Abstract
Actinomycosis is a rare, chronic, and suppurative disease caused by Actinomyces species, which are filamentous, obligate, Gram-positive bacteria. This report presents a case of anterior abdominal actinomycosis in a 40-year-old female with a history of intrauterine contraceptive device placement. The patient presented with severe abdominal pain, an abdominal mass, low-grade fever, and weight loss. Imaging studies revealed thickening of the left rectus abdominis muscle and pericolic fat stranding. An exploratory laparotomy confirmed dense adhesions from the transverse colon and omentum to the abdominal wall with a purulent discharge. Resection of the affected colon segment and primary anastomosis were performed. Histopathological examination revealed characteristic colonies of Actinomyces within abscesses, confirming the diagnosis of actinomycosis. The patient received appropriate antibiotic therapy and showed improvement. This case highlights the rare occurrence of abdominal wall actinomycosis associated with an intrauterine contraceptive device and emphasizes the importance of considering actinomycosis in the differential diagnosis of abdominal pathologies. Thus, medical history related to intrauterine contraceptive device use should be regarded as in differentials if a patient presents vague abdominal mass and pain, and small details in history should be emphasized and looked upon so that a timely decision can be made for the betterment of the patient.
Keywords: Actinomycosis, abdominal actinomycosis, retained IUCD, abdominal pain, abdominal mass
Introduction
Actinomycosis is an uncommon condition characterized by a subacute or persistent suppurative (pus-forming) disease. It is attributed to the presence of specific types of bacteria known as Actinomyces species. 1 These are Gram-positive non-acid-fast, anaerobic, or microaerophilic/capnophilic, filamentous, obligate bacteria. Actinomycosis infection is extremely rare, occurring in approximately 1 out of every 300,000 individuals. 1 More than 30 species of Actinomyces have been identified to date, of which few are part of the flora of various body regions, including the oropharynx (throat and mouth), gastrointestinal tract, and urogenital tract. Actinomyces israelii and Actinomyces odontolyticus are the most frequently reported pathogens associated with infections among these. 1
Actinomycosis commonly affects the facial and cervical region in about 60% of cases, followed by the abdominal region in approximately 30%. The thoracic region is involved in about 20% of cases, while the pelvic region is affected in roughly 3%–5% of instances. 2 Abdominal actinomycosis develops slowly and can mimic symptoms of other conditions like diverticulitis, appendicitis, inflammatory bowel disease, and malignant tumours. Intrauterine contraceptive devices (IUCDs) can lead to actinomycotic infections in the pelvic area, with bacteria migrating from the uterus. 3 Actinomycosis of the abdominal wall associated solely with an IUCD, without pelvic or intraperitoneal involvement, is extremely rare, and reported cases are limited. 4 As such, only seven other cases have been reported, details of which are reported in Table 1.
Table 1.
Case reports presenting the association between IUCD and actinomycosis of the anterior abdominal wall.
| Study name | Length of IUCD usage | Duration of disease | History and symptoms | Examination and histopathological findings |
|---|---|---|---|---|
| Polat et al. 5 | 2 years | 3 months | A 37-year-old woman, gravida 4 para 3 abortus 1, was referred to our clinic with lower abdominal pain and persistent purulent discharge below the umbilicus for 3 months | Physical examination revealed a 2 cm × 2 cm sized sub umbilical skin ulcer Gynaecologic examination was unremarkable Bacteriological analysis of the IUD revealed the presence of A. israelii (‘sulphur granules’), Streptopeptococcus and Bacteroides fragilis infection |
| Çöl et al. 6 | 17 years | 1 year | A 48-year-old woman presented with complaints of weight loss, intermittent low-grade fever, and a mass localized to the left lower abdominal quadrant which she had noticed initially 2 weeks prior to admission, also presented with a history of occasional malodorous vaginal discharge for the past year | The blood pressure was 110/70 mmHg, pulse rate 112 beats/min, and body temperature 37.8°C. Further examination showed no abnormalities except for the painful irregular mass with a 5-cm diameter On histopathological examination of the mass, sulphur granules which were characteristic of actinomycosis were seen |
| Groot et al. 7 | N/A | N/A | The patient, a 24-year-old White woman, presented with lower abdominal pain, dysuria, urgency, and frequency | Histologic examination of the omentum demonstrated the typical Actinomycotic picture of gram-positive filamentous bacteria within the mass and club-like extensions beyond the periphery of the mass |
| Adachi et al. 8 | N/A | N/A | The patient, a 39-year-old woman, para 4-0-1-4, presented with lower abdominal pain | Pap smear findings were reported as cervical intraepithelial neoplasia, grade I–II, and endocervical curettage showed colonies of Actinomyces species. A subsequent cone biopsy revealed carcinoma in situ but no evidence of Actinomyces |
| Carkman et al. 4 | 8 years | 2 years | A 48-year-old Caucasian woman presented with a painful abdominal wall mass in June, 2003. She did not have any history of trauma, surgery, or malignancy After initiating empirical antibiotic therapy with amoxicillin-clavulanic acid per oral, the patient was discharged; however, she was lost to medical follow up. In March 2005, she was readmitted to our clinic with the deterioration of her symptoms |
Physical examination revealed a fixed and firm mass, about 5 cm in size, located around the umbilicus. The patient was afebrile Gynaecological examination was unremarkable except for an IUCD Histopathological examination showed acute and chronic inflammatory changes due to Actinomycotic colonies |
Case reports presenting the association between IUCD and actinomycosis of the anterior abdominal wall: There have been only seven other known cases of Actinomycosis of the abdominal wall associated solely with an IUCD, without pelvic or intraperitoneal involvement. The data from Lunca et al. 9 and Pearlman et al. 10 could not be extracted due to unavailability of full text and lack of information from abstract. Groot et al. 7 and Adachi et al., 8 only partial information was extracted due to unavailability of full text.
This paper will discuss a case of anterior abdominal actinomycosis in a middle-aged female with no known comorbidities but a positive history of IUCD placement 21 years back.
Case report
We present a case of a 40-year-old female patient who was admitted to our hospital in May 2020. She presented with complaints of severe abdominal pain for three months and gradually increasing abdominal mass for 15 days. The pain was accompanied by a low-grade fever and a weight loss of 2 kgs. The patient had a history of retaining an IUCD for 21 years, which was subsequently removed in April 2020. Notably, the patient had a history of retaining an IUCD for an extensive period of 21 years, until its removal in April 2020. The pain escalated in intensity, prompting the patient to elect for the removal of the IUCD. Additionally, she had pulmonary tuberculosis in 2003, for which she completed her course of Anti-Tuberculosis Therapy for 9 months. No other significant medical or surgical history was noted.
On admission, the physical examination revealed an ill-looking patient with mild pallor. Abdominal examination showed tenderness on superficial and deep palpation of the lower abdomen with a 6 cm × 7 cm ill-defend mass 1 cm lateral to the umbilicus. The swelling was tender, irreducible, mobile, and firm with negative cough impulse and Carnett sign negative. 11 Digital rectal exam was unremarkable. The routine blood tests showed an elevation in white blood cell count (14.2 × 109/L) and neutrophil levels (85.9%), along with a decrease in hemoglobin levels (8.4 gm/L). However, the C-reactive protein value fell within the normal range. The remaining laboratory investigations, including blood, urine cultures, and HIV screening, tuberculosis acid-fast bacilli (TB AFB) staining of sputum samples, and Mycobacterium tuberculosis Polymerase chain reaction (PCR) using GeneXpert platform, all returned negative results, and the results of other components of the laboratory work-up were within normal ranges.
The abdominal and pelvic computed tomography (CT) with intravenous contrast revealed a heterogeneous enhancement of the soft tissue in the left anterior abdominal wall, specifically involving the left rectus abdominis muscle at the level of the umbilicus. The dimensions of this thickening were approximately 5.1 cm × 2.6 cm (transverse × anteroposterior). Additionally, fat stranding was observed, which appeared to be separated from the anterior surface of the transverse colon. There was mild circumferential mural thickening in the distal one-third of the transverse colon, accompanied by pericolonic fat stranding. Multiple prominent lymph nodes were visualized adjacent to the transverse colon, with the largest lymph node measuring 1.1 cm × 0.7 cm. Subsequently, colonoscopy was unremarkable.
Preoperative SARS-CoV-2 RNA was detected by PCR on the nasopharyngeal swab, but with all precautionary measures, patient underwent surgical intervention. An exploratory laparotomy was performed, revealing intraoperatively that a portion of the transverse colon and the root of the omentum were adherent to the anterior abdominal wall just adjacent to the abdominal wall mass. Furthermore, the mass was found to be attached to the omentum (Figure 1). It was separated by sharp and blunt dissection, and purulent discharge was noted coming from the posterior abdominal wall. The cavity was opened from the inside, and the loculi were broken. A large cavity was found containing purulent fluid and necrotic debris. Approximately 2–3 inches of the transverse colon segment, which had adhered to the abdominal wall, was resected, and a primary anastomosis was performed. With suspicion of the abdominal wall sarcoma, the resected mass was sent for histopathological examination. Postoperatively, the patient was transferred to the COVID-19 intensive care unit and was started on intravenous antibiotics (Imipenem and Cilastatin 1 gram thrice a day for 10 days). She was discharged on the 11th postoperative day and was scheduled for a follow-up after 1 week.
Figure 1.

(a) A mass originating from the anterior abdominal wall and (b) an attached mass with omentum after its resection from the anterior abdominal wall.
The histopathologic examination of the abdominal wall mass revealed multiple fibro-fatty tissue pieces. Microscopic evaluation of the colon segment exhibited intact colonic mucosa with preserved crypt architecture, accompanied by moderate chronic inflammation in the lamina propria, characterized by lymphoplasmacytic cells. Sections taken from the surrounding fat of the colon and abdominal wall demonstrated the presence of micro abscesses composed of neutrophilic sheets mixed with lymphoplasmacytic cells, surrounded by histocytes and multinucleated giant cells. Additionally, evidence of fat necrosis was observed. Further analysis revealed characteristic colonies of Actinomyces within the abscesses present in multiple sections from the colon, abdominal wall, and adipose tissue (Figure 2). Crucially, acid-fast staining for Mycobacterium tuberculosis (MTB AFB) was performed and found to be negative. Based on these findings, the histopathologist concluded that the specimen indicated actinomycosis involving the colon pericolic adipose tissue and abdominal wall, with no evidence of malignancy; however, the specific Actinomyces species was not specified in the provided histopathological report.
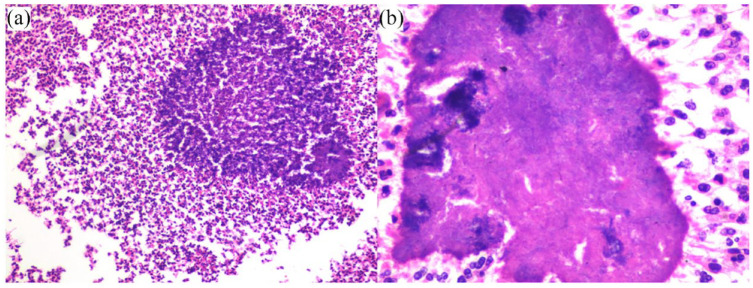
Figure 2.
(a) Low power view actinomycosis surrounded by dense inflammation on H&E stain (100×) and (b) high power view of actinomycosis surrounded by dense inflammation on H&E stain (400×).
Following the diagnosis, the patient’s treatment plan was adjusted accordingly. She was initiated on intravenous Penicillin G, administered at a dosage of 1.2 million units every 6 h for 14 days. Subsequently, she transitioned to oral Augmentin (amoxicillin and clavulanic acid) for 3 months. The patient is currently under close follow-up for 1 year, displaying no symptoms and demonstrating an improved condition.
Discussion
Actinomycosis is an uncommon, chronic suppurative infectious disease caused by Actinomyces species of which the most prevalent type which causes disease in humans is A. israelii, a gram-positive microaerophilic and anaerobic bacterium. This condition manifests with characteristic colonies distinguished by sulphur granules. 12 Actinomyces encompass six subgroups, among which A. israelii is the most prevalent, typically residing as normal flora in the oral cavity without causing disease under normal circumstances. However, infection occurs when the bacteria breach the mucosal barrier and invade the surrounding tissues. 12
Cervicofacial actinomycosis can sometimes develop following dental extractions, while the thoracic type is associated with pulmonary infections. Abdominopelvic actinomycosis is believed to occur after the disruption of mucous membranes in various conditions, often affecting patients who have undergone previous surgeries.13–15 The appendix and colon are the most commonly affected abdominal organs, although anterior abdominal wall involvement is rare.13,16 Notably, an increased incidence of abdominopelvic actinomycosis has been observed in patients with IUCDs. 17 IUCDs have been linked to pelvic actinomycosis infection, as they can lead to a foreign body reaction and concomitant pelvic infection in some patients. However, the precise mechanism behind their association with infection in intra-abdominal organs remains unclear. It is hypothesized that the IUCD may traumatize the cervical and uterine mucosa, facilitating the dissemination of infection. Furthermore, over time, the disintegration of the device could cause the distribution of small calcified fragments throughout the genital tract, acting as a nidus for Actinomycete collection. 18
In advanced stages of the disease, fistulation frequently occurs, indicating the bacteria’s aggressive tendency to invade adjacent tissue, while the mucosa largely remains unaffected in many cases. Hematogenous dissemination of the infection is rare, and lymphatic spread is notably absent. 19 The incidence of actinomycosis increases with IUCD use, with an average duration of 8 years. 20 This observation underscores the importance of long-term follow-up and regular evaluation for individuals using IUCDs. However, the presence of an IUCD alone does not necessarily imply the development of actinomycosis, as other factors may contribute to its occurrence.
Clinical presentations of abdominopelvic actinomycosis include low-grade pyrexia, vague abdominal pain, nausea, vomiting, and an abdominal mass or fistula. 4 Imaging techniques such as CT scans or ultrasounds can identify the presence of a mass, but they lack distinctive diagnostic features. However, detecting an infiltrative mass on abdominal CT scans should raise suspicions of actinomycosis, particularly in patients with mild constitutional symptoms. 21 CT-guided aspiration, with or without a core biopsy of suspicious lesions, can aid in the diagnosis. 22 The gynaecological differential diagnosis of abdominal actinomycosis presenting as an abdominal mass includes conditions such as pelvic inflammatory disease, tubo-ovarian abscesses and ovarian malignancy while non-gynaecological diseases that may be confused with abdominal actinomycosis includes appendicitis, diverticulitis, inflammatory bowel disease, tuberculosis, or malignancies affecting the colon or abdominal musculature.20,23 In this case, the mass’s involvement of the transverse colon raised suspicion of malignancy.
Surgical intervention becomes necessary when there is an abdominal abscess, sinuses, intestinal obstruction, or an abdominal mass. However, in patients without an abdominal emergency, preoperative diagnosis aided by aspiration or biopsy of lesions can help avoid unnecessary surgical resection and potential complications. Nevertheless, antibiotic treatment is essential for all patients diagnosed with actinomycosis infection. The antibiotic of choice for actinomycosis is Penicillin G, administered at high doses ranging from 18 to 24 million units per day. 24 In cases where a penicillin allergy exists, alternative treatments such as tetracycline, clindamycin, or doxycycline can be used. Prolonged treatment with amoxicillin and penicillin is often necessary for 6 to 12 months in the case of abdominal actinomycosis. 20
The confirmation of diagnosis involves the microbiological examination of pus, sinus drainage, or tissue biopsy. 20 Gram staining of the specimens reveals the typical filamentous branching of gram-positive rods. Due to the rarity of the disease and nonspecific findings, the preoperative suspicion of actinomycosis is often lacking, and definitive diagnosis is typically made through histopathological examination, observing the presence of sulphur granules in the resected specimen or by positive cultures of the organism. Extended courses of high-dose penicillin are required for complete eradication of the organism, followed by oral antibiotics for an extended period. In this particular case, the significant finding was the previously unnoticed IUCD, which had been retained for 21 years before its recent removal. This discovery emphasizes the importance of considering abdominal actinomycosis infection in the differential diagnosis when a patient presents with abdominal pain, mass, and fever, particularly in those with a prolonged history of IUCD use.
Conclusion
In conclusion, this case report highlights abdominopelvic actinomycosis as a rare but important consideration in patients with a history of IUCD use. The disease can present with nonspecific symptoms and imaging findings, making it challenging to diagnose preoperatively. Surgical intervention may be necessary in advanced cases, while antibiotic therapy with high-dose penicillin remains the mainstay of treatment. Timely recognition and appropriate management are crucial to ensure favourable outcomes. Increased awareness among healthcare professionals regarding this condition can aid in early diagnosis and prevent unnecessary interventions.
Acknowledgments
Not applicable.
Footnotes
Author’s contribution: Conception and design: SMFZ and SA. Acquisition of data: SA and RS. Drafting of the manuscript: SMFZ and BSR. Critical revision for important intellectual content: NAK and BSR. Final approval of the study: SA, SMFZ, RS, NAK, and BSR.
Availability of data and materials: Not applicable.
Consent for publication: Written informed consent was obtained for publication from the patient.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics approval: Our institution does not require ethical approval for reporting individual cases or case series.
Informed consent: Written informed consent was obtained from the patient(s) for their anonymized information to be published in this article.
ORCID iD: Burhanuddin Sohail Rangwala  https://orcid.org/0009-0008-5812-9049
https://orcid.org/0009-0008-5812-9049
References
- 1. Montori G, Allegri A, Merigo G, et al. Intra-abdominal actinomycosis, the great mime: case report and literature review. Emerg Med Heal Care 2015; 3(1): 2. [Google Scholar]
- 2. Boyanova L, Kolarov R, Mateva L, et al. Actinomycosis: a frequently forgotten disease. Future Microbiol 2015; 10(4): 613–628. [DOI] [PubMed] [Google Scholar]
- 3. Raymond A, Smego J, Foglia G. Actinomycosis. Clin Infect Dis 1998; 26(6): 1255–1263. [DOI] [PubMed] [Google Scholar]
- 4. Carkman S, Ozben V, Durak H, et al. Isolated abdominal wall actinomycosis associated with an intrauterine contraceptive device: a case report and review of the relevant literature. Case Rep Med 2010; 2010: 340109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Polat I, Gungorduk K, Polat G, et al. Persistent subumbilical discharge associated with actinomycosis caused by intrauterine contraceptive device: a case report. Arch Gynecol Obstet 2008; 277(5): 457–460. [DOI] [PubMed] [Google Scholar]
- 6. Çöl C, Çöl M, Albayrak L. A case report of abdominal wall actinomycosis associated with prolonged use of an intrauterine device. Antimic Infect Dis Newslet 2000; 18(10): 77–79. [Google Scholar]
- 7. Groot G, Rivers L, Smith T, et al. Abdominal wall actinomycosis associated with use of an intrauterine device: a case report. Can J Surg 1991; 34(5): 450–453. [PubMed] [Google Scholar]
- 8. Adachi A, Kleiner GJ, Bezahler GH, et al. Abdominal wall actinomycosis associated with an IUD. A case report. J Reprod Med 1985; 30(2): 145–148. [PubMed] [Google Scholar]
- 9. Lunca S, Bouras G, Romedea NS, et al. Abdominal wall actinomycosis associated with prolonged use of an intrauterine device: a case report and review of the literature. Int Surg 2005; 90(4): 236–240. [PubMed] [Google Scholar]
- 10. Adachi A, Kleiner GJ, Bezahler GH, et al. Abdominal wall actinomycosis associated with an IUD. A case report. J Reprod Med 1985; 30(2): 145–148. [PubMed] [Google Scholar]
- 11. Jones J. Carnett sign: radiology reference article. Radiopaedia.org, https://radiopaedia.org/articles/carnett-sign?lang=us (2021, accessed 20 October 2023). [Google Scholar]
- 12. McFarlane ME, Coard KC. Actinomycosis of the colon with invasion of the abdominal wall: an uncommon presentation of a colonic tumour. Int J Surg Case Rep 2010; 1(1): 9–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Garner JP, Macdonald M, Kumar PK. Abdominal actinomycosis. Int J Surg 2007; 5(6): 441–448. [DOI] [PubMed] [Google Scholar]
- 14. Cintron JR, Del Pino A, Duarte B, et al. Abdominal actinomycosis: report of two cases and review of the literature. Dis Colon Rectum 1996; 39: 105–108. [DOI] [PubMed] [Google Scholar]
- 15. Könönen E, Wade WG. Actinomyces and related organisms in human infections. Clin Microbiol Rev 2015; 28(2): 419–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lau WY, Boey J, Fan ST, et al. Primary actinomycosis of the abdominal wall. ANZ J Sur 1986; 56: 873–875. [DOI] [PubMed] [Google Scholar]
- 17. Henderson SR. Pelvic actinomycosis associated with an intrauterine device. Obstet Gynecol 1973; 41(5): 726–732. [PubMed] [Google Scholar]
- 18. Santa MC, Buschmann BO, Daniel SJ. Actinomyces infection associated with intra-uterine device. J Med Assoc State Ala 1978; 47(11): 31–33. [PubMed] [Google Scholar]
- 19. Wagenlehner FM, Mohren B, Naber KG, et al. Abdominal actinomycosis. Clin Microbiol Infect 2003; 9(8): 881–885. [DOI] [PubMed] [Google Scholar]
- 20. Duguid HL. Actinomycosis and IUDs. IPPF Med Bull 1983; 17(3): 1–2. [PubMed] [Google Scholar]
- 21. Ha HK, Lee HJ, Kim H, et al. Abdominal actinomycosis: CT findings in 10 patients. AJR Am J Roentgenol 1993; 161(4): 791–794. [DOI] [PubMed] [Google Scholar]
- 22. Pombo F, Rodriguez E, Martin R, et al. CT-guided core-needle biopsy in omental pathology. Acta Radiol 1997; 38(6): 978–981. [DOI] [PubMed] [Google Scholar]
- 23. Shin D, Hwang J, Hong SS, et al. Pelvic actinomycosis mimicking malignancy of the uterus: a case report. Investig Magn Reson Imaging 2019; 23(2): 136–141. [Google Scholar]
- 24. Valour F, Sénéchal A, Dupieux C, et al. Actinomycosis: etiology, clinical features, diagnosis, treatment, and management. Infect Drug Resist 2014: 183–197. [DOI] [PMC free article] [PubMed] [Google Scholar]