Abstract
Veterinary personnel are an essential yet often underappreciated workforce, critical for zoonotic disease prevention and response efforts that impact human health. During the early COVID-19 pandemic, the veterinary workforce supported emergency responses by promoting zoonotic disease risk communication, sharing animal health expertise, and boosting laboratory surge capacity against SARS-CoV-2 in animals and people. However, small animal veterinary workers (SAVWs), similar to healthcare workers, faced organizational challenges in providing clinical care to family pets, including those susceptible to SARS-CoV-2. We analyzed a cross-sectional survey of 1,204 SAVWs in the United States to assess veterinary clinic adaptations and their associations with SAVWs' self-perceived readiness, willingness, and ability to respond to the COVID-19 pandemic as a workforce. SAVWs who worked fewer hours than before the pandemic (ready, OR 0.59; willing, OR 0.66; able, OR 0.52) or used personal protective equipment less frequently for protection in the clinic (ready, OR 0.69; willing, OR 0.69; able, OR 0.64) felt less ready, willing, and able to respond to COVID-19. SAVWs working remotely felt less ready (OR 0.46) but not less willing or able to respond to COVID-19. Lastly, SAVWs with dependents felt less ready (OR 0.67) and able (OR 0.49) to respond to COVID-19 than SAVWs without dependents. Our findings highlight the importance of proactively managing work schedules, having access to personal protective equipment, and addressing caregiving concerns to enhance SAVW preparedness and response outcomes. SAVWs are knowledgeable, motivated personnel who should be integrated into local public health emergency preparedness and response plans, supporting a One Health framework that unites multidisciplinary teams to respond to future zoonotic disease threats.
Keywords: Veterinary workforce, Public health preparedness/response, Veterinary clinic operations, Ready Willing Able framework, COVID-19, Pandemic response
Introduction
The COVID-19 pandemic, caused by SARS-CoV-2, rapidly disrupted global health security and stability in early 2020. Unprecedented global disease spread quickly, leading to personal protective equipment (PPE) shortages, overburdened hospitals, and disruptions to medical services in many parts of the world. As of March 10, 2023, when the Johns Hopkins Coronavirus Resource Center stopped collecting data), COVID-19 had infected 677 million people and killed more than 6.9 million people globally.1 At the start of the pandemic in 2020, many US regulatory authorities implemented social distancing recommendations and stay-at-home orders and ceased nonessential services. Although the World Organisation for Animal Health designated veterinary services as essential for disease prevention,2 the small animal veterinary profession struggled to safely maintain clinical operations while treating SARS-CoV-2 susceptible species, such as cats and dogs.3-5
Veterinary services were strongly impacted early in the pandemic. A March 2020 survey by Garcia et al6 found that fewer than 50% of veterinarians felt prepared to manage the complexities of practice operations during COVID-19. In August 2020, the US Centers for Disease Control and Prevention recommended that veterinary clinics prioritize the most urgent cases to preserve PPE and supplies.7 They also recommended virtual and curbside consultations to reduce SARS-CoV-2 virus exposures between clients and veterinary staff.7 Shifts to telehealth and curbside appointments, changes in work schedules, and prioritization of essential procedures affected preventive care, as more veterinary clinics and owners delayed annual pet exams and routine vaccinations. In a 2020 survey, more than 20% of US veterinarians reported a reduction in animal vaccinations due to the pandemic.8 In other parts of the world, such as the United Kingdom, vaccination rates fell for 60% of veterinarians.8 Importantly, vaccinations and other preventive services for animals include rabies vaccination and other services intended for public health benefits to manage human exposure to zoonotic disease threats.
Beyond clinical care, SAVWs also contributed to the pandemic response through surveillance of SARS-COV-2 in dogs and cats, zoonotic disease risk communication, and COVID-19 laboratory surge testing capacity.9,10 SARS-CoV-2 animal-to-human transmission remains uncommon, but the increasing evidence of human-to-animal transmission in wildlife (deer),11 companion (dogs, cats),12 and food animals further highlights the need for ongoing engagement of frontline SAVWs in SARS-CoV-2 prevention, early detection, and response.5 Veterinary workers routinely promote biosecurity, infection control, and risk communication strategies to the public.13 Promoting COVID-19 veterinary workforce adaptations will advance the profession's ability to respond to future public health emergencies (PHEs) affecting people and animals.
There have been many attempts to assess the quality of PHE responses among healthcare workers (HCWs) and allied medical professionals using validated frameworks such as the Ready, Willing, and Able (RWA) framework.14,15 This framework evaluates readiness by an entity's availability for an effective and timely response, willingness by an entity's predisposition to respond favorably, and ability through the collection of knowledge, skills, and competencies.14,16 Weighed equally, these components standardize preparedness assessments across professional disciplines and provide a common language for discussing and evaluating workforce preparedness for PHEs. However, the veterinary workforce has received little evaluation as a public health preparedness and response asset after previous PHEs, such as pandemic (H1N1) influenza, Zika, Ebola, and West Nile virus outbreaks.6,17,18 In addition, the literature on the veterinary workforce's role during PHEs is sparse,10,19 and even fewer researchers have considered the relationship between small animal veterinary clinic adaptations and SAVWs' self-perception of their readiness, willingness, and ability to respond during these stressful events.16,20
Therefore, we evaluated survey responses from SAVWs to (1) describe reported veterinary workplace adaptations in the initial response to the COVID-19 pandemic, (2) evaluate associations between these organizational factors and workers' self-perception of preparedness using an established workforce preparedness and response framework, and (3) develop recommendations to improve small animal veterinary workplace preparedness and response to future PHEs such as pandemics and natural disasters.
Methods
This cross-sectional study used national survey data obtained by the Johns Hopkins Bloomberg School of Public Health Veterinary and Animal Care Workers' Perceived Risk and Willingness to Respond to the Coronavirus Pandemic (CoVET) study, approved by the Johns Hopkins Bloomberg School of Public Health Institutional Review Board (IRB00012854). Following the methodology from Dalton et al,16 which evaluated the veterinary and animal workforce's perceived transmission risk and roles during the COVID-19 pandemic, this secondary data analysis explored the small animal veterinary workplace adaptations and their effects on worker preparedness. Data were exported from the REDCap (Research Electronic Data Capture) platform21 and analyzed using Microsoft Excel and R version 4.1.2 (R Core Team, Vienna, Austria).
Respondent Selection
Small animal veterinary personnel, which included veterinarians, veterinary technicians and assistants, and administrative and support staff, were reached between July 6 and October 25, 2020, using a combination of professional group email lists, social media, and state veterinary boards to distribute the survey. Respondents could anonymously access the survey more than once, but only completed surveys were included in data collection, which minimized duplicate entries. Of the 2,415 individuals who accessed the survey link, 1,577 completed the survey. From this population, we selected a subset of 1,204 survey respondents who specified small animal (dog, cat) medicine as their primary job role for further analysis. Survey responses with missingness on individual variables—changed any workforce adaptations (n=6), schedule changes (n=3), self-reported level of PPE use (n=18), worksite location changes (n=4), facility status to employees (n=9), facility status to public (n=7), readiness to respond (n=14), willingness to respond (n=8), ability to respond (n=12), job title (n=4), gender (n=3), age (n=2), job leader status (n=9), essential employee (n=11), job region (n=43), years of job experience (n=98)—were dropped from respective analyses.
Data Analysis
Data analysis focused on 18 categorical (single or multiple) and ordinal (Likert scale) response questions regarding small animal operational practices and SAVW attitudes toward self-efficacy and response during PHEs. Specifically, the study team examined survey questions assessing demographic data and worker characteristics (job title, years in practice, US Department of Agriculture geographic regions, job leader status, job essential status, gender, age, dependent status), as well as small animal veterinary clinic adaptations, such as changes to SAVW schedules, remote vs onsite work, clinic access by employees and the public, and the frequency in wearing PPE. For this survey, PPE included surgical or cloth face masks, respirators, face shields, goggles, gowns, gloves, or a combination of items. Lastly, questions were asked about SAVWs' perceived risk from person-to-person transmission within the veterinary clinic and self-reported perceptions of their readiness, willingness, and ability to respond to COVID-19. For analysis, administrative (receptionists, office managers) and support (kennel workers) staff were merged into 1 category, and veterinary assistants and technicians were merged into another. Survey responses were aggregated from 10 US Department of Agriculture regions into 6 larger geographic areas: Northeast/Mid-Atlantic, Southeast, North Midwest, South Midwest, Mountain, and Pacific. Supplemental Material: Appendix A (www.liebertpub.com/doi/suppl/10.1089/hs.2023.0041) lists survey questions and responses used for our secondary data analysis.
Exposure variables (with the exception of PPE use) were identified via categorical questions about clinic adaptations. Questions assessing SAVW schedules and locations included “Are you working more or fewer hours compared to prior to the pandemic?” (more hours, fewer hours, same hours/no change in schedule) and “Do you work at a job site or remotely during the pandemic?” (work primarily from home, primarily remotely, even mix of onsite and remotely, work primarily at job site). Questions about restricted access to small animal veterinary clinics included “What is the status of your clinic for employees due to contact precautions during COVID-19?” (closed for all employees, currently open for a select few essential employees, open for all employees, other free-text option), and “What is the status of your clinic for the public (clients/visitors) due to contact precautions during COVID-19?” (closed to the public, currently open for a select/small portion of the public, open to the public, other free-text option). Lastly, data from the question “How often do you use PPE, such as gloves and masks, for protection against COVID-19 exposure?” ranked on a 1 to 5 Likert scale, were dichotomized into less frequent PPE use (less than median score) and more frequent PPE use (greater than or equal to median scores).
Analysis of outcome variables follows the RWA public health preparedness framework, first described by McCabe et al14 and more recently by Dalton et al,16 to evaluate SAVWs' preparedness and responses to the COVID-19 pandemic. Associations between RWA outcomes and organizational factors related to workplace adaptations were examined using chi-square and Fisher exact tests. Logistic regression models were developed to test associations between clinic adaptations (hours worked, PPE use, remote vs onsite work), clinic status (for employees and the public), and SAVWs' RWA response outcomes, adjusting for SAVW demographics and characteristics (job title, years in practice, job region, clinic leadership role, essential worker status, gender, age, responsibility for dependents).
Results
SAVW Study Population Demographics
This study focused on the 1,204 survey respondents who completed the survey and specified small animal (dog, cat) medicine as their primary job role. Respondents surveyed outside the continental United States (including Puerto Rico, Alaska, Hawaii) were excluded from analysis. The largest proportions of surveys originated from the Northeast/Mid-Atlantic (34.0%), followed by North Midwest (19.4%), Southeast (16.1%), and Pacific (12.5%) regions. There was an even distribution between self-reported clinic leadership (53.6%) and nonleaders (46.4%). Most of the survey responses came from respondents who were White (91.5%), female (92.7%), or between 30 and 39 years old (36.4%). Respondents' age and race demographics resembled the general US veterinarian population.22 Twenty-five percent of respondents reported having responsibility for dependents, such as children (20.1%), seniors (2.8%), or other dependents (4.6%).
Clinic Staff Schedules, Telework, and Other Small Animal Clinic Adaptations to COVID-19
Small animal veterinary clinic adaptation associations with RWA outcomes are summarized in the Table. Adaptations differed among SAVWs, such as staff schedule changes, frequency of PPE use, shift to telework operations, and clinic access restrictions for both employees and the public. Supplemental analysis, which evaluated differences between SAVW characteristics and clinic adaptations, can be found in Supplemental Material: Appendix B (www.liebertpub.com/doi/suppl/10.1089/hs.2023.0041). Only 5.3% of surveyed respondents reported no changes to clinic operations during the pandemic. More than half (52.7%) of SAVWs reported working more hours than before the pandemic; a smaller percentage (14.2%) of SAVWs worked fewer hours. Most (74.3%) SAVWs reported using PPE more often for protection against SARS-CoV-2 exposures, and this group had significantly higher self-perceptions of RWA outcomes. SAVWs continued working primarily onsite (95.5%) during the pandemic, and those who worked remotely were significantly less likely to report being ready, willing, or able to respond to COVID-19. Most clinics (78.7%) utilized curbside or telehealth appointments and either kept their clinics closed to the public or remained available only for certain appointments, such as over-the-counter sales and appointments necessitating pet euthanasia. Clinic access restrictions for employees and the public were not significantly associated with greater RWA outcomes for SAVWs.
Table.
Odds Ratios for Small Animal Clinic Adaptations Contributing to Ready, Willing, and Able Preparedness and Response Perceptions During the COVID-19 Pandemic (N=1,204)
| Small Animal Clinic Work Adaptation | Respondents n (%) | Ready to Respond During COVID-19 Pandemic |
Willing to Respond During COVID-19 Pandemic |
Able to Respond During COVID-19 Pandemic |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Low Score | High Score | OR | Low Score | High Score | OR | Low Score | High Score | OR | ||
| Changed any clinic operation | ||||||||||
| Yes | 1,134 (94.2) | 436 | 685 | Ref | 450 | 677 | Ref | 368 | 755 | Ref |
| No | 64 (5.3) | 24 | 40 | 1.06 | 26 | 38 | 0.971 | 21 | 43 | 0.998 |
| Hours worked | ||||||||||
| Same hours/no change | 396 (32.9) | 133 | 258 | Ref | 149 | 246 | Ref | 114 | 277 | Ref |
| Worked more hours | 634 (52.7) | 241 | 385 | 0.824 | 243 | 387 | 0.965 | 195 | 434 | 0.915 |
| Worked fewer hours | 171 (14.2) | 87 | 84 | 0.498a | 85 | 84 | 0.599b | 80 | 90 | 0.463a |
| PPE use for protection | ||||||||||
| PPE used more often for protection | 895 (74.3) | 323 | 564 | Ref | 336 | 554 | Ref | 267 | 619 | Ref |
| PPE used less often for protection | 291 (24.2) | 133 | 154 | 0.663a | 134 | 155 | 0.702b | 118 | 173 | 0.632b |
| Remote vs onsite work | ||||||||||
| Primarily present at work/no change | 1,150 (95.5) | 429 | 708 | Ref | 448 | 695 | Ref | 363 | 777 | Ref |
| Either partially or fully remote work | 50 (4.2) | 30 | 20 | 0.404a | 27 | 23 | 0.549c | 24 | 25 | 0.487c |
| Clinic access restrictions for employees | ||||||||||
| Completely open to employees | 1,131 (94.0) | 427 | 692 | Ref | 449 | 678 | Ref | 363 | 760 | Ref |
| Restricted clinic access to employees | 62 (5.1) | 31 | 30 | 0.597 | 25 | 35 | 0.927 | 23 | 36 | 0.748 |
| Clinic access restrictions for public | ||||||||||
| Completely open to public | 249 (20.7) | 107 | 139 | Ref | 104 | 144 | Ref | 89 | 158 | Ref |
| Restricted clinic access to public | 948 (78.7) | 352 | 586 | 1.282 | 370 | 572 | 1.117 | 299 | 640 | 1.206 |
Notes: RWA outcomes were dichotomized into low (below median) and high (above and equal to median) scores for analyses with chi-square and Fisher exact tests. Some respondents did not answer all the questions. The percentages are calculated using the total study population as the denominator. Due to rounding and missing data, percentages may not add up to 100%.
P<.005; bP<.01; cP<.05. Abbreviations: OR, odds ratio; PPE, personal protective equipment; RWA, Ready, Willing, and Able Framework.
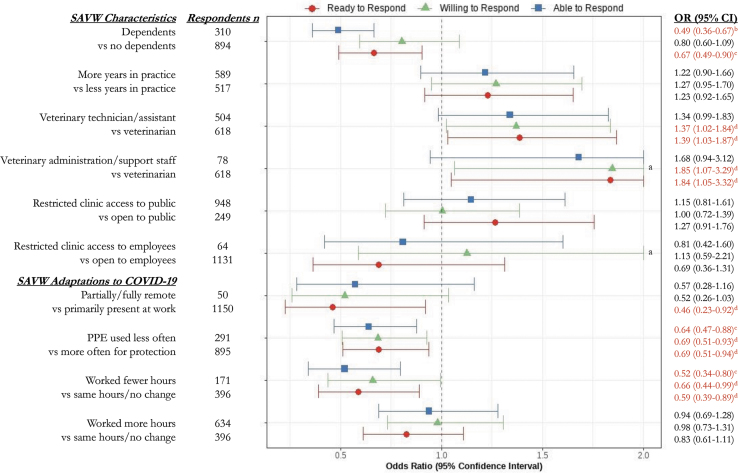
Small Animal Veterinary Workplace Adaptations and Negative RWA Associations
Adjusted associations between workplace adaptations and the odds of high RWA outcomes are summarized in the Figure. SAVWs who worked fewer hours than before the pandemic had lower odds of feeling ready (OR 0.59; 95% CI, 0.39 to 0.89), willing (OR 0.66; 95% CI, 0.44 to 0.99), and able (OR 0.52; 95% CI, 0.34 to 0.80) to respond to COVID-19 compared with SAVWs working the same number of hours before the pandemic. SAVWs who reported using PPE less often for protection against COVID-19 (below the median score) had lower odds of feeling ready (OR 0.69; 95% CI, 0.51 to 0.94), willing (OR 0.69; 95% CI, 0.51 to 0.93), and able (OR 0.64; 95% CI, 0.47 to 0.88) to respond to COVID-19 compared with SAVWs who used PPE more often for protection. Lastly, SAVWs who worked either primarily remotely or a mix of onsite and remotely had lower odds of feeling ready (OR 0.46; 95% CI, 0.23 to 0.92) to respond to COVID-19 compared with SAVWs working primarily at their job site. As with unadjusted results, clinic access restrictions to employees and the public were not significantly associated with the veterinary workforce's readiness, willingness, and ability to respond to COVID-19.
Figure.
Adjusted odds ratios for small animal veterinary workforce adaptations and characteristics contributing to ready, willing, and able preparedness and response perceptions during the COVID-19 pandemic. All adjusted models are controlled for hours worked, personal protective equipment use, remote vs onsite work, clinic status (for employees and the public), job title, years in practice, job region, clinic leadership role, essential worker status, gender, age, and responsibility for dependents. Due to rounding and missing data, percents may not add up to 100%.
aCI upper limits exceed 2.0 in regression models; bP<.005; cP<.01; dP<.05.
Abbreviations: CI, confidence interval; OR, odds ratio; PPE, personal protective equipment; SAVW, small animal veterinary worker.
Associations Between SAVW Characteristics and RWA Outcomes During the COVID-19 Pandemic
In addition to associations with workplace changes, associations between SAVWs characteristics and self-reported readiness, willingness, and ability to respond are also shown in the Figure.
Compared with veterinarians, small animal veterinary administrative and support staff had the most substantial positive associations of preparedness and response, reporting 1.8 times the odds of feeling ready (OR 1.84; 95% CI, 1.05 to 3.32) and willing (OR 1.85; 95% CI, 1.07 to 3.29) to respond to COVID-19, controlling for clinic adaptations. Veterinary technicians and assistants also had positive associations for preparedness and response, reporting 1.4 times higher odds of feeling ready (OR 1.39; 95% CI, 1.03 to 1.87) and willing (OR 1.37; 95% CI, 1.02 to 1.84) to respond to COVID-19 compared with veterinarians. However, after controlling for clinic adaptations, there was no statistically significant increase in veterinary technical and support staff's ability to respond to COVID-19 compared with veterinarians. Lastly, SAVWs with dependents reported being 33% less ready (OR 0.67; 95% CI, 0.49 to 0.90) and 51% less able to respond to COVID-19 than their colleagues without dependents (OR 0.49; 95% CI, 0.36 to 0.67), even after adjusting for demographics and clinic adaptations.
Discussion
This study aimed to characterize and assess small animal veterinary workplace adaptations and SAVWs' self-perceptions of preparedness and response to the COVID-19 pandemic from July to October 2020. We found that a majority (75%) of SAVWs used PPE (primarily surgical or cloth face masks and gloves) more often for protection against COVID-19, exceeding previously published usage rates and infection control standards before the pandemic.23,24 Those who used PPE less often for protection against COVID-19 felt less ready, willing, and able to respond to work during the pandemic. We also found that SAVWs either felt less ready, willing, or able to respond when they had dependents, worked partially or primarily remotely, or worked fewer hours than before the pandemic. Despite these factors, around half (46%) of surveyed respondents stated they would be willing to participate in public health response activities, confirming the critical roles they could fill in PHE response efforts. Additional support for dependents could further improve response within this essential workforce, but future studies would be needed to determine which workplace resources could best support SAVWs during PHEs. Regardless, SAVWs should be accounted for by public health and emergency management professionals who coordinate local, state, and federal responses to provide a One Health preparedness approach that increases multidisciplinary collaboration for a more robust and timely response.25
Impacts of Workplace Adaptations on RWA Response Outcomes
SAVWs' schedule adaptations were among the most reported changes in our study, with 67% of surveyed workers reporting changes to their shift schedules after the start of the pandemic. Reasons for adjusting hours included increasing demand, implementation of safety precautions, and managing staffing and supply shortages.26 Veterinary clinics have used different strategies to reduce SARS-CoV-2 exposure risk, including split or rotational staff shifts to reduce crowded environments and “all in, all out” scheduling of employee teams.3,4,26
In the context of preparedness and response, our study shows that SAVWs who worked fewer hours felt less ready, willing, and able to respond to COVID-19. It is uncertain whether SAVWs working fewer hours felt less prepared because of missed occupational trainings or less familiarity with newly implemented occupational protective practices (reverse causation) or whether illness or other unrelated causes led to an altered work schedule and reduced perception of PHE preparedness. Further assessment of open-ended questions and free-text responses, along with follow-up interviews among respondents, will be important to determine if veterinary clinic operational changes and SARS-CoV-2 exposure fears led to reduced worked hours and low self-perceived preparedness among SAVWs or the other way around. Nevertheless, innovative administrative controls or organizational approaches that maintain the veterinary workforce and clinic operations, such as flexible or rotating shifts, as well as curbside, telehealth, and drop-off appointments, may hold promise to improve resiliency in pandemic response among SAVWs.
Our study identified 2 significant associations between physical precautions and RWA outcomes. First, SAVWs working either primarily remotely or a mix of onsite and remotely reported feeling 54% less ready to respond to COVID-19 than those who worked primarily at the clinic. After controlling for other adaptations and demographics, however, SAVWs were not less willing or able to respond to PHEs when working remotely. As a cross-sectional study, it is impossible to determine if remote work preceded or followed the veterinary and animal care worker's pandemic preparedness; therefore, our study findings may not suggest that telehealth impedes preparedness but instead may point to the current telehealth gaps during disaster or pandemic events that may impede preparation for a successful SAVW response. This is reinforced by the small proportion of respondents in our study who reported working partially or fully remote. SAVW are limited by state laws that govern telehealth use to ensure standards of care and veterinary–client–patient relationships are maintained.27 State and federal preparation and support for veterinary telemedicine during future PHEs would increase SAVWs' ability and willingness to respond to these events. As the veterinary profession develops access to new telehealth technologies, efforts should prioritize addressing telehealth-specific preparedness gaps. Remote and online access to medical records, ability to prescribe medications through local or online pharmacies, and development of better tools to evaluate the health of pets by phone or video are all steps that can increase telemedicine preparedness for future PHEs. Future studies should evaluate the preparedness and response outcomes of SAVWs engaged in effective telemedicine practices to assess the benefits and barriers to telemedicine during future health emergencies.
Various other physical precautions were implemented at most US small animal veterinary clinics. SAVWs increased contact precautions, most notably by washing hands more frequently and using additional PPE around clients.8 Our analysis identified a strong association between SAVWs' PPE use and RWA outcomes. Those who used PPE less often reported feeling 31% less ready, willing, and able to respond to COVID-19 compared with those who used PPE more frequently for protection against COVID-19. We could not ascertain from the surveys if PPE were used less frequently due to organizational policies, personal preference, or supply shortages. Despite clinic considerations on PPE use (such as cost, comfort, transmission risk, medical waste generated, availability), prioritizing SAVWs for access and providing organizational flexibility and autonomy to wear additional PPE, even if not required by regulatory authorities, may be of benefit during future PHE responses.
Small Animal Worker Characteristics and RWA Response Outcomes
We identified 1.4 and 1.8 times the odds of PHE readiness and willingness among veterinary technicians, assistants, and support staff compared with veterinarians, respectively. Even after adjusting for clinic adaptations and worker characteristics (eg, age, experience, gender, dependent status), veterinary technical, administrative, and support staff proved to be a motivated and willing workforce during the pandemic. As technical and administrative staff generally have greater face-to-face interactions with clients in small animal clinics, it is remarkable to see this group is highly prepared and willing to respond during this PHE.16 Because of the small number of administrative and support staff surveyed (n=78, 6.5%), additional studies should further investigate the preparedness and response capabilities of this critical workforce. Regardless, our study adds evidence that SAVWs are important assets for a One Health preparedness approach and should receive organizational attention (eg, through the American Veterinary Medical Association, humane societies, and other groups engaged in response) and support before, during, and after PHEs. The public health community should not underestimate the value of this SAVW population in emergency planning; they are experienced and skilled professionals who could be tapped to increase surge capacity during future health emergencies.16
Dependent care is an important barrier for all medical professionals working during a crisis event, particularly during infectious disease emergencies, due to the potential for a worker to transmit pathogens to family members. Absenteeism due to illness and fear during epidemics has been well documented in HCWs. In the United States, Brazil, and Spain, studies similarly reported absenteeism rates at or above 5% among HCWs from March to April of 2020.28-30 A study by Mercer et al31 showed that emergency department HCWs with dependents predicted they would likely have a higher level of absenteeism than their counterparts without dependents if a public health disaster (eg, general disaster, earthquake, epidemic, nuclear event) occurred. A study by Morton et al32 estimated that approximately 50% of HCWs would not report to work during a major disease outbreak due to disease exposure risk and the need for family care.
In our study, 27.4% of SAVWs listed family and dependent care as the primary personal barrier preventing them from reporting to work during the pandemic, and we further identified that those with dependents were, on average, 33% less ready and 51% less able to respond to COVID-19 than their counterparts. It is important to note there was no statistically significant evidence that they were less willing to respond. SAVWs are skilled and knowledgeable HCWs experienced in infection control and risk management, but their readiness and ability to respond to COVID-19 may be hampered by dependent stay-at-home orders, school closures, or dependent illnesses. Future research should evaluate compounding stressors (eg, having dependents, working fewer hours) associated with poor RWA responses and identify resources and organizational practices to assist SAVWs with dependents. Small animal clinic policies that recognize SAVW caretaker gaps and promote flexibility and commitments to family care may improve workforce responses during PHEs.
While this study was novel and important, our research had limitations. As with any cross-sectional study design, there are likely impacts from respondent self-selection, noncompletion, and recall biases. We were unable to determine the temporality of negative RWA outcomes among SAVWs who used PPE less frequently and worked fewer hours than before the pandemic. We did not analyze individual PPE use, such as the use of medical face shields versus cloth masks, on RWA outcomes. The generalizability of various small animal job roles was limited, as technical and support staff often cross over in interactions with clients and staff, which may have influenced self-perceptions of person-to-person transmission risk and potentially influenced RWA outcomes. There is the threat that a healthy worker effect may have influenced results, especially if SAVWs who were ill from COVID-19 were less likely to participate. There is also limited external generalizability regarding demographics, as most respondents were White (n=1,100, 91.4%) and female (n=1,115, 92.6%). Female respondents comprised a much larger percentage of survey completions than expected, considering the proportion of US small animal female veterinarians is approximately 65%, according to the American Veterinary Medical Association and US Census Bureau.22,33 As most respondents were women of childbearing age, it is surprising that only 25% of respondents reported responsibility for dependents, which may not be truly representative of the US female veterinary worker population. Similar reports have found that compared with male veterinarians, female veterinarians often delay family planning to a later age while in clinical practice,34,35 which may influence their responses about perceived efficacy during PHEs. Future studies should incorporate additional respondents with dependents who are more representative of the US veterinary workforce. Lastly, survey data were collected from July till October 2020, during the first major COVID-19 wave, and inferences may not be representative of subsequent waves or the current pandemic state.
Conclusion
With over 60% of the world's emerging infectious diseases and all recent pandemics (severe acute respiratory syndrome, Middle East respiratory syndrome, influenza) arising from animals, veterinary workers play an ever-increasing role in disease prevention and health security.36 In addition to animal disease surveillance, integrating veterinary and medical resources can improve pandemic response efforts and fill capacity gaps in human healthcare. As the pandemic progresses to become endemic in people and potentially enzootic in animal reservoirs, and as future biological and other threats emerge, the veterinary workforce must be engaged to protect human and animal health.25
The American Veterinary Medical Association recommends that veterinary practices develop disaster plans to address business operations during human-caused and natural disasters (such as COVID-19).4,6 Our study findings emphasize the positive impacts that organizations can have on preparedness and response when they proactively sustain clinic schedules and business continuity operations. Organizations that plan for family caregiving may alleviate an important barrier that can impede effective preparedness and responses for SAVWs. Future studies should assess the impacts of providing caregiving resources and flexible work arrangements (including telehealth) on SAVWs' preparedness efforts. Research into other workplace factors, such as the implementation of PHE preparedness training, may predict the ability of SAVWs to respond to future zoonotic disease threats. Beyond veterinary clinics, local, state, and national public health systems should incorporate a One Health framework in their preparedness and response plans, leveraging the full potential of SAVWs to contribute to surge capacity in emergencies.
Supplementary Material
Acknowledgments
We are thankful for the entire CoVET Research team (Jennifer Nuzzo, Kayla Meza, Kaitlin Waite, Sharmaine Miller, Erin Beasley, Cody Swilley, Kimberly Guyer, Meghan Brino, Paige Laughlin, Justin Edwards, Francesca Schiaffino Salazar, Cusi Ferradas Carrillo), as well as all research respondents and students supporting the CoVET study. The opinions expressed by authors contributing to this journal do not necessarily reflect the opinions of the Department of Defense or the institutions with which the authors are affiliated. Mention of trade names, commercial products, or organizations does not imply endorsement by the US Government.
References
- 1. Johns Hopkins University and Medicine. Johns Hopkins Coronavirus Resource Center. Last updated March 10, 2023. Accessed September 15, 2023. https://coronavirus.jhu.edu/map.html
- 2. World Organisation for Animal Health. COVID-19 and veterinary activities designated as essential. Published March 18, 2020. Accessed September 15, 2023. https://www.woah.org/en/covid-19-and-veterinary-activities-designated-as-essential/
- 3. Steele SG, Toribio JLML, Mor SM. Global health security must embrace a One Health approach: contributions and experiences of veterinarians during the COVID-19 response in Australia. One Health. 2021;13:100314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wayne AS, Rozanski EA. Cataloguing the response by emergency veterinary hospitals during the COVID-19 pandemic via weekly surveys. J Vet Emerg Crit Care (San Antonio). 2020;30(4):493-497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hedman HD, Krawczyk E, Helmy YA, Zhang L, Varga C. Host diversity and potential transmission pathways of SARS-CoV-2 at the human-animal interface. Pathogens. 2021;10(2):180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Garcia LN, Stefanou C, Huston CL, Bell SA. Assessing veterinary practice and practitioner preparedness for natural and man-made disasters, including COVID-19. J Vet Med Educ. 2022;49(6):733-739. [DOI] [PubMed] [Google Scholar]
- 7. US Centers for Disease Control and Prevention. Interim infection prevention and control guidance for veterinary clinics during the COVID-19 response. Published June 12, 2020. Accessed September 15, 2023. https://stacks.cdc.gov/view/cdc/89195
- 8. CM Research Ltd. VetsSurvey 2020 Part 1: COVID-19 Global Pandemic Impact on the Veterinary Market.. Leatherhead, UK: Vetspanel; 2021. Accessed September 15, 2023. https://cm-research.com/covid-19-global-pandemic-impact-on-the-veterinary-market/ [Google Scholar]
- 9. Cima G. Animal health laboratories aid testing for COVID-19 in people. American Veterinary Medical Association. Updated June 1, 2020. Accessed September 15, 2023. https://www.avma.org/javma-news/2020-06-01/animal-health-laboratories-aid-testing-covid-19-people [Google Scholar]
- 10. Wohl JS, Nusbaum KE. Public health roles for small animal practitioners. J Am Vet Med Assoc. 2007;230(4):494-500. [DOI] [PubMed] [Google Scholar]
- 11. Feng A, Bevins S, Chandler J, et al. Transmission of SARS-CoV-2 in free-ranging white-tailed deer in the United States. Nat Commun. 2023;14(1):4078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Meisner J, Baszler TV, Kuehl KE, et al. Household transmission of SARS-CoV-2 from humans to pets, Washington and Idaho, USA. Emerg Infect Dis. 2022;28(12):2425-2434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. King LJ. Veterinary medicine's role in biodefense and public health. J Vet Med Educ. 2003;30(2):161-163. [DOI] [PubMed] [Google Scholar]
- 14. McCabe OL, Barnett DJ, Taylor HG, Links JM. Ready, willing, and able: a framework for improving the public health emergency preparedness system. Disaster Med Public Health Prep. 2010;4(2):161-168. [DOI] [PubMed] [Google Scholar]
- 15. Chiang SC, Fisher HH, Bridwell ME, Trigoso SM, Rasulnia BB, Kuwabara SA. Applying the Ready, Willing, and Able framework to assess agency public health emergency preparedness: the CDC perspective. Health Secur. 2020;18(2):75-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Dalton KR, Guyer KM, Schiaffino F, et al. Assessing COVID-19 pandemic risk perception and response preparedness in veterinary and animal care workers. Health Secur. 2022;20(2):116-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ablah E, Benson LN, Tinius AM, Gebbie KM. Assessment of emergency preparedness of veterinarians in New York. J Vet Med Educ. 2009;36(1):122-127. [DOI] [PubMed] [Google Scholar]
- 18. Dunning D, Martin MP, Tickel JL, Gentry WB, Cowen P, Slenning BD. Preparedness and disaster response training for veterinary students: literature review and description of the North Carolina State University Credentialed Veterinary Responder Program. J Vet Med Educ. 2009;36(3):317-330. [DOI] [PubMed] [Google Scholar]
- 19. Holmquist LS, O'Neal JP, Swienton RE, Harris CA. The role of veterinarians in mass casualty disasters: a continuing need for integration to disaster management. Front Public Health. 2021;9:644654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ferradas C, Hernandez N, Dalton KR, Davis MF, Schiaffino F. COVID-19 pandemic response preparedness and risk perceptions among Peruvian veterinarians and animal care workers. Health Secur. 2022;20(6):445-456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Harris PA, Taylor R, Minor BL, et al; REDCap Consortium. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Data USA. Veterinarians. Accessed September 15, 2023. https://datausa.io/profile/soc/veterinarians
- 23. Elchos BL, Scheftel JM, Cherry B, et al. Compendium of veterinary standard precautions for zoonotic disease prevention in veterinary personnel. J Am Vet Med Assoc. 2008;233(3):415-432. [DOI] [PubMed] [Google Scholar]
- 24. Anderson MEC. Contact precautions and hand hygiene in veterinary clinics. Vet Clin North Am Small Anim Pract. 2015;45(2):343-360. [DOI] [PubMed] [Google Scholar]
- 25. Ferri M, Lloyd-Evans M. The contribution of veterinary public health to the management of the COVID-19 pandemic from a One Health perspective. One Health. 2021;12:100230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. American Veterinary Medical Association (AVMA). COVID-19 Veterinary Impacts and Responses. Schaumburg, IL: AVMA; 2021. Accessed September 15, 2023. https://ebusiness.avma.org/files/coronavirus/COVID-19-practice-effects-report-2021.pdf [Google Scholar]
- 27. American Veterinary Medical Association (AVMA) Practice Advisory Panel. Final Report on Telemedicine. Schaumburg, IL: AVMA; 2017. Accessed September 15, 2023. https://www.avma.org/sites/default/files/resources/Telemedicine-Report-2016.pdf [Google Scholar]
- 28. Groenewold MR, Burrer SL, Ahmed F, Uzicanin A, Free H, Luckhaupt SE. Increases in health-related workplace absenteeism among workers in essential critical infrastructure occupations during the COVID-19 pandemic — United States, March–April 2020. MMWR. Morb Mortal Wkly Rep. 2020;69(27):853-858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. de Paiva LG, Dos Santos WM, Dalmolin GL. The impact of the SARS-CoV-2 pandemic on sickness absenteeism among hospital workers. Rev Bras Med Trab. 2022;20(1):65-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Alquézar-Arbé A, Piñera P, Jacob J, et al. Impact of the COVID-19 pandemic on hospital emergency departments: results of a survey of departments in 2020 - the Spanish ENCOVUR study. Emergencias. 2020;32(5):320-331. [PubMed] [Google Scholar]
- 31. Mercer MP, Ancock B, Levis JT, Reyes V. Ready or not: does household preparedness prevent absenteeism among emergency department staff during a disaster? Am J Disaster Med. 2014;9(3):221-232. [DOI] [PubMed] [Google Scholar]
- 32. Morton MJ, Kirsch TD, Rothman RE, et al. Pandemic influenza and major disease outbreak preparedness in US emergency departments: a survey of medical directors and department chairs. Am J Disaster Med. 2020;14(4):279-286. [DOI] [PubMed] [Google Scholar]
- 33. American Veterinary Medical Association. U.S. veterinarians. Accessed September 15, 2023. https://www.avma.org/resources-tools/reports-statistics/market-research-statistics-us-veterinarians
- 34. Colopy SA, Buhr KA, Bruckner K, Morello SL. The intersection of personal and professional lives for male and female diplomates of the American College of Veterinary Surgeons in 2015. J Am Vet Med Assoc. 2019;255(11):1283-1290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Morello SL, Colopy SA, Chun R, Buhr KA. Work, life, and the gender effect: perspectives of ACVIM Diplomates in 2017. Part 2—The intersection of personal life and professional career. J Vet Intern Med. 2020;34(5):1837-1844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Jones KE, Patel NG, Levy MA, et al. Global trends in emerging infectious diseases. Nature. 2008;451(7181):990-993. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.