Abstract
This study investigates the changes in physical church closings years 2013 to 2019 in New York City (NYC), Philadelphia, and Baltimore and the association with COVID-19 infection rates. We applied Bayesian spatial binomial models to analyze confirmed cases of COVID-19 as of February 28, 2022, in each city at the zip code-level. A one unit increase in the number of churches closed corresponded to a 5% higher COVID-19 infection rate, in NYC (rate ratio = 1.05, 95% credible interval = 1.02–1.08%), where the association was significant. Church closings appears to be an important indicator of neighborhood social vulnerability. Church closings should be routinely monitored as a structural determinant of community health and to advance health equity.
Introduction
The public health burden of the COVID-19 pandemic is massive, with 94.7 million infections and 1.04 million deaths in the USA [1]. Geographic inequalities in COVID-19 burden have been correlated with sociodemographic characteristics (e.g., older age distribution and racial composition), socioeconomic deprivation, and inequitable distribution of other built environment characteristics such as the density of testing locations [2–4]. Religious institutions including churches contributed to the spread of COVID-19 during early waves of the pandemic [5], for example, through person-to-person close contact performing rituals such as singing in the choir [6].
However, many churches were instrumental in augmenting public health interventions. Churches were used as COVID-19 testing locations and vaccination sites [7–9]. These efforts contributed to flattening the curve of infection in later waves. In New York City, the State Department of Health partnered with Northwell Health to establish 24 temporary COVID testing sites at Black churches in predominantly minority neighborhoods (21 zip codes with greater than average Black or Latino populations) [10]. In Philadelphia, PA, clinicians in two health care systems partnered with faith-based organizations in predominantly Black neighborhoods to roll out a text message platform that contributed to high vaccine uptake among residents (of whom 85% were Black) [11]. In Baltimore, the Johns Hopkins Health System provided free community-based testing by partnering with religious leaders across the city to reach the Latinx population [9].
The religious institution (a broad term, which includes churches), therefore, is a key social determinant of health [12] and can mitigate social vulnerability within a neighborhood. Specifically, these institutions perform several functions within populations that address vulnerability [13] (e.g., feeding the poor through food pantries and soup kitchens, providing daycare for free, health screenings, and substance use treatment for those under insured or with no insurance, or fail to present due to stigma in healthcare) [14–16]. Religious institutions are more adept at serving several social safety functions, especially when it comes to serving populations that traditional public health institutions cannot (or do not do an adequate job of reaching), such as the unhoused/homeless, undocumented, and low-income racial minorities [17, 18].
Given the potential for religious institutions to partner with public health organizations to deliver care to vulnerable populations and reach a wider segment of the population, it is important to quantify the availability of these establishments and understand trends, such as the extent to which they have closed. Understanding these trends, especially within neighborhoods, can possibly help forecast the potential impact of the presence (or lack thereof) of these institutions in the event of public health crises that alone, traditional public health systems are not prepared to handle. Early during the COVID-19 pandemic, existing public health institutions (e.g., community health clinics and hospitals) were not prepared to serve the volume of people susceptible to infection and to reduce inequities in the infection rates [19–21]. Understanding, then, pre-pandemic changes in the distribution of churches (e.g., extent to which they are closing) on the COVID crisis, could provide a template for the kinds of epidemiologic analyses that should be conducted at the outset of other major public health threats.
While studies showed that individual religious attendance is correlated with COVID-19 outcomes [6, 22], the public health impact of the potential absence of churches on rates of COVID-19 in the population remains unknown. We therefore sought to quantify the impact of church closings before the pandemic on subsequent rates of COVID-19 infections in three northeast US cities.
Methods
Religious institutions describes a broad range of institutions such as convents, mosques, and temples, all which fall under Standard Industry Classification (SIC) code 8661 [23]. In this study, we focused on “churches,” which is operationalized based on the extended (SIC) code 866,107. We focus on churches because they are the largest by volume compared to other institution types [24]. These data were obtained from a proprietary database hosted by Data Axle Inc (formerly named Infogroup Business USA) [25]. This database can be searched (e.g., using SIC codes) to retrieve historical data on businesses across the USA. These data can be accessed through university libraries and other platforms [25, 26]. A church closure is defined as four consecutive years where no data were reported by the church indicating it is no longer physically present at the end of the period [27]. A pattern, for instance, of “1110000” would indicate data (i.e., open) in 2013, 2014, and 2015 but no data in 2016, 2017, 2018, and 2019, coded as “closed” [27].
We obtained COVID-19 data, as of February 28, 2022, from open-source data maintained by the Departments of Health within New York City (NYC), NY, Philadelphia, PA, and Baltimore, MD. We selected these three cities for one primary reason. The first author personally started observing the trend of churches closing in specific NYC neighborhoods, and then started to observe evidence of similar trends Philadelphia, PA and other cities including Baltimore, MD. We included covariates based on theory and prior COVID-19-related studies [28–30]. These variables included socioeconomic deprivation, % 65 + years of age, % renters, % Hispanic, % Black/African American, population density, overcrowding, and number of community health centers per 10,000 population. We extracted these covariates from the American Community Survey (ACS) 5-year estimates, 2015–2019, and Health Resources & Services Data Warehouse for the community health centers.
We fitted hierarchical Bayesian spatial binomial models to analyze zip code-level confirmed cases of COVID-19 in each city. The model was specified as Yi ~ Binomial(pi, Ni), where Yi, pi, and Ni are the number of confirmed COVID-19 cases, the probability of COVID-19 infection, and the total population at risk at the ith zip code, respectively. A logit function was used to link pi and covariates including church closings. Spatial autocorrelations in COVID-19 cases (i.e., neighboring areas with similar COVID-19 infection risks) [31] were accounted for with the Leroux conditional autoregressive model [32]. Zip codes that share at least one vertex were considered neighbors, a simple yet effective approach to define neighbors [33]. The models were implemented using the computationally efficient Integrated Nested Laplace Approximation algorithm via the R (version 4.2.1) package R-INLA, version 22.5.7. We report the rate ratio of COVID-19 infection (i.e., posterior mean and 95% credible interval (95% CrI)).
Results
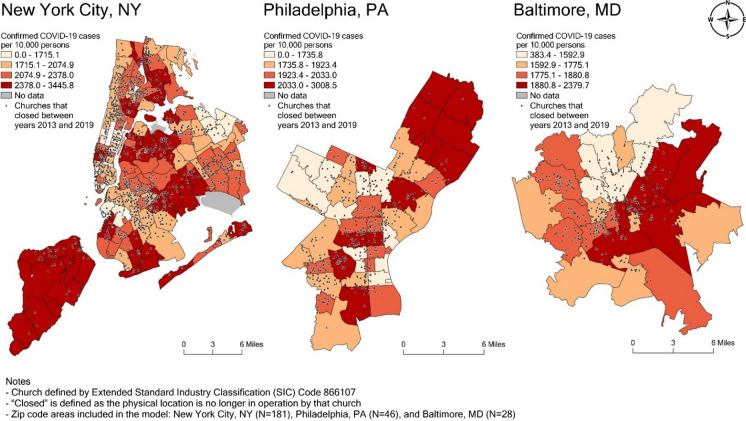
Church closings were significantly spatially clustered across zip codes in all cities (Fig. 1). Church closings per 10,000 population was significantly associated with higher COVID-19 infection in NYC only. A one-unit increase in churches closed corresponded to 5% higher case rates (RR = 1.05, 95% CrI: 1.02–1.08, Table 1). In Philadelphia, PA and Baltimore, MD, church closings were positively related to COVID-19 infection rates, but not statistically significant.
Fig. 1.
Association between churches closing and COVID-19 case rates
Table 1.
Multivariable results showing church closing is associated with higher COVID-19 case rates
| New York City, NY (181 zip codes) |
Philadelphia, PA (46 zip codes) |
Baltimore, MD (28 zip codes) |
|
|---|---|---|---|
| Rate ratio and 95% credible interval | |||
| Rate of churches closing between 2013 and 2019, per 100,000 population | 1.05 (1.02, 1.08) | 1.04 (0.97, 1.11) | 1.11 (0.90, 1.38) |
| Number of churches closing in 2013 | 0.98 (0.96, 1.01) | 0.98 (0.93, 1.04) | 0.94 (0.77, 1.12) |
| Socioeconomic deprivation | 1.12 (1.05, 1.19) | 1.18 (1.02, 1.38) | 0.95 (0.64, 1.36) |
| % 65 + years of age | 1.00 (0.95, 1.06) | 1.03 (0.96, 1.11) | 1.24 (1.05, 1.46) |
| % Renters | 1.04 (0.98, 1.10) | 1.00 (0.92, 1.08) | 0.95 (0.72, 1.23) |
| % Hispanic | 1.03 (0.98, 1.10) | 0.97 (0.88, 1.06) | 1.24 (0.89, 1.68) |
| % Black/African American | 0.97 (0.93, 1.01) | 0.96 (0.85, 1.07) | 1.18 (0.89, 1.54) |
| Population density | 0.94 (0.90, 0.98) | 0.94 (0.88, 1.00) | 1.08 (0.84, 1.36) |
| Overcrowding | 0.99 (0.95, 1.02) | 0.98 (0.91, 1.06) | 0.87 (0.63, 1.16) |
| Number of community health centers per 10,000 population | 0.98 (0.95, 1.01) | 1.03 (0.97, 1.09) | 1.18 (0.99, 1.40) |
| Spatial autocorrelation in the random effects | 0.84 (0.68, 0.95) | 0.65 (0.25, 0.93) | 0.53 (0.11, 0.92) |
| Moran’s I coefficient and p value | |||
| Moran’s I of COVID-19 cases | 0.42 (p < 0.001) | 0.30 (p < 0.001) | 0.09 (p = 0.15) |
| Moran’s I of church closing rates, 2013–2019 | 0.19 (p < 0.001) | 0.26 (p < 0.01) | 0.14 (p = 0.06) |
| Moran’s I of church closing in 2013 | 0.18 (p < 0.001) | 0.21 (p < 0.01) | − 0.02 (p = 0.44) |
Discussion
Churches closing corresponded to a higher rate of COVID-19 infection cases although this association was statistically significant in NYC only. The magnitude of risk associated with church closings was 5%. The significant result in NYC only could possibly be due to limited power to detect significance in Philadelphia and Baltimore because the number of zip codes in NYC was substantially larger than the other cities (N = 188 vs 46 and 28, respectively). The results in NYC were also significant and larger than that of % Black and % Hispanic racial composition, which has been well documented as a contributor of geographic disparities in COVID-19 outcomes, such as positivity and incidence and mortality [2]. Although, in previous analyses, church closings were spatially concentrated in predominantly Black neighborhoods [27], these novel multivariable findings reveal excess risk, independent of racial composition.
Other structural inequality mechanisms that possibly link church closings to higher COVID-19 infections remain to be investigated. The current direction of results may appear contrary to expectations. Churches have been used as sites of COVID-19 testing and vaccinations [7, 8], which would be expected to correlate positively with COVID-19 within a geography (as people are diagnosed) but possibly negatively across pandemic waves (potentially as more people learn their status and are vaccinated). It may also be expected that church closings would limit the potential for physical gatherings and subsequently lower virus exposure and lower infection rates [5].
However, the church closing data preceded the pandemic (ending in 2019) and thus, reflects a previous trend, temporally before the outcome. Moreover, we surmise that church closings mechanisms operate differently. From a theoretical perspective, when churches close, they erode social infrastructure opportunities that limit the number of places for public health interventions (such as vaccination sites). Fewer structures then possibly correlate with higher disease burden since other public health infrastructure (e.g., community health centers or clinics) were beyond capacity during the initial waves of the pandemic. Observational longitudinal data that examine church closings from the start of the COVID-19 pandemic into the current pandemic are needed to strengthen causal inference about this topic.
This study is limited in that churches are only one type of religious institution. Other types of religious classifications such as non-profits with a religious mission, or mosques, or temples were not examined neither were differences by denomination type (e.g., share of Catholic churches vs Protestant churches). Our findings may thus reflect church-specific estimates of associations. Residual confounding may be an issue here, as it is in all epidemiologic studies. We attempted to address confounding by adjusting for a vast range of covariates that are often implicated in area-level disparities and those associated with COVID-19, such as socioeconomic status, minority status, housing, household composition, overcrowding, and the presence of community health centers [4, 28, 30].
Other challenges may be that our findings are sensitive to geography. Specifically, COVID-19 case rates across cities will vary based on data capturing systems and by size and number of administrative units within cities. Therefore, results should not be interpreted comparatively across cities. Moreover, the cities cannot be analyzed together since their boundaries are not contiguous. According to the modifiable areal unit problem (MAPU), these findings may not be generalizable to other geographic units (e.g., county or census tract). Results are not generalizable to cities in other census regions such as the south where there is a greater density of churches as well as higher COVID-19 infection rates.
An important strength of this study is that, to our knowledge, it is the first to quantify inequities in church closings across multiple cities. This is the first study to quantify the extent to which inequities in church closings are related to a public health outcome. The findings represent an important methodological advancement in the assessments of social determinants of health risks. We present a novel way to operationalize the religious ecology/landscape and test the associations with population health. Replicate studies across different regions and at different geographic boundaries are next research steps. This work also advances religious ecology/landscape theory, which traditionally focuses on mechanisms that are specific to when churches exist or social networks within churches (e.g., health care provisions provided by churches to address some concern). Here, we launch a new program of research to theorize on and study the effects of what happens when church infrastructure is eroded and networks of people are displaced physically (or as they start to move completely online).
Conclusion: Community Health Implications
Churches are sacred spaces that often perform critical safety net functions to buttress disease risk that correspond to inequities in distribution of social and economic resources that lead to social vulnerability. These establishments are indispensable to public health prevention efforts aimed at advancing health equity. When churches close, all people (not only those who attend religious services) in that geographic context become vulnerable to higher exposure of risk that results in higher disease rates. The physical closings of churches should be monitored, included, and routinely analyzed in epidemiologic studies as an indicator of neighborhood social vulnerability. Results from this study provides preliminary evidence to inform conversations about public policy, economic development, and other health equity policy initiatives to protect the public’s health.
Acknowledgements
This project/publication was made possible through the support of Grant 62646 from the John Templeton Foundation. The opinions expressed in this publication are those of the author(s) and do not necessarily reflect the views of the John Templeton Foundation.
Declarations
Competing Interests
All authors have no competing interests to report.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.The COVID Tracking Project. The COVID racial data tracker. 2020. Available from: https://covidtracking.com/race. Accessed 3 Aug 2023.
- 2.Kim B, et al. Neighborhoods and COVID-19: current research, future directions, and place-based interventions. In: Duncan DT, Kawachi I, Morse SS, et al., editors. The social epidemiology of the COVID-19 pandemic. Oxford, UK: Oxford University Press; 2023. pp. 341–362. [Google Scholar]
- 3.Wali B, Frank LD. Neighborhood-level COVID-19 hospitalizations and mortality relationships with built environment, active and sedentary travel. Health Place. 2021;71:102659. doi: 10.1016/j.healthplace.2021.102659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schmiege D, et al. Associations between built environment factors and SARS-CoV-2 infections at the neighbourhood level in a metropolitan area in Germany. J Urban Health. 2023;100:40–50. doi: 10.1007/s11524-022-00708-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ransome Y, Taggart T, Kawachi I. Religion, spirituality and COVID-19. In: Duncan DT, Kawachi I, Morse SS, editors. The social epidemiology of the COVID-19 pandemic. Oxford: Oxford University Press; 2023. pp. 395–419. [Google Scholar]
- 6.Hammer L, et al. High SARS-CoV-2 attach rate following exposure at a choir practice-Skagit County Washington. Morb Mortal Wkly Rep. 2020;69(19):606–610. doi: 10.15585/mmwr.mm6919e6. [DOI] [PubMed] [Google Scholar]
- 7.Brewer LC, et al. Establishing a SARS-CoV-2 (COVID-19) drive-through collection site: a community-based participatory research partnership with a federally qualified health center. Am J Public Health. 2021;111(4):658–662. doi: 10.2105/AJPH.2020.306097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dada D, et al. Strategies that promote equity in COVID-19 vaccine uptake for Black communities: a review. J Urban Health. 2022;99(1):15–27. doi: 10.1007/s11524-021-00594-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bigelow BF, et al. Community testing and SARS-CoV-2 rates for Latinxs in Baltimore. Am J Prev Med. 2021;60(6):e281–e286. doi: 10.1016/j.amepre.2021.01.005. [DOI] [PubMed] [Google Scholar]
- 10.Eyewitness News. Coronavirus news: New York City churches to become temporary COVID-19 testing sites. 2020. Available from: https://abc7ny.com/nyc-coronavirus-testing-update-corona-virus-cases/6166852/. Accessed 3 Aug 2023.
- 11.Lee KC, et al. Operationalizing equity: a rapid-cycle innovation approach to COVID-19 vaccination in Black neighborhoods. NEJM Catalyst. 2021;2(2):1–19. [Google Scholar]
- 12.Idler EL, editor. Religion as a social determinant of public health. New York, NY: Oxford University Press; 2014. [Google Scholar]
- 13.Neuman S. The faithful see both crisis and opportunity as churches close across the country. Religion. 2023. Available from: https://www.npr.org/2023/05/17/1175452002/church-closings-religious-affiliation. Accessed 3 Aug 2023.
- 14.Jordan A, et al. Breaking through social determinants of health: results from a feasibility study of Imani Breakthrough, a community developed substance use intervention for Black and Latinx people. J Subst Use Addict Treat. 2023;153(October):209057. doi: 10.1016/j.josat.2023.209057. [DOI] [PubMed] [Google Scholar]
- 15.Trinitapoli J, Ellison CG, Boardman JD. US religious congregations and the sponsorship of health-related programs. Soc Sci Med. 2009;68(12):2231–2239. doi: 10.1016/j.socscimed.2009.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Riediger ND, et al. A descriptive analysis of food pantries in twelve American states: hours of operation, faith-based affiliation, and location. BMC Public Health. 2022;22(1):525. doi: 10.1186/s12889-022-12847-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kiser M, Lovelace K. A national network of public health and faith-based organizations to increase influenza prevention among hard-to-reach populations. Am J Public Health. 2019;109(3):371–377. doi: 10.2105/AJPH.2018.304826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.DeHaven MJ, et al. Health programs in faith-based organizations: are they effective? Am J Public Health. 2004;94(6):1030–1036. doi: 10.2105/AJPH.94.6.1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stack L. Cathedral of St. John the Divine, including Crypt, will become a hospital. The New York Times. 2020. Available from: https://www.nytimes.com/2020/04/06/nyregion/cathedral-st-john-the-divine-coronavirus-fieldhospital.html. Accessed 3 Aug 2023.
- 20.Northwell Health. Raising health raises everyone: mobilizing for health equity, 2020 annual report. Annual Report. 2021. Available from: https://www.northwell.edu/sites/northwell.edu/files/2021-08/nwh-annual-report-2020.pdf. Accessed 3 Aug 2023.
- 21.Evans A, Webster J, Flores G. Partnering with the faith-based community to address disparities in COVID-19 vaccination rates and outcomes among US Black and Latino populations. JAMA. 2021;326(7):609–610. doi: 10.1001/jama.2021.12652. [DOI] [PubMed] [Google Scholar]
- 22.Gaughan CH, et al. Religious affiliation and COVID-19-related mortality: a retrospective cohort study of prelockdown and postlockdown risks in England and Wales. J Epidemiol Community Health. 2021;75(6):509–514. doi: 10.1136/jech-2020-215694. [DOI] [PubMed] [Google Scholar]
- 23.SICCODE.COM. SIC code 8661 - religious organizations. 2023. Available from: https://siccode.com/sic-code/8661/religious-organizations. Accessed 3 Aug 2023.
- 24.NAICS Association. SIC industry description - industry 8661 - religious organizations. 2023. Available from: https://www.naics.com/sic-industry-description/?code=8661. Accessed 3 Aug 2023.
- 25.Data Axle USA. Creative solutions to reach your target audience. 2023. Available from: https://leads.dataaxleusa.com/UsBusiness/Selections. Accessed 3 Aug 2023.
- 26.Data Planet. Data axle reference solutions: exploring data axle historical US business in data planet. 2023. Available from: https://data-planet.libguides.com/c.php?g=1205021&p=8813556. Accessed 3 Aug 2023.
- 27.Ransome Y, et al. Churches are closing in predominantly Black communities - why public health officials should be concerned. 2022. Available from: https://www.brookings.edu/blog/how-we-rise/2022/05/03/churches-areclosing-in-predominantly-black-communities-why-public-health-officials-should-be-concerned/. Accessed 3 Aug 2023.
- 28.Kim B, et al. COVID-19 testing, case, and death rates and spatial socio-demographics in New York City: an ecological analysis as of June 2020. Health Place. 2021;68:102539. doi: 10.1016/j.healthplace.2021.102539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ransome Y, et al. Neighborhood social cohesion and inequalities in COVID-19 diagnosis rates by area-level Black/African American racial composition. J Urban Health. 2021;98(2):222–232. doi: 10.1007/s11524-021-00532-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tipirneni R, et al. Associations of 4 geographic social vulnerability indices with US COVID-19 incidence and mortality. Am J Public Health. 2022;112(11):1584–1588. doi: 10.2105/AJPH.2022.307018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Luan H, et al. HIV infection prevalence significantly intersects with COVID-19 infection at the area level: a US county-level analysis. J Acquir Immune Defic Synd. 2021;88(2):125. doi: 10.1097/QAI.0000000000002758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Leroux BG, Lei X, Breslow N. In: Estimation of disease rates in small areas: a new mixed model for spatial dependence. Halloran ME, Berry D, editors. New York, NY: Springer-Verlag; 1999. pp. 179–191. [Google Scholar]
- 33.Duncan EW, White NM, Mengersen K. Spatial smoothing in Bayesian models: a comparison of weights matrix specifications and their impact on inference. Int J Health Geogr. 2017;16(1):1–16. doi: 10.1186/s12942-017-0120-x. [DOI] [PMC free article] [PubMed] [Google Scholar]