Abstract
Laparoscopic sleeve gastrectomy (LSG) is the most widely performed bariatric surgery and has been associated with excellent outcomes and a significant reduction in obesity-related morbidity and mortality. Traditionally, this surgery is performed using five to seven trocars. However, LSG performed through a single trocar is emerging as a less invasive method of performing this surgery. This systematic review and meta-analysis compare the outcomes and complication rates of single-port versus multi-port LSG.
We searched PubMed, Medline, Scopus, and the Cochrane Library for articles published from 2008 to 2023, in accordance with the PRISMA 2020 guidelines. Data on variables such as operative time, excess weight loss, intraoperative bleeding, postoperative leak, and incisional hernia rates were collected and analyzed using a random-effects model.
Fourteen articles met the inclusion criteria and were included in the meta-analysis. No significant differences were found between the single-port LSG (SILSG) and conventional LSG (CLSG) groups in terms of operative time, rate, intraoperative complications, length of hospital stay, postoperative complications, and excess weight loss (EWL). Furthermore, single incision sleeve gastrectomy showed better satisfaction with the cosmetic score.
SILSG is a viable alternative procedure, showing comparable outcomes to multiport conventional sleeve gastrectomy, in addition, to a better cosmetic satisfaction score.
Keywords: bariatric surgery, laparoscopic surgery, multiport, sleeve gastrectomy, single-incision
Introduction and background
Over the past few decades, obesity rates and associated metabolic diseases have rapidly increased worldwide [1]. As our understanding of weight regulation has advanced, treating obesity has become increasingly complex. While pharmacologic treatments targeting weight regulation yield limited results, bariatric surgery remains the only effective, long-lasting solution for a significant and enduring reduction in body weight [2]. Nowadays, sleeve gastrectomy (SG) is widely recognized as the foremost bariatric technique by numerous surgeons. It has become the most performed bariatric procedure due to its simplicity and efficacy in facilitating substantial weight loss and remission of co-morbidities. The procedure was first performed in 1990 as part of a two-step surgical intervention known as biliopancreatic diversion with a duodenal switch. Subsequently, the first laparoscopic SG (LSG) procedure was conducted in 1999 and has since become the most common weight loss surgery performed in the United States [3].
Recent advancements in surgical techniques have aimed to achieve better outcomes using fewer resources. These innovations focus on minimizing pain, improving aesthetic outcomes, and shortening hospital stays, all while maintaining efficacy and minimizing complications [4]. Conventional LSG (CLSG) typically involves three to seven trocar incisions. However, it is especially suited for a single-incision approach due to its limited range of motion and the requirement to enlarge only one trocar incision to remove a specimen. This makes it an ideal candidate for single-incision LSG (SILSG) [5].
Reducing the number of abdominal incisions has the potential to bring about improvements in terms of pain and postoperative complications while mitigating the surgical stress response. This has resulted in the growth of SILSG in various domains, including bariatric surgery [6]. Based on these observations, our study aims to conduct a meta-analysis in order to compare the surgical outcomes of CLSG and SILSG in the treatment of morbid obesity.
Review
Method
Study Design
The present study was conducted with the utmost fidelity to a previously established methodology that had been collectively approved by all contributing authors, in conjunction with adherence to the directives outlined in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Figure 1). We conducted a comprehensive literature review to ensure a meticulous and thorough analysis.
Figure 1. PRISMA 2020 Flow Diagram for Systematic Reviews.
Literature Search
This systematic review was conducted by searching multiple databases, including PubMed, Medline, Scopus, and the Cochrane Central Register, from 2008 to 2023. We used specific search terms in various combinations, including “single-incision,” “single-port,” “trans-umbilical,” “conventional,” “multiport,” and “sleeve gastrectomy.” Out of the 100 studies retrieved, 71 were excluded after screening their abstracts. The remaining 29 articles underwent full-text review, and 14 were selected for directly comparing the outcomes and complications of CLSG and SILSG.
Statistical Analysis
For categorical outcomes, we calculated the odds ratio (OR) and 95% confidence interval (CI) utilizing a random-effects model based on the Mantel-Haenszel statistical method. An OR of less than one indicated a higher prevalence of the outcome in the SILSG group. The continuous outcomes were determined by utilizing the weighted mean difference (WMD) and its 95% CI with random-effects models based on the inverse variance statistical method. A WMD of less than 0 indicated elevated values in the SILSG group. Data analysis was performed using the Cochrane Collaboration’s Review Manager (RevMan) version 5.3.
Inclusion Criteria
The inclusion criteria for this study were as follows: (1) comparative studies between CLSG and SILSG in obese patients; (2) studies published between 2008 and 2023; and (3) studies reporting original research in English. Excluded from this analysis were conference abstracts, review articles, and clinical practice guidelines.
Quality and Publication Bias Evaluation
We used the Newcastle-Ottawa Quality Assessment Scale (NOS) to evaluate non-randomized controlled trials (non-RCTs). The scale ranges from 0 to 9 stars. Studies with a score of five or higher were deemed to have sufficient methodological quality for inclusion. No RCTs met the criteria for inclusion. Two investigators, KA and AB independently rated the studies, and a final decision was made through consensus. The risk of publication bias was evaluated through the visual inspection of funnel plots.
Data Extraction
Data were extracted from each included study pertaining to demographics such as sample size for each group, age, sex, preoperative body mass index (BMI), and comorbidities. We also compiled data on perioperative outcomes, including the use of single-port devices, mean operative time, mean hospital stay, bougie diameter, conversion rate, doses of analgesics, and incidence of intraoperative and postoperative complications. Two investigators, KA and AA, carried out the data extraction process. They verified the validity of the data by reaching a consensus, with any disagreements resolved either through third-party adjudication (AAA) or by mutual agreement.
Results
Overview of Article Selection
This meta-analysis included a total of 14 studies, comprising 1,560 patients in the multiport group and 1,554 patients in the single-port group. These studies were published between 2010 and 2022 and originated from various countries, including the United States, Italy, France, Japan, Egypt, India, Qatar, Spain, Iran, and Austria. Detailed characteristics of the studies are presented in Table 1. The average body mass index (BMI) was 40 for the multiport group and 42.2 for the single-port group.
Table 1. Detailed Characteristics of the Studies Included.
| Patients | Female Patients | Mean Age | Mean Preop BMI | |||||||||
| Study ID | Type of Study | Journal | Country | Date Published | Multiport | Single port | Multiport | Single port | Multiport | Single port | Multiport | Single port |
| Gomberawalla et al. [7] | Matched Cohort | Obesity Surgery | USA | 2014 | 36 | 36 | 29 | 34 | 46 (31-72) | 43.33 (27-62) | 43.72 (34-50) | 43.06 (37-48) |
| Porta et al. [8] | Cohort | Obesity surgery | Italy | 2017 | 65 | 65 | 51 | 53 | 39±2,3 | 36±2,9 | 41.01±0.4 | 40.09±0.3 |
| Mauriello et al. [9] | Cohort | Obesity surgery | France | 2018 | 187 | 90 | 106 | 80 | 52±15 | 45±12 | 53.3±3.6 | 45.3±2.4 |
| Tranchart et al. [5] | Cohort | Surgical endoscopy | France | 2020 | 512 | 610 | 377 | 509 | 40.75±2.83 | 42±3 | 44.07±1.40 | 40.4±2.37 |
| Amiki et al. [10] | Cohort | Obesity surgery | Japan | 2019 | 31 | 31 | 31 | 31 | 39.7±9.0 | 39.1±8.7 | 33.7±2.0 | 33.5±2.6 |
| Alkashty et al. [11] | Case Control | International surgery journal | Egypt | 2022 | 20 | 20 | NA | NA | 35 (25-45) | 30 (20-40) | 45(40-50) | 42(38-46) |
| Lakdawala et al. [4] | Cohort | Obesity surgery | India | 2011 | 50 | 50 | 39 | 40 | 32±9 | 30±8 | 44.75±6.25 | 43±6.5 |
| Lakdawala et al. [12] | Cohort | Obesity Surgery | India | 2015 | 300 | 300 | 150 | 279 | 35.5±7.8 | 35.5±9.7 | 39.9±5.1 | 39.9±5.2 |
| Muir et al. [13] | Cohort | Obesity Surgery | USA | 2016 | 30 | 32 | 27 | 31 | 35 | 32.4 | 46.5 | 42.1 |
| Khidir et al. [14] | Cohort | Surgical innovations | Qatar | 2020 | 220 | 200 | 121 | 153 | 34.7±16.5 | 33.3±10.5 | 48.6±8.1 | 43.8±5.6 |
| Saber et al. [15] | Cohort | Surgery for obesity and related diseases | USA | 2010 | 12 | 14 | 7 | 7 | 43.1±13.6 | 44.2±11 | 52.6±6.8 | 53.8±6.6 |
| Delgado et al. [16] | Cohort | Surgical endoscopy | Spain | 2012 | 22 | 20 | 15 | 15 | 50 (26–69) | 46 (20–66) | 40.6 (34.5–55.3) | 40.1 (35.6-55.6) |
| Hosseini et al. [17] | Cohort | Iranian journal of medical scienses | Iran | 2017 | 51 | 51 | 35 | 46 | 34.4±1.2 | 34.7±1.2 | 45.3±1.2 | 42.8±0.7 |
| Sucher et al. [18] | Cohort | Journal of laparoendoscopic and advanced surgical techniques | Austria | 2014 | 40 | 40 | 40 | 40 | 43 (24–73) | 37 (19–62) | 43.8 (35.0–47.8) | 40.8 (35.1–45.0) |
Mean Operative Time
The mean operative time ranged from 42 to 170 min in the multiport group and from 45 to 148.7 min in the single-port group. The mean difference in operative time was -8.84 [95% CI: -22.38-4.70; p = 0.2; I2: 99%]. These results indicate no statistically significant difference between the two procedures, as shown in Figure 2.
Figure 2. Mean Operative Time.
Gomberawalla et al. [7], Lakdawala et al. [4], Saber et al. [15], Porta et al. [8], Muir et al. [13], Mauriello et al. [9], Tranchart et al. [5], Amiki et al. [10], Alkashty et al. [11], Lakdawala et al. [12], Khidir et al. [14], Sucher et al. [18], Delgado et al. [16], Hosseini et al. [17]
Length of Hospital Stay
Among the 14 studies included, 10 discussed the length of hospital stay, involving a total of 1,174 patients in the multiport group and 1,157 in the single-port group. The mean length of hospital stay was comparable for both groups: it ranged from 1.75 to six days in the multiport group and from 1.7 to five days in the single-port group. The absolute mean difference was 0.38 [95% CI: -.025-1; p = 0.24; I2 = 99%]. These results demonstrate no statistically significant difference in the length of hospital stay between the two groups (Figure 3).
Figure 3. Length of Hospital Stay.
Gomberawalla et al. [7], Saber et al. [15], Porta et al. [8], Mauriello et al. [9], Tranchart et al. [5], Amiki et al. [10], Alkashty et al. [11], Khidir et al. [14], Sucher et al. [18], Hosseini et al. [17].
Post-op Leak
Postoperative leaks were examined in six studies. In these studies, there were 20 incidents in the single-port group and 10 in the multiport group, resulting in leak rates of 1.28% and 0.6% for patients who underwent single-port and multiport LSG, respectively. However, the difference was not statistically significant, with an OR of 0.63 [95% CI: 0.3-1.31; p = 0.21; I2 = 0%] (Figure 4).
Figure 4. Post-op Leak.
Gomberawalla et al. [7], Lakdawala et al. [4], Saber et al. [15], Porta et al. [8], Muir et al. [13], Mauriello et al. [9], Tranchart et al. [5], Amiki et al. [10], Alkashty et al. [11], Lakdawala et al. [12], Khidir et al. [14], Sucher et al. [18], Delgado et al. [16], Hosseini et al. [17]
Bleeding
Intraoperative bleeding was almost equally distributed between the multiport and single-port groups, with 23 incidents in the single-port group compared to 22 in the multiport group, resulting in an OR of 0.96 [95%CI: 0.51-1.79; p = 0.9; I2 = 0] (Figure 5).
Figure 5. Bleeding.
Gomberawalla et al. [7], Lakdawala et al. [4], Saber et al. [15], Porta et al. [8], Muir et al. [13], Mauriello et al. [9], Tranchart et al. [5], Amiki et al. [10], Alkashty et al. [11], Khidir et al. [14], Sucher et al. [18], Hosseini et al. [17]
Surgical Site Infection
Surgical site infections occurred at nearly the same rate in both the multiport and single-port LSG groups. Analyses revealed no statistical significance, The OR was 0.98 [95% CI: 0.41-2.31; p = 0.96; I2 = 0] (Figure 6).
Figure 6. Surgical Site Infection.
Lakdawala et al. [4], Saber et al. [15], Porta et al. [8], Muir et al. [13], Mauriello et al. [9], Amiki et al. [10], Alkashty et al. [11], Lakdawala et al. [12], Khidir et al. [14], Delgado et al. [16], Hosseini et al. [17]
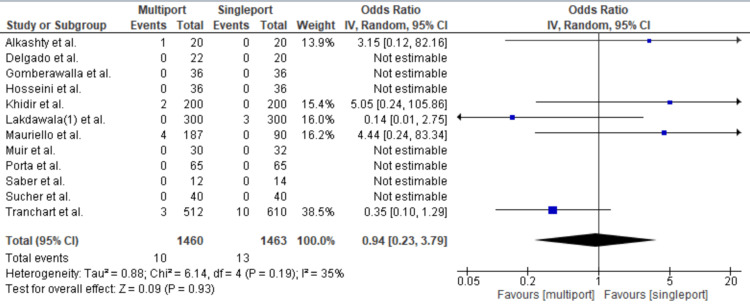
Incisional Hernia
Incisional hernias occurred in 13 cases in the single-port group compared with 10 cases in the multiport group, resulting in an OR of 0.94 [95% CI: 0.23-3.79, p = 0.93, I2: 35%] (Figure 7).
Figure 7. Incisional Hernia.
Gomberawalla et al. [7], Saber et al. [15], Porta et al. [8], Muir et al. [13], Mauriello et al. [9], Tranchart et al. [5], Alkashty et al. [11], Lakdawala et al. [12], Khidir et al. [14], Sucher et al. [18], Delgado et al. [16], Hosseini et al. [17]
Excess Weight Loss at Six Months
Twelve studies were included. At six months post-operation, the mean percentage of excess weight loss was 43.9% in the multiport group and 49.01% in the single-port group. Statistical analysis revealed no significant difference between the two groups, with a mean difference of -0.92 [95% CI: -2.76, 0.92; p = 0.33; I2: 96%] (Figure 8).
Figure 8. Excess Weight Loss at 6 Months.
Gomberawalla et al. [7], Lakdawala et al. [4], Saber et al. [15], Porta et al. [8], Muir et al. [13], Mauriello et al. [9], Tranchart et al. [5], Alkashty et al. [11], Lakdawala et al. [12], Sucher et al. [18], Delgado et al. [16], Hosseini et al. [17]
Cosmetic Satisfaction Score
Two studies were included in the analysis. The cosmetic satisfaction score used a scale ranging from 1 to 5 (1 = excellent; 2 = good; 3 = fair; 4 = acceptable; 5 = poor). The analysis revealed a mean difference of 1.45 and a significant p-value, indicating superior cosmetic results in the single-incision group (Figure 9).
Figure 9. Cosmetic Satisfaction Score.
Gastroesophageal Reflux Disorder
Gastroesophageal reflux disorder was reported in only three articles. These articles revealed 18 cases in both the single-port and multiport groups, resulting in an OR of 1.01 [95% CI: 0.52-1.97; p = 0.98; I2 = 0%] (Figure 10).
Figure 10. Gastroesophageal Reflux Disorder.
Amiki et al. [10], Lakdawala et al. [12], Sucher et al. [18]
Discussion
Minimally invasive surgeries offer new techniques for obese patients and present fewer side effects compared with open surgeries [19]. In 2013, LSG accounted for 43% of all bariatric surgeries in North America, 37% in Europe, 24.7% in Latin America, and 49% in the Asia-Pacific regions [20]. Consequently, significant resources and efforts are allocated to advancing this procedure and developing less invasive techniques. The emergence of single-port LSG presents a novel approach to this well-established surgery. This comprehensive evaluation and meta-analysis compare the outcomes and complication rates between traditional multi-port and single-port sleeve gastrectomy methods.
This meta-analysis found no significant differences in operative times between the two procedures. This finding aligns with a study by Delgato et al. [16], which initially indicated a statistically significant difference in operative times, with a mean of 96.5 min (60-130 min) for single-port surgery compared with 69.5 min (45-80 min) for conventional laparoscopic surgery. However, this discrepancy disappeared in the final ten cases, which suggests that initial disparities in operative time may be attributed to the learning curves of surgeons. As techniques are more widely practiced, improvements in the learning curve, as well as suturing and stapling techniques, have occurred. In contrast, Sucher et al. [18] found shorter operative times for the single-incision approach, which may be due to multiple factors. Once surgeons overcome the initial learning stage, technically challenging steps can be executed more efficiently. Furthermore, closing a single, slightly larger incision tends to be quicker than closing multiple smaller incisions, particularly in obese patients [18].
In terms of incisional hernias, we found no significant differences between the two groups. SILSG requires introducing a device to facilitate the use of instruments within the abdomen. This necessitates not only a larger skin incision but also a more substantial fascial incision, which could predispose patients to future incisional hernias. This risk was highlighted by Agaba et al. [21] who reported a port-site hernia rate of 2.9% at 30 to 36 months - a significant drawback for patients. Several factors contribute to the occurrence of port-site hernias (PSH), including both operative and patient-related elements. Most laparoscopic surgeons agree that the diameter of the cannula or port is a common cause of PSH. In SILSG, the fascial opening is larger than in conventional laparoscopy, and multiple smaller openings are combined into a single, larger one. Consequently, SILSG inherently carries a risk of PSH development [21]. However, we cannot evaluate this method in isolation; patient factors also contribute to the risk. The patient population undergoing these procedures often has a BMI above 40, adding another layer of risk alongside other factors such as diabetes and social habits.
As for cosmetic outcomes, single-incision surgery clearly offers better results and patient satisfaction. The specimen is extracted through the single-port site, which eliminates the need for additional incisions, unlike conventional LSG. Sucher et al. [18] supported this claim; at the three-month follow-up, patients evaluated their scar satisfaction using an assessment questionnaire. As expected, the SILSG group expressed greater satisfaction with their cosmetic outcomes, resulting in significantly higher scores compared to the conventional group.
Conclusions
The findings of this systematic review indicate that SILSG is technically feasible and increasingly practiced internationally. It appears to yield clinical outcomes comparable to those of conventional multiport sleeve gastrectomy. While we caution against drawing definitive conclusions from this study, we believe there is a viable future for single-incision laparoscopic surgery as more data emerge on its safety and feasibility. We recommend further randomized controlled trials, stronger control groups, reduced heterogeneity, and extended follow-up periods to better evaluate the safety and long-term outcomes of this procedure.
The authors have declared that no competing interests exist.
Author Contributions
Concept and design: Karim Ataya, Ayman M. Bsat, Almoutuz Aljaafreh, Amir Rabih Al Ayoubi
Acquisition, analysis, or interpretation of data: Karim Ataya, Ayman M. Bsat, Almoutuz Aljaafreh, Abdul Hafiz Al Tannir
Drafting of the manuscript: Karim Ataya, Ayman M. Bsat, Almoutuz Aljaafreh, Amir Rabih Al Ayoubi, Abdul Hafiz Al Tannir
Critical review of the manuscript for important intellectual content: Karim Ataya, Ayman M. Bsat, Almoutuz Aljaafreh, Amir Rabih Al Ayoubi, Abdul Hafiz Al Tannir
Supervision: Karim Ataya, Ayman M. Bsat, Amir Rabih Al Ayoubi, Abdul Hafiz Al Tannir
References
- 1.Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19·2 million participants. NCD Risk Factor Collaboration. Lancet. 2016;387:1377–1396. doi: 10.1016/S0140-6736(16)30054-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Surgical treatment of obesity. Albaugh VL, Abumrad NN. F1000Res. 2018;7 doi: 10.12688/f1000research.13515.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Seeras K, Sankararaman S, Lopez PP. Treasure Island (FL): StatPearls Publishing; 2023. Sleeve gastrectomy. [PubMed] [Google Scholar]
- 4.Single-incision sleeve gastrectomy versus conventional laparoscopic sleeve gastrectomy--a randomised pilot study. Lakdawala MA, Muda NH, Goel S, Bhasker A. Obes Surg. 2011;21:1664–1670. doi: 10.1007/s11695-011-0478-y. [DOI] [PubMed] [Google Scholar]
- 5.Short-term outcomes of single-port versus conventional laparoscopic sleeve gastrectomy: a propensity score matched analysis. Tranchart H, Rebibo L, Gaillard M, Dhahri A, Lainas P, Regimbeau JM, Dagher I. Surg Endosc. 2020;34:3978–3985. doi: 10.1007/s00464-019-07175-1. [DOI] [PubMed] [Google Scholar]
- 6.Postoperative pain after conventional laparoscopic versus single-port sleeve gastrectomy: a prospective, randomized, controlled pilot study. Morales-Conde S, Del Agua IA, Moreno AB, Macías MS. Surg Obes Relat Dis. 2017;13:608–613. doi: 10.1016/j.soard.2016.11.012. [DOI] [PubMed] [Google Scholar]
- 7.Outcome analysis of single incision vs traditional multiport sleeve gastrectomy: a matched cohort study. Gomberawalla A, Salamat A, Lutfi R. Obes Surg. 2014;24:1870–1874. doi: 10.1007/s11695-014-1312-0. [DOI] [PubMed] [Google Scholar]
- 8.Prospective comparison and quality of life for single-incision and conventional laparoscopic sleeve gastrectomy in a series of morbidly obese patients. Porta A, Aiolfi A, Musolino C, Antonini I, Zappa MA. Obes Surg. 2017;27:681–687. doi: 10.1007/s11695-016-2338-2. [DOI] [PubMed] [Google Scholar]
- 9.Retrospective comparison of single-port sleeve gastrectomy versus three-port laparoscopic sleeve gastrectomy: a propensity score adjustment analysis. Mauriello C, Chouillard E, d'alessandro A, Marte G, Papadimitriou A, Chahine E, Kassir R. Obes Surg. 2018;28:2105–2112. doi: 10.1007/s11695-018-3244-6. [DOI] [PubMed] [Google Scholar]
- 10.Reduced-port sleeve gastrectomy for morbidly obese japanese patients: a retrospective case-matched study. Amiki M, Seki Y, Kasama K, Pachimatla S, Kitagawa M, Umezawa A, Kurokawa Y. Obes Surg. 2019;29:3291–3298. doi: 10.1007/s11695-019-03987-1. [DOI] [PubMed] [Google Scholar]
- 11.Comparison of short-term outcomes between multi-port and single-port sleeve gastrectomy: a prospective study. Alkashty ME, Bakr AA, Nashed GA, Fahmy MH, Elward AS. Int Surg J. 2022;9:276–279. [Google Scholar]
- 12.Single-incision sleeve gastrectomy versus laparoscopic sleeve gastrectomy. A 2-year comparative analysis of 600 patients. Lakdawala M, Agarwal A, Dhar S, Dhulla N, Remedios C, Bhasker AG. Obes Surg. 2015;25:607–614. doi: 10.1007/s11695-014-1461-1. [DOI] [PubMed] [Google Scholar]
- 13.Weight-loss outcomes of SPIDER(®) sleeve gastrectomy at 6 months compared to traditional laparoscopic technique. Muir KB, Rice WV. Surg Endosc. 2016;30:2043–2048. doi: 10.1007/s00464-015-4451-z. [DOI] [PubMed] [Google Scholar]
- 14.Single-port sleeve gastrectomy compared with conventional laparoscopic sleeve gastrectomy: 5-year follow-up of weight loss, comorbidity resolution, and cost. Khidir N, Gagner M, El Matbouly M, et al. Surg Innov. 2020;27:265–271. doi: 10.1177/1553350620902550. [DOI] [PubMed] [Google Scholar]
- 15.Single-incision laparoscopic sleeve gastrectomy versus conventional multiport laparoscopic sleeve gastrectomy: technical considerations and strategic modifications. Saber AA, El-Ghazaly TH, Dewoolkar AV, Slayton SA. Surg Obes Relat Dis. 2010;6:658–664. doi: 10.1016/j.soard.2010.03.004. [DOI] [PubMed] [Google Scholar]
- 16.Transumbilical single-port sleeve gastrectomy: initial experience and comparative study. Delgado S, Ibarzabal A, Adelsdorfer C, Adelsdorfer W, Corcelles R, Momblán D, Lacy AM. Surg Endosc. 2012;26:1247–1253. doi: 10.1007/s00464-011-2002-9. [DOI] [PubMed] [Google Scholar]
- 17.Comparison of early results and complications between multi-and single-port sleeve gastrectomy: a randomized clinical study. Hosseini SV, Hosseini SA, Al-Hurry AM, Khazraei H, Ganji F, Sadeghi F. https://pubmed.ncbi.nlm.nih.gov/28533573/ Iran J Med Sci. 2017;42:251–257. [PMC free article] [PubMed] [Google Scholar]
- 18.Single-incision laparoscopic sleeve gastrectomy versus multiport laparoscopic sleeve gastrectomy: analysis of 80 cases in a single center. Sucher R, Resch T, Mohr E, Perathoner A, Biebl M, Pratschke J, Mittermair R. J Laparoendosc Adv Surg Tech A. 2014;24:83–88. doi: 10.1089/lap.2013.0250. [DOI] [PubMed] [Google Scholar]
- 19.Surgical management of obesity: current state of procedure evolution and strategies to optimize outcomes. Miller MR, Choban PS. Nutr Clin Pract. 2011;26:526–533. doi: 10.1177/0884533611418336. [DOI] [PubMed] [Google Scholar]
- 20.Bariatric surgery worldwide 2013. Angrisani L, Santonicola A, Iovino P, Formisano G, Buchwald H, Scopinaro N. Obes Surg. 2015;25:1822–1832. doi: 10.1007/s11695-015-1657-z. [DOI] [PubMed] [Google Scholar]
- 21.Incidence of port-site incisional hernia after single-incision laparoscopic surgery. Agaba EA, Rainville H, Ikedilo O, Vemulapali P. JSLS. 2014;18:204–210. doi: 10.4293/108680813X13693422518317. [DOI] [PMC free article] [PubMed] [Google Scholar]