Abstract
Introduction- Subscapularis augmented Bankart repair (SB) is a novel arthroscopic technique of tenodesis of upper 1/3rd fibers of subscapularis tendon to capsulo-labral repair of Bankart lesion. Treatment of Bony Bankart lesion with glenoid bone loss % (GBL%) 10%–20 % is still a grey zone where bone augmentation procedures are an overtreatment and capsulo-labral repair is associated with high recurrence.
Methodology
A retrospective study of 30 patients with h/o anterior instability with GBL%<20 % were classified into two groups. SB group included patients managed with arthroscopic subscapularis augmentation while CB group included patients managed with arthroscopic capsulo-labral repair. These patients were followed up after a minimum of 24 months post-surgery and functional outcomes evaluated using WOSI, ASES and ROWE scores.
Results
Patients in the SB group showed superior functional outcomes for WOSI and ROWE scores. Considering postoperative shoulder pain, the median ROWE-P (pain) score was better for SB group (10/10) when compared to CB group (5/10). Patients under SB group were more comfortable with physical symptoms of their shoulder (WOSI-P average 60/1000) and were more likely to continue their recreational sports activity (WOSI- sports for SB 63.7 and CB 119.5. In our study, none of the 15 SB patients had any restriction in range of shoulder movements [ROWE-M score of 10]. Subscapularis augmented Bankart repair is associated with minimal restriction of shoulder range, better pain relief, better acceptability and smoother return to daily living and occupation and can be considered as a routine for every patient with GBL<20 %.
Keywords: Subscapularis augmentation, Bankart repair, Anterior instability, Glenoid bone loss, Arthroscopic repair
1. Introduction
Burkhart and De Beer1 in 2000 emphasized on importance of bony defects (bony Bankart and Hill Sach lesion) in anterior instability and its role in his arthroscopic surgical failure. A ‘Bipolar’ pathology responsible for recurrence was theorised. The technique of arthroscopic ‘REMPLISSAGE’ by Wolf and Arianjam2 was introduced for humeral head lesions, with subsequent studies confirming better response with both tehniques used together over an isolated Bankart repair for engaging Hill Sach lesions3.
Arthroscopic capsulo-labral Bankart repair (CB) prove to be effective for GBL <10 %. GBL of over 25 % requires some bone augmentation procedure such as Latarjet procedure, which is preferred owing to its low recurrence rates of 1–8%.4 It also is the procedure of choice for instability in collision sports irrespective of the GBL. However, a grey area of moderate GBL (10–20 %) exists where bone augmentation can be considered as an over treatment and higher failure rates are seen with conventional arthroscopic Bankart repair.
Symenoidis5 studied the role of subscapularis muscle in pathogenesis of recurrent anterior instability. Owing to the inferior direction of repeatedly falling humeral head, the subscapularis muscle becomes lax along with injury to the inferior glenoid labrum and the adjacent capsule. Johnson in 1986 mentioned the inferior glenohumeral ligament as ‘virtually non-existent’ in chronic dislocations.6 Thus, a consistent soft tissue envelope remains lax antero-inferiorly in chronic recurrent dislocations which alter stabilisation dynamics of the shoulder, irrespective of presence of any bony defect. The importance of this subscapularis strengthening of a deficient glenohumeral ligament shoulder was mentioned by Maoitti7 when he introduced Subscapularis augmentation (SB) of capsulo-tenodesis of Bankart defect. In his studies that followed, SB Bankart repair proved to be a valid choice even for collision sport athletes and for shoulder hyperlaxity.7,8 In a multicentric study, a recurrence rate of only 2.7% was reported for SB for GBL between 5 % and 25 %.
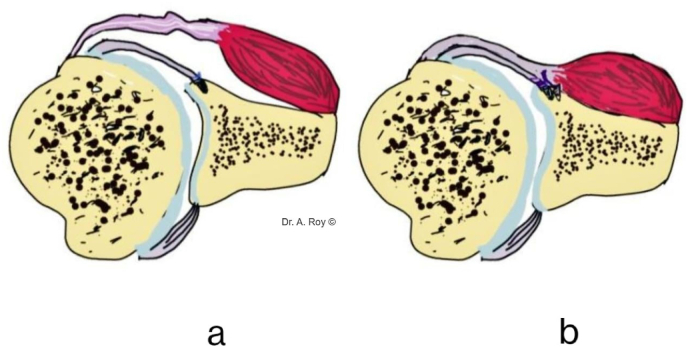
Subscapularis augmented Bankart repair (SB) is an arthroscopic surgery involving tenodesis of upper 1/3rd fibres of subscapularis tendon to the framework of capsulolabral repair. Used with remplissage, SB provides a more physiological treatment for the triad of anterior instability i.e., Hill Sach lesion, Bankart defect and inferior glenohumeral ligament laxity (See Fig. 1). We believe that subscapularis augmentation should be a routine part of arthroscopic management of chronic anterior instability of shoulder with moderate glenoid bone loss (<20 %) as it restabilises and strengthens the compromised anterior soft tissue strut.
Fig. 1.
1a- Capsulolabral bankart repair with lax anteroinferior soft tissue. 1b- Subscapularis augmented Bankart repair with strengthened soft tissue strut.
In our study we compared postoperative shoulder scores of 30 patients divided in two groups (15 each) – subscapularis augmented repair group (SB) and capsulo-labral repair group (CB) after a minimum follow up of 48 months. The purpose of our study is to compare the functional outcomes assessing broadly - pain, instability, and stiffness of managed shoulder in both groups.
2. Design
An observational study comparing functional outcomes of SB approach vs CB approach during patient follow up, with three shoulder scoring systems (ROWE, ASES, WOSI). Preoperative and intraoperative details were confirmed retrospectively.
2.1. Materials and methodology
The study group consisted of patients below age of 60 years, professionally non athletes/sportsmen, may be involved in sports for recreation, who were operated in our institute at least 48 months prior to start of study for diagnosed anterior instability of glenohumeral joint with MRI proven Bankart lesion (<20 % GBL) managed with arthroscopic Bankart repair. (The GBL% being mentioned in CT scan reports). Engaging Hill Sachs lesion if present were managed with an additional Remplissage procedure.
Records with any history of global instability/habitual dislocation were excluded. Any documented associated lesions i.e. Humeral avulsion of inferior glenohumeral ligament (HAGL)/Kim's lesion/ALPSA lesion/other labral tears/rotator cuff tear or pathology/capsulitis were excluded from the study. Patients without remplissage done for engaging Hill Sachs defect were excluded.
SB group included patients managed with arthroscopic subscapularis augmentation of capsulo-labral repair while CB group included patients managed with arthroscopic capsulo-labral repair. Proper informed consent was taken for every participant. Patient in either group were subdivided depending upon the level of their activity into low (eg-desk job) and moderate (eg-labourer) functional requirement group. A physical examination of every patient evaluating range of motion, apprehension test was carried out. Functional scores of WOSI, ASES and ROWE SCORES for every participant were documented by a single observer. Assessment of pain, stability and stiffness in operated shoulder was carried out with the scores for comparison among both the groups. (WOSI- WESTERN ONTARIO SHOULDER INSTABILITY INDEX) (ASES- American Shoulder and Elbow Surgeons Shoulder Score) (ROWE being an objective score)
2.2. Surgical technique
2.2.1. Common steps in both groups
General anaesthesia (G.A.) ± regional block was used for induction. Surgery was carried out in Floppy lateral position with upper limb in abduction and forward flexion with a traction system and weights in place.
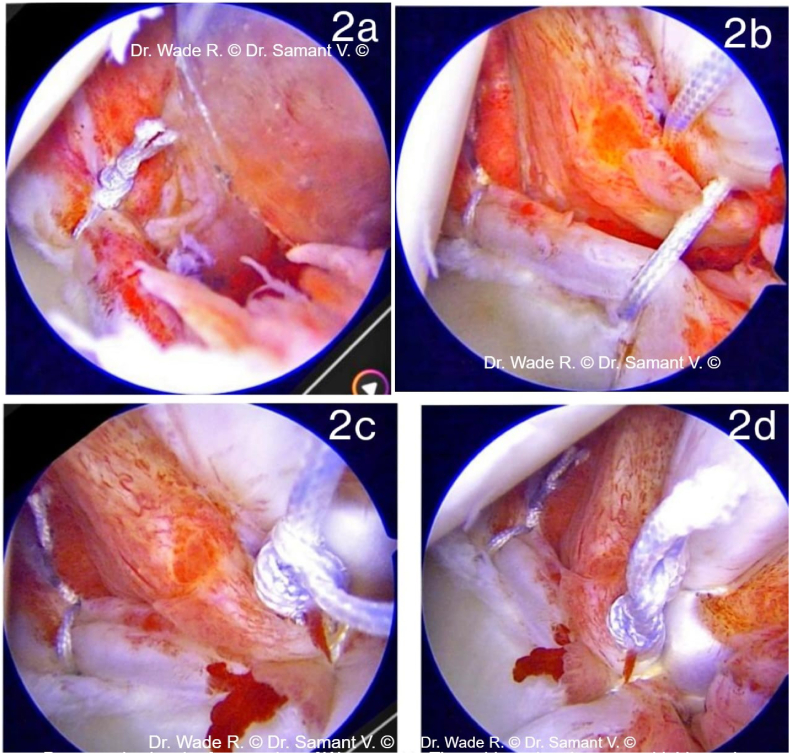
2.2.2. Subscapularis augmented bankart repair (see Fig. 2)
Fig. 2.
2a- First knot for labral repair, 2b-suture passed for Subscapularis augmentation. 2c- Tightening of suture passed for tenodesis. 2d-subscapularis augmentation of capsulo-labral repair.
The basic steps involved preparation of glenoid bed at anteroinferior aspect of glenoid (3–5 o clock for Right shoulder and 7–9 o clock for Left shoulder) followed by capsulo-labral repair using 2–3 suture anchors (single loaded or double loaded) and use of articular portion of subscapularis tendon to augment the repair. The tendon fibres are penetrated using appropriate suture passing device.
2.2.3. Capsulo-labral bankart repair
2-3 Suture anchors (single or double loaded) were used for capsulo-labral repair after preparation of glenoid bed for labral defect like above mentioned positions on glenoid.
Rehabilitation protocol- Similar protocols were followed for both groups. The shoulder was immobilised for 4 weeks with a sling. Post 4th week shoulder pendulum exercises and active assisted range of motion were started. Resistance exercises were initiated at 7 weeks and patient was allowed to carry out professional activity at postoperative 4 months.
2.3. Analysis
Evaluation of the association between categorical variables is done using Fischer's exact test, and for continuous variables is done using the t-test or Mann-Whitney test as appropriate. The assumption of normality is checked by the Shapiro-Wilk test and homogeneity of variances is checked using the Folded F method. p-values less than 0.05 are considered statistically significant. Mean differences or Hodges-Lehmann estimates with 95 % confidence intervals are reported with p-values as appropriate. p-values and confidence intervals are adjusted using the Bonferroni correction for multiple comparisons. Analysis is done using SAS 9.4 (SAS Institute Inc., Cary, NC)
3. Results
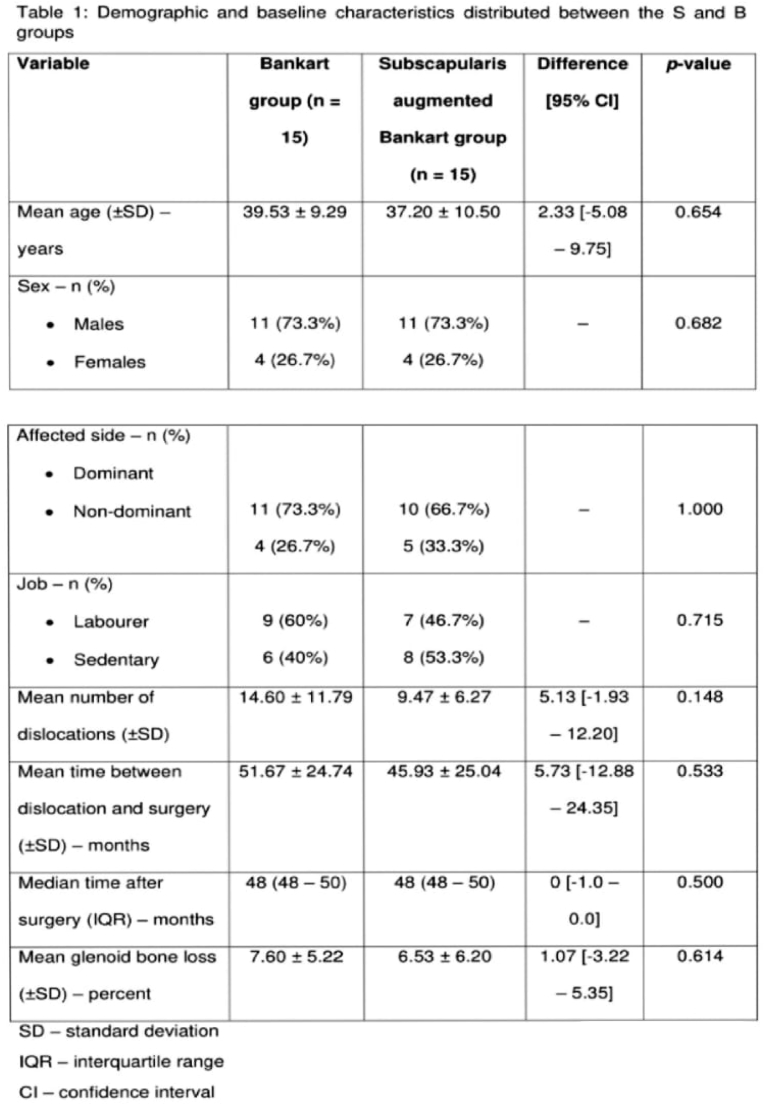
The average follow-up period at which functional score were recorded post-surgery was 48 months for both the groups. For SB and CB respectively, the average age was 37.2 years and 39.5, both groups had 4 female participants each while 10 SB and 11 CB participants had shoulder of their dominant limb involved. For the SB group, 7 patients were involved in labour for livelihood while 8 followed a sedentary or low shoulder activity job profile. Similarly, 9 patients from CB group were involved in labour while rest 6 followed a sedentary routine. Hence adequate matching was ensured between both the groups ( (See Fig. 4).
Fig. 4.
Demographic and baseline characteristics distributed between the S and B groups.
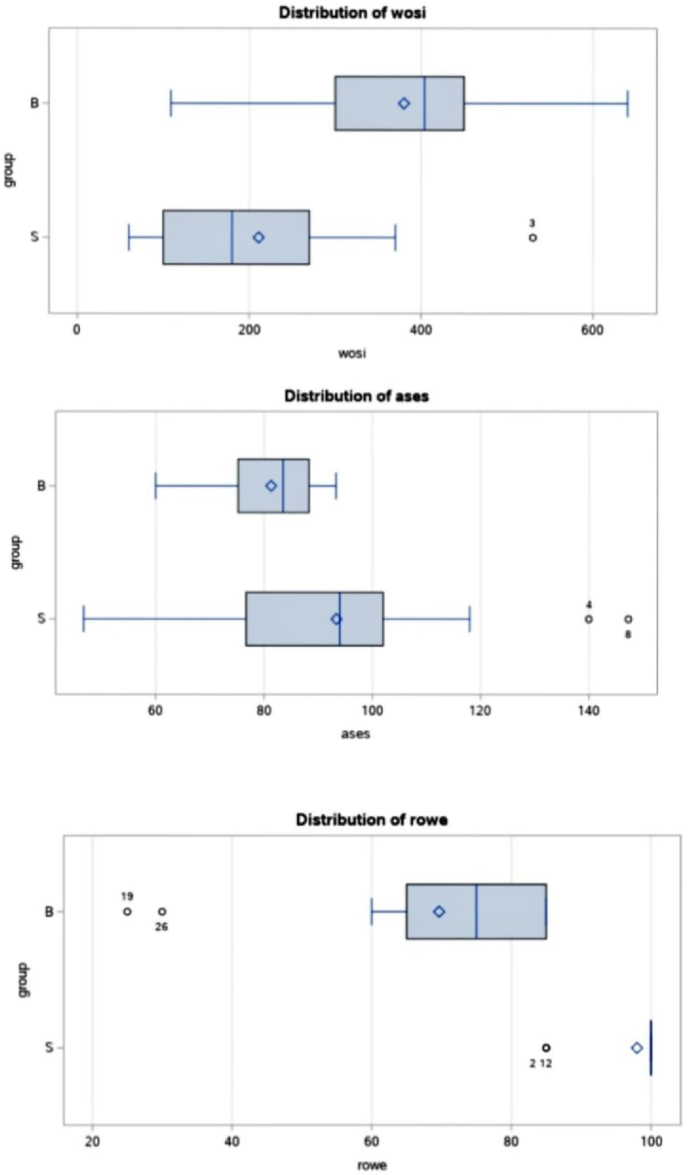
Impact of subscapularis augmented Bankart procedure versus traditional Bankart procedure on orthopaedic scores: The effect of the two procedures on different scores are presented in Table 1 at the end. Patients in the CB group had higher WOSI and WOSI-L scores than patients in the SB group. Patients in the SB group had lower ROWE, ROWE-F, and ROWE-P scores than patients in the CB group.
Table 1.
Impact of the S and B procedures on orthopaedic shoulder scores.
| Score | Bankart group (n = 15) | Subscapularis augmented Bankart group (n = 15) | Difference [Adjusted 95 % CI] (B–S scores) | Statistic | Adjusted p-value |
|---|---|---|---|---|---|
| Mean WOSI scores (±SD) | 379.9 ± 136.2 | 211.0 ± 125.4 | 168.9 [19.01–318.9] | 3.53 | 0.018* |
| Median WOSI P scores (IQR) | 90 (60–120) | 60 (40–90) | 30 (-30–70) | 192.00 | 1.000 |
| Mean WOSI S scores (±SD) | 119.5 ± 49.83 | 63.67 ± 48.49 | 55.8 [-0.50–112.1] | 3.11 | 0.056 |
| Median WOSI L scores (IQR) | 100 (70–120) | 40 (10–50) | 70 (28–104) | 138.00 | 0.007** |
| Mean WOSI E scores (±SD) | 73.07 ± 34.97 | 44.00 ± 30.66 | 29.07 [-8.60–66.73] | 2.42 | 0.289 |
| Mean ASES scores (±SD) | 81.31 ± 10.16 | 93.39 ± 28.29 | −12.09 [-36.43–12.25] | −1.56 | 1.00 |
| Median ASES P scores (IQR) | 40 (35–45) | 50 (30–60) | −5 (-25–15) | 276.50 | 0.997 |
| Median ASES ADL scores (IQR) | 41.6 (38.6–46.7) | 46.7 (45.0–50) | −5.4 (−12.1–1.2) | 289.50 | 0.334 |
| Median ROWE scores (IQR) | 75 (65–85) | 100 (100–100) | −25 (−15–−35) | 341.00 | <.001*** |
| Median ROWE F scores (IQR) | 35 (35–35) | 50 (50–50) | −15 (−15–15) | 332.00 | <.001*** |
| Median ROWE P scores (IQR) | 55, 6, 7, 8, 9, 10 | 1010 | −5 (0–5) | 292.50 | 0.042* |
| Median ROWE S scores (IQR) | 30 (1–30) | 30 (30–30) | 0 (-15–0) | 277.50 | 0.163 |
| Median ROWE M scores (IQR) | 55, 6, 7, 8, 9, 10 | 1010 | 0 (-5–0) | 277.5 | 0.169 |
SD – standard deviation.
IQR – interquartile range.
CI – confidence interval.
*p < 0.05, **p < 0.01, ***p < 0.001.
4. Discussion
Patients managed with subscapularis augmentation performed better in all three scoring systems however the difference was not significant for ASES scores (See Fig. 3). For the objective ROWE score (p < 0.01) and the subjective WOSI index (p < 0.018), the difference was significant and SB group had superior shoulder activity and scores after a minimum 2-year postoperative follow up.
Fig. 3.
Boxplot of WOSI/ASES/ROWE score distribution by procedure.
The mean time between event of first dislocation and surgery was 45.9 months for SB group with an average of 9.47 dislocations while it was 51.67 months for CB group with a mean number of 14.60 dislocations prior to surgery. This is very well longer than the average time taken by professional athletes to seek surgical intervention which in a study by Domos et al. was 7.2/8.6 weeks for 40 high collision athletes.3 This shows that a delay in undergoing surgical intervention can be regularly expected in non-athlete populations when compared to athletes with recurrent shoulder instability. Hence the augmentation may be justifiable in these shoulders that become pathologically lax over time.
Among the SB group the average preoperative Glenoid bone loss was 6.5 % with a maximum GBL for a patient undergoing subscapularis augmented repair being 18 %. For CB cohort the average GBL was 7.6% with maximum value for the same being 20 %. In total, 5 participants from each group i.e. 10 patients had a GBL in the grey area of 10%–20 %. The average ROWE score for these 5 + 5 individuals was higher for the SB group 94 in comparison to CB group 67. These findings are like that of Maoitti et al. in his study on 110 patients with GBL% <25 % where it was concluded that subscapularis augmented repair can be reliably used to restore joint stability with moderate GBL.4
While considering postoperative shoulder pain, the median ROWE-P (pain) score was better for SB group [10/10] when compared to CB group [5/10]. Using components of the WOSI score, patients under SB group were more comfortable with physical symptoms of their shoulder [WOSI-P average 60/1000] and were more likely to continue their recreational sports activity [WOSI- sports for SB 63.7 and CB 119.5]. However, the difference was not statistically significant. SB group patients also scored better in Lifestyle and Emotion sections of WOSI implying a better acceptability of operated shoulder among SB group patients when compared to CB with difference being statistically significant. We believe that the return of anteriorly lax soft tissue envelope to its former tautness by subscapularis tenodesis during SB Bankart repair is responsible for better rehabilitation and performance of shoulders that are operated using this technique. As none of the participant involved in the study had an episode of re-dislocation post-surgery or needed any revision surgery, it can be concluded that both surgical options have been reliable to restore shoulder stability effectively, however better rehabilitation, better pain relief scores and overall comfort with a shoulder which was once dislocating habitually is seen with subscapularis augmentation. However further research to support this hypothesis is warranted. An important reason for zero recurrence of instability post-surgery in all 30 patients may be since the study involves non-athlete patients who are not prone to repeated stresses or dislocating forces.
Maotti in his two separate studies4,7 on athletes concluded that a minimal restriction of external rotation in adducted and 90-degree abducted position is seen with Subscapularis augmented repairs. In our study, none of the 15 patients had any restriction in range of shoulder movements [ROWE-M (MOTION) score of 10] during physical examination for SB group. In the CB group, two patients had severe restriction of abduction and rotations (ROWE-M score 0) while 4 patients had moderate restriction of motion arc not severely affecting their activities of daily living and occupation (ROWE-M score 5). In non-athlete population, rehabilitation is slower and weaker than in athletes, and subscapularis augmentation may be considered by some as an overtreatment in these. However similar results of shoulder range in SB group are promising as it supports the belief of a more confident shoulder after subscapularis augmentation leading to better rehabilitation and hence better gain of normal range even in low activity level patients.
In previous studies, Domos3 compared the results of subscapularis augmented repair in GBL<25 % vs Latarjet procedure in collision sport athletes and found the prior to be equally effective in return to sports and prevention of re-dislocations. Maiotti8 confirmed promising results in his study of subscapularis augmented repair in 397 athletes with shoulder hyperlaxity. None of the studies discussed the efficacy, acceptability of SB approach in moderate activity patients. We observed superior pain relief, rehabilitation and return to daily life with subscapularis augmentation for anterior recurrent dislocations of shoulder in these patients. This implies broader applicability and routine use of this physiologic technique irrespective of patient's activity for any glenoid bone defect <20–25 % as its combination with remplissage is an effective ‘trident’ solution for the triad of shoulder destabilising lesions seen in chronic shoulder dislocations.
Our study has several limitations-the study involves 30 patients who have been assessed at a mean post operative duration of 2 years. Further studies are needed to evaluate the technique under study and long-term complications that may arise if any. It is a retrospective study which is influenced by recall and observer bias. The study does not involve sportsmen who are more prone to surgical failure which is reflected in zero recurrence observed in all study participants.
5. Conclusion
Subscapularis augmented Bankart repair is an effective surgical technique for managing recurrent anterior glenohumeral instability with GBL <20 % in low to moderate activity level patients. It is associated with minimal restriction of shoulder range, better pain relief, better acceptability and smoother return to daily living and occupation and can be considered as a routine for every patient with GBL<20 %.
Funding declaration
We have not received any funding/financial aid/research grant for this manuscript.
Declaration of competing interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Acknowledgements
Concept and Design – Dr. Wade R; Administrative support-none; Collection and assembly of data- Dr. Samant V; Data analysis and interpretation- Dr. Samant V; Manuscript writing- Dr. Samant V; Final approval- All authors.
Contributor Information
Vinay Samant, Email: samantorthopaedics@gmail.com.
Roshan Wade, Email: roshanwade@gmail.com.
References
- 1.Burkhart S.S., De Beer J.F. Traumatic glenohumeral bone defects and their relationship to failure of Arthroscopic Bankart repairs. Arthrosc J Arthrosc Relat Surg. 2000;16(7):677–694. doi: 10.1053/jars.2000.17715. [DOI] [PubMed] [Google Scholar]
- 2.Wolf E.M., Arianjam A. Hill-Sachs remplissage, an arthroscopic solution for the engaging hill-sachs lesion: 2- to 10-year follow-up and incidence of recurrence. J Shoulder Elbow Surg. 2014;23(6):814–820. doi: 10.1016/j.jse.2013.09.009. [DOI] [PubMed] [Google Scholar]
- 3.Domos P., Ascione F., Wallace A.L. Arthroscopic Bankart repair with remplissage for non-engaging hill-sachs lesion in professional collision athletes. Shoulder Elbow. 2017;11(1):17–25. doi: 10.1177/1758573217728414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maiotti M., Massoni C., Russo R., Schroter S., Zanini A., Bianchedi D. Arthroscopic subscapularis augmentation of Bankart Repair in chronic anterior shoulder instability with bone loss less than 25% and capsular deficiency: clinical multicenter study. Arthrosc J Arthrosc Relat Surg. 2017;33(5):902–909. doi: 10.1016/j.arthro.2016.09.008. [DOI] [PubMed] [Google Scholar]
- 5.Symeonides PanP. The significance of the subscapularis muscle in the pathogenesis of recurrent anterior dislocation of the shoulder. The Journal of Bone and Joint Surgery British. 1972;54-B(3):476–483. [PubMed] [Google Scholar]
- 6.Johnson L.L. Mosby; St. Louis: 1986. Arthroscopic Surgery: Principle and Practice; pp. 1420–1424. (Chapter 15) [Google Scholar]
- 7.Maiotti M, Massoni C. Arthroscopic augmentation with subscapularis tendon in anterior shoulder instability with capsulolabral deficiency [Internet]. U.S. National Library of Medicine; [cited 2023 Oct 17]. Available from: https://pubmed.ncbi.nlm.nih.gov/24266004/. [DOI] [PMC free article] [PubMed]
- 8.Maiotti M., Russo R., Zanini A., et al. https://pubmed.ncbi.nlm.nih.gov/33581299/ Bankart repair with subscapularis augmentation in athletes with shoulder Hyperlaxity [Internet]. U.S. National Library of Medicine; [cited 2023 Aug 24]. Available from: [DOI] [PubMed]
- 9.Maiotti M;Russo R;Zanini A;Schröter S;Massoni C;Bianchedi D; Arthroscopic Bankart Repair and Subscapularis augmentation: An alternative technique treating anterior shoulder instability with bone loss [Internet]. U.S. National Library of Medicine; [cited 2023 Aug 24]. Available from: https://pubmed.ncbi.nlm.nih.gov/26613984/. [DOI] [PubMed]
- 10.Russo R;Della Rotonda G;Cautiero F;Ciccarelli M;Maiotti M;Massoni C;Di Pietto F;Zappia M; Arthroscopic Bankart repair associated with subscapularis augmentation (ASA) versus open latarjet to treat recurrent anterior shoulder instability with moderate glenoid bone loss: Clinical comparison of two series [Internet]. U.S. National Library of Medicine; [cited 2023 Aug 24]. Available from: https://pubmed.ncbi.nlm.nih.gov/28004306/. [DOI] [PubMed]