Abstract
Introduction
Neural mobilization (NM) is a physiotherapy technique involving the passive mobilization of limb nerve structures with the aim to attempt to restore normal movement and structural properties. In recent years, human studies have shown pain relief in various neuropathic diseases and other pathologies as a result of this technique. Improvement in the range of motion (ROM), muscle strength and endurance, limb function, and postural control were considered beneficial effects of NM. To determine which systems generate these effects, it is necessary to conduct studies using animal models. The objective of this study was to gather information on the physiological effects of NM on the peripheral and central nervous systems (PNS and CNS) in animal models.
Methods
The search was performed in Medline, Pubmed and Web of Science and included 8 studies according to the inclusion criteria.
Results
The physiological effects found in the nervous system included the analgesic, particularly the endogenous opioid pathway, the inflammatory, by modulation of cytokines, and the immune system.
Conclusion
On the basis of these results, we can conclude that NM physiologically modifies the peripheral and central nervous systems in animal models.
Keywords: physical therapy, animal models, neural mobilization, biomarkers, central nervous system, peripheral nervous system
1. Introduction
Neural mobilization (NM) is a physiotherapy procedure involving the passive mobilisation of limb nerve structures to restore normal movement and structural properties (1). Most research has been conducted using this technique in patients with chronic peripheral nerve pathologies who present with pain. Studies have shown a decrease in these symptoms in patients with cervical radiculopathy (2, 3), tension headache (4), cervical-brachialgia (5–7), sciatica (8), low back pain (9) and an increase in pain threshold in people with no pathology (10, 11). This technique also reduces pain caused by other pathologies that cause neuropathies, such as leprosy (12) or cancer (13), or due to other causes such as rheumatoid arthritis (14), osteoarthritis (15) and epicondylalgia (16).
Other effects of NM are increased ROM in subjects with (10, 17–20) and without pathology (3, 5, 21), changes in the muscular system, increasing strength (12, 15) and endurance (3), and increased recovery from fatigue (22). NM has also shown positive effects at a functional level by reducing disability in the affected limbs (3, 5, 6, 8, 12) and improving postural control in athletes (23). Finally, another phenomenon studied in cadavers has been the increased dispersion of intraneural fluid after the technique, which may be beneficial if intra-aneural edema is present (24, 25).
Even if these studies show that NM generates beneficial effects on different systems and subjects, research in humans does not allow us to describe which physiological mechanisms are involved in changes in pain perception and intensity, range of motion, and muscle strength, among others. To determine which systems are involved, it is necessary to look for basic research articles in which this technique has been used in animal models. In the literature, there are studies where physiotherapy techniques are applied to measure changes in biomarkers related to pain and inflammation and others to understand the processes involved in the changes produced by the techniques of this profession.
Suppose we use massage as an example and apply it to animal models. In this case, it has been studied to generate analgesic effects related to increased oxytocin in the periaqueductal gray matter (26) and changes in some genes that regulate inflammation (27). Another example that we can consider is passive joint mobilisations. They decrease pain by activating serotonergic and noradrenergic pathways (28, 29), whereas they decrease pro-inflammatory cytokines and increase anti-inflammatory cytokines (30, 31). The technique has also been studied to improve the repair of tissues such as bone (32) and cartilage (33, 34) by stimulating the tissues.
This systematic review aims to unify the information in the basic research literature on the physiological effects of NM on the peripheral and central nervous system (PNS and CNS) in animal models.
2. Methods
2.1. Search strategy
This review was performed following the guidelines of the Systematic Review Center for Laboratory Animal Experimentation (SYRCLE) (35) and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) principles (36). The protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO, CRD42022316225).
Two independent researchers performed the search (F.S. and L.M.-C.) in MEDLINE/PubMed and the Web of Science (WoS) between the 10th and 13th of February 2022 of articles published between January 1, 2012, and December 31, 2021. The search included the terms: “Neural mobilization OR Neurodynamics OR Nerve Mobilization” AND “Rats [MeSH] OR Mice [MeSH] OR Rabbits [MeSH] OR Cats [MeSH] OR Guinea Pigs [MeSH].” The search was limited to articles published only in English and performed in non-human species (other animals).
2.2. Study selection
For the study selection, two independent review authors (F.S. and L.M.-C.) screened titles and abstracts of retrieved documents to exclude irrelevant studies. After the duplicates were eliminated, abstracts were reviewed to identify eligible trials; at this stage, the inclusion and exclusion criteria were applied, and the selection was performed. Discrepancies between reviewers were resolved by discussion.
Studies meeting the following PICO criteria were selected: (i) Participants: rats, mice, rabbits, cats or guinea pigs with a model of neuropathic pain, (ii) Interventions: nerve mobilisation technique performed manually by an experimenter, (iii) Comparators: healthy controls and/or sham-operated animals, different intensity and frequency of interventions and (iv) Outcomes: central and/or peripheral biomarkers, pain-behavioral or other outcomes. The manuscripts selected included preclinical animal interventional studies.
Articles were excluded if they performed medical, veterinary studies, human studies or “in vitro” and “ex vivo” studies. They were also excluded if any drugs, invasive techniques, therapeutic exercise as the only therapy, or any bandages as treatment were applied. Systematic reviews, case reports and descriptive studies were excluded too. At least one control group had to be included.
2.3. Data extraction
Two independent reviewers (F.S. and L.M.-C.) extracted data from the selected studies. A third author was consulted in case of uncertainty (SV). The following data were extracted: (1) Authors and publication year, (2) Type of neuropathic pain model, (3) Groups, (4) Animal species, (5) Information about the intervention, (6) Outcomes.
2.4. Risk of bias and quality assessment
SYRCLE tool was used to analyse the risk of bias in each study (SV). This tool is based on Cochrane’s Risk of Bias tool for randomised clinical trials (RoB Tool) (37). It contains 10 items related to 6 types of bias (selection, performance, detection, attrition, reporting and others). The items were labelled as “yes” if they were free of risk of bias and “no” if they were not. When information was not reported, the risk of bias could not be discarded, and authors labelled the entry as “unclear.”
The methodological quality of the selected studies was evaluated by two independent authors (F.S. and S.V.) with the ARRIVE tool (38), consisting of 21 items to assess the reliability of the animal studies; the items were reported as “yes” (information included in the manuscript), “no” (information not included in the manuscript) or “X” (not applicable).
3. Results
3.1. Selection of the studies
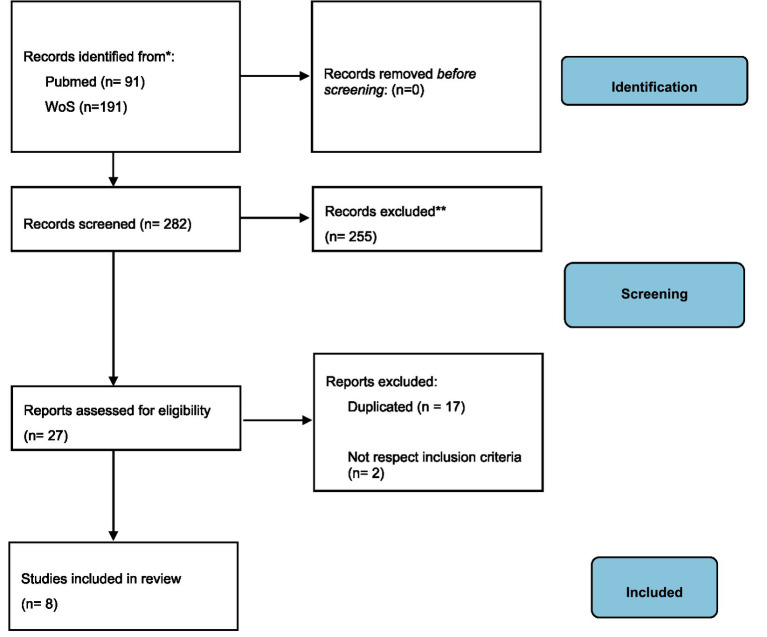
A total of 137 manuscripts were retrieved after the systematic search. After duplicate exclusion, 94 publications were assessed for eligibility. Of those, 85 were excluded because they did not meet the inclusion criteria. Finally, 8 articles were included in the systematic review. Figure 1 shows the flow diagram of the selection process.
Figure 1.
Flow Diagram PRISMA.
3.2. Study characteristics
Table 1 shows the methodological characteristics of the studies. 7 articles performed preclinical studies of neuropathic pain in male Wistar and one in male Sprague–Dawley rats (39). 5 of them used a chronic constriction injury (CCI) model in the sciatic nerve. The CCI injury model was described by Bennet and Xie (40) and in brief, it consists of the exposure and ligation of the sciatic nerve (4 ligatures at a spacing of 1 mm) with a 4.0 chromic gut (41–45). In 2 studies (46, 47) the median nerve compression (MNC) protocol described by Chen et al. (48), performing 4 ligatures around the median nerve, was used. Only in one study (39) diabetic neuropathy (DN) induced by streptozocin injection was developed in Sprague–Dawley rats.
Table 1.
Methodological characteristics of the selected studies.
| Author, year | Neuropathic Pain model | Groups | Animal sp. | Treatment(s) | Measurements |
|---|---|---|---|---|---|
| Santos et al. (2012) | NP CCI |
E1: (n = 6) CCI + NM E2: (n = 6) CCI S: (n = 6) Sham + NM N: (n = 6) |
Male Wistar Rats | NM SN 2 | NGF GFAP Mechanical Hyperalgesia Mechanical Allodynia Thermal Hyperalgesia |
| Marcioli et al. (2013) | NP MNC |
E1: (n = 6) MNC only E2: (n = 6) MNC + 1 min NM E3: (n = 6) MNC + 3 min NM |
Male Wistar Rats | NM MN | Mechanical Allodynia Fibre diameter Axon diameter Myelin sheath diameter |
| Santos et al. (2014) | NP CCI |
E1: (n = 5) CCI + NM E2: (n = 5) CCI S1: (n = 5) Sham + NM S2: (n = 5) Sham N: (n = 5) |
Male Wistar Rats | NM SN 2 | DOR KOR MOR Sciatic Functional Index Muscle Function |
| da Silva et al. (2015) | NP CCI |
E1: (n = 6) CCI + NM E2: (n = 6) CCI S: (n = 6) Sham + NM N: (n = 6) |
Male Wistar Rats | NM SN 2 | NGF MPZ Fibre diameter Axon diameter Myelin sheath diameter |
| Giardini et al. (2017) | NP CCI |
E1: (n = 5) CCI + NM E2: (n = 5) CCI N: (n = 5) |
Male Wistar Rats | NM SN 2 | BDNF GFAP OX-42 |
| Santos et al. (2018) | NP CCI |
E1: (n = 10) CCI + NM E2: (n = 10) CCI S1: (n = 10) Sham + NM S2: (n = 10) Sham N: (n = 10) |
Male Wistar Rats | NM SN 2 | Substance P TRPV1 DOR KOR MOR |
| Marcioli et al. (2018) | NP MNC |
E1: (n = 6) MNC only E2: (n = 6) MNC + 1 min NM E3: (n = 6) MNC + 3 min NM |
Male Wistar Rats | NM MN | NGF BDNF |
| Zhu et al. (2018) | DN | E: (n = 6) S: (n = 6) N: (n = 6) |
Male Sprague–Dawley | NM SN 2 | TNFα IL-1β |
BDNF, Brain-derived neurotropic factor; CCI, Chronic Constriction Injury; DN, Diabetic Neuropathy; DO, δ-opioid receptor; E, Experimental; GFAP, Glial Fibrillary Acidic Protein; IL-1β, Interleukin 1 beta; KOR, κ-opioid receptor; MNC, Median Nerve Compression; MOR, μ-opioid receptor; MPZ, Myelin Protein Zero; N, Naive; NGF, Neural Growth Factor; NM, Neural Mobilization; OX-42, Microglial Cell OX-42; S, Sham; SFI, Sciatic Functional Index; TNFα, Tumor Necrosis Factor Alpha; TRPV1, Transient Receptor Potential Vanilloid 1.
All the studies included at least one control group. In those cases where the CCI injury was performed, a sham group (nerve exposure without compression) and a naive group were used as controls (41–45). The MNC protocol without NM served as a control in the articles of Marcioli et al. (46, 47) and the diabetic neuropathy model included a sham (saline injection) and a naïve group (39). The sample size varied from 5 to 10 animals per group. A total of 192 animals were included in the studies.
Regarding the interventions, the NM protocol started 3 (46, 47, 49), 10 (39) or 14 (41–45) days after the neuropathic induction and consisted of repeated oscillations of the scapular limb (46, 47) or the ankle joint (39, 41–45, 49). The mobilisations were performed in a wide range of time, from 1 or 3 min (46, 47) to 10 min (39, 41–45, 49) and the duration of the treatment lasted from 10 days (41–47, 49) to 3 weeks (39).
3.3. Risk of bias and reporting quality
All the selected articles were assessed for six different types of risks of bias using SYRCLE tool Table 2. When information was reported, most of the studies (41, 43–46, 49) were free of selection bias, whereas one (39) was not for showing differences between animal groups at the baseline. None of the studies reported information about allocation generation and concealment. Concerning performance bias, none of the studies reported random housing, so those whose dependent variables could be affected by light or room temperature (pain, mostly) were not considered free of performance bias (39, 41, 46, 49). However, the rest of the articles were not performance-biased (42–47). Similarly, although investigator blinding was not reported in any study, outcome assessment was considered free of detection bias in most cases (39, 41, 42, 45–47, 49) since computer-based techniques were used. The attrition bias could not be studied since most of the studies did not report information about it, except for two studies (39, 41) which were not biased. Only one did show unexplained missing data and was considered likely to have attrition bias (45). When reported, all the articles but one (47) were free of reporting bias due to the use of thorough study protocols. Lastly, the authors considered 5 studies bias-free for other reasons (39, 41, 42, 44, 45). Only 3 studies (43, 46, 47) did show some concerns, mainly about study design or lack of data dispersion. In summary, most of the studies (41, 43–45, 47, 49) only showed one risk of bias, or two (39, 46) and (42) were free of any analysed bias when enough information was reported.
Table 2.
Risks of bias analysis of the selected studies using the SYRCLE tool.
| Selection bias | Performance bias | Detection bias | Attrition bias | Reporting bias | Other | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Study | 1. Sequence generation | 2. Baseline characteristics | 3. Allocation concealment | 4. Random housing | 5. Researchers or caregivers blinding | 6. Random outcome assessment | 7. Assessors blinding | 8. Incomplete outcome reporting | 9. Selective outcome reporting | 10. Other sources of bias |
| Santos et al. (2012) | Unclear | Yes | Unclear | No | Unclear | Unclear | Yes | Yes | Yes | Yes |
| Marcioli et al. (2013) | Unclear | Yes | Unclear | No | Unclear | Unclear | Yes | Unclear | Yes | No |
| Santos et al. (2014) | Unclear | Unclear | Unclear | Yes | Unclear | Unclear | Yes | Unclear | Yes | Yes |
| da Silva et al. (2015) | Unclear | Yes | Unclear | Yes | Unclear | Unclear | Unclear | Unclear | Yes | No |
| Giardini et al. (2017) | Unclear | Yes | Unclear | Yes | Unclear | Unclear | Unclear | Unclear | No | Yes |
| Santos et al. (2018) | Unclear | Yes | Unclear | Yes | Unclear | Unclear | Yes | No | Yes | Yes |
| Marcioli et al. (2018) | Unclear | Unclear | Unclear | Yes | Unclear | Unclear | Yes | Unclear | Unclear | No |
| Zhu et al. (2018) | Unclear | No | Unclear | No | Unclear | Unclear | Yes | Yes | Yes | Yes |
Items are labelled “yes” when are free of risk of bias, “no” when they are not, and “unclear” when information was not reported, and risk of bias cannot be discarded.
Table 3 summarises the reporting quality of the selected studies using the updated ARRIVE tool. In agreement with SYRCLE tool, there was a significant lack of information for several items (labelled as “no”). None of the studies reported information about allocation randomisation, investigators blinding or describing protocols to reduce suffering. Remarkably, experimental procedures were reported in all cases, providing detailed information about time, frequency and reasons for intervention. Moreover, in all cases, the background was enough and coherent, and the objectives and rationale were well scientifically explained. Also, animal handling and wellness are maintained across the studies as required in animal research to preserve their welfare and prevent or reduce their suffering during studies (ethics and husbandry).
Table 3.
Quality report of the selected studies using the updated ARRIVE tool.
| 1. Study design | 2. Sample size | 3. Inclusion and exclusion criteria | 4. Randomisation | 5. Blinding | 6. Outcome measures | 7. Statistical methods | 8. Experimental animals | 9. Experimental procedures | 10. Results | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1.a | 1.b | 2.a | 2.b | 3.a | 3.b | 3.c | 4.a | 4.b | 5.a | 6.a | 6.b | 7.a | 7.b | 8.a | 8.b | 9.a | 9.b | 9.c | 9.d | 10.a | 10.b | |
| Santos et al. (2012) | Yes | Yes | Yes | No | No | No | Yes | No | No | No | Yes | No | No | No | Yes | No | Yes | Yes | Yes | Yes | Yes | x |
| Marcioli et al. (2013) | Yes | Yes | No | No | No | No | Yes | No | No | No | Yes | No | No | Yes | No | No | Yes | Yes | Yes | Yes | Yes | x |
| Santos et al. (2014) | Yes | Yes | No | No | No | No | Yes | No | No | No | Yes | No | Yes | No | Yes | No | Yes | Yes | Yes | Yes | Yes | x |
| da Silva et al. (2015) | Yes | Yes | No | No | No | No | Yes | No | No | No | Yes | No | Yes | No | Yes | No | Yes | Yes | Yes | Yes | No | x |
| Giardini et al. (2017) | Yes | Yes | No | No | No | No | Yes | No | No | No | Yes | No | Yes | No | Yes | No | Yes | Yes | Yes | Yes | Yes | x |
| Santos et al. (2018) | Yes | Yes | No | No | No | No | Yes | No | No | No | Yes | No | Yes | No | No | No | Yes | Yes | Yes | Yes | Yes | x |
| Marcioli et al. (2018) | No | Yes | No | No | No | No | Yes | No | No | No | Yes | No | Yes | No | Yes | No | Yes | Yes | Yes | Yes | Yes | x |
| Zhu et al. (2018) | Yes | Yes | Yes | No | Yes | No | Yes | No | No | No | Yes | No | Yes | No | No | No | Yes | Yes | Yes | Yes | Yes | x |
| 11. Abstract | 12. Background | 13. Objectives | 14. Ethical statement | 15. Housing and husbandry | 16. Animal care and monitoring | 17. Interpretation/ scientific implications | 18. Generalisability/ translation | 19. Protocol registration | 20. Data access | 21. Declaration of interests | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 11. a | 12. a | 12. b | 13. a | 14. a | 15. a | 16. a | 16. b | 16. c | 17. a | 17. b | 18. a | 19. a | 20. a | 21. a | 21. b | |
| Santos et al. (2012) | Yes | Yes | Yes | Yes | Yes | Yes | No | No | No | Yes | No | Yes | No | Yes | Yes | No |
| Marcioli et al. (2013) | Yes | Yes | Yes | Yes | Yes | Yes | No | No | No | Yes | No | Yes | No | Yes | Yes | No |
| Santos et al. (2014) | Yes | Yes | Yes | Yes | Yes | Yes | No | No | No | Yes | No | Yes | No | Yes | Yes | No |
| da Silva et al. (2015) | Yes | Yes | Yes | Yes | Yes | Yes | No | No | No | Yes | No | No | No | Yes | Yes | No |
| Giardini et al. (2017) | yes | yes | no | yes | yes | yes | no | no | no | yes | no | yes | no | yes | yes | no |
| Santos et al. (2018) | Yes | Yes | Yes | Yes | Yes | Yes | No | No | No | Yes | No | Yes | No | Yes | Yes | Yes |
| Marcioli et al. (2018) | No | Yes | Yes | Yes | Yes | Yes | No | No | No | Yes | Yes | No | No | Yes | Yes | No |
| Zhu et al. (2018) | Yes | Yes | Yes | Yes | Yes | Yes | No | No | No | Yes | Yes | Yes | No | Yes | Yes | No |
Items are labelled “yes” when requirements are met by the publication, “no” when they are not and “x” if question is not applicable to the study.
3.4. Main outcomes and results
Table 4 shows the main results of the studies included in the review. Among the selected studies, only two performed NM on the upper limbs (46, 47) and the rest on the lower limbs (39, 41–45, 49).
Table 4.
Results of the selected studies.
| Author | Peripheral Biomarkers | Central Biomarkers | Pain-Behavioral Outcomes | Others |
|---|---|---|---|---|
| Santos et al. (2012) |
DRG ↓ NGF ↓ GFAP |
SC NGF: No differences ↓ GFAP |
↓ from 2nd session: Mechanical Hyperalgesia Mechanical Allodynia Thermal Hyperalgesia |
─ |
| Marcioli et al. (2013) | _ | _ | Mechanical Allodynia: No differences | No differences: Fibre diameter Axon diameter Myelin sheath diameter |
| Santos et al. (2014) | _ |
PAG ↑ DOR ↑ KOR MOR: No differences |
─ | ↑ SFI ↑ Muscle Function |
| da Silva et al. (2015) |
Nerve ↑ NGF ↑ MPZ |
_ | ─ | ↑ Fibre diameter ↑Axon diameter ↑ Myelin sheath diameter |
| Giardini et al. (2017) | _ |
Thalamus and PAG ↓ BDNF ↓ GFAP ↓ OX-42 |
─ | ─ |
| Santos et al. (2018) |
DRG ↓Substance P ↓TRPV1 ↑ MOR DOR: No differences KOR: No differences |
_ | ─ | ─ |
| Marcioli et al. (2018) |
Nerve NGF: No differences BDNF: No differences |
_ | ─ | ─ |
| Zhu et al. (2018) |
Nerve ↓ TNFα ↓ IL-1β |
_ | ↓ Mechanical Allodynia | ─ |
BDNF, Brain-derived neurotropic factor; DOR, δ-opioid receptor; DRG, Dorsal Root Ganglion; GFAP, Glial Fibrillary Acidic Protein; IL-1β, Interleukin 1 beta; KOR, κ-opioid receptor; MOR, μ-opioid receptor; MPZ, Myelin Protein Zero; NGF, Neural Growth Factor; OX-42, Microglial Cell OX-42; PAG, Periaqueductal Gray; SC, Spinal Cord; SFI, Sciatic Functional Index; TNFα, Tumor Necrosis Factor Alpha; TRPV1, Transient Receptor Potential Vanilloid 1.
The NM treatment induced changes in biomarkers at both central and peripheral levels when applied at least 10 days after the neuropathic pain induction protocol. Thus, in the CCI injury model, there was a decrease in Neural Growth Factor (NGF), Glial Fibrillary Acidic Protein (GFAP), substance P and Transient Receptor Potential Vanilloid 1 (TRPV1) and an increase of μ-opioid receptor (MOR) in dorsal root ganglion (39, 41, 45) after NM. In contrast, in the peripheral nerve, an increase of NGF and Myelin Protein Zero (MPZ) (43) and a decrease of Tumor Necrosis Factor Alpha (TNFα) and Interleukin 1 beta (IL-1β) (39) were shown. Others opioid receptors, DOR and KOR did not suffer changes in the dorsal root ganglion (45). Significant changes were found in the spinal cord, where there was a decrease in NGF levels (41) and periaqueductal grey and thalamus, showing an increase in opioid receptors DOR and KOR (42) and a decrease of Brain-derived neurotrophic factor (BNDF), GFAP and markers of Microglial Cell OX-42 (OX-42) levels (44). On the contrary, when the NM was applied only 3 days after the neuropathy induction, it did not change the peripheral nerve’s NGF and BDNF (47).
The same pattern was observed regarding pain-behavioral outcomes: both mechanical and thermal hyperalgesia and allodynia decreased when the nerve mobilisation was applied at least 10 days after the neuropathy induction (39, 41), but no differences with the control group were found in mechanical allodynia in the study of Marcioli et al. (46), where the mobilisation protocol started only 3 days after surgery.
The fibre diameter, axon diameter and myelin sheath diameter of the injured nerves were studied by Marcioli et al. (46), who did not find changes using the nerve mobilisation protocol applied 3 days after surgery, while da Silva et al. (43) found an increase in axon, sheath and myelin diameters when the NM protocol was applied 14 days after the CCI was performed.
4. Discussion
This review gathered information on the physiological effects of NM on the PNS and CNS. Our results show that there is medium to high evidence, considering that all studies were RCTs, but it has not been possible to perform a meta-analysis of the results.
Concerning bias and quality of studies, none of the studies provided information about allocation concealment and researchers’ blinding. Implementation of tools preventing the risk of bias.
According to the results of this systematic review, inflammation decreases when NM is applied 10 days after CCI, as shown by the reduction of most inflammatory molecules. GFAP is a marker of activated satellite glial cells in PNS, which increases after CCI and nerve ligation in rodents (50, 51). Substance P, IL-1β and TRPV1 also contribute to inflammatory responses related to rodent neuropathic pain (52–55). NGF appears to mediate chronic neuropathic pain and increases after CCI in rodents (56). However, its levels are reduced after NM only in the DRG and spinal cord, whereas the peripheral nerve remains unchanged.
Moreover, the increase in MPZ may be related to Schwann cell regeneration, nerve recovery, and remyelination. An increase in opioid receptors has been linked to higher tolerance to pain (57). Thus, the increase of MOR in the PNS observed after NM, along with the reduction of the inflammatory mediators listed above, may contribute to the analgesic effects of NM reported in the studies of this systematic review. These effects have not been found if NM was performed only 3 days after surgery, probably because the effects are not the same if it is an acute pathology phase.
Animal models of neuropathic pain have limitations, and their translation to humans is complex. However, it is well described how nerve damage-induced release of inflammatory mediators sensitises and activates nociceptors and contributes to chronic pain (58). Therefore, we hypothesized that the NM induces analgesia observed in patients (2–16), which may be mediated by the reduction of inflammatory mediators by glial cells and the activation of the opioid system.
The information found in this study agrees with a recent review of the effects of other physical therapy techniques on biomarkers related to neuropathic pain (59). The authors conclude that most physiotherapeutic interventions modulate the expression of molecular mediators of pain.
Finally, although NM has been shown to cause changes in the muscular system in humans (3, 12, 15, 22), no studies in animal models have examined the physiological mechanisms involved. This could be an area of research for future studies.
5. Conclusion
We conclude that NM changes the peripheral and central nervous systems of animal models. The physiological changes studied are related to pain modulation and include the endogenous opioid analgesic system at both the central and peripheral levels and inflammatory modulators at the central and peripheral levels. Another system involved in both the PNS and CNS is the immune system, which relates to and modulates the other two systems, analgesic and inflammatory. We suggest further investigation and focus on improving the quality of the studies following the ARRIVE criteria and finding if more systems are involved in the changes in muscles and other structures.
6. Limitations
There are some limitations to be considered when reading this study. First, we included only studies in English. Regarding the quality of the studies, none described the randomization of groups, blinding of investigators, or protocols to reduce animal suffering. Another significant limitation was that we could not perform a meta-analysis because the articles did not study the same outcomes. Finally, more research is needed to transfer the effects studied in these animal trials to humans.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
FS: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Writing – original draft, Writing – review & editing. SV: Data curation, Formal analysis, Methodology, Supervision, Writing – review & editing, Writing – original draft. LM-C: Conceptualization, Methodology, Writing – original draft.
Funding Statement
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2023.1289361/full#supplementary-material
References
- 1.Basson A, Olivier B, Ellis R, Coppieters M, Stewart A, Mudzi W. The effectiveness of neural mobilization for Neuromusculoskeletal conditions: a systematic review and meta-analysis. J Orthop Sports Phys Ther. (2017) 47:593–615. doi: 10.2519/jospt.2017.7117, PMID: [DOI] [PubMed] [Google Scholar]
- 2.Ayub A, Osama M, Ahmad S. Effects of active versus passive upper extremity neural mobilization combined with mechanical traction and joint mobilization in females with cervical radiculopathy: a randomized controlled trial. J Back Musculoskelet Rehabil. (2019) 32:725–30. doi: 10.3233/BMR-170887, PMID: [DOI] [PubMed] [Google Scholar]
- 3.Kim DG, Chung SH, Jung HB. The effects of neural mobilization on cervical radiculopathy patients’ pain, disability, ROM, and deep flexor endurance. J Back Musculoskelet Rehabil. (2017) 30:951–9. doi: 10.3233/BMR-140191, PMID: [DOI] [PubMed] [Google Scholar]
- 4.Ferragut-Garcías A, Plaza-Manzano G, Rodríguez-Blanco C, Velasco-Roldán O, Pecos-Martín D, Oliva-Pascual-Vaca J, et al. Effectiveness of a treatment involving soft tissue techniques and/or neural mobilization techniques in the Management of Tension-Type Headache: a randomized controlled trial. Arch Phys Med Rehabil. (2017) 98:211–219.e2. doi: 10.1016/j.apmr.2016.08.466 [DOI] [PubMed] [Google Scholar]
- 5.Sanz DR, Solano FU, López DL, Corbalan IS, Morales CR, Lobo CC. Effectiveness of median nerve neural mobilization versus oral ibuprofen treatment in subjects who suffer from cervicobrachial pain: a randomized clinical trial. Arch Med Sci. (2018) 14:871–9. doi: 10.5114/aoms.2017.70328, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rodríguez-Sanz D, Calvo-Lobo C, Unda-Solano F, Sanz-Corbalán I, Romero-Morales C, López-López D. Cervical lateral glide neural mobilization is effective in treating Cervicobrachial pain: a randomized waiting list controlled clinical trial. Pain Med. (2017) 18:2492–503. doi: 10.1093/pm/pnx011 [DOI] [PubMed] [Google Scholar]
- 7.Rodríguez-Sanz D, López-López D, Unda-Solano F, Romero-Morales C, Sanz-Corbalán I, Beltran-Alacreu H, et al. Effects of median nerve neural mobilization in treating Cervicobrachial pain: a randomized waiting list-controlled clinical trial. Pain Pract. (2018) 18:431–42. doi: 10.1111/papr.12614, PMID: [DOI] [PubMed] [Google Scholar]
- 8.Almeida RSD, Machado E, Yamato TP, Santos De Melo L, Nogueira LAC. Pragmatic neural tissue management improves short-term pain and disability in patients with sciatica: a single-arm clinical trial. J Man Manip Ther. (2019) 27:208–14. doi: 10.1080/10669817.2019.1580420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alshami AM, Alghamdi MA, Abdelsalam MS. Effect of neural mobilization exercises in patients with low Back-related leg pain with peripheral nerve sensitization: a prospective, controlled trial. J Chiropr Med. (2021) 20:59–69. doi: 10.1016/j.jcm.2021.07.001, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Martins C, Pereira R, Fernandes I, Martins J, Lopes T, Ramos L, et al. Neural gliding and neural tensioning differently impact flexibility, heat and pressure pain thresholds in asymptomatic subjects: a randomized, parallel and double-blind study. Phys Ther Sport. (2019) 36:101–9. doi: 10.1016/j.ptsp.2019.01.008 [DOI] [PubMed] [Google Scholar]
- 11.Beltran-Alacreu H, Jiménez-Sanz L, Fernández Carnero J, La Touche R. Comparison of Hypoalgesic effects of neural stretching vs neural gliding: a randomized controlled trial. J Manip Physiol Ther. (2015) 38:644–52. doi: 10.1016/j.jmpt.2015.09.002 [DOI] [PubMed] [Google Scholar]
- 12.Véras LST, Vale RGDS, Mello DBD, Castro JAFD, Lima V, Trott A, et al. Electromyography function, disability degree, and pain in leprosy patients undergoing neural mobilization treatment. Rev Soc Bras Med Trop. (2012) 45:83–8. doi: 10.1590/S0037-86822012000100016, PMID: [DOI] [PubMed] [Google Scholar]
- 13.Casanova-García C, Lerma Lara S, Pérez Ruiz M, Ruano Domínguez D, Santana SE. Non-pharmacological treatment for neuropathic pain in children with cancer. Med Hypotheses. (2015) 85:791–7. doi: 10.1016/j.mehy.2015.10.007, PMID: [DOI] [PubMed] [Google Scholar]
- 14.Lau YN, Ng J, Lee SY, Li LC, Kwan CM, Fan SM, et al. A brief report on the clinical trial on neural mobilization exercise for joint pain in patients with rheumatoid arthritis. Z Rheumatol. (2019) 78:474–8. doi: 10.1007/s00393-018-0521-7 [DOI] [PubMed] [Google Scholar]
- 15.Villafañe JH, Cleland JA, Fernández-de-Las-Peñas C. The effectiveness of a manual therapy and exercise protocol in patients with thumb carpometacarpal osteoarthritis: a randomized controlled trial. J Orthop Sports Phys Ther. (2013) 43:204–13. doi: 10.2519/jospt.2013.4524, PMID: [DOI] [PubMed] [Google Scholar]
- 16.Arumugam V, Selvam S, MacDermid JC. Radial nerve mobilization reduces lateral elbow pain and provides short-term relief in computer users. Open Orthop J. (2014) 8:368–71. doi: 10.2174/1874325001408010368, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nunes MK, Dos Santos GF, Silva DCM, de Freitas ACM, Henriques IF, Andrade PM, et al. Acute effects of neural mobilization and infrared on the mechanics of the median nerve. J Phys Ther Sci. (2016) 28:1720–3. doi: 10.1589/jpts.28.1720, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Neal Hanney R, Ridehalgh C, Dawson A, Lewis D, Kenny D. The effects of neurodynamic straight leg raise treatment duration on range of hip flexion and protective muscle activity at P1. J Man Manip Ther. (2016) 24:14–20. doi: 10.1179/2042618613Y.0000000049, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sharma S, Balthillaya G, Rao R, Mani R. Short term effectiveness of neural sliders and neural tensioners as an adjunct to static stretching of hamstrings on knee extension angle in healthy individuals: a randomized controlled trial. Phys Ther Sport. (2016) 17:30–7. doi: 10.1016/j.ptsp.2015.03.003 [DOI] [PubMed] [Google Scholar]
- 20.Beneciuk JM, Bishop MD, George SZ. Effects of upper extremity neural mobilization on thermal pain sensitivity: a sham-controlled study in asymptomatic participants. J Orthop Sports Phys Ther. (2009) 39:428–38. doi: 10.2519/jospt.2009.2954, PMID: [DOI] [PubMed] [Google Scholar]
- 21.Calvo-Lobo C, Unda-Solano F, López-López D, Sanz-Corbalán I, Romero-Morales C, Palomo-López P, et al. Is pharmacologic treatment better than neural mobilization for cervicobrachial pain? A randomized clinical trial. Int J Med Sci. (2018) 15:456–65. doi: 10.7150/ijms.23525, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kim MK, Cha HG, Ji SG. The initial effects of an upper extremity neural mobilization technique on muscle fatigue and pressure pain threshold of healthy adults: a randomized control trial. J Phys Ther Sci. (2016) 28:743–6. doi: 10.1589/jpts.28.743, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ferreira J, Bebiano A, Raro D, Martins J, Silva AG. Comparative effects of tensioning and sliding neural mobilization on static postural control and lower limb hop testing in football players. J Sport Rehabil. (2019) 28:840–6. doi: 10.1123/jsr.2017-0374, PMID: [DOI] [PubMed] [Google Scholar]
- 24.Brown CL, Gilbert KK, Brismee JM, Sizer PS, Roger James C, Smith MP. The effects of neurodynamic mobilization on fluid dispersion within the tibial nerve at the ankle: an unembalmed cadaveric study. J Man Manip Ther. (2011) 19:26–34. doi: 10.1179/2042618610Y.0000000003, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gilbert KK, Roger James C, Apte G, Brown C, Sizer PS, Brismée JM, et al. Effects of simulated neural mobilization on fluid movement in cadaveric peripheral nerve sections: implications for the treatment of neuropathic pain and dysfunction. J Man Manip Ther. (2015) 23:219–25. doi: 10.1179/2042618614Y.0000000094, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fritschy JM, Sarter M. Repeated massage-like stimulation induces long-term effects on nociception: contribution of oxytocinergic mechanisms. Eur J Neurosci. (2009) 29:868. doi: 10.1111/j.1460-9568.2009.06687.x [DOI] [PubMed] [Google Scholar]
- 27.Waters-Banker C, Butterfield TA, Dupont-Versteegden EE. Immunomodulatory effects of massage on nonperturbed skeletal muscle in rats. J Appl Physiol. (2014) 116:164–75. doi: 10.1152/japplphysiol.00573.2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Skyba DA, Radhakrishnan R, Rohlwing JJ, Wright A, Sluka KA. Joint manipulation reduces hyperalgesia by activation of monoamine receptors but not opioid or GABA receptors in the spinal cord. Pain. (2003) 106:159–68. doi: 10.1016/S0304-3959(03)00320-8, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Martins DF, Mazzardo-Martins L, Cidral-Filho FJ, Gadotti VM, Santos ARS. Peripheral and spinal activation of cannabinoid receptors by joint mobilization alleviates postoperative pain in mice. Neuroscience. (2013) 255:110–21. doi: 10.1016/j.neuroscience.2013.09.055, PMID: [DOI] [PubMed] [Google Scholar]
- 30.Ferretti M, Srinivasan A, Deschner J, Gassner R, Baliko F, Piesco N, et al. Anti-inflammatory effects of continuous passive motion on meniscal fibrocartilage. J Orthop Res. (2005) 23:1165–71. doi: 10.1016/j.orthres.2005.01.025, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ferretti M, Gassner R, Wang Z, Perera P, Deschner J, Sowa G, et al. Biomechanical signals suppress proinflammatory responses in cartilage: early events in experimental antigen-induced arthritis. J Immunol. (2006) 177:8757–66. doi: 10.4049/jimmunol.177.12.8757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Feehan LM, Tang CS, Oxland TR. Early controlled passive motion improves early fracture alignment and structural properties in a closed extra-articular metacarpal fracture in a rabbit model. J Hand Surg. (2007) 32:200–8. doi: 10.1016/j.jhsa.2006.11.004, PMID: [DOI] [PubMed] [Google Scholar]
- 33.Chang NJ, Lin CC, Li CF, Wang DA, Issariyaku N, Yeh ML. The combined effects of continuous passive motion treatment and acellular PLGA implants on osteochondral regeneration in the rabbit. Biomaterials. (2012) 33:3153–63. doi: 10.1016/j.biomaterials.2011.12.054, PMID: [DOI] [PubMed] [Google Scholar]
- 34.Chang NJ, Lin CC, Li CF, Su K, Yeh ML. The effect of osteochondral regeneration using polymer constructs and continuous passive motion therapy in the lower weight-bearing zone of femoral trocheal groove in rabbits. Ann Biomed Eng. (2013) 41:385–97. doi: 10.1007/s10439-012-0656-7, PMID: [DOI] [PubMed] [Google Scholar]
- 35.Hooijmans CR, Rovers MM, de Vries RB, Leenaars M, Ritskes-Hoitinga M, Langendam MW. SYRCLE’s risk of bias tool for animal studies. BMC Med Res Methodol. (2014) 14:43. doi: 10.1186/1471-2288-14-43, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. (2011) 343:d5928. doi: 10.1136/bmj.d5928, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Du Sert NP, Ahluwalia A, Alam S, Avey MT, Baker M, Browne WJ, et al. Reporting animal research: explanation and elaboration for the ARRIVE guidelines 2.0. PLoS Biol. (2020) 18:e3000411. doi: 10.1371/journal.pbio.3000411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhu GC, Tsai KL, Chen YW, Hung CH. Neural mobilization attenuates mechanical allodynia and decreases Proinflammatory cytokine concentrations in rats with painful diabetic neuropathy. Phys Ther. (2018) 98:214–22. doi: 10.1093/ptj/pzx124 [DOI] [PubMed] [Google Scholar]
- 40.Bennett GJ, Xie YK. A peripheral mononeuropathy in rat that produces disorders of pain sensation like those seen in man. Pain. (1988) 33:87–107. doi: 10.1016/0304-3959(88)90209-6, PMID: [DOI] [PubMed] [Google Scholar]
- 41.Santos FM, Silva JT, Giardini AC, Rocha PA, Achermann APP, Alves AS, et al. Neural mobilization reverses behavioral and cellular changes that characterize neuropathic pain in rats. Mol Pain. (2012) 8:1744-8069-8-57. doi: 10.1186/1744-8069-8-57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Santos FM, Grecco LH, Pereira MG, Oliveira ME, Rocha PA, Silva JT, et al. The neural mobilization technique modulates the expression of endogenous opioids in the periaqueductal gray and improves muscle strength and mobility in rats with neuropathic pain. Behav Brain Funct. (2014) 10:19. doi: 10.1186/1744-9081-10-19, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.da Silva JT, Santos FMD, Giardini AC, Martins DDO, de Oliveira ME, Ciena AP, et al. Neural mobilization promotes nerve regeneration by nerve growth factor and myelin protein zero increased after sciatic nerve injury. Growth Factors. (2015) 33:8–13. doi: 10.3109/08977194.2014.953630, PMID: [DOI] [PubMed] [Google Scholar]
- 44.Giardini AC, Dos Santos FM, da Silva JT, de Oliveira ME, Martins DO, Chacur M. Neural mobilization treatment decreases glial cells and brain-derived neurotrophic factor expression in the central nervous system in rats with neuropathic pain induced by CCI in rats. Pain Res Manag. (2017) 2017:1–9. doi: 10.1155/2017/7429761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Santos FM, Silva JT, Rocha IRC, Martins DO, Chacur M. Non-pharmacological treatment affects neuropeptide expression in neuropathic pain model. Brain Res. (2018) 1687:60–5. doi: 10.1016/j.brainres.2018.02.034, PMID: [DOI] [PubMed] [Google Scholar]
- 46.Marcioli MAR, Coradini JG, Kunz RI, Ribeiro LDFC, Brancalhão RMC, Bertolini GRF. Nociceptive and histomorphometric evaluation of neural mobilization in experimental injury of the median nerve. Sci World J. (2013) 2013:476890: 1–6. doi: 10.1155/2013/476890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Marcioli MAR, Silva JLDC, Ribeiro LDFC, Brancalhão RMC, Bertolini GRF. Neurotrophin expression and histomorphometric evaluation in Wistar rats subjected to neural mobilization after compression of the median nerve. Rev Bras Ortop. (2018) 53:276–80. doi: 10.1016/j.rbo.2017.03.019, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chen JJ, Lue JH, Lin LH, Huang CT, Chiang RPY, Chen CL, et al. Effects of pre-emptive drug treatment on astrocyte activation in the cuneate nucleus following rat median nerve injury. Pain. (2010) 148:158–66. doi: 10.1016/j.pain.2009.11.004, PMID: [DOI] [PubMed] [Google Scholar]
- 49.Bertolini GRF, Silva TS, Trindade DL, Ciena AP, Carvalho AR. Neural mobilization and static stretching in an experimental sciatica model: an experimental study. Braz J Phys Ther. (2009) 13:493–8. doi: 10.1590/S1413-35552009005000062 [DOI] [Google Scholar]
- 50.Wu JR, Chen H, Yao YY, Zhang MM, Jiang K, Zhou B, et al. Local injection to sciatic nerve of dexmedetomidine reduces pain behaviors, SGCs activation, NGF expression and sympathetic sprouting in CCI rats. Brain Res Bull. (2017) 132:118–28. doi: 10.1016/j.brainresbull.2017.04.016, PMID: [DOI] [PubMed] [Google Scholar]
- 51.Li J, Ouyang Q, Chen CW, Chen QB, Li XN, Xiang ZH, et al. Neuron-derived ADAM10 production stimulates peripheral nerve injury-induced neuropathic pain by cleavage of E-cadherin in satellite glial cells. Pain Med. (2017) 18:1752–66. doi: 10.1093/pm/pnw316 [DOI] [PubMed] [Google Scholar]
- 52.Jiang BC, Ding TY, Guo CY, Bai XH, Cao DL, Wu XB, et al. NFAT1 orchestrates spinal microglial transcription and promotes microglial proliferation via c-MYC contributing to nerve injury-induced neuropathic pain. Adv Sci. (2022) 9:e2201300. doi: 10.1002/advs.202201300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Li YS, Xi Y, Li XJ, Leng CL, Jia MM, Zhang WK, et al. Up-regulation of the biosynthesis and release of substance P through Wnt/β-catenin Signaling pathway in rat dorsal root ganglion cells. PLoS One. (2015) 10:e0129701. doi: 10.1371/journal.pone.0129701, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ma Y, Deng Q, Li S, Chen M, Jin B, Wang M. TRPV1, targeted by miR-338-3p, induces neuropathic pain by interacting with NECAB2. J Mol Neurosci. (2021) 71:55–65. doi: 10.1007/s12031-020-01626-4, PMID: [DOI] [PubMed] [Google Scholar]
- 55.Wang C, Gu L, Ruan Y, Gegen T, Yu L, Zhu C, et al. Pirt together with TRPV1 is involved in the regulation of neuropathic pain. Neural Plast. (2018) 2018:1–10. doi: 10.1155/2018/4861491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.da Silva JT, Evangelista BG, Venega RAG, Seminowicz DA, Chacur M. Anti-NGF treatment can reduce chronic neuropathic pain by changing peripheral mediators and brain activity in rats. Behav Pharmacol. (2019) 30:79–88. doi: 10.1097/FBP.0000000000000422, PMID: [DOI] [PubMed] [Google Scholar]
- 57.Vicario N, Denaro S, Turnaturi R, Longhitano L, Spitale FM, Spoto S, et al. Mu and Delta opioid receptor targeting reduces Connexin 43-based Heterocellular coupling during neuropathic pain. Int J Mol Sci. (2022) 23:5864. doi: 10.3390/ijms23115864, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Springer Link (n.d.) Status of immune mediators in painful neuropathies. Available at: https://link.springer.com/article/10.1007/s11916-008-0029-y [DOI] [PubMed]
- 59.Matesanz-García L, Schmid AB, Cáceres-Pajuelo JE, Cuenca-Martínez F, Arribas-Romano A, González-Zamorano Y, et al. Effect of physiotherapeutic interventions on biomarkers of neuropathic pain: a systematic review of preclinical literature. J Pain. (2022) 23:1833–55. doi: 10.1016/j.jpain.2022.06.007, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.