Abstract
Introduction: Rhinitis is defined as inflammation of nasal mucosa. Allergic rhinitis is the most common type of chronic rhinitis with increasing prevalence. Tests such as nasal smear for eosinophilia, Skin prick test, Serum absolute eosinophil count and Immunoglobulin IgE helps us in diagnosis of allergic rhinitis. Objective: To evaluate the efficacy of the nasal smear for eosinophilia and blood absolute eosinophil count tests to diagnose allergic rhinitis in patients with varied severity of symptoms. Materials and methods: In this prospective study, all patients above 12 years of age with symptoms suggestive of allergic rhinitis were enrolled in our study. Severity assessment was done by visual analog scoring and Total nasal outcome scoring. Diagnostic nasal endoscopy with nasal smear for eosinophilia, complete blood count and blood absolute eosinophil count tests were done. Results: A total of 60 patients were enrolled in the present study. Age ranged from 13 to 55 years with female preponderance. The most common symptom was rhinorrhea found in 100% of study population, followed by sneezing present in 57 (93.5%) patients. 10 out of 12 patients with mild intermittent symptoms had < 5% of eosinophil elicited in nasal smear and 2 patients had negative smear of eosinophils. Only 13% had mild eosinophilia. In this study, in those patients with mild intermittent symptoms neither nasal smear eosinophilia nor Blood absolute eosinophil count was found to be significant. Conclusions: Nasal smear cytology and blood absolute eosinophil count were found to be significant only in patients with moderate-severe symptoms. Those patients with mild intermittent symptoms need not be tested as it will be insignificant. In these patients, we must rely on the visual analogue score based on the severity of symptoms rather than laboratory tests.
Supplementary Information
The online version contains supplementary material available at 10.1007/s12070-023-03945-5.
Keywords: Absolute eosinophil count, Allergic rhinitis, Nasal smear eosinophilia, Total nasal symptoms score
Introduction
Rhinitis is defined as inflammation of nasal mucosa. Allergic rhinitis is the most common type of chronic rhinitis affecting up to 40% of the population with increasing prevalence [2]. It is a type I hypersensitivity reaction.
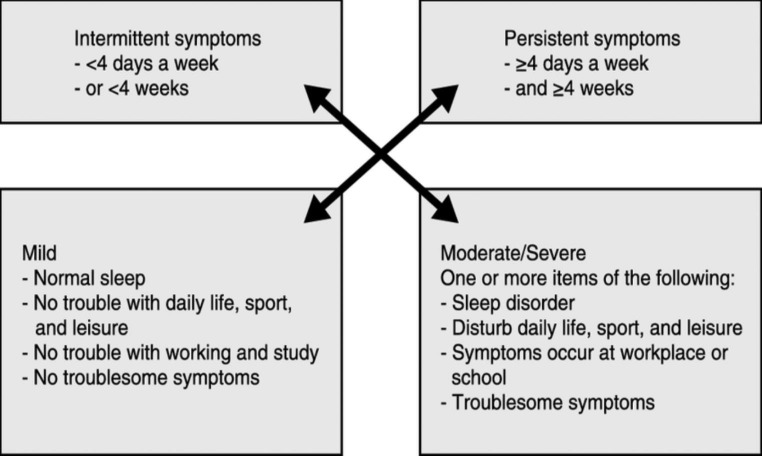
ARIA (Allergic rhinitis and its impact on asthma) guidelines define allergic rhinitis as “rhinorrhea, nasal itching, nasal obstruction and sneezing which are reversible spontaneously or with treatment”. According to ARIA, patients are stratified as those with intermittent or persistent symptoms & based on severity further classified as mild and moderate-severe [1].
Fig. 1.
ARIA Classification of allergic rhinitis
Tests such as nasal smear for eosinophilia, Skin prick test, Serum absolute eosinophil count and Immunoglobulin IgE helps us come to a diagnosis of allergic rhinitis. Other invitro tests such as Radioallergosorbent test (RAST), Enzyme-linked immunosorbent assay (ELISA) also have a diagnostic significance.
Materials and Methods
In this prospective study, 60 consecutive patients above 12 years of age presented to Tertiary Health Care Centre, Tamil Nadu, India with clinical diagnosis of allergic rhinitis were enrolled in our study. Patients were divided into two groups by block randomization, based on the persistence of symptoms as Intermittent, and Persistent, both groups were subdivided in two groups based on severity as mild and moderate-severe. Total 4 groups – Group IA – Mild intermittent, Group IB – Moderate-severe intermittent, Group IIA – Mild persistent, Group IIB Moderate-severe persistent. Following ethical clearance, Informed and written consent obtained from April 2021 to April 2022 with the following exclusion criteria.
Exclusion Criteria
Less than 12 years of age.
Patients who have taken any antihistamines, mast cell stabilizers, nasal corticosteroids or antileukotrienes for at least 1 week prior.
Patients with evidence of other nasal pathologies such as chronic rhinosinusitis with nasal polyposis, allergic fungal rhinosinusitis.
A detailed history and clinical examination was done. History to rule out other causes of chronic rhinitis was taken. The Total Nasal Symptom Score comprising of four symptoms: nasal obstruction, nasal itching, sneezing and rhinorrhea was noted. Each symptom is graded from 0–3, where 0 indicates no symptoms, a score of 1 for mild symptoms that are easily tolerated, 2 for awareness of symptoms which are bothersome but tolerable and 3 is reserved for severe symptoms that are hard to tolerate and interfere with daily activity. TNSS is calculated by adding the score for each of the symptoms to a total out of 12 [3]. A score of ≥ 5 is considered for a clinical diagnosis of allergic rhinitis. Visual analogue scoring was done based on the severity ranging from 0 to 10, (0 being normal and 10 being worst).
All patients were subjected to diagnostic nasal endoscopy with nasal smear for eosinophilia and blood absolute eosinophil count tests. Nasal smear eosinophilia scoring was done based on the percentage of eosinophils. Less than 5 (Rare); 5 to 15 (Mild); 16 to 25 (Moderate), and more than 25 (Severe) [4]. Degree of blood eosinophilia was categorized as mild (600–1500 cells/µL), moderate (1500–5000 cells/µL), and severe (> 5000 cells/µL) [5].
Results
A total of 60 patients were enrolled in the present study. Age ranged from 13 to 55 years with a mean age of 28.3. Male patient were 26 (43.3%), while female patients were 34 (56.6%) with female preponderance. The most common symptom was rhinorrhea found in 100% of study population, followed by sneezing present in 57 (93.5%) patients. Total nasal symptoms score was 5–7 (out of 12) in 53% of population, whereas 8 to 10 (out of 12) in 43% of population. Visual analogue scoring based on the severity of symptoms revealed 42% of patients with mild symptoms and 58% of patients with moderate-severe symptoms. Most of the patients (18 out of 60) in our study fell under Group IB (Moderate-Severe Intermittent). 10 out of 12 patients with mild intermittent symptoms had < 5 percentage of eosinophil elicited in nasal smear and 2 patients had negative smear of eosinophils. The nasal smear for eosinophilia correlated well with severity of clinical score. Majority (85%) of the patients had no eosinophilia while 13% had mild eosinophilia. No correlation of blood AEC with severity of clinical score was noted. In this study, in those patients with mild intermittent symptoms neither nasal smear eosinophilia nor Blood absolute eosinophil count was found to be significant.
Table 1.
Correlation between nasal smear eosinophil count and severity of symptoms
| Nasal smear eosinophil count | Visual Analogue Score | |||||
|---|---|---|---|---|---|---|
| Mild (0–4) | Moderate (5–7) | Severe (8–10) | ||||
| Intermittent | Persistent | Intermittent | Persistent | Intermittent | Persistent | |
| Rare (< 5) | 10 | 4 | 0 | 0 | 0 | 0 |
| Mild (5–15) | 0 | 9 | 3 | 1 | 0 | 0 |
| Moderate (16–25) | 0 | 0 | 6 | 8 | 5 | 2 |
| Severe (25) | 0 | 0 | 0 | 2 | 4 | 4 |
Table 2.
Correlation between blood absolute eosinophil count and severity of symptoms
| Blood absolute eosinophil count | Visual Analogue Score | |||||
|---|---|---|---|---|---|---|
| Mild (0–4) | Moderate (5–7) | Severe (8–10) | ||||
| Intermittent | Persistent | Intermittent | Persistent | Intermittent | Persistent | |
| No eosinophilia (< 600) | 12 | 11 | 9 | 8 | 8 | 3 |
| Mild eosinophilia (600–1500) | 0 | 2 | 0 | 3 | 1 | 2 |
|
Moderate eosinophilia (1500–5000) |
0 | 0 | 0 | 0 | 0 | 1 |
| Severe eosinophilia (> 5000) | 0 | 0 | 0 | 0 | 0 | 0 |
Discussion
Allergic rhinitis is a localized type I hypersensitivity reaction of the nasal mucosa in response to inhaled allergens [6]. The initial response is characterized by vasodilation, vascular leakage, and glandular secretion which are brought about by Immunoglobulin E (IgE) antibodies and mast cells [7]. This is followed by Infiltration of leukocytes including eosinophils and neutrophils. Eosinophils are responsible for type I hypersensitivity reactions. There are many ways to detect eosinophils and proteolytic proteins and enzymes liberated by eosinophils such as major basic protein and eosinophil cationic protein [8].
Since the main objective of our study is only to evaluate the efficacy of Nasal smear for eosinophilia (NSE) and blood Absolute eosinophil count (AEC), other investigations such as Serum IgE, Skin prick test, Radioallergosorbent test (RAST), Enzyme-linked immunosorbent assay (ELISA) were not performed. In our study, we only did nasal smear and not biopsy. While Chanda et al. [9] reported the diagnostic efficacy of biopsy over smears for the detection of eosinophils, Mygind et al. [10] showed smears to be better than biopsies. Berkiten G et al. [11] found positive correlations between Total Nasal Symptom Scores and allergic rhinitis patients. Miller et al. [12] claimed that the nasal smear for eosinophils appears to be a reliable diagnostic test with moderately high sensitivity and high specificity, though Bousquet et al. [1] in their study concluded that raised eosinophilia alone was not adequate for the diagnosis of allergic rhinitis. Akeem et al. [13] reported that the severity of symptoms have a positive correlation with the degree of nasal eosinophilia and Chen et al. [14] in their study of patients with perennial Allergic Rhinitis, reported the nasal eosinophil count and serum Immunoglobulin (IgE) to be independent predictors of the severity of AR which supports our study. Although nasal smear has been proposed as a one of the diagnostic tools for allergic rhinitis, no consensus exists. Lans et al. [15] used a cut-off value of 20 per cent whereas Sood [16] adopted 5 per cent. In our study we used 20 per cent as cut off value. A study in a Chinese population conducted by Liu et al. [17] showed Eosinophilia and mast cell numbers were higher in persistent allergic rhinitis patients than intermittent allergic rhinitis patients.
In our study we noted that, in allergic rhinitis patients with mild intermittent symptoms, nasal smear eosinophilia and blood Absolute eosinophil count was insignificant, and results were undifferentiable from normal individuals and those with non-allergic eosinophilia. The study Olusesi et al. [18] showed increasing incidence of eosinophilia with severity of clinical score in patients of both allergic and NAR patients which augments our study report.
Conclusion
Nasal smear cytology and blood absolute eosinophil count tests were found to be significant only in patients with moderate-severe symptoms and in some patients with mild persistent symptoms. Those patients with mild intermittent symptoms need not be subjected to these tests as it will be insignificant. In these patients, we must rely on the Total nasal symptom score and visual analogue score based on the severity of symptoms rather than laboratory tests.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Declarations
Conflict of Interest
Author declares no conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bousquet J, Schünemann HJ, Togias A, Bachert C, Erhola M, Allergic Rhinitis and Its Impact on Asthma Working Group (2020) Jan;145(1):70–80.e3 ;. Next-generation Allergic Rhinitis and Its Impact on Asthma (ARIA) guidelines for allergic rhinitis based on Grading of Recommendations Assessment, Development and Evaluation (GRADE) and real-world evidence. J Allergy Clin Immunol. doi: 10.1016/j.jaci.2019.06.049. Epub 2019 Oct 15. Erratum in: J Allergy Clin Immunol. 2022 Jun;149(6):2180. PMID: 31627910 [DOI] [PubMed]
- 2.Small P, Keith PK, Kim H (2018) Allergic rhinitis. Allergy Asthma Clin Immunol. Sep 12;14(Suppl 2):51. doi: 10.1186/s13223-018-0280-7. PMID: 30263033; PMCID: PMC6156899 [DOI] [PMC free article] [PubMed]
- 3.Ellis AK, Soliman M, Steacy L. The allergic rhinitis - clinical Investigator Collaborative (AR- CIC): nasal allergen challenge protocol optimization for studying AR pathophysiology and evaluating novel therapies. Allergy Asthma Clin Immunol. 2015;11(1):16. doi: 10.1186/s13223-015-0082-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Patel AK, Nagpal TP. Comparison of blood absolute eosinophil count and nasal smear eosinophils with symptoms and severity of clinical score in patients of allergic rhinitis. Indian J Allergy Asthma Immunol. 2014;28:74–77. doi: 10.4103/0972-6691.140774. [DOI] [Google Scholar]
- 5.BritoBabapulle F. The eosinophilias, including the idiopathic hypereosinophilic syndrome. Br J Haematol. 2003;121:203–223. doi: 10.1046/j.1365-2141.2003.04195.x. [DOI] [PubMed] [Google Scholar]
- 6.Robbins & . Cotran pathologic basis of Disease. 8. Philadelphia: Elsevier; 2010. pp. 504–505. [Google Scholar]
- 7.Galli SJ, Tsai M, Piliponsky AM. The development of allergic inflammation. Nature. 2008;454(7203):445. doi: 10.1038/nature07204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Romagnani S. Cytokines and chemoattractants in allergic inflammation. Mol Immunol. 2002;38(12–13):881–885. doi: 10.1016/S0161-5890(02)00013-5. [DOI] [PubMed] [Google Scholar]
- 9.Chanda R, Aggarwal AK, Kohli GS, Jaswal TS, Gupta KB. Comparative study of nasal smear and biopsy in patients of allergic rhinitis. Ind J Allergy Asthma Immunol. 2002;16(1):27–31. [Google Scholar]
- 10.Mygrind N, Weeks B, Dirksin A, Johnson NJ. Perenial rhinitis: an analysis of skin testing, serum IgE and blood and smear eosinophilla in 201 patients. Clin Otolaryngol. 1978;3:189–196. doi: 10.1111/j.1365-2273.1978.tb00681.x. [DOI] [PubMed] [Google Scholar]
- 11.Berkiten G, Aydoğdu İ, Kumral TL, Saltürk Z, Uyar Y, Arslanoğlu A, Tutar B, Göker AE (2018) Nasal eosinophilia in nasal smears of patients with persistent and intermittent allergic rhinitis. J Laryngol Otol 1–4. 10.1017/S0022215118001986 [DOI] [PubMed]
- 12.Miller RE, Paradise JL, Friday GA, et al. The nasal smear for eosinophils. Am J Dis Child. 1982;136:1009–1011. doi: 10.1001/archpedi.1982.03970470053015. [DOI] [PubMed] [Google Scholar]
- 13.Akeem O, Lasisi MBChB, Hakeem FWACSFMCORL, Lawal O, Ogun MBBSGO, Path MBBSFMC, Oluwasola A FWAC P, M. O. Odubanjo, MBBS, FMCPath, Alli Salisu, MBBS, and Shuaib K. Aremu, MBBS.
- 14.Chen ST, Sun HL, Lu KH, et al. Correlation of immunoglobulin E, eosinophil cationic protein, and eosinophil count with the severity of childhood perennial allergic rhinitis. J Microbiol Immunol Infect. 2006;39(3):212–218. [PubMed] [Google Scholar]
- 15.Lans DM, Alfano N, Rocklin R. Nasal eosinophilia in allergic and non-allergic rhinitis: usefulness of the nasal smear in the diagnosis of allergic rhinitis. Allergy Proc. 1989;10:275–280. doi: 10.2500/108854189778959984. [DOI] [PubMed] [Google Scholar]
- 16.Sood A. Diagnostic significance of nasal eosinophilia in allergic rhinitis. Ind J Otorhinolaryngol Head Neck Surg. 2005;57:13–16. doi: 10.1007/BF02907618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liu F, Zhang J, Liu Y, Zhang N, Holtappels G, Lin P, et al. Inflammatory profiles in nasal mucosa of patients with persistent vs intermittent allergic rhinitis. Allergy. 2010;65:1149–1157. doi: 10.1111/j.1398-9995.2010.02340.x. [DOI] [PubMed] [Google Scholar]
- 18.OlusesiAD, SaidMA AmoduEJ. Acorrelation of symptomatology with nasal smear eosinophilia in noninfectious chronic rhinitis preliminary report. Niger J Clin Pract. 2007;10:238–242. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.