Abstract
To evaluate the efficacy of cognitive behavioural therapy (CBT) as a psychological intervention for elderly patients with extensive burns, focusing on its impact on emotional well‐being, self‐efficacy and quality of life. A prospective, randomized study involving 200 elderly burn patients was conducted from November 2021 to January 2023. The patients were randomly assigned to receive either standard care (control group) or burn care based on cognitive behavioural therapy (CBT‐B) (study group), with 100 patients in each group. Outcome measures included the Visual Analog Scale (VAS) for pain assessment, 36‐item Short Form Survey (SF‐36) for quality of life, General Self‐Efficacy Scale (GSES) and Rosenberg Self‐Esteem Scale (RSES). The study revealed that CBT‐based intervention significantly reduced anxiety and depression scores compared with standard care (p < 0.05). Additionally, patients in the CBT group exhibited improved self‐efficacy, self‐esteem and quality of life (p < 0.05). CBT proves to be a valuable intervention for elderly burn patients, effectively addressing emotional distress and enhancing their psychological well‐being. By modifying negative cognitive patterns, providing coping mechanisms and fostering problem‐solving skills, CBT‐based care contributes to a more positive recovery experience and improved quality of life.
Keywords: cognitive behavioural therapy, elderly burn patients, emotional well‐being, quality of life, self‐efficacy
1. INTRODUCTION
Extensive burns in the elderly are a severe physical trauma that imposes critical physical and psychological impact on the patient, 1 , 2 including alterations in physical appearance, functional loss, pain and social difficulties. These may give rise to negative emotions such as anxiety, depression and low self‐esteem. 3 , 4 , 5 Therefore, effective psychological interventions are essential to improve the psychological well‐being of elderly patients with extensive burns.
Cognitive behavioural therapy (CBT) has been extensively employed in the treatment of various psychological distress and post‐traumatic stress disorders due to its notable effectiveness. Cognitive behavioural therapy ameliorates the emotions and behaviours of patients by proactively assisting individuals in recognizing and eliminating negative thoughts and daily habits. 6 , 7 , 8 , 9 , 10 , 11 Nevertheless, there has been relatively limited research on the use of CBT, especially in terms of emotional improvement, for elderly patients with extensive burns.
Thus, this study was performed to investigate the effects of a psychological regimen based on CBT on emotional improvement in elderly patients with extensive burns. We hope to alleviate the prevalent negative emotions such as anxiety, depression and self‐doubt of patients after experiencing extensive burns through systematic intervention measures, thereby enhancing their mental health and quality of life. The significance of this study lies in enriching the research on psychological intervention for elderly patients with extensive burns and providing an effective intervention alternative for rehabilitation teams. By understanding the effectiveness of CBT in elderly burn patients, we can offer guidance for clinical practice and further contribute to the development of psychological intervention methods in the rehabilitation of elderly patients with extensive burns.
This study is structured as follows: firstly, we reviewed relevant literature, explored the impact of extensive burns on mental health in the elderly and summarized the previous effective applications of CBT in analogous psychological distress cases. Then, we provided detailed descriptions of the research methodology, including participant selection criteria, intervention measures, data collection and analysis methods. Subsequently, we presented the research results and conducted in‐depth interpretations. Finally, we summarized the main findings of the study and put forward recommendations for clinical practice and future research.
2. PATIENTS AND METHODS
2.1. Study design
This is a prospective, randomized study, in compliance with the Helsinki Declaration, and has received approval from the Institutional Review Board. A total of 200 burn patients admitted to our hospital from November 2021 to January 2023 were included in this study. All patients were elderly individuals who provided informed consent and signed a consent form, which has been ratified by the Institutional Review Board. To achieve a familywise error rate of less than 0.05, a power analysis was conducted, and a sample size of 100 patients per group was determined to be sufficient for difference analysis. After obtaining consent, patients were randomly assigned in a 1:1 ratio to receive either standard care (control group) or burn care based on cognitive behavioural therapy (CBT‐B) (study group), with 100 patients in each group.
2.2. Inclusion and exclusion criteria
2.2.1. Inclusion criteria
The participants in this study were individuals aged 65 years or older. They had sustained burns where the total body surface area (TBSA) affected ranged from 15% to 20%. These burns penetrated beyond the surface layers, reaching into the dermal and, in some cases, even the muscular layers. The causes of these burns were attributed to incidents involving fire, scalding with hot liquids or exposure to chemical substances. These injuries were not the result of intentional self‐harm or any other non‐accidental circumstances. Additionally, these individuals did not have any other significant underlying health issues or complications and were deemed suitable candidates for receiving comprehensive and complex treatment and care.
2.2.2. Exclusion criteria
Patients with severe complications, such as severe complications of the heart, lungs or kidneys, multi‐organ failure or severe physical debilitation were deemed ineligible for study recruitment. Moreover, patients who were considered unsuitable for complex surgical interventions or other treatment measures by preoperative assessment were also excluded.
2.3. Nursing interventions
2.3.1. Control group: Standard care
Injury assessment: The medical staff assessed the extent of the burns, including determining the area, depth and severity of the injuries. This aided in formulating subsequent treatment and care plans.
Treatment of burned areas: The medical staff cleaned the burn surface, removed residual burned tissue and performed necessary wound debridement.
Wound coverage and dressing changes: The medical staff used appropriate dressings to cover the burn wounds to prevent infection and promote wound healing. Dressings were typically sterile gauze or other suitable dressing materials. The frequency of dressing changes depended on the severity of the burns and the recommendations of the medical team.
Pain management: Due to the higher sensitivity of elderly individuals to pain, the medical staff performed appropriate pain management measures based on the patient's level of pain, such as oral analgesics and topical anaesthetic ointment.
Fluid and nutritional support: Extensive burns might lead to fluid loss and metabolic disturbances. The medical staff monitored the patient's fluid balance and nutritional status and provided appropriate fluid and nutritional support as needed, including intravenous fluids and nutritional supplements.
Infection prevention and treatment: Burn patients were prone to infection, especially in elderly individuals with potentially weakened immune functions. The medical staff closely monitored the wounds, maintained wound cleanliness, performed appropriate disinfection and administered antibiotics as needed for infection prevention.
2.3.2. Study group: Cognitive behavioural therapy
Phase 1 (Duration: one day)—Individualized treatment plan
Tailored treatment plans were formulated based on each patient's burn severity, personal characteristics and specific needs. This ensured that the plan catered to the unique requirements of each patient and could be adjusted flexibly to accommodate changes during the rehabilitation process.
Phase 2 (Duration: one week)—Health education and emotional management
Detailed education on burn recovery was provided, covering aspects such as physiological recovery after burns, pain management, wound care and activity limitations. Additionally, emotional management techniques were taught, including emotion recognition and regulation.
Phase 3 (Duration: three days)—Cognitive reconstruction
Cognitive reconstruction was employed to assist patients in dealing with negative emotions and pessimistic thoughts. The patients were instructed to recognize potential irrational thoughts, such as overgeneralization, magnification and dichotomous thinking, helping them to view themselves and the burn incident in a more positive and objective manner.
Phase 4 (Duration: one day)—Confidence and self‐esteem restoration
Support was provided to help patients rebuild confidence and self‐esteem. They were encouraged to engage in activities that aligned with their abilities and comfort levels, such as rehabilitation exercises, social activities and hobbies. Positive feedback and recognition were offered to aid them in re‐establishing a positive self‐evaluation.
Phase 5 (Duration: two days)—Psychological management techniques
Patients were taught techniques to cope with potential anxiety, fear and pain following the burn. This included deep breathing, progressive muscle relaxation, mindfulness practices and distraction methods. These skills assist patients in relaxing both their mind and body, alleviating pain and anxiety.
Phase 6 (Duration: one day)—Family support
The medical staff communicated with the patient's family members and caregivers to help them understand and support the patient's rehabilitation process. Family support and resources, such as family meetings, family therapy or support groups, were provided to address challenges during family care.
Phase 7 (Duration: one day)—Rehabilitation transition plan
A rehabilitation transition plan was formulated for the patient before discharge. This plan included rehabilitation goals, recommendations for continued treatment and arrangements for long‐term psychological support. This ensured that patients received necessary psychological intervention and rehabilitation services after discharge.
Phase 8 (Duration: one day)—Regular re‐assessment
The psychological status and progress of patients were regularly monitored, with adjustments and interventions made as needed. This ensured that patients received continuous psychological support and attention throughout the rehabilitation process.
2.4. Outcome measures
2.4.1. Visual Analog Scale 12
The Visual Analog Scale (VAS) was used to measure burn pain. Scores were recorded by placing a handwritten mark on a 10‐centimetre line, which signifies a spectrum ranging from ‘no pain (0 points)’ to ‘most severe pain (10 points)’. Specifically, mild pain is represented by 1–3 points, moderate pain by 4–7 points and severe pain by 8–10 points. Higher scores indicate greater pain severity. The test–retest reliability of VAS is 0.89.
2.4.2. Quality of life 13
The 36‐item Short Form Survey (SF‐36) questionnaire assesses patient's quality of life. It consists of 36 questions covering eight health domains: physical functioning (10 questions), role limitations due to physical health (4 questions), role limitations due to emotional health (3 questions), bodily pain (2 questions), general health perceptions (5 questions), vitality (4 questions), social functioning (2 questions), mental health (5 questions) and one question about health change. Scores range from 0 to 100 for each domain, with 100 indicating the best perceived quality of life.
2.4.3. Self‐efficacy 14
Participants completed the General Self‐efficacy Scale (GSES) before baseline care and after care completion. The GSES is a validated self‐management tool consisting of 10 items designed to assess self‐efficacy or the belief in one's ability to successfully cope with demands in life. Individual item scores are summed to obtain a total GSES score ranging from 10 to 40. Higher scores indicate stronger self‐efficacy.
2.4.4. Rosenberg self‐esteem scale 15 , 16
Participants completed the Rosenberg Self‐esteem Scale (RSES) before baseline care and after care completion. The RSES is a validated self‐management scale comprising 10 items used to assess self‐worth. Individual item scores are summed to obtain a total RSES score ranging from 0 to 30. Scores below 15 suggest potential self‐esteem issues, 15–25 indicate typical self‐esteem and 26–30 signify high self‐esteem.
2.4.5. Social Skill Rating Scale (SSRS) 17
The scale was compiled by Xiao et al. with a total of 10 items, including three dimensions of subjective support, objective support and utilization of support. The scale comprises items categorized into subjective support (items 1, 3, 4 and 5), objective support (items 2, 6 and 7) and support utilization degree (items 8, 9 and 10). Scoring involves a range of 1–4 for items 1–4 and 8–10, with respondents making single‐choice selections. The 5th item offers options A, B, C and D, each yielding a total score from 1 to 4, reflecting the extent of support. These scores range from minimal to full support. Items 6 and 7 are rated as 0 if ‘no source’ is selected, while respondents indicating ‘the following sources’ can choose multiple sources. The total scale score is the cumulative score across the three dimensions, with higher scores indicating greater social support. Judging by the criteria, a total score of ≤22 denotes a low level, 23–44 signifies a moderate level and 45–66 suggests a high level. The domestic norm score stands at 34.56 ± 3.73.
2.4.6. Hamilton Anxiety/Depression Rating Scale (HAMA/D) 18
From pre‐care to post‐care, both groups of patients were assessed using HAMD and HAMA. These two scales were to assess the severity of depression and anxiety. HAMD 19 items are scored on a 5‐point Likert scale (0–4 points), with a total score ranging from 0 to 68 points. Higher scores indicate more severe depressive symptoms. The total Cronbach's alpha coefficient for HAMD is 0.89 (95% CI 0.86–0.92). HAMA consists of 14 items, scored on a 5‐point Likert scale (0–4), with a total score range of 0–56 points. Higher scores indicate more severe anxiety symptoms.
2.4.7. Complications
Complications may include systemic infections, pulmonary infections, stress ulcers, acute renal failure, heart failure and multi‐organ dysfunction.
2.5. Quality control
Caregivers distributed survey questionnaires to patients, ensuring they were completed independently without any interference. A total of 200 questionnaires were distributed and subsequently collected, resulting in a 100% response rate. The data from the questionnaires were transcribed, calculated and coded by two independent investigators.
2.6. Statistical analysis
Measurement data in this study were presented as mean ± standard deviation and analysed using the t‐test. Count and ordinal data were presented as percentages and subjected to the χ 2 test. Statistical tests in this study were performed using SPSS 22.0 software. GraphPad Prism v. 6 (GraphPad Software, La Jolla, CA, USA) was utilized for data analysis and figure processing. All tests were two‐tailed, with a significance level set at α = 0.05.
3. RESULTS
3.1. Baseline profiles
The two groups were well‐balanced in terms of baseline characteristics (p > 0.05), as shown in Table 1.
TABLE 1.
Patient characteristics.
| Control group | Study group | t/χ 2 | p | |
|---|---|---|---|---|
| n | 100 | 100 | ||
| Gender (n) | 1.557 | 0.212 | ||
| Male | 66 | 62 | ||
| Female | 34 | 38 | ||
| Age ( ± s, years old) | 67.55 ± 12.05 | 68.18 ± 13.25 | 2.092 | 0.321 |
| Cause of burns (n) | 1.562 | 0.211 | ||
| Chemical exposure | 21 | 19 | ||
| Fire | 48 | 50 | ||
| Scalding | 31 | 31 | 2.066 | 0.356 |
| BMI | 23.21 ± 3.01 | 22.90 ± 3.21 | ||
| Burn area | 43.65 ± 5.01 | 43.90 ± 5.67 |
3.2. VAS scores
Before care, the two groups showed similar VAS scores (p > 0.05). After care, patients receiving CBT‐based nursing had significantly stronger pain mitigation than those with standard care (p < 0.05), as depicted in Figure 1.
FIGURE 1.
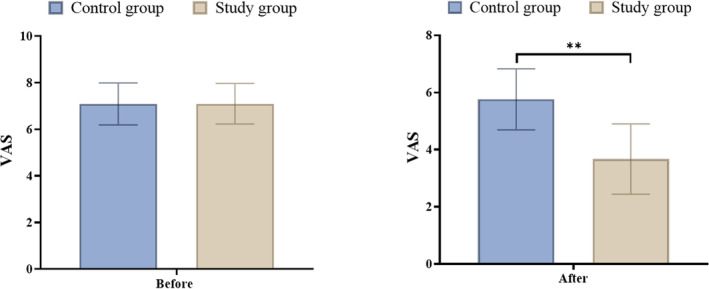
VAS scores. **Represents a statistical difference.
3.3. SSRS scores
Before care, similar SSRS scores were observed between the two groups (p > 0.05). Following care, patients given CBT‐based care exhibited significantly higher social skill levels compared to those receiving conventional care, as evidenced by the higher SSRS scores in the study group (p < 0.05), as illustrated in Figure 2.
FIGURE 2.
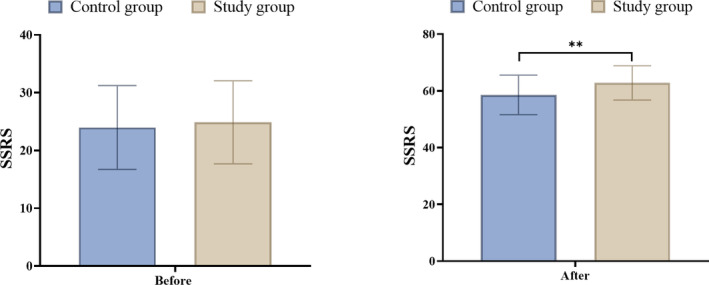
SSRS scores. **Represents a statistical difference.
3.4. HAMA and HAMD scores
Prior to the nursing care, the two groups of patients showed similar psychosocial health conditions, as suggested by the similar HAMA and HAMD scores (p > 0.05). After care, significant mitigation in negative emotions was observed in the two groups of patients, and the CBT‐based therapy appeared to provide more alleviation in negative emotions of patients than routine care (p < 0.05), as shown in Figure 3, where the study group showed significantly lower HAMA and HAMD scores than the control group.
FIGURE 3.
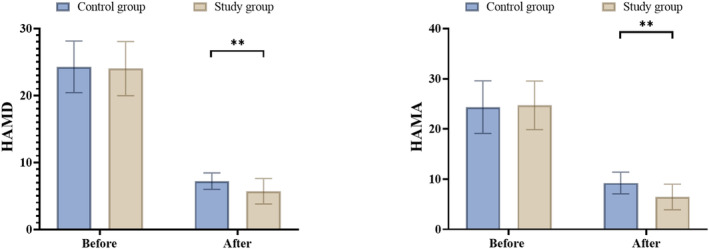
HAMA and HAMD scores. **Represents a statistical difference.
3.5. GSES and RSES scores
Before care, patients in both groups showed similar self‐efficacy and self‐esteem levels (p > 0.05). After care, the significantly higher GSEA and RSES scores in the study group compared with the control group suggested higher self‐efficacy and self‐esteem of patients after CBT‐based care (p < 0.05), as depicted in Figure 4.
FIGURE 4.
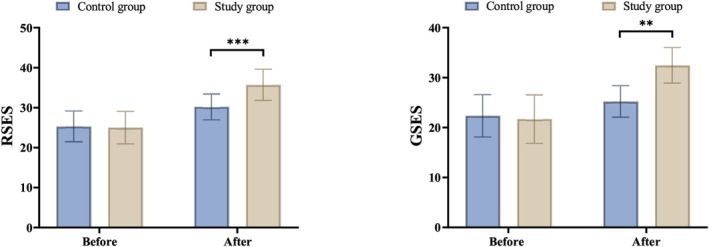
GSES and RSES scores. **Represents a statistical difference.
3.6. SF‐36 scores
Before care, no significant differences were obtained in the SF‐36 scores between the two groups (p > 0.05). After care, patients receiving CBT‐based care exhibited significantly higher quality of life scores than those with routine care (p < 0.05), as shown in Table 2.
TABLE 2.
SF‐36 scores of the two groups.
| Control group | Study group | t | p | |
|---|---|---|---|---|
| n | 100 | 100 | ||
| General health | ||||
| Before | 56.76 ± 20.78 | 57.06 ± 19.98 | ||
| After | 66.86 ± 20.98 | 68.89 ± 20.76 | 15.67 | <0.001 |
| Physical functioning | ||||
| Before | 91.45 ± 5.69 | 90.95 ± 5.60 | ||
| After | 94.22 ± 4.88 | 97.32 ± 5.01 | 23.29 | <0.001 |
| Role‐physical | ||||
| Before | 73.11 ± 20.69 | 74.11 ± 19.89 | ||
| After | 87.90 ± 18.22 | 89.92 ± 20.32 | 22.11 | <0.001 |
| Bodily pain | ||||
| Before | 63.34 ± 25.67 | 62.39 ± 25.71 | ||
| After | 67.38 ± 20.33 | 78.87 ± 21.88 | 7.954 | <0.001 |
| Social functioning | ||||
| Before | 66.34 ± 18.24 | 67.04 ± 18.21 | ||
| After | 76.76 ± 8.02 | 80.09 ± 7.32 | 10.672 | <0.001 |
| Role‐emotional | ||||
| Before | 65.32 ± 21.76 | 64.82 ± 22.05 | ||
| After | 77.43 ± 27.34 | 81.82 ± 25.87 | 9.986 | <0.001 |
| Mental health | ||||
| Before | 64.57 ± 14.98 | 63.77 ± 15.02 | ||
| After | 69.80 ± 12.34± | 71.23 ± 11.56 | 10.652 | <0.001 |
| Vitality | ||||
| Before | 56.98 ± 14.76 | 57.06 ± 15.16 | ||
| After | 59.90 ± 11.67 | 62.88 ± 13.78 | 16.870 | <0.001 |
3.7. Complications
There were no statistically significant differences observed between the two groups in terms of complications, including systemic infection, pulmonary infection, stress ulcers, acute renal failure, heart failure and multi‐organ dysfunction (p > 0.05).
4. DISCUSSION
Elderly individuals who experience extensive burns often face significant physical and emotional challenges. Emotional issues such as anxiety, depression and fear can have severe repercussions on their recovery and quality of life. In such cases, psychological interventions based on cognitive behavioural therapy can play a crucial role in improving the emotional well‐being of elderly patients.
4.1. Eliminating negative cognitive patterns
The results of this study demonstrated that both groups of patients showed significant reductions in HAMA and HAMD scores after care, with the observation group displaying lower scores than the control group. This finding is consistent with the results of the study by Meyerhoff et al. 10 The core principle of CBT is that emotions and behaviours are influenced by the response patterns to events. Cognitive behavioural therapy can help elderly patients identify and modify negative cognitive patterns, such as overgeneralization, self‐blame or feelings of helplessness.
4.2. Coping with anxiety and fear
This study substantiated that CBT‐based care provided significant improvements in the social skills of patients than conventional care. Extensive burns may lead to anxiety and fear in elderly patients during the recovery process. The CBT‐based regimen helps patients confront these fears and anxieties by teaching coping skills such as deep breathing, relaxation training and systematic desensitization. 20
4.3. Enhancing problem‐solving abilities
The study findings indicated that both groups of patients showed significant increases in GSES and RSES scores after care, and patients receiving CBT‐based care showed higher self‐efficacy and self‐esteem than the controls. The CBT care protocol provides tools and techniques for problem‐solving, helping elderly patients deal with challenges and difficulties in the recovery process. By teaching problem‐solving strategies such as goal setting, breaking down problems, formulating action plans and evaluating outcomes, CBT can strengthen the self‐efficacy and coping abilities of elderly patients, reducing their emotional distress. 21
4.4. Improving self‐awareness and self‐care
After care, patients receiving CBT‐based nursing had significantly stronger pain mitigation and higher quality of life than those with standard care. This is consistent with the results of the study by Cherkin et al. 6 CBT promotes physical and psychological recovery by helping patients cultivate positive self‐awareness and self‐care habits, such as self‐acceptance and self‐esteem enhancement, and proactive self‐care behaviours.
5. LIMITATIONS
Firstly, the data collected through questionnaires such as SF‐36 and RSES are self‐reported, so caution is needed when interpreting the study results. Additionally, the sample size in our study is relatively small, which remains a potential limitation. Given these limitations, our study results should be considered exploratory, and follow‐up studies are necessitated for verification.
6. CONCLUSION
Psychological intervention based on CBT provides powerful tools and strategies for improving the emotional well‐being of elderly patients with extensive burns. By helping patients change negative cognitive patterns, cope with anxiety and fear, enhance problem‐solving abilities and improve self‐awareness and self‐care, CBT‐based care can facilitate the recovery process and enhance the psychological well‐being and quality of life of elderly patients. However, individual differences and the personalization of intervention plans should be emphasized to ensure the effectiveness and adaptability of CBT.
FUNDING INFORMATION
No external funding received to conduct this study.
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no competing interests.
ACKNOWLEDGEMENTS
We are particularly grateful to all the people who have given us help on our article.
Yu H‐M, Wang L, Pan C‐Z. The impact of cognitive behavioural therapy‐based psychological intervention on emotional improvement in elderly patients with extensive burns. Int Wound J. 2024;21(2):e14594. doi: 10.1111/iwj.14594
DATA AVAILABILITY STATEMENT
The relevant supporting data are available from the author upon request.
REFERENCES
- 1. Jeschke MG, van Baar ME, Choudhry MA, Chung KK, Gibran NS, Logsetty S. Burn injury. Nat Rev Dis Primers. 2020;6(1):11. doi: 10.1038/s41572-020-0145-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Greenhalgh DG. Management of burns. N Engl J Med. 2019;380(24):2349‐2359. doi: 10.1056/NEJMra1807442 [DOI] [PubMed] [Google Scholar]
- 3. Houschyar M, Borrelli MR, Tapking C, et al. Burns: modified metabolism and the nuances of nutrition therapy. J Wound Care. 2020;29(3):184‐191. doi: 10.12968/jowc.2020.29.3.184 [DOI] [PubMed] [Google Scholar]
- 4. Gacto‐Sanchez P. Surgical treatment and management of the severely burn patient: review and update. Med Intensiva. 2017;41(6):356‐364. English, Spanish. doi: 10.1016/j.medin.2017.02.008 [DOI] [PubMed] [Google Scholar]
- 5. Young AW, Dewey WS, King BT. Rehabilitation of burn injuries: an update. Phys Med Rehabil Clin N Am. 2019;30(1):111‐132. doi: 10.1016/j.pmr.2018.08.004 [DOI] [PubMed] [Google Scholar]
- 6. Cherkin DC, Sherman KJ, Balderson BH, et al. Effect of mindfulness‐based stress reduction vs cognitive behavioral therapy or usual care on Back pain and functional limitations in adults with chronic low Back pain: a randomized clinical trial. JAMA. 2016;315(12):1240‐1249. doi: 10.1001/jama.2016.2323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sprich SE, Safren SA, Finkelstein D, Remmert JE, Hammerness P. A randomized controlled trial of cognitive behavioral therapy for ADHD in medication‐treated adolescents. J Child Psychol Psychiatry. 2016;57(11):1218‐1226. doi: 10.1111/jcpp.12549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Jiskoot G, Timman R, Beerthuizen A, Dietz de Loos A, Busschbach J, Laven J. Weight reduction through a cognitive behavioral therapy lifestyle intervention in PCOS: the primary outcome of a randomized controlled trial. Obesity (Silver Spring). 2020;28(11):2134‐2141. doi: 10.1002/oby.22980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Milgrom J, Danaher BG, Gemmill AW, et al. Internet cognitive behavioral therapy for women with postnatal depression: a randomized controlled trial of MumMoodBooster. J Med Internet Res. 2016;18(3):e54. doi: 10.2196/jmir.4993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Meyerhoff J, Young MA, Rohan KJ. Patterns of depressive symptom remission during the treatment of seasonal affective disorder with cognitive‐behavioral therapy or light therapy. Depress Anxiety. 2018;35(5):457‐467. doi: 10.1002/da.22739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wood JJ, Sze Wood K, Chuen Cho A, et al. Modular cognitive behavioral therapy for autism‐related symptoms in children: a randomized controlled trial. J Consult Clin Psychol. 2021;89(2):110‐125. doi: 10.1037/ccp0000621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Beletsky A, Lu Y, Nwachukwu BU, et al. Preoperative psychometric properties of visual analog scale assessments for function, pain, and strength compared with legacy upper extremity outcome measures in glenohumeral osteoarthritis. JSES Int. 2020;4:443‐448. doi: 10.1016/j.jseint.2020.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ware JJ, Sherbourne C. The MOS 36‐item short‐form health survey (SF‐36): I. Conceptual framework and item selection. Med Care. 1992;30:473‐483. doi: 10.1097/00005650-199206000-00002 [DOI] [PubMed] [Google Scholar]
- 14. Clavijo M, Yévenes F, Gallardo I, Contreras AM, Santos C. Escala de autoeficacia general: reevaluación de su evidencia de confiabilidad y validez en Chile [the general self‐efficacy scale (GSES): reevaluation of its reliability and validity evidence in Chile]. Rev Med Chil. 2020;148(10):1452‐1460. Spanish. doi: 10.4067/S0034-98872020001001452 [DOI] [PubMed] [Google Scholar]
- 15. Luszczynska A, Scholz U, Schwarzer R. The general self‐efficacy scale: multicultural validation studies. J Psychol. 2005;139:439‐457. doi: 10.3200/JRLP.139.5.439-457 [DOI] [PubMed] [Google Scholar]
- 16. Sinclair SJ, Blais MA, Gansler DA, Sandberg E, Bistis K, LoCicero A. Psychometric properties of the Rosenberg self‐esteem scale: overall and across demographic groups living within the United States. Eval Health Prof. 2010;33:56‐80. doi: 10.1177/0163278709356187 [DOI] [PubMed] [Google Scholar]
- 17. Xiao SY. Theoretical basis and research application of 《social support rating scale》. J Clin Psychiatry. 1994;4(2):98‐100. [Google Scholar]
- 18. Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56‐62. doi: 10.1136/jnnp.23.1.56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. 1959;32(1):50‐55. doi: 10.1111/j.2044-8341.1959.tb00467.x [DOI] [PubMed] [Google Scholar]
- 20. van Loenen I, Scholten W, Muntingh A, Smit J, Batelaan N. The effectiveness of virtual reality exposure‐based cognitive behavioral therapy for severe anxiety disorders, obsessive‐compulsive disorder, and posttraumatic stress disorder: meta‐analysis. J Med Internet Res. 2022;24(2):e26736. doi: 10.2196/26736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Vîslă A, Allemand M, Flückiger C. Within‐ and between‐patients associations between self‐efficacy, outcome expectation, and symptom change in cognitive behavioral therapy for generalized anxiety disorder. J Clin Psychol. 2023;79(1):86‐104. doi: 10.1002/jclp.23407 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The relevant supporting data are available from the author upon request.


