Abstract
Strengthening the field of imaging informatics by further defining standards and advocating for continuous education are the cornerstones of the American Board of Imaging Informatics (ABII). ABII is the non-profit organization that governs the Imaging Informatics Professional certification program. ABII is responsible for awarding the Certified Imaging Informatics Professional (CIIP) designation to candidates who meet specified educational and experience-based criteria and pass a qualifying exam (1). For this paper, we analyzed Quality Improvement (QI) projects submitted to ABII for satisfaction of the 10-year requirements in 2017–2021. The project reports demonstrated a variety of interventions undertaken to ultimately improve patient care. A retrospective review of these reports exemplifies the critical role the Certified Imaging Informatics Professionals have in delivery of high quality, safe healthcare and their vital contributions to the healthcare industry and practice of medicine.
Keywords: CIIP, ABII, SIIM, Imaging Informatics, Quality Improvement (QI)
Background
The American Board of Imaging Informatics (ABII) was founded in 2007 through a partnership between the Society for Imaging Informatics in Medicine (SIIM) and the American Registry of Radiologic Technologists (ARRT). SIIM’s mission is “to advance medical imaging informatics across the enterprise through education, research, and innovation in a multi-disciplinary community” [1]. The ARRT’s mission is “to promote high standards of patient care by recognizing qualified individuals in medical imaging, interventional procedures, and radiation therapy” [1]. SIIM and the ARRT identified a need to define the effective application of imaging informatics and recognize individuals who possess and apply the necessary body of knowledge to enhance patient care by promoting competence in imaging informatics. The collaboration of these two organizations was the formation of the independent credentialing organization ABII, which is focused on carrying out this mission.
ABII uses a flexible 7-point qualification system that requires both educational and experiential components to determine if candidates meet the qualification criteria for the certification exam.
The exam consists of 10 categories totaling 130 questions with varying weights based on relative importance [1–5]. The categories include Procurement, Project Management, Operations, Communications, Training and Education, Image Management, Information Technology, Systems Management, Clinical Engineering, and Medical Imaging Informatics [1]. Individuals who successfully pass the examination earn the credential of Certified Imaging Informatics Professional (CIIP) (Fig. 1).
Fig. 1.
ABII test content outline: current and future allocation of the weighted scored questions
Ten-Year Requirements
Certified Imaging Informatics Professionals must renew their certification annually, complete 24 hours of continuing education (CE) requirements biannually and seek recertification every 10 years through ABII’s 10-Year Requirements process. The recertification requirement is designed for CIIP’s to demonstrate their growing knowledge and skills reflective of their engagement in professional development. The recertification process is also a way for ABII to better understand trends and changes in the field.
ABII currently offers four options to CIIPs for completing the 10-year recertification requirements: Practice, Education, Research, or Examination. Practice allows the CIIP to submit an Imaging Informatics Quality Improvement (QI) project with a detailed summary report of the quality issue that was identified and intervention performed to address the issue. Education can be supported by the mentorship of a non-CIIP to prepare for the CIIP examination with a detailed summary report to include the activities, objectives, projects, and goals the mentee participated in as part of the relationship. Additionally, this category can be met by preparing and presenting lectures or serving as a volunteer on the ABII Examination Committee. The Research choice requires the CIIP to publish an article in a peer-reviewed journal as the first or second corresponding author based on a minimum of one topic from the ABII Test Content Outline. The completion timeline requirement for the Practice, Education, and Research options is within 36 months of the end of the candidate’s compliance period, and the Examination option must be completed during the year of the compliance period [1].
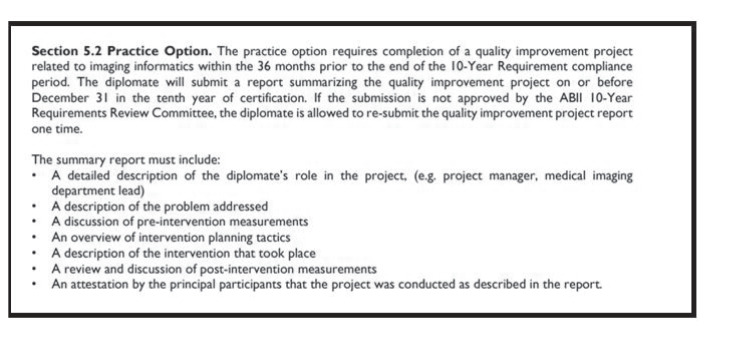
The primary focus for this research was on the Practice option, specifically in reviewing the types of QI projects submitted for the 10-year recertification. The general outline for the Practice option is listed in Table 1 as it appears in Sect. 5.2 of the ABII 10-Year Requirements available on the ABII Web site.
Table 1.
This table provides content for Sect. 5.2 of the ABII Practice Option
Methods
The investigators reviewed a total of 97 anonymized reports for QI projects that were led by a CIIP or where the CIIP held a significant role on the project team. The reports were submitted to comply with the ABII 10-Year Recertification Requirements through the ABII online portal from January 2017 through December 2021. During that timeframe, a total of 105 reports were submitted for the Practice option. Of the reports submitted, 97 were reviewed by an ABII committee of certified CIIPs and approved to meet the requirements for the ABII 10-Year recertification. The remaining eight reports did not meet the minimum requirements for documentation of completion; therefore, these reports were not included for review in this study. The project reports were anonymized for research purposes.
Upon initial assessment of the submissions, the investigators identified prevalent themes related to healthcare quality and categorized the reports into the following four categories: data quality, patient safety, regulatory compliance, and technology (Fig. 2).
Fig. 2.
CIIP quality improvement projects submitted for 10-year recertification between 2017 and 2021
Examples of data quality project submissions included methods of ensuring data integrity were not compromised, quality assurance (QA) improvement efforts, and enhanced structured reports. Examples of patient safety project submissions detailed changes made to decrease turnaround times, improvements in reporting accuracy, and enhanced imaging details. The regulatory compliance project submissions involved concentrated efforts to standardize workflows. The technology project submissions included implementing cloud platforms and introducing new applications to reduce errors while increasing performance.
Results
Of the projects reviewed, 47 were categorized as data quality, eight were categorized as patient safety, three were categorized as regulatory compliance, and 39 were categorized as technology. An overview of each category is as follows.
Data Quality Projects
A recurring theme among the data quality projects was awareness and understanding of the importance of data integrity. Inaccurate reports, bottlenecks in continuing care, and inconsistencies in acquiring prior studies were examples of patient care issues that instigated quality improvement projects. Passion for providing accurate, reliable data drove CIIP’s to seek alternative solutions. Some of the solutions included designing technical and clinical workflows to streamline critical findings, enhanced structured reporting, developing and establishing baselines for data analytic systems, and tracking performance. There was also correlation that these types of projects drove teams toward establishing standardized data management throughout the enterprise. Standardization leads to consistency in reporting, increased access to the reports rendered by the radiologists, and more timely information to facilitate follow-up imaging when indicated.
One of the data quality projects took a deep dive into streamlining workflows for critical cases, such as stroke and aortic rescues, where time is of the essence. Establishing workflows requires buy-in and change management to ensure consistency; creating formal documentation is necessary, especially for staff who work off-peak hours, part-time, or per diem and may not be as familiar with protocols or have as much experience. The documentation should be updated regularly (as determined by the team) and may include cheat sheets and swim lane diagrams, which are easily accessible, permitting the entire team to be on the same page and know what to do in a trauma or crisis situation.
Patient Safety Projects
CIIPs consistently reported that the primary goal for these types of projects was to improve patient safety guidelines and minimize risk. From organizing and managing clinical imaging system downtime drills, creating more efficient workflows in the emergency department (ED), improving stroke protocol workflows, and establishing post-implementation processes, CIIPs reported these projects resulted in improved access to patient records and treatment plans across health systems.
One of the patient safety projects submitted was focused on improving the imaging department’s participation in enterprise-wide downtime drills. Downtimes often require teams to work as well-oiled machines as imaging system outages may delay or halt the organization's ability to provide services, access scheduling systems and patient records, and provide timely notification of examination results. Compromised infrastructures and non-imaging system outages may also profoundly affect an imaging department’s ability to perform, read, retrieve, view, or store exams. In either scenario, safety concerns arise as staff may need to switch to manual workflows such as typing in patient demographics, increasing the likelihood of human error. It is important during any downtime situation that communication between leadership, information technology teams, and clinical teams is clear. All groups should be frequently informed of an issue’s status and what is being done to address the issue. Imaging informatics participation in regular downtime drills, during all shifts, ensures that individuals responsible for technical systems, and departments, are informed and updated.
Regulatory Compliance Projects
A strong example of a regulatory compliance project submission was related to the comprehensive analysis of anonymized DICOM data. Imaging informaticists are all too familiar with utilizing anonymization tools that do not always eliminate identifiable protected health information (PHI) from pixel, meta-data, and object data. Each imaging modality should be reviewed to highlight the variations in how they present identifiable patient information so it can be removed with consistency, which may require the use of multiple tools. As a secondary measure to ensure exams do not contain protected health information (PHI), spot checks should also be conducted on each set of anonymized exams.
Technology Projects
CIIPs submitted various technology related projects that included successful integration of imaging workflows across the enterprise and removing barriers for previously siloed departments, groups, and teams. CIIPs are integrally involved with evaluating and resolving delays in transfer speeds, integrating systems, data migration, system upgrades, and replacing imaging solutions. Managing projects effectively takes time, skill, effort, dedication, organization, and institutional buy-in. For the technology project submissions, CIIPs demonstrated their understanding of the need for adequate training and education. A thorough handoff to support teams upon the close of a project is vital to sustaining the task, which also requires follow-up and review of the metrics for each task.
One technology project submission involved formulating a strategy to assess the transfer speed between the server virtual machine hosts and their VNA’s SAN. Measuring transmission speeds involves conducting tests to review the network pathway from the modality to the Picture Archiving and Communication System (PACS) and from PACS to reading workstations. Optimizing network speeds is pivotal in reducing workflow delays and bottlenecks.
Discussion
A considerable amount of experience, training, and education is required to successfully manage the layered complexities of imaging informatics systems. The ABII Quality Improvement project reports reviewed demonstrate how CIIPs are bringing value to healthcare systems as leaders in improving the quality of healthcare technology. The four Quality Improvement project categories of data quality, patient safety, regulatory compliance, and technology are reflective of integral components of a CIIP’s scope of responsibility.
Decisions in healthcare, based on imaging informatics, are directly correlated with the quality of the data provided; therefore, optimal patient care equates to access to quality data. The best outcomes are a result of accurately informed practitioners. CIIPs must continually strive to provide timely, reliable data to have a lasting impact. The efficacy of decisions made directly results from examining and utilizing quality data [5–11].
Patient safety is key to improving patient outcomes. CIIPs that explored patient safety related projects added value by uncovering ways to reduce healthcare waste, benefiting the patient, referring providers, and the organization [12]. Identifying, reporting, and acting upon patient safety concerns is not just the responsibility of safety officers but of every member of the healthcare team. Healthcare regulations are necessary to maintain a safe environment for patients and healthcare providers. CIIPs must stay abreast of changing regulatory requirements. An organization’s reputation can be affected by non-compliance with rules, which can be costly considering the fines associated with a lack of adherence to laws and regulations.
Developing and adhering to standards is at the heart of imaging informatics. Identifying opportunities for the healthcare system to improve compliance with the Health Insurance Portability and Accountability Act (HIPAA), such as recommending updates to processes or programming that remove PHI and preserve the integrity of patient privacy, should consistently be performed at healthcare organizations.
A primary goal of automated systems is to increase efficiency by reducing turnaround times when bottlenecks are identified in workflows. When CIIPs help design and implement environments that eliminate these issues, they not only contribute to reduced employee burnout but also allow practitioners to provide optimal patient care [13–18].
As the industry continues to grow, we anticipate future QI projects may delve further into topics such as:
Implementing AI in the clinical environment
Cybersecurity and data privacy
Development of effective training programs
Dashboards and key performance indicators
Mobile imaging
Cloud computing
Standardizing protocols
Conclusion
Our review and analysis of the QI projects submitted by CIIPs seeking 10-year recertification concluded that CIIPs add significant value to healthcare organizations. CIIPs who are diligent at expanding their knowledge and skills in imaging informatics have a direct impact on improved patient care. As healthcare technology advances, there is a need to further expand the scope and capabilities of CIIPs through progressive educational training and ongoing standards assessments.
Continuing education and innovative thinking bring forth developments in the field, and CIIPs improve patient outcomes by remaining engaged and aware of the swift changes in the imaging informatics industry [19].
Acknowledgements
We want to acknowledge the CIIPs who submitted reports for quality improvement projects they have participated in, and ABII for approving the use of their anonymized work for research.
Author Contribution
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Ameena Elahi, Nikki Fennell, and Liana Watson. The first draft of the manuscript was written by Ameena Elahi, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
The authors declare that they did not receive any funds, grants, or other support while preparing this manuscript.
Declarations
Competing Interests
The authors have personal and professional relationships with ABII. Ameena Elahi volunteers as an ABII Item Writer and is a member of the ABII 10-Year Requirements Review Committee. Nikki Fennell is the current Chair of the ABII Board of Trustees, a member of the ABII 10-Year Requirements Review Committee, and a member of the ABII Examination Committee. Liana Watson is the CEO of ARRT and the former ABII Coordinator.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
9/4/2024
A Correction to this paper has been published: 10.1007/s10278-024-01246-z
References
- 1.American Board of Imaging Informatics (2023). Retrieved from American Board of Imaging Informatics (abii.org).
- 2.Kho, D.Y., Bluth, E.I., Meenan, C. et al. Certification of Imaging Informatics Professionals (CIIP): 2010 Survey of Diplomates. J Digit Imaging 25, 678–681 (2012). 10.1007/s10278-012-9486-2 10.1007/s10278-012-9486-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Langlotz, C. From the Chair: The Top 10 Myths About Imaging Informatics Certification (January 2008–SIIM News). J Digit Imaging 21, 1–2 (2008). 10.1007/s10278-007-9100-1 10.1007/s10278-007-9100-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Raymond, M., Nagy, P.G. Developing and Verifying the Psychometric Integrity of the Certification Examination for Imaging Informatics Professionals. J Digit Imaging 23, 241–245 (2010). 10.1007/s10278-009-9241-5 10.1007/s10278-009-9241-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Babcock, B., Nagy, P. The IIP Examination: an Analysis of Group Performance 2009–2011. J Digit Imaging 26, 378–382 (2013). 10.1007/s10278-012-9508-0 10.1007/s10278-012-9508-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guha S, Kumar S. Emergence of Big Data Research in Operations Management, Information Systems, and Healthcare: Past Contributions and Future Roadmap. Production and Operations Management Society. 2018, 27:9. Accessed at University Library (ebscohost.com) August 10, 2022
- 7.Reiner BI. Creating Accountability in Image Quality Analysis. Part 4: Quality Analytics. J Digit Imaging (2013) 26:825–829. Accessed at University Library (ebscohost.com) August 10, 2022 [DOI] [PMC free article] [PubMed]
- 8.Yeager D. Measuring quality to improve imaging care. Radiology Today. December 2012. Accessed at University Library (ebscohost.com) August 10, 2022
- 9.Bui AA, Hsu W, Arnold C, El-Saden S, Aberle DR, Taira RK. Imaging-based observational databases for clinical problem solving: the role of informatics. J Am Med Inform Assoc 2013;20:1053–1058. Accessed at University Library (ebscohost.com) August 10, 2022 [DOI] [PMC free article] [PubMed]
- 10.Lobo-Stratton, G., Mercer, T. & Polman, R. Patient Exam Data Reconciliation Tool. J Digit Imaging 19 (Suppl 1), 60–65 (2006). 10.1007/s10278-006-0926-8 10.1007/s10278-006-0926-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Quality improvement and confirmation projects: Facilitating rapid, measurable performance improvement. Radiographics. 2013; 33: e225-e235 10.1148/rg.337135058 [DOI] [PubMed] [Google Scholar]
- 12.Implementation of total quality management: conventional wisdom versus reality. Hosp Health Serv Admin. 1996; 41: 143-159 [PubMed] [Google Scholar]
- 13.Karami M, Hafizi N. Enhancing Patient Safety Using Medical Imaging Informatics. Radiologist Management March/April 2017. Accessed at University Library (ebscohost.com) August 10, 2022 [PubMed]
- 14.Towbin AJ, Perry LA, Larson DB. Improving efficiency in the radiology department. Pediatr Radiol. 2017 Jun;47(7):783-792. 10.1007/s00247-017-3828-7. Epub 2017 May 23. PMID: 28536767. 10.1007/s00247-017-3828-7 [DOI] [PubMed] [Google Scholar]
- 15.Sammer, M.B.K., Stahl, A., Ozkan, E. et al. Implementation of a Software Distribution Intervention to Improve Workload Balance in an Academic Pediatric Radiology Department. J Digit Imaging 34, 741–749 (2021). 10.1007/s10278-021-00451-4 10.1007/s10278-021-00451-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ziegler, S.E. Rapid Design and Development of a Network Isolated DICOM Service Class Provider Device. J Digit Imaging 33, 1009–1015 (2020). 10.1007/s10278-020-00335-z 10.1007/s10278-020-00335-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sachs, P.B., Long, G. Process for Managing and Optimizing Radiology Work Flow in the Electronic Heath Record Environment. J Digit Imaging 29, 43–46 (2016). 10.1007/s10278-015-9819-z 10.1007/s10278-015-9819-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Roth, C.J., Harten, H.H., Dewey, M. et al. How Image Exchange Breaks Down: the Image Library Perspective. J Digit Imaging 35, 785–795 (2022). 10.1007/s10278-022-00684-x 10.1007/s10278-022-00684-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Siegel E. Imaging Informatics: Waking up to 50 Years of Progress. Applied Radiology, Nov/Dec 2021; 50(6): 27–30. Accessed at University Library (ebscohost.com) August 10 2022