Abstract
We present a case of orthodromic atrioventricular re-entrant tachycardia exhibiting both right and left bundle branch block pattern wide QRS morphologies caused by bilateral bystander nodoventricular (NV) accessory pathways. These wide QRS morphologies came from pre-excitation accompanied by delta waves. In the context of NV accessory pathways, left-sided manifest NV accessory pathways are rare.
Key Words: atrioventricular accessory pathway (Kent bundle), bundle branch block, catheter ablation, delta wave, pre-excitation
Central Illustration
History of Presentation
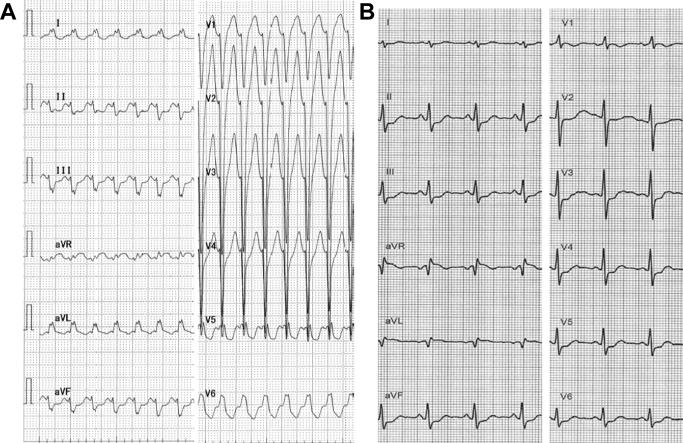
A 51-year-old woman presented to the emergency department with rapid palpitations and dizziness. She was mentally alert. Her blood pressure was 60/40 mm Hg, and her heart rate was 200 beats/min. Other physical examination findings were unremarkable. The electrocardiogram showed a regular wide QRS tachycardia with left bundle branch block (LBBB) pattern and superior QRS axis, with a rate of 214 beats/min (Figure 1A). A 10 mg infusion of adenosine triphosphate terminated the tachycardia. After restoration of sinus rhythm, a slur in the beginning of the QRS complex, which could be barely identified in lead V1 with a PR interval of 0.12 millisecond, became apparent (Figure 1B).
Learning Objectives
-
•
To be able to make a differential diagnosis of wide QRS tachycardia without overlooking rare types of accessory pathways.
-
•
To understand that bundle branch block QRS morphology can be caused by pre-excitation as well as conduction block.
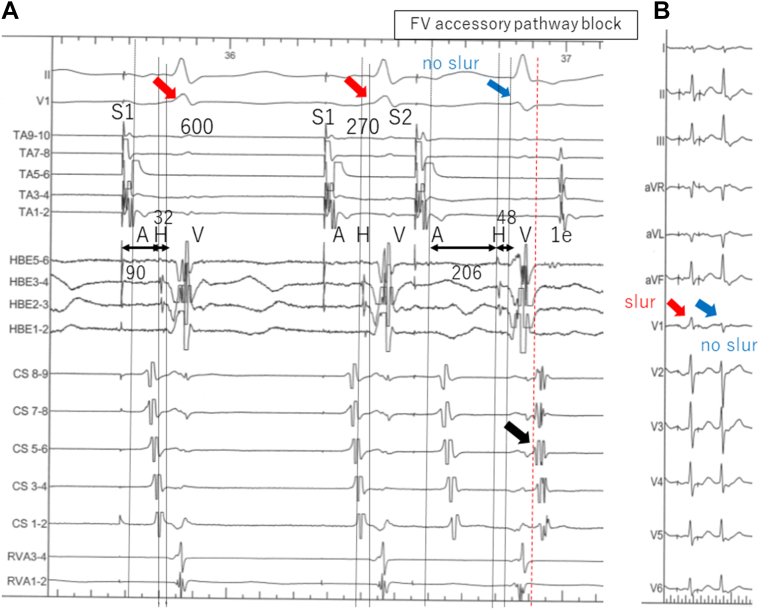
Figure 1.
12-Lead Electrocardiogram
Electrocardiogram on arrival (A) and after sinus rhythm restoration by adenosine triphosphate infusion (B).
Past Medical History
The patient had no significant medical history.
Differential Diagnosis
The differential diagnosis included supraventricular tachycardia with aberrancy, antidromic atrioventricular re-entrant tachycardia (AVRT), and ventricular tachycardia.
Investigations
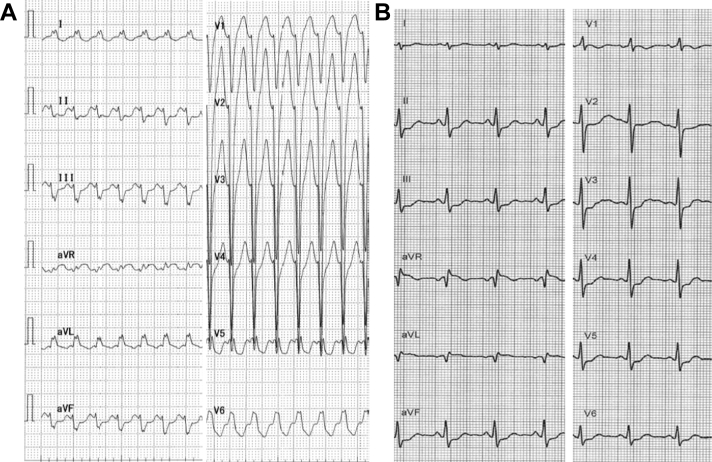
After recovery of sinus rhythm, the patient was challenged with an additional injection of 20 mg of adenosine triphosphate. This made the PR interval slightly prolonged and resulted in transient atrioventricular (AV) block. During this time, QRS morphology was unchanged (Figure 2), leading us to exclude a manifest AV accessory pathway (bundle of Kent).
Figure 2.
Effects of ATP Injection on Electrocardiogram During Sinus Rhythm
The arrows point at QRS morphology, which was unchanged. ATP = adenosine triphosphate.
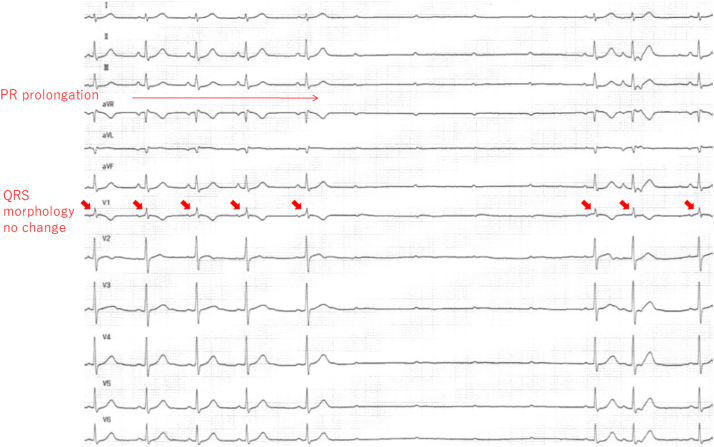
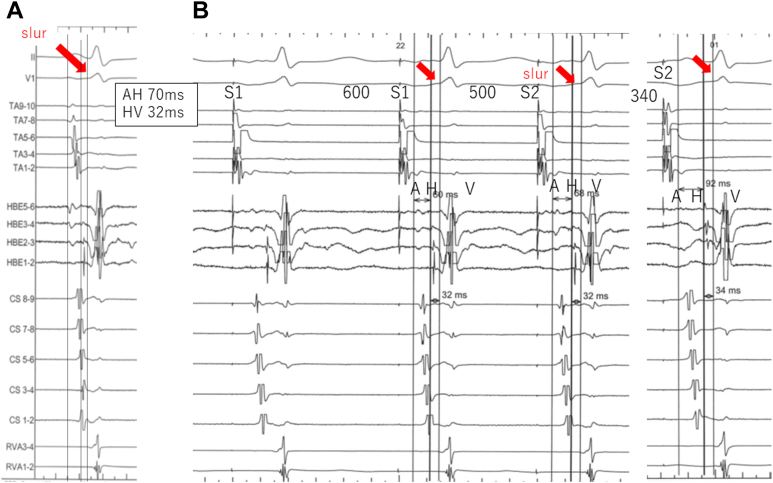
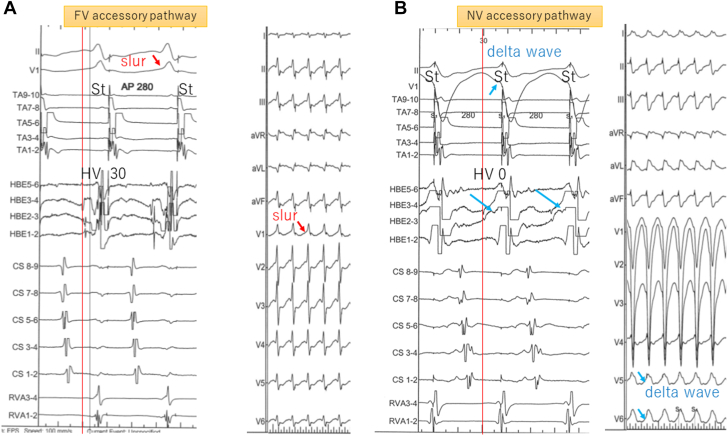
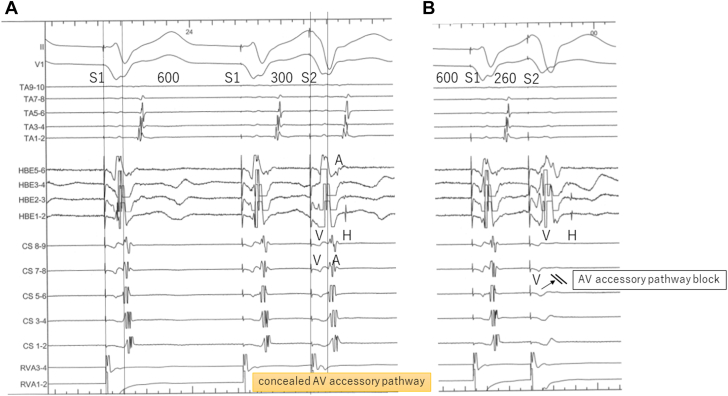
We then performed an electrophysiological study. In sinus rhythm, the atrio-His (AH) and His-ventricular (HV) intervals were 70 and 32 milliseconds, respectively. During atrial programmed stimulation at a cycle length of 600 milliseconds, the AH interval prolonged as the S1-S2 interval was shortened, but the HV interval remained fixed (Figure 3). When the S1-S2 interval was shortened further to 270 milliseconds, the slur disappeared and was accompanied by prolongation of the HV interval from 36 to 48 milliseconds in addition to AH interval prolongation. As a result, we diagnosed the presence of a fasciculoventricular (FV) accessory pathway. At the same time, an atrial echo beat with earliest activation in one of the coronary sinus leads was noted (Figure 4). When rapid atrial pacing was applied at 280-millisecond intervals, a different QRS morphology of an LBBB pattern accompanied by prominent delta waves appeared briefly (Figure 5). During QRS of LBBB configuration, the earliest ventricular site among the shown catheters was HBE3-4 with the local HV interval of 0 milliseconds, and the His electrograms were activated in an antegrade fashion, implying existence of a nodoventricular (NV) accessory pathway connecting the AV node and right ventricle. Ventriculoatrial conduction was eccentric without any decrements, with the same atrial activation sequence as the echo beat noted earlier, leading us to diagnose a left-sided AV accessory pathway (Figure 6). Para-Hisian pacing results were consistent with a pattern of mixed nodal and AV accessory pathway response.
Figure 3.
The Diagnosis of a Fasciculoventricular Accessory Pathway
Intracardiac electrograms during sinus rhythm (A) and atrial programmed stimulation (B).
The atrio-His (AH) interval prolong as the S1-S2 interval is shortened to 340 milliseconds with no change in the slur (arrows) or in the His-ventricular (HV) interval. A fasciculoventricular accessory pathway is diagnosed.
Figure 4.
Atrial Programmed Stimulation
Intracardiac electrograms (A) and 12-lead electrocardiogram (B) during atrial programmed stimulation. When the S1-S2 interval is shortened to 270 milliseconds, in addition to the atrio-His interval prolongation, the His-ventricular interval is prolonged by 16 milliseconds and the slur wave disappears. This is accompanied by an echo beat (1e) with earliest activation in lead CS 5-6 (black arrow). Fasciculoventricular (FV) accessory pathway block is diagnosed. Red arrows point at the slur and blue arrows at QRS complexes without the slur.
Figure 5.
Atrial Constant Stimulation
Intracardiac electrograms and 12-lead electrocardiogram with fasciculoventricular (FV) accessory pathway (A) and right-sided nodoventricular (NV) accessory pathway (B) conduction during atrial constant stimulation of 280 milliseconds. Red arrows in panel A point at the slur. Blue arrows in B point at the local ventricular electrogram in HBE3-4, which fuses with His potential, resulting in a local His-ventricular (HV) interval of 0 milliseconds and delta waves in leads V5 and V6.
Figure 6.
Intracardiac Electrograms During Ventricular Programmed Extrastimulation
(A) Ventriculoatrial conduction is eccentric without decrements. (B) The atrioventricular (AV) accessory pathway is blocked, and His-atrial block also occurs via AV nodal conduction while drive train (S1) is 600 milliseconds and S1-S2 is 260 milliseconds.
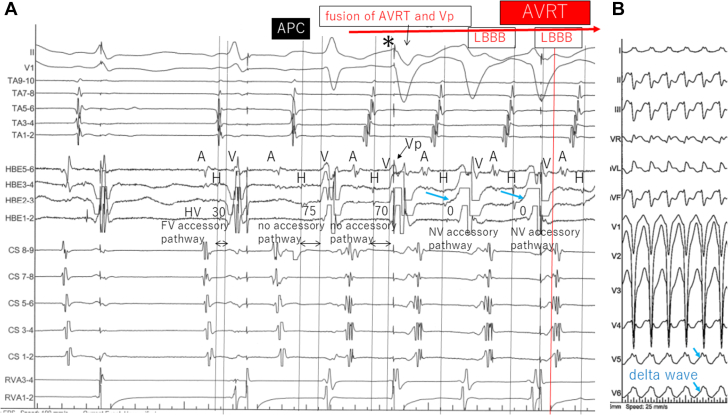
Two other tachycardias were uncovered. One was an LBBB pattern tachycardia with a cycle length of 286 milliseconds. It was initiated by an atrial premature contraction, with the same atrial activation sequence as that via the AV accessory pathway during ventricular pacing. QRS converted to LBBB configuration accompanied by a change in local HV interval to 0 milliseconds in HBE2-3 and was diagnosed as orthodromic AVRT with bystander right NV accessory pathway (Figure 7). There were prominent delta waves on the surface electrocardiogram, signifying that the LBBB pattern was not caused by conduction block but by pre-excitation with additional bystander right NV accessory pathway conduction. The tachycardia terminated before detailed study was possible.
Figure 7.
Initiation of Orthodromic AVRT With LBBB Configuration
(A) After an atrial premature contraction (APC) with narrow QRS complex during ventricular pacing, a tachycardia with retrograde AV accessory pathway conduction starts. The second beat (asterisk) is a fusion of QRS without any accessory pathway tracts (HV interval of 70 milliseconds) and ventricular pacing, when suddenly QRS transitions to a left bundle branch block (LBBB) configuration accompanied by a change in local HV interval to 0 milliseconds in HBE2-3 (blue arrows). (B) On the surface electrocardiogram, blue arrows point at delta waves in leads V5 and V6. AVRT = atrioventricular re-entrant tachycardia; Vp = ventricular pacing; other abbreviations as in Figures 3, 5, and 6.
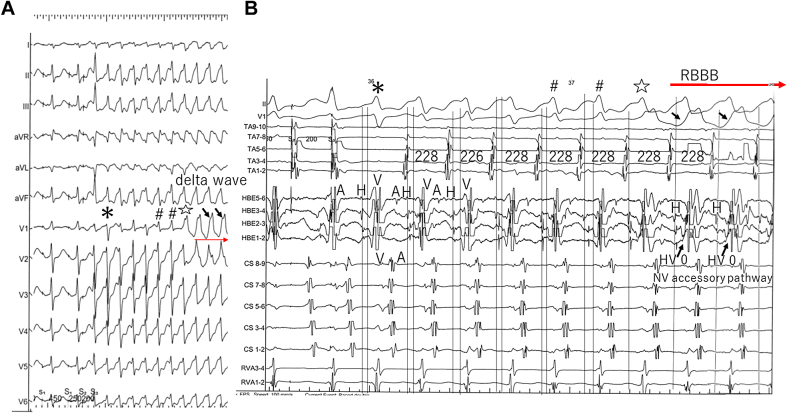
A second tachycardia, this time with right bundle branch block (RBBB) configuration with a cycle length of 228 milliseconds, was induced during programmed atrial pacing with 2 extrastimuli (Figure 8). The atrial activation sequence was again the same as for the AV accessory pathway, and a ventricular single scan during the His refractory period advanced the next atrial excitation. The tachycardia continued with V-A-V sequence after entrainment from the right ventricle and was diagnosed as orthodromic AVRT. When the AVRT first started, various QRS morphologies, including narrow-complex QRS, were observed before it converted to RBBB morphology, signifying that RBBB was not essential for AVRT. However, the shift to RBBB configuration was accompanied by a local HV interval change to 0 milliseconds in HBE1-2 and appearance of prominent delta waves, leading us to diagnose a bystander left NV accessory pathway (Figure 9).
Figure 8.
Induction of Orthodromic AVRT With RBBB Configuration
Surface 12-lead electrocardiogram (A) and intracardiac electrograms (B) during induction of orthodromic AVRT with right bundle branch block (RBBB) configuration. During programmed atrial stimulation with 2 extrastimuli (S1-S1 = 450 milliseconds, S1-S2 = 250 milliseconds, S2-S3 = 200 milliseconds), tachycardia with retrograde AV accessory pathway conduction starts, with the initial beat a narrow QRS complex without FV accessory pathway conduction (asterisk). A series of various QRS configurations is subsequently followed by a switch to RBBB configuration, accompanied by change in local HV interval to 0 milliseconds and the initial deflection of local ventricular electrogram from negative to positive in HBE1-2. QRS complexes with the same signs (∗, #, ⋆, and Δ) are identical in A and B. Black arrows point at delta waves in V1 and the local ventricular electrogram in HBE1-2.Abbreviations as in Figures 3, 5, 6, and 7.
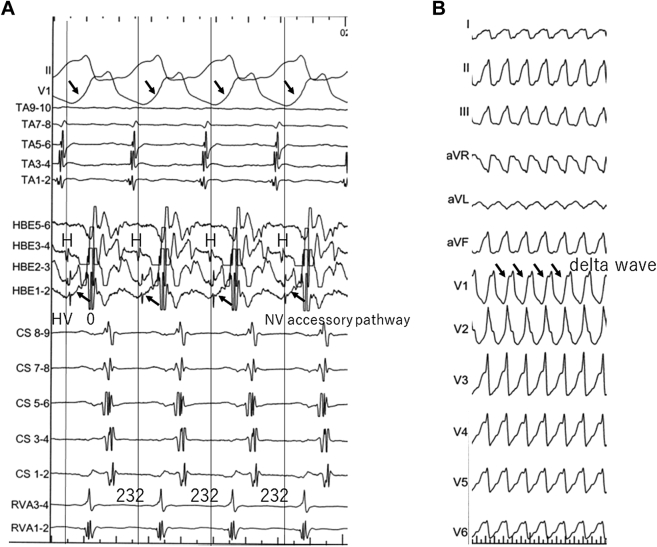
Figure 9.
Orthodromic AVRT With RBBB Configuration
Intracardiac electrograms (A) and 12-lead electrocardiogram (B) during orthodromic AVRT with RBBB configuration. After the QRS morphology of the tachycardia stabilizes to RBBB configuration, the tachycardia cycle also stabilizes (to 232 milliseconds). Black arrows in A point at the local ventricular electrogram in HBE1-2, which fuses with His potential, resulting in the local HV interval of 0 milliseconds. Note that the QRS has a delta wave (black arrows). Abbreviations as in Figures 5, 7, and 8.
Management
The concealed left posterior AV accessory pathway was targeted with radiofrequency catheter ablation. Although the antegrade FV accessory pathway conduction was left intact, no tachycardia was inducible even with isoproterenol administration.
Discussion
Nodofascicular (NF) and NV accessory pathways are uncommon accessory pathway variants. They connect the inferior extensions of the AV node with the Purkinje system or the ventricles; therefore, the target site for radiofrequency ablation is the slow pathway region.1,2 Among NF/NV accessory pathways, the left-sided accessory pathways are even rarer, especially manifest ones.2,3
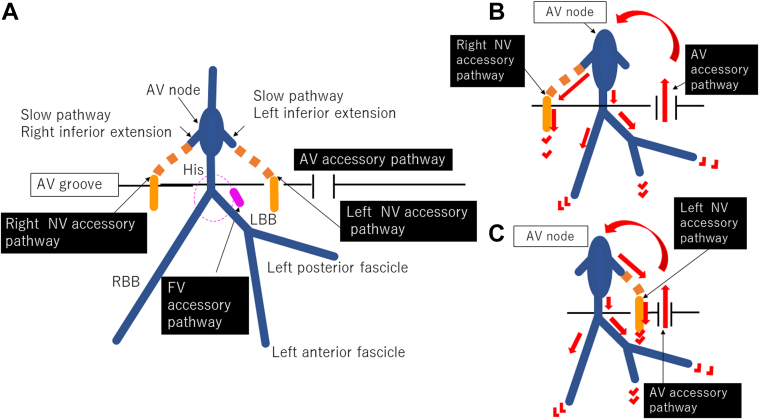
In our case, conduction along the NV accessory pathways was intermittent, and thus we were unable to perform activation mapping to assess their connecting sites. We therefore had to make educated guesses as to the location of the accessory pathways in this patient based on intracardiac and surface electrograms (Figure 10). It has been reported that NF/NV accessory pathways connect to the slow pathway.1, 2, 3, 4 The human compact AV node contains rightward and leftward inferior extensions histologically5; thus, the most likely explanation in this case was that the right-sided NV accessory pathway connected the right inferior extension and right ventricle, and the left-sided NV accessory pathway connected the left inferior extension and left ventricle. The reasons for why the NV accessory pathway conduction was intermittent for both accessory pathways are unclear.
Figure 10.
Schematic Diagram
Schematic diagram of the putative accessory pathways in this patient (A), and the circuits of AVRT when displaying LBBB configuration (B) and RBBB configuration (C). The normal cardiac conduction system is described in blue in A; both NV accessory pathways are described in orange, and the FV accessory pathway in pink. The putative parts of the accessory pathways are shown with a dotted line. Abbreviations as in Figures 5 to 8.
The shift of QRS configuration to bundle branch block pattern and the change of local HV interval to 0 milliseconds in HBE arose at the same time in all circumstances. This scenario might indicate that bundle branch block pattern was a result of pre-excitation via the NV accessory pathways instead of conduction block.
Follow-up
The patient was doing well without palpitations at her 1-year follow-up visit.
Conclusions
We described a case in which orthodromic AVRT displayed 2 wide QRS patterns accompanied by delta waves, caused by 2 different bystander conducted NV accessory pathways.
Funding Support and Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
References
- 1.Nazer B., Walters T.E., Dewland T.A., et al. Variable presentations and ablation sites for manifest nodoventricular/nodofascicular fibers. Circ Arrhythm Electrophysiol. 2019;12 doi: 10.1161/CIRCEP.119.007337. [DOI] [PubMed] [Google Scholar]
- 2.Hoffmayer K.S., Lee B.K., Vedantham V., et al. Variable clinical features and ablation of manifest nodofascicular/ventricular pathways. Circ Arrhythm Electrophysiol. 2015;8:117–127. doi: 10.1161/CIRCEP.114.001924. [DOI] [PubMed] [Google Scholar]
- 3.Cardona-Guarache R., Han F.T., Nguyen D.T., et al. Ablation of supraventricular tachycardias from concealed left-sided nodoventricular and nodofascicular accessory pathways. Circ Arrhythm Electrophysiol. 2020;13 doi: 10.1161/CIRCEP.119.007853. [DOI] [PubMed] [Google Scholar]
- 4.Ho S.Y. Anatomy of the atrioventricular junction, atrioventricular grooves, and accessory pathways. Card Electrophysiol Clin. 2020;12:437–445. doi: 10.1016/j.ccep.2020.07.001. [DOI] [PubMed] [Google Scholar]
- 5.Inoue S., Becker A.E. Posterior extensions of the human compact atrioventricular node: a neglected anatomic feature of potential clinical significance. Circulation. 1998;97:188–193. doi: 10.1161/01.cir.97.2.188. [DOI] [PubMed] [Google Scholar]