Summary
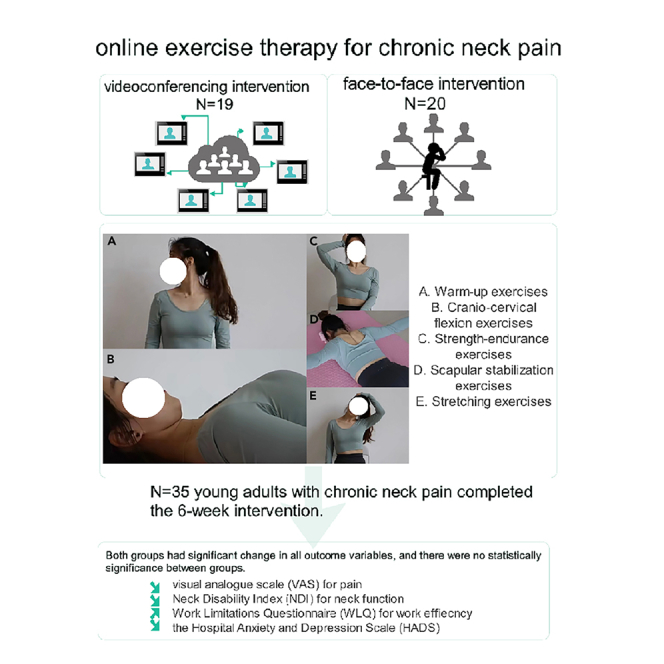
This study aimed to compare the efficacy of online exercise therapy with conventional exercise therapy for young adults with chronic neck pain. A randomized clinical trial recruiting 35 university students with self-reported chronic neck pain was conducted. The experimental group receiving 6-week online exercise therapy and active control group receiving the same face-to-face conventional exercise therapy. Visual analogue scale (VAS) for pain, Neck Disability Index (NDI), Work Limitations Questionnaire (WLQ), Hospital Anxiety and Depression Scale (HADS) and its subscales were evaluated. Both groups had improvements in VAS, NDI, HADS and WLQ scores from baseline to 6 weeks. All comparisons of changes in outcome variables between groups were not statistically significant. For young adults with chronic neck pain, both the online and conventional exercise interventions could improve their pain level, neck disability, anxiety state, and work efficiency. The online exercise intervention appeared feasible as an alternative treatment option for them.
Subject areas: Health sciences, Physics, Mechanics, Psychology
Graphical abstract
Highlights
-
•
For chronic neck pain, online exercise therapy can improve physical and mental state
-
•
For chronic neck pain, online exercise therapy can be an alternative treatment option
-
•
Clear demonstration with video conferencing is essential in online exercise therapy
Health sciences; Physics; Mechanics; Psychology
Introduction
Neck pain is one of the most common musculoskeletal disorders causing significant burden in public health worldwide.1 In China, neck pain is also prevalent, with an age standardized point prevalence of neck pain of 4532.6 per 100,000 persons, which was higher than the global age standardized point prevalence of 3551.1 per 100,000 persons in 2017.1,2 The China Mental Health Survey reported that the prevalence of chronic back or neck pain among people with any mental disorders was more than twice of those without mental disorder.3 It is believed that psychological factors such as stress, distress, anxiety, mood and emotions, cognitive function and pain-related behaviors are important factors related to chronic neck pain.4
Most chronic neck pain is non-specific with no identifiable pathoanatomical cause.5 Many therapies have been used to treat patients with non-specific chronic neck pain but exercise therapy is considered as the integral component of interventions.6 It has been shown that exercise can reduce the symptoms of depression, anxiety, and pain in patients with neck pain.7 However, since the start of COVID-19 pandemic in 2020, the reduction in the volume and accessibility to all non-emergency healthcare services due to stringent infection control measures had resulted in increasing difficulty for physiotherapists to provide conventional exercise therapy to patients. In response to the service demand, telerehabilitation, as a new service mode of delivering rehabilitation, has become an alternative way for physiotherapists to treat various musculoskeletal, neurological and cardiopulmonary disorders.8 Telerehabilitation has the advantages of alleviating the travel time and economic cost of patients, as well as reducing the pressure on the healthcare system.9 In addition, physiotherapists can also provide effective interventions via online means to those patients living in remote areas. Recent review on telerehabilitation in physiotherapy provides preliminary evidence that “telerehabilitation in physical therapy could be comparable with in-person rehabilitation and better than no rehabilitation for conditions such as osteoarthritis, low-back pain, hip and knee replacement, and multiple sclerosis and also in the context of cardiac and pulmonary rehabilitation”.10 However, the efficacy of telerehabilitation for patients with chronic non-specific neck pain is still unknown. A Cochrane review protocol on telerehabilitation for neck pain has been published but the review results are not available yet.11
Therefore, the objective of the present study was to compare the efficacy of online exercise therapy on physical and mental health with that of conventional exercise therapy in young adults with self-reported chronic non-specific neck pain.
Results
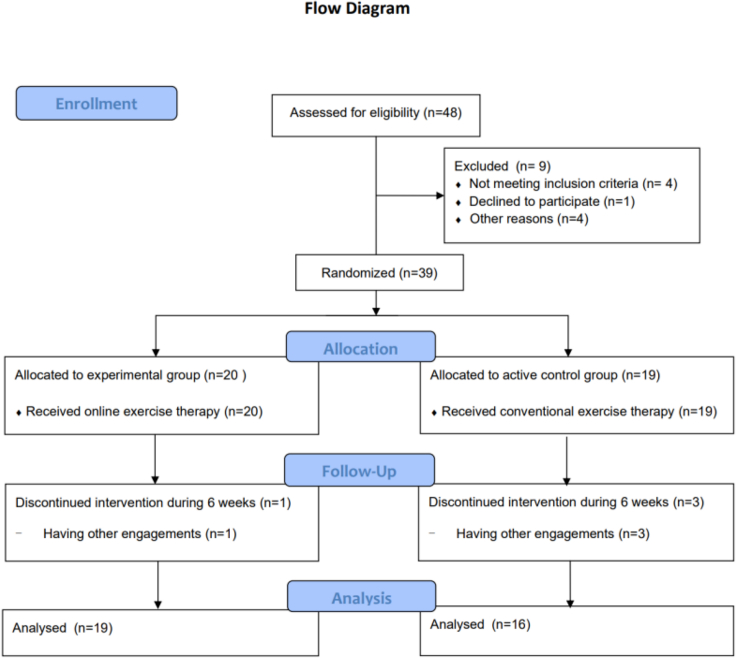
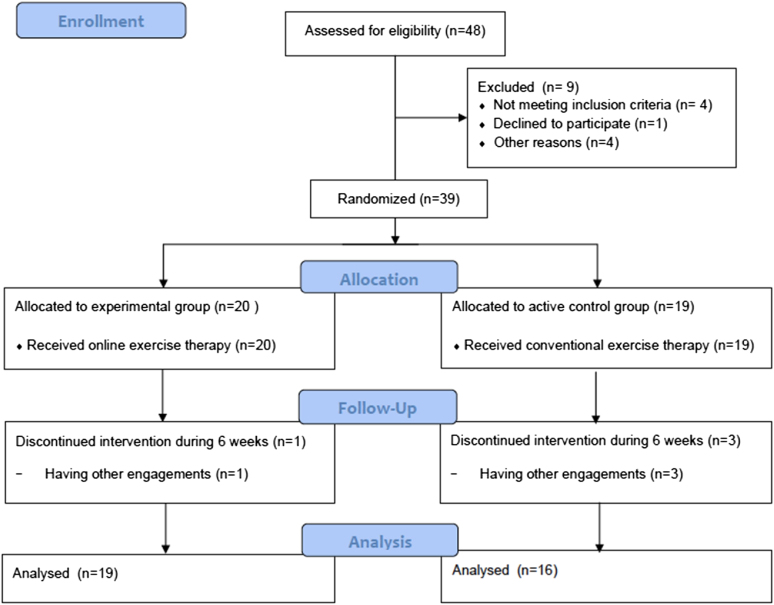
From April to June 2021, 48 potentially eligible participants were recruited and screened for eligibility. Nine participants were excluded for the reasons of not meeting the inclusion criteria (n = 4), declining to participate (n = 1) or other reasons (n = 4). Finally, 39 participants were included for stratified randomization. Twenty participants were assigned to the experimental group and 19 participants were assigned to the active control group respectively. Figure 1 shows the flow diagram of participants of the two groups. All participants received the exercise therapy for 6 weeks. Due to lack of time, 4 participants dropped out during follow-up, with 3 participants from the active control group and 1 from the experimental group. In total, the data of 35 participants were analyzed, with 19 participants in the experimental group and 16 participants in the active control group. All the participants were university students. The baseline characteristics of the participants are shown in Table 1. The characteristics of the 2 groups appeared to be well balanced at baseline. The primary and secondary outcomes are shown in Table 2.
Figure 1.
CONSORT flow diagram of participants
Table 1.
Baseline characteristics of participants
| Baseline Characteristics | Experimental Group (n = 19) | Active Control Group(n = 16) | p value |
|---|---|---|---|
| Male(%) | 12 (63%) | 9 (56%) | 0.739a |
| Height (cm) | 169.2 ± 8.5 | 169.7 ± 7.8 | 0.864b |
| Weight(kg) | 63.3 ± 11.9 | 65.6 ± 10.9 | 0.547b |
| Age (year) | 21.0 ± 2.9 | 22.0 ± 3.2 | 0.339b |
| Student athletes (%) | 3 (16%) | 4 (25%) | 0.677a |
| Duration of neck pain (week) | 63.9 ± 56.9 | 48.4 ± 61.6 | 0.392c |
| VAS (mean) | 3.8 ± 1.4 | 3.4 ± 1.7 | 0.504b |
| VAS (max) | 5.6 ± 1.7 | 5.6 ± 1.9 | 0.945b |
| NDI | 20.3 ± 7.6 | 19.5 ± 8.8 | 0.784b |
| HADS | 9.2 ± 4.5 | 8.9 ± 6.8 | 0.883b |
| HADS-A | 6.2 ± 2.6 | 6.1 ± 4.4 | 0.937b |
| HADS-D | 3.0 ± 2.9 | 2.8 ± 2.8 | 0.847b |
| WLQ | 55.5 ± 9.3 | 49.4 ± 9.1 | 0.060b |
VAS (mean) = mean pain level; VAS (max) = maximum pain level; NDI = Neck Disability Index; HADS = Hospital Anxiety and Depression Scale; HADS-A = Hospital Anxiety and Depression Scale-Anxiety Subscale; HADS-D = Hospital Anxiety and Depression Scale-Depression Subscale; WLQ = Work Limitations Questionnaire.
Fisher Exact test.
Independent t test.
Mann-Whitney U test.
Table 2.
Mean difference within groups and difference between groups from baseline to 6 weeks
| Outcome | Time | Experimental Group |
Active Control Group |
Mean difference between groups in change from baseline | Effect size (between-group) | p value (between-group) | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean score | Mean change from baseline (95% CI) | p value (within- group) | Mean score | Mean change from baseline (95% CI) | p value (within- group) | |||||
| Primary outcomes | ||||||||||
| VASmean | Baseline | 3.8 ± 1.4 | 3.4 ± 1.7 | |||||||
| 6 weeks | 3.0 ± 1.4 | 0.8 (0.1, 1.5) | 0.022 | 2.0 ± 0.9 | 1.4 (0.7, 2.1) | 0.001 | 0.6 (−0.4, 1.5) | 0.61 | 0.219 | |
| VASmax | Baseline | 5.6 ± 1.7 | 5.6 ± 1.9 | |||||||
| 6 weeks | 4.4 ± 1.8 | 1.2 (0.4, 2.0) | 0.005 | 3.7 ± 1.8 | 1.9 (0.9, 2.9) | 0.001 | 0.7 (−0.6, 1.9) | 0.39 | 0.282 | |
| NDI | Baseline | 20.3 ± 7.6 | 19.5 ± 8.8 | |||||||
| 6 weeks | 15.4 ± 6.1 | 4.9 (2, 7.9) | 0.002 | 14.0 ± 7.1 | 5.5 (0.8, 10.2) | 0.024 | 0.6 (−4.8, 6.0) | 0.21 | 0.822 | |
| Secondary outcomes | ||||||||||
| HADS | Baseline | 9.2 ± 4.5 | 8.9 ± 6.8 | |||||||
| 6 weeks | 7.3 ± 3.4 | 1.9 (0.2, 3.6) | 0.029 | 6.9 ± 5.5 | 1.9 (0.1, 3.7) | 0.037 | 0 (−2.3, 2.4) | 0.09 | 0.971 | |
| HADS-A | Baseline | 6.2 ± 2.6 | 6.1 ± 4.4 | |||||||
| 6 weeks | 5 ± 2.7 | 1.2 (0.1,2.2) | 0.035 | 4.5 ± 2.8 | 1.6 (0.2, 2.9) | 0.029 | 0.4 (−1.2, 2.1) | 0.18 | 0.621 | |
| HADS-D | Baseline | 3 ± 2.9 | 2.8 ± 2.8 | |||||||
| 6 weeks | 2.3 ± 1.6 | 0.7 (−0.4,1.9) | 0.197 | 2.4 ± 2.9 | 0.4 (−6.3, 1.4) | 0.440 | −0.4 (−1.9, 1.1) | −0.04 | 0.629 | |
| WLQ | Baseline | 55.5 ± 9.3 | 49.4 ± 9.1 | |||||||
| 2 weeks | 50.9 ± 12.5 | 4.6 (−2.1,11.3) | 0.165 | 47.9 ± 9.8 | 1.6 (−3.8, 7.0) | 0.547 | −3.1 (−11.6, 5.5) | 0.26 | 0.469 | |
| 4 weeks | 47.5 ± 18.6 | 8.0 (−2.0, 18.0) | 0.110 | 45.3 ± 10.3 | 4.2 (−1.7, 10.1) | 0.150 | −3.8 (−15.6, 8.0) | 0.14 | 0.514 | |
| 6 weeks | 39.4 ± 13.1 | 16.1 (8.7, 23.5) | <0.001 | 37.6 ± 8.4 | 11.9 (6.4, 17.4) | <0.001 | −4.2 (−13.4, 4.9) | 0.16 | 0.355 | |
VASmean = average pain intensity; VASmax = maximum pain intensity; NDI = Neck Disability Index; HADS = Hospital Anxiety and Depression Scale; HADS-A = Hospital Anxiety and Depression Scale-Anxiety Subscale; HADS-D = Hospital Anxiety and Depression Scale-Depression Subscale; WLQ = Work Limitations Questionnaire.
VAS and NDI
Both the experimental group and the active control group had improvements in the average and maximum pain level (mean: 1.4 vs. 0.8 and 1.9 vs. 1.2 respectively) from the baseline to 6 weeks with statistical significance. The mean differences between groups in average and maximum pain level were only 0.6 (95% CI -0.4 to 1.5) and 0.7 (95% CI -0.6 to 1.9) respectively with no statistical significance. Both groups also improved in the NDI scores from the baseline to 6 weeks with a mean change of 4.9 point in the experimental group and a mean change of 5.5 point in the active control group with statistical significance. The mean difference between groups in NDI was only 0.6 (95% CI -4.8 to 6.0). The effect sizes of group differences in average and maximum pain level and NDI were 0.61, 0.39 and 0.21 respectively, which were deemed to be small to medium in magnitude.
HADS
Both the experimental group and the active control group had statistically significant reductions in the HADS scores (mean changes of 1.9 in both groups) from the baseline to 6 weeks. The HADS-A was also diminished with a mean of 1.2 in the experimental group and a mean of 1.6 in the active control group, and a mean between-group difference of 0.4 (95% CI -1.2 to 2.1). The reduction in HADS-D was minimal in both groups (mean: 0.7 vs. 0.4 in experimental group and active control group respectively) from the baseline to 6 weeks without statistically significant mean between-group difference of −0.4 (95% CI -1.9 to 1.1). The effect sizes of group differences in HADS, HADS-A, and HADS-D were 0.09, 0.18, and -0.04 respectively, which were considered as small in magnitude.
WLQ
For the WLQ, there were no statistically significant improvements in the first 4 weeks in both groups. Statistically significant improvements were observed from baseline to 6 weeks in WLQ for the experimental group (mean: 16.1) and active control group (mean: 11.9) with a mean between-group difference of −4.2 (−13.4 to 4.9). There were steady percentage reductions in WLQ for the experimental group at 2 weeks (−6.7%), 4 weeks (−10.7%), and 6 weeks (−28.4%) and for the active control group at 2 weeks (−3.2%), 4 weeks (−8.5%), and 6 weeks (−24.0%). The effect sizes of group differences in WLQ in 2 weeks, 4 weeks, and 6 weeks were 0.26, 0.14, and 0.16 respectively, which were small in magnitude.
Discussion
This study aimed to examine the efficacy of online exercise therapy compared with the conventional exercise therapy in young adults with self-reported non-specific chronic neck pain. Six weeks of the online exercise therapy appeared as effective as the conventional exercise therapy in the reduction of pain and disability, and also the improvement in anxiety. In terms of meeting the minimal clinically important change (MCIC) in pain intensity and neck disability, the improvements in the active control group seemed better than the experimental group. The MCIC of pain intensity and NDI score for patients with chronic neck pain are about 1.5 and 5.5 respectively.12 The mean within-group changes in maximum pain intensity (1.9) and NDI (5.5) in the active control group were able to meet the MCIC of these outcomes while those within-group changes in the experimental group (VASmax = 1.2 and NDI = 4.9) did not exceed the MCIC. The effect sizes of group differences in the maximum pain intensity and NDI were small, though the effect size of group difference in average pain level appeared moderate. However, this group difference did not reach statistical significance. It was possible that the conventional exercise therapy might have a slightly better effect in reducing the average neck pain level of those participants than the online exercise therapy.
The literature on the use of telerehabilitation for adults with chronic neck pain is scarce. Compared with previous studies, the present study obtained slightly smaller effects in pain and functional improvement. In a randomized controlled trial of home telerehabilitation consisting of phone calls to remind participants with chronic neck pain to continue neck stretching exercise, there were improvements of mean pain level of 2.9 and mean NDI score of 7.4 from baseline to 6 months.13 The greater reductions of pain level and disability in these patients were likely resulted from a much longer duration of intervention of 6 months as compared with the present study of 6 weeks. In another randomized controlled trial of telerehabilitation-based structured exercise therapy consisting of stretching, strengthening, stabilization and proprioceptive exercises for 4 weeks, the mean pain level and NDI reduced 3.6 and 7.3 respectively in the remote supervised group with online video conferencing twice a week.14 However, the baseline pain level of participants of studies of Gialanella et al.13 and Özel and Kaya14 was much higher (6.8) than that of participants (3.8) in the present study. On the other hand, the baseline NDI score in the present study (20.3 in experimental group) was comparable to that in participants of Gialanella et al.’s study13 (NDI = 20.0) and slightly higher than that in participants of the study of Özel and Kaya14 (NDI = 16.0). These discrepancies in the pain and NDI reductions of the present study with the above 2 studies reported in the literature may be attributed to the differences in the intensity, repetitions, types of exercise therapy and duration of intervention.
It has been shown that exercise therapy is also effective in improving mental conditions in patients with neck pain.7 In both groups of the present study, the mean HADS scores had been improved with a mean change of 1.9 from the baseline to 6 weeks. The reduction in the HADS scores was largely resulted from the reduction in the HADS-A scores. The baseline HADS-D scores were low in both groups. Anxiety is often considered to precede depression in the response to stressors. Individuals usually show higher level of anxiety before the onset of depression.15 This may explain the higher level of anxiety but lower level of depression in the participants of the present study. In addition, the anxiety and depression levels showed an inverse association with occupational skill level, especially for depression.16 As all the participants were university students with high occupational skill level, their low HADS-D scores would be expected. It is generally accepted that with a HADS score less than 8, there is a clinically significant improvement in the anxiety and depressive state.16 On the other hand, the MCID of the HADS has been reported to be 1.7 in cardiovascular patients,17 but no such information is available for people with chronic neck pain. Based on these results, both the online exercise therapy and conventional exercise therapy could effectively reduce the anxiety state of participants in both groups. The effect sizes of group differences in HADS and their subscale were only small with no statistical significance.
The results of the present study also show that the work efficiency of participants in both groups had improved. The WLQ had been used to assess the extent to which the health problems affecting specific aspects of job performance and the productivity impact of these work limitations.18 The WLQ scores of both groups decreased by more than 20% from the baseline to 6 weeks. It had been reported that with every 10% reduction in WLQ score, there will be an increase in the work efficiency by 4–5%.19 Therefore, both the conventional exercise therapy and online exercise therapy were effective in improving job the performance and productivity of the participants, with the online exercise therapy achieving a larger but statistically non-significant improvement. The effect sizes of group differences in WLQ scores were only small. The improvement in the job performance and productivity was consistent with the improvement in the anxiety state of the participants as the work limitation is positively related to the psychological dysfunction.20
There are many potential benefits of telerehabilitation for patients in the form of online exercise therapy. The patients receiving online exercise therapy can save travel time and expenses. It is also more flexible for the patients to choose the time to perform the exercises themselves. However, the lack of direct supervision by the physiotherapist may reduce the effectiveness of the exercises. Therefore, clear exercise demonstration with regular video conferencing with the physiotherapist should be an essential component of the online exercise therapy. In a previous study, familiarity with technology was related to age and resilience; participation with telerehabilitation was associated with younger ages and higher cognitive reserves.21 As all the participants were university students, it was expected that their understanding and compliance to the online exercise would be good. More difficulties and compliance problems may be encountered if older adults or people with low educational level were involved. In addition, self-discipline is also important for the successful implementation of the online exercise therapy. In this study, many participants in the experimental group followed the instructions to perform the online exercise and attended the videoconferencing once a week, and posted their exercise records on WeChat app twice a week. However, a minority of participants need to be reminded by the physiotherapist to continue the exercise, to attend the videoconferencing and to post their exercise records.
The primary strength of the present study was the use of a randomized controlled trial design to compare the conventional exercise therapy and online exercise therapy. However, there were several limitations of the study: first, the 6-week intervention period might not be long enough for those with chronic neck pain to achieve a large improvement in the primary outcomes. Second, the exercise compliance of both groups had not been formally assessed. Third, the sample size of the study was likely to be limited as all the between-group comparisons were statistically non-significant with wide confidence intervals. Lastly, as the recruited participants were young adults, the study results could not be generalized to the older populations.
Overall, for young adults with chronic neck pain, both the online and conventional exercise interventions could improve their pain level, neck disability, anxiety state and work efficiency. The online exercise intervention appeared feasible as an alternative treatment option to improve the physical and mental health of young adults with chronic neck pain, with comparable results as conventional exercise intervention. Future studies with larger sample size in wider population are recommended.
Limitations of the study
The findings of this study have to be seen in light of some limitations. The first is the limited participants for the trial. Because of the COVID-19 lockdown, only on-campus subjects could be recruited, which might cause bias. The second limitation concerns the short duration of the trial intervention. The duration of the trial could be longer, however in order to avoid the period preparing the university examinations, which might be a confusing variable for affecting the levels of anxiety and depression of the participants, the duration of trial had to be shortened.
STAR★Methods
Key resources table
| REAGENT or RESOURCE | SOURCE | IDENTIFIER |
|---|---|---|
| Software and algorithms | ||
| G∗Power 3.1.9.2 (University Kiel, Germany) | Kang H.22 | https://www.psychologie.hhu.de/arbeitsgruppen/allgemeine-psychologie-und-arbeitspsychologie/gpower |
| IBM SPSS Statistics for Windows, Version 24.0 (Armonk, NY: IBM Corp). | IBM SPSS® | https://www.ibm.com/cn-zh/products/spss-statistics |
| Other | ||
| Raw and analyzed data | This paper |
https://data.mendeley.com/datasets/xmnhphn7v7/draft?a=7992b05f-974b-4b43-9d02-46e51f62482b user name:1061455650@qq.com password:linyiting05 |
Resource availability
Lead contact
Further information and requests for resources and reagents should be directed to and will be fulfilled by the lead contact, Jinghua Qian (15601679152@163.com).
Materials availability
This study did not generate new unique reagents.
Data and code availability
-
•
data have been deposited at Mendeley Data and are publicly available as of the date of publication. Accession numbers are listed in the key resources table.
-
•
This paper does not report original code.
-
•
Any additional information required to reanalyze the data reported in this paper is available from the lead contact upon request.
Experimental model and study participant details
Participants
In this experiment, all participants were all Chinese university students, who were born in China and spoke mandarin as mother tongue, aged between 18 to 32. There were totally 21 adult males and 14 adults females. The experimental group contained 12 adult males and 7 adult females (n = 19), and the active control group contained 9 adult males and 7 adult females (n = 16). Stratified block randomization was performed with gender and status as student athletes as the strata, and the characteristics of the 2 groups appeared to be well balanced at baseline.
Method details
Study design
A randomized clinical trial recruiting 35 university students with self-reported chronic neck pain was conducted. Participants were randomly assigned into the experimental group receiving 6-week online exercise therapy and the active control group receiving the same face-to-face conventional exercise therapy. The primary outcomes were visual analogue scale (VAS) for pain and Neck Disability Index (NDI). The secondary outcomes were Work Limitations Questionnaire (WLQ), the Hospital Anxiety and Depression Scale (HADS) and its subscales (HADS-A and HADS-D). Participants were assessed at baseline and at 6 weeks while the changes in WLQ were assessed biweekly.
Sample size
| Treatment | N= | |
|---|---|---|
| Experimental group | Online exercise therapy | 20 |
| Active control group | Conventional exercise therapy | 19 |
Participants were randomly assigned into the experimental group receiving 6-week online exercise therapy and the active control group receiving the same face-to-face conventional exercise therapy. There are 20 participants in experimental group and 19 participants in active control group.
The sample size for the study was calculated to be 32 using the G∗Power 3.1.9.2 (University Kiel, Germany),22 with an estimated effect size of group difference of 0.9 in primary outcomes and a level of significance of 0.05, statistical power of 80% with 2-tailed independent sample t test. The estimated effect size was based on previous studies of home exercise on patients with neck pain.23 With an anticipated dropout rate of 15%, a total of 39 participants was required.
Inclusion and exclusion criteria
Forty-eight participants were randomized into the study, of which 9 did not meet our inclusion and exclusion criteria because NDI didn’t reach 4, having cervical radiculopathy, decline to participate and other reasons. A total of 39 participants were therefor included in this study. Four participants dropped out before their final assessment: one from the experimental group and three from the active control group. A total of 35 participants were therefore included in the final analysis.
The experimental group contained 12 adult males and 7 adult females (n = 19), and the active control group contained 9 adult males and 7 adult females (n = 16). All the participants were Chinese university students. The characteristics of the 2 groups appeared to be well balanced at baseline.
Randomization
Stratified block randomization was performed with gender and status as student athletes as the strata. After baseline assessments, participants were randomized to either the experimental group or active control group. The list of random allocation with one-to-one allocation ratio was generated with computer by an independent member of the research team who was not involved in the trial. The allocation sequence was concealed with the use of sealed numbered opaque envelopes.
Blinding
This study was performed as a single-blind experiment. The outcome measures were completed by particular investigators, who did not participate in the intervention process and were not clear about the grouping of participants.
Outcome measures
There were 3 primary outcomes. The first 2 were the average and maximum neck pain from baseline to the end of intervention, measured by 100-mm visual analog scale (VAS).24 The measurement of average and maximum pain levels is important to have more complete understanding of the pain state of subjects in clinical trials and this is a common practice and recommended by the Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials (IMMPACT).25 The third outcome was the neck dysfunction from baseline to the end of intervention, which was measured with the Neck Disability Index (NDI).26 Previous studies had shown that the reliability and validity of the VAS27,28 and NDI7,26,29,30,31,32 are acceptable to good. There were 2 secondary outcomes: the mental condition from baseline to the end of intervention, which was measured with the Hospital Anxiety and Depression Scale (HADS),33,34 and the work efficiency from baseline to the end of 2, 4 and 6 weeks of intervention, which were assessed with the Work Limitations Questionnaire (WLQ).18,35,36 The HADS, which was originally developed by Zigmond and Snaith,37 is a widely used screening and evaluative tool for clinically relevant anxiety and depression.38,39 Those with score ≥8 on HADS-A or HADS-D were considered to be at high risk of having anxiety or depression.40
The sample size for the study was calculated to be 32 using the G∗Power 3.1.9.2, with an estimated effect size of group difference of 0.9 in primary outcomes and a level of significance of 0.05, statistical power of 80% with 2-tailed independent sample t test. With an anticipated dropout rate of 15%, a total of 39 participants was required.
Statistical methods
Continuous data were expressed as means and standard deviations. Categorical data were shown as frequencies or percentages, with group comparisons performed using the Fisher exact test. The normality of continuous data was checked with the Shapiro-Wilk test. The change scores of the primary and secondary outcome variables from baseline to end of intervention between the 2 groups were compared using independent sample t test with approximate data normality. The Cohen’s effect sizes of between-group comparisons were calculated.41 The Mann-Whitney U test was used for group comparison of non-normal continuous data. Within-group comparisons were done using paired sample t test. The level of significance of all statistical tests was set with 2-tailed at 0.05.
Experimental procedures
As shown in the flowchart, randomized clinical trial with 39 adults (totally 48 participants were recruited, 9 participants were excluded) with self-reported chronic neck pain recruited. They were randomly assigned into two groups, 20 participants in the experimental group and 19 participants in the active control group. The experimental group received online exercise therapy and the control group received conventional exercise therapy. Participants in both groups completed the same exercise program three times a week for six weeks with either face-to-face or online mode of delivery by physiotherapists. The degree of pain was assessed by the improvement in average and maximum visual analogue scale (VAS). Neck function and work limitations were assessed by the Neck Disability Index (NDI) and Work Limitations Questionnaire (WLQ) respectively. The Hospital Anxiety and Depression Scale (HADS) and its subscales were used to evaluate anxiety and depressive symptoms. Participants were assessed at baseline and at 6 weeks while the changes in WLQ were assessed biweekly. To ensure the effectiveness of online exercise therapy, therapists delivered the online exercise 3 times a week for 6 weeks, with videoconferencing once a week and posting of exercise record on WeChat app twice a week. After the intervention and measurements, all data was analysed. Finally, 19 participants’ data in the experimental group (1 participants dropped out) and 16 participants’ data in the active control group (3 participants dropped out) were analyzed.
Intervention
At baseline, the suitable elastic bands (Thera-band®) for performing the exercises in both experimental group and active control group were selected by testing the 15 repetitions maximum (15RM) of the Modified Brügger’s Exercise (MBE) and the Modified Proprioceptive Neuromuscular Facilitation Diagonal Flexion Exercise (MPNFDFE). The details of the MBE and MPNFDFE were described in File S1.
Participants in the active control group were divided into several small groups of 3-5 participants to perform the following exercises 3 sessions per week for 6 weeks in the laboratory of the Sport Medicine and Rehabilitation School of the Beijing Sport University. The exercises included (See Figures S2–S4):
-
A.
Warm-up exercises
-
B.
Cranio-cervical flexion exercises
-
C.
Strength-endurance exercises
-
D.
Scapular stabilization exercises
-
E.
Stretching exercises
Participants in the experimental group performed the same set of exercises 3 sessions per week for 6 weeks in their home, with the following arrangements:
The participants had weekly online exercise meetings with the physiotherapist in a group of 3-5 participants using the Tencent Meeting app. Then the participants performed the remaining 2 sessions themselves weekly. If they had encountered any problems, they could consult the physiotherapist during the online session or send messages to the physiotherapist using the WeChat app. All the participants of the experimental group received a package of exercise pamphlet and a video disc containing 17-minute exercise demonstrations by the physiotherapist.
Quantification and statistical analysis
Statistical details of experiments
In the result description, flow diagram and Table 1, n represents number of participants. In Table 2, mean, SD and CI of outcomes can be found.
The statistical tests used
Continuous data were expressed as means and standard deviations. Categorical data were shown as frequencies or percentages, with group comparisons performed using the Fisher exact test. The normality of continuous data was checked with the Shapiro-Wilk test. The change scores of the primary and secondary outcome variables from baseline to end of intervention between the 2 groups were compared using independent sample t test with approximate data normality. The Cohen’s effect sizes of between-group comparisons were calculated. The Mann-Whitney U test was used for group comparison of non-normal continuous data. Within-group comparisons were done using paired sample t test. All statistical analyses were conducted using the IBM SPSS Statistics for Windows, Version 24.0 (Armonk, NY: IBM Corp). The level of significance of all statistical tests was set with 2-tailed at 0.05. Per-protocol analysis was used.
Randomization and stratification
Stratified block randomization was performed with gender and status as student athletes as the strata. After baseline assessments, participants were randomized to either the experimental group or active control group. The experimental group received online exercise therapy while the active control group received conventional face-to-face exercise therapy. The list of random allocation with one-to-one allocation ratio was generated with computer by an independent member of the research team who was not involved in the trial. The allocation sequence was concealed with the use of sealed numbered opaque envelopes.
Sample size estimation
The sample size for the study was calculated to be 32 using the G∗Power 3.1.9.2 (University Kiel, Germany), with an estimated effect size of group difference of 0.9 in primary outcomes and a level of significance of 0.05, statistical power of 80% with 2-tailed independent sample t test. The estimated effect size was based on previous studies of home exercise on patients with neck pain. With an anticipated dropout rate of 15%, a total of 39 participants was required.
Inclusion and exclusion of subjects
The target participants were adults with self-reported non-specific neck pain for more than 3 months. They were recruited through posters and social media in the campus of the Beijing Sport University. The inclusion criteria were: (1) adults between age of 18 and 50 years with non-specific neck pain (from occiput to 7th cervical vertebra) for at least 3 months; (2) the Neck Disability Index score ≥ 4/50. Those participants with the following were excluded: (1) adults with a history of previous neck surgery, cervical radiculopathy, acute neck injury or fracture; (2) persons who had more than 2 hours of moderate intensity exercise or more than 4 hours of low intensity exercise per week; (3) persons who had received any form of physiotherapy treatment for the neck pain in the last 6 months; and (4) persons with cardiopulmonary or chronic diseases which would pose health risk to them in performing neck exercises. The eligibility of the participants was assessed using a standardized questionnaire.
Additional resources
Clinical trial registry number:NCT05992051.
Protocol download website:https://clinicaltrials.gov/study/NCT05992051?cond=NCT05992051&rank=1.
Acknowledgments
The research was supported by the Fundamental Research Funds for the Central Universities (the Laboratory of Exercises Rehabilitation Science). The author gratefully acknowledges the support by Beijing Sport University. Useful help given by Yang Zhang, Heming Zhou, Yuxin Yuan are also acknowledged.
Author contributions
Conceptualization, Y.L.; Methodology, Y.L., R.T., J.Q., J.H., and N.Z.; Investigation, Y.L., J.H., N.Z., X.Z., and J.L.; Data collection and processing, Y.L., R.T., J.H., N.Z., X.Z., and J.L.; Writing – Original Draft, Y.L. and R.T.; Writing –Review and Editing, R.T. and J.Q.; Supervision, J.Q.
Declaration of interests
The authors declare no competing interests.
Inclusion and diversity
We support inclusive, diverse, and equitable conduct of research.
Published: November 23, 2023
Footnotes
Supplemental information can be found online at https://doi.org/10.1016/j.isci.2023.108543.
Supplemental information
References
- 1.Safiri S., Kolahi A.A., Hoy D., Buchbinder R., Mansournia M.A., Bettampadi D., Ashrafi-Asgarabad A., Almasi-Hashiani A., Smith E., Sepidarkish M., et al. Global, regional, and national burden of neck pain in the general population, 1990-2017: systematic analysis of the Global Burden of Disease Study 2017. BMJ. 2020;368:m791. doi: 10.1136/bmj.m791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wu A., Dong W., Zeng X., Xu X., Xu T., Zhang K., Tian H., Zhao J., Wang X., Zhou M. Neck pain is the leading cause of disability burden in China: findings from the Global Burden of Disease Study 2017. Ann. Transl. Med. 2021;9:777. doi: 10.21037/atm-20-6868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Xu Y., Wang Y., Chen J., He Y., Zeng Q., Huang Y., Xu X., Lu J., Wang Z., Sun X., et al. The comorbidity of mental and physical disorders with self-reported chronic back or neck pain: results from the China Mental Health Survey. J. Affect. Disord. 2020;260:334–341. doi: 10.1016/j.jad.2019.08.089. [DOI] [PubMed] [Google Scholar]
- 4.Kazeminasab S., Nejadghaderi S.A., Amiri P., Pourfathi H., Araj-Khodaei M., Sullman M.J.M., Kolahi A.A., Safiri S. Neck pain: global epidemiology, trends and risk factors. BMC Musculoskelet. Disord. 2022;23:26. doi: 10.1186/s12891-021-04957-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beltran-Alacreu H., López-de-Uralde-Villanueva I., Calvo-Lobo C., Fernández-Carnero J., La Touche R. Clinical features of patients with chronic non-specific neck pain per disability level: a novel observational study. Rev. Assoc. Med. Bras. 2018;64:700–709. doi: 10.1590/1806-9282.64.08.700. [DOI] [PubMed] [Google Scholar]
- 6.Blanpied P.R., Gross A.R., Elliott J.M., Devaney L.L., Clewley D., Walton D.M., Sparks C., Robertson E.K. Neck pain: revision 2017. J. Orthop. Sports Phys. Ther. 2017;47:A1–A83. doi: 10.2519/jospt.2017.0302. [DOI] [PubMed] [Google Scholar]
- 7.Nazari G., Bobos P., Billis E., MacDermid J.C. Cervical flexor muscle training reduces pain, anxiety, and depression levels in patients with chronic neck pain by a clinically important amount: A prospective cohort study. Physiother. Res. Int. 2018;23 doi: 10.1002/pri.1712. [DOI] [PubMed] [Google Scholar]
- 8.Havran M.A., Bidelspach D.E. Virtual physical therapy and telerehabilitation. Phys. Med. Rehabil. Clin. N. Am. 2021;32:419–428. doi: 10.1016/j.pmr.2020.12.005. [DOI] [PubMed] [Google Scholar]
- 9.De Biase S., Cook L., Skelton D.A., Witham M., Ten Hove R. The COVID-19 rehabilitation pandemic. Age Ageing. 2020;49:696–700. doi: 10.1093/ageing/afaa118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Seron P., Oliveros M.J., Gutierrez-Arias R., Fuentes-Aspe R., Torres-Castro R.C., Merino-Osorio C., Nahuelhual P., Inostroza J., Jalil Y., Solano R., et al. Effectiveness of telerehabilitation in physical therapy: a rapid overview. Phys. Ther. 2021;101 doi: 10.1093/ptj/pzab053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fandim J.V., Costa L.O.P., Yamato T.P., Almeida L., Maher C.G., Dear B., Kamper S.J., Saragiotto B.T. Telerehabilitation for neck pain. Cochrane Database Syst. Rev. 2021;2021:CD014428. [Google Scholar]
- 12.Young I.A., Dunning J., Butts R., Mourad F., Cleland J.A. Reliability, construct validity, and responsiveness of the neck disability index and numeric pain rating scale in patients with mechanical neck pain without upper extremity symptoms. Physiother. Theory Pract. 2019;35:1328–1335. doi: 10.1080/09593985.2018.1471763. [DOI] [PubMed] [Google Scholar]
- 13.Gialanella B., Ettori T., Faustini S., Baratti D., Bernocchi P., Comini L., Scalvini S. Home-based telemedicine in patients with chronic neck pain. Am. J. Phys. Med. Rehabil. 2017;96:327–332. doi: 10.1097/PHM.0000000000000610. [DOI] [PubMed] [Google Scholar]
- 14.Özel M., Kaya Ciddi P. The effectiveness of telerehabilitation-based structured exercise therapy for chronic nonspecific neck pain: A randomized controlled trial. J. Telemed. Telecare. 2022 doi: 10.1177/1357633X221095782. [DOI] [PubMed] [Google Scholar]
- 15.Stern A.F. The Hospital Anxiety and Depression Scale. Occup. Med. 2014;64:393–394. doi: 10.1093/occmed/kqu024. [DOI] [PubMed] [Google Scholar]
- 16.Sanne B., Mykletun A., Dahl A.A., Moen B.E., Tell G.S., Hordaland Health Study Occupational differences in levels of anxiety and depression: the Hordaland Health Study. J. Occup. Environ. Med. 2003;45:628–638. doi: 10.1097/01.jom.0000069239.06498.2f. [DOI] [PubMed] [Google Scholar]
- 17.Lemay K.R., Tulloch H.E., Pipe A.L., Reed J.L. Establishing the minimal clinically important difference for the hospital anxiety and depression scale in patients with cardiovascular disease. J. Cardiopulm. Rehabil. Prev. 2019;39:E6–E11. doi: 10.1097/HCR.0000000000000379. [DOI] [PubMed] [Google Scholar]
- 18.Lerner D., Amick B.C., 3rd, Rogers W.H., Malspeis S., Bungay K., Cynn D. The Work Limitations Questionnaire. Med. Care. 2001;39:72–85. doi: 10.1097/00005650-200101000-00009. [DOI] [PubMed] [Google Scholar]
- 19.Lerner D., Amick B.C., 3rd, Lee J.C., Rooney T., Rogers W.H., Chang H., Berndt E.R. Relationship of employee-reported work limitations to work productivity. Med. Care. 2003;41:649–659. doi: 10.1097/01.MLR.0000062551.76504.A9. [DOI] [PubMed] [Google Scholar]
- 20.Toyoshima K., Inoue T., Shimura A., Uchida Y., Masuya J., Fujimura Y., Higashi S., Kusumi I. Mediating Roles of Cognitive Complaints on Relationships between Insomnia, State Anxiety, and Presenteeism in Japanese Adult Workers. Int. J. Environ. Res. Public Health. 2021;18:4516. doi: 10.3390/ijerph18094516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Milani G., Demattè G., Ferioli M., Dallagà G., Lavezzi S., Basaglia N., Straudi S. Telerehabilitation in Italy during the COVID-19 lockdown: A feasibility and acceptability study. Int. J. Telerehabil. 2021;13 doi: 10.5195/ijt.2021.6334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kang H. Sample size determination and power analysis using the G∗Power software. J. Educ. Eval. Health Prof. 2021;18:17. doi: 10.3352/jeehp.2021.18.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zronek M., Sanker H., Newcomb J., Donaldson M. The influence of home exercise programs for patients with non-specific or specific neck pain: a systematic review of the literature. J. Man. Manip. Ther. 2016;24:62–73. doi: 10.1179/2042618613Y.0000000047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Huskisson E.C. Measurement of pain. Lancet. 1974;2:1127–1131. doi: 10.1016/s0140-6736(74)90884-8. [DOI] [PubMed] [Google Scholar]
- 25.Dworkin R.H., Turk D.C., Farrar J.T., Haythornthwaite J.A., Jensen M.P., Katz N.P., Kerns R.D., Stucki G., Allen R.R., Bellamy N., et al. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain. 2005;113:9–19. doi: 10.1016/j.pain.2004.09.012. [DOI] [PubMed] [Google Scholar]
- 26.Vernon H., Mior S. The Neck Disability Index: a study of reliability and validity. J. Manip. Physiol. Ther. 1991;14:409–415. [PubMed] [Google Scholar]
- 27.Gialanella B., Comini L., Olivares A., Gelmini E., Ubertini E., Grioni G. Pain, disability and adherence to home exercises in patients with chronic neck pain: long term effects of phone surveillance. A randomized controlled study. Eur. J. Phys. Rehabil. Med. 2020;56:104–111. doi: 10.23736/S1973-9087.19.05686-7. [DOI] [PubMed] [Google Scholar]
- 28.Li L., Liu X., Herr K. Postoperative pain intensity assessment: a comparison of four scales in Chinese adults. Pain Med. 2007;8:223–234. doi: 10.1111/j.1526-4637.2007.00296.x. [DOI] [PubMed] [Google Scholar]
- 29.Falla D., Jull G., Hodges P.W. Feedforward activity of the cervical flexor muscles during voluntary arm movements is delayed in chronic neck pain. Exp. Brain Res. 2004;157:43–48. doi: 10.1007/s00221-003-1814-9. [DOI] [PubMed] [Google Scholar]
- 30.Falla D., Jull G., Russell T., Vicenzino B., Hodges P. Effect of Neck Exercise on Sitting Posture in Patients With Chronic Neck Pain. Phys. Ther. 2007;87:408–417. doi: 10.2522/ptj.20060009. [DOI] [PubMed] [Google Scholar]
- 31.Jorritsma W., Dijkstra P.U., de Vries G.E., Geertzen J.H.B., Reneman M.F. Detecting relevant changes and responsiveness of Neck Pain and Disability Scale and Neck Disability Index. Eur. Spine J. 2012;21:2550–2557. doi: 10.1007/s00586-012-2407-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wu S., Ma C., Mai M., Li G. Translation and validation study of Chinese versions of the Neck Disability Index and the Neck Pain and Disability Scale. Spine. 2010;35:1575–1579. doi: 10.1097/BRS.0b013e3181c6ea1b. [DOI] [PubMed] [Google Scholar]
- 33.Leung C.M., Ho S., Kan C.S., Hung C.H., Chen C.N. Evaluation of the Chinese version of the Hospital Anxiety and Depression Scale. A cross-cultural perspective. Int. J. Psychosom. 1993;40:29–34. [PubMed] [Google Scholar]
- 34.Wang W., Chair S.Y., Thompson D.R., Twinn S.F. A psychometric evaluation of the Chinese version of the Hospital Anxiety and Depression Scale in patients with coronary heart disease. J. Clin. Nurs. 2009;18:1908–1915. doi: 10.1111/j.1365-2702.2008.02736.x. [DOI] [PubMed] [Google Scholar]
- 35.Dong X.F., Liu Y.J., Wang J.X., Peng Z.M. Development of the Work Limitations Questionnaire Chinese version (WLQ-C) Chin. J. Practical Nurs. 2013;29:54–57. [Google Scholar]
- 36.Stewart W.F., Ricci J.A., Leotta C. Health-related lost productive time (LPT): recall interval and bias in LPT estimates. J. Occup. Environ. Med. 2004;46:S12–S22. doi: 10.1097/01.jom.0000126685.59954.55. [DOI] [PubMed] [Google Scholar]
- 37.Zigmond A.S., Snaith R.P. The Hospital Anxiety and Depression Scale. Acta Psychiatr. Scand. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 38.Philippot A., Dubois V., Lambrechts K., Grogna D., Robert A., Jonckheer U., Chakib W., Beine A., Bleyenheuft Y., De Volder A.G. Impact of physical exercise on depression and anxiety in adolescent inpatients: A randomized controlled trial. J. Affect. Disord. 2022;301:145–153. doi: 10.1016/j.jad.2022.01.011. [DOI] [PubMed] [Google Scholar]
- 39.Kannampallil T., Ajilore O.A., Lv N., Smyth J.M., Wittels N.E., Ronneberg C.R., Kumar V., Xiao L., Dosala S., Barve A., et al. Effects of a virtual voice-based coach delivering problem-solving treatment on emotional distress and brain function: a pilot RCT in depression and anxiety. Transl. Psychiatry. 2023;13:166. doi: 10.1038/s41398-023-02462-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Huang X., Meyers K., Liu X., Li X., Zhang T., Xia W., Hou J., Song A., He H., Li C., et al. The double burdens of mental health among AIDS patients with fully successful immune restoration: a cross-sectional study of anxiety and depression in China. Front. Psychiatry. 2018;9:384. doi: 10.3389/fpsyt.2018.00384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hojat M., Xu G. Visitor's guide to effect sizes: statistical significance versus practical (clinical) importance of research findings. Adv. Health Sci. Educ. Theory Pract. 2004;9:241–249. doi: 10.1023/B:AHSE.0000038173.00909.f6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
-
•
data have been deposited at Mendeley Data and are publicly available as of the date of publication. Accession numbers are listed in the key resources table.
-
•
This paper does not report original code.
-
•
Any additional information required to reanalyze the data reported in this paper is available from the lead contact upon request.