Abstract
Prosthetic mechanical valve thrombosis has traditionally been managed with urgent surgical intervention. However, the risk of redo sternotomy can be prohibitively high in some patients. Thrombolytic therapy as a noninvasive treatment of mechanical valve thrombosis is a well-recognized alternative, but optimal dosing and patient selection remain incompletely characterized for right-side mechanical valves.
Key Words: 3D echocardiography, fluoroscopy, mechanical tricuspid valve, thrombolytics, thrombosis, tissue plasminogen activator
Graphical abstract
Case Presentation
A 53-year-old man with a history of hypertension, hyperlipidemia, diabetes mellitus, and a tricuspid valve replacement (bileaflet tilting disc prosthesis) after a motor vehicle accident in 1999 that resulted in blunt chest trauma and flail tricuspid valve with severe tricuspid regurgitation (TR) was maintained on therapeutic anticoagulation with warfarin and followed clinically.
Learning Objectives
-
•
To select appropriate imaging modalities to diagnose prosthetic valve thrombosis.
-
•
To recognize thrombolytic therapy as an option for management of right-side prosthetic valve thrombosis.
He presented to the emergency department with a 4-day history of progressive substernal chest pain, nausea, vomiting, and dyspnea on exertion. He reported adherence to warfarin but also admitted that he had begun taking vitamin K a few weeks earlier at the suggestion of a family member, who thought it was a health supplement. Physical examination revealed temperature 97.9 °F, pulse 63 beats/min, blood pressure 162/109 mm Hg, respiratory rate 18, and oxygenation 100% on room air. S1 metallic closing sound was audible but soft. There was no murmur. Lungs were clear, and estimated jugular venous pressure was 8 mm Hg. The remainder of the physical examination was unremarkable. Initial laboratory tests demonstrated subtherapeutic international normalized ratio (INR) at 1.46, and chart review showed the last therapeutic INR was more than 5 weeks earlier. Complete blood count, comprehensive metabolic panel, and initial high-sensitivity troponin level were within normal ranges. Electrocardiography showed sinus rhythm with new ST-segment depression in anterolateral leads.
Question 1: What is the differential diagnosis, and what initial diagnostic work-up should be performed?
The differential diagnosis included acute coronary syndrome (unstable angina), prosthetic valve obstruction, and pulmonary embolus, and initial work-up included coronary angiography, echocardiography, and computed tomographic angiography (CTA) of the chest. Given that both prosthetic valve obstruction and unstable angina were high on the differential, the patient was admitted to the hospital and first underwent simultaneous coronary angiography and fluoroscopy of the tricuspid mechanical valve.
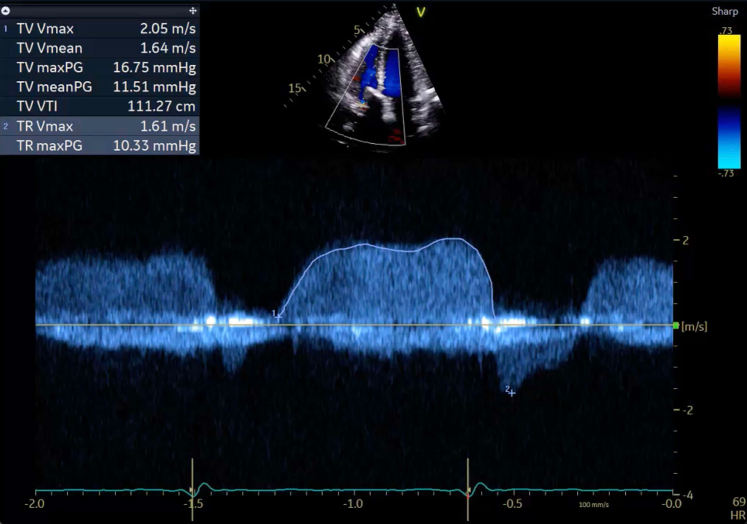
Angiography revealed nonobstructive coronary artery disease, but fluoroscopy identified severe restriction of one of the mechanical valve discs with complete immobility of the second disc (Video 1). Transthoracic echocardiography (TTE) done immediately after catheterization showed color flow acceleration across the prosthesis with mean gradient 11 mm Hg, which was significantly elevated compared to previous mean gradient of 3.6 mm Hg 6 months earlier (Figure 1). The pressure half-time was 232 ms. Right ventricular size and function were normal. Reassuringly, the patient’s chest pain rapidly resolved without specific intervention, and in the absence of hypoxia or tachycardia, pulmonary embolism was thought to be unlikely. CTA was therefore deferred, and decision was made to perform transesophageal echocardiography (TEE) for new diagnosis of mechanical valve obstruction. This revealed a large burden of soft echogenic material covering and extending into the prosthesis with new moderate transvalvular TR, which was most consistent with mechanical tricuspid valve thrombosis (Video 2A, Video 2B).
Figure 1.
Elevated Peak and Mean Prosthetic Tricuspid Valve Gradients
Transthoracic echocardiogram with continuous-wave Doppler across the mechanical tricuspid valve (TV) in the apical 4-chamber view, demonstrating elevated velocity and mean gradient. Pressure half-time was 230 ms, consistent with valvular obstruction.
Question 2: What is the incidence of mechanical tricuspid valve thrombosis, and what clinical findings aid in diagnosis and inform treatment options?
Thrombosis is a well described complication in mechanical tricuspid valves, occurring more frequently than in valves in the aortic position at a rate of anywhere from 0.5% to 6.8% per patient-year.1,2 TTE is critical for early identification of valvular obstruction, first evidenced by an elevated early tricuspid peak velocity ≥1.9 m/s and mean tricuspid pressure gradient ≥6 mm Hg, with or without evidence of leaflet thickening or mobile echogenic material. Prolonged pressure half-time ≥230 ms is also supportive of the diagnosis.3 When suspected, confirming the diagnosis of obstruction and determining the cause requires careful history and a multimodality imaging approach. Use of both TTE and fluoroscopy has been shown to be superior to either modality alone to confirm prosthetic dysfunction.4 On history, acute onset of symptoms, missed doses of anticoagulation, or frequently subtherapeutic INR are more suggestive of thrombus. TEE and chest computed tomography further help to distinguish thrombus from pannus or patient-prosthesis mismatch. This crucial distinction can inform major treatment decisions, including whether thrombolytic therapy can be considered.5 Importantly, the risk of mechanical valve thrombosis is lifelong, especially given that intentional or unintentional suspension of anticoagulation is not uncommon. Clinicians must therefore remain vigilant for this complication in all patients with prosthetic valves and emphasize the importance of minimizing interruption to anticoagulation as much as possible.
Question 3: What are the treatment options for acute mechanical valve thrombosis?
Mechanical valve thrombosis can be managed with either surgical intervention or thrombolysis, with American Heart Association (AHA) and European Society of Cardiology (ESC) guidelines conflicting on the optimal approach to management.5,6 Given the paucity of data available to guide management on right-side valve thrombosis specifically, a multidisciplinary team approach is needed. Current AHA guidelines only recommend the use of a slow infusion of low-dose thrombolytics as first-line therapy for symptomatic left-side mechanical valve thrombosis, with equal consideration for emergency surgery based on patient clinical factors (such as hemodynamic instability or NYHA functional class III/IV symptoms) and local expertise (Class Ib).5 Whereas the AHA guidelines do not address right-side mechanical valve thrombosis, the ESC guidelines support the use of fibrinolysis in this context (Class IIb).6 As a result, there is now a small but growing body of evidence demonstrating the success of fibrinolytics for mechanical tricuspid prostheses, especially in patients at increased operative risk and without indications for emergency surgical intervention.7, 8, 9, 10
Our patient was admitted to the intensive care unit, and a multidisciplinary heart team was consulted. Reassuringly, his chest pain resolved at the time of admission. Because he was hemodynamically stable without any clinical evidence of heart failure, the decision of the heart team was to treat the valve thrombosis with ultraslow low-dose infusion of tPA (25 mg over 25 hours). Limited TTE after infusion showed evidence of improving mean gradient (6 mm Hg), and after another heart team meeting, a second infusion of ultraslow low-dose tPA was given per the protocol established in recent scientific literature.7 TEE and fluoroscopy performed the following day showed no residual thrombus or regurgitation (Video 3A, Video 3B) and normal disc motion (Video 4A, Video 4B) with appropriate opening and closing angles for the type of prosthesis (85º and 35º, respectively). The patient was bridged to warfarin with unfractionated heparin, educated on the mechanism of action of warfarin, and advised to avoid all vitamin K–containing supplementation. Before discharge, TTE demonstrated complete resolution of obstruction and TR: mean gradient was 2.5 mm Hg, pressure half-time 133 ms, and no TR (Figure 2). The patient returned for outpatient evaluation 1 month later with no recurrence of chest pain or dyspnea, and his weekly INR remained in therapeutic range.
Figure 2.
Normalization of Peak and Mean Prosthetic Tricuspid Valve Gradients
Transthoracic echocardiogram with continuous-wave Doppler across the mechanical tricuspid valve (TV) in the right ventricular inflow tract view, demonstrating normal velocity and improvement in peak and mean gradients.
Question 4: What different types, doses, and infusion rates of thrombolytics are recommended for treating prosthetic valve thrombosis?
Though data in tricuspid valve thrombosis specifically are sparse, successful outcomes have been described with a variety of doses and types of thrombolytics (Table 1). In an effort to reduce bleeding complications while ensuring successful outcomes, recent studies have focused on lower thrombolytic doses with repeated infusions as needed and slower infusion rates. Ozkan et al described the first multicenter observational study comparing slow (6-hour) and ultraslow (25-hour) low-dose (25 mg) alteplase infusions vs surgical intervention in 158 patients with prosthetic valve thrombosis in any position, including 9 cases of tricuspid valve thrombosis. The authors were able to demonstrate promising rates of success (90.4%) and dramatic reduction in rates of major complications, minor complications, duration of hospital stay, and 3-month mortality.7 Although further investigation is still needed, these promising results support the use of thrombolytics as a viable treatment option for right-side prosthetic valve thrombosis in patients at elevated surgical risk.
Table 1.
Cases of Mechanical Tricuspid Valve Thrombosis Treated With Thrombolyticsa
| First Author | Year | N | Dose(s) | Success |
|---|---|---|---|---|
| Ozkan et al1 | 2022 | 9 | Bolus: none Infusion: alteplase 25 mg/25 h Max: 200 mg Bolus: none Infusion: alteplase 25 mg/6 h Max: 200 mg |
90.4% (all valves) |
| Zaghloul et al2 | 2018 | 1 | Bolus: alteplase 2 mg (catheter-directed) Infusion: alteplase 24 mg/24 h |
0% |
| Ozkan et al3 | 2015 | 4 | Bolus: none Infusion: alteplase 25 mg/25 h Max: 200 mg |
100% |
| Taherkhani et al4 | 2015 | 8 | Patients >30 kg: Bolus: alteplase 15 mg Infusion: alteplase 30 mg/0.5 h followed by 50 mg/h Bolus: streptokinase 200,000 IU Infusion: 100,000 IU/h Max: 72 h Patients <30 kg: Bolus: none Infusion: alteplase 0.3 mg/kg/h Max: NR; median duration 12 h |
75% |
| Ozkan et al5 | 2013 | 14 | Bolus: alteplase 10 mg Infusion: alteplase 90 mg/5 h Max: 200 mg Bolus: none Infusion: alteplase 50 mg/6 h Max: 150 mg Bolus: none Infusion: alteplase 25 mg/6 h Max: 150 mg |
78.6% |
| Zhang et al6 | 2011 | 1 | Bolus: alteplase 2 mg (catheter-directed) Infusion: alteplase 6 mg/6 h (catheter-directed) followed by 8 mg/6 h (catheter-directed) |
100% |
| Kaul et al7 | 2009 | 1 | Bolus: none Infusion: alteplase 100 mg/3 h |
100% |
| Roudaut et al8 | 2009 | 2 | NR | 100% |
| Caceres-Loriga et al9 | 2006 | 9 | Bolus: streptokinase 250,000 IU Infusion: streptokinase 100,000 IU/h Max: 72 h |
100% |
| Tong et al10 | 2004 | 15 | Bolus: none Infusion: streptokinase (dose NR) Max: 120 h Bolus: none Infusion: urokinase (dose NR) Max: 48 h Bolus: alteplase 10 mg Infusion: alteplase 90 mg/2-6 h Max: 120 h |
93.3% |
| Roudaut et al11 | 2003 | 1 | NR | 100% |
| Ramos et al12 | 2003 | 4 | Bolus: streptokinase 250,000 IU Infusion: streptokinase 100,000 IU/h Max: 72 h |
75% |
| Lopez et al13 | 2002 | 2 | Bolus: streptokinase 250,000 IU Infusion: 100,000 IU/h Max: 103 h |
100% |
NR = not reported.
References are listed in the Supplemental Appendix. Only cases published since 2000 are listed.
Funding Support and Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For supplemental table references and videos, please see the online version of this paper.
Appendix
Fluoroscopy of Thrombosed Mechanical Tricuspid Valve
Anterior-posterior fluoroscopy of the mechanical tricuspid valve, demonstrating severe restriction of valve leaflets with complete immobility of one leaflet.
Transesophageal Echocardiogram Showing the Right Heart Chambers With a Well Seated Bileaflet Tilting Disc Mechanical Prosthesis Across the Tricuspid Annulus
(A) The discs are immobile during cardiac cycle and appear to be covered by a soft echo dense layer which extends into the valve ring, most consistent with an acute thrombus that is obstructing the valve. The right ventricle is not well seen owing to the shielding artifact caused by the mechanical discs. (B) Color Doppler across the prosthesis shows turbulent flow in diastole consistent with elevated velocities seen on spectral Doppler. Normal washing jets are replaced by pathologic valvular regurgitation caused by partially open and immobile discs.
Transesophageal Echocardiogram Showing the Right Heart Chambers With a Well Seated Bileaflet Tilting Disc Mechanical Prosthesis Across the Tricuspid Annulus
(A) The discs are immobile during cardiac cycle and appear to be covered by a soft echo dense layer which extends into the valve ring, most consistent with an acute thrombus that is obstructing the valve. The right ventricle is not well seen owing to the shielding artifact caused by the mechanical discs. (B) Color Doppler across the prosthesis shows turbulent flow in diastole consistent with elevated velocities seen on spectral Doppler. Normal washing jets are replaced by pathologic valvular regurgitation caused by partially open and immobile discs.
Normal Tricuspid Valve Bileaflet Motion After Thrombolysis on Transesophageal Echocardiography (TEE)
TEE in the mid-esophageal position at 10°, demonstrating (A) normal leaflet motion and (B) no Doppler evidence of residual tricuspid regurgitation.
Normal Tricuspid Valve Bileaflet Motion After Thrombolysis on Transesophageal Echocardiography (TEE)
TEE in the mid-esophageal position at 10°, demonstrating (A) normal leaflet motion and (B) no Doppler evidence of residual tricuspid regurgitation.
Normal Tricuspid Valve Bileaflet Motion After Thrombolysis on Fluoroscopy
Fluoroscopy showing normal motion of mechanical tricuspid valve tilting discs without evidence of restriction in (A) right anterior oblique and (B) anteroposterior views.6
Normal Tricuspid Valve Bileaflet Motion After Thrombolysis on Fluoroscopy
Fluoroscopy showing normal motion of mechanical tricuspid valve tilting discs without evidence of restriction in (A) right anterior oblique and (B) anteroposterior views.
References
- 1.Lancellotti P., Pibarot P., Chambers J., et al. Recommendations for the imaging assessment of prosthetic heart valves: a report from the European Association of Cardiovascular Imaging endorsed by the Chinese Society of Echocardiography, the Inter-American Society of Echocardiography, and the Brazilian Department of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2016;17(6):589–590. doi: 10.1093/ehjci/jew025. [DOI] [PubMed] [Google Scholar]
- 2.Dangas G.D., Weitz J.I., Giustino G., et al. Prosthetic heart valve thrombosis. J Am Coll Cardiol. 2016;68:2670–2689. doi: 10.1016/j.jacc.2016.09.958. [DOI] [PubMed] [Google Scholar]
- 3.Zhu X., Luo Y., Zhang E., et al. Ten-year experience of tricuspid valve replacement with the St. Jude medical valve. Sci Rep. 2018;8(1) doi: 10.1038/s41598-018-35142-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Muratori M., Fusini L., Ghulam Ali S., et al. Detection of mechanical prosthetic valve dysfunction. Am J Cardiol. 2021;150:101–109. doi: 10.1016/j.amjcard.2021.03.055. [DOI] [PubMed] [Google Scholar]
- 5.Otto C.M., Nishimura R.A., Bonow R.O., et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2021;77(4):e25–e197. doi: 10.1016/j.jacc.2020.11.018. [DOI] [PubMed] [Google Scholar]
- 6.Vahanian A., Beyersdorf F., Praz F., et al. 2021 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J. 2022;43(7):561–632. doi: 10.1093/eurheartj/ehab395. [DOI] [PubMed] [Google Scholar]
- 7.Ozkan M., Gunduz S., Guner A., et al. Thrombolysis or surgery in patients with obstructive mechanical valve thrombosis: the multicenter HATTUSHA study. J Am Coll Cardiol. 2022;79(10):977–989. doi: 10.1016/j.jacc.2021.12.027. [DOI] [PubMed] [Google Scholar]
- 8.Betancur-Gutierrez A., Bayon-Fernandez J., Garcia-Rodriguez M.A., Garcia-Egido A., Garrote-Coloma C., Fernandez-Vazquez F. Thrombosis of a mechanical tricuspid valve prothesis resolved with fibrinolysis. Rev Esp Cardiol (Engl Ed) 2014;67(12):1064–1066. doi: 10.1016/j.rec.2014.07.018. [DOI] [PubMed] [Google Scholar]
- 9.Ozkan M., Cakal B., Karakoyun S., et al. Thrombolytic therapy for the treatment of prosthetic heart valve thrombosis in pregnancy with low-dose, slow infusion of tissue-type plasminogen activator. Circulation. 2013;128(5):532–540. doi: 10.1161/CIRCULATIONAHA.113.001145. [DOI] [PubMed] [Google Scholar]
- 10.Keuleers S., Herijgers P., Herregods M.C., et al. Comparison of thrombolysis versus surgery as a first line therapy for prosthetic heart valve thrombosis. Am J Cardiol. 2011;107(2):275–279. doi: 10.1016/j.amjcard.2010.09.013. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Fluoroscopy of Thrombosed Mechanical Tricuspid Valve
Anterior-posterior fluoroscopy of the mechanical tricuspid valve, demonstrating severe restriction of valve leaflets with complete immobility of one leaflet.
Transesophageal Echocardiogram Showing the Right Heart Chambers With a Well Seated Bileaflet Tilting Disc Mechanical Prosthesis Across the Tricuspid Annulus
(A) The discs are immobile during cardiac cycle and appear to be covered by a soft echo dense layer which extends into the valve ring, most consistent with an acute thrombus that is obstructing the valve. The right ventricle is not well seen owing to the shielding artifact caused by the mechanical discs. (B) Color Doppler across the prosthesis shows turbulent flow in diastole consistent with elevated velocities seen on spectral Doppler. Normal washing jets are replaced by pathologic valvular regurgitation caused by partially open and immobile discs.
Transesophageal Echocardiogram Showing the Right Heart Chambers With a Well Seated Bileaflet Tilting Disc Mechanical Prosthesis Across the Tricuspid Annulus
(A) The discs are immobile during cardiac cycle and appear to be covered by a soft echo dense layer which extends into the valve ring, most consistent with an acute thrombus that is obstructing the valve. The right ventricle is not well seen owing to the shielding artifact caused by the mechanical discs. (B) Color Doppler across the prosthesis shows turbulent flow in diastole consistent with elevated velocities seen on spectral Doppler. Normal washing jets are replaced by pathologic valvular regurgitation caused by partially open and immobile discs.
Normal Tricuspid Valve Bileaflet Motion After Thrombolysis on Transesophageal Echocardiography (TEE)
TEE in the mid-esophageal position at 10°, demonstrating (A) normal leaflet motion and (B) no Doppler evidence of residual tricuspid regurgitation.
Normal Tricuspid Valve Bileaflet Motion After Thrombolysis on Transesophageal Echocardiography (TEE)
TEE in the mid-esophageal position at 10°, demonstrating (A) normal leaflet motion and (B) no Doppler evidence of residual tricuspid regurgitation.
Normal Tricuspid Valve Bileaflet Motion After Thrombolysis on Fluoroscopy
Fluoroscopy showing normal motion of mechanical tricuspid valve tilting discs without evidence of restriction in (A) right anterior oblique and (B) anteroposterior views.6
Normal Tricuspid Valve Bileaflet Motion After Thrombolysis on Fluoroscopy
Fluoroscopy showing normal motion of mechanical tricuspid valve tilting discs without evidence of restriction in (A) right anterior oblique and (B) anteroposterior views.