Abstract
Small bowel internal hernias (IHs), a rare cause of small bowel occlusion (SBO) and small bowel strangulation, while more commonly seen in young adults, can also affect elderly patients and pose a significant diagnostic challenge due to their nonspecific symptoms. In most cases, laparotomy was used to diagnose IHs. However, multidetector computed tomography (MDCT) is usually the best imaging tool to use in the emergency setting for the diagnosis of IHs. An 83-year-old man was admitted to emergency with acute abdominal pain and a coffee-ground vomitus. The abdominal MDCT showed a clustered-like appearance of proximal jejunal loops at the level of the Treitz ligament with the absence of transit of the medium water-soluble iodine oral contrast agent (Gastrografin). Mesenteric edema was also present with initial suffering of the intestinal wall. A left paraduodenal hernia (LPDH) with strangulation was suspected following the radiological report. The emergency laparotomy revealed about 20 cm of proximal jejunal loops herniated through a 3 cm wide hernia orifice (HO) along the Treitz ligament, at the level of Landzert fossa, located in the confluence of the descending mesocolon, posterior to the inferior mesenteric vein (IMV) and confirming the LPDH. The patient was discharged in good condition some days later. IHs do not have sufficient coverage in literature, especially in cases regarding elderly patients, however, they can be a cause of SBO in people older than 80 years of age. Radiologists and surgeons should be aware of the anatomical aspects of the IHs.
Keywords: Internal hernia; Small bowel obstruction; Emergency, Multidetector computed tomography; Left paraduodenal hernia; Emergency laparotomy
Introduction
As the world gradually recovers from the COVID-19 pandemic, healthcare professionals are observing a resurgence of rare conditions in the elderly population [1].
Internal hernias (IHs) are characterized by the protrusion of abdominal viscera, particularly small bowel loops, through peritoneal or mesenteric apertures. While most IHs have a congenital origin, acquired forms can occur due to previous surgeries. They represent a rare cause of acute abdomen as a result of small bowel obstruction (SMO) and small bowel strangulation [2–5]. Due to the predominance of congenital origin, most cases are diagnosed in young adults until the fourth decade. Occurrence in elderly patients (> 70 years) is very rare and occurrence in patients over 80 years old is usually under-reported [6–10]. These conditions represent the 5.8% of all small bowel obstruction (SBO) and carry a high mortality rate [2–5,11,12].
Case presentation
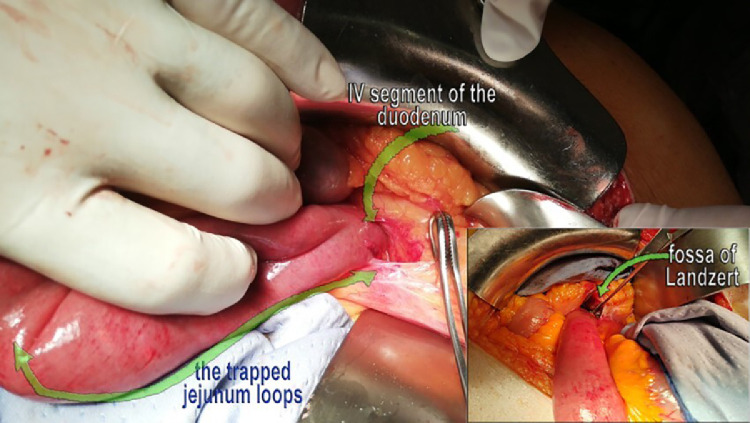
An 83-year-old man was admitted to the emergency room of our Hospital with acute abdominal pain and coffee-ground vomitus. The patient had no history of previous surgeries but had a medical history of arterial hypertension. Clinical examination revealed tenderness on deep palpation of the left flank. Laboratory results indicated decreased hemoglobin level (10.9 g/dL) (normal value range 13-17 g/dL) and hematocrit level (31.7%) (normal value range 40%-52%) with normal value of the mean cell volume (MCV) (87.8 Fl) (normal value range 82-96 Fl). The other laboratory values were within the normal limits. Because of the low hemoglobin values, an urgent gastroscopy was performed that showed gastric stagnation. The patient was initially treated with hydration, electrolyte replacement, and a nasogastric tube. The abdomen multidetector computed tomography (MDCT) with contrast administration revealed a marked distended stomach and clustered-like appearance of proximal jejunal loops with thickened walls at the level of the Treitz ligament. These findings were well visible on the coronal plane (Fig. 1A). No signs of necrosis or ischemia were initially visible. An anteromedial displacement of the descending colon was also present. However, the patient's symptoms worsened and a few hours later an additional MDCT with water-soluble iodine contrast agent (Gastrografin) confirmed the absence of transit of the oral contrast medium, highlighting a more delineated sac-like mass appearance of the previous small bowel loops at the level of the duodenal-jejunal region (Fig. 1B). The other intestinal loops were collapsed. A mesenteric edema was also present as a sign of vascular suffering of the intestinal wall. A left paraduodedenal hernia (LPDH) was diagnosed and soon after the surgical team was informed. Subsequently, an emergency laparotomy was promptly performed, and it revealed about 20 cm of proximal jejunal loops herniated through a 3 cm wide hernia orifice (HO) along the Treitz ligament, at the level of Landzert fossa, located in the confluence of the descending mesocolon, posterior to the inferior mesenteric vein (IMV) and confirming the LPDH (Fig. 2).
Fig 1.
The MDCT made in emergency. In image (A) clustered jejunal loops near the descending colon are well visible on coronal plane and behind the tail of pancreas; in image (B) the clustered jejunal loops described looked like a sac-like mass with an interruption of the Gastrographin transit in the MDCT carried out 6 hours after the first examination.
Fig 2.
The surgical pictures showing in the image (A) the jejunal loops trapped (green long curve arrow) at the level of Landzert fossa, that was laterally to the fourth part of the duodenum (short green curve arrow).
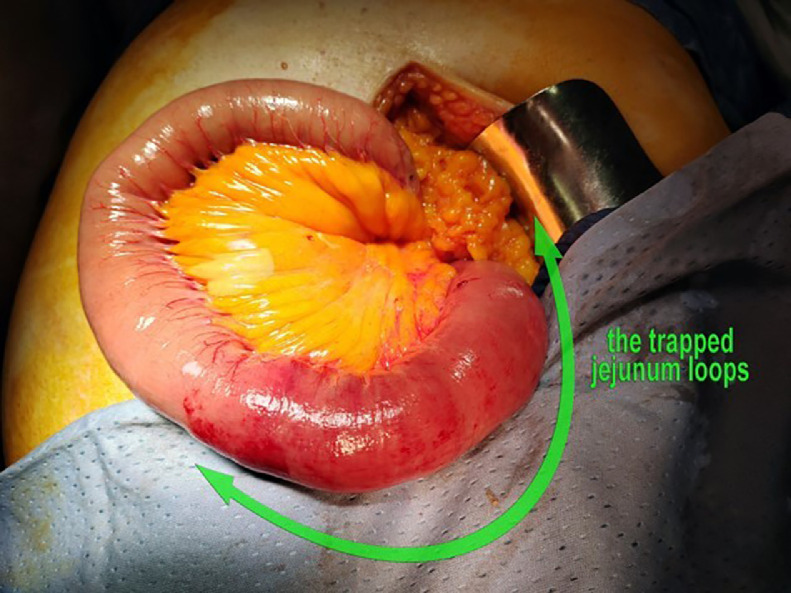
The intestinal walls were pale as a sign of ischemic sufferance but no sign of intestinal necrosis was found (Fig. 3). The LPDH was reduced and the HO was closed. The patient had a smooth postoperative recovery and was discharged 5 days later.
Fig 3.
This image describes the closed U loops appearance of the proximal jejunal bowels.
Discussion
Abdominal Internal hernias (IHs) are a rare cause of abdominal obstruction in older population. In fact, they are more frequently found in the pediatric population and young adults because of the congenital origin of the presence of peritoneal attachment anomalies and anatomical foramina or recesses in which small bowel loops could herniate [2–14]. However, their incidence is increasing, in particular when considering the acquired forms. This is, related to the increase of bariatric surgeries, among others [15]. IHs are usually classified on the base of the anatomic location of the IH orifice, following the Welch classification that divides them into 8 types [2–4] (Table 1).
Table 1.
This table reports the main types of IHs, based on the location of the anatomic hernia orifice (HO) and in order of frequencies on the base of the current literature [2], [3], [4].
| Type of Internal Hernia | Frequency | Anatomic HO Location |
|---|---|---|
Paraduodenal Internal Hernia
|
53%-55% | Duodenal-djunal area |
| 25% 75% |
|
|
| Pericecal Hernia | 13% | Ileo-cecal recesses |
| Foramen of Winslow Hernia | 8% | Foramen of Winslow |
| Transmesenteric Hernia | 8% | Ligament of Treitz and Ileo-cecal junction |
| Roux –en-Y anastomosis related Hernias | 0.2%-9% | Surgical defects in the transverse mesocolon, jejunojejunostomy, Petersen defect |
| Sigmoid-mesocolon related Hernias | 6% | Intersigmoid fossa |
| Supravescical and pelvic internal Hernia | 6% | Supravescical fossa,Perirectal Fossa and Douglas Fossa |
| Transomental Hernia | 1%-4% | Abnormal defect of the greater omentum |
PDHs were firstly described by Neubauer in 1756 and by Treitz, in 1857 [9]. The latter made the first scientific description, hypothesizing the pathological mechanisms at the origin of the development of PDHs. PDHs consist of small bowel herniations through the peritoneal sac near the duodenum-jejunal area. They are the most common type of IHs and they are usually divided into two main groups: the right (RPDH) and left LPDH paraduodenal hernia [2–13,16]. The LPDH is the most frequent with the HO typically occurring at the level of the Landzert fossa [2,5,11]. The Landzert fossa is an unusual peritoneal defect, present in 2% of the population, and located lateral to the fourth part of the duodenum, posterior to the IMV and the ascending branch of the ascending left colic artery (LCA) [2,11,16]. It also extends behind the descending mesocolon [2,11,16–19]. This anatomical region is the crossroad between the descending mesocolon, transverse mesocolon, and small bowel mesentery [11,17,18]. The IMV and the ascending LCA are the most important vascular landmarks. In fact, when the hernial sac is located in the Landzert fossa, it is usually formed by the descending mesocolon and part of IMV is in the anterior wall [2–5,11,16,17].
PDHs are usually congenital and caused by a malrotation of the mid-gut and they lead to an incomplete fusion of the retroperitoneum [17,18]. The LPHs are usually caused by the unsuccessful fusion of part of the descending mesocolon to the posterior peritoneum [11,17,18].
PDHs are three times more frequent in men than in women [2,17,18]. There were only 5 documented cases of LPDH developed in patients older than 80 years of age [6–10] (Table 2). There was, however, a female prevalence and only one published case in recent years [10].
Table 2.
This table reports previously published cases of LPDHs in people older than 80 years of age, describing sex, diagnostic tools, major complications, type of surgical intervention, and outcome.
| Author/Reference | Year | Sex | Age | Diagnostic imaging | Complications | Surgical intervention | Outcome |
|---|---|---|---|---|---|---|---|
| Catalano et al. [6] | 2004 | M | 82 | MDCT | Necrosis | Laparatomy | Survived |
| Zonca et al. [7] | 2008 | F | 80 | Abdominal X ray | Necrosis | Laparatomy | Survived |
| Uchiyama et al. [8] | 2009 | F | 80 | MDCT | No major complications | Laparoscopy | Survived |
| Suwanthanma et al. [9] | 2015 | M | 80 | MDCT | Necrosis | Laparatomy | Survived |
| Fernandes et al. [10] | 2022 | F | 80 | MDCT | Ischemic damage | Laparatomy | Survived |
Imaging with MDCT continues to play a crucial role in the diagnosis of IHs for its rapidity and for its panoramic view through multiplanar visualizations[2–13,17–19]. On MDCT, LPDHs usually appear as an encapsulated circumscribed mass of jejunal loops in the left quadrant, lateral to ascending duodenum or just above and exterior to the ligament of Treitz and posterior to the IVM that could be displaced upward [2–5]. On an enhanced MDCT, the major IHs vascular complications, such as small bowel incarcerations, can be recognized and it is possible to stage the ischemic suffering, till the necrosis and small bowel perforations [2–5,14]. The vascular damages usually associated with IHs are caused by small bowel strangulations that primarily involve the venous return causing hemorrhagic congestion. It is usually shown in a MDCT with an increased thickness of the walls with “target sign,” hyperdensity in the noncontrastgraphic phase and lack of diminished enhancement after the contrast administration [14]. Mesenteric congestion generally appears earlier in vascular strangulations. Afterward, if the small bowel incarceration persists, the arterial damages with ischemia become prevalent and it is shown on CT scan as thin bowel's walls, pneumatosis, and absence of contrast medium. It can worsen till necrosis and perforations [14]. Nevertheless, an integrated radiological approach with the use of oral radiopaque contrast (Gastrographin) on an MDCT can be very useful for the management of SBO, especially for those related to adhesions, in which Gastrographin, as an hyper-osmolar agent, can also have a therapeutic role [20]. The early use of Gastrographin in these cases is recommended especially for patients who do not require emergency surgery. However, when Gastrographin is not able to transit and in cases in which it is not effective, surgical intervention is recommended within 72 hours [20]. MDCT makes it possible to incidentally detect asymptomatic PDHs and in some cases PDHs could reduce spontaneously [21].
The surgical approaches usually depend on the SBO onset, the absence/presence of complications and the experience of the surgical team [11,19,[22], [23]–24]. The laparoscopic approach is usually associated with reduced morbidity, postoperative pain, and length of hospital stay and it is usually adopted when there are no complications [10,22–24]. Afterward, the mesenteric defects are usually closed with nonabsorbable sutures or mesh [17,19,22–24]. However, in cases of necrosis and perforations or in cases of significant suspicion of ischemic changes, the laparotomy approach is preferred, because in these cases the laparoscopy becomes more difficult and increases the risk of iatrogenic injuries [11,17,19]. In the cases previously published, laparotomy was frequently used because in often, at surgical evaluation, there was already a small bowel infarction [6,9–11]. In our cases, our surgeons decided on laparotomy because they suspected ischemic complications. This also consented to rule out other causes of SBO and to consider that the surgical team was not completely confident with advanced laparoscopic techniques in these situations. In fact, in some cases, there is also a discrepancy between the imaging findings on MDCT and the results found by surgeons after laparotomy. In the study by Surel et al. [25], the diagnosis of IHs made by radiologists following MDCT was confirmed by laparotomy in only 37% of cases. The most doubtful diagnosis following MDCT was with SBO caused by adhesions that were mistaken for IHs. Therefore, diagnosis of IHs continue to be a challenge for clinicians and radiologists. A multilevel evaluation should be preferred taking into account patient's history, a physical examination, laboratory tests and radiological findings. Nevertheless, MDCT remains the diagnostic tool to prefer when IHs evaluations have to be done urgently.
Conclusion
IHs could pose diagnostic challenges due to their nonspecific manifestations. On the other hand, in an emergency setting, it is difficult to suspect them in elderly patients as they generally affect younger people. Nevertheless, MDCT represents the primary imaging modality to detect and diagnose an IH. The presence of small bowels clusters on CT with a closed configuration should raise the suspicion of an IH. We want to emphasize that establishing a correct diagnosis preoperatively is fundamental because it can improve patient management and reduce both the length of hospitalization and the risk of death, mainly in the elderly, who might have a lot of comorbidities. Radiologists and surgeons should be aware of the anatomical remarks of the IHs and they should take into account that IHs can be a cause of SBO also in patients over 80 years of age, although they are very rare in this age range.
Institutional review board statement
Not applicable.
Patient consent
Written informed consent has been obtained by the patient.
Author contributions
B.B., U.L., Radiological investigation and Manuscript draft; B.B., made the diagnosis on CT; LI made the surgical intervention; L.A.M., L.I, Supervision. All authors have read and agreed to the published version of the manuscript.
Data availability statement
The data that support the findings of this case report are available upon request.
Footnotes
Acknowledgments: This research received no external funding.
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Brogna B, Bignardi E, Megliola A, Laporta A, La Rocca A, Volpe M, et al. A pictorial essay describing the CT imaging features of COVID-19 cases throughout the pandemic with a special focus on lung manifestations and extrapulmonary vascular abdominal complications. Biomedicines. 2023;11(8):2113. doi: 10.3390/biomedicines11082113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Monica ML, Antonella M., Gloria A, Diletta C, Nicola M, Ginevra D, et al. Internal hernias: a difficult diagnostic challenge. Review of CT signs and clinical findings. Acta BioMed. 2019;90(S-5):20. doi: 10.23750/abm.v90i5-S.8344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Martin LC, Merkle EM, Thompson WM. Review of internal hernias: radiographic and clinical findings. AJR Am J Roentgenol. 2006;186(3):703. doi: 10.2214/AJR.05.0644. [DOI] [PubMed] [Google Scholar]
- 4.Akyildiz H, Artis T, Sozuer E, Akcan A, Kucuk C, Sensoy E, et al. Internal hernia: complex diagnostic and therapeutic problem. Int J Surg Case Rep. 2009;7(4):334–337. doi: 10.1016/j.ijsu.2009.04.013. [DOI] [PubMed] [Google Scholar]
- 5.Doishita S, Takeshita T, Uchima Y, Kawasaki M, Shimono T, Yamashita A, et al. Internal hernias in the era of multidetector CT: correlation of imaging and surgical findings. Radiographics. 2016;36(1):88–106. doi: 10.1148/rg.2016150113. [DOI] [PubMed] [Google Scholar]
- 6.Catalano OA, Bencivenga A, Abbate M, Tomei E, Napolitano M, Vanzulli A. Internal hernia with volvulus and intussusception: case report. Abdom Imaging. 2004;29:164–165. doi: 10.1007/s00261-003-0122-y. [DOI] [PubMed] [Google Scholar]
- 7.Zonca P, Maly T, Mole DJ, Stigler J. Treitz's hernia. Hernia. 2008;12:531–534. doi: 10.1007/s10029-008-0339-3. [DOI] [PubMed] [Google Scholar]
- 8.Uchiyama S, Imamura N, Hidaka H, Maehara N, Nagaike K, Ikenaga N, et al. An unusual variant of a left paraduodenal hernia diagnosed and treated by laparoscopic surgery: report of a case. Surg today. 2009;39:533–535. doi: 10.1007/s00595-008-3875-7. [DOI] [PubMed] [Google Scholar]
- 9.Suwanthanma W, Euanorasetr C, Soom-Im S, Lertbannaphong S. Left paraduodenal hernia as a rare cause of small bowel obstruction in elderly: a case report and review of literature. J Med Assoc Thai. 2015;98(7):713–718. [PubMed] [Google Scholar]
- 10.Fernandes U, Moreira H, Pinto-de-Sousa J. Hernia of Landzert: a rare cause of intestinal obstruction. J Gastrointest Surg. 2022;26(5):1113–1114. doi: 10.1007/s11605-022-05256-6. [DOI] [PubMed] [Google Scholar]
- 11.Giordano G, La Mirata E, Politi V, Veroux M, Meli GA, Evola G, et al. Left paraduodenal hernia in a young patient with recurrent abdominal pain: a case report and short literature review. Am J Case Rep. 2022;23:e935411–e935413. doi: 10.12659/AJCR.935413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Milani D, Corsi A, Cirocchi R, Santoro A, Rocco G, Renzi C, et al. A case of a paraduodenal hernia with a concomitant mesosigmoid defect. Open Med. 2013;8(1):99–102. [Google Scholar]
- 13.Manojlović D, Čekić N, Palinkaš M. Left paraduodenal hernia–A diagnostic challenge: case report. Int J Surg Case Rep. 2021;85 doi: 10.1016/j.ijscr.2021.106138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hayakawa K, Tanikake M, Yoshida S, Yamamoto A, Yamamoto E, Morimoto T. CT findings of small bowel strangulation: the importance of contrast enhancement. Emerg Radiol. 2013;20:3–9. doi: 10.1007/s10140-012-1070-z. [DOI] [PubMed] [Google Scholar]
- 15.Francesco T, Antonio Z, Stefano C, Michelina F, Matteo R., Edoardo B, et al. Abdominal pain and internal hernias after Roux-en-Y Gastric Bypass: are we dealing with the tip of an iceberg? Acta BioMed. 2019;90(2):251. doi: 10.23750/abm.v90i2.7145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cundy TP, Di Marco AN, Hamady M, Darzi A. Giant left paraduodenal hernia. BMJ Case Rep. 2014 doi: 10.1136/bcr-2013-202465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sleiman Y, El-Kheir A, El-Khoury M, Hamdach O, Ismail L, Allouch M. Small bowel obstruction secondary to left paraduodenal hernia: a case report and literature review. Int J Surg Case Rep. 2018;53:29–31. doi: 10.1016/j.ijscr.2018.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vanmali A, Maharajh J, Haines M. Left paraduodenal hernia: Embryological and radiological findings. SA J Radiol. 2021;25(1):1979. doi: 10.4102/sajr.v25i1.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barbosa L, Ferreira A, Póvoa AA., Maciel J.P. Left paraduodenal hernia: a rare cause of small bowel obstruction in the elderly. BMJ Case Rep. 2016;2016 doi: 10.1136/bcr-2015-209678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Almafreji I, Chinaka U, Hussain A, Lynch M, Cottrell R. Role of Gastrografin in patients with small bowel obstruction. Cureus. 2020;12(8):e9695. doi: 10.7759/cureus.9695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Maheshwari S, Khadka A, Bhattacharjee S, Rajesh U, Maria V. A case report of left paraduodenal hernia with a spontaneous reduction on follow-up: the rare demonstration on computed tomography. Egypt J Radiol Nuclear Med. 2020;5:1–4. [Google Scholar]
- 22.Shadhu K, Ramlagun D, Ping X. Para-duodenal hernia: a report of five cases and review of literature. BMC Surg. 2018;18(1):1–7. doi: 10.1186/s12893-018-0365-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Parmar BPS, Parmar RS. Laparoscopic management of left paraduodenal hernia. J Minim Access Surg. 2010;6(4):122. doi: 10.4103/0972-9941.72601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Al-Khyatt W, Aggarwal S, Birchall J, Rowlands TE. Acute intestinal obstruction secondary to left paraduodenal hernia: a case report and literature review. World J Emerg Surg. 2013;8(1):5. doi: 10.1186/1749-7922-8-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Surel AA, Işık Nİ, Yazla M. Untangling diagnostic confusion in internal abdominal hernias. Ulus Travma Acil Cerrahi Derg. 2023;29(10):1114–1121. doi: 10.14744/tjtes.2023.36037. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this case report are available upon request.