Abstract
Background: Intraoral adenoid cystic carcinoma (ACC) arising from minor salivary glands (MSG) is a rare malignancy associated with delayed diagnosis and unfavorable outcomes. This study aimed to comprehensively review ACC of MSGs, focusing on clinical characteristics, imaging modalities, treatment approaches, and long-term outcomes. Methods: A systematic search was conducted in PubMed, Web of Science, and MEDLINE databases to identify relevant articles reporting cases of ACC of MSGs between January 1997 and March 2023. The study was registered in PROSPERO (ID: CRD42023449478). A total of 10 studies that met the inclusion criteria were selected for critical review. In total, 902 patients were diagnosed with ACC of MSGs with an age range of 44.3 to 63 years, and an average age of 56.6 years. The female to male ratio ranges from 1:1 to 2.4:1. Regarding the primary site of ACC, the palate was the most common location, accounting for 30.5% to 83.3%, followed by the buccal mucosa, floor of the mouth, and lip and the retromolar area. For histology, the solid mass pattern was the most prevalent, seen in 95.2% of patients, followed by the cribriform pattern. Regarding treatment modalities, surgery was the most common approach, applied in 76.3% of cases, with a combination of surgery and radiotherapy used in 29.0% of cases. A smaller fraction, 3.2%, received a combination of surgery, chemotherapy, and radiotherapy, and 8.3% underwent radiotherapy alone. Local recurrence rates varied between 1% and 28.5%, and distant metastasis occurred in 18.2% to 33.3% of cases, predominantly to lymph nodes (14.5%). An analysis of overall survival across various stages and patient numbers indicated a 5-year survival rate of 68.0%. The findings of this study provide valuable insights for physicians in making treatment decisions and emphasize the need for ongoing research and collaborative clinical efforts to improve the management and outcomes of this challenging disease. Conclusion: ACC of MSGs is a multifaceted condition typically manifesting as asymptomatic enlargement and ulceration. This disease is marked by distinct histopathological patterns and perineural invasion (PNI). Recognizing these distinctive aspects is key in shaping the treatment plan, which can range from surgical procedures to radiation therapy, chemotherapy, and evolving targeted treatments. Continuous research and collaborative clinical efforts remain critical for ongoing progress in the treatment and management of this challenging condition.
Keywords: adenoid cystic carcinoma, minor salivary glands, head and neck tumor, chemotherapy and radiotherapy of the head and neck
1. Introduction
Adenoid cystic carcinoma was first described by Billroth in 1859 and characterized by its unique combination of connective and epithelial tissue. ACC is known for its slow progression, local recurrence, and regional and systemic metastasis [1]. ACC represents approximately 1% of all head and neck cancers and 10% of salivary gland tumors. ACC arising from minor salivary glands is rare, comprising only 10–20% of all ACC cases, and it exhibits a high propensity for PNI, contributing to its spread [2].
ACC primarily affects individuals aged 40 to 60 years, with a slight female predominance [3,4]. The most common sites within the oral cavity include the palate, tongue, and floor of the mouth, with additional occurrences in the lips, buccal mucosa, retromolar trigone, and tonsillar area [4,5,6].
The exact etiology of ACC remains unknown. However, recent studies have shed light on molecular abnormalities associated with ACC development and progression. The most common genetic abnormalities involve translocations of the myeloblastosis (MYB) gene on chromosome 6q and the Nuclear factor 1 B (NFIB) gene on chromosome 9p. These translocations result in the overexpression of MYB and NFIB, which play crucial roles in cell growth, differentiation, and survival regulation [7,8].
ACC arising from minor salivary glands typically presents as a painless, slow-growing mass. Patients may also experience numbness or tingling in the affected area due to perineural invasion, which is a characteristic feature of ACC. Clinical presentation may resemble other salivary gland tumors, such as pleomorphic adenoma and mucoepidermoid carcinoma, making biopsy essential for accurate diagnosis [9,10].
Histological examination of a biopsy specimen is necessary for the definitive diagnosis of ACC. The typical histological features of ACC include a cribriform or tubular pattern, with hyaline or basophilic material within the cribriform spaces. ACC comprises two distinct cell types: ductal and myoepithelial cells. Immunohistochemical stains, such as S100 and smooth muscle actin, aid in identifying these cell types and differentiating ACC from other salivary gland tumors [11,12,13]. Differential diagnosis includes benign and malignant tumors, such as pleomorphic adenoma, polymorphic adenocarcinoma, and mucoepidermoid carcinoma.
There is no universally recommended treatment for ACC, highlighting the need for personalized treatment plans based on clinical and histological factors to achieve optimal outcomes. Treatment approaches are typically multidisciplinary and may involve surgery, radiotherapy, chemotherapy, or various combinations thereof. Combined therapies, such as surgery with radiotherapy or radiotherapy with chemotherapy, are often favored [14,15,16]. The prognosis for ACC arising from minor salivary glands is generally poor, with a 5-year survival rate of 50–60%. Prognosis is influenced by factors such as tumor location, size, PNI, and histological grade. Previous reports indicated that ACC with a solid pattern carries a worse prognosis compared to the cribriform pattern, and high-grade transformation is associated with poorer outcomes [17,18].
Due to the rarity of ACC, single studies often lack the comprehensive data needed for definitive findings. The infrequency of ACC cases contributes to the limitations of individual studies, emphasizing the importance of an exhaustive review that amalgamates data from various studies. Additionally, ACC is characterized by a diverse range of clinical symptoms and treatment strategies, coupled with an absence of consensus on certain aspects of its management and clinical presentation. Consequently, a systematic review (SR) and meta-analysis (MA) can methodically compile and scrutinize these diverse elements, enhancing our understanding of ACC’s clinical manifestations. Such reviews not only provide a deeper insight into the disease but also establish a consolidated resource for future research, and identify areas that warrant further exploration; thus, the objectives of this study were to evaluate the epidemiological aspects of ACC arising from minor salivary glands, explore different therapeutic options, and assess survival rates among patients with this tumor.
2. Materials and Methods
2.1. Protocol and Registration
The protocol was developed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis Protocols (PRISMA-P) [19] and registered in PROSPERO (ID: CRD42023449478).
2.2. Information Sources and Search Strategy
A comprehensive literature search was conducted to identify relevant studies using various databases, including PubMed/MEDLINE, EMBASE, Cochrane databases, Scopus, Web of Science, and Google Scholar. These were used to identify studies published in the English language between January 1997 and March 2023. Additionally, a manual search of reference lists from retrieved articles and relevant journals was performed. Medical Subject Headings (MeSH) were employed, including “Adenoid cystic carcinoma” OR “Minor salivary gland tumor” and “Clinical manifestation” OR “Characteristics” OR “Symptoms” OR “Head and neck radiotherapy” OR “Chemotherapy” OR “Surgery.” In this systematic review, the PICO encompassed Population (male/female patients), Interventions (surgery, radiotherapy, chemotherapy), Comparisons between different treatment modalities, and Outcomes of interest (prevalence of ACC of MSGs, recurrence, metastasis).
Based on the detailed search strategy and PICO framework outlined, the specific research question for this systematic review was: “How do clinical characteristics and different treatment modalities (surgery, radiotherapy, chemotherapy) compare in terms of effectiveness and outcomes (prevalence of ACC, recurrence, metastasis) in both male and female patients diagnosed with ACC of MSGs?”
2.3. Eligibility Criteria
2.3.1. Inclusion Criteria
Studies needed to be available as full-text articles and only in the English language. Moreover, selection was categorized on original studies including retrospective studies, prospective studies, studies containing at least one clinically diagnosed case of ACC of minor salivary glands, studies with a follow-up period of more than 12 months, and studies evaluating the treatment and patient survival.
2.3.2. Exclusion Criteria
Exclusion criteria included non-English articles, non-original articles, duplicate publications (risk of bias), articles without complete demographic information of each patient, editorial letters, case reports, review articles, and studies with a follow-up lower than 12 months.
2.4. Data Extraction
Studies were initially selected based on the title and abstract information. Next, the selected articles were read in full text to check for their eligibility. A list of excluded studies was maintained to avoid selection bias between two of the authors (M.H. and E.A.) who reviewed independently. In the case of disagreement between the authors, a consensus was attained. Data extracted included author(s) and year of publication, studied population, sample size, age range of the sample, and study design; gender: the patient’s gender was determined in terms of percentage and ratio, intraoral site of the tumor; histological features: dividing it into cribriform, tubular, and solid type, and linked to the outcome; therapy: the therapeutic approaches used on different patients were analyzed, classified into either surgery or surgery combined with radiation therapy, surgery combined with radiotherapy and chemotherapy, radiation therapy, or chemotherapy; survival analysis: perineural; metastasis: local and/or distant metastasis.
2.5. Methodological Assessment of Study Quality
The recommended Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) [20] checklist was used to assess the quality in all identified and collected full-text articles included in this study (Table 1). The quality of the included studies was assessed independently by two authors (M.H. and E.A.).
Table 1.
Strobe Quality Assessment.
| Author/ Year |
Title/ Abstract |
Background | Objectives | Study Design |
Setting | Participants | Variables | Data/ Sources |
Bias | Study Size |
Quantitative Variables |
Statistical Method |
Descriptive Data |
Outcome Data |
Main Results |
Other Analysis |
Key Results |
Limitations | Interpretation | Generalizability | Funding |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bardwil et al. 1966 [21] |
Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes |
| Charles et al. 1988 [22] |
Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes |
| Kusama et al. 1997 [23] |
Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes |
| Jansisyanont et al. 2002 [24] |
Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes |
| Hyam et al. 2004 [25] |
Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes |
| Ito et al. 2005 [26] |
Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes |
| Jaber 2006 [27] |
Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes |
| Buchner et al. 2007 [28] |
Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes |
| Tian et al. 2010 [29] |
Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes |
| Triantafillidou et al. 2006 [30] |
Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes |
Twenty-two checklist criteria were selected, and the collected studies were classified into three categories: studies presenting 19 out of 22 criteria were selected as having a low risk of bias, 18–15 criteria were considered as having a moderate risk of bias, and studies which had less than 15 criteria were selected as having a high risk of bias.
The value of weighted kappa statistic between author agreements was 87%. After confirming the quality of each study, two authors independently extracted the data from each selected study. Disagreements were resolved by discussion and by a third person (M.J.) if the two reviewers could not reach a consensus.
2.6. Certainty of the Level of Evidence
The GRADE tool (Grading of Recommendations, Assessment, Development, and Evaluation) [31] was used to assess the quality of a body of evidence. The quality of evidence was rated per outcome into one of four categories (high, moderate, low, and very low) (Table 2).
Table 2.
Certainty of the level of evidence.
| Author/Year | Limitation | Inconsistency | Indirectness | Imprecision | Publication Bias | Overall Level of Evidence |
|---|---|---|---|---|---|---|
| Bardwil et al. 1966 [21] | No serious limitation | No serious inconsistency | No serious indirectness | No serious imprecision | No serious publication bias | High |
| Charles et al. 1988 [22] | No serious limitation | No serious inconsistency | No serious indirectness | No serious imprecision | No serious publication bias | High |
| Kusama et al. 1997 [23] | No serious limitation | No serious inconsistency | No serious indirectness | No serious imprecision | No serious publication Bias | High |
| Jansisyanont et al. 2002 [24] | No serious limitation | No serious inconsistency | No serious indirectness | No serious imprecision | No serious publication bias | High |
| Hyam et al. 2004 [25] | No serious limitation | No serious inconsistency | No serious indirectness | No serious imprecision | No serious publication bias | High |
| Ito et al. 2005 [26] | No serious limitation | No serious inconsistency | No serious indirectness | No serious imprecision | No serious publication bias | High |
| Jaber 2006 [27] | No serious limitation | No serious inconsistency | No serious indirectness | No serious imprecision | No serious publication bias | High |
| Buchner et al. 2007 [28] | No serious limitation | No serious inconsistency | No serious indirectness | No serious imprecision | No serious publication bias | High |
| Tian et al. 2010 [29] | No serious limitation | No serious inconsistency | No serious indirectness | No serious imprecision | No serious publication bias | High |
| Triantafillidou et al. 2006 [30] | No serious limitation | No serious inconsistency | No serious indirectness | No serious imprecision | No serious publication bias | High |
2.7. Risk of Bias (RoB) Assessments
Studies that met the inclusion criteria were assessed using The Joanna Briggs Institute Critical Appraisal tools for JBI Systematic Reviews [32]. The tool focuses on method selection, sufficient demographics, presentation, diagnosis, and proper intervention. Studies scoring 4 were deemed as having a “high quality”, scoring 3 was “moderate quality”, and scores of ≤2 were “poor quality”.
2.8. Data Analysis
Data analysis was performed using the comprehensive meta-analysis software, version 4, (CMA-V4). Pooled prevalence and 95% confidence intervals (CI) were estimated using the random-effects model. Heterogeneity among studies was assessed using Cochran’s Q statistics, I-squared statistic, and the tau square (T2) test. Sensitivity analysis was conducted by removing one study at a time to evaluate its impact on the overall results. Heterogeneity among the included studies was assessed using the chi-squared test and the I-squared statistic. A funnel plot was used to assess potential publication bias, with a symmetrical distribution indicating no significant bias.
3. Results
3.1. Search of Literature
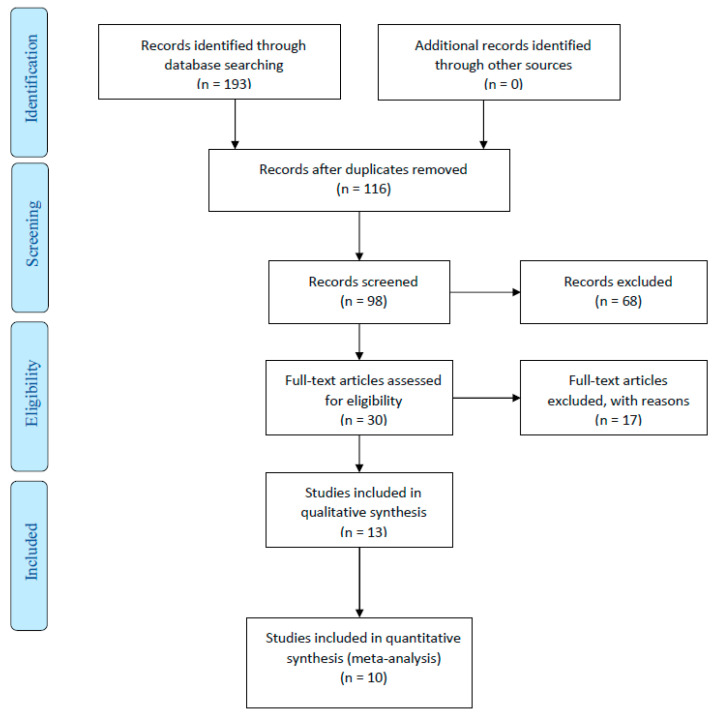
The search strategy yielded a total of 43 articles from all databases. Of the 43 articles, 13 were excluded after an examination of the titles and abstracts, and full-text articles of the remaining 30 studies were reviewed independently for eligibility. Of these 30 studies, 20 were excluded because they did not meet the inclusion criteria. Finally, a total of 10 studies met the inclusion criteria and were processed for critical review (Figure 1). The initial examiners’ average agreement (kappa score) on quality assessment was 0.83. The agreement reached 1.00 after discussion and consensus.
Figure 1.
PRISMA flow diagram.
3.2. Risk of Bias (RoB) Assessments
In the risk of bias assessments using JBI tools for Systematic Reviews, 8 studies were scored as high quality and 2 scored as moderate quality. Moderate scores were due to a lack of data on some criteria (Table 3).
Table 3.
Risk of Bias Assessment.
| Author/Year | 1. Were There Clear Criteria for Inclusion in the Case Series? | 2. Was the Condition Measured in a Standard, Reliable Way for All Participants Included in the Case Series? | 3. Were Valid Methods Used for Identification of the Condition for All Participants Included in the Case Series? | 4. Did the Case Series Have Consecutive Inclusion of Participants? | 5. Did the Case Series Have Complete Inclusion of Participants? | 6. Was There Clear Reporting of the Demographics of the Participants in the Study? | 7. Was There Clear Reporting of Clinical Information of the Participants? | 8.Were the Outcomes or Follow-Up Results of Cases Clearly Reported? | 9. Was There Clear Reporting of the Presenting Sites’/Clinics’ Demographic Information? | 10. Was Statistical Analysis Appropriate? | Quality Score |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Bardwil et al. 1966 [21] |
Yes | NA | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | High quality |
| Charles et al. 1988 [22] |
Yes | NA | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | High quality |
| Kusama et al. 1997 [23] |
Yes | NA | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | High quality |
| Jansisyanont et al. 2002 [24] |
Yes | NA | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | High quality |
| Hyam et al. 2004 [25] |
Yes | NA | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | High quality |
| Ito et al. 2005 [26] |
Yes | NA | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | High quality |
| Jaber 2006 [27] | Yes | NA | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | High quality |
| Buchner et al. 2007 [28] |
Yes | NA | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | High quality |
| Tian et al. 2010 [29] |
Yes | NA | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | High quality |
| Triantafillidou et al. 2006 [30] |
Yes | NA | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | High quality |
3.3. Study Characteristics
A total of 10 studies that met the inclusion criteria were selected for critical review [21,22,23,24,25,26,27,28,29,30]. The sample size was 902 cases, which were analyzed using descriptive statistics and evaluated based on variables such as frequency and proportions. In total, 902 patients were diagnosed with ACC with an age range of 44.3 [27] to 63 [24] years, and an average age of 56.6 years. Concerning gender, out of 902 patients studied, women were more affected, accounting for up to 56.6% of the patients. The female to male ratio ranges from 1:1 [25] to 2.4:1 [23]. Regarding the primary site of ACC, the palate was the most common location, accounting for 30.5% [29] to 83.3% [24], followed by the buccal mucosa, 4.1% [28] to 33.3% [25], floor of the mouth, 8.3% [28] to 35.2% [23], and lastly, lip and the retromolar area.
For histology, the solid mass pattern was the most prevalent, seen in 95.2% of patients, followed by the cribriform pattern in 4.8% of cases. Regarding treatment modalities, surgery was the most common approach, applied in 76.3% of cases, with a combination of surgery and radiotherapy used in 29.0% of cases (Table 4 and Table 5). A smaller fraction, 3.2%, received a combination of surgery, chemotherapy, and radiotherapy, and 8.3% underwent radiotherapy alone. In terms of disease control and survival among cases with available data, 79.2% demonstrated no evidence of disease. Local recurrence rates varied between 1% [23] and 28.5% [24], and distant metastasis occurred in 18.2% [30] to 33.3% [25] of cases, predominantly to lymph nodes (14.5%) [21]. An analysis of overall survival across various stages and patient numbers indicated a 5-year survival rate of 68.0% among 398 patients.
Table 4.
Characteristics of the included studies.
| Author/Year | Study Type | Country | No. of Cases | Mean Age | M/F Ratio | Clinical Feature Mass/Ulcer/Pain |
Main Location |
|---|---|---|---|---|---|---|---|
| Bardwil et al. 1966 [21] | Retrospective | USA | 48 | 48.5 years | - | No features (35.42%) Painless swelling (41.67%) No ulceration (22.92%) |
Hard palate (79.17%) Lip (20.83%) |
| Charles et al. 1988 [22] | Retrospective | USA | 40 | 57.7 ± 17.59 years | F/M ratio = 1.5/1 | Painless ulceration (87.5%) Swelling (12.5%) |
Hard palate (47.5%) Upper lip (5%) Buccal mucosa (17.5%) Floor of the mouth and retromolar (22.5%) |
| Kusama et al. 1997 [23] | Retrospective | Japan | 17 | 55.1 ± 15 years | F/M ratio = 2.4/1 | Painless swelling (100%) | Hard palate (41.18%) Retromolar (5.88%) Buccal mucosa (17.65%) Floor of the mouth (35.29%) |
| Jansisyanont et al. 2002 [24] | Retrospective | USA | 6 | 63 years | F/M ratio = 1.9/1 | Painless swelling (100%) | Hard palate (83.3%) Upper lip (16.7%) |
| Hyam et al. 2004 [25] | Retrospective | Australia | 12 | 62 years | Male = 6 Female = 6 |
Pain and swelling (100%) | Hard palate (58.33%) Buccal mucosa (33.33%) Oropharynx (8.33%) |
| Ito et al. 2005 [26] | Retrospective | Brazil | 39 | 57 years | Male = 19 Female = 20 |
Not mentioned | Palate (67.5%) Other (7.7%) |
| Jaber 2006 [27] | Retrospective | Libya | 13 | 44.3 years | F/M ratio = 1/0.7 | Swelling (38.46%) Ulcer (30.77%) Pain (15.38%) Ill-fitting prosthesis (15.38%) |
Palate (38.46%) Tongue (23.08%) Other (38.46%) |
| Buchner et al. 2007 [28] | Retrospective | USA | 24 | 57 years | F/M ratio = 2:1 | Painless swelling (100%) | Hard palate (75%) Upper lip (8.3%) Floor of the mouth (8.3%) Buccal mucosa (4.17%) Retromolar region (4.17%) |
| Tian et al. 2010 [29] | Retrospective | China | 681 | 51.45 years | F/M ratio = 1.25/1 | Swelling (80–90%) | Hard palate (30.59%) Parotid (11.6%) Submandibular (10.87%) Others (46.84%) |
| Triantafillidou et al. 2006 [30] | Retrospective | Greece | 22 | 22–87 | 1.2:1 | Swelling (100%) | Palate (18%) Buccal mucosa (3%) Floor of the mouth (1%) |
Table 5.
Histology and treatment outcomes of ACC.
| Author/Year | Histological Pattern | Perineural Invasion | Treatment Received | Treatment Margins | Follow-Up Duration | Metastasis/ Recurrence |
Location of Metastasis |
|---|---|---|---|---|---|---|---|
| Bardwil et al. 1966 [21] | Not mentioned | Yes (45.83%) | 1. Surgical excision and en bloc resection (77.08%) 2. Excision followed by radiation (14.58%) 3. Radiation only (8.33%) |
90% negative 10% positive |
3 years | Distant metastasis (22.92%) Recurrence (20.83%) |
Lymph nodes (14.58%) Intracranial (8.33%) |
| Charles et al. 1988 [22] | Cribriform appearance (80%) Solid (5%) Tubular (15%) |
No | Not mentioned | Not mentioned | Not mentioned | No metastasis Recurrence not reported |
Not applicable |
| Kusama et al. 1997 [23] | Solid (100%) | No | Not mentioned | Not mentioned | 16 years | Local metastasis Recurrence (1%) |
Cervical lymph nodes |
| Jansisyanont et al. 2002 [24] | Not mentioned | No | Wide local excision (70.8%) Surgery + radiation + chemotherapy (18%) Chemotherapy and/or radiation (3.2%) Other (8%) |
100% negative | 7 years, 6 months | Distant metastasis Recurrence (28.57%) |
Cervical lymph nodes, lung, bone, and brain (16.67%) |
| Hyam et al. 2004 [25] | Solid mass | Yes (60%) | Surgery as the primary modality (33.33%) Patients with a positive surgical margin were recommended adjuvant radiotherapy (66.67%) |
47% positive surgical margin 10% close margin (<2 mm) negative |
5 years | Metastasis (33.3%) Recurrence (8.3%) |
Bone |
| Ito et al. 2005 [26] | Not mentioned | No | Surgical excision (100%) | 100% negative | 29 years | No metastasis Recurrence not reported |
Not applicable |
| Jaber 2006 [27] | Not mentioned | No | Surgery or radiotherapy alone or a combination of both |
Not mentioned | 7 years | No metastasis Recurrence (15.3%) |
Not applicable |
| Buchner et al. 2007 [28] | Solid mass | No | Not mentioned | Not mentioned | 20 years | Not mentioned Recurrence not reported |
Not applicable |
| Tian et al. 2010 [29] | Solid mass | No | Not mentioned | Not mentioned | 23 years | No metastasis Recurrence not reported |
Not applicable |
| Triantafillidou et al. 2006 [30] | Solid mass | Yes | Surgery as the primary modality (100%) Surgery + radiation, 17 patients |
Not mentioned | 21 years | Metastasis 4 cases (18.2%) Recurrence (9.1%) |
Lung (9.1%) Lymph nodes (9.1%) |
3.4. Meta-Analysis
A meta-analysis was conducted to summarize the findings of various studies investigating different aspects of ACC (Table 6). Ten studies were included in the analysis. The mean age of affected patients was 56.68 years (95% CI: 53.42–59.9 years), and there was a predominance of females. The most prevalent clinical feature of ACC was painless swelling (81.41%, 95% CI: 58.43% to 93.17%), followed by oral ulceration (14.9%). The most common sites of ACC were the hard palate (47.54%), buccal mucosa (24.05%), and tongue (22.18%), while the retromolar area had the lowest prevalence (10.7%). Heterogeneity among studies ranged from moderate to substantial (I2 values: 30.66% to 90.99%). The overall effects were significant for all features except the hard palate, indicating a significant association between clinical features and ACC. There was no significant publication bias based on Egger’s test (p-values: 0.0049 to 0.8864) in the included studies.
Table 6.
Meta-analysis of the selected studies.
| Demographical Characteristics | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Age (mean in years) |
|||||||||
| Female | 10 | 56.68 | 53.42–59.9 | 9 | 5.13 | 0 | 0 | <0.001 | 0.0677 |
| Clinical features | |||||||||
| Painless swelling | 10 | 81.41 | 58.43–93.17 | 9 | 99.95 | 90.99 | 2.333 | <0.001 | 0.8864 |
| Ulceration | 10 | 14.9 | 0.6–3.22 | 9 | 63.67 | 85.86 | 1.63 | 0.0262 | 0.7274 |
| Hard palate | 10 | 47.54 | 32.98–62.53 | 9 | 64.19 | 85.98 | 0.73 | 0.0921 | 0.0921 |
| Lip | 7 | 16.97 | 11.73–23.91 | 6 | 10.96 | 45.24 | 0.12 | 0.0897 | 0.5506 |
| Buccal mucosa | 9 | 24.05 | 16.21–34.13 | 8 | 25.39 | 68.49 | 0.30 | 0.0013 | 0.0049 |
| Floor of mouth | 8 | 17.82 | 10.81–27.94 | 7 | 23.35 | 70.02 | 0.39 | 0.0015 | 0.4604 |
| Retromolar | 3 | 10.7 | 0.04–24.99 | 2 | 2.88 | 30.66 | 0.29 | 0.2364 | 0.0997 |
| Tongue | 5 | 22.18 | 7.2–51.15 | 4 | 18.57 | 78.46 | 1.46 | 0.0009 | 0.6772 |
Q Cochran’s Q statistic for heterogeneity. I2 index for the degree of heterogeneity. T2 tau-squared measure of heterogeneity.
4. Discussion
ACC is a rare malignancy with limited available data on treatment and survival outcomes. The objective of this systematic review was to provide a comprehensive understanding of ACC in minor salivary glands and its clinical features, treatment patterns, and survival outcomes. The findings of this study contribute to the existing literature by synthesizing the available evidence and highlighting key aspects of ACC management. The prevalence of ACC varies across different geographical regions, and in some studies, it was identified as the most common malignant tumor in certain areas. For example, a study from Southern Poland highlighted ACC as a leading malignant salivary gland tumor in the region [33]. Contrary to the findings in some European centers, the WHO designates mucoepidermoid carcinoma as the most common malignant salivary gland tumor [34]. This discrepancy might stem from variations in demographic factors.
The average age of patients in this study aligns with previous reports, indicating that ACC commonly affects individuals in their late forties [35,36,37,38,39,40,41]. The extended time span between symptom onset and diagnosis observed in this study aligns with most case series, although it differs from a few reports [35,42,43]. This discrepancy could be attributed to the slow-growing nature of ACC and its manifestation through nonspecific signs.
The gender distribution of ACC in minor salivary glands shows a female predominance; female to male ratios vary across different studies, such as 2.4:1 in Kusama et al. [23] and 2:1 in Buchner et al. [28]. This is consistent with recent literature, where some studies have reported a higher incidence in women, although the reason for this gender bias remains unclear [44].
The current review encompassed data from different countries like the USA, Japan, Australia, Brazil, Libya, China, and Greece. Such variations may hint at regional differences in etiology, such as genetic factors, environmental exposures, or lifestyle choices. A review by Coca-Pelaz et al. [1] highlighted the importance of understanding regional variations in the presentation of ACC.
In the current review, the most common clinical feature of intraoral ACC is painless swelling. This symptom aligns with the findings in contemporary literature, where painless masses have been reported as a common initial sign [45,46,47,48,49,50,51,52]. The underlying pathophysiology, although not entirely clear, may be attributed to the slow-growing nature of the tumor. Ulceration is also a notable clinical feature in the present study. Ouyang et al. [22] reported painless ulceration in 3.5% of the cases. This may be a sign of the local aggressiveness of the tumor or associated with advanced-stage disease [53]. It is important to note that variations in symptom reporting may be due to the small sample sizes of previous studies, highlighting the need for larger-scale investigations. Some studies have noted the occurrence of pain, despite ACC being predominantly a painless swelling. Pain and other neurological symptoms might be linked to PNI, a characteristic feature of ACC. Hyam et al. [25] reported PNI in 60% of cases. This pattern supports findings in the broader literature, highlighting the complex nature of pain in ACC [54].
The location of ACC in minor salivary glands varies, with a strong predilection for the hard palate. The studies included in the review show palatal involvement with a range from 30.59% in Tian et al. [29] to 79.17% in Bardwil et al. [21]. Other locations include the buccal mucosa, floor of the mouth, and upper lip. The varied distribution may be reflective of the widespread distribution of minor salivary glands [55].
There are three main histopathological patterns for ACC: cribriform, tubular, and solid. All these subtypes can be identified based on the dominant shape and arrangement of the epithelial secreting cells, the myoepithelial cells, and the extracellular matrix. Histologically, a tumor is classified as the solid subtype when this pattern comprises over 30% of the tumor [56]. A study analyzing 87 cases of ACC found the cribriform pattern to be the most prevalent, with the solid form being the rarest [57]. These patterns were used to assess the clinicopathological and prognostic attributes of each subtype. It was observed that the solid subtype had the least differentiated cells, denser extracellular stroma, and was highly locally aggressive, showing the greatest frequency of PNI and the poorest prognosis. Contrarily, Belulescu et al. reported that 46% of their cases showed the solid pattern, challenging the previously observed rarity of this subtype [58]. Such discrepancies might be due to factors like study sample, methodology, and population demographics. Another significant histological feature in ACC is PNI, which has been closely associated with distant metastasis and adverse disease outcomes [59,60]. Additionally, studies focusing on immunohistochemistry labeling have indicated that in ACC, the proliferation and differentiation of myoepithelial cells significantly contribute to the progression of carcinogenesis, more so than the epithelial/secreting cells [61].
PNI is a hallmark feature of ACC, occurring in up to 80% of cases [62]. It is a phenomenon where cancer cells invade the surrounding nerves, leading to a more complex clinical presentation. PNI in ACC has been linked with local recurrence, distant metastasis, and reduced overall survival [63]. The presence of PNI may necessitate more aggressive treatment approaches and has been considered as a predictor of disease progression and unfavorable outcomes [64].
Treatment for ACC is multifaceted, encompassing surgery, radiation therapy, and chemotherapy, tailored to the specific histological pattern and presence or absence of PNI. However, surgical intervention remains the principal method for addressing ACCs that originate from both major and minor salivary glands in the head and neck region. In a systematic review, Ran and coworkers [65] examined current treatment strategies for ACC and reported that surgery alone was the primary treatment for over 40% of cases. Combined surgery and postoperative radiotherapy were used in 35% of cases, while standalone radiotherapy was administered in 19%. This study specifically focused on evaluating the efficacy of the two predominant treatment modalities: surgery only and surgery supplemented with postoperative radiotherapy. The findings indicated superior 5-year and 10-year survival rates for the combination of surgery and postoperative radiotherapy, with respective survival rates of 97.3% and 44.4%, compared to 86.4% and 55.6% for surgery alone. Furthermore, another systematic review explored the role of elective neck dissection in conjunction with surgery in managing ACC. This review revealed that patients who underwent surgery combined with elective neck dissection experienced longer periods without metastasis. However, it was advised that elective neck dissection should be restricted to the first three levels of the lymph nodes to optimize outcomes [66]. Additionally, Su and Yang [67] in a systematic review addressed the outcomes of surgical intervention for ACC metastases in the lungs, underscoring that the surgical excision of metastatic lesions can impede disease progression and enhance overall survival. The success of this approach, however, is contingent on various factors, including the patient’s lung health, the size of the metastases, and the patient’s overall physical condition. Radiotherapy as a standalone treatment is rarely employed for ACC due to its limited effectiveness. It is typically reserved for advanced and inoperable cases of ACC [68]. In contrast, the application of postoperative radiotherapy in conjunction with surgery is acknowledged as a beneficial approach and has gained widespread acceptance in ACC management [69]. Notably, studies have shown that patients who did not receive postoperative radiotherapy were 13 times more susceptible to local recurrence compared to those who underwent the treatment [70]. Chemotherapy as a standalone intervention has shown limited efficacy in the treatment of ACC. This has been evidenced through a range of clinical trials that have assessed various chemical compounds for their potential as systemic therapies. This situation underscores the critical necessity for more comprehensive research in the clinical, pathological, and genetic domains. Such research endeavors are pivotal for a deeper understanding of the processes involved in the carcinogenesis and pathogenesis of ACC. They are also crucial in the quest to discover and develop innovative therapeutic approaches that directly address the root causes and mechanisms of this form of cancer.
The effectiveness of systemic molecular treatments in advanced ACC has been documented. Initial trials using multi-kinase inhibitors like sunitinib did not demonstrate significant response rates, although most patients experienced disease stability and moderate toxicity [71]. When mTOR was targeted, neither complete nor partial responses were seen, but the median time before disease progression was 11.2 months, and tumor reduction was noted in 44% of the patients [72]. Furthermore, the use of the multi-kinase inhibitor lenvatinib led to partial responses in 5 out of 33 patients, with 75% (24 patients) showing disease stability, indicating that molecular target therapy holds potential [73].
A significant portion of the literature focusing on ACC in the head and neck does not discuss the status of the margins. Garden et al. [74] reported that of 198 patients, 42% had microscopically positive margins, while another 28% presented with margins that were either close or ambiguous. In Erovic et al.’s research [75], positive surgical margins were detected in 60% of ACC cases. Lee et al. [76] documented a 50.82% occurrence of tight or positive surgical margins.
The findings of this study indicated that a 5-year survival rate of patients undergoing surgery followed by radiotherapy was 68.0%. Postoperative radiation therapy is generally recommended for all patients with ACC of the minor salivary glands, regardless of the extent of resection [59,60].
The high frequency of relapses and resistance to therapy in ACC has been connected to both its tendency for topical and regional invasion, and its property of PNI [77]. The common malignant feature of ACC is distant metastasis.
ACC is characterized by both local and systemic dissemination to various organs. In this study, local and distant metastases were reported among 18.2% [30] to 22.9% [21] of the cases, especially in the lymph nodes and lungs. In a retrospective analysis of patients with distant metastases, the lungs were identified as the exclusive site of metastasis in the majority of the cases [78]. Further, cervical lymph node involvement is seen in approximately 14.5% of ACC patients, as evidenced by a large-scale retrospective study in China, which documented cervical lymph node metastasis in 10% of 798 ACC cases [79]. Multiple studies have also reported the liver as a primary site for systemic disease spread. While metastasis to the breast and larynx is less frequent, extremely rare instances of metastasis have been noted in areas such as the pituitary gland, sternum, dorsal spine [80], choroid, bones of the toe, and the pericardium [80,81,82,83,84,85,86]. Recurrences in ACC are frequent, and in post-initial treatment, the chances of reoccurrence can be up to 50% in particular cases [77]. This significant likelihood of reoccurrence, coupled with the absence of thorough and effective treatment, leads to an unfavorable prognosis. The resistance of recurrent and metastasized ACC to treatment over lengthy durations further complicates disease control. Research has shown a more favorable prognosis in younger patients and females, with survival rates of 90.34%, 79.88%, and 69.22% at 5, 10, and 15 years, respectively [87]. However, a 2020 study with a small sample size of 49 participants reported overall survival rates varying between 68% to 80% for 5 years and 52% to 65% for 10 years, with long-term survival rates ranging from 23% to 40% [88]. The combination of PNI with locoregional invasion has been identified as significant risk factors that contribute to recurrence and resistance to therapy, with risks rising sharply when these factors are present together [77]. The management and prognosis of recurrent and metastasized ACC that results from PNI and conventional spread are often intricate and difficult. Such cases might necessitate multiple surgeries and subsequent radiotherapy after resection. Furthermore, both recurrence and metastasis are frequently linked with adverse long-term prognosis and a lack of disease-free survival [89]. Moreover, even in patients where ACC was diagnosed and resected in the early stage, there is a high risk of distant metastases, particularly in patients with age >45 years, lymph node involvement, and high-grade solid subtype histological features [90]; thus, a follow-up period of approximately 15 years with annual chest CT scans with contrast post-treatment is recommended.
The continued study of ACC’s molecular biology may lead to new targeted therapies. Furthermore, developing refined imaging techniques for better assessment of PNI and improving early detection will be critical in advancing ACC management [91].
Several limitations should be considered when interpreting the findings of this study. The included studies varied in quality, with inconsistent reporting of observational variables. The rarity of ACC and limited data availability result in lower levels of evidence. The wide time span covered by the studies may have influenced outcome results due to advancements in technology, terminology, and treatment. Furthermore, within this systematic review, the work conducted by Tian et al. [29] stands out as the largest, comprising 681 cases out of the total cases examined. As a result, it is crucial to approach the interpretation of this study’s findings with caution. The potential for variations in diagnosis and reporting has the potential to influence the accuracy and dependability of the study’s conclusions. Consequently, while the study offers invaluable insights, researchers and clinicians must recognize the inherent limitations and exercise caution when applying its findings. Nevertheless, the findings of this study provide valuable insights for physicians in making treatment decisions and emphasize the need for ongoing research and collaborative clinical efforts to improve the management and outcomes of this challenging disease.
5. Conclusions
ACC of the minor salivary glands is a multifaceted condition typically manifesting as asymptomatic enlargement and ulceration. This disease is marked by distinct histopathological patterns and PNI. Recognizing these distinctive aspects is key in shaping the treatment plan, which can range from surgical procedures to radiation therapy, chemotherapy, and evolving targeted treatments. Continuous research and collaborative clinical efforts remain critical for ongoing progress in the treatment and management of this challenging condition.
Author Contributions
Conceptualization, M.A.J. and M.I.; methodology, A.M.E. and M.H., formal analysis, M.H. and M.A.J.; investigation, M.H. and A.M.E.; writing—original draft preparation, M.A.J.; writing—review and editing, M.H., M.I. and A.M.E.; supervision, M.A.J. and M.I.; project administration, M.A.J. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Coca-Pelaz A., Rodrigo J.P., Bradley P.J., Vander Poorten V., Triantafyllou A., Hunt J.L., Strojan P., Rinaldo A., Ferlito A. Adenoid cystic carcinoma of the head and neck-An update. Oral Oncol. 2015;51:652–661. doi: 10.1016/j.oraloncology.2015.04.005. [DOI] [PubMed] [Google Scholar]
- 2.Nightingale J., Lum B., Ladwa R., Simpson F., Panizza B. Adenoid cystic carcinoma: A review of clinical features, treatment targets and advances in improving the immune response to monoclonal antibody therapy. Biochim. Biophys. Acta Rev. Cancer. 2021;1875:188523. doi: 10.1016/j.bbcan.2021.188523. [DOI] [PubMed] [Google Scholar]
- 3.Billings S.D., McKenney J.K., Folpe A.L. Hardacre MC. Adenoid cystic carcinoma of the oral cavity: A clinicopathologic review of 109 cases. Head Neck Pathol. 2014;8:288–297. [Google Scholar]
- 4.Kokemueller H., Eckardt A., Brachvogel P., Hausamen J.E. Adenoid cystic carcinoma of the head and neck-a 20 years experience. Int. J. Oral Maxillofac. Surg. 2004;33:25–31. doi: 10.1054/ijom.2003.0448. [DOI] [PubMed] [Google Scholar]
- 5.Luna M.A., Batsakis J.G., el-Naggar A.K. Salivary gland tumors in children. Pt 1Ann. Otol. Rhinol. Laryngol. 1991;100:403–405. doi: 10.1177/000348949110001016. [DOI] [PubMed] [Google Scholar]
- 6.Seethala R.R. An update on grading of salivary gland carcinomas. Head Neck Pathol. 2009;3:69–77. doi: 10.1007/s12105-009-0102-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wysocki P.T., Izumchenko E., Meir J., Ha P.K., Sidransky D., Brait M. Adenoid cystic carcinoma: Emerging role of translocations and gene fusions. Oncotarget. 2016;4:66239–66254. doi: 10.18632/oncotarget.11288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moskaluk C.A. Adenoid cystic carcinoma: Clinical and molecular features. Head Neck Pathol. 2013;7:17–22. doi: 10.1007/s12105-013-0426-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Huang Z., Pan J., Chen J., Wu S., Wu T., Ye H., Zhang H., Nie X., Huang C. Multicentre clinicopathological study of adenoid cystic carcinoma: A report of 296 cases. Cancer Med. 2021;10:1120–1127. doi: 10.1002/cam4.3707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moro Melón M., Manrique Estrada C., Maseda Alvarez E., Pomar Blanco P., Llorente Pendás J., Suárez Nieto C. Adenoid cystic carcinoma of the minor salivary glands. Our experience. Acta Otorinolaringol. Esp. 1999;50:387–391. [PubMed] [Google Scholar]
- 11.Toida M., Shimokawa K., Makita H., Kato K., Kobayashi A., Kusunoki Y., Hatakeyama D., Fujitsuka H., Yamashita T., Shibata T. Intraoral minor salivary gland tumors: A clinicopathological study of 82 cases. Int. J. Oral Maxillofac. Surg. 2005;34:52832. doi: 10.1016/j.ijom.2004.10.010. [DOI] [PubMed] [Google Scholar]
- 12.Dhanuthai K., Boonadulyarat M., Jaengjongdee T., Jiruedee K. A clinico-pathologic study of 311 intra-oral salivary gland tumors in Thais. J. Oral Pathol. Med. 2009;38:495–500. doi: 10.1111/j.1600-0714.2009.00791.x. [DOI] [PubMed] [Google Scholar]
- 13.Dillon P.M., Chakraborty S., Moskaluk C.A., Joshi P.J., Thomas C.Y. Adenoid cystic carcinoma: A review of recent advances, molecular targets, and clinical trials. Head Neck. 2016;38:620–627. doi: 10.1002/hed.23925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rinaldo A., Shaha A.R., Pellitteri P.K., Bradley P.J., Ferlito A. Management of malignant sublingual salivary gland tumors. Oral Oncol. 2004;40:2–5. doi: 10.1016/S1368-8375(03)00104-0. [DOI] [PubMed] [Google Scholar]
- 15.Avery C.M., Moody A.B., McKinna F.E., Taylor J., Henk J.M., Langdon J.D. Combined treatment of adenoid cystic carcinoma of the salivary glands. Int. J. Oral Maxillofac. Surg. 2000;29:277–279. doi: 10.1016/S0901-5027(00)80028-4. [DOI] [PubMed] [Google Scholar]
- 16.Triantafillidou K., Dimitrakopoulos J., Iordanidis F., Koufogiannis D. Management of adenoid cystic carcinoma of minor salivary glands. J. Oral Maxillofac. Surg. 2006;64:1114–1120. doi: 10.1016/j.joms.2005.06.017. [DOI] [PubMed] [Google Scholar]
- 17.Perzin K., Gullane P., Clairmont A. Adenoid cystic carcinomas arising in salivary glands. A correlation of histologic features and clinical course. Cancer. 1978;42:265–282. doi: 10.1002/1097-0142(197807)42:1<265::AID-CNCR2820420141>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 18.De Morais E.F., da Silva L.P., Moreira D.G.L., Mafra R.P., Rolim L.S.A., de Moura Santos E., de Souza L.B., de Almeida Freitas R. Prognostic factors and survival in adenoid cystic carcinoma of the head and neck: A retrospective clinical and histopathological analysis of patients seen at a cancer center. Head Neck Pathol. 2021;15:416–424. doi: 10.1007/s12105-020-01210-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Page M.J., Moher D., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Von Elm E., Altman D.G., Egger M., Pocock S.J., Gøtzsche P.C., Vandenbroucke J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet. 2007;370:1453–1457. doi: 10.1016/S0140-6736(07)61602-X. [DOI] [PubMed] [Google Scholar]
- 21.Bardwil J.M., Reynolds C.T., Ibanez M.L., Luna M.A. Report of one hundred tumors of the minor salivary glands. Am. J. Surg. 1966;112:493–497. doi: 10.1016/0002-9610(66)90310-2. [DOI] [PubMed] [Google Scholar]
- 22.Ouyang D.Q., Liang L.Z., Zheng G.S., Ke Z.F., Weng D.S., Yang W.F., Su Y.X., Liao G.Q. Risk factors and prognosis for salivary gland adenoid cystic carcinoma in southern china: A 25-year retrospective study. Medicine. 2017;96:e5964. doi: 10.1097/MD.0000000000005964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kusama K., Iwanari S., Aisaki K., Wada M., Ohtani J., Itoi K., Hanai K., Shimizu K., Komiyama K., Kudo I., et al. Intraoral minor salivary gland tumors: A retrospective study of 129 cases. J. Nihon Univ. Sch. Dent. 1997;39:128–132. doi: 10.2334/josnusd1959.39.128. [DOI] [PubMed] [Google Scholar]
- 24.Jansisyanont P., Blanchaert R.H., Ord R.A. Intraoral minor salivary gland neoplasm: A single institution experience of 80 cases. Int. J. Oral Maxillofac. Surg. 2002;31:257–261. doi: 10.1054/ijom.2002.0223. [DOI] [PubMed] [Google Scholar]
- 25.Hyam D.M., Veness M.J., Morgan G.J. Minor salivary gland carcinoma involving the oral cavity or oropharynx. Aust. Dent. J. 2004;49:16–19. doi: 10.1111/j.1834-7819.2004.tb00044.x. [DOI] [PubMed] [Google Scholar]
- 26.Ito F.A., Ito K., Vargas P.A., De Almeida O.P., Lopes M.A. Salivary gland tumors in a Brazilian population: A retrospective study of 496 cases. Int. J. Oral Maxillofac. Surg. 2005;34:533–536. doi: 10.1016/j.ijom.2005.02.005. [DOI] [PubMed] [Google Scholar]
- 27.Jaber M.A. Intraoral minor salivary gland tumors: A review of 75 cases in a Libyan population. Int. J. Oral Maxillofac. Surg. 2006;35:150–154. doi: 10.1016/j.ijom.2005.07.006. [DOI] [PubMed] [Google Scholar]
- 28.Buchner A., Merrell P.W., Carpenter W.M. Relative frequency of intra-oral minor salivary gland tumors: A study of 380 cases from northern California and comparison to reports from other parts of the world. J. Oral Pathol. Med. 2007;36:207–214. doi: 10.1111/j.1600-0714.2007.00522.x. [DOI] [PubMed] [Google Scholar]
- 29.Tian Z., Li L., Wang L., Hu Y., Li J. Salivary gland neoplasms in oral and maxillofacial regions: A 23-year retrospective study of 6982 cases in an eastern Chinese population. Int. J. Oral Maxillofac. Surg. 2010;39:235–242. doi: 10.1016/j.ijom.2009.10.016. [DOI] [PubMed] [Google Scholar]
- 30.Saleh E., Ukwas A. Adenoid Cystic Carcinoma of Salivary Glands: A Ten-Year Review and an Assessment of the Current Management, Surgery, Radiotherapy, and Chemotherapy. Int. J. Otolaryngol. 2023;2023:7401458. doi: 10.1155/2023/7401458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Guyatt G., Oxman A.D., Akl E.A., Kunz R., Vist G., Brozek J., Norris S., Falck-Ytter Y., Glasziou P., DeBeer H., et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J. Clin. Epidemiol. 2011;64:383–394. doi: 10.1016/j.jclinepi.2010.04.026. [DOI] [PubMed] [Google Scholar]
- 32.Aromataris E., Fernandez R., Godfrey C., Holly C., Kahlil H., Tungpunkom P. Summarizing systematic reviews: Methodological development, conduct and reporting of an Umbrella review approach. Int. J. Evid. Based Healthc. 2015;13:132–140. doi: 10.1097/XEB.0000000000000055. [DOI] [PubMed] [Google Scholar]
- 33.Gontarz M., Bargiel J., Gąsiorowski K., Marecik T., Szczurowski P., Zapała J., Wyszyńska-Pawelec G. Epidemiology of Primary Epithelial Salivary Gland Tumors in Southern Poland-A 26-Year, Clinicopathologic, Retrospective Analysis. J. Clin. Med. 2021;10:1663. doi: 10.3390/jcm10081663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.El-Naggar A.K., Chan J.K.C., Grandis J.R., Takata T., Slootweg P.J., editors. WHO Classification of Head and Neck Tumours. World Health Organization; Geneva, Switzerland: 2017. IARC. [Google Scholar]
- 35.Boyle T.A., Semus S., Joseph N. Epidemiology of adenoid cystic carcinoma in the United States. J. Clin. Oncol. 2020;38:13600. doi: 10.1200/JCO.2020.38.15_suppl.e13600. [DOI] [Google Scholar]
- 36.Yang H., Yao F., Tantai J., Zhao Y., Tan Q., Zhao H. Resected tracheal adenoid cystic carcinoma: Improvements in outcome at a single institution. Ann. Thorac. Surg. 2016;101:294–300. doi: 10.1016/j.athoracsur.2015.06.073. [DOI] [PubMed] [Google Scholar]
- 37.Hsu A.A., Tan E.H., Takano A.M. Lower Respiratory Tract Adenoid Cystic Carcinoma: Its Management in the Past Decades. Clin. Oncol. 2015;27:732–740. doi: 10.1016/j.clon.2015.06.012. [DOI] [PubMed] [Google Scholar]
- 38.Je H.U., Song S.Y., Kim D.K., Kim Y.H., Jeong S.Y., Back G.M., Choi W., Kim S.S., Park S.I., Choi E.K. A 10-year clinical outcome of radiotherapy as an adjuvant or definitive treatment for primary tracheal adenoid cystic carcinoma. Radiat. Oncol. 2017;12:196. doi: 10.1186/s13014-017-0933-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gamboa-Hoil S.I., Silva-Godínez J.C., Abrego-Vásquez J.A. Adenoid cystic carcinoma of head and neck. A 5-year retrospective study: Experience in a single third-level reference center. Cirugía Cir. 2020;88:34–40. doi: 10.24875/CIRUE.M20000109. [DOI] [PubMed] [Google Scholar]
- 40.Young A., Okuyemi O. Stat Pearls. Stat Pearls Publishing; Treasure Island, FL, USA: 2022. Malignant Salivary Gland Tumors. [PubMed] [Google Scholar]
- 41.Li N., Xu L., Zhao H., El-Naggar A.K., Sturgis E.M. A comparison of the demographics, clinical features, and survival of patients with adenoid cystic carcinoma of major and minor salivary glands versus less common sites within the Surveillance, Epidemiology, and End Results registry. Cancer. 2012;118:3945–3953. doi: 10.1002/cncr.26740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jaso J., Malhotra R. Adenoid cystic carcinoma. Arch. Pathol. Lab. Med. 2011;135:511–515. doi: 10.5858/2009-0527-RS.1. [DOI] [PubMed] [Google Scholar]
- 43.Jang S., Patel P.N., Kimple R.J., McCulloch T.M. Clinical Outcomes and Prognostic Factors of Adenoid Cystic Carcinoma of the Head and Neck. Anticancer Res. 2017;37:3045–3052. doi: 10.21873/anticanres.11659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gondivkar S.M., Gadbail A.R., Chole R., Parikh R.V. Adenoid cystic carcinoma: A rare clinical entity and literature review. Oral Oncol. 2011;47:231–236. doi: 10.1016/j.oraloncology.2011.01.009. [DOI] [PubMed] [Google Scholar]
- 45.Ferlito A. Cervical lymph node metastasis in adenoid cystic carcinoma of the major salivary glands. J. Laryngol. Otol. 2015;131:96–105. doi: 10.1017/S0022215116009749. [DOI] [PubMed] [Google Scholar]
- 46.Huo Z., Wu H., Li S., Liang Z. Molecular genetic studies on EGFR, KRAS, BRAF, ALK, PIK3CA, PDGFRA, and DDR2 in primary pulmonary adenoid cystic carcinoma. Diagn. Pathol. 2015;10:161. doi: 10.1186/s13000-015-0409-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Maziak D.E. Biology of adenoid cystic carcinoma of the tracheobronchial tree and principles of management. Thorac. Surg. Clin. 2018;28:145–148. doi: 10.1016/j.thorsurg.2018.01.002. [DOI] [PubMed] [Google Scholar]
- 48.Agrawal S., Jackson C., Celie K.B., Dodhia C., Monie D., Monzon J., Kaufman T., Hellenthal N.J. Survival trends in patients with tracheal carcinoma from 1973 to 2011. Am. J. Otolaryngol. 2017;38:673–677. doi: 10.1016/j.amjoto.2017.08.005. [DOI] [PubMed] [Google Scholar]
- 49.Pearson F.G., Thompson D.W., Weissberg D., Simpson W.J., Kergin F.G. Adenoid cystic carcinoma of the trachea. Experience with 16 patients managed by tracheal resection. Ann. Thorac. Surg. 1974;18:16–29. doi: 10.1016/S0003-4975(10)65713-X. [DOI] [PubMed] [Google Scholar]
- 50.Wright C.L., Gandhi M., Mitchell C.A. Adenoid cystic carcinoma of the left main bronchus mimicking MacLeod’s syndrome. Thorax. 1996;51:451–452. doi: 10.1136/thx.51.4.451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Nuwal P., Dixit R., Singhal A.K. Primary adenoid cystic carcinoma of trachea presenting as midline neck swelling and mimicking thyroid tumor: A case report and review of literature. Lung India. 2010;27:167–169. doi: 10.4103/0970-2113.68330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lloyd S., Yu J.B., Wilson L.D., Decker R.H. Determinants and patterns of survival in adenoid cystic carcinoma of the head and neck, including an analysis of adjuvant radiation therapy. Am. J. Clin. Oncol. 2011;34:76–81. doi: 10.1097/COC.0b013e3181d26d45. [DOI] [PubMed] [Google Scholar]
- 53.Fernandes H., D’souza C.R., Khosla C., George L., Katte N.H. Role of FNAC in the preoperative diagnosis of salivary gland lesions. JCDR. 2014;8:FC01. doi: 10.7860/JCDR/2014/6735.4809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Spiro R.H., Huvos A.G., Strong E.W. Adenoid cystic carcinoma: Factors influencing survival. Am. J. Surg. 1979;138:579–583. doi: 10.1016/0002-9610(79)90423-9. [DOI] [PubMed] [Google Scholar]
- 55.Bradley P.J. Adenoid cystic carcinoma of the head and neck: A review. Curr. Opin. Otolaryngol. Head Neck Surg. 2012;29:85–92. doi: 10.1097/00020840-200404000-00013. [DOI] [PubMed] [Google Scholar]
- 56.Du F., Zhou C.X., Gao Y. Myoepithelial differentiation in cribriform, tubular and solid pattern of adenoid cystic carcinoma: A potential involvement in histological grading and prognosis. Ann. Diagn. Pathol. 2016;22:12–17. doi: 10.1016/j.anndiagpath.2016.03.001. [DOI] [PubMed] [Google Scholar]
- 57.Nagao T., Gaffey T.A., Serizawa H., Sugano I., Ishida Y., Yamazaki K., Tokashiki R., Yoshida T., Minato H., Kay P.A., et al. Dedifferentiated Adenoid Cystic Carcinoma: A Clinicopathologic Study of 6 Cases. Modern Pathol. 2003;16:1265–1272. doi: 10.1097/01.MP.0000097366.88165.08. [DOI] [PubMed] [Google Scholar]
- 58.Belulescu I., Margaritescu C., Dumitrescu C., Daguci L., Munteanu C., Margaritescu C. Adenoid cystic carcinoma of salivary gland: A ten-year single institute experience. Curr. Health Sci. J. 2020;46:56–65. doi: 10.12865/CHSJ.46.01.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Stelow E.B., Bishop J.A. Update from the 4th Edition of the World Health Organization Classification of Head and Neck Tumours: Tumors of the Nasal Cavity, Paranasal Sinuses and Skull Base. Head Neck Pathol. 2017;11:3–15. doi: 10.1007/s12105-017-0791-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Liu X., Yang X., Zhan C., Zhang Y., Hou J., Yin X. Perineural Invasion in Adenoid Cystic Carcinoma of the Salivary Glands: Where We Are and Where We Need to Go. Front. Oncol. 2020;10:1493. doi: 10.3389/fonc.2020.01493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Prasad M.L., Barbacioru C.C., Rawal Y.B., Husein O., Wen P. Hierarchical cluster analysis of myoepithelial/basal cell markers in adenoid cystic carcinoma and polymorphous low-grade adenocarcinoma. Mod Pathol. 2008;21:105–114. doi: 10.1038/modpathol.3800983. [DOI] [PubMed] [Google Scholar]
- 62.Ju J., Li Y., Chai J. The role of peri neural invasion on head and neck adenoid cystic carcinoma prognosis: A systematic review and meta-analysis. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2016;122:691–701. doi: 10.1016/j.oooo.2016.08.008. [DOI] [PubMed] [Google Scholar]
- 63.Zhang M., Wu J.S., Xian H.C. CXCR5 induces perineural invasion of salivary adenoid cystic carcinoma by inhibiting microRNA-187. Aging. 2021;13:15384–15399. doi: 10.18632/aging.203097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Spiro R.H. Distant metastasis in adenoid cystic carcinoma of salivary origin. Am. J. Surg. 1997;174:495–498. doi: 10.1016/S0002-9610(97)00153-0. [DOI] [PubMed] [Google Scholar]
- 65.Ran J., Qu G., Chen X., Zhao D. Clinical features, treatment and outcomes in patients with tracheal adenoid cystic carcinoma: A systematic literature review. Radiat. Oncol. 2021;16:38. doi: 10.1186/s13014-021-01770-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Luksic I., Suton P. Elective neck dissection in adenoid cystic carcinoma of head and neck: Yes, or no? A systematic review. Euro Arch. Oto-Rhino-Laryngol. 2019;276:2957–2962. doi: 10.1007/s00405-019-05669-1. [DOI] [PubMed] [Google Scholar]
- 67.Su W., Yang H.Y. Treatment plan and prognosis of salivary adenoid cystic carcinoma with lung metastasis. West China J. Stomatol. 2019;37:214–219. doi: 10.7518/hxkq.2019.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Bahl A., Panda N.K., Elangovan A., Bakshi J., Verma R., Mohindra S., Gupta R., Oinam A.S., Kaur S., Vashishta R.K., et al. Evaluation of multimodality management of adenoid cystic carcinoma of the head and neck. Indian J. Otolaryngol. Head Neck Surg. 2019;71:628–632. doi: 10.1007/s12070-018-1442-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Cassidy R.J., Switchenko J.M., El-Deiry M.W., Belcher R.H., Zhong J., Steuer C.E., Saba N.F., McDonald M.W., Yu D.S., Gillespie T.W., et al. Disparities in postoperative therapy for salivary gland adenoid cystic carcinomas. Laryngoscope. 2019;129:377–386. doi: 10.1002/lary.27302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ali S., Palmer F.L., Katabi N. Long-term local control rates of patients with adenoid cystic carcinoma of the head and neck managed by surgery and postoperative radiation. Laryngoscope. 2017;127:2265–2269. doi: 10.1002/lary.26565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Chau N.G., Hotte S.J., Chen E.X., Chin S.F., Turner S., Wang L., Siu L.L. A phase II study of sunitinib in recurrent and/or metastatic adenoid cystic carcinoma (ACC) of the salivary glands: Current progress and challenges in evaluating molecularly targeted agents in ACC. Ann. Oncol. 2012;23:1562–1570. doi: 10.1093/annonc/mdr522. [DOI] [PubMed] [Google Scholar]
- 72.Kim D.W., Oh D.Y., Shin S.H., Kang J.H., Cho B.C., Chung J.S., Kim H., Park K.U., Kwon J.H., Han J.Y., et al. A multicenter phase II study of everolimus in patients with progressive unresectable adenoid cystic carcinoma. BMC Cancer. 2014;14:795. doi: 10.1186/1471-2407-14-795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Tchekmedyian V., Sherman E., Dunn L., Tran C., Baxi S., Katabi N., Antonescu C., Ostrovnaya I., Haque S., Pfister D. Phase II Study of Lenvatinib in Patients with Progressive, Recurrent or Metastatic Adenoid Cystic Carcinoma. J. Clin. Oncol. 2019;37:1529–1537. doi: 10.1200/JCO.18.01859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Garden A.S., Weber R.S., Morrison W.H., Ang K.K., Peters L.J. The influence of positive margins and nerve invasion in adenoid cystic carcinoma of the head and neck treated with surgery and radiation. Int. J. Radiat. Oncol. Biol. Phys. 1995;32:619–626. doi: 10.1016/0360-3016(95)00122-F. [DOI] [PubMed] [Google Scholar]
- 75.Erovic B.M., Shah M.D., Bruch G., Johnston M., Kim J., O’Sullivan B., Perez-Ordonez B., Weinreb I., Atenafu E.G., de Almeida J.R., et al. Outcome analysis of 215 patients with parotid gland tumors: A retrospective cohort analysis. J. Otolaryngol. Head Neck Surg. 2015;44:43. doi: 10.1186/s40463-015-0097-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Lee S.Y., Kim B.H., Choi E.C. Nineteen-year oncologic outcomes and the benefit of elective neck dissection in salivary gland adenoid cystic carcinoma. Head Neck. 2014;36:1796–1801. doi: 10.1002/hed.23537. [DOI] [PubMed] [Google Scholar]
- 77.Ho A.S., Ochoa A., Jayakumaran G., Zehir A., Mayor C.V., Tepe J., Makarov V., Dalin M.G., He J., Bailey M., et al. Genetic hallmarks of recurrent/metastatic adenoid cystic carcinoma. J. Clin. Investig. 2019;129:4276–4289. doi: 10.1172/JCI128227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Fang Y., Peng Z., Wang Y., Gao K., Liu Y., Fan R., Zhang H., Xie Z., Jiang W. Current opinions on diagnosis and treatment of adenoid cystic carcinoma. Oral Oncol. 2022;130:105945. doi: 10.1016/j.oraloncology.2022.105945. [DOI] [PubMed] [Google Scholar]
- 79.Zhang W., Wang S., Jiang Y. Fatty acid synthase contributes to epithelial-mesenchymal transition and invasion of salivary adenoid cystic carcinoma through PRRX1/Wnt/β-catenin pathway. J. Cell. Mol. Med. 2020;24:11465–11476. doi: 10.1111/jcmm.15760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kumar V., Nair R., Upadhyaya S., Nayal B., Shetty A. Extradural spinal metastasis of adenoid cystic carcinoma (acc): A case report. J. Clin. Diagn. Res. 2015;9:XD09–XD10. doi: 10.7860/JCDR/2015/10644.5498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Krucoff K., Shammas R., Stoecker M., Tolnitch L. Rare breast metastasis from adenoid cystic carcinoma of the submandibular gland. BMJ Case Rep. 2018;2018:223345. doi: 10.1136/bcr-2017-223345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ishikawa T., Tateda M., Oshima H. Metastasis of adenoid cystic carcinoma from a submandibular gland to the larynx. Auris Nasus Larynx. 2019;46:907–911. doi: 10.1016/j.anl.2018.11.001. [DOI] [PubMed] [Google Scholar]
- 83.Hughes J., Retzlaff A., Sims J., Obrien E., Giannini C., Huston J. Adenoid cystic carcinoma metastatic to the pituitary: A case report and discussion of potential diagnostic value of magnetic resonance elastography in pituitary tumors. World Neurosurg. 2016;91:669. doi: 10.1016/j.wneu.2016.03.044. [DOI] [PubMed] [Google Scholar]
- 84.Alshammari A., Eldeib O., Eldeib A., Saleh W. Adenoid cystic carcinoma of the submandibular gland with rare metastasis to the sternum in a 52-year-old male. Ann. Thorac. Med. 2016;11:82–84. doi: 10.4103/1817-1737.165307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Zhang J., Wang Y., Cao D. Primary adenoid cystic carcinoma of the liver: Case report and review of the literature. Ann. Hepatol. 2019;18:209–214. doi: 10.5604/01.3001.0012.7915. [DOI] [PubMed] [Google Scholar]
- 86.Nasir N., Monroe C., Hagerty B. Adenoid cystic carcinoma of the salivary gland metastasizing to the pericardium and diaphragm: Report of a rare case. Diagn. Cytopathol. 2021;49:E31–E35. doi: 10.1002/dc.24566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Alali F., Kochaji N. Proliferative activity of myoepithelial cells in normal salivary glands and adenoid cystic carcinomas based on double immunohistochemical labeling. Asian Pac. J. Cancer Prev. 2018;19:1965–1970. doi: 10.22034/APJCP.2018.19.7.1965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Yang C., Zhang L., Sanati S. SOX10 Is a sensitive marker for breast and salivary gland adenoid cystic carcinoma: Immunohistochemical characterization of adenoid cystic carcinomas. Breast Cancer Basic Clin. Res. 2019;13:117822341984218. doi: 10.1177/1178223419842185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Gao T., Shen Z., Ma C., Li Y., Kang X., Sun M. The CCL5/CCR5 Chemotactic pathway promotes perineural invasion in salivary adenoid cystic carcinoma. J. Oral Maxillofac. Surg. 2018;76:1708–1718. doi: 10.1016/j.joms.2018.02.009. [DOI] [PubMed] [Google Scholar]
- 90.Bhayani M.K., Yener M., El-Naggar A., Garden A., Hanna E.Y., Weber R.S., Kupferman M.E. Prognosis and risk factors for early-stage adenoid cystic carcinoma of the major salivary glands. Cancer. 2012;118:2872–2878. doi: 10.1002/cncr.26549. [DOI] [PubMed] [Google Scholar]
- 91.Stenman G. Molecular classification of mucoepidermoid carcinomas—Prognostic significance of the MECT1–MAML2 fusion oncogene. Genes Chromosomes Cancer. 2014;45:470–481. doi: 10.1002/gcc.20306. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.