Abstract
Background
Domestic abuse is a widespread health issue that negatively impacts both mental health and quality of life.
Objectives
To determine the prevalence of domestic violence and anxiety among women visiting primary healthcare facilities in the rural Ismailia governorate.
Methods
Between October 2021 and December 2021, a cross-sectional study was conducted. Simple random methods were used to choose the participants from those who attended a clinic. 350 married women were included in the estimated sample size. By using an interview questionnaire, data were gathered including the following parts: The socio-demographic data, designed scale for assessment of violence and anxiety symptoms were assessed by the Hamilton anxiety scale.
Results
The prevalence of domestic violence was 41% and both physical and sexual abuse was 43%. The most predominant sexual abuse was practice without consent (63%). The prevalence of anxiety was 76%, the predominance was mild degree 46% followed by mild to moderate 18%. The significant predictors for anxiety in the total sample were the increase in age of women, rural residence, and exposure to abuse (OR = 11.2 (4.9–25.4). The use of the husband's stimulant drugs was the most predictor factor for women's abuse (OR = 2.3 (1.4–3.9).
Conclusion
forty-one of the women exposed to every form of violence, anxiety was present in more than three-quarters of the studied women. It is essential to screen any wife attending primary health care for the manifestation of domestic violence especially in rural areas and increase the awareness of family physicians towards screening of mental health problems.
Keywords: Women, Anxiety, Domestic violence, Primary health care, Sexual abuse
Introduction
In Egypt, 30% of ever-married women aged 15–49 reported having been ever subjected to at least one episode of physical, sexual, and/or emotional violence [1]. Domestic violence is a common problem among married women, yet this problem is under-researched there are structural and individual level factors that make women vulnerable to violence. While some point to exogenous factors such as poverty, another factor such as husbands' substance abuse may be included [2]. The mental health of abused women, particularly their anxiety, depression, stress, and quality of life, is significantly impacted by domestic violence, whether it be verbal, physical, emotional, or sexual [3]. More than half of the women seen in mental health facilities in Middle Eastern countries are currently being abused by an intimate partner or have experienced such abuse in the past. These women frequently suffer from post-traumatic stress disorder (PTSD), depression, and anxiety, according to specific diagnoses. Physiological, arousal, emotional, cognitive, and memory changes brought on by traumatic events are significant and long-lasting, but they don't always lead to a psychological diagnosis [4]. In Egypt, 30% of ever-married women aged 15–49 reported having been ever subjected to at least one episode of physical, sexual, and/or emotional violence.
Unfortunately, women who are poor and from disadvantaged groups are more likely to experience domestic violence in various communities around the world. Abused women's physical and mental health may suffer significantly because of domestic violence. Additionally, it jeopardizes the victimized women's social, economic, spiritual, and emotional wellbeing well-being. It even has the potential to have an impact on the entire society. It is thought to be a significant factor in the poor health of women [5]. The difficulties with being productive at work and school, with caregiving, with establishing and participating in healthy relationships, and with adapting to change and coping with adversity can all have an impact on survivors' mental health [4]. Several psychological, social, familial, emotional, and systemic factors play a role in substance use disorders (SUDs), which are complex phenomena [5]. Chronic substance use causes a complex set of physiological and neurologic adaptations as well as the development of tolerance to a substance's effects, meaning that users must take more of the substance to get the desired results [6]. The disruption of executive function, the reward pathway, and the stress pathway, which includes the various neurobiological mechanisms triggered in response to stressful stimuli like the “fight or flight” response triggered by the hypothalamic-pituitary-adrenal axis, all increase with increased substance use. These disturbances cause husbands to become irate and aggressive, and they may engage in criminal behavior or domestic violence against their family members, particularly their wives [6]. Egypt's healthcare system is characterized by a mix of public and private providers. Access to care varies, with urban areas generally having better-equipped facilities. Public healthcare services are provided at minimal costs, but quality can be a concern. Many Egyptians rely on government-sponsored insurance programs, while others, particularly in rural areas, face challenges accessing adequate healthcare due to geographical constraints and limited infrastructure. Out-of-pocket payments are common, impacting affordability. In rural settings, healthcare accessibility is often hindered by insufficient facilities and transportation, exacerbating disparities. The government is working on healthcare reform initiatives, yet rural areas continue to grapple with unique challenges in accessing and affording quality care.
We aimed to promote the health of women's bodies and minds in the childbearing period by detecting the prevalence, different types, and factors associated with abused women compared to non-abused women in the same category from October 2021 to December 2021 in primary healthcare facilities in rural Ismailia Egypt.
Methods
Study setting and material
Study design: From October 2021 to December 2021, primary healthcare facilities in rural Ismailia, Egypt, undertook a cross-sectional study.
Study population: Adult females attending antenatal, family planning and child health care clinics in the primary health care unit.
Inclusion criteria: Married women in childbearing period (aged 18–50 years).
Exclusion criteria-:
-
1.
Women refused to participate in the study.
-
2.
Never married females.
-
3.
Women have a mental disability or chronic psychiatric disorders which interfere with interview.
Sample size: The amount of data collected, as determined by the equation below:
n = (Z/SE)2 x p x(1-p) [7] n = Sample size, p = the percentage of Egyptian women who had ever been married who reported having experienced any type of violence was 29.4% [8], z = Percentile of the standard normal distribution which equals 1.96% and 95% confidence level. SE =0.05.
Sample size (n) = (1.96/0.05) 2 × 0.5 (1–0.5) = 317 women, add dropout (10%), so the total number will be 349 women.
Sampling technique: stratified random sampling methods were used to choose the participants. Three working days a week, specifically Sundays, Mondays, and Thursdays, are yielded at random by the lottery approach. Then, every 4th eligible participant was selected.
Tools of data collection: semi-structure interview questionnaire containing the following data:
First part: Demographic data related to married women as age, marital status, income, occupation, education, address, social class, and presence of chronic diseases. Demographic data related to the husband as age, income, chronic diseases, educational levels and drug addiction and abuse.
Second part: Designed Scale to detect the history of exposure to abuse and types of abuse either physical, emotional or sexual (Unwanted sexual contact, nonconsensual sex that was both completed and attempted and unwanted sexual situations) and its frequencies were conducted to the abused group [9].
Third part: Assessment of anxiety disorders by using the validated and reliable Arabic version of the anxiety checklist [10]. It contains 14 questions with responses ranging from 0 to 5 (0 = have no symptoms, (1) Mild, (2) Moderate, (3) Severe, and (4) Extremely Severe symptoms. A score of 14 or less indicates mild anxiety, 18 to 24, mild to moderate, and 25 to 30 indicates moderate to severe anxiety. The total scores ranged from 0 to 56. [11]. A pilot sample was done on 20 individuals who were not included in the study population and any modification had been done. The questionnaire utilized in this study is available in Fig. S1 and Fig. S2..
Well-trained physicians were interviewed at the Family Health Unit (FHU) in a dedicated and private room during regular working hours on three selected days, spanning from 9 AM to 2 PM, within the timeframe of October to December 2021. To ensure the utmost privacy and confidentiality for the participants, the interviews were conducted in a separate room away from the routine clinical areas. Before the interviews, participants were informed about the voluntary nature of their involvement, and explicit consent was obtained. Additionally, all personal identifiers were anonymized, and any data collected were securely stored to prevent the disclosure of individual participants' information.
were.
Data Management and Analytical Statistics: Using SPSS software, version 25 (IBM Inc., Chicago, IL, USA), data were entered and analyzed. Using the Kolmogorov-Smirnov test, the normality of the data was determined. Categorical data were shown as percentages and numbers. Range (minimum and maximum), mean, standard deviation, and median were used to express quantitative data. Two groups were compared using the chi-square test (χ2) for qualitative factors. If >20% of the cells have an expected count of <5, the Monte Carlo correction test was instead used. A t-test for parametric variables and the Mann-Whitney U test for non-parametric variables were used to compare quantitative variables between groups. To find the factor affecting anxiety that is most independently influenced, a logistic regression analysis was used.
Participant consent and ethics approval
The study received ethical approval number 002 from the Port-Said University Faculty of Medicine's Ethics and Clinical Research Committee. After outlining the study's aims and objectives, each participant provided their written informed consent. The subjects of the study were made aware of their right to discontinue the investigation at any time. The participants' confidentiality was protected. Data was collected at suitable times to avoid any interference with participant's flow of work or schedules. Participants have been informed of the study results.
Results
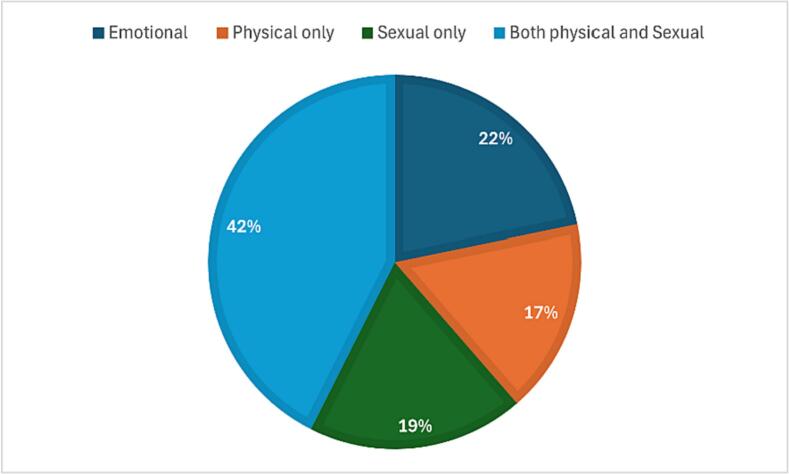
The study population included 350 women in the reproductive age group attending the family health unit to evaluate the types and frequency of domestic violence as well as the anxiety levels of women who have been abused versus those who have not. The study's women had a mean age of 32.3 ± 8.1 years, more than two-thirds of them were educated to the secondary school level, most of them are housewives (86%) and residents in a rural area, the mean number of parities was 2. About one-third live in extended family (22%), nearly one-quarter of them have chronic diseases and about half of studied women revealed she has sufficient income Table 1. The mean age of the husbands was 37. Most of them are working and educated at the secondary school level. More than two-thirds of the husbands smoke. More than a quarter of them use stimulating drugs. The husband's use of stimulant drugs was a risk factor for abuse. Table S1. Regarding the prevalence of domestic violence in the studied population, less than half of the studied women revealed that they are exposed to domestic violence (41%). Regarding types of abuse, less than half of them were exposed to both physical and sexual abuse (43%). While about one-third of them were exposed to physical abuse alone and one-fourth of them were exposed to sexual abuse alone. The most predominant sexual abuse was practice without consent (63%) followed by undesired position as shown in Table 2 and Fig. 1. More than three-quarters of women show anxiety symptoms. The predominance was mild degree 47% followed by mild to moderate 18% then moderate to severe 6% and severe degree 5.7. Table S2 women who experienced violence were more prone to anxiety, and this difference between the two groups was statistically significant. About 12% of abused women complain of severe forms of violence compared only to 1.5 of non-abused women. The total score of anxiety was higher in abused women (16.9 ± 10.8) compared with non-abused (6.9 ± 8.6). Table S3 an analysis of multivariate logistic regression was done to determine parameters affecting anxiety symptoms in the studied sample. The significant predictors for anxiety in the total sample were the increase in age of women (OR = 1.1(1.0–1.2), rural residence (OR 2.9 (1.1–7.2), and exposure to abuse (OR = 11.2 (4.9–25.4). We found a change in direction of the influence of the husband's age on domestic violence. Initially identified as a risk factor in the univariate model, OR = 1.0 (p = 0.009), the direction changed to being a protective factor in the multivariable model, OR = 0.9 (p = 0.019). This could imply that when considering other factors simultaneously in the model, the age of the husband may interact differently with other variables, influencing the outcome. Table 3 A single- and multiple-variable regression analysis was conducted to identify parameters that affected domestic violence in the studied sample, residents in separate homes, the increase in the number of rooms, and the husband's use of stimulant drugs are the most predictor factor for abusing women, while the sufficient income of the family was protective against violence (OR = 0.4 (0.3–0.7) Table S4.
Table 1.
shows the distribution of the study sample's socio-demographic characteristics of the study participants.
| Socio-demographic characteristics of women | Total (n = 350) |
Abuse |
Test of Sig | p | |
|---|---|---|---|---|---|
| No (n = 206) |
Yes (n = 144) |
||||
| Age | |||||
| Mean ± SD. | 32.3 ± 8.1 | 32.4 ± 8.8 | 32.3 ± 7.1 | U = 14,569.5 |
0.778 |
| Median (Min. – Max.) | 32 (16–55) | 31 (16–55) | 32 (17–50) | ||
| Occupation | |||||
| Working | 99 (28%) | 53 (26%) | 46 (32%) | χ2 = 1.615 | 0.204 |
| Housewife | 251 (72%) | 153 (74%) | 98 (68%) | ||
| Education | |||||
| Not educated | 28 (8%) | 19 (9%) | 9 (6%) | χ2 = 5.534 | 0.237 |
| Read and write | 23 (7%) | 13 (6%) | 10 (6%) | ||
| Secondary education | 211 (60%) | 122 (59%) | 89 (62%) | ||
| Graduate | 82 (23%) | 46 (22%) | 36 (25%) | ||
| Postgraduate | 6 (1%) | 6 (3%) | 0 (0%) | ||
| Residence | |||||
| Rural | 304 (87%) | 183 (89%) | 121 (84%) | χ2 = 1.716 | 0.190 |
| Urban | 46 (13%) | 23 (11%) | 23 (16%) | ||
| Gravidity | |||||
| 0 | 1 (0.3%) | 0 (0.0%) | 1 (0.7%) | χ2 = 6.364 |
MCp = 0.071 |
| 1 | 66 (19%) | 46 (22%) | 20 (14%) | ||
| 2 | 76 (22%) | 39 (19%) | 37 (26%) | ||
| >2 | 207 (59%) | 121 (59%) | 86 (60%) | ||
| Mean ± SD. | 2.71 ± 1.20 | 2.6 ± 1.2 | 2.8 ± 1.2 | U = 13,843.5 |
0.271 |
| Median (Min. – Max.) | 3 (0–6) | 3(1–6) | 3 (0–6) | ||
| N of children | |||||
| Mean ± SD. | 2.6 ± 1 | 2.5 ± 1.1 | 2.6 ± 1 | U = 14,188.0 |
0.471 |
| Median (Min. – Max.) | 3 (0–6) | 3 (1–6) | 3 (0–5) | ||
| N of rooms | |||||
| Mean ± SD. | 2.5 ± 0.6 | 2.4 ± 0.6 | 2.5 ± 0.6 | U = 12,924.5⁎ |
0.021⁎ |
| Median (Min. – Max.) | 2 (1–4) | 2 (1–4) | 3 (1–4) | ||
| Separate home | |||||
| Yes | 272 (78%) | 170 (83%) | 102 (71%) | χ2 = 6.689⁎ | 0.010⁎ |
| No | 78 (22%) | 36 (18%) | 42 (29%) | ||
| Chronic disease | |||||
| Yes | 43 (12%) | 20 (10%) | 23 (16%) | χ2 = 3.085 | 0.079 |
| No | 307 (88%) | 186 (90%) | 121 (84%) | ||
| Income | |||||
| Sufficient | 193 (55%) | 100 (49%) | 93 (65%) | χ2 = 8.815⁎ | 0.003⁎ |
| Not | 157 (45%) | 106 (52%) | 51 (35%) | ||
SD; Standard deviation, χ2; Chi-square test, U; Mann WhitneyU test, p: p -value for contrasting abuse and no abuse, Significant statistically at p 0.05.
Table 2.
The studied sample's distribution by type of abuse.
| Type of abuse | No. (%) |
|---|---|
| No | 206 (59%) |
| Yes | 144 (41%) |
| Type of abuse | |
| Physical only | 24 (16%) |
| Sexual only | 27 (19%) |
| Both Physical and Sexual | 62 (43%) |
| Emotional | 31 (22%) |
| Physical abuse | |
| Yes | 117 (33%) |
| No | 233 (67%) |
| Frequency of abuse | (n = 117) |
| Mean ± SD. | 4.41 ± 4.27 |
| Median (Min. – Max.) | 3 (1−30) |
| Sexual abuse | |
| Yes | 89 (25%) |
| No | 261 (75%) |
| Type of sexual abuse | (n = 89) |
| Undesired position | 23 (25%) |
| Undesired touch | 16 (18%) |
| Practice without consent | 56 (63%) |
| End the relation without consent | 20 (23%) |
| Physical abuse during relation | 21 (24%) |
SD: Standard deviation.
Fig. 1.
Distribution of the studied sample according to type of abuse.
Table 3.
Analysis of the parameters affecting anxiety using both single- and multiple-variable logistic regression (n = 350).
| Cases (N) |
Control (N) |
Univariate |
#Multivariate |
|||
|---|---|---|---|---|---|---|
| p |
Adjusted OR 95% confidence interval |
p |
AdjustedOR 95% confidence interval |
|||
| Socio -economic about wife | ||||||
| Age | – | – | 0.001⁎ | 1.06 (1.02–1.09) | 0.008⁎ | 1.12 (1.03–1.22) |
| Working | 46 | 53 | 0.432 | 0.8 (0.5–1.4) | 0.312 | 1.3 (0.4–4.1) |
| Education | ||||||
| Not educated | 9 | 19 | 0.020⁎ | 4.5 (1.3–16.2) | 0.114 | 3.4 (0.7–15.9) |
| Read and write | 101 | 13 | 0.968 | 1.0 (0.4–2.7) | 0.300 | 0.5 (0.1–1.8) |
| Secondary education | 89 | 122 | 0.003⁎ | 2.3 (1.3–4.1) | 0.177 | 1.6 (0.8–3.7) |
| Graduate + Post graduate® | – | – | – | – | – | – |
| Rural residence | 121 | 183 | 0.003⁎ | 2.6 (1.4–5.2) | 0.020⁎ | 2.9 (1.2–7.2) |
| Gravidity | 144 | 206 | 0.001⁎ | 1.4 (1.2–1.8) | 0.751 | 0.9 (0.5–1.6) |
| N of children | – | – | 0.001⁎ | 1.5 (1.2–1.9) | 0.264 | 1.4 (0.8–2.6) |
| N of rooms | – | – | 0.002⁎ | 1.9 (1.3–3.1) | 0.157 | 1.4 (0.9–2.5) |
| Separate home | 102 | 170 | 0.699 | 0.8 (0.5–1.6) | 0.213 | 0.2 (0.7–2.3) |
| Chronic disease | 232 | 20 | 0.722 | 0.8 (0.4–1.8) | 0.112 | 0.7 (0.5–1.3) |
| Income (Not sufficient) | 51 | 106 | 0.956 | 0.9 (0.6–1.6) | 0.122 | 0.4 (0.3–1.4) |
| Socio-economic about husband | ||||||
| Age | – | – | 0.009⁎ | 1.04 (1.01–1.08) | 0.019⁎ | 0.91 (0.84–0.99) |
| Not working | 45 | 27 | 0.077 | 3.7 (0.9–16.3) | 0.521 | 1.3 (0.3–2.4) |
| Education | ||||||
| Not educated | 33 | 21 | 0.697 | 1.2 (0.4–3.9) | 0.133 | 0.3 (0.7–1.4) |
| Read and write | 24 | 27 | 0.604 | 1.4 (0.3–5.8) | 0.654 | 0.6 (0.1–3.9) |
| Secondary eduation | 12 | 26 | 0.023⁎ | 1.9 (1.1–3.4) | 0.743 | 1.1 (0.5–2.6) |
| Graduate® | – | – | – | – | – | – |
| Smoking | 28 | 21 | 0.946 | 1.0 (0.6–1.7) | 0.142 | 1.1 (0.2–2.3) |
| Stimulant drugs | 19 | 12 | 0.005⁎ | 2.6 (1.3–5.2) | 0.131 | 1.9(0.8–4.6) |
| Abuse | 21 | 19 | <0.001⁎ | 8.2 (3.9–17.1) | <0.001⁎ | 11.2 (4.9–25.4) |
OR: Odd's ratio.
®: Reference group.
Discussion
Gender-based violence is the human rights violation and a global issue of public health. It affects people of all genders, but women and girls are disproportionately affected. In this study 350 women were included to detect physical, sexual and psychological abuse. About half of the studied women revealed she has sufficient income. Approximately similar results were found, in a cross-sectional study about domestic violence against women. Domestic violence is strongly linked to the husband, according to the majority of studies tetrahydrocannabinol consumption, khat chewing in different countries in an Africa, synthetic cannabinoids, Tramadol and Marijuana abuse as well as Datura abuse [12]. The convergence between the results of both studies may be due to substance abuse consumption especially stimulating abuse increases aggression and irritability, making a person more likely to act out violently, as violence against women is often about exerting power and control over the victim. Tetrahydrocannabinol and central nervous system (CNS) stimulant substance abuse use can be used as a tool to reinforce this power dynamic and maintain control over the victim [13]. Our study showed that less than half of studied women are exposed to domestic violence (41%). Regarding the type of abuse less than half of them were exposed to both physical and sexual abuse (43%). About a third of them exposed to physical abuse alone and a fourth of them were exposed to sexual abuse alone. The most predominant sexual abuse was practiced against their well followed by undesired position. Our findings agree with another study conducted among married women in the Arab countries which reported half of the participants were exposed to every form of violence [14]. However, it was high compared to the rate previously reported by Egypt Demographic and Health Survey, 2014 (EDHS) in Egypt (30%) among ever-married women aged 15–49 [15].
A cross-sectional community-based study of 1104 women in Ethiopia, conducted from March to April 2003, found an overall prevalence of 50, 8% of women who had experienced physical, sexual, or psychological abuse in their lifetime. Three hundred and fifty-five (32%) women reported experiencing physical violence at some point in their lives. Thirty-five (30.5%) reported experiencing physical assault in the past six months. About 200 (19%) of the interviewees said they were forced to have sex with their partners, about 194 people (17%) were forced to get pregnant, and about 56 people (5%) reported they were forced to terminate a pregnancy. About 46% of physical abuse victims reported rape [16].. The results of the two studies are slightly different, the incidence of both sexual and physical abuse violence in our study was, however, smaller than that of Northwest Ethiopia. The observed variations in reported rates of sexual violence may be attributed to several factors, including differences in the definitions of sexual violence employed across studies. Variability in cultural norms and societal perceptions of what constitutes sexual abuse can influence individuals' willingness to disclose such experiences. Additionally, discrepancies in the characteristics of the studied populations, such as socio-cultural backgrounds, economic status, and educational levels, can contribute to divergent findings. Overall, the prevalence of this condition is very high physical and sexual violence against women may be a result of cultural norms as in some cultures; violence against women is seen as acceptable or even encouraged. This can include practices such as female genital mutilation or forced marriage. In our paper, more than three-fourths of women show anxiety symptoms. The predominance was mild degree (46%) followed by mild to moderate (18%) then moderate to severe (5%) and sever degree (5%). Results show that the relation between anxiety symptoms and women abuse in the studied sample is highly significant. In a cross-sectional study that was conducted in Tunisia about Women's mental health: acute impact of COVID-19 pandemic on domestic violence, using an online survey, between April 25 and May 6, 2020 (n = 751), during lockdown, the incidence of violence against women rose by 4.4–14.8 percentage points. Women who reported experiencing violence during lockdown also had higher scores for depression, anxiety and stress. About 85% of women reported experiencing anxiety, depression symptoms and stress. [12]. >50% of participants reported severe symptoms for all three axes on the (DASS-21) depression anxiety and stress scale. Those with a pre-existing history of mental health disorders and abuse were associated with more severe depression, anxiety and stress symptoms. Women who were abused prior to the lockdown were associated with a higher risk for violence during lockdown. [12] In the current study, although most of the participants showed anxiety symptoms as a result of exposure to violence, most of their symptoms were mild to moderate symptoms, on the other hand, the results of the Tunisian study show a difference from our study, as most of their participants show severe depressive and anxiety symptoms, the additional effect of COVID-19 lockdown may explain the difference between results of the two studies. A second study on the impact of Domestic Violence on Anxiety, Depression and Quality of Life of Pakistani Women was carried out in the population of all female patients who had been victims of Domestic Violence (n = 116) from January 2019–December 2019 in Rawalpindi IHS (Institute of Health Sciences). The results of this study showed a strong positive correlation between verbal, Physical, Emotional and Sexual Domestic Violence on Anxiety, Depression and Stress, as well as a negative relationship between Domestic Violence and Quality of Life. [17] According to these three studies, women who are victims of domestic violence are more likely to develop anxiety and depression than those who have not experienced such violence. The physical and emotional trauma of domestic violence can cause a woman to feel overwhelmed, anxious, and fearful, which can lead to depression. [17,16,15] In this study regarding parameters affecting anxiety symptoms in women in the studied sample, the most predictor factor is women abuse. Other predictor factors as the age of the wife, the age of the husband and the residence.
Ethiopia's study looked at mental distress and related factors among 423 female participants in South Ethiopia who had experienced gender based violence (GBV) and were attending court. The overall prevalence of women with mental distress attending court after GBV was 59%, with a 95% confidence interval (95% CI) of 55.1–64.2. Factors such as husband's substance use, social support, formal education, lifestyle in rural areas, age (33 years and above) and monthly income (<698) were all significantly related to mental distress. [17] The approximate similarity between parameters affecting anxiety symptoms in our study and the study that was conducted in Ethiopia may be due to the convergence in a number of studied populations and the slight similarity between African countries in customs and traditions. In our paper, regarding parameters affecting domestic violence in the studied sample, the insufficient income of the family and the use of stimulant drugs are the most predictor's factors for abusing women followed by staying in separated homes and number of rooms per home.These findings were consistent with other studies [[18], [19], [20], [21], [22], [23]] The correlation between sexual violence and substance abuse by the husband could be explained by the fact that Dopamine is the neurotransmitter responsible for the regulation of pleasure (e.g. euphoria and satisfaction) and is directly and indirectly influenced by stimulants. Stimulation also causes the release of the neurotransmitter Norepinephrine in the brain. Norepinephrine is involved in mood regulation, attention and learning, memory and arousal regulation, and may be involved in substance withdrawal. [24] The majority of the studies found that Domestic Violence is significantly related to Husband's Alcohol Consumption, Khat Chewing, Partner Education, Residence (Rural women are more likely to be victims of Violence), and Women Under 18 at First Sex or Marriage become victims of Violence. Women's literacy is negatively related to Domestic Violence and increases the risk of Violence. Housewives are less likely to report Sexual Violence than working women. [13] Women's Income and Risk of Intimate Partner Violence (IPV): A Randomized, Compound Trial in North-West Tanzania (n = 740) found that women in the highest quartiles of income had a lower risk of experiencing physical IPV compared to those in the lowest quartile. However, the lowest risk was found in women who were not employed at all. [25] Approximately the three studies agreed on the same parameters affecting domestic violence, emphasizing that domestic violence against women is a complex issue and these factors are not exclusive predictors, and many other factors may increase the risk of women being victims of domestic violence. [17,16,15] It's also essential to recognize that domestic violence is never the victim's fault, and the responsibility lies solely with the perpetrator.
Study limitation
Our study has several limitations that warrant consideration. First, the use of a one-year recall for violence introduces the potential for recall bias, as the accuracy of recall may vary, and mental health unrelated to violence experience can impact reporting. Second, selection bias may arise from limiting participation to married women within a specific age range, neglecting insights into violence against unmarried and divorced women. Third, unmeasured confounding variables could introduce bias to reported associations. Fourth, outcome mismeasurement concerns include the accuracy of depression and anxiety assessment relative to clinical diagnosis and potential underreporting or overreporting risks of Covid-19 period. Fifth, the use of a one-year timeframe for abuse measurement raises concerns about the temporal precision of reported incidents. Lastly, subgroup analyses, particularly stratification by age, were not extensively explored, leaving potential differences unexamined. Addressing these limitations is crucial for a more nuanced interpretation of study findings.
Recommendation
Screening for domestic violence among women attending primary health care, particularly in rural areas, is crucial, given the documented prevalence in our study. However, it is essential to consider existing screening practices and their effectiveness before implementing new measures. Evaluating the current screening protocols and understanding their limitations can provide valuable insights for improvement. Additionally, raising awareness among family physicians about the importance of mental health screening is vital. Assessing the current extent of such awareness and identifying gaps can guide targeted educational interventions. Furthermore, community awareness programs should emphasize the impact of stimulants and illegal drugs on families, aligning with the need for tailored interventions based on prevailing substance abuse patterns within the community.
Conclusion
In this study, we found that less than half of the women reported exposure to domestic violence, with physical and sexual abuse being prevalent. Anxiety symptoms were notably high, primarily of mild to moderate intensity, and significantly associated with experiences of abuse. Husband's substance use and insufficient family income emerged as key predictors of domestic violence. Our findings underscore the importance of routine screening for domestic violence in primary healthcare, particularly in rural settings, and highlight the need for heightened awareness regarding stimulant and illegal drug use within communities.
Funding
The research was not financed by any funding agency.
CRediT authorship contribution statement
Almaza A. Salim: Supervision, Investigation, Conceptualization. Mona Elsayed: Writing – review & editing, Writing – original draft, Formal analysis. Heba Yousef: Writing – original draft, Visualization, Validation. Mohamed S. Hemeda: Writing – review & editing, Writing – original draft, Formal analysis. Alaa Ramadan: Writing – review & editing, Writing – original draft. Nathan Ezie Kengo: Writing – review & editing, Writing – original draft. Noha M. Abu Bakr Elsaid: Supervision.
Declaration of competing interest
The authors did not declare any conflicts of interest related to the field of study, authorship, or publication of this article.
Acknowledgement
We would like to extend our sincere thanks to all the women who took part in this study.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.gloepi.2024.100139.
Contributor Information
Almaza A. Salim, Email: Almaza.Ali@med.psu.edu.eg.
Heba Yousef, Email: Heba.mohamed@med.psu.edu.eg.
Mohamed S. Hemeda, Email: mohamudsadawy@med.psu.edu.eg.
Nathan Ezie Kengo, Email: kengonathan6@gmail.com.
Noha M. Abu Bakr Elsaid, Email: Noha.abubakr@med.suez.edu.eg.
Appendix A. Supplementary data
Supplementary material
References
- 1.Alesina Alberto, Brioschi Benedetta, La Ferrara Eliana. Violence against women: a cross-cultural analysis for Africa. 2016. http://www.nber.org/papers/w21901
- 2.Kawuki Joseph, Sserwanja Quraish, Mukunya David, et al. Sexual violence is a serious global health problem with short- and long-term physical, mental, and reproductive adverse effects. Public Health. 2021;196, July 2021:35–42. doi: 10.1016/j.puhe.2021.05.004. [DOI] [PubMed] [Google Scholar]
- 3.Malik Mazhar, Munir Nargis, Ghali M. Usman, et al. Domestic violence and its relationship with depression, anxiety and quality of life: A hidden dilemma of Pakistani women. Pakistan J Med Sci. 2021;37(1):191–194. doi: 10.12669/pjms.37.1.2893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brenisen Loss of Agency: How Domestic Violence impacts Mental Health. Women Advocat. 2020;2020 [Google Scholar]
- 5.National Institute on Drug Abuse . 2018, July. The science of drug use and addiction: The basics. https://www .drugabuse .gov/publications/media-guide /science-drug-use-addiction-basics [Reference list] [Google Scholar]
- 6.Koob & Volkow 2016, neurobiology of addiction: a neurocircuitry analysis. Lancet Psychiatry. August 2016;3(8):760–777. doi: 10.1016/S2215-0366(16)00104-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ratian J., Hochbbege M. Clinical tial:Aguide to understanding and interpreting results. Arthritis Rheum. 1990;1990(33):131. doi: 10.1002/art.1780330118. [DOI] [PubMed] [Google Scholar]
- 8.Yaya S., Hudani A., Buh A., Bishwajit G. Prevalence and predictors of intimate partner violence among married women in Egypt. J Interpers Violence. 2021;36(21−22):10686–10704. doi: 10.1177/0886260519888196. [DOI] [PubMed] [Google Scholar]
- 9.Basile K.C. In: Handbook of women, stress, and trauma. Kendall-Tackett K., editor. Brunner-Routledge; New York: 2005. Sexual violence in the lives of girls and women; pp. 101–122. [Google Scholar]
- 10.Souheil H., Chahine M., Salameh P., Haddad C., Sacre H., Soufia M., et al. Suicidal ideation among Lebanese adolescents: scale validation, prevalence and correlates. BMC Psychiatry. 2024;20(1):1–11. doi: 10.1186/s12888-020-02726-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Maier W., Buller R., Philipp M., Hamilton Heuser. Anxiety Scale:reliability,validity and sensenvity to change in anexity ad depressive disorders. J Affect Disord. 1988;14(1):61–68. doi: 10.1016/0165-0327(88)90072-9. [DOI] [PubMed] [Google Scholar]
- 12.Semahegn A., Mengistie B. Domestic violence against women and associated factors in Ethiopia; systematic review. Reprod Health. 2015 Aug;29(12):78. doi: 10.1186/s12978-015-0072-1. PMID: 26319026; PMCID: PMC4553009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Avois L., Robinson N., Saudan C., Baume N., Mangin P., Saugy M. Central nervous system stimulants and sport practice. Br J Sports Med. 2006;40(Suppl. 1) doi: 10.1136/bjsm.2006.027557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.El-Nimr N.A., Mamdouh H.M., Ramadan A., El Saeh H.M., Shata Z.N. Intimate partner violence among Arab women before and during the COVID-19 lockdown. J Egypt Public Health Assoc. 2021;96(1):15. doi: 10.1186/s42506–021-00077-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ministry of Health and Population [Egypt], El-Zanaty and Associates [Egypt], and ICF International Egypt Demographic and Health Survey 2014. Cairo and Rockville: Ministry of Health and Population and ICF International. 2015. https://www.unicef.org/egypt/reports/egypt-demographic-and-health-survey-2014 Available from: [Cited 16 Oct 2021]
- 16.Yigzaw T., Yibric A., Kebede Y. Domestic violence around Gondar in Northwest Ethiopia. Ethiopian J Health Develop. 2005;18(3) doi: 10.4314/ejhd.v18i3.9846. [DOI] [Google Scholar]
- 17.Malik M., Munir N., Ghani M.U., Ahmad N. Domestic violence and its relationship with depression, anxiety and quality of life: a hidden dilemma of Pakistani women. Pakistan J Med Sci. 2021;37(1):191–194. doi: 10.12669/pjms.37.1.2893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barnawi F.H. Prevalence and risk factors of domestic violence against women attending a primary care center in Riyadh. Saudi Arabia J Inter-pers Violen. 2017;32(8):1171–1186. doi: 10.1177/0886260515,587669. [DOI] [PubMed] [Google Scholar]
- 19.Abo-Elfetoh N.M., Abd El-Mawgod M.M. Violence against wives: a silent suffering in northern Saudi community. J Egypt Public Health Assoc. 2015;90(3):87–93. doi: 10.1097/01.EPX.0000467223.22719.36. [DOI] [PubMed] [Google Scholar]
- 20.Guimei M., Fikry F.E., Esheiba O.M.A.E. Patterns of violence against women in three communities in Alexandria, Egypt MCN. Am J Matern Child Nurs. 2012;37(5):331–338. doi: 10.1097/NMC.0b013e31825c99d8. [DOI] [PubMed] [Google Scholar]
- 21.Mohamadian F., Hashemian A., Bagheri M., Direkvand-Moghadam A. Prevalence and risk factors of domestic violence against Iranian women: a cross-sectional study. Korean J Fam Med. 2016;37(4):253–258. doi: 10.4082/kjfm.2016.37.4.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ali R., Radwan R. Magnitude and determinants of domestic violence against ever married women in Sohag, Egypt. Int J Med Sci Public Health. 2017:1. doi: 10.5455/ijmsph.2017.0513307062017. [DOI] [Google Scholar]
- 23.Sarkar M. A study on domestic violence against adult and adolescent females in a rural area of West Bengal. Indian J Community Med. 2010;35(2):311–315. doi: 10.4103/0970-0218.66881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.National Center for Chronic Disease Prevention and Health Promotion (US) office on smoking and health. The health consequences of smoking – 50 years of Progress: A report of the surgeon general. Centers for Disease Control and Prevention; Atlanta (GA): 2014. http://www.ncbi.nlm.nih.gov/books/NBK179276/.Data [Brief 294. Drug Overdose Deaths in the United States, 1999–2016] [PubMed] [Google Scholar]
- 25.Abramsky T., Lees S., Stöckl H., et al. Women’s income and risk of intimate partner violence: secondary findings from the MAISHA cluster randomized trial in North-Western Tanzania. BMC Public Health. 2019;19:1108. doi: 10.1186/s12889-019-7454-158. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material