Abstract
Background & Aims:
Liver transplantation for alcohol-related liver disease (ARLD) has increased. We examined temporal trends in ARLD listing practices by neighborhood deprivation and evaluated the impact of neighborhood deprivation on waitlist mortality.
Methods:
We included all adults>18 years listed 2008–2019 in the UNOS registry. Our primary exposure was the neighborhood socioeconomic deprivation index based on patients’ listing zip code. We determined temporal trends in an ARLD listing diagnosis. We modeled ARLD listing diagnosis using logistic regression and waitlist mortality using Cox proportional hazards models.
Results:
The waitlist contained an increasing proportion of patients listed with ARLD over the study period; however, this rate increased the least for patients from the most deprived tertile (p<0.001). Patients from the most deprived tertile were the least likely to be listed with ARLD (OR 0.97, 95CI 0.95 – 0.98). In our adjusted model, patients from the most deprived tertile had an increased hazard of waitlist mortality (OR 1.10, 95CI 1.06–1.14).
Conclusion:
Neighborhood deprivation was associated with a decreased likelihood of being listed with ARLD, suggesting that transplant for ARLD is inequitably available. The increased mortality associated with neighborhood deprivation demands future work to uncover the underlying reasons for this disparity.
Keywords: socioeconomic deprivation, cirrhosis, outcomes, waitlist, liver transplant
INTRODUCTION
The social determinants of health are “conditions in the environments where people are born, live, learn, work, play, worship, and age that affect a wide range of health.”1,2 Neighborhood and community-level measures of socioeconomic status have been linked to adverse health outcomes in adults and children undergoing liver transplant.3,4 For example, previous research has demonstrated that those with end-stage liver disease who live further from a transplant center are less likely to be listed for transplant.5 Patients living in neighborhoods with more resources may have improved health outcomes because of several mediating pathways: social supports – such as the medical knowledge of your community – may impact when disease, specifically a decompensating event, is identified; access to care – such as transportation, distance, and telehealth – may impact the ability to seek care earlier; access to clinical supports – such as substance abuse treatment, nutrition, physical therapy, and occupational therapy – may impact the ability of our patients to rehabilitate, influencing those who are referred for evaluation and those who can maintain the clinical reserve necessary to undergo liver transplant. However, to date, it has been challenging to capture with granularity how environmental context impacts transplant outcomes.
Previous research in adult liver transplant candidates has shown on a county-level or a community type-level (i.e., urban, rural, suburban) that patients from neighborhoods with lower socioeconomic status have worse waitlist and post-liver transplant outcomes.6,7 However, county-level studies lack the granularity that neighborhood-level studies offer. Consider, for example, in San Francisco County, the median household income in the wealthiest zip code is $213,987 but only $46,372 in the poorest. The one study that used zip code level data only included 43% of waitlist registrants and was completed >10 years ago when transplant for alcohol-related liver disease (ARLD) and, more specifically, alcohol-associated hepatitis (AAH) was less common.8,9 This is particularly salient given that lower-income and minoritized patients are at increased risk for harmful drinking patterns. Furthermore, Black patients and those who have ARLD are less likely to be listed for transplant.10–12
Therefore, our objective was to complete a comprehensive, contemporary, and zip code-level assessment of the impact of social adversity on transplant indications and waitlist outcomes using the national transplant registry. To measure social adversity, we used a comprehensive and well-studied index of neighborhood socioeconomic deprivation.3,4,13
METHODS
Study Population and Datasets
All patients listed in the United Network for Organ Sharing/Organ Procurement and Transplantation Network (UNOS/OPTN) registry from January 1st, 2008, through December 1st, 2019, were included in this analysis. Patients less than 18 years old were excluded, as were those who received exception points, including for HCC were excluded. We obtained home zip codes from the UNOS/OPTN. We excluded those with no zip code data (<1%). We linked these data with the deprivation index, a validated metric derived using the U.S. Census Bureau’s 2015 American Community Survey.13 We excluded those with zip codes not found in the deprivation index (<1%).
Primary Exposure
Our primary exposure was the deprivation index. This metric is a marker of neighborhood socioeconomic deprivation.3,4,13 It is a continuous metric, from 0 – 1, with values closer to 1 indicating more-deprived neighborhoods. This metric is a composite of the proportion of residents below the poverty line, inflation-adjusted median household income, the proportion of residents with high school or General Education Development (GED) equivalency, the proportion of residents without health insurance, the proportion of households receiving public assistance income or food stamps or Supplemental Nutrition Assistance Program (SNAP) benefits, and the fraction of houses that are vacant.13 We analyzed the deprivation index as a continuous variable and as a categorical variable by tertile (high, intermediate, and low).
Covariates
Data included sex, age at listing, race, body mass index at listing, listing diagnoses, date of listing, date of removal from the waitlist, reason or removal, transplant date, presence of hepatic encephalopathy, and presence of ascites. The Model for End-Stage Liver Disease with Sodium (MELD-Na) score was calculated using the standard formula using a lower limit of 1 for all variables.14 The lower and upper limits of 6 and 40 were used as standard practice. The distance from the transplant center was defined as the distance from the centroid from a registrant’s zip code to the centroid of the zip code for the closest transplant center.15 Listing diagnoses were grouped into the following diagnostic categories: hepatitis C virus (HCV), hepatitis B virus (HBV), nonalcoholic fatty liver disease (NAFLD), including cryptogenic cirrhosis and nonalcoholic steatohepatitis), ARLD, autoimmune etiologies (including primary biliary cirrhosis, primary sclerosing cholangitis, and autoimmune hepatitis), and other etiologies of cirrhosis (any other listing code that met inclusion criteria).
Trend Analysis
The trend of interest in this study was the proportion of registrants with a listing diagnosis for ARLD or AAH per year. ARLD was defined as a primary listing code of any code from 4215 – 4217 and AAH was defined as a primary listing code of 4217. We determined the percentage of patients listed with either a listing diagnosis of ARLD or AAH by listing year and tertile of deprivation index from 2008 – 2018. We used Cuzick’s extension of the Wilcoxon rank-sum test to compare the trend in the percentage of patients listed for ARLD or AAH per year in three deprivation tertiles. Linear regression provided the percent change per year.
Logistic Regression for an Alcohol-Related Listing Diagnosis
To better characterize who gets listed for transplant with an ARLD diagnosis, we evaluated socio-demographic factors that are associated with being listed for ARLD. Our primary outcome for this was an ARLD listing diagnosis. We utilized logistic regression to model the association between our covariates and our outcome. Given that each transplant center has different listing practices for ARLD, we clustered all our logistic regression analyses on the center. To inform our findings, we tested for the following interactions with deprivation: sex, age, MELDNa score, education status, and insurance status.
Cox Regression for Waitlist Mortality
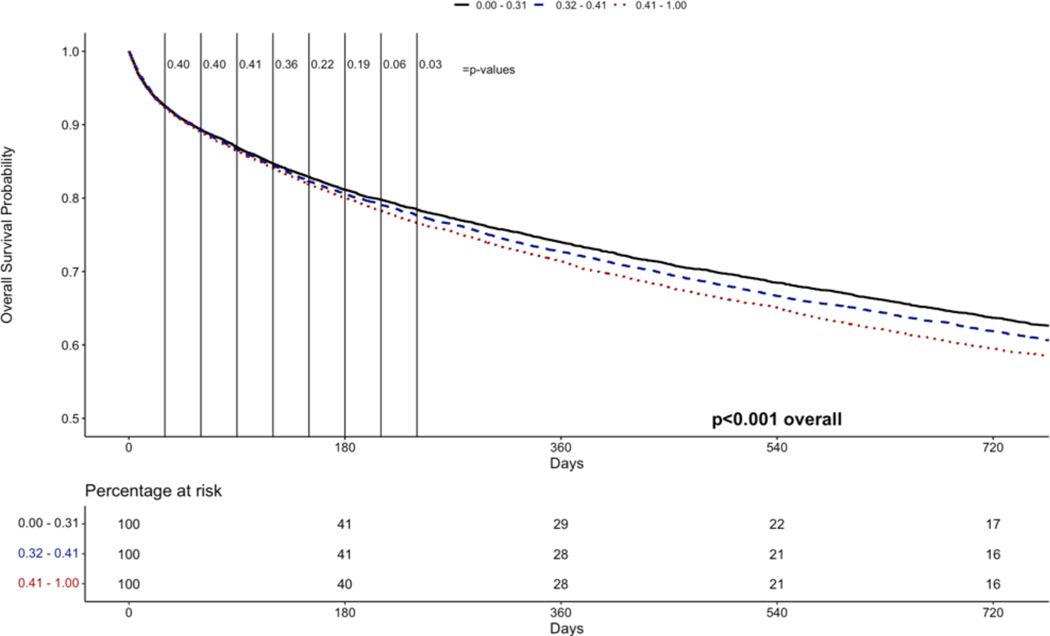
Our outcome of interest for this analysis was waitlist mortality, defined as death or delisting for being too sick for liver transplantation. We chose Cox regression models because we hypothesized that the deprivation index would have a biological impact on outcomes, rather than be an access issue as all patients were already listed for transplant. More specifically, we hypothesized that patients from higher deprivation zip codes would have less access to rehabilitation (e.g., physical therapy, nutrition, substance abuse treatment), making them more susceptible to rapid decompensation. We include competing risk models, treating liver transplant as a competing risk, in the supplemental data. We used Kaplan-Meir methods to visualize these survival data. We performed a series of time-censored survival analyses at 30-day intervals after listing to determine whether there a differences in survival between the tertiles of deprivation index. To understand the impact of deprivation on waitlist outcomes, we tested the following interactions with deprivation: sex, age, MELDNa score, education status, and distance from the transplant center.
Logistic Regression for Receiving a Donor Offer
Our outcome of interest for this analysis was the number of liver transplant offers received. These were obtained using the donor offer file present in the UNOS database. Given that each transplant center has different offer acceptance practices, we clustered all our logistic regression analyses on the center.
Statistical Analysis
Categorical variables were compared between groups by chi-square test. Continuous variables were compared between groups by rank-sum. Unadjusted models were used initially to test the association of the listed covariates (p<0.10). Backward elimination was utilized to remove covariates that were not significant. All covariates with significance p <0.05 were included in multivariate models. Two-sided p-values <0.05 were determined statistically significant. All analyses were performed using RStudio.
This work was supported in part by Health Resources and Services Administration contract 234– 2005-370011C. The content is the responsibility of the authors alone and does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. Government. This study was approved by the IRB at the University of California, San Francisco.
RESULTS
DEMOGRAPHICS
Among the 69,514 waitlist registrants included in this study, we found a median deprivation index of 0.36 (Interquartile Range [IQR] 0.29 – 0.44). To facilitate this analysis, we divided registrants into tertiles representative of their deprivation index. These included 23,264 patients in the high deprivation index (IQR 0.44 – 0.53), 23,264 patients in the intermediate deprivation index (IQR 0.34 – 0.39), and 23,268 in the lowest deprivation index (IQR 0.23 – 0.29). To provide further context, those in the lower deprivation index tertiles, as compared to those in the higher tertiles, had higher median household incomes, higher proportions of non-public insurance, male sex, white race, ARLD, and AAH (Table 1). We found that the metrics of disease severity at listing (e.g., model for end-stage liver disease with serum sodium [MELDNa] score, hepatic encephalopathy status, ascites status) were clinically similar (Table 1).
Table 1.
Demographics by Tertile of Deprivation Index
| Tertile of Deprivation Index | ||||
|---|---|---|---|---|
| <0.32 N = 23,2681 | 0.32 – 0.41 N = 23,2641 | >0.41 N = 23,2641 | p-value | |
| Sex | <0.001 | |||
| Female | 8,712 (37%) | 9,038 (39%) | 9,738 (42%) | |
| Male | 14,556 (63%) | 14,226 (61%) | 13,526 (58%) | |
| Age at listing | 56 (48, 62) | 56 (49, 61) | 55 (48, 61) | <0.001 |
| Self-Identified Race | <0.001 | |||
| Black | 1216 (5%) | 1698 (7%) | 3540 (15%) | |
| Self-Identified Ethnicity | <0.001 | |||
| Non-Hispanic White | 19271 (83%) | 18336 (79%) | 12690 (55%) | |
| Hispanic White | 1577 (7%) | 2362 (10%) | 5877 (25%) | |
| Asian | 968 (4%) | 585 (3%) | 639 (3%) | |
| Other | 1452 (6%) | 1981 (8%) | 4058 (17%) | |
| BMI at listing | 27.7 (24.2, 32.0) | 28.4 (24.7, 32.9) | 28.6 (24.9, 33.1) | <0.001 |
| MELD-Na at listing | 23 (17, 31) | 23 (17, 31) | 23 (17, 31) | 0.008 |
| Etiology | <0.001 | |||
| Alcohol | 5,818 (25%) | 5,327 (23%) | 5,013 (22%) | |
| Autoimmune | 2,935 (13%) | 2,723 (12%) | 2,520 (11%) | |
| HCV | 5,066 (22%) | 5,665 (24%) | 6,113 (26%) | |
| NASH | 4,422 (19%) | 4,916 (21%) | 4,669 (20%) | |
| Other | 5,027 (22%) | 4,633 (20%) | 4,949 (21%) | |
| Encephalopathy | <0.001 | |||
| Hepatic Encephalopathy | 4,783 (21%) | 4,738 (20%) | 5,079 (22%) | |
| No Hepatic Encephalopathy | 18,485 (79%) | 18,526 (80%) | 18,185 (78%) | |
| Ascites | 0.3 | |||
| Ascites | 11,616 (50%) | 11,462 (49%) | 11,578 (50%) | |
| No Ascites | 11,652 (50%) | 11,802 (51%) | 11,686 (50%) | |
| Blood Type | <0.001 | |||
| A | 8,912 (38%) | 8,906 (38%) | 8,314 (36%) | |
| AB | 1,090 (4.7%) | 920 (4.0%) | 817 (3.5%) | |
| B | 2,987 (13%) | 2,841 (12%) | 2,856 (12%) | |
| O | 10,279 (44%) | 10,597 (46%) | 11,277 (48%) | |
| Distance from Transplant Center | 25 (14, 57) | 50 (18, 110) | 43 (10, 116) | <0.001 |
| Median Household Income (Dollars) | 89,460 (76,398, 106,241) | 60,245 (53,050, 68,852) | 44,926 (38,183, 52,330) | <0.001 |
| Deprivation Index | 0.27 (0.23, 0.29) | 0.36 (0.34, 0.39) | 0.47 (0.44, 0.53) | <0.001 |
| Insurance Status | <0.001 | |||
| Other | 273 (1.2%) | 181 (0.8%) | 263 (1.1%) | |
| Private | 14,967 (64%) | 13,034 (56%) | 10,730 (46%) | |
| Public | 8,028 (35%) | 10,049 (43%) | 12,271 (53%) | |
| Alcohol Associated Hepatitis | <0.001 | |||
| Alcohol Associated Hepatitis | 270 (1.2%) | 211 (0.9%) | 170 (0.7%) | |
| No Alcohol Associated Hepatitis | 22,998 (99%) | 23,053 (99%) | 23,094 (99%) | |
| Education | <0.001 | |||
| Associates | 5,070 (22%) | 3,737 (16%) | 2,657 (11%) | |
| Grad School | 2,359 (10%) | 1,286 (5.5%) | 896 (3.9%) | |
| Grade School | 454 (2.0%) | 836 (3.6%) | 1,993 (8.6%) | |
| High School/GED | 13,664 (59%) | 15,529 (67%) | 15,634 (67%) | |
| None | 43 (0.2%) | 44 (0.2%) | 119 (0.5%) | |
| Unknown | 1,678 (7.2%) | 1,832 (7.9%) | 1,965 (8.4%) | |
| Days on Waiting List | 112 (17, 449) | 104 (17, 433) | 101 (15, 421) | <0.001 |
| Waitlist Outcome | <0.001 | |||
| Death/Too Sick | 5,829 (25%) | 5,953 (26%) | 6,167 (27%) | |
| Transplant | 12,243 (53%) | 12,652 (54%) | 12,700 (55%) | |
| Waiting | 5,196 (22%) | 4,659 (20%) | 4,397 (19%) | |
n (%); Median (IQR)
Pearson’s Chi-squared test; Kruskal-Wallis rank sum test
BMI: body mass index; MELD-Na: Model for End-Stage Liver Disease – Sodium; GED: General Educational Development
Legend: Hepatitis C (HCV); Non-alcoholic steatohepatitis (NASH)
TRENDS BY TERTILE OF SOCIOECONOMIC STATUS
Next, we wanted to determine the impact of deprivation index tertiles on the adoption of liver transplant for ARLD and AAH. For each tertile of deprivation, the utilization of liver transplant for ARLD is increasing: High; β = 0.97% per year, p<0.001; Intermediate: β = 0.75% per year, p<0.001; Low: β = 0.66% per year, p<0.001. However, we found these trends were increasing the least in those in the highest deprivation index tertiles (p<0.001) (Figure 1). We found that for each tertile the utilization of liver transplant for AAH is increasing: High; β = 2.82% per year, p<0.001; Intermediate: β = 5.10% per year, p<0.001; Low: β = 4.87% per year, p<0.001. However, we found these trends were increasing the least in those in the highest deprivation index tertiles (p<0.001) (Figure 2).
Figure 1.
Trends in Percentage of Listings for Alcohol-Related Listing Diagnosis by Tertile of Deprivation Index
Figure 2.
Trends in Percentage of Listings for Alcohol Associated Hepatitis Listing Diagnosis by Tertile of Deprivation Index
LOGISTIC REGRESSION FOR ODDS OF BEING LISTED WITH AN ALCOHOL-RELATED DIAGNOSIS
Given these trends, we next completed a logistic regression analysis clustered on center to determine the factors associated with an ARLD listing. We describe the factors associated with a listing diagnosis of ARLD in Table 2. Compared to the lowest deprivation index tertile, those in the intermediate tertile (OR 0.98, 95CI 0.97 – 0.99) and the high tertile (OR 0.97, 95CI 0.95 – 0.98) were less likely to be listed with an ARLD diagnosis (Table 2). When treated as a continuous variable, the deprivation index was significantly associated with a lower risk of an ARLD listing diagnosis (OR 0.99 per 0.1 points, 95CI 0.98 – 0.99). In the final multivariate model, after clustering on center and adjusting for confounders, as compared to the low deprivation index tertile, patients in the intermediate tertile (adjusted OR [aOR] 0.98, 95CI 0.97 – 0.99) and the high tertile (aOR 0.97, 95CI 0.96 – 0.98) were less likely to have an ARLD listing diagnosis (Table 2). Similarly, after clustering on center and adjusting for confounders, higher deprivation, as a continuous variable, was significantly associated with a lower odds of an ARLD listing diagnosis (aOR 0.99 per 0.1, 95CI 0.98 – 0.99). In our models testing interactions, we found that: 1) Compared to women, men from higher deprivation neighborhoods were more likely to have an ARLD diagnosis (aOR 1.01 per 0.1 points, 95CI 1.00 – 1.02). 2) Patients from more deprived neighborhoods with higher MELDNa scores were less likely to have an ARLD diagnosis (aOR 0.99 per 0.1 deprivation index points and 10 MELDNa points, 95CI 0.98 – 0.99); 3) Patients from higher deprivation index neighborhoods with private insurance were more likely to have an ARLD diagnosis than those from higher deprivation index neighborhoods with public insurance (aHR 1.01 per 0.1 deprivation index points and private insurance, 95CI 1.00 – 1.01).
Table 2.
Logistic Regression for the Odds of an Alcohol-Related Listing Diagnosis
| Univariable | Multivariable | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| OR | 95% CI | p-value | aOR | 95% CI | p-value | |
|
Tertile of Deprivation Index Low |
- | - | - | - | - | - |
| Intermediate | 0.99 | 0.99 – 1.00 | <0.001 | 0.98 | 0.97 – 0.99 | <0.001 |
| High | 0.97 | 0.95 – 0.98 | <0.001 | 0.97 | 0.96 – 0.98 | <0.001 |
| Self-identified White Race | 1.08 | 1.07 – 1.09 | <0.001 | 1.08 | 1.07 – 1.09 | <0.001 |
| Age per 10 years | 0.99 | 0.99 – 1.00 | <0.001 | 0.99 | 0.99 – 1.00 | <0.001 |
| Male sex | 1.06 | 1.05 – 1.07 | <0.001 | 1.06 | 1.05 – 1.06 | <0.001 |
| Body Mass Index per kg/m2 | 1.00 | 1.00 – 1.00 | <0.001 | |||
| MELDNa per 10 points | 1.03 | 1.03 – 1.04 | <0.001 | 1.03 | 1.03 – 1.04 | <0.001 |
| No Ascites | 0.99 | 0.98 – 1.00 | 0.13 | |||
| No Hepatic Encephalopathy | 0.99 | 0.98 – 1.00 | 0.22 | |||
|
Insurance Status
Public |
- | - | - | - | - | - |
| Private | 0.99 | 0.99 – 1.00 | 0.11 | 1.00 | 0.99 – 1.01 | 0.29 |
| Other | 0.97 | 0.94 – 1.00 | 0.047 | 0.96 | 0.93 – 0.98 | 0.001 |
|
Education Level High School/GED |
- | - | - | - | - | - |
| Grade School | 1.00 | 0.98 – 1.02 | 0.90 | 0.99 | 0.99 – 1.02 | 0.59 |
| Associates | 1.02 | 1.01 – 1.03 | 0.001 | 0.99 | 1.00 – 1.02 | 0.03 |
| Graduate School | 1.01 | 0.89 – 1.00 | 0.41 | 0.99 | 0.99 – 1.01 | 0.03 |
| None | 0.94 | 0.89 – 1.00 | 0.04 | 0.94 | 0.90 – 1.01 | 0.08 |
| Unknown | 1.00 | 0.98 – 1.02 | 0.98 | 0.99 | 0.98 – 1.01 | 0.72 |
MELD Na: Model for End-stage Liver Disease- Sodium; GED: General Educational Development
COX REGRESSION FOR WAITLIST MORTALITY
There were significant differences in waitlist mortality (High – 26%; Intermediate – 26%; Low – 25%; p<0.001) and receipt of a liver transplant (High – 55%; Intermediate – 54%; Low – 53%; p<0.001) by deprivation index tertile. The factors associated with waitlist mortality in the univariate and multivariate models are included in Table 3. In univariate Cox regression analysis, we found the tertile of deprivation index was associated with waitlist mortality – compared to the lowest tertile, Intermediate: Hazard Ratio (HR) 1.05, 95CI 1.01 – 1.09; High: HR 1.11, 95CI 1.07 – 1.15. When treated as a continuous variable, the deprivation index was significantly associated with waitlist mortality (HR 1.05 per 0.1 points, 95CI 1.03 – 1.06). We demonstrate the Kaplan-Meir survival plots in Figure 3. We performed a series of time-censored analyses and found that beginning at 240 days after listing there was a significant difference in survival between the groups (Figure 3). In multivariate analysis, after adjusting for confounders, we found that the tertile of deprivation index was significantly associated with waitlist mortality: compared to the low tertile, high tertile - adjusted HR [aHR] 1.12, 95CI 1.08 – 1.16; intermediate – aHR 1.07, 95CI 1.03 – 1.11. This was true of the continuous deprivation index (aHR 1.05 per 0.1 points, 95CI 1.03 – 1.06). To investigate further, we found a significant interaction between the index and distance from the transplant center; patients living in higher deprivation neighborhoods had increasing rates of waitlist mortality the further they lived from a center (aHR 1.01 per 0.1 deprivation index and 100 miles, 95CI 1.00 – 1.02). We found no interactions between the deprivation index and insurance status and education status (p>0.05 for both interaction terms).
Table 3.
Cox Regression for the Hazard of Waitlist Mortality
| Univariable | Multivariable | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| HR | 95% CI | p-value | aHR | 95% CI | p-value | |
|
Tertile of Deprivation Index Low |
- | - | - | - | - | - |
| Intermediate | 1.05 | 1.01 – 1.09 | 0.008 | 1.06 | 1.02 – 1.10 | 0.002 |
| High | 1.11 | 1.07 – 1.15 | <0.001 | 1.10 | 1.06 – 1.14 | <0.001 |
| Self-identified White Race | 0.84 | 0.79 – 0.88 | <0.001 | |||
| Age per 1 years | 1.02 | 1.02 – 1.03 | <0.001 | 1.03 | 1.03 – 1.03 | <0.001 |
| Male sex | 0.89 | 0.86 – 0.92 | <0.001 | 0.92 | 0.89 – 0.94 | <0.001 |
|
Body Mass Index per kg/m2 <24.6 |
- | - | - | - | - | - |
| 24.6 – 28.2 | 1.08 | 1.04 – 1.13 | <0.001 | 0.93 | 0.89 – 0.97 | <0.001 |
| 28.2 – 32.7 | 0.94 | 0.90 – 0.98 | 0.002 | 0.92 | 0.89 – 0.96 | <0.001 |
| >32.7 | 0.97 | 0.93 – 1.01 | 0.16 | 1.02 | 10.98 – 1.06 | 0.32 |
| MELDNa per 1 point | 1.12 | 1.12 – 1.13 | <0.001 | 1.12 | 1.12 – 1.13 | <0.001 |
| No Ascites | 0.61 | 0.59 – 0.63 | <0.001 | |||
| No Hepatic Encephalopathy | 0.29 | 0.28 – 0.30 | <0.001 | 0.40 | 0.38 – 0.41 | <0.001 |
|
Insurance Status Public |
- | - | - | - | - | - |
| Private | 1.31 | 1.27 – 1.35 | <0.001 | 1.15 | 1.12 – 1.19 | <0.001 |
| Other | 1.68 | -1.48 – 1.90 | <0.001 | 1.63 | 1.41 – 1.88 | <0.001 |
|
Education Status High School/GED |
- | - | - | - | - | - |
| Grade School | 1.21 | 1.14 – 1.29 | <0.001 | 1.03 | 0.96 – 1.09 | 0.44 |
| Associates | 0.88 | 0.84 – 0.92 | <0.001 | 0.89 | 0.86 – 0.93 | <0.001 |
| Graduate School | 0.83 | 0.77 – 0.88 | <0.001 | 0.86 | 0.81 – 0.92 | <0.001 |
| None | 1.40 | 1.12 – 1.78 | 0.004 | 0.89 | 0.70 – 1.13 | 0.35 |
| Unknown | 1.33 | 1.27 – 1.41 | <0.001 | 1.27 | 1.21 – 1.34 | <0.001 |
| Distance per 100 miles | 0.99 | 0.99 – 1.00 | 0.09 | |||
|
Blood Type A |
- | - | - | - | - | - |
| AB | 1.01 | 0.97 – 1.04 | 0.74 | 1.01 | 0.98 – 1.04 | 0.56 |
| B | 0.78 | 0.71 – 0.86 | <0.001 | 0.97 | 0.88 – 1.08 | 0.61 |
| O | 0.88 | 0.83 – 0.92 | <0.001 | 0.93 | 0.89 – 0.98 | 0.006 |
MELD Na: Model for End-stage Liver Disease- Sodium; GED: General Educational Development
Figure 3.
Kaplan-Meir Plot of Waitlist Mortality by Tertile of Deprivation Index
LOGISTIC REGRESSION FOR RECEIVING A DONOR OFFER
We found no clinical difference between deprivation index tertiles and the number of offers received: High – 4 offers (IQR 2 – 10); Intermediate – 4 offers (2 – 10); Low – 4 offers (2 – 10). In univariate analyses clustered on center, neither the continuous deprivation index (OR 1.23, 95CI 0.93 – 1.63) nor tertiles (as compared to the lowest tertile, intermediate tertile OR 1.27 (95CI 0.79 – 2.02) and the high tertile OR 1.54 (95CI 0.77 – 3.08) were associated with the number of liver transplant offers received. For each of these analyses, the p-value was >0.1 and therefore multivariate models were not pursued.
DISCUSSION
This study evaluated the association of neighborhood material economic deprivation with the demographics of waitlist registrants and waitlist outcomes. We highlight several key findings from our work. First, demographic and clinical parameters vary by deprivation for waitlist registrants – registrants from higher deprivation neighborhoods are more likely to identify as Black, to be female, and less likely to have an ARLD listing diagnosis. Second, it appears that there has been a greater utilization of liver transplant for ARLD and AAH among patients from lower deprivation neighborhoods compared to those from higher deprivation neighborhoods. Third, deprivation is associated with waitlist mortality; for each 0.1 increase in the deprivation index, we saw a 5% increase in the rate of waitlist mortality. Finally, the neighborhood deprivation did not impact their odds of receiving an offer for a liver transplant, suggesting that a decrease in access is not driving the increased risk of waitlist mortality.
Why would neighborhood deprivation impact the sociodemographics of the waitlist registrant? We hypothesize that there are factors intrinsic to the lower deprivation index neighborhoods that are driving the differences in sociodemographics by deprivation seen in this study. For example, because of historically racist policies (i.e., red-lining), Black patients are more likely to live in socioeconomically deprived neighborhoods; because of limited access to nutrient-dense foods and a more sedentary lifestyle, residents of lower deprivation index neighborhoods have a greater burden of obesity; because of limited access to finances, residents of lower deprivation index neighborhoods are less likely to be insured. However, what is not clear is why there was a greater proportion of women from high deprivation neighborhoods compared to the low deprivation neighborhoods. Future studies should investigate why men from higher deprivation index neighborhoods are less likely to be listed for a liver transplant – this may be related to behavior, means, or a systemic bias, but this could not be adequately addressed in this dataset.
Why would neighborhood deprivation impact transplant indication? Specifically, patients with ARLD and AAH were more likely to be from lower deprivation neighborhoods. We highlight in adjusted analyses that compared to the lowest deprivation tertile, both the intermediate deprivation index tertile and high deprivation index tertiles were less likely to be listed with an ARLD listing diagnosis even after adjusting for race and individual socioeconomic status (SES) (e.g., insurance and education level). Although equivocal, some studies suggest that substance abuse is higher in socioeconomically deprived patients, which, if true, would make this finding counterintuitive.10 We hypothesize that this may reflect several factors. First, patients from higher deprivation neighborhoods may have lower access to alcohol rehabilitation and/or the social supports needed to pursue liver transplant safely for ARLD. As a result, these patients are less likely to be referred and/or listed for a liver transplant. Second, patients from higher deprivation index zip codes are more likely to have public insurance. Previous studies have demonstrated that restrictive Medicaid policies for liver transplant for ARLD have led to a lower proportion of liver transplants for this indication.16 Our findings support this previous study: compared to patients with public insurance, those with private insurance were more likely to be listed with an ARLD at higher deprivation indices. That being said, even after adjusting for insurance status in the final multivariate model, higher deprivation index zip codes were associated with lower odds of listing with an ARLD diagnosis—suggesting that the environment, rather than deprivation serving as a surrogate for individual SES, is contributing to these findings. Finally, one must consider interpersonal racism – previous studies have demonstrated that Blacks and patients with ARLD were the least likely to be referred for liver transplantation – and it is possible that such interpersonal racism and bias contribute to these socioeconomic disparities.11,12
Why is there higher waitlist mortality among liver transplant candidates from higher deprivation index zip codes? When treated as a continuous variable, the deprivation index was significantly associated with waitlist mortality (sHR 1.05 per 0.1 points, 95CI 1.03 – 1.06). We hypothesized that this effect was seen for several reasons. First, socioeconomically deprived patients, particularly those who live at a greater distance from the nearest transplant center, may have less access to higher-level care and may not have the resources to present at an earlier time – an effect seen in other studies.6,7,15 We show evidence for this hypothesis through our interaction analysis demonstrating that waitlist registrants from higher deprivation index neighborhoods had an increasing risk for waitlist mortality the further they lived from the nearest transplant center. Second, socioeconomically deprived patients may not have adequate resources (e.g., adequate nutrition, physical therapy) to combat the deleterious impact of decompensated cirrhosis on frailty and sarcopenia. As a result, patients from higher deprivation index neighborhoods might become progressively frailer and more sarcopenic and ultimately delisted for being “too sick” for liver transplantation. Unfortunately, the UNOS/STAR database does not capture quantitative metrics of frailty or sarcopenia, limiting our ability to validate this hypothesis. However, it is notable that the survival analysis became significant beginning only at 240 days after listing— a finding that suggests that patients from lower deprivation zip codes get “sicker” on the waitlist rather than being referred later in their disease progression. Third, we hypothesize that neighborhood deprivation may indicate an increased risk of having material economic hardship (e.g., food insecurity, housing instability) that could interfere with one’s ability to manage their liver disease.17 This study lays the groundwork for future studies to determine how the presence of social needs impacts waitlist outcomes. Finally, we hypothesized that being from a higher deprivation index zip code may impact the number of donor offers a liver transplant registrant may receive. More specifically, patients from higher deprivation index zip codes may not have the means to be called in for a “backup” liver; as a result, they would receive fewer offers and have a greater likelihood of dying on the waitlist. Our analysis of the number of liver offers highlights that this was not the case, that waitlist registrants from each deprivation index tertile received a similar number of liver transplant offers.
Our study has some significant limitations. First, the material neighborhood deprivation index is not an individualized variable. Therefore, ascribing an area-level measure to an individual risks ecological fallacy. However, we found that neighborhood deprivation was associated with listing for ARLD and also waitlist mortality after adjusting for individual SES variables—suggesting a direct contribution of living in these deprived environments that warrants further exploration.17 Second, the geographical resolution of our deprivation index was at the zip code level. In contrast to census tracts, which are fixed in time and drawn for the explicit purpose of population-level studies, zip codes are drawn by the U.S. Postal Service to ensure efficient mail delivery. As such, they can be redrawn to optimize efficiency. Therefore, there are drawbacks to using zip code spatial resolution. However, the zip codes are available and collected by UNOS and allow us to group patients within relatively small geographical units. Third, this study was limited to waitlist registrants. It was out of the scope of this manuscript to investigate the social determinants that impact referral for liver transplant, and these analyses should be planned with different databases that allow such analyses.
Nevertheless, our study highlights that the degree of deprivation of a waitlist registrant’s zip code impacts their demographics and is associated with a greater risk of death. Our data support the application of targeted interventions to ensure the equitable availability of liver transplant for ARLD and to offset the deleterious impact of neighborhood deprivation (e.g., telehealth, nutritional resources, home-based therapies).
Financial Support:
This study was funded by the UCSF Liver Center P30 DK-026743 (Cullaro, Wadhwani, Lai). These funding agencies played no role in the analysis of the data or the preparation of this manuscript. Research reported in this publication was supported by the National Institute of Diabetes and Digestive and Kidney Diseases (K23DK131278 (GC), K23 K23DK132454 (SIW)), and the AASLD Clinical, Translational, and Outcomes Research Award (Cullaro). The content is solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Research Support:
Giuseppe Cullaro - Mallinckrodt Pharmaceuticals. Brian P. Lee - none. Jin Ge - none. Jennifer C. Lai -
Consultant:
Axcella Health, Inc. Sharad I Wadhwani - none.
Abbreviations:
- GED
General Educational Development
- ARLD
alcohol-related liver disease
- AAH
alcohol-associated hepatitis
- UNOS/OPTN
United Network for Organ Sharing/Organ Procurement and Transplantation Network
- SNAP
Supplemental Nutrition Assistance Program
- SES
socioeconomic status
- HCV
hepatitis C virus (HCV)
- HBV
hepatitis B virus (HBV)
- NAFLD
nonalcoholic fatty liver disease
Footnotes
Disclosures: The authors of this manuscript have conflicts of interest to disclose:
Data statement
The data that support the findings of this study are openly available in UNOS STAR File at https://optn.transplant.hrsa.gov/data/view-data-reports/request-data/.
REFERENCES
- 1.Rosenblatt R, Lee H, Liapakis A, et al. Equitable Access to Liver Transplant: Bridging the Gaps in the Social Determinants of Health. Hepatology 2021;74(5):2808–12. [DOI] [PubMed] [Google Scholar]
- 2.Social Determinants of Health - Healthy People 2030 | health.gov [Internet]. [cited 2022 Jan 24];Available from: https://health.gov/healthypeople/objectives-and-data/social-determinants-health [Google Scholar]
- 3.Wadhwani SI, Beck AF, Bucuvalas J, Gottlieb L, Kotagal U, Lai JC. Neighborhood socioeconomic deprivation is associated with worse patient and graft survival following pediatric liver transplantation. Am J Transplant 2020;20(6):1597–605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wadhwani SI, Bucuvalas JC, Brokamp C, et al. Association Between Neighborhood-level Socioeconomic Deprivation and the Medication Level Variability Index for Children Following Liver Transplantation. Transplantation 2020;104(11):2346–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goldberg DS, French B, Forde KA, et al. Association of Distance From a Transplant Center With Access to Waitlist Placement, Receipt of Liver Transplantation, and Survival Among US Veterans. Jama 2014;311(12):1234–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ross K, Patzer RE, Goldberg DS, Lynch RJ. Sociodemographic Determinants of Waitlist and Posttransplant Survival Among End-Stage Liver Disease Patients. Am J Transplant 2017;17(11):2879–89. [DOI] [PubMed] [Google Scholar]
- 7.Axelrod DA, Guidinger MK, Finlayson S, et al. Rates of Solid-Organ Wait-listing, Transplantation, and Survival Among Residents of Rural and Urban Areas. Jama 2008;299(2):202–7. [DOI] [PubMed] [Google Scholar]
- 8.Quillin RC, Wilson GC, Wima K, et al. Neighborhood Level Effects of Socioeconomic Status on Liver Transplant Selection and Recipient Survival. Clin Gastroenterol H 2014;12(11):1934–41. [DOI] [PubMed] [Google Scholar]
- 9.Lee BP, Vittinghoff E, Dodge JL, Cullaro G, Terrault NA. National Trends and Long-term Outcomes of Liver Transplant for Alcohol-Associated Liver Disease in the United States. Jama Intern Med 2019;179(3):340–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grant BF, Chou SP, Saha TD, et al. Prevalence of 12-Month Alcohol Use, High-Risk Drinking, and DSM-IV Alcohol Use Disorder in the United States, 2001–2002 to 2012–2013: Results From the National Epidemiologic Survey on Alcohol and Related Conditions. Jama Psychiat 2017;74(9):911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kanwal F, Hernaez R, Liu Y, et al. Factors Associated With Access to and Receipt of Liver Transplantation in Veterans With End-stage Liver Disease. Jama Intern Med 2021;181(7):949–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rosenblatt R, Wahid N, Halazun KJ, et al. Black Patients Have Unequal Access to Listing for Liver Transplantation in the United States. Hepatology 2021;74(3):1523–32. [DOI] [PubMed] [Google Scholar]
- 13.Brokamp C, Beck AF, Goyal NK, Ryan P, Greenberg JM, Hall ES. Material community deprivation and hospital utilization during the first year of life: an urban population–based cohort study. Ann Epidemiol 2019;30:37–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim WR, Biggins SW, Kremers WK, et al. Hyponatremia and Mortality among Patients on the Liver-Transplant Waiting List. New Engl J Medicine 2008;359(10):1018–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Goldberg DS, Newcomb C, Gilroy R, et al. Increased Distance to a Liver Transplant Center Is Associated With Higher Mortality for Patients With Chronic Liver Failure. Clin Gastroenterol H 2017;15(6):958–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee BP, Vittinghoff E, Pletcher MJ, Dodge JL, Terrault NA. Medicaid Policy and Liver Transplant for Alcohol-Associated Liver Disease. Hepatology 2020;72(1):130–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cottrell EK, Hendricks M, Dambrun K, et al. Comparison of Community-Level and Patient-Level Social Risk Data in a Network of Community Health Centers. Jama Netw Open 2020;3(10):e2016852. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are openly available in UNOS STAR File at https://optn.transplant.hrsa.gov/data/view-data-reports/request-data/.