Abstract
Background
The decision to treat a refluxing anterior saphenous vein (ASV) should be a clinical decision based on the assessment on the ASV’s contribution to patient’s signs and symptoms. Once the decision to treat has been made, there are anatomic, clinical, and technical considerations in treatment planning.
Methods
Clinical scenarios were discussed by a panel of experts and common anatomic, clinical, and technical considerations were identified.
Results
There are unique clinical considerations such as whether both the great saphenous vein (GSV) and ASV should be concomitantly treated, if a normal ASV should be treated when treating a refluxing GSV and when and how to treat the associated tributary varicose tributaries. Being aware of the anatomic, clinical, and technical considerations allows development of a treatment plan that optimizes long-term outcomes in patients with ASV reflux.
Conclusion
Ultimately the treatment plan should be tailored to address these types of variables in a patient-centered discussion.
Keywords: Anatomy, chronic venous insufficiency, recurrent varices, radiofrequency ablation, varicose veins
Introduction
Chronic venous disease (CVD) most commonly results from reflux in the great saphenous vein (GSV) and/or small saphenous veins. 1 Anterior saphenous vein (ASV) reflux is the next most common source of superficial reflux in up to 22% of patients presenting for first time treatment and approximately a third of patients presenting after prior varicose vein treatment.1–5 In the past, there has been a debate about whether the ASV is simply an accessory vein of the GSV or a defined truncal saphenous vein with a distinct natural history that requires different treatment considerations than a tributary. It is now understood that anatomically the ASV is a truncal saphenous vein with its own proper fascial compartment that is distinct from the GSV. Further, recent studies have demonstrated that ASV reflux can be worse in terms of progression to more advanced stages at presentation and complications such as an increased risk of superficial venous thrombosis. 6 Appreciating the variety of anatomic and clinical considerations in patients with ASV reflux can optimize outcomes and lower the risk of recurrence. The purpose of this paper is to review these differences and discuss case scenarios with the goal of enhancing understanding of the anatomic, technical and clinical considerations which are important in developing a treatment plan for the patient with ASV reflux. This manuscript is part 4 of a 4 part series where a panel recommends changing the terminology such that the “anterior accessory saphenous vein” (AASV) now be designated the anterior saphenous vein (ASV). This recommendation is supplemented by three accompanying parts to this series: Part 1: The Anterior Saphenous Vein. A position statement endorsed by the American Vein and Lymphatic Society (AVLS), the American Venous Forum (AVF) and the International Union of Phlebology (UIP). Part 2: an ultrasound study of ASV anatomy in normal controls and patients with anteromedial thigh varicosities; The Anterior Saphenous Vein. Part 3. Systematic review of the literature and payor coverage policies.
Methods
An international, multi-societal panel of experts was convened by the American Vein and Lymphatic Society (AVLS), the Union International of Phlebology (UIP), and the American Venous Forum (AVF) was assembled and charged reviewing the existing anatomic and clinical literature pertaining to the term “anterior accessory saphenous vein.” Common case presentation scenarios and anatomic, clinical, and technical considerations were discussed and assembled for this manuscript. Institutional Review Board approval was waived, and no patient consent was required for the research conducted in this study.
Anatomic considerations
There are three major anatomic considerations when planning treatment of patients with ASV reflux: (1) the location of the ASV reflux source in the groin or pelvis; (2) the path from origin to termination; and (3) the fate of the tributaries associated with the ASV reflux. Any combination of these anatomic factors can present different treatment challenges.
In most patients, the ASV terminates at the saphenofemoral junction (SFJ) proximal to the preterminal valve (PTV) of the GSV. 6 In about half the cases, ASV reflux presents with concurrent GSV reflux. In this case, when treating both the GSV and the ASV, one will likely need to separately cannulate and ablate each vein. Less frequently, the ASV can terminate well distal the PTV. When the ASV terminates well below the PTV, it may be possible to exclude the ASV by ablating the GSV more proximally toward the SFJ. However, more often than not, there is insufficient length when the ASV terminates at or close to the GSV termination, necessitating a separate cannulation and ablation of both the ASV and GSV.
One should be aware that the SFJ is frequently not the source of the reflux in the ASV. In one analysis, SFJ reflux into the ASV or GSV was noted in only 87/221 (39%) cases. In the remaining cases, segmental ASV reflux distal to a competent SFJ was found in 72 (32%) and ASV reflux arising from other veins in 62/221 (28%). Of the 62 from other sources with a competent SFJ, reflux was from the pelvis in 27% (59/221) and epigastric veins in 1.4% (3/221). 1 The superficial epigastric vein drains into the SFJ and rarely into the ASV. When the SFJ is competent and the GSV or ASV is incompetent at the level of their confluence with the superficial epigastric vein, the latter may be the primary source of reflux. Additionally, ASV reflux can be associated with the veins of the inguinal nodes as well as a variety of pelvic connections and connections with superficial tributaries from the abdominal wall. 7 This can occur when the ASV at the SFJ has a common trunk with inguinal tributaries (superficial epigastric or superficial circumflex iliac vein, or both). In mapping for preoperative planning, these are important anatomic details to note so the operator is aware they may not find a connection or reflux from the SFJ.
In most cases of ASV incompetence, reflux is transmitted distally to varicose tributaries that descend obliquely from the anteromedial thigh to the lateral knee and lateral calf. This contrasts with GSV reflux which mostly terminates in varicose tributaries over the thigh, at the knee, and in the calf. When both GSV and ASV reflux are present, varicose tributaries in the mid-thigh and below can derive from both truncal saphenous veins resulting in large varicose tributaries over the thigh. This can make it difficult on physical exam to determine if the varicose tributaries arise primarily from the GSV or from the ASV. In this case, treating only the GSV, as some insurance companies require before treatment of the ASV, may not adequately treat these varicose tributaries.
In all cases, a detailed venous ultrasound examination documenting the presence of the ASV and its relationship to any symptomatic varicose tributaries is critical for preoperative planning. One should also be aware that not all lateral thigh varicose tributaries arise from the ASV. In some cases, these tributaries can arise from reflux in the anterior thigh circumflex veins, the lateral plexus, or incompetent perforators in the thigh. 8 Even in the absence of concomitant GSV reflux, it is important to recognize that the origin can start more medially. Thus, ASV reflux can be associated with tributaries over the knee and medial thigh rather than purely in the lateral thigh.
Clinical considerations
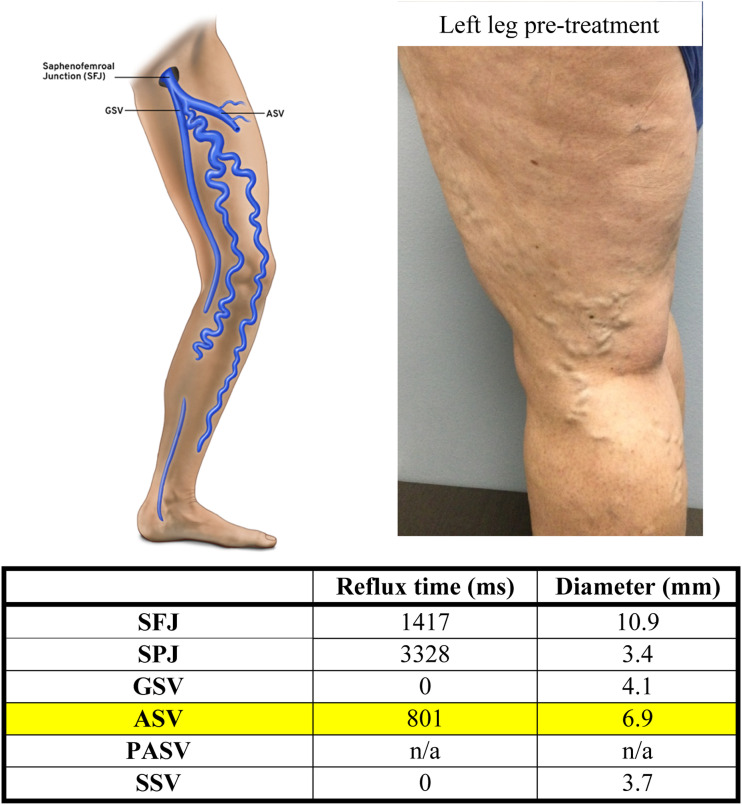
Concomitant GSV and ASV reflux with symptomatic tributaries
A common clinical question when the GSV and ASV are both refluxing is should the ASV be treated concomitantly with the GSV at initial presentation? An example is noted in Figure 1 where the tributary varicosities in the mid-thigh derive both from the GSV and ASV and will require ablation of both to optimally reduce this patient’s symptoms (Figure 1.) Ablation of the refluxing GSV and/or ASV should be a clinical decision based on the assessment of which veins are responsible for the current symptoms. When there is concomitant reflux, the ASV and GSV can often be ablated in the same session. A patient-centered approach, where the values of the patient are considered in the treatment planning, is always preferable. In most cases the ASV and GSV can be ablated in the same session. However, in some cases, it may be an option to treat each vein in a separate session.
Figure 1.
ASV and GSV reflux treated with a concomitant ablation and ultrasound-guided sclerotherapy of the branch tributary veins.
Isolated ASV reflux without proximal GSV reflux
In up to 18% of patients, ASV reflux (in the absence of GSV reflux) can be the sole source of symptoms. 2 This tends to occur when there is a competent preterminal valve of the GSV, but incompetence of the terminal valve directing reflux into the ASV.9,10 In the example in Figure 2, the patient has a competent GSV, an incompetent ASV, and a large number of superficial tributary varicose tributaries in the anterior and lateral thigh.
Figure 2.
Isolated ASV reflux with normal GSV with varicose tributaries in the lateral thigh.
When ASV reflux is present as the sole source of truncal saphenous reflux, it is appropriate to treat only the ASV and leave the non-refluxing GSV untreated. This has been a source of controversy as some insurance payers in the United States require that the GSV be ablated before one can submit for preauthorization to have the ASV reflux subsequently treated. This mandate is not supported by common sense or any published evidence. Thus, when treatment planning for a patient with isolated ASV reflux where the pre terminal valve is competent, along with a competent GSV, it is desirable to avoid an unnecessary GSV ablation.
Another insurance payer regulation that does not make clinical sense is the requirement that when symptomatic GSV and ASV reflux are both present, the GSV always be ablated before the ASV, waiting 3 months and reassessing symptoms prior to secondary treatment of the ASV. A one-size-fits-all blanket policy like this can unnecessarily increases resource utilization, wastes patients’ time, and can lead to an earlier recurrence than if both had been treated initially.
ASV reflux with a hypoplastic proximal GSV and incompetent distal GSV
Occasionally, it is necessary to treat a refluxing distal GSV concomitantly with the proximal ASV, leaving the non-refluxing proximal GSV untreated.11,12 This occurs when the reflux arises from a dominant ASV, the GSV is hypoplastic or competent from the lower thigh to the groin, and the venous drainage in the distal GSV arborizes with the ASV and is incompetent. 11 In this case, it may be necessary to ablate the ASV in the thigh, and possibly also the GSV in the lower leg, but leave the non-refluxing GSV in the thigh without treatment (Figure 3).
Figure 3.
Dilated ASV in the thigh with proximal hypoplastic GSV in the thigh that dilates and refluxes at and below the knee.
Should the normal ASV be treated when initially treating refluxing GSV?
Given that the ASV is one of the most common sources of recurrence after prior GSV treatment. An example is shown in Figure 4 where an initially normal ASV was later a source of reflux after prior GSV treatment 5 years later (Figure 4). Some investigators have postulated that ablating the normal ASV at the time of GSV ablation would reduce the risk of recurrence. In the most recent Appropriate Use Criteria, prophylactic treatment of a non-refluxing ASV at the time a refluxing GSV is treated, with the goal of reducing recurrence is deemed inappropriate due to lack of evidence.13,14 Thus, treating an ASV in the absence of significant reflux for purposes of reducing recurrence is without any indication and could be cause for action against a treating physician by payers or government entities for providing unindicated and inappropriate care. Patients should be advised that this may be a source of future recurrence and that they should be reevaluated if symptoms return. The impact of synchronous prophylactic treatment of the ASV on the incidence of recurrence in patients undergoing thermal ablation of an incompetent GSV is being studied in a randomized prospective trial (the SYNCHRONOUS-Study) with 1150 patients. 15 Studies such as this will help determine if there is sufficient evidence to recommend such a prophylactive approach to reduce recurrence in the future.
Figure 4.
GSV reflux treated in 2017 with normal ASV. ASV reflux in 2022 after prior GSV ablation in 2017.
Patients may benefit from concomitant treatment of the varicose tributaries at the time of ablation
It is important for the treating physician to carefully evaluate and identify any varicose tributaries during the preoperative assessment and consider appropriate treatment at the time of ASV ablation. One option is to treat the ASV reflux, then allow the patient to recover, and only treat the tributary veins that remain after an interval of recovery. Another is to treat the tributary veins concurrently with the ASV ablation. The multi-societal (American Vein and Lymphatic Society, American Venous Forum, and Society for Vascular Surgery) guidelines for the management of varicose veins recommend ablation of refluxing venous trunks with concomitant phlebectomy or ultrasound-guided foam sclerotherapy (GSV and ASV GRADE 1C; accessory saphenous veins GRADE 2C) staged management of tributaries is only suggested in the presence of compelling anatomic or medical reasons. 16 A shared decision-making with the patient is recommended so that individual circumstances and wishes can be considered when the final treatment plan is developed. 17 From an evidenced-based perspective, it appears there may be an advantage to early concomitant treatment of the varicose tributaries rather than waiting to see if they regress with time.18,19
Inadequate resolution of symptoms and varicose tributaries after ASV ablation
In preoperative planning and follow-up after treatment, it is important to consider there can be other sources of varicose tributaries distinct from the ASV reflux. These most often occur in the anterior and lateral thigh where tributaries connect with posterolateral thigh perforators and the anterior thigh circumflex vein. 8 This can lead to multiple varicose tributaries that do not resolve simply by treating the ASV reflux and thus may not adequately solve the patients’ problem. Differentiation between the ASV and the anterior thigh circumflex vein can be difficult and may require reassessment after the initial treatment plan is complete and further treatment of the remaining tributary varicose tributaries.
Technical considerations
There are several technical considerations when treating the ASV. For example, when treating both the ASV and GSV, the second vein to be cannulated can go into spasm when the first is treated and make it more difficult to treat at the same time. A double pre-puncture can help reduce the risk of spasm in the second vein after initial ablation of the first. 20
Another consideration is that in some patients with a dilated ASV, the vein may be located very close to the superficial femoral artery (SFA) just at or distal to the groin (Figure 5). When using a thermal ablation technique, one should make sure to assess the distance between the ASV and the SFA and place ample tumescent anesthesia to further separate these vessels as an AV fistula has been reported in this situation. 21
Figure 5.
ASV 21 mm from the superficial femoral artery (SFA).
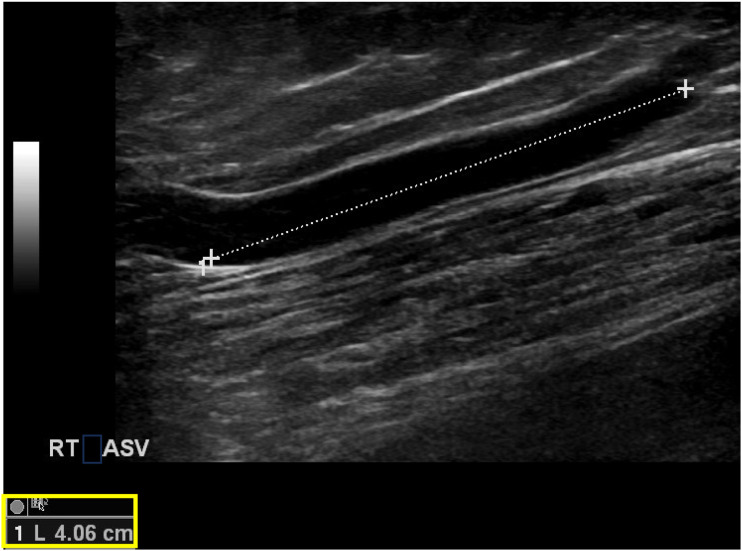
The ASV is generally shorter than the GSV and in some cases, it can be too short to cannulate with a thermal ablation catheter and ablate. In obese patients, it can be hard to locate, cannulate, and treat the ASV as it may leave the fascia and become a varicose tributary just distal to the groin crease where it can be less easily identified with ultrasound for needle and wire placement. Similarly, tumescent anesthesia can be difficult in such patients. When targeting the ASV within the fascia, the length can be shorter than the catheter heating zone. Depending on the manufacturer, a catheter with a 2.5 or 3 cm treatment zone can often be used to insure that the length of the ASV can be ablated without exposing the skin to the radiofrequency ablation (RFA) coil (Figure 6). In these cases, non-thermal approaches such as cyanoacrylate, proprietary foam sclerotherapy, or mechanochemical ablation may be additional non-thermal non-tumescent options. Alternatively, surgical options such as high ligation or phlebectomies only can be considered.
Figure 6.
Short length (4.06 cm) of intrafascial ASV that can be difficult to cannulate for RFA.
Conclusion
There are a number of anatomic, technical, and clinical considerations when planning treatment for patients with symptomatic ASV reflux. Taking these into account is critical in achieving optimal clinical results. Ultimately, a patient-centered approach that considers not only the anatomic and technical but also the clinical features of a patient’s presentation as well as their treatment goals and values is critical in achieving the best outcomes.
Take Home Message: There are unique clinical considerations when treating ASV reflux. Being aware of the anatomic and technical variations in presentation allows development of a treatment plan that optimizes long-term outcomes.
Authors represented: Meissner M (MM); Boyle EM; (EB) Labropoulos N (NL); Caggiati A (AC); Drgastin R (RD); Suat Doganci (SD); and Gasparis A (AG).
Acknowledgments
The authors acknowledge Michael Thompson for helping organize the group to develop and complete the project and Mesa Schumacher for her artistic contributions.
Footnotes
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: RD, EB, AC, SD, and MM reports no conflicts. NL is a Consultant/Speaker with Philips, Medtronic, BD Bard, and Boston Scientific; AG is a Consultant/Speaker: Medtronic, BD Bard, and Boston Scientific.
Funding: The open access publication fees for this article was financially supported by Boston Scientific Corporation. No other funding was provided.
Guarantor: Mark Meissner, MD
Contributorship: MM, AG, NL, and SD conceived of the project. MM, AG, NL, EB, RD, AC, and SD all contributed to developing the articles and contributing to the analysis and conclusions. EB, RD, and AC wrote the drafts of the articles and all parties approved and agree to be accountable for the final manuscripts.
ORCID iDs
Edward M Boyle https://orcid.org/0009-0000-4266-759X
Alberto Caggiati https://orcid.org/0000-0001-5322-2190
Nicos Labropoulos https://orcid.org/0000-0002-3984-1582
References
- 1.Garcia-Gimeno M, Rodriguez-Camarero S, Tagarro-Villalba S, et al. Duplex mapping of 2036 primary varicose veins. J Vasc Surg 2009; 49(3): 681–689. [DOI] [PubMed] [Google Scholar]
- 2.Labropoulos N, Kang SS, Mansour MA, et al. Primary superficial vein reflux with competent saphenous trunk. Eur J Vasc Endovasc Surg 1999; 18(3): 201–206. [DOI] [PubMed] [Google Scholar]
- 3.Bush RG, Bush P, Flanagan J, et al. Factors associated with recurrence of varicose veins after thermal ablation: results of the recurrent veins after thermal ablation study. Sci World J 2014; 2014: 505843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Garner JP, Heppell PS, Leopold PW. The lateral accessory saphenous vein - a common cause of recurrent varicose veins. Ann R Coll Surg Engl 2003; 85(6): 389–392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Svidersky Y, Goshchynsky V, Migenko B, et al. Anterior accessory great saphenous vein as a cause of postoperative recurrence of veins after radiofrequency ablation. J Med Life 2022; 15(4): 563–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ahmed T, Portnoy R, Chachati G, et al. Correlation of body mass index with recanalization risk after endovenous thermal ablation. J Vasc Surg Venous Lymphat Disord 2022; 10(1): 82–86. [DOI] [PubMed] [Google Scholar]
- 7.Riabinska O, Mendoza E. Ultrasound Anatomy of the accessory anterior saphenous vein. Phlebologie 2021; 50: 24–38. [Google Scholar]
- 8.Labropoulos N, Delis K, Mansour MA, et al. Prevalence and clinical significance of posterolateral thigh perforator vein incompetence. J Vasc Surg 1997; 26(5): 743–748. [DOI] [PubMed] [Google Scholar]
- 9.Zollmann P, Zollmann C, Zollmann P, et al. Determining the origin of superficial venous reflux in the groin with duplex ultrasound and implications for varicose vein surgery. J Vasc Surg Venous Lymphat Disord 2017; 5(1): 82–86. [DOI] [PubMed] [Google Scholar]
- 10.Stucker M, Moritz R, Altmeyer P, et al. New concept: different types of insufficiency of the saphenofemoral junction identified by duplex as a chance for a more differentiated therapy of the great saphenous vein. Phlebology 2013; 28(5): 268–274. [DOI] [PubMed] [Google Scholar]
- 11.Ricci S, Moro L, Ferrini A, et al. The E point: a new echographic great saphenous identification sign in specific anatomical variants and applications. Phlebology 2017; 32(2): 120–124. [DOI] [PubMed] [Google Scholar]
- 12.Caggiati A, Mendoza E. Segmental hypoplasia of the great saphenous vein and varicose disease. Eur J Vasc Endovasc Surg 2004; 28(3): 257–261. [DOI] [PubMed] [Google Scholar]
- 13.Gibson K, Khilnani N, Schul M, et al. American College of Phlebology Guidelines - treatment of refluxing accessory saphenous veins. Phlebology 2017; 32(7): 448–452. [DOI] [PubMed] [Google Scholar]
- 14.Masuda E, Ozsvath K, Vossler J, et al. The 2020 appropriate use criteria for chronic lower extremity venous disease of the American venous Forum, the society for vascular surgery, the American vein and lymphatic society, and the society of interventional radiology. J Vasc Surg Venous Lymphat Disord 2020; 8(4): 505–525. [DOI] [PubMed] [Google Scholar]
- 15.Fink C, Hartmann K, Mattausch T, et al. Impact of a synchronous prophylactic treatment of the anterior accessory saphenous vein on the recurrent varicose vein rate in patients undergoing thermal ablation of an insufficient great saphenous vein (SYNCHRONOUS-Study): study protocol for a prospective, multicentre, controlled observational study. BMJ Open 2022; 12(6): e061530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gloviczki PLP, Wasan SM, Meissner MH, et al. The 2022 society for vascular surgery, American venous Forum, and American vein and lymphatic society clinical practice guidelines for the management of varicose veins of the lower extremities. Part II. Duplex scanning and treatment of superficial truncal reflux: endorsed by the society for vascular medicine and the international union of Phlebology. J Vasc Surg Venous Lymphat Disord 2023; 11(2): 231–261. In Press. [DOI] [PubMed] [Google Scholar]
- 17.De Maeseneer MG, Kakkos SK, Aherne T, et al. Editor's choice - European society for vascular surgery (ESVS) 2022 clinical practice guidelines on the management of chronic venous disease of the lower limbs. Eur J Vasc Endovasc Surg 2022; 63(2): 184–267. [DOI] [PubMed] [Google Scholar]
- 18.Deol ZK, Lakhanpal S, Pappas PJ. Severity of disease and treatment outcomes of anterior accessory great saphenous veins compared with the great saphenous vein. J Vasc Surg Venous Lymphat Disord 2021; 10: 654–660. [DOI] [PubMed] [Google Scholar]
- 19.Theivacumar NS, Darwood RJ, Gough MJ. Endovenous laser ablation (EVLA) of the anterior accessory great saphenous vein (AAGSV): abolition of sapheno-femoral reflux with preservation of the great saphenous vein. Eur J Vasc Endovasc Surg 2009; 37(4): 477–481. [DOI] [PubMed] [Google Scholar]
- 20.Hao S, Cox S, Monahan TS, et al. Double prepuncture as a valuable adjunctive technique for complex endovenous ablation. J Vasc Surg Venous Lymphat Disord 2017; 5(4): 507–513. [DOI] [PubMed] [Google Scholar]
- 21.Watanabe S, Tsuji T, Fujita S, et al. A case of recurrent varicose veins due to the multiple fistulas from superficial femoral artery. SAGE Open Med Case Rep 2020; 8: 2050313X20926423. [DOI] [PMC free article] [PubMed] [Google Scholar]