Abstract
Background
In neurorehabilitation, problems with visuospatial attention, including unilateral spatial neglect, are prevalent and routinely assessed by pen-and-paper tests, which are limited in accuracy and sensitivity. Immersive virtual reality (VR), which motivates a much wider (more intuitive) spatial behaviour, promises new futures for identifying visuospatial atypicality in multiple measures, which reflects cognitive and motor diversity across individuals with brain injuries.
Methods
In this pilot study, we had 9 clinician controls (mean age 43 years; 4 males) and 13 neurorehabilitation inpatients (mean age 59 years; 9 males) recruited a mean of 41 days post-injury play a VR visual search game. Primary injuries included 7 stroke, 4 traumatic brain injury, 2 other acquired brain injury. Three patients were identified as having left sided neglect prior to taking part in the VR. Response accuracy, reaction time, and headset and controller raycast orientation quantified gameplay. Normative modelling identified the typical gameplay bounds, and visuospatial atypicality was defined as gameplay beyond these bounds.
Results
The study found VR to be feasible, with only minor instances of motion sickness, positive user experiences, and satisfactory system usability. Crucially, the analytical method, which emphasized identifying 'visuospatial atypicality,' proved effective. Visuospatial atypicality was more commonly observed in patients compared to controls and was prevalent in both groups of patients—those with and without neglect.
Conclusion
Our research indicates that normative modelling of VR gameplay is a promising tool for identifying visuospatial atypicality after acute brain injury. This approach holds potential for a detailed examination of neglect.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12984-023-01283-9.
Keywords: Brain injury, Cognitive assessment, Classification, Immersive virtual reality, Unilateral visuospatial neglect
Background
Assessments of visuospatial attention problems following brain injury have focused on unilateral spatial neglect, which classically manifests as a bias toward ipsilesional space that renders objects in the contralesional space difficult to orient toward, perceive, and act upon [1–4]. Symptoms can manifest in activities of daily living, such as eating, when a person might eat food only from one side of their plate, and associate robustly and independently with poor prognosis, including long-term functional disability [5–9]. Although attention can recover during rehabilitation [10], current treatments produce uncertain evidence of efficacy [11, 12]. Neglect occurs most commonly following right-hemisphere stroke [13], but can also follow left-hemisphere stroke [14], traumatic brain injury (TBI) [15], and other causes of acquired brain injury (ABI) [16, 17]. Prevalence estimates of neglect vary widely (e.g., 24–68%) [18, 19], reflecting a variety of factors, including limitations of standard assessments [20].
In neurorehabilitation practice and research, pen-and-paper tests, such as clock drawing and letter cancellation, and behavioural tests routinely assess neglect [21–23]. While convenient, pen-and-paper tests have limited sensitivity, sometimes failing to detect even severe neglect symptoms [24, 25]. They also have variable specificity, for example, detecting problems with executive function rather than visuospatial attention [26, 27]. Many pen-and-paper tests do not assess severity or identify subtypes [22, 28]. For neglect assessment, computer-based methods provide alternatives. Among computer-based methods, immersive virtual reality (VR) appears ideally suited for neurorehabilitation and detailed neglect assessment [22, 29–33].
Immersive VR involves a headset (i.e., a head-mounted display) that simulates stereoscopic vision and allows the player to turn their head to explore three-dimensional (3D) computer-generated worlds [34]. VR hand controllers allow the player to select and interact with virtual objects requiring motoric coordination. VR uniquely and flexibly combines experimental control with sensory experiences that simulate naturalistic perception and motivate naturalistic behaviour [30]. This provides accessibility, the opportunity to individualise gameplay, and the capacity to map visuospatial attention with ecological validity (i.e., closer to a person's full field of vision as opposed to an A4 sheet of paper size).
VR is well suited to clinical settings as it is possible to manipulate the virtual world and build environments that might be unsafe for patients in the real world [35, 36, 49]. VR is also easily gamified therefore highly engaging [37, 38] facilitating participation in treatment [39]. The potential for VR to motivate patients in treatment, and for continuity in assessment and treatment approach, is another benefit to VR over current assessment approaches.
VR neglect tests have long been of interest and have been systematically reviewed and discussed [22, 33, 40–43]. However, the term “VR” has broadly included immersive VR [31, 44–57], precursor systems with stereoscopic shutter glasses [29, 58–61], headsets with incomplete degrees of freedom [62, 63], augmented reality systems [64–66], and 3D virtual environments presented on two-dimensional (2D) displays [54, 67–71]. There are also parallel computer-based neglect tests using 2D displays [24, 25], touch screens [28], and eye tracking [72–78]. Among these methods, immersive VR motivates behaviour most naturalistically while providing maximal sensory control.
In Table 1, we have summarised immersive VR neglect assessment studies [31, 44–57]. Collectively, these studies have shown that immersive VR manifests neglect symptoms in gameplay based on navigation, detection, obstacle avoidance, free viewing, street crossing, and cancellation. Additionally, these studies have shown that immersive VR can measure attention in ecologically valid contexts [49, 54, 55], correlate with neglect severity on standard tests [31, 50], detect mild neglect [51], distinguish between acute and chronic injuries [48], scale in difficulty for the individual [50], reflect behavioural responses to changing task demands [45, 55], measure orientation [47, 57] and heading direction [46], reveal the time course of recovery [51, 56], and reveal both spatial and non-spatial attention problems [53].
Table 1.
Immersive VR neglect assessments
| Study | Gameplay | Samplea | Neglect determinationb | Feasibilityc | Chronicityd (M days) |
Chronicityd (SD days) |
Case inferences |
|---|---|---|---|---|---|---|---|
| Current study | Localisation | Stroke, TBI, ABI, L/R/B | CLOX**, LCT**, LiCT**, observation* | GEQ, SUS, SSQ, chronicity | 41 | 29 | Normative modelling |
| Aravind et al. [38] | Navigation, avoidance | LHS, RHS | MVPT**, LCT** | None | 413 | 706 | Descriptives |
| Aravind and Lamontagne [39] | Navigation, avoidance | RHS | MVPT**, LCT**, BeT** | None | 339 | 150 | None |
| Aravind and Lamontagne [40] | Navigation, avoidance | RHS | MVPT**, LCT**, BeT** | None | 339 | 148 | Example results |
| Hougaard et al. [41] | Free viewing | RHS | KF-NAP^ | None | 84 | 103 | Normative modelling |
| Jannink et al. [42] | Detection | LHS, RHS | BIT^ | None | 69 | 25 | None |
| Kim et al. [43] | Street crossing | RHS | Deficits in ADLs^ | None | 116 | 97 | None |
| Knobel et al. [30] | Cancellation | RHS | SNT** | SUS, SSQ | 76 | 36 | None |
| Knobel et al. [44] | Detection | RHS | CBS^, SNT** | SUS, SSQ, IPQ, PGTQ | 64 | 33 | Descriptives |
| Numao et al. [45] | Detection | RHS | Observation, LBT**, LiCT**, SCT**, CBS^ | None | 10 | Case study | |
| Ogourtsova et al. [46] | Navigation | RHS | LBT**, SCT**, AT**, observation* | None | 675 | 589 | Descriptives |
| Ogourtsova et al. [47] | Navigation, detection | RHS | LBT**, SCT**, AT**, observation* | None | 675 | 589 | Descriptives |
| Ogourtsova et al. [48] | Navigation, detection | RHS | LBT**, SCT**, AT**, observation* | None | 675 | 589 | Descriptives |
| Peskine et al. [49] | Navigation | RHS | BeT**, CBS^ | None | 490 | 865 | Descriptives |
| Yasuda et al. [50] | Detection | RHS | Observation^, LiCT**, LBT**, CBS^ | None | 15 | Case study | |
| Yasuda et al. [51] | Detection | RHS | Observation^, TMT**, BIT** | Motion sickness | 109 | Case study |
aLHS = left hemisphere stroke, RHS = right hemisphere stroke, L/R/B = left, right, and bilateral injuries
b** = pen-and-paper test, ^ = behavioral test, * = clinical observation, ADLs^ = Activities of daily living, Albert’s Test** = Albert’s Test, AT** = Apples Test, BIT^ = Behavioural Inattention Test, BeT** = Bells test, CBS† = Catherine Bergego Scale, CLOX** = CLOX: An Executive Clock Drawing Task, LBT** = Line Bisection Test, LC** = Letter Cancellation, LCT** = Letter Cancellation Test, LiCT** = Line Cancellation Test, KF-NAP^ = Kessler Foundation Neglect Assessment Process, MVPT** = Motor Free Visual Perceptual Test, SCT** = Star Cancellation Test, SNT** = Sensitive Neglect Test, TMT** = Trail Making Test
cGEQ** = Game Experience Questionnaire, IPQ** = Igroup Presence Questionnaire, PGTQ** = Perception of Game Training Questionnaire, SSQ** = Simulator Sickness Questionnaire, SUS** = System Usability Scale
dTime since injury
Immersive VR supports the notion that neglect affects both spatial and non-spatial attention [53]. A touchscreen neglect assessment recently extended this result and showed that neglect comprises subtype clusters defined by spatial and non-spatial effects [28]. Thus, neglect may not be unitary but reflect interactions between spatial and non-spatial attentional processes [28, 53, 79–81]. By extension, attention problems following brain injury may manifest distinctly across individuals in multidimensional trait space [82–84], defined here as individual-level behavioural performance patterns across a comprehensive suite of visuospatial attentional metrics.
Immersive VR neglect tests have progressed considerably, previous studies have several characteristics in common, as highlighted in Table 1. First, previous studies almost exclusively used right hemisphere stroke samples. While this approach provides scientific control, attention problems following left hemisphere stroke and ABIs were potentially missed. Second, previous studies determined neglect using existing assessments: pen-and-paper tests, behavioural tests, and clinical observation. These tests defined neglect and non-neglect groups, and thus the accuracy of existing pen-and-paper tests proceeded the accuracy of immersive VR. Third, previous studies focused on lateralised effects with an incomplete evaluation of non-lateralised effects. Fourth, most previous studies did not report feasibility, operationalised here as the acceptability of the VR gameplay and hardware. Further, most group studies recruited patients several months to years post-injury. Hence, feasibility for acute and subacute brain injury has not been broadly established. Fifth, although case studies and some group studies reported individual-level VR descriptive statistics, all but one study [47] did not report individual-level VR inferential statistics. This limits immersive VR for individualised rehabilitation.
To build on past work, we developed a self-referential immersive VR assessment of brain injury attention problems, including neglect. We achieved this via normative modelling, which provides individual-level statistical inferences based on expected patterns [47, 85–88]. We implemented normative modelling using a simple modification of outlier analysis. This leads us to introduce a new concept and mathematical property named “visuospatial atypicality”, which refers to whether the player’s performance on attentional metrics fell beyond outlier cut-offs based on patient and control groups. Visuospatial atypicality allowed us to examine attention problems across a variety of metrics that mapped flexibly onto individual-level patterns in multidimensional trait space.
This study was a pilot to examine the overall feasibility of VR, to prototype game levels, and to prototype the atypicality analysis among a broadly defined brain injury sample. The data were collected during heightened restrictions due to the global COVID pandemic and thus were challenging to obtain and of historical significance. The following results were based on the limited sample size and heterogeneous clinical characteristics of participants and are therefore preliminary. Therefore, the purpose of this report was to highlight the analysis methods, rather than the results. We recommend that future studies perform similar analyses with a larger sample size to establish atypicality cut-offs. Nonetheless, our new approach yields insights that can inform future extensive investigations.
Methods
Ethics approval
The current pilot study was part of a research protocol investigating the feasibility and validity of The Attention Atlas (AA) for neglect detection for inpatients with brain injury [32]. The study was approved by The Human Research Ethics Committees of Metro South Health (HREC/2021/QMS/70556) and Griffith University (GU Ref. No: 2021/179) and received Site-Specific Assessment authorisation from Metro South Health (SSA/2021/QMS/70556). All participants provided informed written voluntary consent consistent with the Declaration of Helsinki. The experiment was performed in accordance with relevant guidelines and regulations.
Participants
We recruited clinician controls without brain injury and patients with brain injury from The Rehabilitation and Geriatrics Ward at Logan Hospital in Logan, Australia. Patients were eligible if they were clinically stable, had no history of epilepsy, had no reported visual field problems, had intact mobility of one or both hands, were not strongly susceptible to motion sickness (Simulator Sickness Questionnaire (SSQ) [89] scores < moderate nausea), and had high cognitive functioning on the orientation to time and space questions of Mini-Mental State Examination (scores ≥ 6 out of 10) [84]. Clinician controls were also required to be unsusceptible to motion sickness (SSQ scores < moderate nausea).
For patients and controls, we recorded age and sex. For patients, we additionally recorded time since injury, time in rehabilitation, diagnosis (stroke, TBI, and other ABIs), injured hemisphere (left, right, bilateral), and the Functional Independence Measure (FIM) [85]. The FIM is often routinely collected in Australian clinical practice and assesses independence on 18 activities of daily living on a 7-point scale (1 = total assistance, 2 = maximal assistance, 3 = moderate assistance, 4 = minimal assistance, 5 = supervision, 6 = modified independence, 7 = complete independence). The FIM is composed of two subscales, Motor and Cognition, with FIM Total calculated as the sum of the two. We expressed FIM on the original 7-point scale by dividing summary scores by the number of items (13 for Motor, 5 for Cognition, and 18 for Total).
Procedure
A clinician team member examined medical files to assess patient eligibility, and eligible and interested patients provided verbal consent for academic team members to undertake recruitment. Following recruitment, an experienced neuropsychologist (author ML) administered three pen-and-paper tests of neglect to patients. Two days later, patients played VR for 19.5 to 28.7 min (see “Game levels”).
For the VR game, the experimenter first described immersive VR and the game and informed participants that there were free to discontinue at any time and for any reason. The experimenter fitted the VR headset. Participants first experienced the aurora night environment of Steam VR, with colourful auroras, mountains in the background, stars in the sky, and a ringed grid on the floor. After the game, participants reported their subjective experiences of VR on questionnaires assessing simulator sickness, game experience, and system usability. The experimenter also described the gameplay results, emphasising the developmental nature of the technology and analyses, describing areas of strengths, and avoiding phrases such as “attention deficit”, “spatial bias”, and “abnormality”.
Pen-and-paper neglect tests
Three pen-and-paper tests presented a page at the patient’s midline. Patients had neglect if indicated on ≥ 1 test, and the neuropsychologist attributed the results to neglect rather than other causes. CLOX required patients to draw the numbers and hands on an analogue clock face to read legibly a time of 1:45. Once patients understood and drawing began, we provided no further help [95]. A preponderance of numbers on either side of the clock indicated neglect. The single letter cancellation test (SLCT) asked patients to cross out each letter “H” among an array of uppercase letters on a page. Four or more omissions on one half of the page compared with the other indicated neglect. Albert’s Test asked patients to cross out all the lines [87]. The neuropsychologist illustrated this by crossing out the five central lines. We encouraged patients to continue until they had crossed out all the lines. If > 70% of uncrossed lines were on one half of the page, neglect was indicated [88].
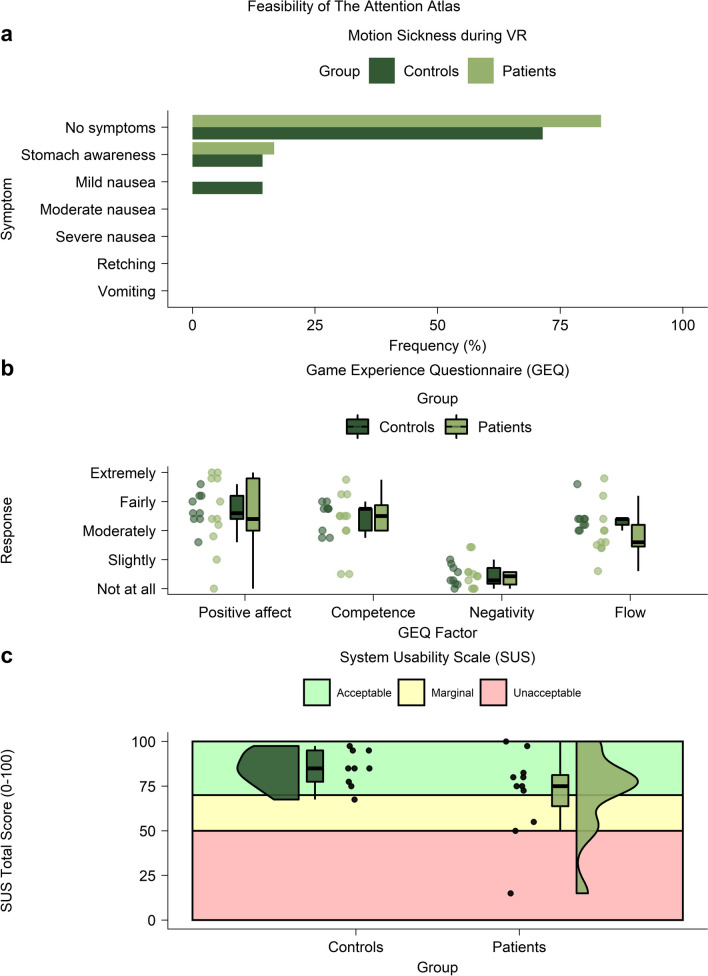
Feasibility of The Attention Atlas
The SSQ [89] asked players whether they felt motion sickness during VR (1 = no symptoms, 2 = stomach awareness, 3 = mild nausea, 4 = moderate nausea, 5 = severe nausea, 6 = retching, 7 = vomiting). The game experience questionnaire revised (GEQ-R) [90, 91] asked players to indicate gameplay experiences on a five-point scale (1 = not at all, 2 = slightly, 3 = moderately, 4 = fairly, 5 = extremely) on 25 items, including “I felt content” and “I felt skilful”. Four factors of positive affect, competence, negativity, and flow were the mean of individual items. The SUS [92–94] asked players to rate VR hardware usability on 10 five-point (strongly disagree, disagree, neutral, agree, strongly agree) items, including “I think I would like to use this system frequently” and “I found the system unnecessarily complex”. Summed total scores categorised system usability as acceptable (70 to 100), marginal (50 to 70), or unacceptable (0 to 50).
The Attention Atlas
Overview
We used The Attention Atlas [32] to assess visuospatial atypicality. The Attention Atlas has the player search for a single target among distractors (Fig. 1a) [94, 95]. Players sat in a non-swivelling chair or wheelchair. Players used their preferred hand or both hands for increased stability as preferred. Patients with upper limb paralysis used their more mobile hand. The experimenter sat or stood directly behind the player where possible and provided ongoing instructions, monitoring, and encouragement facilitated by the experimenter’s computer display. We used spherical coordinates (12.5° radial spacing, 15.0° concentric spacing, 2-m radius) to position search array elements (Fig. 1b) and an HTC Vive Pro headset (HTC, Taiwan) running on an Alienware Aurora R8 desktop computer (i7 9700, RTX 2070).
Fig. 1.
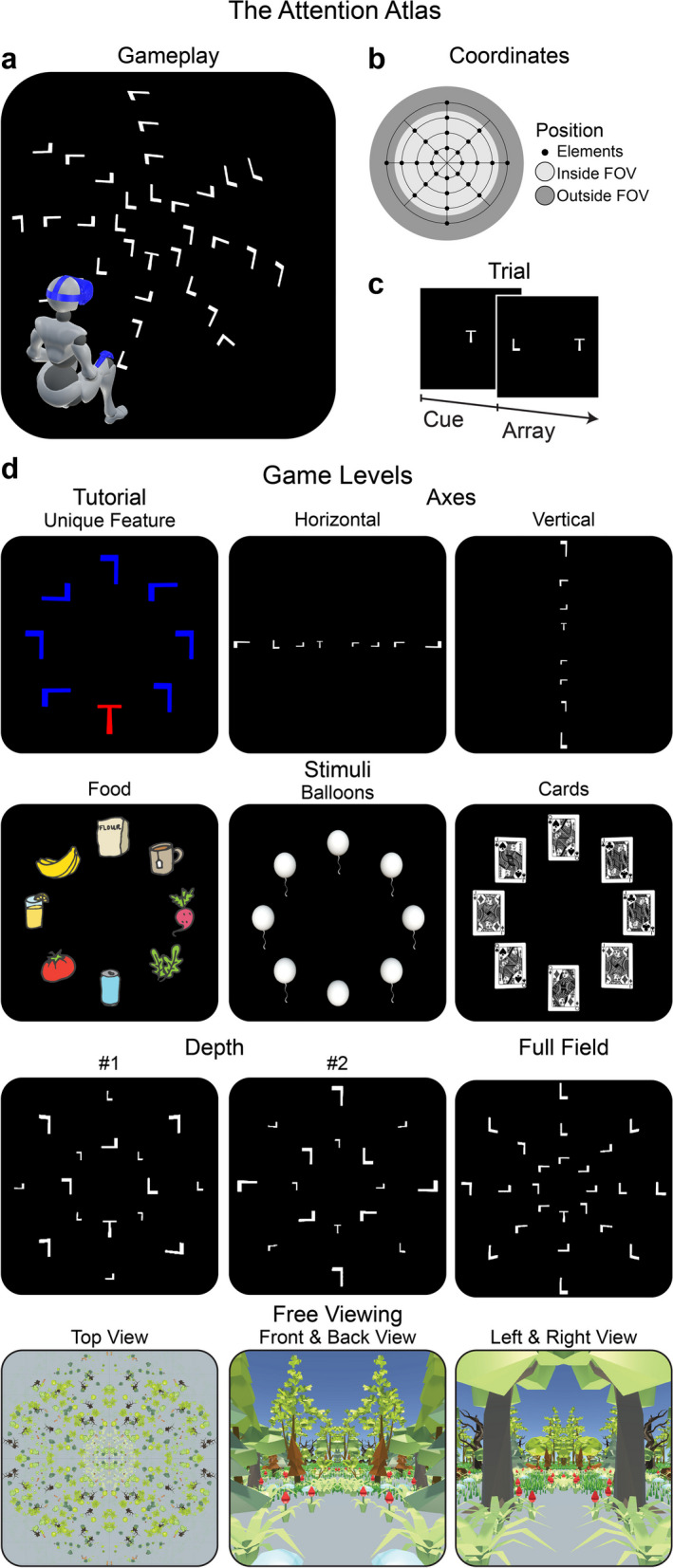
The Attention Atlas. a Visual search localisation gameplay. Array elements were positioned on a spherical surface with an origin at the headset position, calibrated at the start of each level [31]. This panel depicts the full field level. b Coordinates. Array elements were presented on a spherical grid. Each game level used a subset of possible positions, which could appear within the central field of view (FOV) or towards or beyond its edge, requiring head and eye movements for target localisation. For the axes level, the most eccentric horizontal and vertical positions fell outside the central FOV. c Cue/array trial structure. Cues and arrays were presented until an element was selected. d Game levels are depicted from the first-person perspective. Stimuli are scaled for clarity. Those with eight elements were presented on a single concentric ring presented 15° from central vision. The tutorial, excluded from analysis, was a search of a red “T” among blue “Ls”. Axes was a search for a “T” among “Ls” positioned horizontally or vertically on separate trials. Stimuli were food, cards, and balloons on separate trials. For food, the target and distractors are randomly selected at the beginning of each trial from 121 food icons. The queen of diamonds was the target for cards. For balloons, the target was a balloon without a string located among balloons with strings. Depth presented elements simultaneously at one of two depths: a near-surface (2 m) and a far-surface (4 m). Full field presented elements in four concentric rings. Free viewing depicted a low-resolution polygon forest, which surrounded the player in 360°. We instructed players to “look around” and report what they could see
On each trial, a target cue appeared centrally. After the player selected the cue, the search array appeared, and the player located the target among distractors (Fig. 1c). The player selected the cue and target by pointing the VR hand controller and virtual laser pointer and pressing the thumb button. We instructed the player to perform as quickly and accurately as possible. If the player could not find the target, we instructed them to select one of the distractors. We did not assign such responses a unique error type. Without constraints, the player moved their head, eyes, and hand to locate and select the target. Correct target localisation was rewarded with a colourful confetti particle system instantiated at the target’s 3D coordinates. Distractor selection produced no confetti. The AA uses basic gamification features such as goals, rapid feedback and reinforcement, visible feedback [96–98], using levels (or an increase in difficulty), clear and simple game ‘rules’ [97, 98] and most importantly for patient engagement, fun and playfulness [97].
Game levels
Of the clinician controls, the first n = 4 undertook a longer game with eight levels. Based on their feedback, we reduced the total minimum level gameplay duration from 28.7 min to 19.5 min by dropping two levels and shortening others. Thus, the remaining controls (n = 5) and all patients (N = 13) undertook a shorter game with six levels (named tutorial, axes, stimuli, depth, full field, and free viewing). All levels lasted a fixed minimum duration and ended when an element (target or distractor) was selected. There was no fixed maximum duration (i.e., time-out). The level duration was proportional to the number of array elements multiplied by the number of stimulus combinations (tutorial, 0.5 min; axes, 3.0 min; stimuli, 4.5 min; depth 6.0 min; full field, 4.5 min; free viewing, 1.0 min). Variations of spatial extent and stimulus properties across game levels provided game progression (Fig. 1; see Additional file 1: Video S1 online—note, this is the clinician view, patients only saw the targets and distractors as in Fig. 1).
Statistical analysis
Inferential statistics
We used non-parametric methods throughout to account for non-Gaussian distributions. The univariable and bivariable outlier analyses described below make no distributional assumptions.
Demographics
We compared FIM Motor and FIM Cognitive scores using Wilcoxon signed-rank tests.
Feasibility of The Attention Atlas
We compared the subjective experiences of the patient and control groups. For motion sickness, we used a χ2 goodness-of-fit test. For game experience and system usability, we used Wilcoxon ranked sum tests to assess midpoints and Levene’s test of homogeneity to assess variance.
Definition and summary of visuospatial atypicality
Visuospatial atypicality was a Boolean variable (0, 1) calculated for each attention metric and summarised across game levels as the mean, a Boolean proportion (0 to 1). We tabulated atypicality in a summary matrix (attention metric × player identifier [ID]). Player IDs were uniquely assigned and sequentially numbered according to the participation order. For each attention metric, we defined atypical gameplay as:
where Bplayer is the Boolean (0, 1) of whether the game was an outlier, Mplayer is the game measurement, Q1 is the first quartile, Q3 is the third quartile, and IQR is the inter-quartile range for the specific metric. We chose a Boolean representation for atypicality to standardize various measures onto a single scale, making it easier both to compare them and to visualize patterns of atypicality.
We compared atypicality prevalence between patient and control groups using a χ2 goodness-of-fit test, with typicality (typical, atypical) counts tabulated by group. Counts were derived by summing across players and metrics within each summary matrix.
Attention metrics
There were 14 attention metrics based on three primary categories: accuracy (%), RT (s), and raycasts (°) for the headset and controller. Accuracy, RT, headset latitude mean, headset longitude means, controller latitude means, and controller longitude means were computed for each game level. The headset and controller forward vectors cast rays to hit a spherical surface (2-m radius) positioned at the headset origin, calibrated before each game level [31]. Raycasts were converted from Cartesian (x, y, z) to spherical coordinates (latitude, longitude, 2-m radius).
Accuracy and RT were pooled across game levels to derive “spatial preference” difference scores (Δ% and Δs, respectively), contrasting four spatial quadrants (left, right, up, down) and three eccentricities (12.5°, 25.0°, 37.5°). We recombined the same trials separately for each contrast. We contrasted left and right (LR) quadrants, up and down (UD) quadrants, eccentricities of 12.5° and 25.0°, and eccentricities of 25.0° and 37.5°. For quadrants, we ordered subtraction terms separately for RT and accuracy, such that positive scores showed a spatial preference for right and up quadrants, and negative scores showed a spatial preference for left and down quadrants. For eccentricity, we ordered subtraction terms similarly for accuracy and RT. RTs were calculated for correct trials after individual-level outlier removal, performed separately for each level (level performance) or trials altogether (spatial preference). RTs outliers were defined by:
where BRT is the Boolean of whether the trial RT was an outlier, TRT is the trial RT measurement.
Data availability
All relevant anonymised and cleaned raw data and results are freely and publicly accessible on Open Science Framework (https://osf.io/staj7/) in Study1DataCleanCopy.zip (cleaned game IDs: study.Study1.gameLogMaster.feather; cleaned demographics: study.Study1.GUID.demographics.feather; cleaned feasibility questionnaires: study.Study1.questionnaires.feather; player summary results: PlayerSummary.py\; raw VR data: _RECORDINGS\_DATA; raw results: _RECORDINGS\_RESULTS\).
Code availability
Complete source code for the latest version of the analysis is available at (https://osf.io/staj7/; AA.Diagnostics.zip). Complete source code and most source files for the latest version of The Attention Atlas are available at (https://osf.io/staj7/; AA.Standalone.zip). LemonadePixel’s food illustrations (https://www.shutterstock.com/image-vector/hand-drawn-food-drink-icons-breakfast-716980507) and PolyWorks’ low-resolution polygon forest (https://assetstore.unity.com/packages/3d/environments/low-poly-forest-pack-polyworks-52733) are available in the build but not in the source files, since we do not own the distribution rights.
The games described in this report can be run from the presets (longer: CliniciansTest1.game.json; shorter: CliniciansTests2.game.json; demonstration: CliniciansTestsDemo.game.json) on the HTC Vive, HTC Vive Pro, and HTC Vive Pro Eye. Author DRP programmed the analyses in Python 3.10.6 and R 4.2.1 and The Attention Atlas in The Unity Game Engine 2019.4.20f1 on Windows 10.
Results
Demographics
Clinician controls (N = 9) completed all game levels (axes, stimuli, depth, full field, free viewing). Of the 18 patients recruited, two withdrew before VR, and one was excluded before VR due to susceptibility to motion sickness (SSQ score of vomiting). Incomplete or invalid data excluded two patients; the first patient discontinued during the second game level due to a lack of enjoyment; the second had unreported visual field loss. Therefore, the sample was N = 9 controls and N = 13 patients. Median ages were 59 years (IQR, 21 years) for patients and 43 years (IQR, 14 years) for controls. For patients, there were nine males, and for controls, there were four males.
Table 2 presents patient demographics. We recruited patients at a mean of 41 days (SD, 29 days, range, 17 to 125 days) post-injury, with patients having spent a mean of 14 days (SD, 14 days, range, 3 to 53 days) at inpatient hospital rehabilitation. The hospital diagnosed seven with stroke, four with TBI, and two with other ABI. Brain injuries were right-lateralised for six, left-lateralised for four, and bilateral for three. Patients ranged from complete independence to complete dependence on the functional independence measures (FIMs). Patients showed significantly greater cognitive (median, 5.6; IQR, 1.8) than motoric independence (median, 3.4; IQR, 3.3; W = 8.0, P < 0.001). Three patients (23.1%; patients 17, 19, 21) showed left-side neglect on ≥ 1 pen-and-paper test and the neuropsychologist agreed the result was due to neglect rather than other causes (identified in Table 2 as ‘neglect present’). One patient (patient 9) showed performance consistent with right-side neglect on the SLCT, but the neuropsychologist attributed this to causes other than neglect.
Table 2.
Demographics of the 13 brain injury patients
| Clinical characteristics | Neglect Pen-and-Paper tests | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Game ID | Age (Years) | Sex | Days since injury | Days in rehab | Diagnosis | Injured hemisphere | FIM motora | FIM cognitiona | FIM Totala | Neglect present (0/1)b | Neglected hemispace | CLOX (0/1) | SLCT (0/1) | Albert’s Test (0/1) |
| 9 | 52 | Male | 53 | 6 | TBI | Bilateral | 3.4 | 6.2 | 4.2 | 0 | Right | 0 | 1 | 0 |
| 10 | 59 | Male | 52 | 4 | TBI | Left | 6.5 | 5.8 | 6.3 | 0 | 0 | 0 | 0 | |
| 11 | 37 | Male | 37 | 7 | TBI | Left | 6.6 | 5.0 | 6.2 | 0 | 0 | 0 | 0 | |
| 12 | 83 | Male | 17 | 7 | Stroke | Left | 6.0 | 6.2 | 5.9 | 0 | 0 | 0 | 0 | |
| 13 | 65 | Female | 22 | 6 | ABI | Right | 5.0 | 5.6 | 5.1 | 0 | 0 | 0 | 0 | |
| 14 | 80 | Female | 15 | 7 | Stroke | Right | 1.6 | 4.0 | 2.3 | 0 | 0 | 0 | 0 | |
| 15 | 70 | Male | 23 | 14 | ABI | Left | 2.3 | 4.4 | 2.9 | 0 | 0 | 0 | 0 | |
| 16 | 68 | Male | 125 | 9 | TBI | Bilateral | 1.2 | 2.2 | 1.5 | 0 | 0 | 0 | 0 | |
| 17 | 47 | Female | 40 | 16 | Stroke | Right | 2.4 | 5.6 | 3.3 | 1 | Left | 1 | 1 | 1 |
| 18 | 47 | Male | 22 | 35 | Stroke | Bilateral | 5.3 | 7.0 | 5.8 | 0 | 0 | 0 | 0 | |
| 19 | 66 | Male | 57 | 53 | Stroke | Right | 2.0 | 2.8 | 2.2 | 1 | Left | 1 | 1 | 0 |
| 20 | 48 | Male | 27 | 15 | Stroke | Right | 3.9 | 6.4 | 4.6 | 0 | 0 | 0 | 0 | |
| 21 | 41 | Female | 42 | 3 | Stroke | Right | 1.5 | 5.4 | 2.6 | 1 | Left | 0 | 1 | 0 |
aWe normalised FIM scores to the original 7-point scale (1 = total assistance, 2 = maximal assistance, 3 = moderate assistance, 4 = minimal assistance, 5 = supervision, 6 = modified independence, 7 = complete independence). ID = identifier
bAs described in the methods, an experienced neuropsychologist determined neglect presence based on the results of three pen-and-paper tests. VR gameplay was not used for neglect determination
Feasibility of The Attention Atlas
We operationalised feasibility using subjective reports of the VR experience and present these results in Fig. 2. Because of the vagaries of the inpatient schedule, simulator sickness data were available for 10 patients and 7 controls, and game experience and system usability data were available for 9 controls and 9 patients. During VR, both groups reported no to minimal simulator sickness. Sickness severity did not differ significantly between groups (χ2 = 0.0, P = 1.0; Fig. 2a). The midpoint and variance of the game experience components of positive affect, competence, negativity, and flow did not differ between the groups (Wilcoxon ranked sum tests: Ws < 1.9, Ps > 0.06; Levene’s tests: Ls < 4.0, Ps > 0.06). Overall, participants reported “moderate” positive affect (median, 3.6; IQR, 0.9), competence (median, 3.5; IQR, 0.8), and flow (median, 3.1; IQR, 0.8) and “not at all” negativity (median, 1.4; IQR, 0.4; Fig. 2b). Similarly, the midpoint and variance of system usability did not differ significantly between the groups (Wilcoxon ranked sum test: W = 1.4, P = 0.15; Levene’s test: L = 1.7, P > 0.21). The overall system usability was acceptable (median, 80; IQR, 13.1). System usability was unacceptable for one patient and marginal for two patients (Fig. 2c). Given minimal motion sickness scores, and positive results on the gaming experience, The Attention Atlas was feasible in our acute inpatient neurorehabilitation sample. However, it is worth noting 1 patient did not provide gaming experience data due to withdrawing because they did not enjoy the game. And although only 1 patient scored it as unacceptable, usability could also be improved.
Fig. 2.
Feasibility of The Attention Atlas. a Motion sickness during VR on the SSQ. b Game experience on the GEQ-R (1 = not at all, 2 = slightly, 3 = moderately, 4 = fairly, 5 = extremely). This and subsequent box plots show the median, the 50th and 75th percentiles (at the upper/lower hinges), and 1.5 × IQR from the hinges (whiskers). In this and subsequent plots, points represent players. c System usability on the SUS. Shaded regions show acceptability cut-offs. This and subsequent half-violin plots show the kernel density estimation
Summary of visuospatial atypicality
Normative modelling sought to detect visuospatial atypicality, defined as gameplay beyond the outlier cut-offs. There were 14 attention metrics based on three primary categories: accuracy (%), RT (s), and raycast orientation (°) for the headset and controller. Accuracy, RT, headset latitude mean, headset longitude means, controller latitude means, and controller longitude means were computed for each game level. Accuracy and RT were pooled across game levels to derive “spatial preference” difference scores (Δ% and Δs, respectively), contrasting four spatial quadrants (left, right, up, down) and three eccentricities (12.5°, 25.0°, 37.5°).
Figure 3 depicts the outlier summary matrices for patients and controls. These summary matrices showed that visuospatial atypicality was more prevalent in patients (Fig. 3a) than in controls (Fig. 3b; χ2 = 19.46, P < 0.001). For controls, 2 of 9 (22.2%) showed outliers, but only on one or two attentional metrics. For patients, 8 of 13 (61.5%) showed atypical visuospatial attentional patterns on ≥ 1 metric. For patients, case-wise, the number of atypical attentional metrics ranged from 0 to 9 of 14 (median = 2.0, IQR = 5.0). Further, combinations of outlier metrics differed across patients, suggesting heterogeneous atypical patterns.
Fig. 3.

Summary of visuospatial atypicality. a Patient summary matrix. b Control summary matrix. The six primary performance metrics (response accuracy, RT, headset latitude mean, headset longitude mean, controller latitude mean, controller longitude mean) reflect the mean number of outliers across game levels. The vertical axis plots game ID, and the horizontal axis plots attention metrics. Black rectangles show outlier absence (i.e., typical performance), and non-black squares with red outliers show outlier presence (i.e., atypical performance). Yellow squares show missing data. For the first two metrics (accuracy and RT), outlier Boolean proportion (0–1) reflected the mean across game levels. LF = left/right contrast; UD = up/down contrast; 25.0° diff. = 12.5°/25.0° contrast; 37.5° diff. = 25.0°/37.5° contrast; lat. = latitude; lon. = longitude; M = mean
To explore further, we calculated mean atypicality across all univariable metrics. Figure 4 depicts mean atypicality by group. The groups did not differ overall on mean atypicality (Wilcoxon ranked sum test: W = 1.9, P = 0.06) but differed in the variance of mean atypicality (Levene’s tests: L = 10.5, P = 0.004), with greater variance for patients (median, 0.1; IQR, 0.3) than controls (median, 0.0; IQR, 0.0). In summary, patients showed a greater range of atypical visuospatial patterns than controls.
Fig. 4.
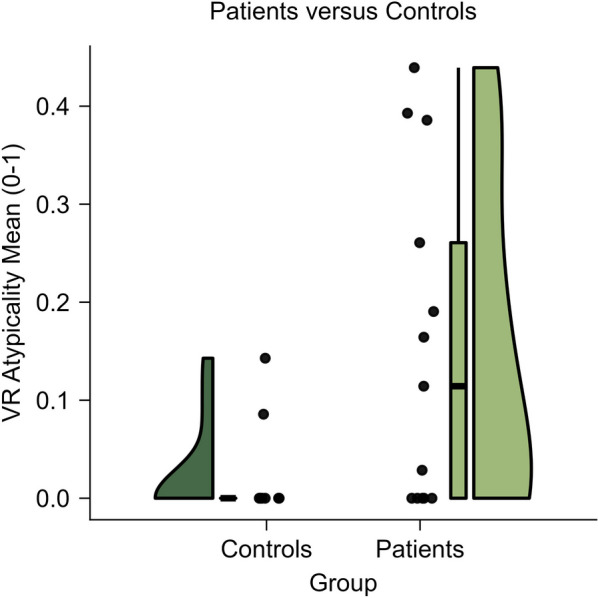
Mean visuospatial atypicality. Patients versus controls
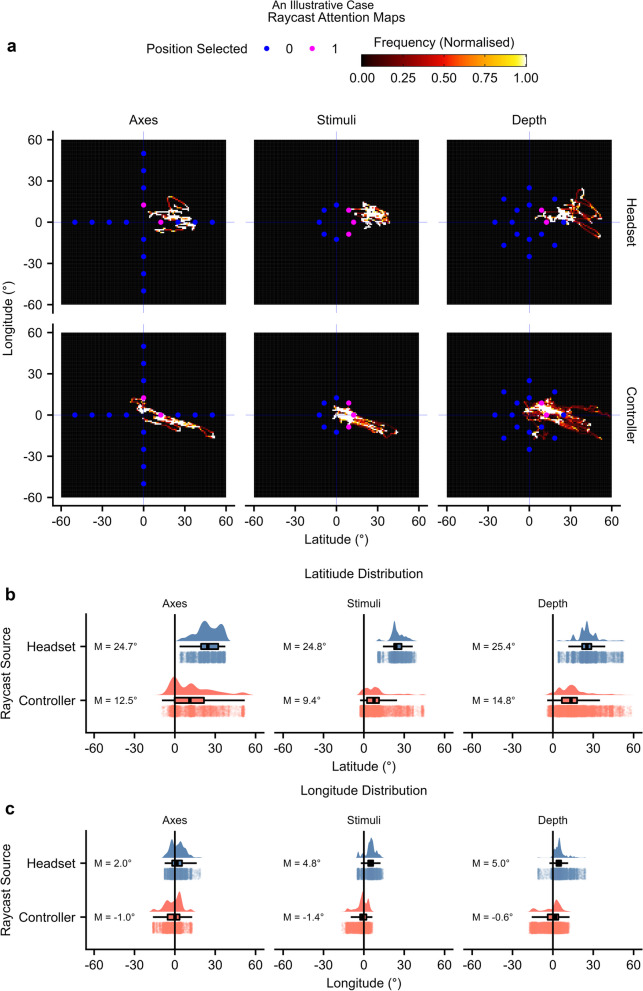
An illustrative case: using VR to elucidate unilateral spatial neglect in detail
Visuospatial atypicality described patterns specific to the individual. To illustrate this further, we will describe the gameplay of patient 17, who was among the most atypical individuals (mean atypicality = 0.19). Patient 17 was a 47-year-old female recruited 40 days post-injury, diagnosed with right hemisphere stroke, requiring maximal help with motor tasks, and showing modified independence with cognitive tasks, with left-side neglect on all three pen-and-paper tests. Indicated visuospatial atypicality constructs were attention challenge, headset orientation, and controller orientation. Patient 17 completed axes, stimuli, and depth game levels. Full field and free viewing level data were not available as the patient discontinued.
Patient 17 completed 18 trials with an average RT of 51.4 s and did not find the target; hence, accuracy for all completed levels was atypically low (0%). The key result was a large spatial orientation and behavioural perseverance toward the right hemispace. Raycast hand controller data showed that the patient tended to select a distractor in the right hemispace (Fig. 5a). The headset and controller latitude means were atypically oriented rightward (9.4° to 25.4°; Fig. 5b). Thus, raycast attentional mapping showed orientational inattention to the contralesional hemispace. For axes and depth levels, many ipsilesional positions were not selected, suggesting additional inattention within ipsilesional space (Fig. 5a). Thus, using VR, we can delve deeper into analysing neglect compared to traditional pen-and-paper methods, examining multiple metrics such as RT, accuracy, and raycasts from various sources.
Fig. 5.
An illustrative case. This figure depicts raycasts for patient 17. a Headset and controller maps. For each level, longitude and latitude coordinates were converted into 2D histograms with bounds of -50° and + 50° and a bin width of 1°. Raycast maps were limited to search array rather than cue periods. Points represent array element locations. Blue points represent unselected locations, and pink points represent selected locations. b-c Raycast distributions. Boxplots, kernel density estimates, and individual frame measurements are depicted. b Raycast latitude means. c Raycast longitude means
Discussion
For attention problems following brain injury, we applied normative modelling of VR gameplay to characterise visuospatial atypicality, which referred to whether the individual fell beyond outlier cut-offs based on both patient and control data. The purpose of this paper was to pilot this approach, and to illustrate this with results, albeit with limited conclusions made on the efficacy of the AA based on these results. The results from this pilot showed that visuospatial atypicality was more prevalent among patients than controls. Atypicality corresponded highly but not entirely with pen-and-paper assessments. Visuospatial atypicality went beyond pen-and-paper, describing neglect in detail, describing attention problems on a variety of metrics, and detecting those missed or under-described on pen-and-paper. It is also worth noting that the frequency of outliers (i.e., potential neglect cases) found with the VR was what might be expected given findings in past literature [18, 19].
Pen-and-paper assessments are convenient and routinely used in neurorehabilitation practice and research [21, 22], including for evaluations of immersive VR neglect assessments. Thus, for integration into health systems, immersive VR must show feasibility. Here, we operationalised feasibility as the acceptability of the VR gameplay and hardware. For VR, the major known risk is simulator sickness, an experience like motion sickness, which is thought to arise through vestibular-visual mismatch [99, 100], although other factors can also contribute [101–103]. Such risks are minimised in modern low-latency systems and in experiences that exclude optic flow resulting from moving elements and the translation or rotation of the player’s perspective through space [104–106]. We verified that motion sickness was minimal for The Attention Atlas. Participants were monitored closely and encouraged to discontinue if they felt motion sickness or for any other reason. It is worth noting that we did exclude those who reported a history of motion sickness, so questions remain about this group. Of the patients recruited, only two discontinued – one because they did not enjoy the game and another who had unreported visual field deficits that made the game impossible [107–109]. Game experiences were overall positive, and system usability was acceptable or marginal for all but one patient. This suggests that the game is generally enjoyable, had a minimal chance of motion sickness, but that usability needs to be developed for patients to be able to fully engage with the AA. We conclude the AA was feasible, but more work needs to be done to explore motion sickness in higher risk patients, and more development to the usability of the game. Of previous immersive VR neglect assessments, only Knobel et al. [31, 50] investigated feasibility. Consistent with the current results, Knobel et al. found that VR produced minimal motion sickness in cancellation and detection games and positive game experiences and high system usability in a detection game. It is vital feasibility is measured in several ways for any new system being developed.
Consistent with feasibility, our sample comprised inpatients with stable cognitive function, who were recruited on a mean of 41 days (SD, 29) post-injury. Thus, VR was feasible within two months post-injury on average. Some previous immersive VR neglect test group studies recruited patients several months to years post-injury (e.g., [46, 53]), while others recruited patients two to three months post-injury [31, 47, 50]. Case studies have shown interpretable gameplay results within two weeks post-injury [51, 56]. Thus, the current study provides evidence for VR feasibility in groups of acute brain injury patients. This suggests that VR is feasible for acute and subacute rehabilitation and sensitive to acute attention problems, however, to validate feasibility in the groups included in this study (stroke, TBI, older/younger patients) larger samples of each will be required.
Consistent with the classical conception of neglect [1–4], visuospatial atypicality identified a spatial preference for and an orientation toward the ipsilesional space. Beyond this classical conception, the AA identified individuals with non-spatial atypicality who were typical spatially. This illustrates the potential for virtual reality and other computerised games to record multiple metrics and measure more than one construct.
The following section discuss the detection of spatial neglect using the AA vs pen-and-paper; however, these results are only preliminary, and should be interpreted as validating the analytical approach, rather than the efficacy of the AA to detect neglect. Visuospatial atypicality showed correspondence with pen-and-paper, detecting all three patients with left-side pen-and-paper neglect. Also, visuospatial atypicality identified three patients that pen-and-paper missed or under-described, with atypicality that could be consistent with spatial or non-spatial attention problems. Although a complete analysis of these patterns is beyond the current scope and statistical power of this paper, the results are broadly consistent with work showing strong positive correlations between VR performance and pen-and-paper metrics of neglect [30, 44] and neglect severity [49]. Note, though, that the current approach differs subtly but importantly from all previous immersive VR neglect assessment studies. Previous studies categorised patients as belonging to neglect and non-neglect groups based on existing tests and then stratified VR analyses accordingly. Thus, the VR results were dependent on the existing tests. By contrast, our VR analyses were self-referential, and our sample was recruited independently of existing tests and conceptualisations (i.e., we included stroke, TBI, and other ABI, and left, right, and bilateral injuries). It will be important for future work to examine the relationship between atypicality and real-world outcomes, such as prognosis and recovery.
Normative modelling of visuospatial atypicality quantified and conceptualised attention problems independently from current assessments. This approach has been used to chart brain morphology changes across the lifespan [80, 109], conceptualise the heterogeneity of various psychiatric disorders [79, 82], identify the consequences of stroke using smartphone interactions [110], and identify white matter anomalies in TBI [111]. In addition to independence from existing tests, normative modelling allowed individual-level statistical inferences, which facilitates potential for individualised rehabilitation.
Of the previous immersive VR studies, only one used normative modelling [41]. That study compared free viewing VR performance between controls and right hemisphere stroke patients with mild to severe neglect, determined via a sensitive behavioural test. The authors used 95th percentile cut-offs to identify gaze and headset horizontal asymmetries based on control group data. The results showed atypical performance was detected more frequently in patients than controls and that 12 of 18 patients showed a rightward preference on one or more horizontal asymmetry metrics. Thus, within a neglect-defined sample, normative modelling can identify atypical gaze and headset neglect-consistent patterns.
The current study differs from Hougaard et al.’s work in three primary ways. First, our sample was defined by brain injury, and hence the VR analysis was independent of existing tests. Second, we used a localisation task rather than free viewing, which allowed RT and accuracy measurement and the quantification of non-spatial attention problems. Third, we used VR without eye tracking. The differences sum to a quantification of performance and orientation trait space following brain injury in the current study and quantification of horizontal asymmetries of orientation and gaze following right hemisphere stroke and neglect in Hougaard et al.’s work. This is an interpretation based on a small sample and larger studies are needed to explore this.
The results of Hougaard et al. and other eye-tracking studies [66–72] suggest that eye tracking can also be a sensitive measure. Converging evidence from multiple sources—performance, orientation, and gaze—may quantify diagnostic certainty for self-referential neglect/non-neglect classification. The trend toward eye tracking as standard in immersive VR headsets for interaction, diagnostics, and foveated rendering should facilitate this approach. Until eye tracking is widely accessible, assessment based on orientation and performance may have greater potential for immediate impact.
Normative modelling, concerning the current study, had several notable characteristics. First, the analysis relied only on broadly defined categories of patients and controls and therefore applied to heterogeneous samples, including various injury categories. Second, the analysis described diverse individual patterns, which were otherwise undetectable to pen-and-paper. Third, the analysis did not show that atypical patterns were necessarily pathological. Fourth, although the analysis weighted all metrics equivalently, all metrics might not have had the same functional significance. Fifth, the analysis did not categorise individuals as having neglect but identified visuospatial atypicality, which may be consistent with neglect. Sixth, the analysis depended on the sample such that the same individual might be typical or atypical, depending on the gameplay of others. Seventh, the analysis quantified atypicality and thus highlighted those who might most need help within the current caseload.
Limitations
As a pilot study this paper has several limitations. The results from the AA are reported to support the main goal of exploring the feasibility of the analytical approach, but efficacy cannot be suggested until we complete larger trials. Secondly, the controls were not matched and were a convenience sample taken from clinicians within the hospital. Future studies would benefit from matched controls e.g., patients’ partners, but this was not possible for the current study, and was a limitation, amongst others, that are a result of COVID reduced accessibility.
This study prototyped VR measures that were independent of current assessments. Due to sample size limitations, we were unable to thoroughly assess the validity and therefore clinical relevance of visuospatial atypicality. Therefore, the functional limitations of the ‘atypicality’ label cannot be used for clinical decision making at this stage. Future validation studies will collect data to explore criterion validity and the correlation of ‘atypicality’ as described by the AA with existing indicators of spatial neglect such as traditional assessments and injury location. Approaches for assessing external validity include measuring correlations between functional disability and atypicality. We do not currently have data to explore whether the AA (and therefore VR more generally) is less susceptible to executive dysfunction than pen-paper assessments. Patient 17 provides a good example of how executive function might be less of a confounder in VR due to the availability of converging evidence across multiple sources. Patient 17 was unable to find any targets, so if we were relying on accuracy and reaction time, we would not be able to identify neglect via an orientation to one side or another, but as we are able to receive data from other sources (headset and controller orientation), it is still possible to make a judgement. In pen-paper tests, data is often only coming from one source (e.g., accuracy across spatial quadrants or the left–right axis—like ‘spatial preference’). However, this is something that needs to be explored.
Conclusions
Neglect, as classically understood, manifests as spatial preference toward ipsilesional space that renders objects in contralesional space difficult to orient toward, detect, and therefore perceive. The current results show that brain injuries produce functionally heterogeneous visuospatial atypicality patterns across individuals that manifest distinctly across bivariable components and metric pairings. Brain injuries affected performance, orientation, attention challenges, spatial preference, or a combination of these. Visuospatial atypicality included lateralised neglect-consistent patterns and other non-spatial attention problems that were undetectable to pen-and-paper. To advance assessment and ultimately promote recovery, future studies might optimise and individualise the game modelling to create self-referential assessments that are accessible for acute injury and applicable throughout rehabilitation. Self-referential neglect/non-neglect classification might benefit from converging evidence across multiple source dimensions. Methods for establishing functional significance, including correspondence with prognosis and recovery, will be important to promote successful rehabilitation.
Supplementary Information
Additional file 1: Video S1. A complete and abbreviated gameplay demonstration.This video demonstrates experienced healthy observer gameplay from a complete and abbreviated game containing all game levels and inter-level calibrations (total level-time duration of 3.9 minutes). Gameplay capture is from the first-person perspective. The information overlay was visible on the experiment computer display and not from within VR. We did not use audio affirmations, instructions, and sounds during this experiment. The depicted frame is from the depth level and shows the target successfully being located before selection. Smaller items are those that appear on the further depth surface. Apparent frame latency jitter, especially during the free viewing level, is due to capture and video compression and does not reflect the smooth, low-latency VR experience. This can be verified by the system performance information on the overlay, which shows a stable 90 Hz. We undertook the recording on a computer with a GTX 980 video card, showing reliable performance on older hardware. This recording used a swivel chair; hence, mobility during free viewing was higher in the demonstration than during the experiment.
Acknowledgements
We acknowledge and pay respect to the past, present, and future Traditional Custodians and Elders of the Yugambeh, Yugarabul, Yuggera, Jagera and Turrbal language regions where we work, and the continuation of cultural, spiritual and educational practices of Aboriginal and Torres Strait Islander peoples. Within The Hopkins Centre’s Brain and Enriched Environment (BEEHIVE) Laboratory for neurorehabilitation, researchers at Griffith University and clinicians at Gold Coast University Hospital and Logan Hospital (Queensland, Australia) co-designed The Attention Atlas. We acknowledge Connor Reid who contributed to The Attention Atlas game development and data collection. We thank all patients and clinicians who took part. A National Health and Medical Research Council Ideas Grant (APP2002362), “Dimensional Attention Modelling for Neglect Detection (DIAMOND): A novel application for brain injury”, a Metro South Health Research Support Scheme (MSH RSS) Project Grant (RSS_2021_173) “3D visuospatial attention mapping in patients with stroke and other neurological conditions”, and First Prize in the Bionics Queensland Challenge 2020 in AI-Enabled Bionics “AI-enabled spatial attention assessment and training system” supported this grant.
Abbreviations
- ABI
Acquired brain injury
- CLOX
An Executive Clock Drawing Task
- FIM
Functional Independence Measure
- GEQ-R
Game Experience Questionnaire Revised
- ID
Identifier
- IQR
Inter-quartile range
- LR
Left-Right Quadrant
- PCA
Principal components analysis
- Q1
First quartile
- Q3
Third quartile
- RT
Reaction time
- SSQ
Simulator Sickness Questionnaire
- SLCT
Single Letter Cancellation Test
- TBI
Traumatic brain injury
- UD
Up-down quadrant
- VR
Virtual reality
- 3D
Three-dimensional
- 2D
Two-dimensional
Author contributions
HZ, DRP, and LG conceptualised the research. DRP, TH, LG, HZ, and JB wrote and/or contributed to funding applications. DRP programmed The Attention Atlas, statistics, and analysis and designed the game based on discussions involving all authors. DRP, MFN, CHM, TH, DH, and HZ play-tested The Attention Atlas. DRP prepared the initial draft and managed revisions and submissions. DRP, MFN, CHM, and ML collected the data. All authors edited and/or commented on the manuscript. HZ, MFN, and LG managed the project.
Funding
This work was conducted in Australia and supported by several Australian sources: National Health and Medical Research Council Ideas Grant (APP2002362), “Dimensional Attention Modelling for Neglect Detection (DIAMOND): A novel application for brain injury”. Metro South Health Research Support Scheme (MSH RSS) Project Grant (RSS_2021_173) “3D visuospatial attention mapping in patients with stroke and other neurological conditions”. Motor Accident Insurance Commission (MAIC) in Queensland, Australia as part of The Hopkins Centre. HZ, DRP, and LG conceptualised the research. DRP, TH, LG, HZ, and JB wrote and/or contributed to funding applications. DRP programmed The Attention Atlas, statistics, and analysis and designed the game based on discussions involving all authors. DRP, MFN, CHM, TH, DH, and HZ playtested The Attention Atlas. DRP prepared the initial draft and managed revisions and submissions. DRP, MFN, CHM, and ML collected the data. All authors edited and/or commented on the manuscript. HZ, MFN, and LG managed the project. First Prize in the Bionics Queensland Challenge 2020 in AI-Enabled Bionics “AI-enabled spatial attention assessment and training system” supported development of the software.
Availability of data and materials
All relevant anonymised and cleaned raw data and results are freely and publicly accessible on Open Science Framework (https://osf.io/staj7/) in Study1DataCleanCopy.zip (cleaned game IDs: study.Study1.gameLogMaster.feather; cleaned demographics: study.Study1.GUID.demographics.feather; cleaned feasibility questionnaires: study.Study1.questionnaires.feather; player summary results: PlayerSummary.py\; raw VR data: _RECORDINGS\_DATA; raw results: _RECORDINGS\_RESULTS\). Complete source code for the latest version of the analysis is available at (https://osf.io/staj7/; AA.Diagnostics.zip). Complete source code and most source files for the latest version of The Attention Atlas are available at (https://osf.io/staj7/; AA.Standalone.zip). LemonadePixel’s food illustrations (https://www.shutterstock.com/image-vector/hand-drawn-food-drink-icons-breakfast-716980507) and PolyWorks’ low-resolution polygon forest (https://assetstore.unity.com/packages/3d/environments/low-poly-forest-pack-polyworks-52733) are available in the build but not in the source files, since we do not own the distribution rights. The games described in this report were tested and can be run without modification on the HTC Vive, HTC Vive Pro, and HTC Vive Pro Eye from the presets (longer: CliniciansTest1.game.json; shorter: CliniciansTests2.game.json; demonstration: CliniciansTestsDemo.game.json). Author DRP programmed the analyses in Python 3.10.6 and R 4.2.1 and The Attention Atlas in The Unity Game Engine 2019.4.20f1 on Windows 10.
Declarations
Ethics approval and consent to participate
The Human Research Ethics Committees of Metro South Health (HREC/2021/QMS/70556). The Human Research Ethics Committees of Griffith University (GU Ref. No: 2021/179). Site-Specific Assessment authorisation from Metro South Health (SSA/2021/QMS/70556).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Corbetta M, Shulman GL. Spatial neglect and attention networks. Annu Rev Neurosci. 2011;34:599. doi: 10.1146/annurev-neuro-061010-113731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.He BJ, et al. Breakdown of functional connectivity in frontoparietal networks underlies behavioral deficits in spatial neglect. Neuron. 2007;53:905–918. doi: 10.1016/j.neuron.2007.02.013. [DOI] [PubMed] [Google Scholar]
- 3.Brain WR. Visual disorientation with spatial reference to lesions of the right cerebral hemisphere. Brain. 1941;64:244–272. doi: 10.1093/brain/64.4.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gainotti G, Messerli P, Tissot R. Qualitative analysis of unilateral spatial neglect in relation to laterality of cerebral lesions. J Neurol Neurosurg Psychiatry. 1972;35:545–550. doi: 10.1136/jnnp.35.4.545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Azouvi P, et al. Behavioral assessment of unilateral neglect: study of the psychometric properties of the Catherine Bergego Scale. Arch Phys M. 2003;84:51–57. doi: 10.1053/apmr.2003.50062. [DOI] [PubMed] [Google Scholar]
- 6.Buxbaum LJ, et al. Hemispatial neglect: subtypes, neuroanatomy, and disability. Neurology. 2004;62:749–756. doi: 10.1212/01.WNL.0000113730.73031.F4. [DOI] [PubMed] [Google Scholar]
- 7.Di Monaco M, et al. Severity of unilateral spatial neglect is an independent predictor of functional outcome after acute inpatient rehabilitation in individuals with right hemispheric stroke. Arch Phys Med. 2011;92:1250–1256. doi: 10.1016/j.apmr.2011.03.018. [DOI] [PubMed] [Google Scholar]
- 8.Katz N, Hartman-Maeir A, Ring H, Soroker N. Functional disability and rehabilitation outcome in right hemisphere damaged patients with and without unilateral spatial neglect. Arch Phys Med. 1999;80:379–384. doi: 10.1016/S0003-9993(99)90273-3. [DOI] [PubMed] [Google Scholar]
- 9.Moore MJ, Demeyere N. Multiverse to inform neurological research: an example using recovery outcome of neglect. J Neurol. 2022;269:233–242. doi: 10.1007/s00415-021-10612-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moore MJ, Vancleef K, Riddoch MJ, Gillebert CR, Demeyere N. Recovery of visuospatial neglect subtypes and relationship to functional outcome six months after stroke. Neurorehabil Neural Repair. 2021;35:823–835. doi: 10.1177/15459683211032977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Longley V, et al. Non-pharmacological interventions for spatial neglect or inattention following stroke and other non-progressive brain injury. Cochrane Database Syst Rev. 2021 doi: 10.1002/14651858.CD003586.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Umeonwuka C, Roos R, Ntsiea V. Current trends in the treatment of patients with post-stroke unilateral spatial neglect: a scoping review. Disabil Rehabil. 2020 doi: 10.1080/09638288.2020.1824026. [DOI] [PubMed] [Google Scholar]
- 13.Azouvi P, et al. Sensitivity of clinical and behavioural tests of spatial neglect after right hemisphere stroke. J Neurol Neurosurg Psychiatry. 2002;73:160–166. doi: 10.1136/jnnp.73.2.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stone SP, Halligan PW, Greenwood RJ. The incidence of neglect phenomena and related disorders in patients with an acute right or left hemisphere stroke. Age Ageing. 1993;22:46–52. doi: 10.1093/ageing/22.1.46. [DOI] [PubMed] [Google Scholar]
- 15.Chen P, Ward I, Khan U, Liu Y, Hreha K. Spatial neglect hinders success of inpatient rehabilitation in individuals with traumatic brain injury: a retrospective study. Neurorehabil Neural Repair. 2016;30:451–460. doi: 10.1177/1545968315604397. [DOI] [PubMed] [Google Scholar]
- 16.Jang Y, Lee E, Kim Y, Park JH. Number processing error as a clinical manifestation of hemispatial neglect following hypoxic brain injury: a case report. Brain Neurorehabil. 2020 doi: 10.12786/bn.2020.13.e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tomaiuolo F, et al. Splenial callosal disconnection in right hemianopic patients induces right visual-spatial neglect. Brain Sci. 2022;12:640. doi: 10.3390/brainsci12050640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chen P, Chen CC, Hreha K, Goedert KM, Barrett AM. Kessler Foundation Neglect Assessment Process uniquely measures spatial neglect during activities of daily living. Arch Phys Med. 2015;96:869–876. e1. doi: 10.1016/j.apmr.2014.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Esposito E, Shekhtman G, Chen P. Prevalence of spatial neglect post-stroke: a systematic review. Ann Phys Rehabil. 2021;64:101459. doi: 10.1016/j.rehab.2020.10.010. [DOI] [PubMed] [Google Scholar]
- 20.Bowen A, McKenna K, Tallis RC. Reasons for variability in the reported rate of occurrence of unilateral spatial neglect after stroke. Stroke. 1999;30:1196–1202. doi: 10.1161/01.STR.30.6.1196. [DOI] [PubMed] [Google Scholar]
- 21.Evald L, Wilms I, Nordfang M. Assessment of spatial neglect in clinical practice: a nationwide survey. Neuropsychol Rehabil. 2021;31:1374–1389. doi: 10.1080/09602011.2020.1778490. [DOI] [PubMed] [Google Scholar]
- 22.Kaiser AP, Villadsen KW, Samani A, Knoche H, Evald L. Virtual reality and eye-tracking assessment, and treatment of unilateral spatial neglect: systematic review and future prospects. Front Psychol. 2022;13:787382. doi: 10.3389/fpsyg.2022.787382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bonato M. Neglect and extinction depend greatly on task demands: a review. Front Hum Neurosci. 2012 doi: 10.3389/fnhum.2012.00195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bonato M, Priftis K, Umiltà C, Zorzi M. Computer-based attention-demanding testing unveils severe neglect in apparently intact patients. Behav Neurol. 2013;26:179–181. doi: 10.1155/2013/139812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Menon A, Korner-Bitensky N. Evaluating unilateral spatial neglect post stroke: working your way through the maze of assessment choices. Top Stroke Rehabil. 2004;11:41–66. doi: 10.1310/KQWL-3HQL-4KNM-5F4U. [DOI] [PubMed] [Google Scholar]
- 26.Shao K, et al. Assessing executive function following the early stage of mild Ischemic stroke with three brief screening tests. J Stroke Cerebrovasc Dis. 2020;29:104960. doi: 10.1016/j.jstrokecerebrovasdis.2020.104960. [DOI] [PubMed] [Google Scholar]
- 27.Takamura Y, et al. Interaction between spatial neglect and attention deficit in patients with right hemisphere damage. Cortex. 2021;141:331–346. doi: 10.1016/j.cortex.2021.03.036. [DOI] [PubMed] [Google Scholar]
- 28.Dvorkin AY, Bogey RA, Harvey RL, Patton JL. Mapping the neglected space: gradients of detection revealed by virtual reality. Neurorehabil Neural Repair. 2012;26:120–131. doi: 10.1177/1545968311410068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Harada Y, Ohyama J. Spatiotemporal characteristics of 360-degree basic attention. Sci Rep. 2019;9:16083. doi: 10.1038/s41598-019-52313-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Knobel SEJ, et al. Immersive 3D virtual reality cancellation task for visual neglect assessment: a pilot study. Front Hum Neurosci. 2020;14:180. doi: 10.3389/fnhum.2020.00180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Norwood MF, et al. The attention atlas virtual reality platform maps three-dimensional (3D) attention in unilateral spatial neglect patients: a protocol. Brain Impair. 2022 doi: 10.1017/BrImp.2022.15. [DOI] [PubMed] [Google Scholar]
- 32.Pedroli E, Serino S, Cipresso P, Pallavicini F, Riva G. Assessment and rehabilitation of neglect using virtual reality: a systematic review. Front Behav Neurosci. 2015 doi: 10.3389/fnbeh.2015.00226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Riva G, Mancuso V, Cavedoni S, Stramba-Badiale C. Virtual reality in neurorehabilitation: a review of its effects on multiple cognitive domains. Expert Rev Med Devices. 2020;17:1035–1061. doi: 10.1080/17434440.2020.1825939. [DOI] [PubMed] [Google Scholar]
- 34.Cavedoni S, Cipresso P, Mancuso V, Bruni F, Pedroli E. Virtual reality for the assessment and rehabilitation of neglect: where are we now? A 6-year review update. Virtual Real. 2022 doi: 10.1007/s10055-022-00648-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ogourtsova T, Souza Silva W, Archambault PS, Lamontagne A. Virtual reality treatment and assessments for post-stroke unilateral spatial neglect: a systematic literature review. Neuropsychol. Rehabil. 2017;27:409–454. doi: 10.1080/09602011.2015.1113187. [DOI] [PubMed] [Google Scholar]
- 36.Pedroli E, et al. The use of virtual reality tools for the assessment of executive functions and unilateral spatial neglect in 115–140. 2016. 10.4018/978-1-4666-9740-9.ch007.
- 37.Tsirlin I, Dupierrix E, Chokron S, Coquillart S, Ohlmann T. Uses of virtual reality for diagnosis, rehabilitation and study of unilateral spatial neglect: review and analysis. Cyberpsychol Behav. 2009;12:175–181. doi: 10.1089/cpb.2008.0208. [DOI] [PubMed] [Google Scholar]
- 38.Aravind G, Darekar A, Fung J, Lamontagne A. Virtual reality-based navigation task to reveal obstacle avoidance performance in individuals with visuospatial neglect. IEEE Trans Neural Syst Rehabil Eng. 2015;23:179–188. doi: 10.1109/TNSRE.2014.2369812. [DOI] [PubMed] [Google Scholar]
- 39.Aravind G, Lamontagne A. Dual tasking negatively impacts obstacle avoidance abilities in post-stroke individuals with visuospatial neglect: task complexity matters! Restor Neurol Neurosci. 2017;35:423–436. doi: 10.3233/RNN-160709. [DOI] [PubMed] [Google Scholar]
- 40.Aravind G, Lamontagne A. Effect of visuospatial neglect on spatial navigation and heading after stroke. Ann Phys Rehabil. 2018;61:197–206. doi: 10.1016/j.rehab.2017.05.002. [DOI] [PubMed] [Google Scholar]
- 41.Hougaard BI, Knoche H, Jensen J, Evald L. Spatial neglect midline diagnostics from virtual reality and eye tracking in a free-viewing environment. Front Psychol. 2021;12:742445. doi: 10.3389/fpsyg.2021.742445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jannink MJA, et al. Assessment of visuospatial neglect in stroke patients using virtual reality: a pilot study. Int J Rehabil Res. 2009;32:280–286. doi: 10.1097/MRR.0b013e3283013b1c. [DOI] [PubMed] [Google Scholar]
- 43.Kim DY, et al. Assessment of post-stroke extrapersonal neglect using a three-dimensional immersive virtual street crossing program. Acta Neurol Scand. 2010;121:171–177. doi: 10.1111/j.1600-0404.2009.01194.x. [DOI] [PubMed] [Google Scholar]
- 44.Knobel SEJ, et al. Development of a search task using immersive virtual reality: proof-of-concept study. JMIR Serious Games. 2021;9:e29182. doi: 10.2196/29182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Numao T, Amimoto K, Shimada T. Examination and treatment of unilateral spatial neglect using virtual reality in three-dimensional space. Neurocase. 2021;27:447–451. doi: 10.1080/13554794.2021.1999478. [DOI] [PubMed] [Google Scholar]
- 46.Ogourtsova T, Archambault PS, Lamontagne A. Post-stroke visual neglect affects goal-directed locomotion in different perceptuo-cognitive conditions and on a wide visual spectrum. Restor Neurol Neurosci. 2018;36:313–331. doi: 10.3233/RNN-170766. [DOI] [PubMed] [Google Scholar]
- 47.Ogourtsova T, Archambault PS, Lamontagne A. Post-stroke unilateral spatial neglect: virtual reality-based navigation and detection tasks reveal lateralized and non-lateralized deficits in tasks of varying perceptual and cognitive demands. J Neuroeng Rehabil. 2018;15:34. doi: 10.1186/s12984-018-0374-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ogourtsova T, Archambault PS, Sangani S, Lamontagne A. Ecological virtual reality evaluation of neglect symptoms (EVENS): effects of virtual scene complexity in the assessment of poststroke unilateral spatial neglect. Neurorehabil Neural Repair. 2018;32:46–61. doi: 10.1177/1545968317751677. [DOI] [PubMed] [Google Scholar]
- 49.Peskine A, et al. Virtual reality assessment for visuospatial neglect: importance of a dynamic task. J Neurol Neurosurg Psychiatry. 2011;82:1407–1409. doi: 10.1136/jnnp.2010.217513. [DOI] [PubMed] [Google Scholar]
- 50.Yasuda K, Muroi D, Hirano M, Saichi K, Iwata H. Differing effects of an immersive virtual reality programme on unilateral spatial neglect on activities of daily living. BMJ Case Rep. 2018 doi: 10.1136/bcr-2017-222860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Yasuda K, Kato R, Sabu R, Kawaguchi S, Iwata H. Development and proof of concept of an immersive virtual reality system to evaluate near and far space neglect in individuals after stroke: a brief report. NeuroRehabilitation. 2020;46:595–601. doi: 10.3233/NRE-203014. [DOI] [PubMed] [Google Scholar]
- 52.Baheux K, Yoshizawa M, Yoshida Y. Simulating hemispatial neglect with virtual reality. J NeuroEng Rehabil. 2007;4:27. doi: 10.1186/1743-0003-4-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Broeren J, Samuelsson H, Stibrant-Sunnerhagen K, Blomstrand C, Rydmark M. Neglect assessment as an application of virtual reality. Acta Neurol Scand. 2007;116:157–163. doi: 10.1111/j.1600-0404.2007.00821.x. [DOI] [PubMed] [Google Scholar]
- 54.Fordell H, Bodin K, Bucht G, Malm J. A virtual reality test battery for assessment and screening of spatial neglect. Acta Neurol Scand. 2011;123:167–174. doi: 10.1111/j.1600-0404.2010.01390.x. [DOI] [PubMed] [Google Scholar]
- 55.Fordell H, Bodin K, Eklund A, Malm J. RehAtt—scanning training for neglect enhanced by multi-sensory stimulation in Virtual Reality. Top Stroke Rehabil. 2016;23:191–199. doi: 10.1080/10749357.2016.1138670. [DOI] [PubMed] [Google Scholar]
- 56.Kim K, et al. A virtual reality assessment and training system for unilateral neglect. Cyberpsychol Behav. 2004;7:742–749. doi: 10.1089/cpb.2004.7.742. [DOI] [PubMed] [Google Scholar]
- 57.Morganti F, Rusconi ML, Cantagallo A, Mondin E, Riva G. A context-based interactive evaluation of neglect syndrome in virtual reality. Virtual Rehabil. 2007 doi: 10.1109/ICVR.2007.4362160. [DOI] [Google Scholar]
- 58.De Luca R, et al. Use of virtual reality in improving poststroke neglect: Promising neuropsychological and neurophysiological findings from a case study. Appl Neuropsychol. 2019;26:96–100. doi: 10.1080/23279095.2017.1363040. [DOI] [PubMed] [Google Scholar]
- 59.Sugarman H, Weisel-Eichler A, Burstin A, Brown R. Use of novel virtual reality system for the assessment and treatment of unilateral spatial neglect: a feasibility study. Int Conf Virtual Rehabil. 2011 doi: 10.1109/ICVR.2011.5971859. [DOI] [Google Scholar]
- 60.Sugihara S, Tanaka T, Miyasaka T, Izumi T, Shimizu K. Assessment of visual space recognition of patients with unilateral spatial neglect and visual field defects using a head mounted display system. J Phys Ther Sci. 2016;28:332–338. doi: 10.1589/jpts.28.332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Buxbaum LJ, Dawson A, Linsley D. Reliability and validity of the virtual reality lateralized attention test in assessing hemispatial neglect in right-hemisphere stroke. Neuropsychology. 2012;26:430–441. doi: 10.1037/a0028674. [DOI] [PubMed] [Google Scholar]
- 62.Dawson AM, Buxbaum LJ, Rizzo AA. The virtual reality lateralized attention test: sensitivity and validity of a new clinical tool for assessing hemispatial neglect. Virtual Rehabil. 2008 doi: 10.1109/ICVR.2008.4625140. [DOI] [Google Scholar]
- 63.Grattan ES, Woodbury ML. Do neglect assessments detect neglect differently? Am J Occup Ther. 2017;71:7103190050p1–7103190050p9. doi: 10.5014/ajot.2017.025015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Pallavicini F, et al. Assessing unilateral spatial neglect using advanced technologies: the potentiality of mobile virtual reality. Technol Health Care. 2015;23:795–807. doi: 10.3233/THC-151039. [DOI] [PubMed] [Google Scholar]
- 65.Spreij LA, Ten Brink AF, Visser-Meily JMA, Nijboer TCW. Simulated driving: the added value of dynamic testing in the assessment of visuo-spatial neglect after stroke. J Neuropsychol. 2020;14:28–45. doi: 10.1111/jnp.12172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kaufmann BC, Cazzoli D, Müri RM, Nef T, Nyffeler T. Test-retest-reliability of video-oculography during free visual exploration in right-hemispheric stroke patients with neglect. Front Neurosci. 2020;14:731. doi: 10.3389/fnins.2020.00731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kaufmann BC, et al. Eyetracking during free visual exploration detects neglect more reliably than paper-pencil tests. Cortex. 2020;129:223–235. doi: 10.1016/j.cortex.2020.04.021. [DOI] [PubMed] [Google Scholar]
- 68.Kaufmann BC, et al. Video-oculography during free visual exploration to detect right spatial neglect in left-hemispheric stroke patients with aphasia: a feasibility study. Front Neurosci. 2021;15:640049. doi: 10.3389/fnins.2021.640049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kaufmann BC, et al. Visual exploration area in neglect: a new analysis method for video-oculography data based on foveal vision. Front Neurosci. 2020;13:1412. doi: 10.3389/fnins.2019.01412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Nyffeler T, Kaufmann BC, Cazzoli D. Visual neglect after an isolated lesion of the superior colliculus. JAMA Neurol. 2021;78:1531. doi: 10.1001/jamaneurol.2021.3863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ohmatsu S, et al. Visual search pattern during free viewing of horizontally flipped images in patients with unilateral spatial neglect. Cortex. 2019;113:83–95. doi: 10.1016/j.cortex.2018.11.029. [DOI] [PubMed] [Google Scholar]
- 72.Paladini RE, et al. Re-fixation and perseveration patterns in neglect patients during free visual exploration. Eur J Neurosci. 2019;49:1244–1253. doi: 10.1111/ejn.14309. [DOI] [PubMed] [Google Scholar]
- 73.Husain M, Rorden C. Non-spatially lateralized mechanisms in hemispatial neglect. Nat Rev Neurosci. 2003;4:26–36. doi: 10.1038/nrn1005. [DOI] [PubMed] [Google Scholar]
- 74.van Kessel ME, van Nes IJW, Brouwer WH, Geurts ACH, Fasotti L. Visuospatial asymmetry and non-spatial attention in subacute stroke patients with and without neglect. Cortex. 2010;46:602–612. doi: 10.1016/j.cortex.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 75.Villarreal S, et al. Unilateral stroke: computer-based assessment uncovers non-lateralized and contralesional visuoattentive deficits. J Int Neuropsychol Soc. 2021 doi: 10.1017/S1355617720001393. [DOI] [PubMed] [Google Scholar]
- 76.Mammola S, Carmona CP, Guillerme T, Cardoso P. Concepts and applications in functional diversity. Funct Ecol. 2021;35:1869–1885. doi: 10.1111/1365-2435.13882. [DOI] [Google Scholar]
- 77.Schleuter D, Daufresne M, Massol F, Argillier C. A user’s guide to functional diversity indices. Ecol Monogr. 2010;80:469–484. doi: 10.1890/08-2225.1. [DOI] [Google Scholar]
- 78.Petchey OL, Gaston KJ. Functional diversity: back to basics and looking forward. Ecol Lett. 2006;9:741–758. doi: 10.1111/j.1461-0248.2006.00924.x. [DOI] [PubMed] [Google Scholar]
- 79.Baumeister CM, et al. From pattern classification to stratification: towards conceptualizing the heterogeneity of Autism Spectrum Disorder. Neurosci Biobehav Rev. 2019 doi: 10.1016/j.neubiorev.2019.07.010. [DOI] [PubMed] [Google Scholar]
- 80.Bethlehem RA, et al. Brain charts for the human lifespan. Nature. 2022;604:525–533. doi: 10.1038/s41586-022-04554-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Marquand AF, Rezek I, Buitelaar JK, Beckmann CF. Understanding heterogeneity in clinical cohorts using normative models: beyond case-control studies. Biol Psychiatry. 2016;80:552–561. doi: 10.1016/j.biopsych.2015.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Marquand AF, et al. Conceptualizing mental disorders as deviations from normative functioning. Mol Psychiatry. 2019;24:1415–1424. doi: 10.1038/s41380-019-0441-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kennedy RS, Lane NE, Berbaum KS, Lilienthal MG. Simulator sickness questionnaire: an enhanced method for quantifying simulator sickness. Int J Aviat Psychol. 1993;3:203–220. doi: 10.1207/s15327108ijap0303_3. [DOI] [Google Scholar]
- 84.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”: practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 85.Linacre JM, Heinemann AW, Wright BD, Granger CV, Hamilton BB. The structure and stability of the functional independence measure. Arch Phys Med. 1994;75:127–132. doi: 10.1016/0003-9993(94)90384-0. [DOI] [PubMed] [Google Scholar]
- 86.Royall DR, Cordes JA, Polk M. CLOX: an executive clock drawing task. J Neurol Neurosurg Psychiatry. 1998;64:588–594. doi: 10.1136/jnnp.64.5.588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Albert ML. A simple test of visual neglect. Neurology. 1973;23:658–664. doi: 10.1212/WNL.23.6.658. [DOI] [PubMed] [Google Scholar]
- 88.Fullerton KJ, Mcsherry D, Stout RW. Albert’s test: a neglected test of perceptual neglect. Lancet. 1986;327:430–432. doi: 10.1016/S0140-6736(86)92381-0. [DOI] [PubMed] [Google Scholar]
- 89.Ijsselsteijn WA, de Kort YAW, Poels K. The Game Experience Questionnaire. Technische Universiteit Eindhoven, 2013.
- 90.Johnson D, Gardner MJ, Perry R. Validation of two game experience scales: The Player Experience of Need Satisfaction (PENS) and Game Experience Questionnaire (GEQ) Int J Hum Comput Stud. 2018;118:38–46. doi: 10.1016/j.ijhcs.2018.05.003. [DOI] [Google Scholar]
- 91.Brooke J. SUS: A “quick and dirty” usability scale. In Jordan P, Thomas B, Weerdmeester B, editors. Usability evaluation in industry, Taylor & Francis; 1996. 189–194
- 92.Brooke J. SUS: a retrospective. J Usability Stud. 2013;8:29–40. [Google Scholar]
- 93.Lewis JR. The system usability scale: past, present, and future. Int J Hum Comput Interact. 2018;34:577–590. doi: 10.1080/10447318.2018.1455307. [DOI] [Google Scholar]
- 94.Painter DR, Dux PE, Travis SL, Mattingley JB. Neural responses to target features outside a search array are enhanced during conjunction but not unique-feature search. J Neurosci. 2014;34:3390–3401. doi: 10.1523/JNEUROSCI.3630-13.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Wolfe JM, Horowitz TS. What attributes guide the deployment of visual attention and how do they do it? Nat Rev Neurosci. 2004;5:495–501. doi: 10.1038/nrn1411. [DOI] [PubMed] [Google Scholar]
- 96.Dicheva D, Dichev C, Agre G, Angelova G. Gamification in education: a systematic mapping study. J Educ Technol Soc. 2015;18:75–88. [Google Scholar]
- 97.Cugelman B. Gamification: what it is and why it matters to digital health behavior change developers. JMIR Serious Games. 2013;1:e3139. doi: 10.2196/games.3139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Wang Y-F, Hsu Y-F, Fang K. The key elements of gamification in corporate training—the Delphi method. Entertain Comput. 2022;40:100463. doi: 10.1016/j.entcom.2021.100463. [DOI] [Google Scholar]
- 99.Bles W, Bos JE, de Graaf B, Groen E, Wertheim AH. Motion sickness: only one provocative conflict? Brain Res Bull. 1998;47:481–487. doi: 10.1016/S0361-9230(98)00115-4. [DOI] [PubMed] [Google Scholar]
- 100.Akiduki H, et al. Visual-vestibular conflict induced by virtual reality in humans. Neurosci Lett. 2003;340:197–200. doi: 10.1016/S0304-3940(03)00098-3. [DOI] [PubMed] [Google Scholar]
- 101.Lin JJ-W, Duh HBL, Parker DE, Abi-Rached H, Furness TA. Effects of field of view on presence, enjoyment, memory, and simulator sickness in a virtual environment. Proc IEEE Virtual Reality. 2002;2002:164–171. doi: 10.1109/VR.2002.996519. [DOI] [Google Scholar]
- 102.Dużmańska N, Strojny P, Strojny A. Can simulator sickness be avoided? A review on temporal aspects of simulator sickness. Front Psychol. 2018 doi: 10.3389/fpsyg.2018.02132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Headless horseman goes bowling: VR locomotion. 2020.
- 104.Farmani Y, Teather RJ. Evaluating discrete viewpoint control to reduce cybersickness in virtual reality. Virtual Real. 2020;24:645–664. doi: 10.1007/s10055-020-00425-x. [DOI] [Google Scholar]
- 105.Stauffert J-P, Niebling F, Latoschik ME. Effects of latency jitter on simulator sickness in a search task. In 2018 IEEE Conference on Virtual Reality and 3D User Interfaces (VR) 121–127, 2018. doi:10.1109/VR.2018.8446195.
- 106.Wroblewski D, Francis BA, Sadun A, Vakili G, Chopra V. Testing of visual field with virtual reality goggles in manual and visual grasp modes. Biomed Res Int. 2014;2014:1–10. doi: 10.1155/2014/206082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Tsapakis S, et al. Visual field examination method using virtual reality glasses compared with the Humphrey perimeter. Clin Ophthalmol. 2017;11:1431–1443. doi: 10.2147/OPTH.S131160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Matsumoto C, et al. Visual field testing with head-mounted perimeter ‘imo’. PLoS ONE. 2016;11:e0161974. doi: 10.1371/journal.pone.0161974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Rutherford S, et al. Charting brain growth and aging at high spatial precision. Elife. 2022 doi: 10.7554/eLife.72904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Ceolini E, et al. A model of healthy aging based on smartphone interactions reveals advanced behavioral age in neurological disease. iScience. 2022 doi: 10.1016/j.isci.2022.104792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Guerrero-Gonzalez JM, et al. Mahalanobis distance tractometry (MaD-Tract) – a framework for personalized white matter anomaly detection applied to TBI. NeuroImage. 2022;260. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Video S1. A complete and abbreviated gameplay demonstration.This video demonstrates experienced healthy observer gameplay from a complete and abbreviated game containing all game levels and inter-level calibrations (total level-time duration of 3.9 minutes). Gameplay capture is from the first-person perspective. The information overlay was visible on the experiment computer display and not from within VR. We did not use audio affirmations, instructions, and sounds during this experiment. The depicted frame is from the depth level and shows the target successfully being located before selection. Smaller items are those that appear on the further depth surface. Apparent frame latency jitter, especially during the free viewing level, is due to capture and video compression and does not reflect the smooth, low-latency VR experience. This can be verified by the system performance information on the overlay, which shows a stable 90 Hz. We undertook the recording on a computer with a GTX 980 video card, showing reliable performance on older hardware. This recording used a swivel chair; hence, mobility during free viewing was higher in the demonstration than during the experiment.
Data Availability Statement
All relevant anonymised and cleaned raw data and results are freely and publicly accessible on Open Science Framework (https://osf.io/staj7/) in Study1DataCleanCopy.zip (cleaned game IDs: study.Study1.gameLogMaster.feather; cleaned demographics: study.Study1.GUID.demographics.feather; cleaned feasibility questionnaires: study.Study1.questionnaires.feather; player summary results: PlayerSummary.py\; raw VR data: _RECORDINGS\_DATA; raw results: _RECORDINGS\_RESULTS\).
All relevant anonymised and cleaned raw data and results are freely and publicly accessible on Open Science Framework (https://osf.io/staj7/) in Study1DataCleanCopy.zip (cleaned game IDs: study.Study1.gameLogMaster.feather; cleaned demographics: study.Study1.GUID.demographics.feather; cleaned feasibility questionnaires: study.Study1.questionnaires.feather; player summary results: PlayerSummary.py\; raw VR data: _RECORDINGS\_DATA; raw results: _RECORDINGS\_RESULTS\). Complete source code for the latest version of the analysis is available at (https://osf.io/staj7/; AA.Diagnostics.zip). Complete source code and most source files for the latest version of The Attention Atlas are available at (https://osf.io/staj7/; AA.Standalone.zip). LemonadePixel’s food illustrations (https://www.shutterstock.com/image-vector/hand-drawn-food-drink-icons-breakfast-716980507) and PolyWorks’ low-resolution polygon forest (https://assetstore.unity.com/packages/3d/environments/low-poly-forest-pack-polyworks-52733) are available in the build but not in the source files, since we do not own the distribution rights. The games described in this report were tested and can be run without modification on the HTC Vive, HTC Vive Pro, and HTC Vive Pro Eye from the presets (longer: CliniciansTest1.game.json; shorter: CliniciansTests2.game.json; demonstration: CliniciansTestsDemo.game.json). Author DRP programmed the analyses in Python 3.10.6 and R 4.2.1 and The Attention Atlas in The Unity Game Engine 2019.4.20f1 on Windows 10.