Natural Science Foundation of Zhejiang Province (No. LSY19H180006) and the Jinhua Science and Technology Bureau (No. 2019-3-012).
ORCID iD: Yang Hu https://orcid.org/0000-0001-6320-4316
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Consent for publication
The infant’s parents provided written informed consent for publication.
Declaration of competing interests
The authors have no conflicts of interest to disclose.
Ethics approval and consent to participate
This work was carried out in accordance with the Declaration of Helsinki (2000) of the World Medical Association. This study was approved by the Department of Ultrasonography, Affiliated Jinhua Hospital, Zhejiang University School of Medicine (approval number: 2022-ethical review-264, approval date: 30 November 2022). The infant’s parents provided written informed consent for participation.
References
- 1.Kathare P, Subramanyam RG, Dash TK, et al. Diagnosis and management of aorto-left ventricular tunnel. Ann Pediatr Cardiol 2015; 8: 103–107. 2015/06/19. DOI: 10.4103/0974-2069.157021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Edwards JE. An atlas of acquired disease of the heart and great vessels. 2nd. Vol. 2. WB Saunders; Philadelphia: 1961. p. 1142. [Google Scholar]
- 3.Levy MJ, Schachner A, Blieden LC. Aortico-left ventricular tunnel: collective review. J Thorac Cardiovasc Surg 1982; 84: 102–109. 1982/07/01. [PubMed] [Google Scholar]
- 4.Xie M, Yin J, Lv Q, et al. Clinical value of diagnosing aortico-left ventricular tunnel by echocardiography. Exp Ther Med 2016; 12: 3315–3319. 2016/11/25. DOI: 10.3892/etm.2016.3747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen LL, Zhang CQ, Gong LG. A special type aortico-left ventricular tunnel with bicuspid aortic valve. Int J Cardiovasc Imaging 2020; 36: 55–57. 2019/09/11. DOI: 10.1007/s10554-019-01692-9. [DOI] [PubMed] [Google Scholar]
- 6.Singh A, Reinhardt Z, Desai T, et al. Case series of antenatally diagnosed aortico-left ventricular tunnel. Pediatr Cardiol 2011; 32: 822–825. 2011/03/08. DOI: 10.1007/s00246-011-9940-9. [DOI] [PubMed] [Google Scholar]
- 7.Jone PN, Mitchell MB, Campbell DN, et al. Prenatal diagnosis and successful outcome in neonate of aorto-left ventricle tunnel. Echocardiography 2014; 31: E20–E23. 2014/01/05. DOI: 10.1111/echo.12396. [DOI] [PubMed] [Google Scholar]
- 8.Grab D, Paulus WE, Terinde R, et al. Prenatal diagnosis of an aortico-left ventricular tunnel. Ultrasound Obstet Gynecol 2000; 15: 435–438. 2000/09/08. DOI: 10.1046/j.1469-0705.2000.00119.x. [DOI] [PubMed] [Google Scholar]
- 9.Nakamura Y, Miyaji K, Yoshii T, et al. Aorto-left ventricular tunnel successfully repaired immediately after birth. Ann Thorac Surg 2016; 101: 1988–1990. 2016/04/24. DOI: 10.1016/j.athoracsur.2015.06.105. [DOI] [PubMed] [Google Scholar]
- 10.Smith BM, Cochran CD, Owens ST. Aortico-left ventricular tunnel and left ventricular non-compaction: a case series. Cardiol Young 2016; 26: 382–385. 2015/06/23. DOI: 10.1017/S1047951115001109. [DOI] [PubMed] [Google Scholar]
- 11.Alpat S, Forgie KA, VonderMuhll I, et al. Valve-sparing aortic root replacement 3 decades after repair of aortico-left ventricular tunnel. Ann Thorac Surg 2020; 109: E37–E39. 2019/06/23. DOI: 10.1016/j.athoracsur.2019.04.092. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-mp4-1-imr-10.1177_03000605231207756 for Diagnosis of an aortico-left ventricular tunnel in a fetus: a case report by Yelin Lou, Yang Hu and Xiaoying Tao in Journal of International Medical Research
Supplemental material, sj-mp4-2-imr-10.1177_03000605231207756 for Diagnosis of an aortico-left ventricular tunnel in a fetus: a case report by Yelin Lou, Yang Hu and Xiaoying Tao in Journal of International Medical Research
Supplemental material, sj-mp4-3-imr-10.1177_03000605231207756 for Diagnosis of an aortico-left ventricular tunnel in a fetus: a case report by Yelin Lou, Yang Hu and Xiaoying Tao in Journal of International Medical Research
Data Availability Statement
All data generated or analyzed during this study are included in this published article.