Abstract
Background:
Failure of digit replantation after traumatic amputation is difficult to predict. The authors aimed to develop a prognostic model to better identify factors that better predict replantation failure following traumatic digit amputation.
Materials and methods:
In this multicenter prospective cohort, the authors identified patients who had received digit replantation between 1 January 2015 and 1 January 2019. Univariable and multivariable analyses were performed successively to identify independently predictive factors for failure of replanted digit. To reduce overfitting, the Bayesian information criterion was used to reduce variables in the original model. Nomograms were created with the reduced model after model selection. This model was then internally validated with bootstrap resampling and further externally validated in validation cohort.
Results:
Digit replantation was failed in 101 of 1062 (9.5%) digits and 146 of 1156 digits (12.6%) in the training and validation cohorts, respectively. The authors found that six independent prognostic variables were associated with digit replantation failure: age, mechanism of injury, ischemia duration, smoking status, amputation pattern (complete or incomplete), and surgeon’s experience. The prediction model achieved good discrimination, with concordance indexes of 0.81 (95% CI: 0.76–0.85) and 0.70 (95% CI: 0.65–0.74) in predicting digit failure in the training and validation cohorts, respectively. Calibration curves were well-fitted for both training and validation cohorts.
Conclusions:
The proposed prediction model effectively predicted the failure rate of digit replantation for individual digits of all patients. It could assist in selecting the most suitable surgical plan for the patient.
Keywords: amputation, replantation, traumatic, nomograms
Highlights
This multicenter prospective cohort is the most large-scale one on finger replantation to date.
A prediction model was well developed based on age, mechanism of injury, duration of ischemia, smoking status, amputation pattern, and surgical experience of surgeon.
After validation, this model can effectively predict the failure rate of digit replantation for individual digits of all patients.
Background
Approximately 1% of all traumatic injuries treated in the emergency room are limb amputations, and of these, 90% involve traumatic digit amputations1–4, mostly in young, active working population. With the global acceleration of industrialization, digit amputation exerts huge economic burden to society and patients, and the average direct and indirect expense of every injury reached $30 7542,5,6. Moreover, traumatic digit amputations severely affect both physical functioning and psychological health, such as depression, anxiety, and PTSD7,8.
To date, treatment of traumatic digit amputation mainly includes procedures such as digit replantation and revision amputation. While revision amputation is less costly and less complex, replantation is still an important treatment for patients with traumatic digit amputation, in that it can partially restore the function and appearance of the affected finger3. However, this sophisticated surgery requires highly experienced hand surgeons and patients require long or extended hospitalization after surgery9,10. Owing to microsurgical advancements, the success rate of digit replantation reached more than 80%11–13. But there is still a certain probability of failure, especially in patients with some adverse influencing factors14. Once replantation fails, patients will suffer unacceptable consequences, such as a secondary revision amputation, higher subsequent treatment costs, prolongment of the treatment, delay in returning to work, and even a shorter finger than received initial revision amputation in ED surgery15,16.
According to current studies, many factors affect the failure rate of digit replantation, including the patient’s demographic and clinical characteristics (e.g. age, smoking status, presence or absence of underlying diseases such as hypertension and diabetes, etc.); injury mechanism; duration of warm ischemia; hospital census at admittance; and surgeon proficiency17–19. However, for the limitation of sample size, no study revealed the ratio of every single factor contributing to the failure rate of replantation to date. Therefore, it would be useful to develop a simple, easy-to-use model that clinicians could apply to predict the failure rate of replantation for each affected finger by integrating different influence factors and to decide whether replantation or revision amputation should ultimately be performed. Having this information in mind, patients and surgeons can weigh the risks of different treatments (e.g. replantation versus no replantation), their respective costs and time requirements, as well as the risk of secondary surgery.
As a developing country with a highly developed industry, China has a huge group of manual workers, which suffered from machine-related traumatic digit amputation. Due to the traditional concept and universal coverage of work-related insurance, patients have a higher replantation rate in China (30–44%) than that in US (18%)9,18,20. Therefore, this study, conducted in three centers, which perform a sufficiently high-volume of digit replantation and distributed in different parts of China, provided a large sample size to develop and validate a model to predict the failure of digit replantation. The three centers contributing data to the development and validation of the nomogram are ideal sources, because they distributed in different part of the country of study, making the proposed nomogram more generalizable.
Materials and methods
Study design and patient population
This is a multicenter prospective cohort study which enrolled all patients with digital traumatic amputation20. We first identified patients who received digit replantation at anyone of the three emergency trauma centers between 1 January 2015 and 1 January 2019, from three hospitals in China. Exclusion criteria were having single or multiple organ failure (n=7), peripheral artery disease (n=15), additional arterial trauma in the ipsilateral arm or forearm (n=145), younger than 18 years old (n=51), contraindications for digit replantation (n=25), refuse to participate or unable to understand Mandarin Chinese (n=988). Patients’ demographic and basic clinical data were collected and recorded in a central electronic data capture system, which was accessible only by study personnel from all three centers. Patient data were de-identified and protected by privacy safeguards appropriate to local regulations.
Patients’ demographic data, including age, sex, smoking status (yes/no), and comorbidities (e.g. hypertension and diabetes mellitus) were self-reported. Patients also self-reported the approximate time and primary cause or mechanism of digit amputation, which we classified as either crush, saw, avulsion, or cut trauma. The surgeon evaluated and recorded the time of arterial revascularization and whether it was a complete/incomplete amputation; we called this latter categorization the pattern of amputation (e.g. Table 1). Radiographs and consultation notes were used to determine the digit(s) involved and the Tamai level(s) of the injury.
Table 1.
Demographic and clinical characteristics of training cohort grouped by outcomea.
| Replantation outcome | |||
|---|---|---|---|
| Success (n=961) | Failure (n=101) | P b | |
| Mean age (±SD) | 36.2±12.0 | 42.3±11.7 | <0.001 |
| Sex | |||
| Male | 831 (86.5) | 86 (85.1) | 0.712 |
| Female | 130 (13.5) | 15 (14.9) | |
| Tamaic | |||
| V | 130 (13.5) | 13 (12.9) | 0.03 |
| IV | 271 (28.2) | 18 (17.8) | |
| III | 293 (30.5) | 46 (45.5) | |
| II | 147 (15.3) | 13 (12.9) | |
| I | 120 (12.5) | 11 (10.9) | |
| Mechanism of injury | |||
| Saw | 421 (43.8) | 44 (43.6) | <0.001 |
| Crush | 137 (14.3) | 17 (16.8) | |
| Avulsion | 118 (12.3) | 29 (28.7) | |
| Blade | 285 (29.7) | 11 (10.9) | |
| Ischemia duration (mean hours±SD) | 8.6±2.9 | 10.8±3.2 | <0.001 |
| Smoking status | |||
| Smoker | 335 (34.9) | 56 (55.4) | <0.001 |
| Nonsmoker | 626 (65.1) | 45 (44.6) | |
| Amputation pattern | |||
| Complete | 701 (72.9) | 91 (90.1) | <0.001 |
| Incomplete | 260 (27.1) | 10 (9.9) | |
| Surgeon’s experienced | |||
| Trainee | 186 (19.4) | 35 (34.7) | <0.001 |
| Specialist | 775 (80.6) | 66 (65.3) | |
| Education level | |||
| Less than college graduate | 817 (85.0) | 83 (82.2) | 0.451 |
| College graduate or higher | 144 (15.0) | 18 (17.8) | |
| Comorbidities | |||
| Hypertension | 139 (14.5) | 17 (16.8) | 0.523 |
| No hypertension | 822 (85.5) | 84 (83.2) | |
| Diabetes mellitus | 87 (9.1) | 10 (9.9) | 0.778 |
| No diabetes mellitus | 874 (90.9) | 91 (90.1) | |
Data are presented as n (%), unless otherwise noted.
Mann–Whitney tests or Fisher’s exact tests were used, depending on whether the variables were continuous or categorical.
Tamai level of injury as described by Yoshimura (2003).
Specialists were defined operationally as surgeons who performed 50 or more-digit replantations in his or her career, and trainees were defined as surgeons who performed 49 or fewer digit replantations.
The experience of the surgeon who performed the digit replantation for each patient was classified as a either trainee level or specialist level, according to the number of digital replantation performed in his or her career. Specialists were defined operationally as surgeons who performed 50 or more-digit replantation in his or her career, and trainees were defined as surgeons who performed 49 or fewer digit replantation.
This study was approved by the ethics committees of Shanghai Sixth People’s Hospital Affiliated to Shanghai Jiao Tong University School of Medicine, 80 PLA Hospital, and Xi’an Honghui Hospital. The study has been reported in line with the strengthening the reporting of cohort studies in surgery (STROCSS) criteria21 and conformed with the reporting TRIPOD guidelines for developing, validating, or updating a prediction model22. Full written informed consent was obtained from all participants.
Surgery and postoperative procedures
All replantation operations were performed in emergency operating rooms soon after the injury. Postoperatively, the patient was kept in a still recumbent position, the affected limb was kept warm by applying incident light from a heat lamp, and the affected limb was elevated above the heart or slightly higher to increase circulation23. The blood supply to the affected finger was closely monitored, and the patient was managed according to standard vascular crisis procedures. Re-exploration after initial surgery, if needed, was performed by specialists with high expertise in microsurgery. All patients were followed up for at least 1 month. Failure was defined as necrosis of the replanted finger, which required revision amputation or a flap cover of the skeleton17.
Statistical analysis
All analyses were performed using SPSS (IBM Corp. Released 2016. IBM SPSS Statistics for Windows, Version 24.0. Armonk, NY: IBM Corp.) and R software version 3.5.3 (R Core Team. Released 2019. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing. https://www.R-project.org). Variables with continuous and categorical values were evaluated using the Mann–Whitney test or Fisher’s exact test, respectively. The significance of each variable in the training cohort was first assessed using univariate analysis. When a variable yielded a P-value of <0.2 in the univariate analysis, it was included in the subsequent binary analysis. The Bayesian information criterion was then used to reduce the number of variables introduced into the model. The nomogram was then developed based on the size of the resulting β coefficients of the multivariate logistic regression analysis and by using the rms package of R software (version 3.4.1). The variable with the largest β coefficient was assigned 100 points, and remaining variables were proportionally transformed along a 0-to-100-point scale according to the size of their β coefficients. For internal validation, the discriminative performance of the nomogram was measured using the concordance index (C-index). Internal calibration was performed using 1000 bootstrap samples of the training cohort data to assess any overfitting bias. For external validation, discriminative performance, and calibration were assessed likewise using the validation cohort data. In all statistical analyses, a P-value of <0.05 was considered to be statistically significant.
Results
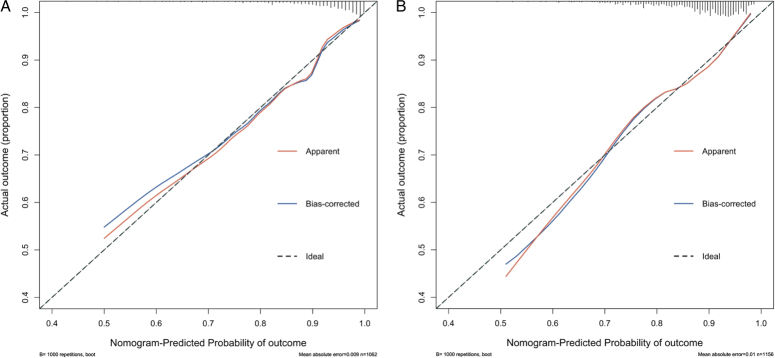
For training and validation cohorts, respectively, we included 745 and 806 patients with 1062 and 1156 replanted digits, respectively, as shown in Figure 1. Overall failure of replantation was 101 of 1062 (9.5%) digits in the training cohort and 146 of 1156 digits (12.6%) in the validation cohort.
Figure 1.
Study screening and enrollment.
Univariable analysis of prognostic factors
Table 1 presents and compares demographic and clinical characteristics of the training cohort based on the replanted digits. All variables were evaluated using univariable analyses according to success or failure of replantation. In the training cohort, the success and failure groups differed significantly along several variables: age, level of amputation (Tamai level), mechanism of injury, duration of ischemia, smoking status, amputation pattern, and surgeon’s experience. There were no statistically significant differences between the success and failure groups in demographic characteristics, comorbidities, or educational level.
Model selection Bayesian information criterion
The variables of patient age, level of amputation (Tamai level), mechanism of injury, duration of ischemia, smoking status, amputation pattern, and surgeon’s experience yielded P-values of <0.2 and thus were included in the binary analysis. To avoid overfitting the model, we used the Bayesian information criterion to reduce the number of variables. Age, mechanism of injury, duration of ischemia, smoking status, amputation pattern, and surgeon’s experience were retained in the final reduced model; these variables are presented in Table 2.
Table 2.
Results of binary logistic regression analysis to construct nomogram.
| Odds ratio | 95% CI | P | |
|---|---|---|---|
| Age | 0.966 | 0.960–0.972 | <0.001 |
| Mechanism of injury | |||
| Avulsion | Reference | ||
| Crush | 1.412 | 1.124–1.774 | 0.003 |
| Saw | 2.139 | 1.778–2.572 | <0.001 |
| Blade | 6.697 | 5.024–8.928 | <0.001 |
| Ischemia duration | 0.799 | 0.777–0.821 | <0.001 |
| Smoking status | |||
| Smoker | Reference | ||
| Nonsmoker | 1.631 | 1.399–1.900 | <0.001 |
| Amputation pattern | |||
| Complete | Reference | ||
| Incomplete | 3.336 | 2.656–4.190 | <0.001 |
| Surgeon’s experience | |||
| Trainee | Reference | ||
| Specialist | 2.406 | 2.039–2.840 | <0.001 |
Development and validation of prognostic model for replantation failure
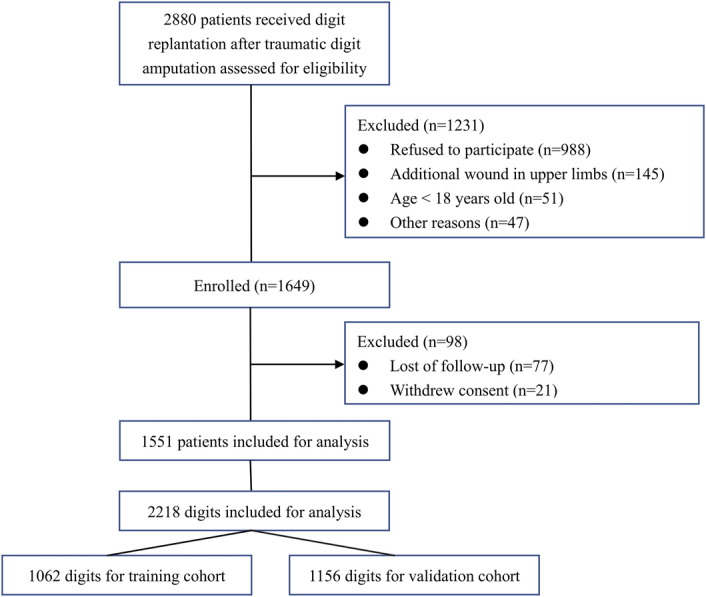
The proposed model for failure rate prediction after digit replantation was constructed using the independently associated variables evaluated and presented in Table 2. These variables and their associated scales are shown in Figure 2. We used the bootstrap validation method to internally and externally validate the prediction accuracy of this prediction model on the training and validation cohorts, respectively (Fig. 3).
Figure 2.
Proposed model for estimating failure rate of digit replantation after traumatic digit amputation. To use the prediction, first, the surgeon determines the subscore of each variable by finding the patient’s value on the corresponding scale and then drawing a vertical line up to the Points scale to obtain the number of points for that variable. This is done for each variable. Second, the surgeon calculates the sum of the variable subscores. Finally, the surgeon finds the sum of the variable subscores on the Total Points scale, and then draws a vertical line (index line or isopleth) from the total points scale down to the lower line (failure rate) of the model to determine the predicted probability of failure.
Figure 3.
Bootstrap analysis results to determine prediction accuracy of model for failure rate of digit replantation. Calibration curve of the model for (A) training and (B) validation cohorts in estimating failure rate. The prediction model was validated with the internal data from the training cohort, and then externally evaluated from data of the validation cohort. Apparent (or actual) accuracy, bias-corrected accuracy, and ideal accuracy are plotted. Analysis used 1000 bootstrap samples.
The prediction model had good accuracy24 in predicting the failure of digit replantation. The C-index for the model was 0.81 (95% CI: 0.76–0.85) for the training cohort and 0.70 (95% CI: 0.65–0.74) for the validation cohort. These were consistent with calibration plots, which showed good agreement for predicted and actual failure rate (Fig. 3). For external validation, although the validation cohort was recruited from the two hospitals geographically distant from the hospital from which the training cohort was recruited, there were no significant differences in many baseline and treatment characteristics between the two groups (Table 3).
Table 3.
Comparison of demographic and clinical characteristics of training and validation cohortsa.
| Training (n=1062) | Validation (n=1156) | P | |
|---|---|---|---|
| Mean age (±SD) | 36.8±12.1 | 37.5±12.6 | 0.151 |
| Sex | |||
| Male | 917 (86.3) | 983 (92.6) | 0.396 |
| Female | 145 (13.7) | 173 (16.3) | |
| Tamai level | |||
| V | 143 (13.5) | 164 (15.4) | 0.853 |
| IV | 289 (27.2) | 333 (31.4) | |
| III | 339 (31.9) | 348 (32.8) | |
| II | 160 (15.1) | 171 (16.1) | |
| I | 131 (12.3) | 140 (13.2) | |
| Mechanism of injury | |||
| Saw | 465 (43.8) | 502 (47.3) | 0.138 |
| Crush | 154 (14.5) | 208 (19.6) | |
| Avulsion | 147 (13.8) | 148 (13.9) | |
| Blade | 296 (27.9) | 298 (28.1) | |
| Ischemia duration (mean hours ±SD) | 7.2±3.5 | 7.0±3.7 | 0.172 |
| Smoking status | |||
| Smoker | 391 (36.8) | 430 (40.5) | 0.86 |
| Nonsmoker | 671 (63.2) | 726 (68.4) | |
| Amputation pattern | |||
| Complete | 792 (74.6) | 845 (79.6) | 0.44 |
| Incomplete | 270 (25.4) | 311 (29.3) | |
| Surgeon’s experience | |||
| Trainee | 221 (20.8) | 255 (24) | 0.501 |
| Specialist | 841 (79.2) | 901 (84.8) | |
| Patient education level | |||
| Less than college graduate | 900 (84.7) | 984 (85.1) | 0.805 |
| College graduate or higher | 162 (15.3) | 172 (14.9) | |
| Comorbidities | |||
| Hypertension | 156 (14.7) | 173 (15.0) | 0.855 |
| No hypertension | 906 (85.3) | 983 (85.0) | |
| Diabetes mellitus | 97 (9.1) | 113 (9.8) | 0.606 |
| No diabetes mellitus | 965 (90.9) | 1043 (90.2) | |
Data are presented as n (%), unless otherwise noted. Mann–Whitney tests or Fisher’s exact tests were used, respectively, for continuous and categorical variables.
Discussion
There are many factors that affect the failure of digit replantation, including demographic characteristics (e.g. age, smoking status, and comorbidities); injury characteristics (e.g. mechanism, pattern of amputation, duration of ischemia, etc.); and replantation surgery characteristics (e.g. surgeon’s experience and quality of vascular anastomosis)25. A huge challenge for hand surgeons in selecting a treatment plan for an individual amputated digit is to estimate accurately the likelihood of replantation failure for each patient. To date, no effective tools exist to assist surgeons in evaluating the failure of digit replantation. Nomograms are widely used in surgical planning and many other medical fields21–23. With a nomogram, physicians can visually estimate the individual probability of a specific clinical event by integrating diverse prognostic variables. With the nomogram and consideration of patients’ financial resources, clinical decisions can be made more rationally together with patients and their treating surgeons.
In the current prospective multicenter study, we developed and validated an evidence-based nomogram that accurately predicts the failure rate of digit replantation in patients with digit amputation(s). Internal and external validation demonstrated that the nomogram was a strong model and had good accuracy in predicting outcome. We found that patient age, mechanism of injury, duration of ischemia, smoking status, amputation pattern (complete or partial), and the surgeon’s experience were good predictors of replantation failure.
When patients arrive in the emergency room with a traumatic digit amputation, typically, hand surgeons estimate the failure rate of replantation. Simultaneously, the surgeon evaluates available information about possible complications, treatment costs, and expectation for recovery of function. Then, the surgeon and patient can weigh all these considerations and determine together what kind of treatment plan to adopt. Some predictors, such as age, mechanism of injury, smoking status, and amputation pattern are unchangeable after traumatic digit amputation, while others, like duration of ischemia and surgeon’s experience, have the potential of being favorably modified and thus can potentially affect the failure rate of replantation.
Whether the duration of ischemia affects replantation survival remains controversial17,26,27. In our study, the duration of ischemia occupies a considerable proportion of points in the nomogram, as it can be an excellent predictor of the failure rate of a replanted digit. Consistent with the findings of previous studies12,18,19,28, our nomogram indicated that a surgeon’s experience is positively correlated with the failure rate of finger digit replantation, and it has a higher weight ratio than smoking status. Therefore, this should be fully considered in future clinical decision-making to patients with traumatic digit amputation. However, its impact on decreasing points of the failure rate is greatly reduced after it reaches a certain level (such as 140, which corresponds to about a 10% failure rate), according to the nonlinear correlation between total points and failure rate indicated by Figure 2. Thus, for a young, nonsmoking patient with an incompletely amputated digit caused by a knife blade injury and who was rushed to the emergency room soon after the injury, the failure rate of digit replantation would be still low even if performed by a trainee. For an older, smoking patient with a completely amputated digit caused by an avulsion injury and having a long-duration ischemia, the failure rate would decrease significantly if performed by a surgeon at a specialist level of experience compared with a trainee.
For a hospital that has a high-volume of digit replantation, several patients with traumatic digit amputations may arrive at the emergency room simultaneously. The overall failure rate of digit replantation would decrease if hand surgeons and patients were matched according to the surgeons’ experience and the patients’ complexity of injury, with experienced surgeons being matched with patients having the more complex injuries and trainees being matched to those with less complex injuries, etc. In cases where patients arrive at a hospital that has a low-volume of digit replantation, patients must weigh whether to leave that hospital and go to a high-volume hospital where they can be treated by a specialist (thus increasing the duration of ischemia) or to remain in the low-volume hospital and undergo digit replantation immediately (thus decreasing the duration of ischemia). Our prognostic model was shown to successfully evaluate the failure rate by integrating all these factors. Also, it can guide patients and surgeons in decision-making about the optimal treatment plan for their individual situation.
Limitations
This study has some limitations. Firstly, multiple future prospective studies are needed to validate and possibly calibrate our model to improve its predictive accuracy across different situations. This is especially the case when intraoperative factors (e.g. the number and quality of vascular anastomosis29) and postoperative factors (e.g. the administration of antithrombotic therapies30) were not considered in the present study. Secondly, our study was conducted in three hospitals that have a high annual volume of replantation and the surgeons there may have more experience with replantation than at low-volume hospitals, biasing the test-bed for our model. Thus, the prediction model needs to be validated in low-volume hospitals. Thirdly, the clinical usefulness of this model is still unknown despite its high predictive accuracy. It can be assessed by designing a future randomized controlled study, in which patients are randomly assigned to nomogram-assisted or non-nomogram-assisted groups and patient outcomes are compared. Finally, our prediction model cannot be used alone to guide clinical decisions because it did not consider the functional prognosis.
Conclusion
The novel model developed for patients with traumatic digit amputation(s) can effectively predict the failure of digit replantation for individual digits of all patients. While considering the patient’s economic status, nature of work, etc. physicians and patients can use the prediction model to jointly decide on the most suitable surgical plan for the patient. Finally, the results of this study may also be used to guide the development and validation of nomograms for other types of limb amputations.
Ethical approval
The study was approved by the Ethics Committee of Shanghai Sixth People’s Hospital Affiliated to Shanghai Jiaotong University School of medicine. Approval No: 2013-KY-029. The study was approved by the Ethics Committee of 80 PLA Hospital and Xi’an Honghui Hospital.
Sources of funding
This study was supported by National Natural Science Foundation of China (Grant 82002324, Hongyi Zhu; Grant 81974331, Xianyou Zheng); Clinical Technology Innovation Project of Shanghai Hospital Development Center (Grant SHDC12019X06, Xianyou Zheng); the Clinical Research Project of Shanghai Municipal Health Commission (Grant 20194Y0254, Hongyi Zhu).
Author contribution
X.Z.: had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis; T.G., B.B., and J.L.: share co-first authorship, and X.Z., H.Z., and Q.C.: share co-senior authorship; X.Z. and H.Z.: concept and design; T.G., B.B., J.L., M.T., L.X., and H.W.: acquisition, analysis, or interpretation of data; X.Z. and H.Z.: critical revision of the manuscript for important intellectual content; H.Z. and Q.C.: statistical analysis; X.Z. and H.Z.: obtained funding; X.Z., Hongyi Zhu and Qianying Cai
Conflicts of interest disclosure
All authors declares no competing interests.
Research registration unique identifying number (UIN)
Trial registry: Chinese Clinical Trial Registry.
Registration number: ChiCTR1900026268.
Guarantor
Xianyou Zheng.
Data availability statement
No additional data are available.
Footnotes
Tao Gao, Bingbo Bao, and Junqing Lin contributed equally to this work.
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Published online 13 February 2024
Contributor Information
Tao Gao, Email: gaotaofenzi@163.com.
Bingbo Bao, Email: bingbobao@163.com.
Junqing Lin, Email: junqinglinm@163.com.
Maoyuan Tian, Email: 214366366@qq.com.
Lei Xia, Email: xialeifmmu@163.com.
Haifeng Wei, Email: weihaifeng@sjtu.edu.cn.
Qianying Cai, Email: 16111020002@fudan.edu.cn.
Hongyi Zhu, Email: 420308955@qq.com.
Xianyou Zheng, Email: zhengxianyou@126.com.
References
- 1.Win TS, Henderson J. Management of traumatic amputations of the upper limb. BMJ 2014;348:g255. [DOI] [PubMed] [Google Scholar]
- 2.Ro JS, Leigh JH, Jeon I, et al. Trends in burden of work-related upper limb amputation in South Korea, 2004-2013: a nationwide retrospective cohort study. BMJ Open 2019;9:e032793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chung KC, Yoon AP, Malay S, et al. Patient-reported and functional outcomes after revision amputation and replantation of digit amputations: the FRANCHISE multicenter international retrospective cohort study. JAMA Surg 2019;154:637–646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Conn JM, Annest JL, Ryan GW, et al. Non-work-related finger amputations in the United States, 2001-2002. Ann Emerg Med 2005;45:630–635. [DOI] [PubMed] [Google Scholar]
- 5.Crowe CS, Massenburg BB, Morrison SD, et al. Global trends of hand and wrist trauma: a systematic analysis of fracture and digit amputation using the Global Burden of Disease 2017 Study. Inj Prev 2020;26(supp 1):i115–i124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gil JA, Goodman AD, Harris AP, et al. Cost-effectiveness of initial revision digit amputation performed in the emergency department versus the operating room. Hand (N Y) 2020;15:208–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pomares G, Coudane H, Dap F, et al. Psychological effects of traumatic upper-limb amputations. Orthop Traumatol Surg Res 2020;106:297–300. [DOI] [PubMed] [Google Scholar]
- 8.Chen J, Zhang AX, Chen QZ, et al. Long-term functional, subjective and psychological results after single digit replantation. Acta Orthop Traumatol Turc 2018;52:120–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhu H, Bao B, Zheng X. A comparison of functional outcomes and therapeutic costs: single-digit replantation versus revision amputation. Plast Reconstr Surg 2018;141:244e–249ee. [DOI] [PubMed] [Google Scholar]
- 10.Li NY, Kleiner JE, Harris AP, et al. Pediatric digit replantation following traumatic amputation: nationwide analysis of patient selection, outcomes, and cost. Hand (N Y) 2021;16:612–618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hsu CC, Malay S, Chen JS, et al. National population study of the effect of structure and process on outcomes of digit replantation. J Am Coll Surg 2021;232:900–9.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hsu CC, Malay S, Chung TT, et al. The impact of hospital, surgeon, and patient characteristics on digit replantation decision: a national population study. Injury 2020;51:2532–2540. [DOI] [PubMed] [Google Scholar]
- 13.Kwon GD, Ahn BM, Lee JS, et al. The effect of patient age on the success rate of digital replantation. Plast Reconstr Surg 2017;139:420–426. [DOI] [PubMed] [Google Scholar]
- 14.Wang T, Xiong F, Tan JY, et al. Predictors for necrosis after single-digit replantation: a retrospective analysis of 946 patients. Plast Reconstr Surg 2023;152:117–123. [DOI] [PubMed] [Google Scholar]
- 15.Yoon AP, Mahajani T, Hutton DW, et al. Cost-effectiveness of finger replantation compared with revision amputation. JAMA Netw Open 2019;2:e1916509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sears ED, Shin R, Prosser LA, et al. Economic analysis of revision amputation and replantation treatment of finger amputation injuries. Plast Reconstr Surg 2014;133:827–840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhu X, Zhu H, Zhang C, et al. Pre-operative predictive factors for the survival of replanted digits. Int Orthop 2017;41:1623–1626. [DOI] [PubMed] [Google Scholar]
- 18.Brown M, Lu Y, Chung KC, et al. Annual hospital volume and success of digital replantation. Plast Reconstr Surg 2017;139:672–680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yoon AP, Kane RL, Wang L, et al. Variation in surgeon proficiency scores and association with digit replantation outcomes. JAMA Netw Open 2021;4:e2128765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhu H, Wang J, Gao T, et al. Contribution of revision amputation vs replantation for certain digits to functional outcomes after traumatic digit amputations: a comparative study based on multicenter prospective cohort. Int J Surg 2021;96:106164. [DOI] [PubMed] [Google Scholar]
- 21.Agha R, Abdall-Razak A, Crossley E, et al. STROCSS 2019 guideline: strengthening the reporting of cohort studies in surgery. Int J Surg 2019;72:156–165. [DOI] [PubMed] [Google Scholar]
- 22.Moons KG, Altman DG, Reitsma JB, et al. Transparent Reporting of a multivariable prediction model for Individual Prognosis or Diagnosis (TRIPOD): explanation and elaboration. Ann Intern Med 2015;162:W1–W73. [DOI] [PubMed] [Google Scholar]
- 23.Ono S, Chung KC. Efficiency in digital and hand replantation. Clin Plast Surg 2019;46:359–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Harrell FE, Jr, Lee KL, Mark DB. Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med 1996;15:361–387. [DOI] [PubMed] [Google Scholar]
- 25.Bao B, Gao T, Li X, et al. Breaking the technical barrier of microvascular anastomosis with high-speed videography: a prospective cohort study. Int J Surg 2022;98:106214. [DOI] [PubMed] [Google Scholar]
- 26.Shaterian A, Rajaii R, Kanack M, et al. Predictors of digit survival following replantation: quantitative review and meta-analysis. J Hand Microsurg 2018;10:66–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shaterian A, Sayadi LR, Tiourin E, et al. Predictors of hand function following digit replantation: quantitative review and meta-analysis. Hand (N Y) 2021;16:11–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mahmoudi E, Chung KC. Effect of hospital volume on success of thumb replantation. J Hand Surg Am 2017;42:96–103 e5. [DOI] [PubMed] [Google Scholar]
- 29.Zhu H, Zhu X, Zhang C, et al. Patency test of vascular anastomosis with assistance of high-speed video recording in digit replantation. J Bone Joint Surg Am 2018;100:729–734. [DOI] [PubMed] [Google Scholar]
- 30.Zhu H, Zhu X, Zheng X. Antithrombotic therapies in digit replantation with papaverine administration: a prospective, observational study. Plast Reconstr Surg 2017;140:743–746. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No additional data are available.