Abstract
Histoplasmosis is a chronic granulomatous disease seen in immunocompromised individuals, rarely immunocompetent patients. We report disseminated histoplasmosis involving adrenal glands and oral cavity with synchronous squamous cell carcinoma of right pyriform fossa. With early diagnosis and treatment he recovered well.
Supplementary Information
The online version contains supplementary material available at 10.1007/s12070-023-03962-4.
Keywords: Histoplasmosis, Squamous cell carcinoma, Pyriform fossa
Introduction
Histoplasmosis (Darling disease), a systemic fungal infection caused by Histoplasma capsulatum, a saprophytic and dimorphic fungi, affects populations in tropical regions of North America and Africa. Infection spreads via airborne route through fungal spores in the soil from bat or bird droppings. Immunocompromised patients, commonly HIV infected or malignancy are associated with histoplasmosis. It affects the respiratory, gastrointestinal system, oral, cutaneous and neurological manifestations. About30-50% cases, oral lesions have been reported frequently involving the palate, buccal mucosa, and tongue. Among the head and neck cancers, squamous cell carcinoma is seen in about more than 90% of population [1].
In this study, an association of hypopharyngeal malignancy is seen along disseminated histoplasmosis with the adrenal gland involvement and right lower alveolus, which is a unique presentation.
Case Report
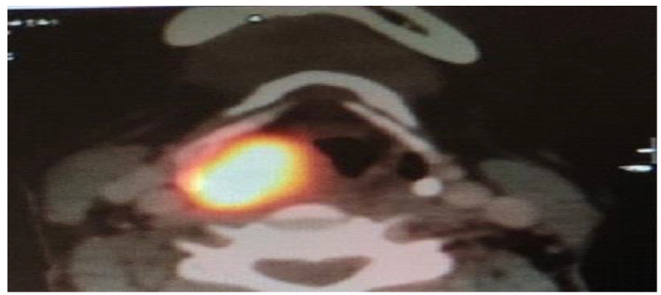
58 year old male without comorbidities presented to a Tertiary Care Centre with throat discomfort and voice change for two months. Known smoker for more than 20 years. No history of dysphagia, dyspnoea, fever, cough, swelling in neck. No history suggestive of emphysema. 2 × 1 cm ulcerated, reddish lesion in right lower alveolus extending from lower second molar to last molar (Fig. 1). Video laryngoscopy revealed ulceroproliferative growth involving right pyriform fossa. PET-CT head and neck showed 3.4 × 2.3 × 2.8 cm heterogenous lesion in right pyriform fossa with FDG prominent right level Ib and II nodes, hypermetabolic bilateral adrenal lesions 4.7 × 3.4 cm and right lower alveolus measuring 2.3 × 1.2 × 0.5 cm without bony erosion (Figs. 2 and 3). Serum cortisol and metanephrine were normal. HPE of right pyriform fossa growth showed poorly differentiated squamous cell carcinoma (Fig. 4A, B). HPE of oral cavity growth was suggestive of histoplasmosis (Fig. 4C, D). He was treated with weekly cisplatin for 6 weeks with concurrent radiation therapy (66 Gy in 33 fraction) and intravenous Amphotericin B once daily for a week. After completion of initial treatment oral Itraconazole 200 mg thrice a day for 2 days followed by 100 mg twice a day for 1 year. Repeat PET CT by the end of 12 weeks after completion of treatment showed complete resolution of disease.
Fig. 1.

2 × 1 cm ulcerated lesion involving right lower alveolus
Fig. 2.
PET CT image showing FDG uptake in Right pyriform fossa
Fig. 3.

PET CT image showing FDG uptake in Bilateral adrenal glands
Fig. 4.

A(H&E-40X) & B(H&E-400X) – Squamous cell carcinoma with keratinisation C(H&E-1000X) D(PAS- 1000X) Scattered Hisptoplasma organisms shown in arrow marks
Discussion
Histoplasmosis can be acute or chronic, asymptomatic or painful ulcers. Acute manifests as influenza, a selflimiting condition and chronic resembles tuberculosis [2].
Disseminated histoplasmosis is fatal where the infection affects spleen, adrenal glands, liver, lymph node, GIT, CNS, kidney and oral mucosa [3].Oral lesions can occur anywhere but frequently seen on tongue, palate and buccal mucosa. Laryngeal histoplasmosis have been detected which mimicks squamous cell carcinoma or tuberculosis. This case is unique in a way that histoplasmosis mimicking as second primary tumor in oral cavity which with deeper biopsy we were able to arrive at a diagnosis and provide treatment. PET CT showed a disseminated form of histoplasmosis involving both the adrenal glands. Dogenski et al. described a 39-year-old female with an ulcer over the tongue, initially diagnosed as Lupus erythematosus received an intralesional Betamethasone injection and was showing clinical improvement, until 2 weeks. Later ulcer worsened and a second biopsy was suggestive of histoplasmosis.7 Due to its varied and misleading presentation, Singh et al. have mentioned Histoplasmosis as the “Syphilus of the Fungal world’ [4].
Histoplasma capsulatum can be identified by histopatholical, cytopathalogical or culture. Sabouraud agar medium, which is most commonly used culture method, is not preferred for assessing histoplasmosis as the fungus is very slow growing and may take upto 6 weeks for its growth to be identified, which may delay diagnosis. Special stains that can be used to visualize the organism are Gomori Methenamine Silver (GMS) and Periodic Acid Schiff (PAS). Under microscopy, they appear as an intracellular, narrow, 2–4 μm sized oval budding yeasts surrounded by a halo. Detection of urine and serum histoplasma antigen can help in early diagnosis. Superficial biopsies would suggest squamous cell carcinoma and would misguide in surgical intervention hence a deeper biopsy is required [5].
Oral Itraconazole is effective in management of histoplasmosis with a cure rate of 85–100%. Other treatments are topical nystatin for 3 weeks followed by oral itraconazole in non responders [6]. Itraconazole is another effective anti-fungal agent which is less toxic compared to Amphotericin B, however its disadvantage being drug interaction [7].A study by Ferster et al. described about a patient having disseminated form of histoplasmosis found in the wall of the abdominal aortic aneurysm and the patients in this study were treated with Amphotericin B and those with the toxicity of Amphotericin B were given Ketoconazole [8].
Jawale et al.’s study stated that in most of the cases, histoplasmosis that are seen as a solitary lesion may have occurred as a result of secondary localization of a former primary lesion [9]. Patients were followed upto a maximum of 16 years. 1 patient died due to Bronchopneumonia, autopsy revealed persistant histoplasmosis of adrenal gland. Few studies also recommended adrenalectomy as the treatment for adrenal histoplasmosis.
Conclusion
The peculiarity of this case is disseminated histoplasmosis with oral cavity and adrenal gland involvement which mimics as second primary in Head and Neck malignancy. With early diagnosis and proper treatment it is easier to treat histoplasmosis without recurrences.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Author Contribution
Dr. Gowthame K- Acquisition, analysis, Dr. Archana L- interpretation of data, Dr. Annapurneswari S- Revising the draft critically, Dr. Kannan S- Final approval of the manuscript
Funding
Nil.
Data Availability
The data that support the findings of this study are available from the corresponding author, Dr. Gowthame K upon reasonable request.
Declarations
Conflict of Interest
Nil.
Informed Consent
His clinical photographs were used after obtaining an informed and written consent.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Prabhash K, Babu G, Chaturvedi P, Kuriakose M, Birur P, Anand AK, Kaushal A, Mahajan A, Syiemlieh J, Singhal M, Gairola M (2020) Indian clinical practice consensus guidelines for the management of squamous cell carcinoma of head and neck. Indian Journal of Cancer. Feb 1;57(5):1 [DOI] [PubMed]
- 2.Randhawa HS, Gugnani HC. Occurrence of histoplasmosis in the indian sub-continent: an overview and update. J Med Res Pract. 2018;7(3):71–83. [Google Scholar]
- 3.Dogenski LC, Pasqualotto EM, Dutra MJ, Rovani G, Trentin MS, De Carli JP (2022) Uncommon case of histoplasmosis with oral manifestation: A case report of diagnosis in a South American patient. International Journal of Surgery Case Reports. Apr 1;93:106920 [DOI] [PMC free article] [PubMed]
- 4.Singh A, Gauri M, Gautam P, Gautam D, Haq M, Handa AC, Handa KK (2019) Head and neck involvement with histoplasmosis; the great masquerader. American journal of otolaryngology. Sep 1;40(5):678 – 83 [DOI] [PubMed]
- 5.Viswanathan S, Chawla N, D’Cruz A, Kane SV (2007 Dec) Head and neck histoplasmosis—a nightmare for clinicians and pathologists! Experience at a tertiary referral cancer centre. Head Neck Pathol 1(1):169–172 [DOI] [PMC free article] [PubMed]
- 6.Wheat J, Sarosi G, McKinsey D, et al. Practice guidelines for the management of patients with histoplasmosis. Clin Infect Dis. 2000;30(4):688–695. doi: 10.1086/313752. [DOI] [PubMed] [Google Scholar]
- 7.Anuradha S, Bhanu K, Aditya R SC J. Localized Mucocutaneous Histoplasmosis of Tonguein an immunocompetent patient: A Rareentity from anon- endemicsub-Himalayanregion
- 8.Ferster AP, Jaworek A, Hu A (2018 Sep) Histoplasmosis of the head and neck in the immunocompetent patient: report of 2 cases. Ear, nose & Throat Journal. 97(9):E28–31 [PubMed]
- 9.Jawale PM, Gulwani HV Histoplasmosis presenting as laryngeal ulcer in a post-renal transplant male: An unusual case from India. Journal de MycologieMedicale. 2017 Dec 1;27(4):573-6 [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, Dr. Gowthame K upon reasonable request.


